Background:
Hemodynamic variations during the induction of general anesthesia are more profound in hypertensive patients, and the risk of hypoperfusion-induced organ damage followed by hypotensive episodes is higher in hypertensive patients than in normotensive patients. Thus, we compared the effects of remimazolam and propofol on hemodynamics during general anesthesia induction in hypertensive patients.
Methods:
Patients were randomly divided into the remimazolam (Group R, n = 48) and propofol (Group P, n = 48) groups: remimazolam was continued at 6 mg/kg/hour until the patient lost consciousness, followed by 1 mg/kg/hour until 5 minutes after tracheal intubation. Propofol was administered as a slow bolus of 1.5 to 2 mg/kg, followed by 3 to 6 mg/kg/hour 5 minutes after tracheal intubation. Hemodynamic parameters including mean blood pressure (MBP), systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate, and incidence of hypotension were analyzed during the induction period, pre-induction (T1), immediately after loss of consciousness (T2), at 1 and 3 minutes after neuromuscular blockade (T3, T4), immediately after tracheal intubation (T5), and at 1, 3, and 5 minutes after tracheal intubation (T6, T7, T8).
Results:
The MBP, SBP, and DBP were significantly lower in the propofol group than in the remimazolam group (MBP: at T2, T3, T4, and T5; SBP: at T2, T3, and T4; DBP: at T5). HR was significantly lower in the propofol group at T3, T4, and T8. The incidence of hypotension was significantly higher in the propofol group than that in the remimazolam group. The incidence of bradycardia was comparable between the groups.
Conclusions:
Remimazolam induction was more stable than propofol induction in preserving normal hemodynamics and was associated with a relatively lower incidence of hypotension. Remimazolam may be preferable to propofol for induction of anesthesia in patients with hypertension.
Keywords: general anesthesia, hemodynamics, propofol, remimazolam
1. Introduction
Hemodynamic variations during the induction of general anesthesia are more profound in patients with hypertension.[1] In particular, hypotension frequently occurs during this period due to the depressant effects on the cardiovascular and central nervous system of anesthetic agents, and is related to adverse outcomes including stroke, myocardial ischemia, and renal events.[2] Patients with hypertension are more vulnerable to hypoperfusion-induced organ damage followed by hypotensive episodes. Thus, hemodynamic stability is more important in patients with hypertension than in those with normotension.
Remimazolam is a novel ultra-short-acting benzodiazepine with rapid induction and recovery properties and a safe hemodynamic profile.[3,4] Moreover, it has wide application prospects for procedural sedation and general anesthesia owing to its lack of accumulation and metabolic effects after continuous infusion.[3]
Propofol is another hypnotic widely used in clinical anesthesia because it provides smooth induction with a rapid onset time and fast awakening with rapid clearance. Although propofol has some advantages, hypotension after anesthetic induction is a noticeable side effect.[5] Some clinical studies have shown the efficacy and safety of propofol and remimazolam sedation[6,7]; however, a comparison of the hemodynamic response after propofol and remimazolam induction in patients with hypertension remains unclear.
Thus, we compared the effects of remimazolam and propofol on hemodynamic response during general anesthesia induction in patients with hypertension. The results were evaluated in relation to the incidence of hypotension associated with both drugs.
2. Materials and methods
After obtaining approval from the Institutional Review Board of our hospital (YUMC202211035), the study was registered at the Clinical Research Information Service (KCT0008191), and written informed consent was obtained from all participants. Among the patients who were scheduled for elective surgery under general anesthesia, 96 (aged 20–64 years), American Society of Anesthesiologists class II, and had taken antihypertensive drugs for >6 months were included in the study. Patients with a body mass index >0 kg/m2; suspected difficult airway; preexisting respiratory disease; severe cardiac, liver, or kidney disease; uncontrolled hypertension; and cognitive dysfunction were excluded from this study.
The patients were divided into remimazolam (Group R, n = 48) and propofol (Group P, n = 48) groups using a computer-generated random table. Standard monitoring was performed in the operating room without premedication. After checking vital signs with bispectral index, remifentanil was infused with 0.15 mcg/kg/minute for all patients. After 1 minute, in the group R, remimazolam was continuously infused at 6 mg/kg/hour until the patient lost consciousness, and in the Group P, a bolus of 1.5 to 2 mg/kg propofol was administered slowly over the course of 1 minute. After confirming loss of consciousness by modified observer’s assessment of alertness/sedation (MOAA/S) scale (score ≤1), 1 mg/kg/hour remimazolam was continuously administered until 5 minutes after tracheal intubation (Group R), and 3 to 6 mg/kg/hour propofol was continuously infused until 5 minutes after tracheal intubation (Group P). Rocuronium was administered (0.8 mg/kg), and the patients were intubated after 3 minutes. After endotracheal intubation, anesthesia was maintained using sevoflurane, oxygen, air, and remifentanil. Anesthesiologists who were not involved in this study performed the anesthetic induction and outcome assessments. Tracheal intubation was performed by another anesthesiologist blinded to the group allocation. We covered the sight of the drug infusion procedure with opaque surgical sheets for blinding of the attending anesthetic, and he was only in the operating room during endotracheal intubation.
Mean blood pressure (MBP), systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were checked at each time point: pre-induction (T1), immediately after confirming loss of consciousness (T2), at 1 and 3 minutes after neuromuscular blockade (T3, T4), immediately after endotracheal intubation (T5), and at 1, 3, and 5 minutes after endotracheal intubation (T6, T7, T8).
If the MBP was <30% of baseline or MAP was <65 mm Hg, a vasoactivator (ephedrine or phenylephrine) was administered, and if the HR decreased to <50 beats/minute, anticholinergics (atropine) was administered. In addition, the percentage changes in the above hemodynamic parameters relative to the baseline value were recorded.
2.1. Statistical analyses
Based on our preliminary study, the MBP immediately before intubation in hypertensive patients was 75 (2.385) and 72.9 (3.253) (mean [standard deviation]) in the remimazolam and propofol groups, respectively. The effect size was 0.7362. A sample size of 40 patients per group was required for 90% power with a 0.05 α. Allowing for the dropout rate, 96 patients were enrolled in this study. We used SPSS (version 23.0; Chicago, Armonk, NY) for the statistical analysis. Student t test was used to compare continuous variables, and the chi-square test or Fisher’s exact test was used to compare categorical variables. To analyze changes in hemodynamic parameters at each time point (T1–T8) within the groups, repeated-measures analysis of variance was performed. Statistical significance was set at P < .05.
3. Results
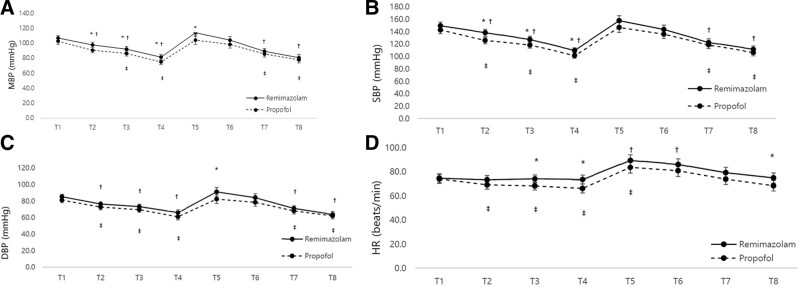
A total of 96 patients were included and analyzed in this study (Fig. 1). Demographic data, including age, sex, height, and weight, were comparable between the two groups (Table 1). MBP was lower in the propofol group than in the remimazolam group at T2, T3, T4, and T5 (P = .005, P = .022, P = .017, and P = .022, respectively) (Fig. 2A). SBP and DBP were lower in the propofol group than in the remimazolam group at T2, T3, T4, and T5 (SBP; P = .002, P = .023, and P = .009, DBP; P = .024, respectively) (Fig. 2B and C). The HR was lower in the propofol group than in the remimazolam group at T3, T4, and T8 (P = .015, P = .006, and P = .041, respectively) (Fig. 2D). In both groups, the MBP, SBP, and DBP were significantly lower at T2, T3, T4, T7, and T8, which was in contrast to baseline values (T1) (P < .0001 at all time points) (Fig. 2A–C). The HR was significantly higher at T5 and T6 than at T1 in the remimazolam group (P < .0001 at all time points) (Fig. 2D). In the propofol group, the HR was significantly lower at T2, T3, T4, and T5 than at T1 (P < .0001 at all time points) (Fig. 2D). The incidence of hypotension was significantly higher in the propofol group than in the remimazolam group (P = .014). There was no significant difference in the incidence of bradycardia between the two groups (Table 2). The percentage changes in MBP and DBP were not significantly different at any of the analyzed time points (T2, T4, T5, or T8) (Table 3). The percent change in SBP at T2 was significantly lower in the remimazolam group than that in the propofol group (P = .033), and the percent change in HR at T4 was lower in the remimazolam group than that in the propofol group (P = .049). However, there was no difference in the percentage change in SBP and HR at the other time points (Table 3).
Figure 1.
Flow diagram for the study.
Table 1.
Demographic and baseline characteristics.
| Group R (n = 48) |
Group P (n = 48) |
P value | |
|---|---|---|---|
| Age (yr) | 52.3 ± 9.09 | 52.8 ± 8.15 | .768 |
| Gender (M/F) | 26/22 | 22/26 | .541 |
| Height (m) | 164.9 ± 7.95 | 162.5 ± 8.69 | .150 |
| Weight (kg) | 73.1 ± 14.5 | 68.8 ± 15.5 | .170 |
Data are presented as mean ± SD, or number.
Group R = remimazolam group, Group P = propofol group.
Figure 2.
Changes in the hemodynamic parameters. (A) Mean blood pressure (MBP). (B) Systolic blood pressure (SBP). (C) Diastolic blood pressure (DBP). (D) Heart rate (HR). T1; baseline, T2; Immediately after LOC, T3; 1 min after muscle relaxation, T4; 3 min after muscle relaxation, T5; Immediately after tracheal intubation, T6; 1 min after tracheal intubation, T7; 3 min after tracheal intubation, T8; 5 min after tracheal intubation. *Statistically significant with a P value < .05 compared with the propofol group, †Statistically significant with a P value < .05 compared with T1 in the remimazolam group, ‡Statistically significant with a P value < .05 compared with T1 in the propofol group.
Table 2.
Incidence of hypotension or bradycardia and fluctuations in hemodynamic parameters.
| Group R (n = 48) |
Group P (n = 48) |
P value | |
|---|---|---|---|
| Total incidence of hypotension | 18 (37.5) | 31 (64.6) | .014* |
| Incidence of bradycardia | 0 (0) | 1 (2.1) | 1.000 |
Data are presented as number (%).
Group R = remimazolam group, Group P = propofol group.
Table 3.
Percent change in hemodynamic parameters.
| Group R (n = 48) |
Group P (n = 48) |
P value | |
|---|---|---|---|
| Percent change in MBP (%) | |||
| T1-T2 | 8.24 ± 10.02 | 11.41 ± 10.43 | .132 |
| T1-T4 | 23.56 ± 12.67 | 26.38 ± 14.33 | .311 |
| T1-T5 | −6.59 ± 17.97 | −2.94 ± 18.89 | .335 |
| T1-T8 | 24.56 ± 11.82 | 23.76 ± 14.27 | .766 |
| Percent change in SBP (%) | |||
| T1-T2 | 6.50 ± 10.23 | 11.30 ± 11.48 | .033* |
| T1-T4 | 25.31 ± 12.25 | 27.67 ± 14.55 | .393 |
| T1-T5 | −6.49 ± 19.36 | −4.44 ± 21.75 | .628 |
| T1-T8 | 24.00 ± 14.33 | 24.34 ± 15.66 | .912 |
| Percent change in DBP (%) | |||
| T1-T2 | 9.83 ± 13.03 | 9.72 ± 13.24 | .968 |
| T1-T4 | 22.05 ± 15.22 | 23.77 ± 19.44 | .631 |
| T1-T5 | −6.98 ± 20.98 | −2.66 ± 20.67 | .313 |
| T1-T8 | 25.20 ± 13.45 | 22.83 ± 15.72 | .429 |
| Percent change in HR (%) | |||
| T1-T2 | 1.82 ± 12.32 | 2.97 ± 21.58 | .750 |
| T1-T4 | 0.16 ± 16.36 | 9.78 ± 15.83 | .049* |
| T1-T5 | −21.54 ± 23.29 | −14.36 ± 20.87 | .115 |
| T1-T8 | −1.79 ± 20.28 | 6.02 ± 22.59 | .077 |
Data are presented as mean ± SD.
DBP = diastolic blood pressure, Group R = remimazolam group, Group P = propofol group, MBP = mean blood pressure, SBP = systolic blood pressure.
T1; baseline, T2; immediately after LOC, T4; 3 min after muscle relaxation, T5; immediately after tracheal intubation, T8; 5 min after tracheal intubation.
4. Discussion
This study showed that the hemodynamics following remimazolam induction were more stable than those following propofol induction in patients with hypertension. The incidence of hypotension during the induction period was significantly lower in the remimazolam group than that in the propofol group.
With regard to anesthetic regimens, considerable selection of induction agents is important to minimize the stress response to detrimental stimuli, such as laryngoscopy and tracheal intubation procedures. Propofol has been the most widely used hypnotic agent with many advantages, including rapid onset, short duration, and antiemetic effect, but it also has disadvantages, such as risk of cardiorespiratory depression, a decrease in systemic vascular resistance, and reduced sympathetic activity, which are associated with hypotension during the anesthetic induction period.[8,9]
Remimazolam is a novel benzodiazepine sedative. It acts on the gamma-aminobutyric acid receptor, has rapid onset and offset, and has a specific antagonist, flumazenil.[10] Its pharmacokinetic properties are a short half-life and high elimination clearance, and a short context sensitive half-life. Remimazolam is rapidly metabolized by tissue esterase (especially, liver carboxyesterase), and predominantly excreted in urine.[11] Moreover, compared to midazolam, remimazolam has lower interindividual variation in the pharmacodynamic properties and its primary metabolite has lower affinity than remimazolam.[10] Recently, the safety and efficacy of remimazolam have been demonstrated in the various sedation and surgical settings.[9,12] Remimazolam has fewer hypotensive events and cardiovascular depressant effects than propofol during general anesthesia.[9,13] However, no studies have compared the induction period hemodynamics of remimazolam and propofol in patients with hypertension.
Intraoperative hypotension, including hypotension during the induction period, is a frequent event that can increase morbidity and mortality. Patients with hypertension are more vulnerable to hypoperfusion organ damage following episodes of hypotension. Pressure dependency on organ perfusion occurs at a higher MAP than normal owing to the rightward shifting of autoregulation in patients with hypertension. Therefore, when hypotension is defined, the degree of deviation in BP based on the baseline value in the awake state may be more suitable than the lower limit value. There are several definitions of intraoperative hypotension in the literature, which cause different incidences of hypotension.[14] Zhang et al selected an MBP decrease of >30% or MBP <60 mm Hg,[2] whereas David et al chose an MBP decrease of >40% and MBP <70 mm Hg or MBP <65 mm Hg.[5] In this study, hypotension was defined as 30% less than the baseline BP value or an MAP <65 mm Hg.
Patients with hypertension are more likely to experience labile intraoperative hemodynamics. Czajka et al reported that MAP < 65 mm Hg and prolonged changes of more than 10 minutes during surgery were related to perioperative negative outcomes in patients with hypertension.[15] Levin et al also described that hypertensive patients have more often blood pressure lability intraoperatively and this property is associated with increased 30 day mortality.[16] These studies suggest that maintaining intraoperative hemodynamic stability is important for minimizing cardiovascular risk, particularly in patients with hypertension. Moreover, according to David et al, the predictors of hypotension during the anesthetic induction period include age, preoperative physical status, and anesthetic regimen, particularly propofol.[5] They suggested avoiding propofol induction in patients with American Society of Anesthesiologists > III and over 50 years of age, showing a correlation between post-anesthetic (within 10 minutes) hypotension and increased morbidity (delayed discharge or death). Our study also showed that MBP lability during the induction period was prevalent in the propofol group. Therefore, given these results, remimazolam can be considered an alternative to propofol to induce anesthesia in patients with hypertension.
This study had some limitations. Generally, the pre-anesthetic baseline BP in the operating room might be higher than that in the ward due to anxiety about anesthesia and surgery. Hypotension was defined as an MAP decrease >30% or MAP <65 mm Hg. As mentioned above, the incidence of hypotension may be high due to different definitions of hypotension and lack of anxiolytic premedication, even though there was no effect in the comparative analysis of both drugs. Second, preoperative volume status can affect the development of hypotension after induction. Several static and dynamic parameters have been proposed for measuring the preoperative volume of patients. Objective evaluation of intravascular volume status may be required despite preoperative hydration. Third, we did not check the intubation procedure time, although we excluded patients with suspected difficult airways. Laryngoscopy and tracheal intubation are strong sympathetic stimuli that affect the BP. Fourth, we measured BP during the 5 minutes post-intubation. In a study by David et al, severe hypotension after general anesthesia induction was more prevalent at 5 to 10 minutes than at 0 to 5 minutes post-induction.[5] Thus, a longer time period may be required to compare the influence of hemodynamic aberrations on remimazolam and propofol induction.
In conclusion, our study showed that remimazolam induction was more stable than propofol induction in preserving normal hemodynamics; in particular, it had a relatively lower incidence of side effects such as hypotension. Remimazolam may be preferable to propofol for induction of anesthesia in patients with hypertension. However, further studies related to expanded sample size and age range should be needed to better characterize this particular advantage.
Author contributions
Conceptualization: Eun Kyung Choi, Sang-Jin Park.
Data curation: Youngjun Jang.
Formal analysis: Eun Kyung Choi.
Investigation: Youngjun Jang.
Methodology: Eun Kyung Choi, Youngjun Jang, Sang-Jin Park.
Software: Youngjun Jang.
Supervision: Sang-Jin Park.
Validation: Eun Kyung Choi.
Writing – original draft: Eun Kyung Choi.
Writing – review & editing: Eun Kyung Choi, Sang-Jin Park.
Abbreviations:
- DBP
- diastolic blood pressure
- HR
- heart rate
- MBP
- mean blood pressure
- SBP
- systolic blood pressure
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no conflicts of interest to disclose.
How to cite this article: Choi EK, Jang Y, Park S-J. Comparison of remimazolam and propofol induction on hemodynamic response in hypertensive patients. Medicine 2023;102:30(e34358).
Contributor Information
Eun Kyung Choi, Email: zzini0527@naver.com.
Youngjun Jang, Email: 501stlegion10@gmail.com.
References
- [1].Ida M, Kimoto K, Iwata M, et al. Retrospective evaluation of predictors and frequency of hypotension in hypertensive patients after induction of general anesthesia. Masui. 2014;63:614–8. [PubMed] [Google Scholar]
- [2].Zhang J, Critchley LA. Inferior vena cava ultrasonography before general anesthesia can predict hypotension after induction. Anesthesiology. 2016;124:580–9. [DOI] [PubMed] [Google Scholar]
- [3].Keam SJ. Remimazolam: first approval. Drugs. 2020;80:625–33. [DOI] [PubMed] [Google Scholar]
- [4].Wesolowski AM, Zaccagnino MP, Malapero RJ, et al. Remimazolam: pharmacologic considerations and clinical role in anesthesiology. Pharmacotherapy. 2016;36:1021–7. [DOI] [PubMed] [Google Scholar]
- [5].Reich DL, Hossain S, Krol M, et al. Predictors of hypotension after induction of general ansesthesia. Anesth Analg. 2005;101:622–8. [DOI] [PubMed] [Google Scholar]
- [6].Chen S, Wang J, Xu X, et al. The efficacy and safety of remimazolam tosylate versus propofol in patients undergoing colonoscopy: a multicentered, randomized, positive-controlled, phase III clinical trial. Am J Transl Res. 2020;12:4594–603. [PMC free article] [PubMed] [Google Scholar]
- [7].Zhang X, Li S, Liu J. Efficacy and safety of remimazolam besylate versus propofol during hysteroscopy: single-centre randomized controlled trial. BMC Anesthesiol. 2021;21:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Jor O, Maca J, Koutna J, et al. Hypotension after induction of general anesthesia: occurrence, risk factors, and therapy. A prospective multicentre observational study. J Anesth. 2018;32:673–80. [DOI] [PubMed] [Google Scholar]
- [9].Doi M, Morita K, Takeda J, et al. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020;34:543–53. [DOI] [PubMed] [Google Scholar]
- [10].Kilpatrick GJ, McIntyre MS, Cox RF, et al. CNS 7056: a novel ultra-short-acting Benzodiazepine. Anesthesiology. 2007;107:60–6. [DOI] [PubMed] [Google Scholar]
- [11].Kim KM. Remimazolam: pharmacological characteristics and clinical applications in anesthesiology. Anesth Pain Med (Seoul). 2022;1:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dai G, Pei L, Duan F, et al. Safety and efficacy or remimazolam compared with propofol in induction of general anesthesia. Minerva Anestesiol. 2021;87:1073–9. [DOI] [PubMed] [Google Scholar]
- [13].Liu T, Lai T, Chen J, et al. Efects of remimazolam induction on hemodynamics in patients undergoing valve replacement surgery: a randomized, double-blind, controlled trial. Pharmacol Res Perspect. 2021;9:e00851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Reich DL, Bodian CA, Krol M, et al. Intraoperative hemodynamic predictors of mortality, stroke, and myocardial infarction after coronary artery bypass surgery. Anesth Analg. 1999;89:814–22. [DOI] [PubMed] [Google Scholar]
- [15].Czajka S, Putowski Z, Krzych LJ. Intraoperative hypotension and its organ-related consequences in hypertensive subjects undergoing abdominal surgery: a cohort study. Blood Press. 2021;30:348–58. [DOI] [PubMed] [Google Scholar]
- [16].Levin MA, Fischer GW, Lin H-M, et al. Intraoperative arterial blood pressure lability is associated with improved 30 day survival. Br J Anaesth. 2015;115:716–26. [DOI] [PubMed] [Google Scholar]