Abstract
Introduction:
Several studies of nonfatal fire fighters (FFs) injuries have been conducted but are limited by inclusion criteria and coverage. The aim of this study is to enhance current knowledge by providing national estimates of nonfatal injuries to fire fighters (FFs) treated in U.S. emergency departments (EDs).
Methods:
Nonfatal injuries from 2003 through 2014 were extracted from the National Electronic Injury Surveillance system occupational supplement (NEISS-Work). NEISS-Work captures nonfatal occupational injuries, illnesses, and exposures treated in a sample of U.S. EDs. Nonfatal injury rates were calculated based on NEISS-Work counts (numerator) and counts from the National Fire Protection Association (denominator). Data were analyzed from 2016 through 2017.
Results:
Between 2003 and 2014, an estimated 351,800 FFs were treated in EDs for nonfatal injuries. The overall rate was 260 per 10,000 FFs. Career FFs had an annual rate of 699; volunteers had a rate of 39. Leading injury events were fires and explosions (36%) and overexertion and bodily reactions (20%). A majority (38%) of injuries occurred during fire fighting activities, 7% occurred during training and 7% occurred during patient care. Sprains and strains accounted for the largest proportion of injuries in all three of these activities: 28%, 32%, and 36%, respectively.
Conclusions:
The results demonstrate that nonfatal injuries for FFs remained high throughout the study period. The predominance of sprains and strains in all fire fighting activities suggests the need for additional research and prevention needs in areas of improved fitness, safer body postures and movements, and situational awareness.
Keywords: fire fighters, nonfatal injuries, surveillance
Introduction
Fire fighters (FFs) perform crucial tasks to ensure public safety and health. With a workforce of over one million,1 FFs are responsible for critical public safety activities such as fighting structure and wildland fires, responding to vehicle and hazardous material incidents, and assisting during medical calls. These tasks can lead to injury and death.
Several studies have investigated nonfatal FF injuries and exposures, but were limited by inclusion and coverage. Poplin et al., characterized injuries in one medium-sized U.S. metropolitan fire department from 2004 to 2009.2 This study included paramedics and inspectors in addition to FFs. Britton et al., studied injuries among federal wildland FFs from 2003 to 2007.3 Frost et al., analyzed injuries in a large Canadian metropolitan department for 2012.4 Jahnke et al., analyzed FF injuries from eleven departments in the central U.S. from 2008 to 2010.5 Walton et al., studied workers’ compensation records for suburban FFs from 77 Illinois municipalities from 1992 to 1999.6 While the findings of these and similar studies provide insight into FF injuries, these findings are not necessarily generalizable beyond the population of interest.
The National Fire Protection Association (NFPA) produces annual national FF injury estimates from its survey of public fire departments.7 The survey collects data on injuries sustained during all types of assignments and is recognized as an important tool for the fire service. However, there are also certain limitations of the survey. The survey excludes state, federal, and private fire departments and the same departments do not consistently participate from year to year. In addition, there are no details on injury severity and it is unknown if fire departments define injuries consistently.
Because existing data are limited by inclusion criteria, comprehensive research is needed to better understand the epidemiological characteristics of FFs at a national level to help inform and direct prevention strategies. To address the gaps of previous research and existing estimates, the current study uses national data with a standardized case definition to describe nonfatal occupational injuries among FFs that were treated in emergency departments (EDs). Our study enhances knowledge of FF injuries by producing national estimates without restrictions such as establishment ownership or worker status (career vs volunteer).
Methods
Data Sources
Nonfatal occupational injuries, illnesses, and exposures to FFs from 2003 through 2014 were extracted from the occupational supplement to the National Electronic Injury Surveillance System (NEISS-Work), an ED-based surveillance system. Because only a small proportion (<5%) of FF illnesses and exposures were identified in NEISS-Work, the term “injury” will be used to refer to injuries, illnesses, and exposures.
The National Institute for Occupational Safety and Health (NIOSH) collects NEISS-Work in collaboration with the Consumer Product Safety Commission (CPSC)a. NEISS-Work is collected from a stratified probability sample of approximately 67 U.S. hospital EDs. Case identification occurs via medical chart review. An injury is considered work-related if it occurred to civilian, non-institutionalized workers working for pay or compensation, working on a farm, or volunteering for an organized group.8,9 To calculate national estimates, each NEISS-Work case is assigned a statistical weight based on the inverse probability of the hospital being selected.8,9 Individual case weights are summed to produce estimates.8,9 The NEISS-Work data are maintained by NIOSH as restricted-access data. Review was not required by NIOSH’s Institutional Review Board since the analysis was conducted using existing surveillance data and did not include any personal identifiers.
NEISS-Work event/exposure information was coded based on the BLS Occupational Injury and Illness Classification System (OIICS). Data prior to 2011 were coded based on version 1.01.10 Data from 2011 to 2014 were coded based on OIICS version 2.01.11 Version 2.01 was a major revision to version 1.01 and was considered a break in series.10
Labor force estimates for FFs were obtained from the NFPA National Fire Experience Survey.12 Survey data are collected two ways: through a sample of fire departments (FDs) stratified into nine categories based on size of the community protected by the FD for populations of 2,500 or more; and from a random sample of FDs protecting communities with less than 2,500.12 National estimates are calculated by weighting results according to the proportion of the total U.S. population accounted for by communities in each of the ten strata. Estimates are available by year, age group, and worker status.
Case Identification
This analysis included FFs treated in EDs for injuries related to on-duty functions. Common on-duty functions included fighting fire; salvage and overhaul; responding to/returning from an incident; training; equipment and building maintenance; public education; and fundraising. FFs are often cross-trained as emergency medical services (EMS) workers so FFs providing patient care are also included. Various occupations were excluded such as administrator, EMS worker with no indication of concurrent FF employment, clerk, communications operator, dispatcher, mechanic, fire investigator, forest service ranger, lifeguard, maintenance worker, cook, and ambulance driver. While the criteria used for this study were more restrictive than criteria used by other systems,13 it insured that correct cases were included with a high degree of confidence.
Since NEISS-Work does not include standardized industry and occupation codes, a stepwise process was used to identify cases. The inclusion/exclusion criteria noted above was used to develop a list of keywords to search ‘business type,’ ‘employer type,’ and ‘occupation type’ from 2003 through 2014. The 12,400 unweighted cases initially identified were categorized as: clearly a FF, not a FF, possibly a FF, or missing information. If all three variables listed above were clearly FF-related, cases were automatically included without further review (n=5,100, 41%). For the remaining cases (n=7,300, 59%), narrative text was manually reviewed to determine FF status. If the worker was participating in any on-duty functions noted above, the case was kept. Three of the study’s authors reviewed all questionable cases; consensus was required to keep the cases. Of the 7,300 cases, 1,900 were included after manual review. As a final step, the 7,000 cases included were assigned a work activity code that reflected the task being done when the IE occurred: activities directly related to fighting fires, training, patient care, physical activity excluding formal training, and all other activities. Training included formal training such as FD drills, FD training, fire training academy, or fire school. Physical activity included non-formal activities. One author initially assigned these codes while a second author reviewed the codes. All questionable code assignments were further reviewed by other authors to reach consensus.
Data analyses
Data were analyzed in 2016–2017. Estimates, variances and 95% confidence intervals (CIs) were calculated using PROC SURVEYMEANS in SAS version 9.3. All variables were analyzed for 2003 to 2014 except two, event and worker status. Due to the OIICS break in series, analyses by event were limited to 2011 through 2014 data. Worker status (career, volunteer) was only available from NEISS-Work for 2009 forward. Career workers include both public and private workers. Average annual rates were calculated as the estimated nonfatal injuries from NEISS-Work divided by the estimated FFs from NFPA and expressed as the number of injuries per 10,000 FFs. For comparison purposes, an annual average rate was calculated for all other workers. This rate was calculated as the estimated nonfatal injuries for all workers except FFs from NEISS-Work divided by the estimated number of all other workers (except FFs) from the Current Population Survey (CPS), a national household survey conducted monthly on approximately 60,000 non-institutionalized residents.14 An annual average rate was calculated for all other workers excluding FFs aged 16 years and older and expressed as the number of nonfatal work injuries per 10,000 workers. Because the CPS is not designed to comprehensively capture volunteers, the CPS was not used to calculate rates for FFs.
Results
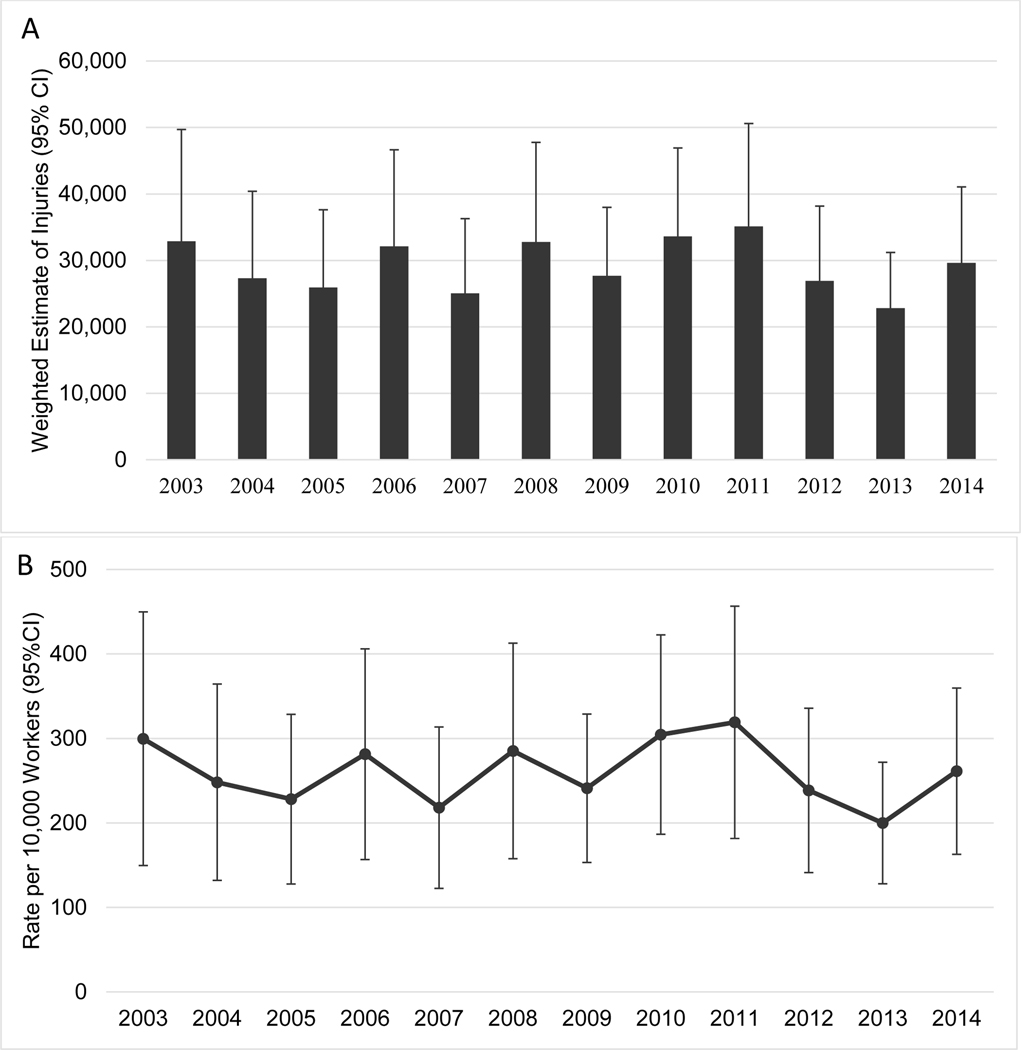
From 2003 through 2014, an estimated 351,800 FF injuries were treated in EDs (Table 1). The highest annual estimate (32,900, CI=16,100, 49,700) occurred in 2003 while the lowest (22,800, CI=14,400, 37,200) occurred in 2013 (Figure 1a). Male FFs sustained a majority of the injuries (95%) (Table 1). FFs aged 30 to 39 years old sustained the largest percentage of injuries (35%). In contrast, workers 20 to 29 years old sustained the largest percentage of injuries for all other U.S. workers (29%, CI=27%, 31%) while workers 30 to 39 accounted for the second largest percentage (24%, CI=23%, 25%) of injuries among all other U.S. workers. Among the 175,800 (CI=113,900, 237,700) FF injuries from 2009 through 2014, 82% (144,200, CI=83,700, 204,700) occurred to career FFs and 10% (18,400, CI=9,400, 27,400) occurred to volunteers (data not shown). The remaining 8% (13,200, CI=93,000, 17,100) had other or unknown worker statuses.
Table 1.
Characteristics of fire fighters treated in emergency departments for a work-related injury, 2003–2014 (NEISS-Work).
| Characteristic | Weighted Estimate (95% CIs) | Weighted Percent | Rates per 10,000 fire fighters (95% CIs) |
|---|---|---|---|
|
| |||
| Total a | 351,800 (225500, 478100) | 100 | 260 (168, 252) b |
| Sex | |||
| Male | 333,500 (210000, 457000) | 95 | --c |
| Female | 18,200 (11300, 25100) | 5 | -- |
| Age (years) | |||
| 16–19 | 12,900 (6600, 19200) | 4 | 269 (141, 410) |
| 20–29 | 95,900 (58300, 133500) | 27 | 332 (205, 459) |
| 30–39 | 124,300 (67100, 181500) | 35 | 330 (182, 182) |
| 40–49 | 80,500 (51100, 109900) | 23 | 232 (149, 381) |
| 50–59 | 30,800 (21300, 40300) | 9 | 145 (101, 189) |
| 60 years and older | 6,900 (3100, 10700) | 2 | 86 (40, 132) |
| Task d | |||
| Fire Fighting | 134,900 (71900, 197900) | 38 | -- |
| Training | 23,100 (12000, 34200) | 7 | -- |
| Patient Care | 23,800 (11800, 35800) | 7 | -- |
| Physical Activity, excluding Training | 5,400 (1700, 9100) e | 2 | -- |
| Other/Unknown Activity | 164,500 (102400, 226600) | 47 | -- |
| Diagnosis d | |||
| Sprain/Strain | 118,200 (63800, 172600) | 34 | -- |
| Contusions/Abrasions | 49,200 (26100, 72300) | 14 | -- |
| Laceration | 26,300 (17600, 35000) | 7 | -- |
| Fracture/Dislocation | 16,900 (11900, 21900) | 5 | -- |
| Puncture | 6,200 (3800, 3800) | 2 | -- |
| Otherf | 135,000 (90600, 57900) | 38 | -- |
| Body part d | |||
| Lower Extremities | 73,400 (46800, 100000) | 21 | -- |
| Trunk | 65,100 (35800, 94400) | 19 | -- |
| Head and Face | 42,600 (29600, 55600) | 12 | -- |
| Hand and Fingers | 41,800 (29300, 54300) | 12 | -- |
| Shoulder | 32,900 (9400, 56400) | 9 | -- |
| Upper Extremities | 27,300 (15800, 38800) | 8 | -- |
| Neck | 15,100 (5200, 25000) | 4 | -- |
| All Other Body Parts | 53,500 (37300, 69700) | 15 | -- |
NEISS-Work: National Electronic Injury Surveillance System—occupational supplement
Weighted estimates and percentages may not add to totals due to rounding
Confidence interval for the rate does not include error associated with the denominator and likely underestimates the total rate variance
Denominator data for sex was not available for the entire 12-year period
Rates were not calculated for task, diagnosis, and body part
Estimate is statistically unreliable with a coefficient of variation of 34%
“Other” diagnosis includes burns, anoxia, dermatitis, internal injuries, poisonings, foreign body, concussions, electric shock, crushing, and other diagnoses that did not meet minimum reporting requirements
Figure 1A:
Weighted estimates of nonfatal injuries to fire fighters treated in emergency departments, 2003–2014
Figure 1B: Rates of nonfatal injuries per 10,000 fire fightersa treated in emergency departments, 2003–2014
a Denominator data are from the NFPA fire department profile [NFPA 2016b]
The annual average rate of injuries per 10,000 FFs was 260 (CI=168, 352) (Table 1). The FF rate was 1.2 times higher than the nonfatal ED-treated injury rate of 214 per 10,000 workers (CI=172, 256) for all other U.S. workers (except FFs). The highest rate (300, CI=150, 450) was in 2003; the lowest (200, CI=128, 272) was in 2013 (Figure 1b). FFs aged 20 to 29 had the highest rate of 332 injuries per 10,000 FFs while FFs 60 years and older had the lowest rate (86). Career FFs had an annual rate of 699 per 10,000 FFs (CI=411, 987) while volunteers had a rate of 39 (CI=20, 58).
From 2003 through 2014, 38% of FF injuries occurred during fire fighting activities while 7% occurred during training and 7% occurred during patient care (Table 1). Forty-seven percent (47%) could not be assigned distinct activity codes due to limited information contained in the record. From 2009 through 2014, career FFs had similar percentages by worker activity (data not shown). However, over half (55%, 10,200, CI=4,600, 15,800) of the injuries to volunteer FFs occurred during fire fighting activities.
Of the FF injuries from 2003 through 2014, 97% (340,200, CI=216,000, 464,400) were treated and released (data not shown). The most common injuries were sprains and strains (34%) and contusions and abrasions (14%) (Table 1). Body parts most commonly affected were lower extremities (21%) and the trunk (19%) (Table 1).
From 2003 through 2014, the most common injuries during fire fighting activities were sprains and strains (28%, 37,200b, CI=13,800, 60,600) and contusions and abrasions (13%, 17,300c, CI=6,100, 28,500) (data not shown). Training and patient care activities both most often involved resulted in sprains and strains. Sprains and strains account for 32% (7,300, CI=3,700, 11,000) of training activities and 36% (8,600d, CI=3,100, 14,100) of patient care activities.
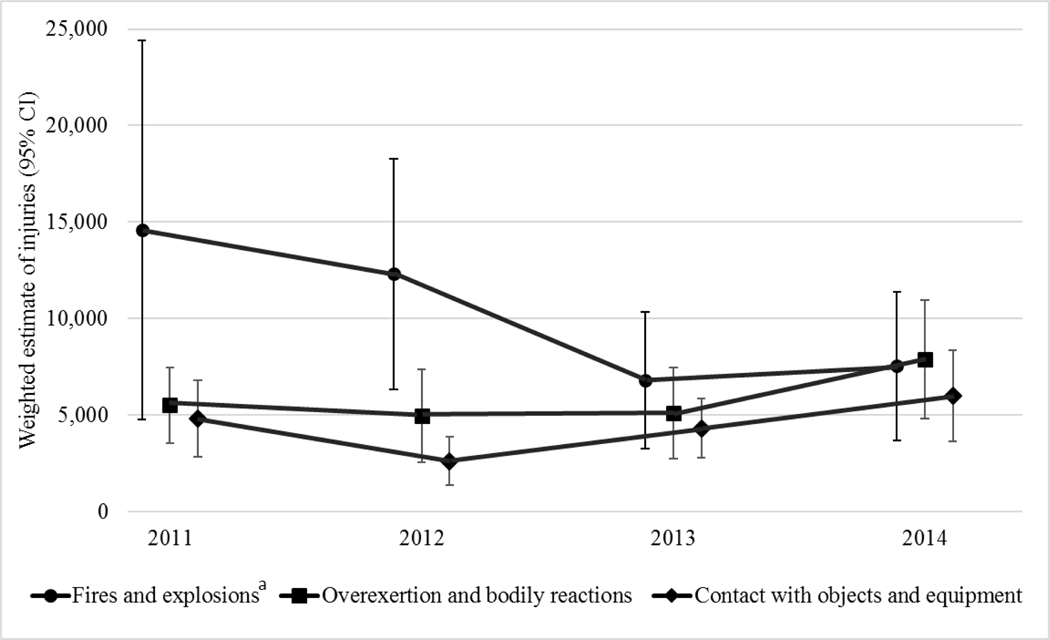
From 2011 through 2014, events frequently leading to nonfatal injuries were fires and explosions (36%) and overexertion and bodily reactions (includes injuries caused by excessive physical effort and working in an awkward position) (20%) (Table 2). Leading events for career and volunteer FFs were similar. However, fires and explosions accounted for almost half of the injuries among volunteers. Between 2011 and 2014, the number of injuries resulting from fires and explosions for all FFs decreased 48%, while the number of injuries resulting from overexertion and bodily reactions increased 43% (Figure 2). For this same period, sprains and strains, the leading diagnosis, were most usually caused by overexertion and bodily reactions (14,400, CI=9,500, 23,900), fires and explosions (10,300, CI=1,900, 18,700), and falls, slips, trips (8,300, CI=4,300, 12,300) (data not shown).
Table 2:
Event by worker status for fire fighters treated in emergency departments, 2011 through 2014 (NEISS-Work).
| Event or exposurea | Career | Volunteer | Total | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Weighted Estimate (95% CIs) | Weighted Percent | Weighted Estimate (95% CIs) | Weighted Percentb | Weighted Estimate (95% CIs) | Weighted Percentb | |
| Fires and explosions | 34,200 b (12900, 34200) | 35 | 6,600 (3100, 10100) | 46 | 41,300 (20400, 62200) | 36 |
|
| ||||||
| Overexertion and bodily reactions | 20,600 (13100, 28100) | 23 | 2,200 (900, 3500) | 16 | 23,400 (15800, 31000) | 20 |
|
| ||||||
| Contact with objects and equipment | 14,600 (9800, 19400) | 14 | 2,700b (1000, 4400) | 16 | 17,800 (12400, 23200) | 16 |
|
| ||||||
| Falls, Slips, Trips | 14,800 (10800, 23500) | 15 | -- c | -- c | 16,900 (8300, 25500) | 15 |
|
| ||||||
| Exposures to harmful substances or environments | 8,600 (4600, 12600) | 7 | -- c | -- c | 9,300 (5000, 13600) | 8 |
|
| ||||||
| Transportation incidents | 2,500b (1000, 4000) | 3 | -- c | -- c | 2,700 (1200, 4200) | 2 |
|
| ||||||
| Violence and other injuries by persons or animals | 1,900b (600, 3200) | 2 | -- c | -- c | 2,200 (900, 3500) | 2 |
|
| ||||||
| Nonclassifiable | -- c | -- c | -- c | -- c | -- c | -- c |
|
| ||||||
| Total d | 98,100 (55600, 140600) | 100 | 14,200 (7300, 21100) | 100 | 114,500 (72800, 187300) | 100 |
NEISS-Work: National Electronic Injury Surveillance System—occupational supplement
Event or exposure coded using the Occupational Injury and Illness Classification System (OIICS) Version 2.01 (2012)
Estimate is statistically unreliable with a coefficient of variation greater than 30%
Estimate did not meet minimum reporting requirements
Weighted estimates and percentages may not add to totals due to rounding
Figure 2:
Weighted estimates of nonfatal injuries to fire fighters treated in emergency departments by event, 2011–2014
a Estimate for 2011 is statistically unreliable with a coefficient of variation of 34%
Note: Data points for each year are adjusted slightly to aid visualization.
Discussion
Identifying and understanding risks that FFs face is complex as no single, comprehensive data source exists.15 Therefore, risks must be identified via analysis of available data, including the ED data used in the current study. This study offers a national perspective of nonfatal FF injuries without establishment ownership or industry restrictions. Based on the findings, it is clear that FF injuries treated in EDs remained high and relatively unchanged throughout the 12-year study period. These findings are similar to the national findings from the NFPA.7
Like other research,5,7,16–20 this study found sprains and strains – not burns – were the most common injury among FFs. Sprains and strains accounted for the largest proportion in the three primary activities that fire fighters undertake: fire fighting, training, and patient care. Because fire fighting involves strenuous work, dangerous and unpredictable environments, and heavy personal protective equipment (PPE),21 it follows that FFs are at an increased risk for sprains and strains. It is crucial to consider possible approaches to preventing sprains and strains from occurring, including fitness, training, and situational awareness.
A FFs overall fitness and health are critical factors in injury occurrence and severity.22,23 Poplin et al.,22 found an association between lower fitness levels and increased injury risk among career FFs. To execute physically demanding jobs properly and safely, FFs should achieve and maintain some degree of physical fitness. This can be encouraged by departments through worksite health promotion.24,25 However, Stefano describes obstacles to workers participating in wellness programs including lack of information on risk, lack of appropriate training, and lack of motivation.26 The NFPA 1583 Standard on Health-Related Fitness Programs is a positive, nonpunitive tool that outlines five components that FDs can implement to improve members’ health and fitness.21,27 The National Volunteer Fire Council, and the International Association of Fire Fighters/International Association of Fire Chiefs also have health and fitness initiatives that can be implemented. Regardless of the program, training FFs on the importance of proper physical fitness can potentially lead to improved fire fighter safety and health2,5–7,19,20,28 and ultimately in a reduction in the number of sprains and strains.
While standard injury prevention recommendations from the Occupational Safety and Health Administration (OSHA) such as keeping the work environment free of clutter, using caution on slippery or uneven surfaces, and avoiding strenuous activity when tired30 are feasible in controlled environments, these practices are generally not options for FFs who have little control over their work environment.31 Therefore, regular education and training for FFs on the risks of heavy and awkward lifting, and working on slippery and uneven surfaces2,5,6,19,20,28 are imperative. Ensuring that staff are trained on safe lifting techniques, the use of ergonomically appropriate equipment, and the importance of proper physical fitness can potentially lead to improved fire fighter safety and health.2,5,6,16–18,28,29
A discussion on injury prevention for FFs would not be complete without mentioning situational awareness and risk management. Many emergency scenes have competing distractions, making situational awareness a challenge for FFs. Kunadharaju et al., noted that risks can in fact “become so commonplace that their significance is diminished to the point that they are accepted as normal….”32 Situational awareness begins the moment a call comes in and involves company officers, safety officers, incident commanders, and fire fighters. Risk management is described in NFPA 1500.33 This standard suggests that the department identify and train someone as a safety officer to ensure that risks are identified and controlled at an emergency scene. Implementing a risk management system that involves risk identification and situational awareness may potentially reduce injuries, including sprains and strains.
A majority of injuries in this study occurred to career FFs (82%) with a rate of 699 per 10,000 workers (CI=411, 987), 18 times higher than the volunteer FF rate (39 per 10,000 workers, CI=20, 58). This finding is similar to previous research.16 Higher rates for career FFs may be explained by the fact that career FFs are on duty more than volunteer FFs.34 Career FFs respond to more incidents and work longer shifts than volunteers who generally work as needed.34,35 Given the differences in levels of emergency response, population-based rates such as those presented here do not adequately account for hours that career and volunteer FFs actually work. Improved data accounting for actual on-duty hours are needed to determine differences in rates between career and volunteer FFs.
Limitations
The most significant limitations of this study are related to case identification using NEISS-Work. First, because NEISS-Work does not include standardized occupation or industry codes, a systematic methodology was established to identify cases. This approach erred on specificity over sensitivity and it is possible that FFs were missed in the case-identification approach. Furthermore, because the data only include ED-treated injuries, the study did not include injuries not needing immediate care, treated in other medical venues, or self-treated. Case capture may be incomplete despite succinct definitions of what constitutes work-relatedness. For example, injuries may not be identified as work-related because of a lack of information provided by the worker at the time of treatment, incomplete medical records, or errors in abstraction. Finally, NEISS-Work does not contain information on potential confounding factors such as work conditions, lifestyle factors, and physical or mental co-morbidities, and does not contain specific details regarding PPE use.
Conclusion
Unlike other studies that have explored FF injuries, the findings from this study are not restricted by establishment ownership or worker status (career vs volunteer). This study provides systematically collected and nationally representative nonfatal ED-treated FF injuries. The results demonstrate that FFs incurred ED-treated occupational injuries at a higher rate than the general workforce from 2003 through 2014. The predominance of sprains and strains suggests additional research and prevention needs in the area of improved physical fitness programming, training on safety body postures and movements, and an increased focus on situational awareness.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC). Mention of any company or product does not constitute endorsement by NIOSH. In addition, citations to websites external to NIOSH do not constitute NIOSH endorsement of the sponsoring organizations or their programs or products. Furthermore, NIOSH is not responsible for the content of these websites. All web addresses referenced in this document were accessible as of the publication date.
Footnotes
While NIOSH collects NEISS-Work in collaboration with CPSC, there are no implied or expressed endorsements of the results presented herein by the CPSC.
Estimate is statistically unreliable with a coefficient of variation of 31%.
Estimate is statistically unreliable with a coefficient of variation of 32%.
Estimate is statistically unreliable with a coefficient of variation of 32%.
The authors of this manuscript do not have any conflicts of interest or financial disclosures.
Contributor Information
Suzanne M Marsh, National Institute for Occupational Safety and Health, Division of Safety Research, Surveillance and Field Investigations Branch, Morgantown, WV..
Melody Gwilliam, National Institute for Occupational Safety and Health, Division of Safety Research, Analysis and Field Evaluations Branch, Morgantown, WV.
Srinivas Konda, National Institute for Occupational Safety and Health, Division of Safety Research, Analysis and Field Evaluations Branch, Morgantown, WV.
Hope M. Tiesman, National Institute for Occupational Safety and Health, Division of Safety Research, Analysis and Field Evaluations Branch, Morgantown, WV.
Rita Fahy, National Fire Protection Association, Applied Research, Quincy, MA.
References
- 1.National Fire Protection Association. Fourth needs assessment of the U.S. fire service. http://www.nfpa.org/news-and-research/fire-statistics-and-reports/fire-statistics/the-fire-service/administration/needs-assessment. Published 2015. Accessed June 2017.
- 2.Poplin GS, Harris RB, Pollack KM, et al. Beyond the fireground: Injuries in the fire service. Inj Prev. 2012;18:228–233. 10.1136/injuryprev-2011-040149. [DOI] [PubMed] [Google Scholar]
- 3.Britton C, Ramirez M, Lynch CF, et al. Risk of injury by job assignment among federal wildland firefighters, United States, 2003–2007. Int J Occup Environ Health. 2013;19:77–84. 10.1179/2049396713Y.0000000019. [DOI] [PubMed] [Google Scholar]
- 4.Frost DM, Beach TAC, Crosby I, et al. The cost and distribution of firefighter injuries in a large Canadian fire department. Work. 2016;55:497–504. 10.3233/WOR-162420. [DOI] [PubMed] [Google Scholar]
- 5.Jahnke SA, Poston WS, Haddock CK, et al. Injury among a population based sample of career firefighters in the central USA. Inj Prev. 2013;19(6):393–398. 10.1136/injuryprev-2012-040662. [DOI] [PubMed] [Google Scholar]
- 6.Walton SM, Conrad KM, Furner SE, et al. Cause, type, and workers’ compensation costs of injury to fire fighters. Am J Ind Med. 2003;43:454–458. http://onlinelibrary.wiley.com/doi/10.1002/ajim.10200/epdf. [DOI] [PubMed] [Google Scholar]
- 7.National Fire Protection Association. Haynes HJG, Molis JL U.S. firefighter injuries - 2016. http://www.nfpa.org/news-and-research/fire-statistics-and-reports/fire-statistics/the-fire-service/fatalities-and-injuries/firefighter-injuries-in-the-united-states. Published 2017. Accessed November 2017. [Google Scholar]
- 8.Jackson LL. Nonfatal occupational injuries and illnesses treated in hospital emergency departments in the United States. Inj Prev. 2001;7(Suppl):i21–i26. 10.1136/ip.7.suppl_1.i21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Derk SJ, Marsh SM, Jackson LL. Nonfatal occupational injuries and illnesses—United States, 2004. MMWR Morb Mortal Wkly Rep. 2007;56:393–397. [PubMed] [Google Scholar]
- 10.U.S. Department of Labor, Bureau of Labor Statistics. BLS handbook of methods, chapter 9. Occupational safety and health statistics. https://www.bls.gov/opub/hom/pdf/homch9.pdf. Published 2012. Accessed June 2017.
- 11.U.S. Department of Labor, Bureau of Labor Statistics. Occupational injury and illness classification manual. http://www.bls.gov/iif/osh_oiics_2010_1.pdf. Published 2012. Accessed June 2017.National Fire Protection Association. [Google Scholar]
- 12.U.S. Fire Department Profil. http://www.nfpa.org/news-and-research/fire-statistics-and-reports/fire-statistics/the-fire-service/administration/us-fire-department-profile. Published 2016. Accessed June 2017. [Google Scholar]
- 13.Estes CR, Marsh SM, Castillo DN. Surveillance of traumatic firefighter fatalities: An assessment of four systems. Pub Health Rep. 2011;126:540–551. http://journals.sagepub.com/doi/pdf/10.1177/003335491112600410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Department of Labor, Bureau of Labor Statistics. BLS handbook of methods, chapter 1. Labor force data derived from the current population survey. https://www.bls.gov/opub/hom/pdf/homch1.pdf. Published 2012. Accessed October 2017.
- 15.Widman SA, LeVasseur MT, Tabb LP, et al. The benefits of data linkage for firefighter injury surveillance. Inj Prev. 2017;0:1–10. doi: 10.1136/injuryprev-2016-042213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reichard AA, Jackson LL. Occupational injuries among emergency responders. Am J Ind Med. 2010;53:1–11. 10.1002/ajim.20772. [DOI] [PubMed] [Google Scholar]
- 17.Griffin SC, Regan TL, Harber P, et al. Evaluation of a fitness intervention for new firefighters: injury reduction and economic benefits. Inj Prev. 2016;22(3):181–188. 10.1136/injuryprev-2015-041785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong O, Chin DL, Phelps S, et al. Occupational injuries, duty status, and factors associated with injuries among firefighters. Workplace Health Saf. 2012;60(12):517–23. 10.3928/21650799-20121116-08. [DOI] [PubMed] [Google Scholar]
- 19.Bureau of Labor Statistics. Kurlick GM Stop, drop, and roll: workplace hazards of local government firefighters, 2009. Monthly Labor Review. 2012. [Google Scholar]
- 20.Moore-Merrell L, Zhou A, McDonald-Valentine S, et al. Contributing factors to firefighter line of duty injury in metropolitan fire departments in the United States. Washington, DC: International Association of Firefighters, 2008. [Google Scholar]
- 21.Denise S. Firefighter fitness: Improving performance and preventing injuries and fatalities. Current Sports Medicine Report. 2011; 10(3):167–172. https://journals.lww.com/acsm-csmr/Fulltext/2011/05000/Firefighter_Fitness__Improving_Performance_and.13.aspx. [DOI] [PubMed] [Google Scholar]
- 22.Poplin GS, Roe DJ, Peate W, et al. The association of aerobic fitness with injuries in the fire service. A J Epi. 178(2):149–155. 10.1093/aje/kwt213. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Fire Administration. Health and wellness guide for the volunteer fire and emergency services. https://www.usfa.fema.gov/downloads/pdf/publications/fa_321.pdf. Published 2009. Accessed February 2018.
- 24.Elliot DL, Goldberg L, Duncan TE, et al. The PHLAME firefighters’ study: Feasibility and findings. Am J Health Behav. 2004;28(1):13–23. [DOI] [PubMed] [Google Scholar]
- 25.MacKinnon DP, Elliot DL, Thoemmes F, et al. Long-term effects of a worksite health promotion program for firefighters. Am J Health Behav. 2010;34(6):695–706. [DOI] [PubMed] [Google Scholar]
- 26.Stefano M. Avoid the 5 reasons fitness plans fail. http://www.howtobefit.com/fitness-success-plan.htm. [Google Scholar]
- 27.National Fire Protection Association. NFPA 1583: Standard on health related fitness programs for fire department members. Quincy, MA. [Google Scholar]
- 28.Jahnke SA, Poston WS, Haddock CK, et al. Obesity and incident injury among career firefighters in the central United States. Obesity. 2013;21(18):1505–1508. [DOI] [PubMed] [Google Scholar]
- 29.Smith TD, Dejoy DM. Safety climate, safety behaviors and line-of-duty injuries in the fire service. Int J Emerg Med. 2014;3:49–64. 10.1108/IJES-04-2013-0010. [DOI] [Google Scholar]
- 30.Public Law 91–596. 1970. Occupational safety and health act of 1970. Washington, D.C.: 91st Congress, s.2193. [Google Scholar]
- 31.Sprains Langbell A., strains and muscle injuries. Fire Engineering. 2016. http://www.fireengineering.com/articles/2016/01/firefighter-training-sprains-strains.html. [Google Scholar]
- 32.Kunadharaju K, Smith TD, Dejoy DM. Line-of-duty deaths among U.S. firefighters: An analysis of fatality investigations. Accid Anal Prev. 2011;43(3):1171–1180. 10.1016/j.aap.2010.12.030. [DOI] [PubMed] [Google Scholar]
- 33.National Fire Protection Association. NFPA 1500: Standard on fire department occupational safety and health program. Quincy, MA. [Google Scholar]
- 34.Plat MJ. Frings-Dresen MHW, Sluiter JK. Which subgroups of fire fighters are more prone to work-related diminished health requirements? Int Arch Occup Env Health. 2012;85(7): 775–82. https://link.springer.com/article/10.1007%2Fs00420-011-0720-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Petruzzello S, Poh PYS, Greenlee TA, et al. Physiological, perceptual and psychological responses of career versus volunteer firefighters to live-fire training drills. Stress and Health. 2014;13: 328–336. 10.1002/smi.2620. [DOI] [PubMed] [Google Scholar]