Abstract
Simple Summary
The challenging early detection of cholangiocarcinoma and the limited availability of less-invasive anticancer therapies contribute to its poor prognosis. Some highly targeted therapies have been explored for cholangiocarcinoma, such as antibody-drug conjugates (ADCs), photodynamic therapy (PDT) with/without systemic chemotherapy, and experimental photoimmunotherapy (PIT). PIT stands out as a novel and promising therapy with less invasiveness; however, it has not yet been performed in human cases of cholangiocarcinoma. In this article, we focus on and review ADC, PDT, and PIT as highly targeted therapies, including experimental therapies for cholangiocarcinoma, and indicate their future prospects.
Abstract
To overcome the poor prognosis of cholangiocarcinoma (CCA), highly targeted therapies, such as antibody-drug conjugates (ADCs), photodynamic therapy (PDT) with/without systemic chemotherapy, and experimental photoimmunotherapy (PIT), have been developed. Three preclinical trials have investigated the use of ADCs targeting specific antigens, namely HER2, MUC1, and glypican-1 (GPC1), for CCA. Trastuzumab emtansine demonstrated higher antiproliferative activity in CCA cells expressing higher levels of HER2. Similarly, “staphylococcal enterotoxin A-MUC1 antibody” and “anti-GPC1 antibody-monomethyl auristatin F” conjugates showed anticancer activity. PDT is effective in areas where appropriate photosensitizers and light coexist. Its mechanism involves photosensitizer excitation and subsequent reactive oxygen species production in cancer cells upon irradiation. Hematoporphyrin derivatives, temoporfin, phthalocyanine-4, talaporfin, and chlorine e6 derivatives have mainly been used clinically and preclinically in bile duct cancer. Currently, new forms of photosensitizers with nanotechnology and novel irradiation catheters are being developed. PIT is the most novel anti-cancer therapy developed in 2011 that selectively kills targeted cancer cells using a unique photosensitizer called “IR700” conjugated with an antibody specific for cancer cells. PIT is currently in the early stages of development for identifying appropriate CCA cell targets and irradiation devices. Future human and artificial intelligence collaboration has potential for overcoming challenges related to identifying universal CCA cell targets. This could pave the way for highly targeted therapies for CCA, such as ADC, PDT, and PIT.
Keywords: cholangiocarcinoma, biliary tract cancer, antibody-drug conjugate, photodynamic therapy, photoimmunotherapy
1. Introduction
The biliary tree is complicated and finely branched into the liver, which is anatomically classified into small intrahepatic (ϕ20–300 μm), large intrahepatic (300–800 μm), and extrahepatic (>800 μm) bile ducts, including the gallbladder [1]. Its numerical bifurcations can cause difficulty in the detection of and approach to early biliary lesions, especially in the periphery, leading to a poor prognosis of cholangiocarcinoma (CCA), with a 5-year relative survival rate of 7–20% [2,3,4]. To improve prognosis, novel therapeutic approaches to CCA are necessary.
There have been a number of clinical and basic studies on CCA regarding etiology, clinicopathology, molecular biology, and immunology that have clarified the characteristics and targeted points of CCA to some extent. Currently, there are six primary modalities of anticancer treatment for CCA: (1) surgical therapy; (2) chemotherapy; (3) radiotherapy, including brachytherapy and proton radiotherapy; (4) immunotherapy, including immune checkpoint inhibitor and chimeric antigen receptor (CAR) T-cell therapy, (5) phototherapy, and (6) combination therapy, such as antibody-drug conjugate (ADC) therapy (2 + 4), photodynamic therapy (PDT; 2 + 5), and photoimmunotherapy (PIT; 4 + 5). Surgical therapy has developed with the increase in skilled surgeons, high-resolution imaging modalities, and the introduction of portal vein embolization [5]. Chemotherapy has been developed with an understanding of the biology and molecular mechanisms of CCA [6]. Radiotherapy has also improved with internal small, sealed sources [7,8] and proton beams [9], mainly with palliative and supportive intent. Immunotherapy has evolved and improved with the advent of immune checkpoint inhibitors, such as durvalumab (a PD-L1 antibody) [10] and CAR-T therapy [11]. Among them, highly targeted therapies such as ADC, PDT, and PIT are attracting much attention for precision medicine because of their expected high effectiveness and low invasiveness.
To provide highly targeted therapies, previous researchers revealed that CCA abnormally expresses some possible antigens/targets or molecules on the cell surface, such as epidermal growth factor receptor (EGFR), HER2 (c-erbB-2), and vascular endothelial growth factor receptor (VEGFR) [12].
In addition, recent genetic investigations of biliary tract cancer have revealed a range of genetic mutations and alterations specific to the primary cancer site. These include fibroblast growth factor receptor-2 (FGFR2) fusion and IDH1/2 in intrahepatic CCA (ICC); HER2 (erbB-2), PRKACA, and PRKACB in extrahepatic CCA (ECC: perihilar and distal CCA); EGFR, ERBB3, and PTEN in gallbladder cancer; and KRAS, SMAD4, and TP53 shared in ICC and ECC [13,14]. Some of these genetic mutations are also common in pancreatic cancer, which is attributed to the adjacent embryologic relationship between the biliary tree and pancreas [15]. These genetic variations often present challenges and emphasize the importance of implementing precision medicine approaches tailored to the specific cancer site.
Here, we focus on and review three types of highly targeted therapies (ADC, PDT, and PIT), including experimental and promising ones, and indicate their future prospects.
2. Antibody-Drug Conjugate
Antibody-drug conjugate (ADC) was developed as a novel drug delivery system for achieving more specific effects on targeted cancer cells and fewer adverse effects on non-targeted normal cells. The first concept of ADC was proposed by Paul Enrlich as a “magic bullet” in 1910 [16], and the first successful conjugation of an antibody and a drug was realized by Mathe et al. in 1958 [17]. The first ADC for malignancy, gemtuzumab ozogamicin, developed for the treatment of acute myeloid leukemia, was approved in 2000 by the US Food and Drug Administration. Since then, 13 other ADCs have been approved for hematological malignancies, such as leukemia and lymphoma (six ADCs), and solid tumors, such as breast cancer and gastric cancer (seven ADCs). Unfortunately, ADCs for CCA have not yet been approved. At present, over 100 ADC candidates have been investigated in clinical stages.
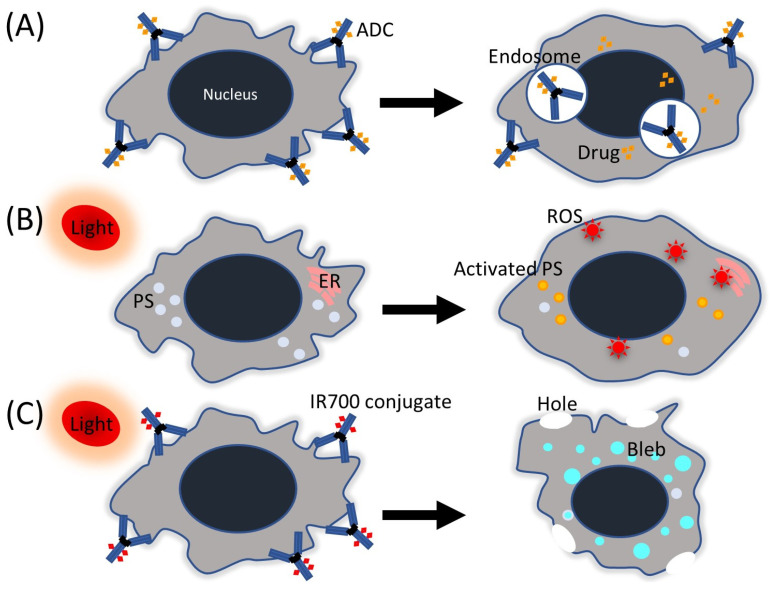
ADC comprises: (1) an antibody against targets expressed on tumor cells, (2) a cytotoxic drug called “payload”, and (3) a linker that connects the two. The relative proportions of these three components can vary among ADCs. Among the four subclasses of antibodies, namely IgG1–4, IgG1 is predominantly employed in ADCs due to its extended serum half-life, which is comparable to that of IgG2 and IgG4 (21 days), but longer than that of IgG3 (7–21 days). Additionally, IgG1 exhibits superior complement-fixation and FcγR-binding capabilities compared to the other subclasses [18,19]. FcγR promotes phagocytosis, the release of inflammatory mediators, and antibody-dependent cytotoxicity by effector cells. The mechanism of action of ADCs is more complex than most clinicians believe, often requiring ADC internalization, followed by intracellular processing and payload release (Figure 1A). In detail, the mechanism can be explained in six phases: (1) ADCs circulate as three components. (2) As they diffuse slowly towards target cells, ADCs can release some payload into the tumor microenvironment. (3) Antibody engagement leads to payload-independent antitumor activity via several mechanisms (Fc-mediated stimulation of immune cell effector function and disruption of downstream signaling). (4) Most ADCs are internalized and processed (acidic or proteolytic cleavage of the ADC), largely via antigen-dependent pathways; (5) the payload is released from endosomes and/or lysosomes and causes cell death; and (6) membrane-permeable payloads enter neighboring cells regardless of target expression and can destroy these cells (termed the bystander effect) [20].
Figure 1.
Simple schemas of highly targeted therapies. (A) Antibody-drug conjugate (ADC), (B) photodynamic therapy (PDT), and (C) photoimmunotherapy (PIT). PS, photosensitizer; ER, endoplasmic reticulum; ROS, reactive oxygen species.
ADCs typically employ specific drugs as payloads, such as auristatins (monomethyl auristatin E and monomethyl auristatin F [MMAF]), calicheamicins (ozogamicin), maytansinoids (DM1), and camptothecin analogues (the exatecan derivative, deruxtecan (DXd), and the irinotecan metabolite, SN-38). These payloads exhibit high cytotoxicity at sub-nanomolar concentrations [21]. Early ADCs designed to carry traditional anticancer drugs were not effective compared to the standard anticancer drugs. To enhance the effectiveness of ADCs, the drug-to-antibody ratios of globally approved ADCs range from 2 to 8, on average, depending on the presence of native cysteine or lysine residues on the monoclonal antibody. However, this variation can lead to heterogeneity within a batch of ADCs, presenting a challenge in ADC development [22].
2.1. Preclinical Studies of ADCs for CCA
There have been three preclinical trials of ADCs for CCA using murine models whose targeted antigens were human epidermal growth factor receptor 2 (HER2) [23], mucin 1 (MUC1) [24], and glypican-1 (GPC1) [25] (Table 1). HER2 is a member of the EGFR family. Protein dimers of HER2 with HER family receptors, such as EGFR, HER2, HER3, or HER4, accelerate cell proliferation and prolong cell survival. Amplification or overexpression of HER2 is predominantly associated with tumorigenesis in the breast (15–30%), stomach, and esophagus (10–30%) [26,27,28]. HER2 overexpression is also observed in 4.8% (95% confidence interval [CI] 0–14.5%) of ICC, 17.4% (95% CI 3.4–31.4%) of ECC, 19.1% (95% CI 11.2–26.8%) of gallbladder cancer, and 27.9% (95% CI 0–60.7%) of ampullary carcinoma [29]. Yamashita-Kashima et al. indicated that the anti-proliferative activity of the ADC trastuzumab emtansine (T-DM1) was higher in CCA cell lines with higher levels of HER2 expression and in proportion to HER2 status [23]. Shinoda et al. showed that the cytotoxicity of lymphokine-activated killer cells (a heterogeneous population consisting of NK, NKT, and T cells) against CCA can be reinforced by staphylococcal enterotoxin A (SEA) conjugated with an antibody directed to MUC1 (MUSE11) in CCA cells [24,30]. SEA is one of the superantigens that bind outside of the peptide-binding groove of MHC class II molecules and activate T cells expressing a certain Vβ type of T cell receptor [31,32]. The transmembrane glycoprotein MUC1 is a mucin family member that can act as a lubricant, moisturizer, and physical barrier in normal cells. MUC1 is also an epithelial mucin antigen that is widely expressed in adenocarcinomas, such as those arising in the pancreas, stomach, ovaries, and bile ducts [33,34,35]. Thus, the SEA-MUSE11 conjugate can work via the above-mentioned phase 4 mechanism alone.
Table 1.
Targets for cholangiocarcinoma cells.
| Preclinical Study | Clinical Study | |||||
|---|---|---|---|---|---|---|
| Name | Type | ADC | ADC-Payload | PIT | ADC | ADC-Payload |
| HER2 | Receptor | ✓ | Emtansine (DM1) | ✓ | ✓ | Emtansine (DM1) Deruxtecan (DXd) |
| EGFR | Receptor | ✓ | ||||
| FGFR2 | Receptor | ✓ | Ixadotin | |||
| MUC1 | Secretion (mucin) | ✓ | ||||
| Glypican-1 (GPC1) | Secretion (proteoglycan) | ✓ | Monomethyl auristatin F (MMAF) |
|||
| CD133/ prominin-1 |
Secretion (glycoprotein) | ✓ | Maleimidocaproyl-valine-citrulline-p-aminobenzoyl-MMAF (vcMMAF) | |||
| TROP2 | Secretion (glycoprotein) | ✓ | ||||
HER2—human epidermal growth factor receptor 2; EGFR—epidermal growth factor receptor; FGFR2—fibroblast growth factor receptor-2; MUC1—transmembrane glycoprotein mucin 1; TROP2—trophoblast cell surface antigen 2. ✓ indicates the existence of previous reports.
GPC1, a cancer antigen, is a heparan sulfate proteoglycan that is linked to the cell surface by a glycosylphosphatidylinositol anchor and promotes tumor growth, metastasis, and invasion by acting as a co-receptor [36]. Yokota et al. reported high expression of GPC1 in 47% of patients with ECC by immunohistochemical staining and that MMAF-conjugated anti-GPC1 antibodies showed potent tumor growth inhibition against GPC1-positive CCA cells in vitro and in vivo [25]. MMAF is a tubulin-polymerizing inhibitor and is also clinically used as a payload in ADCs for relapsed or refractory multiple myeloma. Therefore, anti-GPC1 ADCs should be clinically investigated and developed, especially for ECC, considering other payloads such as DM1 and DXd.
CD133/prominin-1 is a pentaspan transmembrane glycoprotein overexpressed in various solid tumors, including colorectal and glioblastomas. In a study by Smith et al. [37], CD133 was found to be highly expressed in ≥50% of pancreatic, gastric, and intrahepatic CCA. In addition, anti-CD133 ADC (maleimidocaproyl-valine-citrulline-p-aminobenzoyl-MMAF [vcMMAF]) treatment resulted in a significant delay in Hep3B (hepatocellular carcinoma) tumor growth in SCID mice. Thus, the anti-CD133 antibody-vcMMAF conjugate could also be effective for CCA treatment.
2.2. Human Studies of ADCs for CCA
Seven ADCs have been approved for solid tumors worldwide. Among these, three are approved for breast cancer targeting HER2, two for gastric cancer targeting HER2, and one each for head and neck cancers targeting EGFR/tissue factor and urothelial cancer targeting nectin-4 (including duplicate indications). In addition, there have been three clinical trials specifically focused on CCA (Table 1). Two of them target HER2, and one targets FGFR2 on CCA cells.
Mondaca et al. showed one case with a 30% partial response of the primary lesion after trastuzumab (anti-HER2 antibody)-DM1 treatment [38]. Additionally, Tsurutani et al. demonstrated confirmed objective responses in HER2-expressing (IHC ≥1+) non-small cell lung cancer, salivary gland cancer, endometrial cancer, and biliary tract cancer following trastuzumab-DXd treatment. Among these cases, two showed tumor shrinkage of ≥60% [39]. Based on its promising results, a multicenter phase II trial of trastuzumab deruxtecan for HER2-positive unresectable or recurrent biliary tract cancer (HERB trial) is ongoing in Japan [40].
To target FGFR2, aprutumab ixadotin (BAY 1187982) was developed as the first ADC with a novel auristatin-based payload. A phase I trial comprising 20 patients with FGFR2-positive solid tumors, including four CCAs, revealed that aprutumab ixadotin was poorly tolerated due to a high rate of proteinuria and nephropathy. The maximum tolerance dose (MTD) was found to be below the therapeutic threshold estimated preclinically; therefore, the trial was terminated early [41]. The authors hypothesized that severe toxicity might be attributed to the unique combination of an auristatin W derivative payload with aprutumab. As FGFR2 fusion/rearrangement is detected in 7.4−13.6% of ICCs, improvement of anti-FGFR2 antibody-based ADC is also warranted [42,43,44].
3. Photodynamic Therapy
Since the ancient Egyptian era, light has been used in medicine to treat skin diseases such as psoriasis and vitiligo with psoralens. At present, photodynamic therapy (PDT) is extensively used in infectiology, dermatology, gynecology, urology, and oncology [45]. Since the first modern medical concept of photodynamic therapy was introduced in 1900 by Raab and von Tappeiner based on the incidental effect on malaria-causing protozoa, the first-in-human PDT of tumors was performed by von Tappeiner for skin tumors in 1903, according to the literature [45,46,47,48]. Approximately 70 years later, Diamond et al. published a groundbreaking report demonstrating the anticancer effect of PDT with hematoporphyrin and white light on rat gliomas in both in vitro and in vivo settings [49]. Notably, the PDT effect was limited to the area where hematoporphyrin and white light coexisted, thus achieving highly targeted treatment. The mechanism of PDT is explained by the following phases: (1) entering the cell of the photosensitizer; (2) photoexcitation of the photosensitizer from the ground energy state to the exited state; (3) energy transfer from the photosensitizer to the biomolecules from its surroundings (type I reaction) or to the oxygen molecule (type II reaction); (4) production of reactive oxygen species (ROS): superoxide anion radical (O2•−), hydroxyl radical (OH•) by type II, and singlet oxygen (1O2) by type I inside the cells; and (5) oxidative stress resulting in the destruction of cancer cells [50,51] (Figure 1B). Furthermore, recent studies indicate that immunogenic cell death via apoptosis and necroptosis can occur after PDT, leading to the release of danger/damage-associated molecular patterns that can activate an adaptive immune response [52,53].
In 1976, Kelly and Snell conducted the first human study to evaluate the effects of PDT using a hematoporphyrin derivative (HpD) in five patients with bladder cancer. Their study resulted in one successful case, demonstrating the potential of PDT in cancer treatment [54]. Nowadays, PDT has been approved for the treatment of various types of cancer, including head and neck, brain, lung, esophagus, breast, prostate, bladder, skin, pancreas, and bile duct cancers [55]. Many researchers have made efforts to improve the efficacy of PDT through the refinement of photosensitizers and light sources, as described below.
3.1. Photosensitizers
Since the initial report of topical eosin combined with white light for treating skin tumors in 1903, various photosensitizers have been developed to enhance the efficacy of PDT (Table 2). A significant breakthrough occurred in 1942 and 1948 when porphyrins, including hematoporphyrin, coproporphyrin, protoporphyrin, and zinc hematoporphyrin, were found to selectively accumulate in malignant tumors after their exogenous administration for tumor detection experiments [56,57]. Among the porphyrins, HpD was identified as the most phototoxic for killing tumors in mice. In a pivotal study conducted by Dougherty et al. (1975), HpD demonstrated a high antitumor effect of PDT in vivo, while HpD alone or light alone had no effect [58]. In 1976, Kelly et al. indicated the effects of PDT using HpD in five patients with bladder cancer, as described above [54].
Since then, various photosensitizers have been developed. The second generation ones (hematoporphyrin derivatives and synthetic photosensitizers, such as 5-aminolevulinic acid, benzoporphyrin derivatives, texaphyrins, thiopurine derivatives, chlorin, bacteriochlorin analogues, and phthalocyanines) were developed to address the drawbacks of the first-generation ones, such as low chemical purity and poor tissue penetration due to maximum absorption at a relatively short wavelength (630 nm). The third-generation photosensitizers comprise second-generation photosensitizers combined with molecules/LDL and lipoproteins/antibodies specifically targeted to antigens. These approaches increase the affinity and permeability of cancer cells and lower skin toxicity. The first- and second-generation photosensitizers are also classified among the porphyrin family (HpD, benzoporphyrin derivative, ALA [5-aminolevulinic acid]), chlorin family (temoporfin, purlytin [tin-ethyl-etiopurpurin], NPe6 [mono-L-aspartyl chlorin e6] = talaporfin sodium, HPPH (photochlor), and dyes (phthalocyanine and naphthalocyanine) based on their chemical structures [50]. Among them, HpD, temoporfin (m-THPC), phthalocyanine-4, talaporfin, and chlorine e6 derivatives (including chlorin I/chlorin II) have mainly been used clinically and preclinically for CCA/bile duct cancer [59,60,61,62,63,64,65,66,67,68]. In vitro studies have shown varying degrees of efficacy of these photosensitizers against human CCA cells, and similar results have been observed in animal studies. Phthalocyanine and chlorin I/chlorin II have not yet been clinically investigated in patients with CCA.
Among the third-generation photosensitizers, nanoparticle albumin-bound (nab)-mTHPC, which is produced using nanotechnology, showed high cytotoxicity in a CCA cell line called TFK-1 when subjected to illumination. Notably, no toxicity was observed under dark conditions [69]. Furthermore, the use of interstitially targeted liposomes containing metalated phthalocyanines, specifically targeting tumor cells and the tumor microenvironment, has shown promising results. These photodynamically active photosensitizers were able to effectively photosensitize human CCA cells (SK-ChA-1) and non-cancerous cells (human endothelial cells [HUVECs], murine fibroblasts [NIH-3T3], and murine macrophages [RAW 264.7]) [70]. Thus, future animal and clinical studies exploring their efficacy are warranted.
3.2. Light Sources for PDT
Light sources for PDT have evolved over time. Initially, non-laser light sources such as conventional lamps were used, which involved water-cooled incandescent lamps with output defined by filters. However, these light sources had limitations, such as a significant thermal component, making it challenging to accurately calculate the delivered light dose [71]. In recent years, there has been a shift towards more efficient lasers that can produce monochromatic light of a known wavelength and easily perform light dosimetry. Laser light can also be supplied via an optical fiber for localized treatment. The appropriate wavelength for PDT is determined according to the photosensitizer used: 630 nm for HpD, 635 nm for 5-ALA-induced protoporphyrin IX, and 652 nm for tetra (m-hydroxyphenyl) chlorin (Table 2). Moreover, recent advances in semiconductor diode technology have enabled laser systems to be more compact and cheaper [45]. Thus, at present, lasers might be the first choice for a PDT light source. Meanwhile, it has been reported that the use of light emitting diodes (LEDs) of specific wavelengths (610 nm) is effective for PDT of CCA [72,73] and gastrointestinal cancers [74]. Therefore, LEDs can be another light source because of their smaller batteries and lower cost compared to conventional lasers.
3.3. Human Clinical Studies on PDT
Despite ingenuity and improvements in the above-mentioned modalities, PDT monotherapy has limitations, such as incomplete tumor killing or recurrence, and has not replaced existing antitumor therapies. In the field of biliary tract cancer, PDTs mainly for ECC have been clinically performed worldwide since the 1990s (Table 2) [75,76,77]. However, since the 2000s, some RCTs and one meta-analysis have revealed that PDT could yield significantly longer survival/higher survival rates than supportive care with biliary drainage [78,79,80,81,82,83,84]. The 1-year survival rate of the PDT with stent group was 56% (range: 39–75%), and that of the control group was 25% (range: 12–38%). The 2-year survival rate of the PDT with stent group was 16% (range: 14–21%), and that of the control group was 7% (range: 3–10%). Meanwhile, PDT has not shown superiority over conventional systemic chemotherapy in many clinical trials [85,86].
Alternatively, some PDTs combined with systemic chemotherapy (chemophototherapy, CPT) have been shown to be effective treatment options preclinically and clinically [86,87]. During in vitro and in vivo experiments, PDT with novel cancer drugs, such as DMXAA (ASA404: flavone acetic acid analog with TNF-α synthesis), PD166285 (synthetic RTK inhibitors), and TNP-470 (synthetic anti-angiogenesis agent), has demonstrated good outcomes for murine sarcoma, breast, colon, and prostate cancer cells, although CCA cells were not included [85].
There have been several clinical comparative studies that have examined the effectiveness of PDT vs. CPT or chemotherapy vs. CPT for CCA. [86,87]. Regarding PDT vs. CPT, two studies, including one RCT, revealed that CPT had superior outcomes (median overall survival: 8 M vs. 17 M, p = 0.005; 12 M vs. 17 M, p = 0.021), while two studies indicated the equivalence of both treatments (11 M vs. 18 M, p = 0.05; 15 M vs. 20 M, p = 0.727) [87]. Meanwhile, according to a meta-analysis of chemotherapy versus CPT or PDT vs. CPT, CPT had significantly better overall survival than chemotherapy or PDT alone (CPT vs. chemotherapy, hazard ratio (HR): 0.69, p = 0.02; CPT vs. PDT, HR: 0.36, p < 0.01) [86]. Therefore, for unresectable CCA, PDT with systemic chemotherapy (CPT) is expected to yield the most favorable outcomes, although the standard PDT or combined chemotherapy regimen is yet to be determined.
Table 2.
Photosensitizers for photodynamic therapy and photoimmunotherapy.
| Investigations for CCA | ||||||||
|---|---|---|---|---|---|---|---|---|
| Photosensitizer | Potential Indications | Activation Wavelength |
Human | Animal | In Vitro | LED Effect |
LED Wavelength |
Reports Regarding CCA * |
| Photodynamic therapy (PDT) | ||||||||
| HPD (partially purified) porfimer sodium |
Cervical, endobronchial, oesophageal, bladder, gastric cancers, brain tumor, bile duct cancer |
630 nm | ✓ | ✓ | ✓ | ✓ | 620–650 nm | [60,61,75,76,77,78,79,80,81,82,83] |
| Phosphorus tetraphenylporphyrin | Bile duct cancer | 610 nm | ✓ | ✓ | 610 nm | [72,73,74] | ||
| m-THPC (Temoporfin) | Head and neck, prostate, pancreas, lung, skin, bile duct cancer | 652 nm | ✓ | ✓ | ✓ | [62,75] | ||
| Phthalocyanine-4 | Cutaneous/subcutaneous lesions from diverse solid tumor origins, bile duct cancer |
670 nm | ✓ | ✓ | [63] | |||
| Taporfin sodium (Talaporfin, NPe6) | Lung, liver metastasis, pancreas, colon, brain cancer, bile duct cancer, solid tumors from diverse origins | 664 nm | ✓ | ✓ | ✓ | ✓ | 660 nm | [64,65,66,73] |
| Chlorine e6 derivatives | Nasopharyngeal, sarcoma, brain, pancreaticobiliary malignancies | 660 nm | ✓ | ✓ | ✓ | [67,68,75] | ||
| Chlorin I/chlorin II | Bile duct cancer | 650 nm | ✓ | ✓ | [69] | |||
| Nanoparticle albumin-bound mTHPC | Bile duct cancer | 652 nm | ✓ | [70] | ||||
| ITLs encapsulating ZnPC and AlPC | Breast, bile duct cancer | 671 nm | ✓ | [71] | ||||
| 5-ALA | Basal-cell carcinoma, head and neck, gynaecological tumors brain, bladder tumors | 635 nm 375–400 nm |
||||||
| 5-ALA-methylesther | Basal-cell carcinoma | 635 nm | ||||||
| 5-ALA benzylesther | Gastrointestinal cancer | 635 nm | ||||||
| 5-ALA hexylesther | Bladder tumors | 375–400 nm | ||||||
| Boronated protoporphyrin | Brain tumors | 630 nm | ||||||
| BPD-MA (benzoporphyrin) | Basal-cell carcinoma | 689 nm | ||||||
| HPPH | Basal-cell carcinoma, head and neck, esophagus, lung cancer | 665 nm | ||||||
| Lutetium texaphyrin | Cervical, prostate and brain tumours | 732 nm | ||||||
| Motexafin lutetium (Mlu) | Prostate cancer | 732 nm | ||||||
| Padeliporfin | Prostate cancer | 762 nm | ||||||
| Redaporfin | Head and neck cancer | 749 nm | ||||||
| Silicon phthalocyanine | Cutaneous T-cell lymphoma | 675 nm | ||||||
| SnET2 | Cutaneous metastatic breast cancer, basal-cell carcinoma, Kaposi’s sarcoma, prostate cancer | 664 nm | ||||||
| Verteporfin | Skin, pancreas cancer | 690 nm | ||||||
| Photoimmunotherapy (PIT) | ||||||||
| IR700 (IRDye 700DX N-hydroxysuccinimide ester) | Head and neck can, stomach, esophagus, pancreas, bile duct cancer | 690 nm | ✓ | ✓ | ✓ | 680–700 nm | [88,89] | |
CCA—cholangiocarcinoma; LED—light emitting diode; HPD—hematoporphyrin derivative; m-THPC—metatetrahydroxyphenylchlorin = temoporfin; ITLs—Interstitially targeted liposomes; ZnPC—zinc phthalocyanine; AIPC—aluminum phthalocyanine; 5-ALA—5-aminolevulinic acid; BPD-MA—benzoporphyrin derivative-monoacid ring A; HPPH—2-(1-hexyloxyethyl)-2-devinyl pyropheophorbide-alpha; SnET2—tin ethyl etiopurpurin; * Brackets include reference numbers. ✓ indicates the existence of previous reports.
4. Photoimmunotherapy
Photoimmunotherapy (PIT) is a novel anti-cancer therapy developed in 2011 by Kobayashi H. et al. that theoretically selectively kills targeted cancer cells with no damage to normal cells [90]. PIT comprises a unique photosensitizer called “IR700.” This water-soluble photo dye consists of silicon phthalocyanine and hydrophilic side chains (IRDye 700DX N-hydroxysuccinimide ester) (Table 2). In addition, PIT incorporates a specific molecule that enables binding to a target cell, which can be an antibody or a low-molecular-weight compound. Examples include the combination of IR700 with an anti-EGFR antibody or an affibody combined with IR700 as antibody/affibody-photosensitizer conjugates (APCs) [91,92]. IR700 is different from photosensitizers used in PDT because IR700 has a more than five-fold higher extinction coefficient (2.1 × 105 M−1cm−1 at the absorption maximum of 689 nm) [93] than that of conventional photosensitizers, such as the HpD (1.2 × 103 M−1cm−1 at 630 nm), meta-tetrahydroxyphenylchlorin (2.2 × 104 M−1cm−1 at 652 nm), and mono–L-aspartylchlorin e6 NPe6 (4.0 × 104 M−1cm−1 at 654 nm) [94]. Although PIT also requires a light source emitting near-infrared light (NIR) with a wavelength of 689–700 nm (NIR wavelength is usually defined as 650–1700 nm) [90,95], its mechanism differs from that of PDT (Figure 1C). In PIT, the destruction of the target cell starts with a chemical change of IR700 in APCs bound to the cell due to the release of hydrophilic side chains of IR700 after NIR irradiation. This process forms water-insoluble aggregates of APCs or APC-antigen complexes on the cell surface molecules, leading to physicochemical changes within the APC-antigen complex that reduce cell membrane integrity because of damage to transmembrane target proteins. Subsequently, water flows into the cytoplasm, causing cell swelling [96]. In contrast, the mechanism of PDT is based on inner cell destruction by ROS (Figure 1B). In addition, PIT also results in further immunogenic cell death that is initiated by the maturation of immature dendritic cells with released tumor antigens from the treated cancer cell in the adjacent microenvironment. After cancer cell-targeted PIT, CD8+ T cells newly primed by a larger repertoire of cancer antigens proliferate in the treated tumor beds. Finally, anticancer host immunity can be strengthened after cancer-cell-targeted PIT [96]. Although many investigations of PIT and clinical PIT for head and neck cancer use lasers as an NIR light source as well as PDT, LEDs can also produce NIR and yield a PIT effect on CCA cells [88]. As described above, CCA can develop in the extrahepatic and intrahepatic bile ducts that cannot be approached/visualized by an endoscope, while a special catheter with LEDs, such as a biliary drainage tube, can be placed for PIT at the peripheral CCA [88]. Therefore, a dedicated PIT device for CCA would shed light on PIT for CCA.
4.1. Antibody and Low Molecular Weight (LMW) Compound for Targeting Cancer Cells with IR700
IR700 can covalently bind to any kind of antibody (IR700:antibody = approximately 3:1), forming a highly flexible theranostic platform [90]. The selected antibody or low-weight molecule for PIT depends on the cell surface antigen or molecules on the target cancer cell. Various agents, including many APCs and some LMW compound-IR700 conjugates, have been reported in preclinical and clinical settings. EGFR is a representative target on cancer cells for antibodies, followed by HER2, carcinoembryonic antigen (CEA), VEGFR2, cadherin-17, and ICAM-1 in PIT [97]. In addition to the antibody, a partner of IR700 for a conjugate of PIT that has been reported so far includes an affibody (a small protein mimetic [6–7 kDa]) for HER2-overexpressing breast cancer [92], an LMW ligand composed of Glu-Urea-Lys for prostate cancer with prostate-specific membrane antigen [98], and a lection for CEA-expressing pancreatic cancer [99,100]. For CEA, a novel approach with affimer proteins and cubosomes has also been reported in colorectal cancer cell lines [89]. For PIT of CCA, there have been two preclinical reports: one used anti-EGFR and HER2 antibodies [88], while another used an antibody against trophoblast cell surface antigen 2/tumor-associated calcium signal transducer 2 (TROP2), which is overexpressed in trophoblast cancer and many epithelial cancers, including pancreatic cancer and CCA [101]. In both studies, PIT specifically killed the target-expressing CCA cells in vitro and significantly suppressed the growth of CCA in murine xenograft models after NIR irradiation.
4.2. Human Clinical Studies on PIT
In 2020, PIT for unresectable locally advanced/recurrent head and neck cancer was publicly approved and initiated as a clinical modality in Japan ahead of the rest of the world. In the U.S., a phase 3 trial of PIT for the same cancer has been performed. The first in-human PIT for head and neck cancer conducted in the U.S. in 2015 revealed tumor volume reduction with complete remission (13.3%), partial remission (30%), and stable disease (36.7%), which is a promising but somewhat insufficient result [102]. Thereafter, in Japan, a few clinical trials have been performed or initiated for unresectable advanced/recurrent gastric cancer or esophageal cancer (one for gastric cancer or esophageal cancer is completed; another for esophageal cancer is suspended) and advanced or recurrent solid tumors with one or more hepatic metastases (recruitment) (https://jrct.niph.go.jp/search?language=en&page=1, accessed on 1 June 2023). The former used cetuximab-IR700 conjugate targeting cancer cells with anti-PD antibody (nivolumab), while the latter used anti-CD25 antibody-IR700 conjugate targeting regulatory T-cells with anti-CTLA-4 antibody (pembrolizumab). The initial PIT with an APC on a cancer cell alone has some limitations, such as (1) insufficient attainment of an APC to a cancer cell and penetration depth of NIR light into the tissue; (2) lack of a dedicated light device for a deeply located tumor, such as CCA and pancreatic cancer; and (3) non-universality of a single APC for various tumors. Based on these findings, PIT with another anticancer drug, such as an immune check inhibitor (ICI), is ongoing, as described above. Unfortunately, there has been no clinical trial of PIT for CCA. However, recent molecular and immunological investigations and treatments for CCA, including EGFR and FGFR inhibitors (pemigatinib/infigratinib/futibatinib), neurotrophic receptor tyrosine kinase inhibitor (entrectinib/larotrectinib), and ICIs (durvalumab, a PD-L1 inhibitor), will promote and accelerate the use of PIT in the near future.
5. Conclusions and Future Directions
The basic premises of highly targeted therapies for CCA involve the identification of specific targets on CCA cells and directing therapeutic interventions towards those targets. Although several targets have been identified or investigated as described above, they are not universally applicable and are limited to certain types of CCA. Overcoming the discrepancy between the universality of the target and the localization of the attack in cancer therapy is partially controversial. However, it is not an insurmountable challenge, as we can visually differentiate CCA cells from non-CCA cells and select them in vitro using our own judgment. Currently, artificial intelligence (AI) plays an important role in various fields, including clinical diagnosis of cancer through endoscopy and pathology, as well as preclinical analysis using multi-omics approaches [103]. Therefore, the collaboration between human observation and AI has the potential to overcome the obstacles in identifying universal targets in CCA cells, paving the way for the development of highly targeted therapies for CCA, such as in ADC, PDT, and PIT.
Author Contributions
M.K. reviewed previous reports and drafted the manuscript. N.S. supervised and advised on the contents of this paper. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Nakanuma Y., Hoso M., Sanzen T., Sasaki M. Microstructure and development of the normal and pathologic biliary tract in humans, including blood supply. Microsc. Res. Tech. 1997;38:552–570. doi: 10.1002/(SICI)1097-0029(19970915)38:6<552::AID-JEMT2>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 2.Banales J.M., Marin J.J.G., Lamarca A., Rodrigues P.M., Khan S.A., Roberts L.R., Cardinale V., Carpino G., Andersen J.B., Braconi C., et al. Cholangiocarcinoma 2020: The next horizon in mechanisms and management. Nat. Rev. Gastroenterol. Hepatol. 2020;17:557–588. doi: 10.1038/s41575-020-0310-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamsa-Ard S., Luvira V., Suwanrungruang K., Kamsa-Ard S., Luvira V., Santong C., Srisuk T., Pugkhem A., Bhudhisawasdi V., Pairojkul C. Cholangiocarcinoma trends, incidence, and relative survival in Khon Kaen, Thailand from 1989 through 2013: A populationbased cancer registry study. J. Epidemiol. 2019;29:197–204. doi: 10.2188/jea.JE20180007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Cancer Center Japan . Cancer Statistics in Japan 2023. National Cancer Center Japan; Tokyo, Japan: 2023. [(accessed on 30 April 2023)]. Available online: https://ganjoho.jp/public/qa_links/report/statistics/2023_en.html. [Google Scholar]
- 5.Nagino M., Hirano S., Yoshitomi H., Aoki T., Uesaka K., Unno M., Ebata T., Konishi M., Sano K., Shimada K., et al. Clinical practice guidelines for the management of biliary tract cancers 2019: The 3rd English edition. J. Hepato-Biliary-Pancreat. Sci. 2021;28:26–54. doi: 10.1002/jhbp.870. [DOI] [PubMed] [Google Scholar]
- 6.Sutherland M., Ahmed O., Zaidi A., Ahmed S. Current progress in systemic therapy for biliary tract cancers. J. Hepato-Biliary-Pancreat. Sci. 2022;29:1094–1107. doi: 10.1002/jhbp.939. [DOI] [PubMed] [Google Scholar]
- 7.Hosseini Shabanan S., Nezami N., Abdelsalam M.E., Sheth R.A., Odisio B.C., Mahvash A., Habibollahi P. Selective Internal Radiation Therapy with Yttrium-90 for Intrahepatic Cholangiocarcinoma: A Systematic Review on Post-Treatment Dosimetry and Concomitant Chemotherapy. Curr. Oncol. 2022;29:3825–3848. doi: 10.3390/curroncol29060306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taggar A.S., Mann P., Folkert M.R., Aliakbari S., Myrehaug S.D., Dawson L.A. A systematic review of intraluminal high dose rate brachytherapy in the management of malignant biliary tract obstruction and cholangiocarcinoma. Radiother. Oncol. 2021;165:60–74. doi: 10.1016/j.radonc.2021.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Wang N., Huang A., Kuang B., Xiao Y., Xiao Y., Ma H. Progress in Radiotherapy for Cholangiocarcinoma. Front. Oncol. 2022;12:868034. doi: 10.3389/fonc.2022.868034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oh D.Y., He A.R., Qin S., Chen L.T., Okusaka T., Vogel A., Kim J.W., Suksombooncharoen T., Lee M.A., TOPAZ-1 Investigators et al. Durvalumab plus Gemcitabine and Cisplatin in Advanced Biliary Tract Cancer. NEJM Evid. 2022;1:EVIDoa2200015. doi: 10.1056/EVIDoa2200015. [DOI] [PubMed] [Google Scholar]
- 11.Guo Y., Feng K., Liu Y., Wu Z., Dai H., Yang Q., Wang Y., Jia H., Han W. Phase I study of chimeric antigen receptor-modified T cells in patients with EGFR-positive advanced biliary tract cancers. Clin. Cancer Res. 2018;246:1277–1286. doi: 10.1158/1078-0432.CCR-17-0432. [DOI] [PubMed] [Google Scholar]
- 12.Wiggers J.K., Ruys A.T., Groot Koerkamp B., Beuers U., ten Kate F.J., van Gulik T.M. Differences in immunohistochemical biomarkers between intra- and extrahepatic cholangiocarcinoma: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2014;29:1582–1594. doi: 10.1111/jgh.12620. [DOI] [PubMed] [Google Scholar]
- 13.Nakamura H., Arai Y., Totoki Y., Shirota T., Elzawahry A., Kato M., Hama N., Hosoda F., Urushidate T., Ohashi S., et al. Genomic spectra of biliary tract cancer. Nat. Genet. 2015;47:1003–1010. doi: 10.1038/ng.3375. [DOI] [PubMed] [Google Scholar]
- 14.Jain A., Javle M. Molecular profiling of biliary tract cancer: A target rich disease. J. Gastrointest. Oncol. 2016;7:797–803. doi: 10.21037/jgo.2016.09.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cardinale V., Wang Y., Carpino G., Mendel G., Alpini G., Gaudio E., Reid L.M., Alvaro D. The biliary tree—A reservoir of multipotent stem cells. Nat. Rev. Gastroenterol. Hepatol. 2012;9:231–240. doi: 10.1038/nrgastro.2012.23. [DOI] [PubMed] [Google Scholar]
- 16.Strebhardt K., Ullrich A. Paul Ehrlich’s magic bullet concept: 100 years of progress. Nat. Rev. Cancer. 2008;8:473–480. doi: 10.1038/nrc2394. [DOI] [PubMed] [Google Scholar]
- 17.Mathe G., Lou T.B., Bernard J. Effet sur la leucemie 1210 de la souris dune combinaison par diazotation da-methopterine et de gamma- globulines de hamsters porteurs de cette leucemie par heterogreffe. Presse Med. 1958;66:571. [PubMed] [Google Scholar]
- 18.Yu J.F., Song Y.P., Tian W. How to select IgG subclasses in developing anti- tumor therapeutic antibodies. J. Hematol. Oncol. 2020;13:45. doi: 10.1186/s13045-020-00876-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang T.H., Jung S.T. Reprogramming the Constant Region of Immunoglobulin G Subclasses for Enhanced Therapeutic Potency against Cancer. Biomolecules. 2020;10:382. doi: 10.3390/biom10030382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drago J.Z., Modi S., Chandarlapaty S. Unlocking the potential of antibody-drug conjugates for cancer therapy. Nat. Rev. Clin. Oncol. 2021;18:327–344. doi: 10.1038/s41571-021-00470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Senter P.D. Potent antibody drug conjugates for cancer therapy. Curr. Opin. Chem. Biol. 2009;13:235–244. doi: 10.1016/j.cbpa.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 22.Agarwal P., Bertozzi C.R. Site- specific antibodydrug conjugates: The nexus of biorthogonal chemistry, protein engineering, and drug development. Bioconjugate Chem. 2015;26:176–192. doi: 10.1021/bc5004982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamashita-Kashima Y., Yoshimura Y., Fujimura T., Shu S., Yanagisawa M., Yorozu K., Furugaki K., Higuchi R., Shoda J., Harada N. Molecular targeting of HER2-overexpressing biliary tract cancer cells with trastuzumab emtansine, an antibody-cytotoxic drug conjugate. Cancer Chemother. Pharmacol. 2019;83:659–671. doi: 10.1007/s00280-019-03768-8. [DOI] [PubMed] [Google Scholar]
- 24.Shinoda M., Kudo T., Suzuki M., Katayose Y., Sakurai N., Saeki H., Kodama H., Fukuhara K., Imai K., Hinoda Y., et al. Effective adoptive immunotherapy by T-LAK cells retargeted with bacterial superantigen-conjugated antibody to MUC1 in xenografted severe combined immunodeficient mice. Cancer Res. 1998;58:2838–2843. [PubMed] [Google Scholar]
- 25.Yokota K., Serada S., Tsujii S., Toya K., Takahashi T., Matsunaga T., Fujimoto M., Uemura S., Namikawa T., Murakami I., et al. Anti-Glypican-1 Antibody-drug Conjugate as Potential Therapy Against Tumor Cells and Tumor Vasculature for Glypican-1-Positive Cholangiocarcinoma. Mol. Cancer Ther. 2021;20:1713–1722. doi: 10.1158/1535-7163.MCT-21-0015. [DOI] [PubMed] [Google Scholar]
- 26.Yarden Y., Sliwkowski M.X. Untangling the ErbB signalling network. Nat. Rev. Mol. Cell Biol. 2001;2:127. doi: 10.1038/35052073. [DOI] [PubMed] [Google Scholar]
- 27.Wang Z. ErbB receptors and cancer. In: Wang Z., editor. ErbB Receptor Signaling: Methods and Protocols. Springer; New York, NY, USA: 2017. pp. 3–35. [DOI] [PubMed] [Google Scholar]
- 28.Iqbal N., Iqbal N. Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications. Mol. Biol. Int. 2014;2014:852748. doi: 10.1155/2014/852748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galdy S., Lamarca A., McNamara M.G., Hubner R.A., Cella C.A., Fazio N., Valle J.W. HER2/HER3 pathway in biliary tract malignancies; systematic review and meta-analysis: A potential therapeutic target? Cancer Metastasis Rev. 2017;36:141–157. doi: 10.1007/s10555-016-9645-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.West E.J., Scott K.J., Jennings V.A., Melcher A.A. Immune activation by combination human lymphokine-activated killer and dendritic cell therapy. Br. J. Cancer. 2011;105:787–795. doi: 10.1038/bjc.2011.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.White J., Herman A., Pullen A.M., Kubo R., Kappler J.W., Marrack P. The Vβ-specific superantigen staphylococcal enlerotoxin B: Stimulation of mature T cells and clonal deletion in neonatal mice. Cell. 1989;56:27–35. doi: 10.1016/0092-8674(89)90980-X. [DOI] [PubMed] [Google Scholar]
- 32.Marrack P., Kappler J. The staphylococcal enterotoxins and their relatives. Science. 1990;248:705–711. doi: 10.1126/science.2185544. [DOI] [PubMed] [Google Scholar]
- 33.Ioannides C.G., Fisk B., Jerome K.R., Irimura T., Wharton J.T., Finn O.J. Cytoloxic T cells from ovarian malignant tumors can recognize polymorphic epithelial mucin core peptides. J. Immunol. 1993;151:3693–3703. doi: 10.4049/jimmunol.151.7.3693. [DOI] [PubMed] [Google Scholar]
- 34.Ban T., Imai K., Yachi A. Immunohistological and immunochemical characterization of a novel pancreatic cancer-associated antigen MUSE11. Cancer Res. 1989;49:7141–7146. [PubMed] [Google Scholar]
- 35.Yamashita K., Yonezawa S., Tanaka S., Shirahama H., Sakoda K., Imai K., Xing P.X., McKenzie I.F., Hilkens J., Kim Y.S., et al. Immunohistochemical study of mucin carbohydrates and core proteins in hepatolithiasis and cholangiocarcinoma. Int. J. Cancer. 1993;55:82–91. doi: 10.1002/ijc.2910550116. [DOI] [PubMed] [Google Scholar]
- 36.Lund M.E., Campbell D.H., Walsh B.J. The role of Glypican-1 in the tumour microenvironment. Adv. Exp. Med. Biol. 2020;1245:163–176. doi: 10.1007/978-3-030-40146-7_8. [DOI] [PubMed] [Google Scholar]
- 37.Smith L.M., Nesterova A., Ryan M.C., Duniho S., Jonas M., Anderson M., Zabinski R.F., Sutherland M.K., Gerber H.P., Van Orden K.L., et al. CD133/prominin-1 is a potential therapeutic target for antibody-drug conjugates in hepatocellular and gastric cancers. Br. J. Cancer. 2008;99:100–109. doi: 10.1038/sj.bjc.6604437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mondaca S., Razavi P., Xu C., Offin M., Myers M., Scaltriti M., Hechtman J.F., Bradley M., O’Reilly E.M., Berger M.F., et al. Genomic Characterization of ERBB2-Driven Biliary Cancer and a Case of Response to Ado-Trastuzumab Emtansine. JCO Precis. Oncol. 2019;3:PO.19.00223. doi: 10.1200/PO.19.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsurutani J., Iwata H., Krop I., Jänne P.A., Doi T., Takahashi S., Park H., Redfern C., Tamura K., Wise-Draper T.M., et al. Targeting HER2 with Trastuzumab Deruxtecan: A Dose-Expansion, Phase I Study in Multiple Advanced Solid Tumors. Cancer Discov. 2020;10:688–701. doi: 10.1158/2159-8290.CD-19-1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ohba A., Morizane C., Ueno M., Kobayashi S., Kawamoto Y., Komatsu Y., Ikeda M., Sasaki M., Okano N., Furuse J., et al. Multicenter phase II trial of trastuzumab deruxtecan for HER2-positive unresectable or recurrent biliary tract cancer: HERB trial. Future Oncol. 2022;18:2351–2360. doi: 10.2217/fon-2022-0214. [DOI] [PubMed] [Google Scholar]
- 41.Kim S.B., Meric-Bernstam F., Kalyan A., Babich A., Liu R., Tanigawa T., Sommer A., Osada M., Reetz F., Laurent D., et al. First-in-Human Phase I Study of Aprutumab Ixadotin, a Fibroblast Growth Factor Receptor 2 Antibody-Drug Conjugate (BAY 1187982) in Patients with Advanced Cancer. Target Oncol. 2019;14:591–601. doi: 10.1007/s11523-019-00670-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arai Y., Totoki Y., Hosoda F., Shirota T., Hama N., Ojima H., Nakamura H., Furuta K., Shimada K., Okusaka T., et al. Fibroblast growth factor receptor 2 tyrosine kinase fusions define a unique molecular subtype of cholangiocarcinoma. Hepatology. 2014;59:1427–1434. doi: 10.1002/hep.26890. [DOI] [PubMed] [Google Scholar]
- 43.Graham R.P., Barr Fritcher E.G., Pestova E., Schulz J., Sitailo L.A., Vasmatzis G., Murphy S.J., McWilliams R.R., Hart S.N., Halling K.C., et al. Fibroblast growth factor receptor 2 teanslocations in intrahepatic cholangiocarcinoma. Hum. Pathol. 2014;45:1630–1638. doi: 10.1016/j.humpath.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 44.Maruki Y., Morizane C., Arai Y., Ikeda M., Ueno M., Ioka T., Naganuma A., Furukawa M., Mizuno N., Uwagawaet T., et al. Molecular detection and clinicopathological characteristics of advanced/recurrent biliary tract carcinomas harboring the FGFR2 rearrangements: A prospective observational study (PRELUDE Study) J. Gastroenterol. 2021;56:250–260. doi: 10.1007/s00535-020-01735-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ackroyd R., Kelty C., Brown N., Reed M. The history of photodetection and photodynamic therapy. Photochem. Photobiol. 2001;74:656–669. doi: 10.1562/0031-8655(2001)074<0656:THOPAP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 46.Raab O. Uber die Wirkung, fluorescirender Stoffe auf infusorien. Z. Biol. 1900;39:524–546. [Google Scholar]
- 47.von Tappeiner H., Jodlbauer A. Über die Wirkung der photodynamischen (fluorescierenden) Stoffe auf Protozoen und Enzyme. Dtsch. Arch. Klin. Med. 1904;39:427–487. [Google Scholar]
- 48.Kessel D. Photodynamic Therapy: A Brief History. J. Clin. Med. 2019;8:1581. doi: 10.3390/jcm8101581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Diamond I., Granelli S.G., McDonagh A.F., Nielsen S., Wilson C.B., Jaenicke R. Photodynamic therapy of malignant tumours. Lancet. 1972;2:1175–1177. doi: 10.1016/S0140-6736(72)92596-2. [DOI] [PubMed] [Google Scholar]
- 50.Kwiatkowski S., Knap B., Przystupski D., Saczko J., Kędzierska E., Knap-Czop K., Kotlińska J., Michel O., Kotowski K., Kulbacka J. Photodynamic therapy—Mechanisms, photosensitizers and combinations. Biomed. Pharmacother. 2018;106:1098–1107. doi: 10.1016/j.biopha.2018.07.049. [DOI] [PubMed] [Google Scholar]
- 51.Donohoe C., Senge M.O., Arnaut L.G., Gomes-da-Silva L.C. Cell death in photodynamic therapy: From oxidative stress to anti-tumor immunity. Biochim. Biophys. Acta. Rev. Cancer. 2019;1872:188308. doi: 10.1016/j.bbcan.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 52.Yang H., Ma Y., Chen G., Zhou H., Yamazaki T., Klein C., Pietrocola F., Vacchelli E., Souquere S., Sauvat A., et al. Contribution of RIP3 and MLKL to immunogenic cell death signaling in cancer chemotherapy. Oncoimmunology. 2016;5:e1149673. doi: 10.1080/2162402X.2016.1149673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aaes T.L., Kaczmarek A., Delvaeye T., De Craene B., De Koker S., Heyndrickx L., Delrue I., Taminau J., Wiernicki B., De Groote P., et al. Vaccination with Necroptotic cancer cells induces efficient antitumor immunity. Cell Rep. 2016;15:274–287. doi: 10.1016/j.celrep.2016.03.037. [DOI] [PubMed] [Google Scholar]
- 54.Kelly J.F., Snell M.E. Hematoporphyrin derivative: A possible aid in the diagnosis and treatment of carcinoma of the bladder. J. Urol. 1976;115:150–151. doi: 10.1016/S0022-5347(17)59108-9. [DOI] [PubMed] [Google Scholar]
- 55.Dolmans D.E., Fukumura D., Jain R.K. Photodynamic therapy for cancer. Nat. Rev. Cancer. 2003;3:380. doi: 10.1038/nrc1071. [DOI] [PubMed] [Google Scholar]
- 56.Auler H., Banzer G. Untersuchungen uber die Rolle der Porphyrine bei geschwulstkranken Menschen und Tieren. Z. Für Krebsforsch. 1942;53:65–68. doi: 10.1007/BF01792783. [DOI] [Google Scholar]
- 57.Figge F.H.J., Weiland G.S. The affinity of neoplastic embryonic and traumatized tissue for porphyrins and metalloporphyrins. Anat. Rec. 1948;100:659. [PubMed] [Google Scholar]
- 58.Dougherty T.J., Grindey G.B., Fiel R., Weishaupt K.R., Boyle D.G. Photoradiation therapy II: Cure of animal tumors with haematoporphyrin and light. J. Natl. Cancer Inst. 1975;55:115–121. doi: 10.1093/jnci/55.1.115. [DOI] [PubMed] [Google Scholar]
- 59.Rumalla A., Baron T.H., Wang K.K., Gores G.J., Stadheim L.M., de Groen P.C. Endoscopic application of photodynamic therapy for cholangiocarcinoma. Gastrointest. Endosc. 2001;53:500–504. doi: 10.1067/mge.2001.113386. [DOI] [PubMed] [Google Scholar]
- 60.Oertel M., Schastak S.I., Tannapfel A., Hermann R., Sack U., Mössner J., Berr F. Novel bacteriochlorine for high tissue-penetration: Photodynamic properties in human biliary tract cancer cells in vitro and in a mouse tumour model. J. Photochem. Photobiol. B. 2003;71:1–10. doi: 10.1016/S1011-1344(03)00091-5. [DOI] [PubMed] [Google Scholar]
- 61.Wagner A., Denzer U.W., Neureiter D., Kiesslich T., Puespoeck A., Rauws E.A., Emmanuel K., Degenhardt N., Frick U., Beuers U., et al. Temoporfin improves efficacy of photodynamic therapy in advanced biliary tract carcinoma: A multicenter prospective phase II study. Hepatology. 2015;62:1456–1465. doi: 10.1002/hep.27905. [DOI] [PubMed] [Google Scholar]
- 62.Schmidt J., Kuzyniak W., Berkholz J., Steinemann G., Ogbodu R., Hoffmann B., Nouailles G., Gürek A.G., Nitzsche B., Höpfner M. Novel zinc- and silicon-phthalocyanines as photosensitizers for photodynamic therapy of cholangiocarcinoma. Int. J. Mol. Med. 2018;42:534–546. doi: 10.3892/ijmm.2018.3620. [DOI] [PubMed] [Google Scholar]
- 63.Nanashima A., Hiyoshi M., Imamura N., Hamada T., Nishida T., Kawakami H., Ban T., Kubota Y., Nakashima K., Yano K., et al. Two cases of bile duct carcinoma patients who underwent the photodynamic therapy using talaporfin sodium (Laserphyrin®) Clin. J. Gastroenterol. 2020;13:102–109. doi: 10.1007/s12328-019-01006-5. [DOI] [PubMed] [Google Scholar]
- 64.Nanashima A., Abo T., Nonaka T., Nonaka Y., Morisaki T., Uehara R., Ohnita K., Fukuda D., Murakami G., Tou K., et al. Photodynamic therapy using talaporfin sodium (Laserphyrin®) for bile duct carcinoma: A preliminary clinical trial. Anticancer Res. 2012;32:4931–4938. doi: 10.1016/j.jamcollsurg.2015.08.169. [DOI] [PubMed] [Google Scholar]
- 65.Murakami G., Nanashima A., Nonaka T., Tominaga T., Wakata K., Sumida Y., Akashi H., Okazaki S., Kataoka H., Nagayasu T. Photodynamic Therapy Using Novel Glucose-conjugated Chlorin Increases Apoptosis of Cholangiocellular Carcinoma in Comparison with Talaporfin Sodium. Anticancer. Res. 2016;36:4493–4501. doi: 10.21873/anticanres.10995. [DOI] [PubMed] [Google Scholar]
- 66.Choi J.H., Oh D., Lee J.H., Park J.H., Kim K.P., Lee S.S., Lee Y.J., Lim Y.S., Song T.J., Lee S.S., et al. Initial human experience of endoscopic ultrasound-guided photodynamic therapy with a novel photosensitizer and a flexible laser-light catheter. Endoscopy. 2015;47:1035–1038. doi: 10.1055/s-0034-1392150. [DOI] [PubMed] [Google Scholar]
- 67.He C., Xia J., Gao Y., Chen Z., Wan X. Chlorin A-mediated photodynamic therapy induced apoptosis in human cholangiocarcinoma cells via impaired autophagy flux. Am. J. Transl. Res. 2020;12:5080–5094. [PMC free article] [PubMed] [Google Scholar]
- 68.Gao Y.H., Li M.Y., Sajjad F., Wang J.H., Meharban F., Gadoora M.A., Yan Y.J., Nyokong T., Chen Z.L. Synthesis and pharmacological evaluation of chlorin derivatives for photodynamic therapy of cholangiocarcinoma. Eur. J. Med. Chem. 2020;189:112049. doi: 10.1016/j.ejmech.2020.112049. [DOI] [PubMed] [Google Scholar]
- 69.Stein N.C., Mulac D., Fabian J., Herrmann F.C., Langer K. Nanoparticle albumin-bound mTHPC for photodynamic therapy: Preparation and comprehensive characterization of a promising drug delivery system. Int. J. Pharm. 2020;582:119347. doi: 10.1016/j.ijpharm.2020.119347. [DOI] [PubMed] [Google Scholar]
- 70.Dias L.M., de Keijzer M.J., Ernst D., Sharifi F., de Klerk D.J., Kleijn T.G., Desclos E., Kochan J.A., de Haan L.R., Franchi L.P., et al. Photodynamic Therapy Study Group. Metallated phthalocyanines and their hydrophilic derivatives for multi-targeted oncological photodynamic therapy. J. Photochem. Photobiol. B. 2022;234:112500. doi: 10.1016/j.jphotobiol.2022.112500. [DOI] [PubMed] [Google Scholar]
- 71.Whitehurst C., Byrne K., Moore J.V. Development of an alternative light source to lasers for photodynamic therapy: 1. Comparative in vitro dose response characteristics. Lasers Med. Sci. 1993;8:259–267. doi: 10.1007/BF02547849. [DOI] [Google Scholar]
- 72.Matsumoto J., Suzuki K., Yasuda M., Yamaguchi Y., Hishikawa Y., Imamura N., Nanashima A. Photodynamic therapy of human biliary cancer cell line using combination of phosphorus porphyrins and light emitting diode. Bioorg. Med. Chem. 2017;25:6536–6541. doi: 10.1016/j.bmc.2017.10.031. [DOI] [PubMed] [Google Scholar]
- 73.Mai N.N.H., Yamaguchi Y., Choijookhuu N., Matsumoto J., Nanashima A., Takagi H., Sato K., Tuan L.Q., Hishikawa Y. Photodynamic Therapy Using a Novel Phosphorus Tetraphenylporphyrin Induces an Anticancer Effect via Bax/Bcl-xL-related Mitochondrial Apoptosis in Biliary Cancer Cells. Acta Histochem. Cytochem. 2020;53:61–72. doi: 10.1267/ahc.20-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shi X., Yin H., Dong X., Li H., Li Y. Photodynamic therapy with light-emitting diode arrays producing different light fields induces apoptosis and necrosis in gastrointestinal cancer. Front. Oncol. 2022;12:1062666. doi: 10.3389/fonc.2022.1062666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nanashima A., Hiyoshi M., Imamura N., Yano K., Hamada T., Kai K. Recent Advances in Photodynamic Imaging and Therapy in Hepatobiliary Malignancies: Clinical and Experimental Aspects. Curr. Oncol. 2021;28:4067–4079. doi: 10.3390/curroncol28050345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McCaughan JSJr Mertens B.F., Cho C., Barabash R.D., Payton H.W. Photodynamic therapy to treat tumors of the extrahepatic biliary ducts. A case report. Arch. Surg. 1991;126:111–113. doi: 10.1001/archsurg.1991.01410250119022. [DOI] [PubMed] [Google Scholar]
- 77.Abulafi A.M., Allardice J.T., Williams N.S., van Someren N., Swain C.P., Ainley C. Photodynamic therapy for malignant tumours of the ampulla of Vater. Gut. 1995;36:853–856. doi: 10.1136/gut.36.6.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dumoulin F.L., Gerhardt T., Fuchs S., Scheurlen C., Neubrand M., Layer G., Sauerbruch T. Phase II study of photodynamic therapy and metal stent as palliative treatment for nonresectable hilar cholangiocarcinoma. Gastrointest. Endosc. 2003;57:860–867. doi: 10.1016/S0016-5107(03)70021-2. [DOI] [PubMed] [Google Scholar]
- 79.Cheon Y.K., Lee T.Y., Lee S.M., Yoon J.Y., Shim C.S. Longterm outcome of photodynamic therapy compared with biliary stenting alone in patients with advanced hilar cholangiocarcinoma. HPB. 2012;14:185–193. doi: 10.1111/j.1477-2574.2011.00424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee T.Y., Cheon Y.K., Shim C.S., Cho Y.D. Photodynamic therapy prolongs metal stent patency in patients with unresectable hilar cholangiocarcinoma. World J. Gastroenterol. 2012;18:5589–5594. doi: 10.3748/wjg.v18.i39.5589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li Z., Jiang X., Xiao H., Chen S., Zhu W., Lu H., Cao L., Xue P., Li H., Zhang D. Long-term results of ERCP- or PTCS-directed photodynamic therapy for unresectable hilar cholangiocarcinoma. Surg. Endosc. 2021;35:5655–5664. doi: 10.1007/s00464-020-08095-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Quyn A.J., Ziyaie D., Polignano F.M., Tait I.S. Photodynamic therapy is associated with an improvement in survival in patients with irresectable hilar cholangiocarcinoma. HPB. 2009;11:570–577. doi: 10.1111/j.1477-2574.2009.00102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Witzigmann H., Berr F., Ringel U., Caca K., Uhlmann D., Schoppmeyer K., Tannapfel A., Wittekind C., Mossner J., Hauss J., et al. Surgical and palliative management and outcome in 184 patients with hilar cholangiocarcinoma: Palliative photodynamic therapy plus stenting is comparable to r1/r2 resection. Ann. Surg. 2006;244:230–239. doi: 10.1097/01.sla.0000217639.10331.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chen P., Yang T., Shi P., Shen J., Feng Q., Su J. Benefits and safety of photodynamic therapy in patients with hilar cholangiocarcinoma: A meta-analysis. Photodiagnosis Photodyn. Ther. 2022;37:102712. doi: 10.1016/j.pdpdt.2022.102712. [DOI] [PubMed] [Google Scholar]
- 85.Luo D., Carter K.A., Miranda D., Lovell J.F. Chemophototherapy: An Emerging Treatment Option for Solid Tumors. Adv. Sci. 2017;4:1600106. doi: 10.1002/advs.201600106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yu Y., Wang N., Wang Y., Shi Q., Yu R., Gu B., Maswikiti E.P., Chen H. Photodynamic therapy combined with systemic chemotherapy for unresectable extrahepatic cholangiocarcinoma: A systematic review and meta-analysis. Photodiagnosis Photodyn. Ther. 2023;41:103318. doi: 10.1016/j.pdpdt.2023.103318. [DOI] [PubMed] [Google Scholar]
- 87.Inoue T., Yoneda M. Recent Updates on Local Ablative Therapy Combined with Chemotherapy for Extrahepatic Cholangiocarcinoma: Photodynamic Therapy and Radiofrequency Ablation. Curr. Oncol. 2023;30:2159–2168. doi: 10.3390/curroncol30020166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hirata H., Kuwatani M., Nakajima K., Kodama Y., Yoshikawa Y., Ogawa M., Sakamoto N. Near-infrared photoimmunotherapy (NIR-PIT) on cholangiocarcinoma using a novel catheter device with light emitting diodes. Cancer Sci. 2021;112:828–838. doi: 10.1111/cas.14780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pramanik A., Xu Z., Shamsuddin S.H., Khaled Y.S., Ingram N., Maisey T., Tomlinson D., Coletta P.L., Jayne D., Hughes T.A., et al. Affimer Tagged Cubosomes: Targeting of Carcinoembryonic Antigen Expressing Colorectal Cancer Cells Using In Vitro and In Vivo Models. ACS Appl. Mater. Interfaces. 2022;14:11078–11091. doi: 10.1021/acsami.1c21655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mitsunaga M., Ogawa M., Kosaka N., Rosenblum L.T., Choyke P.L., Kobayashi H. Cancer cell-selective in vivo near infrared photoimmunotherapy targeting specific membrane molecules. Nat. Med. 2011;17:1685–1691. doi: 10.1038/nm.2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cognetti D.M., Johnson J.M., Curry J.M., Kochuparambil S.T., McDonald D., Mott F., Fidler M.J., Stenson K., Vasan N.R., Razaq M.A., et al. Phase 1/2a, open-label, multicenter study of RM-1929 photoimmunotherapy in patients with locoregional, recurrent head and neck squamous cell carcinoma. Head Neck. 2021;43:3875–3887. doi: 10.1002/hed.26885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yamaguchi H., Pantarat N., Suzuki T., Evdokiou A. Near-Infrared Photoimmunotherapy Using a Small Protein Mimetic for HER2-Overexpressing Breast Cancer. Int. J. Mol. Sci. 2019;20:5835. doi: 10.3390/ijms20235835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wilson B.C., Patterson M.S. The determination of light fluence distributions in photodynamic therapy. In: Kessel D., editor. Photodynamic Therapy of Neoplastic Disease. Volume 1. CRC Press; Boca Raton, FL, USA: 1990. pp. 129–144. [Google Scholar]
- 94.Detty M.R., Gibson S.L., Wagner S.J. Current clinical and preclinical photosensitizers for use in photodynamic therapy. J. Med. Chem. 2004;47:3897–3915. doi: 10.1021/jm040074b. [DOI] [PubMed] [Google Scholar]
- 95.Zheng F., Huang X., Ding J., Bi A., Wang S., Chen F., Zeng W. NIR-I Dye-Based Probe: A New Window for Bimodal Tumor Theranostics. Front. Chem. 2022;10:859948. doi: 10.3389/fchem.2022.859948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kobayashi H., Choyke P.L. Near-Infrared Photoimmunotherapy of Cancer. Acc. Chem. Res. 2019;52:2332–2339. doi: 10.1021/acs.accounts.9b00273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mohiuddin T.M., Zhang C., Sheng W., Al-Rawe M., Zeppernick F., Meinhold-Heerlein I., Hussain A.F. Near Infrared Photoimmunotherapy: A Review of Recent Progress and Their Target Molecules for Cancer Therapy. Int. J. Mol. Sci. 2023;24:2655. doi: 10.3390/ijms24032655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nakajima K., Miyazaki F., Terada K., Takakura H., Suzuki M., Ogawa M. Comparison of Low-Molecular-Weight Ligand and Whole Antibody in Prostate-Specific Membrane Antigen Targeted near-Infrared Photoimmunotherapy. Int. J. Pharm. 2021;609:121135. doi: 10.1016/j.ijpharm.2021.121135. [DOI] [PubMed] [Google Scholar]
- 99.Furuta T., Oda T., Kiyoi K., Yusuke O., Kimura S., Kurimori K., Miyazaki Y., Yu Y., Furuya K., Akashi Y., et al. Carcinoembryonic antigen as a specific glycoprotein ligand of rBC2LCN lectin on pancreatic ductal adenocarcinoma cells. Cancer Sci. 2021;112:3722–3731. doi: 10.1111/cas.15023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kuroda Y., Oda T., Shimomura O., Hashimoto S., Akashi Y., Miyazaki Y., Furuya K., Furuta T., Nakahashi H., Louphrasitthiphol P., et al. Lectin-based phototherapy targeting cell surface glycans for pancreatic cancer. Int. J. Cancer. 2023;152:1425–1437. doi: 10.1002/ijc.34362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nishimura T., Mitsunaga M., Sawada R., Saruta M., Kobayashi H., Matsumoto N., Kanke T., Yanai H., Nakamura K. Photoimmunotherapy targeting biliary-pancreatic cancer with humanized anti-TROP2 antibody. Cancer Med. 2019;8:7781–7792. doi: 10.1002/cam4.2658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nishikawa D., Suzuki H., Beppu S., Terada H., Sawabe M., Hanai N. Near-Infrared Photoimmunotherapy for Oropharyngeal Cancer. Cancers. 2022;14:5662. doi: 10.3390/cancers14225662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Urman J.M., Herranz J.M., Uriarte I., Rullán M., Oyón D., González B., Fernandez-Urién I., Carrascosa J., Bolado F., Zabalza L., et al. Pilot Multi-Omic Analysis of Human Bile from Benign and Malignant Biliary Strictures: A Machine-Learning Approach. Cancers. 2020;12:1644. doi: 10.3390/cancers12061644. [DOI] [PMC free article] [PubMed] [Google Scholar]