Abstract
Polymer-based hydrogels are hydrophilic polymer networks with crosslinks widely applied for drug delivery applications because of their ability to hold large amounts of water and biological fluids and control drug release based on their unique physicochemical properties and biocompatibility. Current trends in the development of hydrogel drug delivery systems involve the release of drugs in response to specific triggers such as pH, temperature, or enzymes for targeted drug delivery and to reduce the potential for systemic toxicity. In addition, developing injectable hydrogel formulations that are easily used and sustain drug release during this extended time is a growing interest. Another emerging trend in hydrogel drug delivery is the synthesis of nano hydrogels and other functional substances for improving targeted drug loading and release efficacy. Following these development trends, advanced hydrogels possessing mechanically improved properties, controlled release rates, and biocompatibility is developing as a focus of the field. More complex drug delivery systems such as multi-drug delivery and combination therapies will be developed based on these advancements. In addition, polymer-based hydrogels are gaining increasing attention in personalized medicine because of their ability to be tailored to a specific patient, for example, drug release rates, drug combinations, target-specific drug delivery, improvement of disease treatment effectiveness, and healthcare cost reduction. Overall, hydrogel application is advancing rapidly, towards more efficient and effective drug delivery systems in the future.
Keywords: hydrogels, drug delivery, multi-sensitive hydrogels, biopolymers, nanoparticles
1. Introduction
Drug delivery systems (DDS) play a critical role in optimizing the therapeutic efficacy of drugs by addressing the limitations of traditional drug formulations [1,2]. These limitations include low bioavailability, poor solubility, and a short half-life, which can significantly impact drug efficacy and necessitate frequent dosing [2,3]. However, controlled drug delivery systems, such as polymer-based hydrogels [4], offer a promising solution by enabling sustained drug release for a long time [4,5]. This sustained-release property helps maintain therapeutic drug concentrations within the desired range [6], avoiding a sudden increase or decrease that can lead to suboptimal treatment outcomes [7,8,9]. By extending the release duration, polymer-based hydrogels enhance drug bioavailability [8,10] and reduce the frequency of dosing, supporting patient compliance and convenience [7,11]. Additionally, DDSs including polymer-based hydrogels offer the potential for targeted drug delivery to specific tissues or organs [3,8,12]. By incorporating targeting ligands [13] or modifying the polymer-based hydrogel’s properties [10,14], drugs can be directed to their intended sites of action [3,8]. This targeted approach minimizes systemic exposure [15] and reduces the potential for off-target side effects, while maximizing therapeutic efficacy at the desired site [16,17]. Moreover, DDSs can be tailored to accommodate a wide range of drugs with different physicochemical properties [18]. In particular, polymer-based hydrogels offer versatility in drug loading [8] and release mechanisms [19], allowing for the delivery of various types of drugs with small molecules such as proteins [20,21], peptides [22], and nucleic acids [23]. This flexibility makes polymer-based hydrogels an attractive topic for researchers as well as for their applications in the treatment of various medical conditions.
Polymer-based hydrogels are extraordinary materials composed of crosslinked hydrophilic polymers that possess the remarkable ability to absorb and retain large amounts of water and biological fluids while maintaining their three-dimensional structure [24,25]. This unique property, along with their high water content [26,27], porosity [28,29,30,31], and soft consistency [32], makes polymer-based hydrogels highly attractive for a wide range of biomedical applications such as drug delivery [33,34], tissue engineering [35,36], and wound healing [37,38,39]. In fact, polymer-based hydrogels exhibit properties that closely mimic those of natural tissues [40,41], making them an excellent choice for various biomedical applications [17,42,43]. The swelling capability of polymer-based hydrogels is particularly noteworthy, as it allows them to absorb and retain significant amounts of water and biological fluids [44,45], rendering them a highly desirable material for use in medicine and healthcare applications [46,47]. This property enables the polymer-based hydrogels to create a unique environment that facilitates essential biological interactions [48,49], such as cell proliferation [50,51], adhesion [52,53], and differentiation [54,55]. Consequently, polymer-based hydrogels have emerged as promising candidates for tissue engineering [56,57,58] and regenerative medicine applications [59,60].
Polymer-based hydrogels are able to regulate the release of drugs by controlling their swelling behavior leading to sustained drug delivery for a long time [61,62,63]. When loaded with drugs, hydrogels can hold them within their porous structure, gradually releasing them in a controlled manner [63,64]. By modulating the compositions and structures of the hydrogel, the release kinetics and time can be precisely tailored to meet the therapeutic requirements [19,65,66]. This sustained drug release capability of hydrogels offers advantages such as a prolonged therapeutic effect [11,67,68], reduced dosing frequency [3,8,69], and improved patient compliance [8,11]. In addition to sustained drug delivery, polymer-based hydrogels can be engineered to respond to specific stimuli [70,71]. By incorporating responsive components into the hydrogel matrix [72,73], such as temperature-sensitive polymers [74,75] or pH-sensitive moieties [76,77,78], drug release can be triggered [32,79,80] or modulated upon exposure to specific environmental cues [65]. This feature enables targeted drug delivery, where the hydrogel selectively releases the drug at the site of action [81,82], minimizing systemic side effects [8,11,83] and maximizing therapeutic efficacy [6,11,84,85].
The unique properties of polymer-based hydrogels make them versatile for various medical [86,87,88] and healthcare applications [3,8,11,17]. Their biocompatibility, soft consistency, and high water content allow polymer-based hydrogels to closely resemble living tissues [32,41,89], making them suitable for biomedical applications such as tissue engineering [2,56,57,58,90] and regenerative medicine [42,91]. Polymer-based hydrogels can provide a supportive three-dimensional scaffold for cells to proliferate [92,93], adhere, and differentiate, facilitating tissue regeneration [41,89] and repair processes [94,95,96,97]. Moreover, the ability of polymer-based hydrogels to absorb and retain water creates a favorable environment for cellular interactions [98,99,100], promoting favorable biological responses [101,102]. Beyond drug delivery and tissue engineering, hydrogels find utility in biosensing applications [13,15,103]. By incorporating specific bioactive molecules or sensors into the hydrogel network, changes in the surrounding environment [16,17,29], such as the presence of target analytes, can be detected and transduced into measurable signals [81,104,105]. This capability opens up opportunities for the development of diagnostic platforms [11,83,106], implantable biosensors [13,15,69,107,108], and smart drug delivery systems [11,56,109].
The current article presents several notable features and innovations compared to previously published articles in similar fields with analysis and evaluation on the hydrogels produced from polymers applied in drug delivery systems. It adds to the existing body of knowledge by presenting novel concepts, methodologies, and applications that contribute to advancements in the field. These innovations have the potential to enhance the efficacy, safety, and patient compliance of drug delivery systems, paving the way for more modern changes in biomedicine materials.
2. Classification of Drug Delivery Systems
Drug delivery systems play a crucial role in optimizing the therapeutic efficacy of drugs by controlling their release [110,111], targeting specific tissues or organs [12,14,81,82], and reducing potential side effects [8,9,11]. In this article, the classification of drug delivery systems based on conventional and novel systems is presented in Table 1. This classification provides a framework for understanding the different approaches and technologies employed in drug delivery research and development. Drug delivery systems can be classified based on several criteria with two main groups including conventional or traditional drug delivery systems and novel drug delivery systems [3,8,11,112,113].
Table 1.
| Types of Drug Delivery Systems | Categories |
|---|---|
| Conventional or traditional drug delivery systems | Oral delivery |
| Buccal or sublingual delivery | |
| Rectal delivery | |
| Intravenous delivery | |
| Subcutaneous delivery | |
| Intramuscular delivery | |
| Novel or controlled-release drug delivery systems | Rate-preprogrammed |
| Activation-modulated | |
| Feedback-regulated | |
| Site-targeting |
2.1. Conventional Drug Delivery Systems
Conventional drug delivery systems, as the name suggests, refer to the established methods and formulations that have been widely used in pharmaceuticals for many years. These systems have undergone extensive research and have a proven track record of safety and efficacy. They include various dosage forms such as tablets, capsules, injections, and creams. Conventional systems primarily focus on delivering drugs to the target site using passive diffusion or basic release mechanisms. While these systems have been successful in many cases, they often have limitations such as low bioavailability, poor solubility, and short half-life, which can decrease their effectiveness and require frequent dosing [3,8,11,112,113]. However, advancements in formulation techniques, such as the use of excipients and optimization of drug release profiles, have led to significant improvements in conventional drug delivery systems. There are several advantages and disadvantages of traditional DDSs as shown in Table 2.
Table 2.
| Traditional Drug Delivery Methods | Advantages | Disadvantages |
|---|---|---|
| Oral delivery | Convenience in administration Non-invasive Accurate and measured dose Unit dosage form Higher compliance Cheap for the patient |
Unconscious patients cannot take a dose Low permeability Degradation by gastro-intestinal enzymes First pass metabolism Irregular absorption |
| Buccal or sublingual delivery | Bypass first pass metabolism Rapid absorption Low enzymatic activity |
Discomfort during dissolution Probability of swallowing—loss of effect Small doses |
| Rectal delivery | Bypass first pass metabolism Useful for kids and children |
Absorption depends on disease state Degradation by bacterial flora Uncomfortable |
| Intravenous delivery | Drug 100% bioavailable Rapid response Can administer drugs degradable in stomach By-passes first pass metabolism |
Invasive Trained personnel Possible toxicity due to incorrect dosing Sterility |
| Subcutaneous delivery | Patient self-administration Slow complete absorption Bypass first pass metabolism when placed at lower part of rectum |
Invasive Irritation Inflammation Maximum dose volume—2 mL |
| Intramuscular delivery | Drug is absorbed slowly, so prolonged effect Larger volume than subcutaneous Bypass first pass metabolism |
Invasive—patient discomfort Irritation Inflammation May require some training |
2.2. Novel Drug Delivery Systems
New drug delivery systems have emerged as innovative solutions to overcome the limitations of classical drug delivery approaches and enhance the effectiveness as well as safety of therapeutic interventions [2,8]. These systems involve the utilization of specialized carriers or vehicles that can deliver the drug to the desired target site in a controlled and targeted manner [12,114,115]. There are several examples of novel drug delivery systems that have gained significant attention in recent years such as the rate-preprogrammed new drug delivery system [7,8,10]; activation-modulated drug delivery system [8,113,116]; feedback-regulated drug delivery system [3,112,113]; and site-targeting drug delivery system [3,8,112].
2.2.1. Rate-Preprogrammed New Drug Delivery System
This type of DDS is designed to release drugs at a predetermined rate over a specific period. By incorporating various mechanisms such as diffusion [117,118], erosion, or osmosis [74,118], these systems ensure a sustained and controlled release of the drug [119,120], maintaining therapeutic levels in the body for an extended duration [6,11,47,67,68,69]. Rate-preprogrammed systems offer advantages such as reduced dosing frequency, improved patient compliance, and enhanced therapeutic outcomes [84,85].
2.2.2. Activation-Modulated Drug Delivery System
Activation-modulated systems utilize specific triggers or stimuli to initiate drug release at the target site [32,79,80]. The triggers can be external, such as light [121,122,123], heat [124,125], or magnetic fields [126,127,128], or internal [63], including changes in pH [76,77,78,129,130], temperature [131,132], enzyme levels [24,76,132], or redox conditions [11,16,29]. By incorporating responsive materials or incorporating stimuli-responsive components, these systems enable a precise control over drug release, ensuring that the drug is delivered when and where it is needed most [56,70].
2.2.3. Feedback-Regulated Drug Delivery System
This system employs a feedback mechanism to adjust the drug release rate in response to a physiological signal or drug concentrations in the body [91,133,134]. By integrating sensors [103,135] or biomarkers [136,137], these systems can continuously monitor drug levels or the therapeutic response [11,47,84,85] and modulate the drug release accordingly [65,138,139]. The dynamic control mechanism optimizes drug delivery [140,141], minimizes side effects [142,143], and maximizes therapeutic efficacy [144,145,146].
2.2.4. Site-Targeting Drug Delivery System
The site-targeting drug delivery system aims to deliver drugs directly to the desired site or tissue [12,14,115], minimizing off-target effects [3,104,105] and improving treatment outcomes [8,11]. They can utilize various targeting strategies, including ligand–receptor interactions [13], antibody-mediated targeting [81,82], or active targeting using nanocarriers [147,148]. By enhancing drug accumulation at the target site, these systems enhance therapeutic efficacy while reducing systemic toxicity [3,8,149].
These examples represent the exciting advancements in the field of drug delivery systems, where researchers and scientists are actively exploring new approaches to address the challenges associated with conventional drug delivery. By tailoring drug release kinetics, incorporating responsive elements, utilizing feedback mechanisms, and targeting specific sites, these new drug delivery systems offer improved control, precision, and efficiency in drug administration. This aims to optimize drug efficacy, minimize side effects, and improve patient outcomes. Continued research and development in this field holds great promise for revolutionizing the way drugs are delivered, enabling personalized medicine approaches, and ultimately enhancing the overall quality of healthcare.
2.3. Carriers for Drug Delivery Systems
Carriers in drug delivery systems are designed to improve the pharmacokinetics and pharmacodynamics of drugs by addressing their limitations and optimizing their delivery. Carriers are designed to transport drugs to specific sites within the body, enhance drug stability [150,151], control drug release [152,153], and improve therapeutic outcomes [84,85]. These carriers can also enhance drug solubility [71,117,118], protect drugs from degradation [154,155], enable targeted delivery [3,8,112], provide sustained release [64,156], and improve drug stability [150,151] and bioavailability [8,11]. Carriers for drug delivery systems can be classified based on various parameters, such as their composition, structure, size, and mechanism of drug release. Some common classifications include liposomes [68,104,143], polymer micelles [63,144,145], microspheres [157,158,159], inorganic nanoparticles [148,160,161], dendrimers [99,142,162], hydrogels [11,12], and others [163,164,165,166,167,168].
Carriers for drug delivery systems possess several important properties such as biocompatibility, stability, drug-loading capacity, targeting ability, and controlled release. Therefore, the carriers for drug delivery systems play important roles in enhancing drug efficacy, improving patient compliance, and reducing side effects.
3. Polymer-Based Hydrogels
Polymer-based hydrogels are a type of soft material composed of three-dimensional polymer networks that have the ability to absorb and retain large amounts of water or biological fluids while maintaining their structural integrity [169,170,171]. These hydrophilic polymers are capable of swelling in the presence of water, resulting in a gel-like structure [172,173,174,175]. Crosslinking within the polymer network gives hydrogels their three-dimensional structure and prevents them from dissolving in water [16,23,174]. The polymers used to construct hydrogels can be either natural [176,177] or synthetic [177,178]. Natural polymers commonly used include alginate [179,180], chitosan [181,182], collagen [64], hyaluronic acid [17,23], and gelatin [183,184]. Synthetic polymers such as polyethylene glycol (PEG) [185,186], polyacrylamide (PAAm) [179,187], and poly(N-isopropylacrylamide) (PNIPAAm) [17,23] are also widely employed in hydrogel synthesis. The choice of polymer depends on the desired properties and intended applications of the hydrogel.
Polymer-based hydrogels possess several unique characteristics that make them attractive for various applications. Their high water content and soft consistency resemble living tissues [188], allowing for better integration [82] and minimizing immune responses [88,108,136]. Hydrogels are highly biocompatible, meaning they are compatible with biological systems and do not typically cause significant adverse reactions [135]. Their porosity enables the efficient transport of nutrients, oxygen, and bioactive molecules to cells residing within the hydrogel matrix [51,72,73,189]. These hydrogels can undergo controlled swelling and exhibit tunable mechanical properties, allowing them to mimic the physical and mechanical properties of natural tissues [190,191]. Additionally, hydrogels can be engineered to respond to external stimuli such as changes in temperature [192,193], pH [193,194], or light, making them valuable for applications such as targeted drug delivery or biosensing [13,15,69,103].
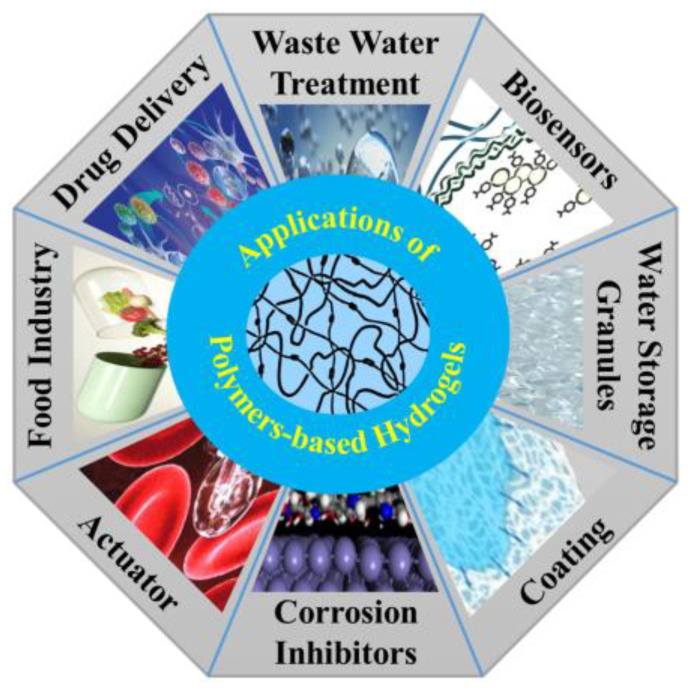
Polymer-based hydrogels have a wide range of applications in various fields, including drug delivery systems [195,196], the food industry [174], wastewater treatment [74], biosensors [103], water storage granules [192,197], coating [108,140], corrosion inhibitors [11,17,23], and actuators [23], as shown in Figure 1. They provide a versatile platform for the controlled release of drugs [111,119], scaffolds for tissue regeneration [198,199], wound dressings [46], and biocompatible materials for medical devices [86]. The design and formulation of polymer-based hydrogels continues to be an active area of research, aiming to develop advanced materials with enhanced properties and functionalities to meet the demands of biomedical applications [9,17,42,43,56,70,87,88,108].
Figure 1.
Applications of polymer-based hydrogels for the various engineering fields of the food industry, drug delivery, wastewater treatment, biosensors, water storage granules, coating, corrosion inhibitors, and actuators.
3.1. Classifications of Polymer-Based Hydrogels with Their Characteristic Aspects Related to DDSs and Biomedical Applications
There are various classifications of polymer-based hydrogels including based on origin, composition, ionic charge, pore size, physical appearance, configuration, crosslinking, external stimuli response, and others.
3.1.1. Classification of Polymer-Based Hydrogels Based on Origin
Polymer-based hydrogels can be classified based on their origin, which can be natural, synthetic, or a combination of both.
Natural polymer-based hydrogels are hydrogels composed of polymers derived from natural sources, such as plants, animals, or microorganisms. These polymers are biocompatible, biodegradable, and often exhibit inherent bioactivity, making them suitable for a wide range of biomedical applications [154]. Natural polymers include collagen, alginate, chitosan, hyaluronic acid, and gelatin. Natural polymer-based hydrogels offer advantages such as their similarity to the natural extracellular matrix, which supports cell growth and tissue regeneration. They can also provide a favorable microenvironment for encapsulated cells or therapeutic agents [176,177]. Additionally, natural polymers often possess inherent bioactivity, allowing for bioactive molecule incorporation or modification to enhance specific functionalities. The properties and structures of natural polymer-based hydrogels can be modified through various techniques such as crosslinking, blending with other polymers, or incorporating bioactive molecules. This versatility enables the customization of hydrogels to suit specific applications and desired properties [177,178]. Natural polymer-based hydrogels have gained significant attention in the field of regenerative medicine, drug delivery, and biomedical engineering due to their biocompatibility, biodegradability, and inherent bioactivity. Ongoing research and development efforts focus on refining their properties, improving their functionality, and exploring new applications in the fields of tissue engineering, wound healing, and controlled drug release systems [176,177,178].
Synthetic polymer-based hydrogels are hydrogels composed of polymers that are chemically synthesized in the laboratory. These polymers are typically derived from monomers through polymerization reactions, allowing for precise control over their chemical structures, properties, and functionality. Synthetic polymer-based hydrogels offer several advantages, including tunable properties, reproducibility, and the ability to incorporate various functionalities for specific applications [2,18,21,200]. Some common synthetic polymers used in the production of hydrogels are poly(acrylic acid) (PAA) [185,186], poly(N-isopropylacrylamide) (PNIPAAm) [17,23], poly(ethylene glycol) (PEG) [201,202], poly(vinyl alcohol) (PVA) [203,204], poly(HEMA) (hydroxyethyl methacrylate) [81], and others [205,206,207]. Synthetic polymer-based hydrogels offer advantages such as precise control over their chemical and physical properties, mechanical strength, and stability [201,202,203,204,205,206,207]. They can be engineered to exhibit specific characteristics such as controlled drug release [11,17,204], stimuli responsiveness [203], and biodegradability [23,186]. Additionally, synthetic polymers can be modified through various chemical reactions, allowing for the incorporation of bioactive molecules, peptides, or targeting ligands to enhance their functionality and specificity [201,202,203,204,205,206,207]. The properties and structures of synthetic polymer-based hydrogels can be tailored through parameters such as the choice of monomers, polymerization techniques, crosslinking methods, and the introduction of functional groups [204,205,206,207]. This versatility enables the design of hydrogels with specific characteristics suited for different applications. Synthetic polymer-based hydrogels find applications in various fields, including drug delivery systems, tissue engineering, biosensors, and wound healing [11,17,23,201,202,203,204,205,206,207]. Ongoing research focuses on developing novel synthetic polymers, optimizing hydrogel properties, and exploring advanced applications in regenerative medicine, controlled release systems, and biomedical engineering.
Hybrid polymer-based hydrogels, also known as semi-synthetic polymer-based hydrogels, are a type of hydrogel material that combines both natural and synthetic polymers to form a network structure [177,184,208,209]. These hydrogels are created by incorporating natural polymers or biomolecules into a synthetic polymer matrix or by chemically modifying natural polymers with synthetic components [208,209]. The concept of hybrid polymer-based hydrogels stems from the desire to capitalize on the advantages offered by both natural and synthetic polymers. Natural polymers, such as proteins and polysaccharides, provide biocompatibility, bioactivity, and inherent biological functionalities. On the other hand, synthetic polymers offer tunable mechanical properties, control over chemical functionality, and ease of synthesis [11,177]. By combining these two types of polymers, hybrid hydrogels can harness the unique characteristics of each component to achieve the desired properties and functions for specific applications [17,184]. There are various approaches to developing hybrid polymer-based hydrogels known as physical blending and covalent incorporation. For physical blending, natural and synthetic polymers can be physically mixed together to form a hybrid hydrogel [177,208]. The polymers may interact through physical entanglement, hydrogen bonding, or electrostatic interactions. While this method is straightforward, the properties of the resulting hybrid hydrogel are predominantly determined by the individual polymers, and there may be limited chemical integration between the components [23,177,209]. For covalent incorporation, natural polymers can be chemically modified to introduce functional groups that can react with synthetic polymers during the crosslinking process. This covalent incorporation ensures a stronger integration between the natural and synthetic components, leading to a more homogeneous and structurally stable hybrid hydrogel [177,184,209]. Examples of hybrid hydrogels include silk fibroin/PVA hydrogels [210] and chitosan/PEG hydrogels [210]. Hybrid polymer-based hydrogels offer several advantages over pure natural or synthetic polymer hydrogels. They combine the desirable properties of both types of polymers, such as biocompatibility, bioactivity, mechanical strength, and control over properties, to create materials with enhanced performance and functionality [11,17,208,210]. These hydrogels can be tailored to exhibit specific characteristics, such as improved mechanical properties, increased stability, controlled degradation rates, and enhanced drug release profiles [209,210]. The specific properties and structures of hybrid polymer-based hydrogels can be customized by adjusting the composition, ratio, and crosslinking density of the natural and synthetic polymers. This versatility allows for the fine-tuning of properties to suit the requirements of various applications, including tissue engineering, drug delivery, regenerative medicine, and biomedical devices [11,17,23,208,209,210].
3.1.2. Classification of Polymer-Based Hydrogels Based on Composition
Polymer-based hydrogels can also be classified based on their composition, which includes homopolymer [11,17,23,211,212], copolymer [24,30,52,63,67,71,79,98,123], multipolymer [63,213,214], and interpenetrating network (IPN) hydrogels [40,209,215].
Homopolymer-based hydrogels are a type of hydrogel that is composed of a single type of polymer. In other words, the hydrogel network is formed by crosslinking repeating units of the same polymer [11,211]. These hydrogels are created by polymerizing a monomer that consists of identical repeating units, leading to a three-dimensional network structure [17,212]. Homopolymer-based hydrogels have the ability of certain polymers to absorb and retain large amounts of water while maintaining their structural integrity. When the polymer chains are crosslinked, either through chemical or physical interactions, a hydrogel is formed [23,211,212]. The crosslinking allows the polymer chains to hold their positions and prevents them from dissolving or leaching out of the gel structure when exposed to aqueous environments. Homopolymer-based hydrogels can be classified into two main categories of chemically crosslinked homopolymer-based hydrogels and physically crosslinked homopolymer based-hydrogels. In chemically crosslinked homopolymer hydrogels, the crosslinking is achieved through covalent bonds formed between the polymer chains [11,17,212]. This can be accomplished by introducing crosslinking agents during the polymerization process or by post-polymerization crosslinking reactions. Examples of chemically crosslinked homopolymer hydrogels include polyacrylamide (PAAm) hydrogels [179,187], polyethylene glycol (PEG) hydrogels [185,186], and poly(N-isopropylacrylamide) (PNIPAAm) hydrogels [17,23]. For physically crosslinked homopolymer hydrogels, the crosslinking is based on physical interactions, such as entanglements, hydrogen bonding, or hydrophobic interactions between the polymer chains. These interactions are reversible, allowing the hydrogel to swell or shrink in response to external stimuli. Physically crosslinked homopolymer hydrogels are advantageous in terms of their ease of preparation and potential for a stimuli-responsive behavior. Examples of physically crosslinked homopolymer hydrogels include agarose hydrogels, gelatin hydrogels [183,184], and poly(N-vinylcaprolactam) hydrogels [11,17,23]. The properties of homopolymer-based hydrogels can be tailored by adjusting the polymer composition, molecular weight, crosslinking density, and environmental conditions. These hydrogels exhibit characteristics such as a high water absorption capacity, soft and flexible consistency, biocompatibility, and the ability to mimic certain aspects of natural tissues [17,23]. They find applications in various fields, including drug delivery, tissue engineering, wound healing, biosensors, and controlled release systems. While homopolymer-based hydrogels have certain advantages, such as simplicity in their composition and preparation, they may also have limitations [23,211,212]. These can include relatively limited control over the hydrogel properties, lack of specific functionalities, and potential for limited mechanical strength. To address these limitations, researchers often explore the use of copolymers or hybrid systems that incorporate multiple types of polymers or functional groups.
Copolymer-based hydrogels are indeed composed of two or more different monomers that undergo polymerization to form a three-dimensional network [98,123]. These hydrogels offer unique properties that can be tailored based on the combination of monomers used in their synthesis [24,30]. One example of a copolymer-based hydrogel is poly(ethylene glycol)-diacrylate (PEGDA). PEGDA hydrogels are formed by copolymerizing PEGDA monomers with a crosslinking agent such as N,N’-methylenebisacrylamide (BIS). PEGDA hydrogels are biocompatible, exhibit low toxicity, and can be crosslinked under mild conditions. These characteristics make them suitable for drug delivery and tissue engineering applications. Another example is poly(acrylic acid)-co-poly(ethylene glycol) (PAA-co-PEG), which is a copolymer hydrogel composed of two monomers, acrylic acid and ethylene glycol. PAA-co-PEG hydrogels demonstrate pH-sensitive swelling behavior due to the presence of acrylic acid. The acrylic acid units can ionize in basic conditions, leading to the swelling of the hydrogel [11,17,23]. This property makes PAA-co-PEG hydrogels useful for drug delivery applications where a pH-responsive release profile is desired. Copolymer-based hydrogels can be designed to have specific mechanical, swelling, and degradation properties by carefully selecting and adjusting the monomers and their ratios. By controlling these parameters, researchers can tailor the hydrogel’s characteristics to meet the requirements of various applications. The ability to modify copolymer hydrogels makes them versatile materials for fields such as tissue engineering and drug delivery, where precise control over properties is essential. Copolymer-based hydrogels offer the advantage of combining different monomers to achieve unique properties and functionalities [24,30,52,63,67,71,79,98,123]. Examples such as PEGDA and PAA-co-PEG demonstrate their utility in drug delivery systems, tissue engineering, and other applications. The specific combination of monomers determines the properties of hydrogels, enabling researchers to design copolymer hydrogels with the desired characteristics for specific applications.
Multipolymer-based hydrogels are hydrogels composed of three or more different polymer chains. These hydrogels are designed to leverage the beneficial properties of each individual polymer, resulting in a unique combination of properties that can be tailored for specific applications [63,113,114]. There are two common methods for preparing multipolymer hydrogels. The first method involves blending different types of pre-synthesized polymers. This blending process allows for the combination of different polymer chains to achieve the desired properties [63,113]. For example, a blend of chitosan, a natural polymer derived from chitin with excellent biocompatibility and biodegradability, and poly(vinyl alcohol) (PVA), a synthetic polymer with high water solubility and film-forming properties, can create a multipolymer hydrogel with improved mechanical strength, swelling properties, and biocompatibility. The second method for preparing multipolymer hydrogels is through the copolymerization of two or more monomers. For instance, a copolymer of poly(ethylene glycol) (PEG) and poly(lactic acid) (PLA) can be synthesized. PEG, being a hydrophilic polymer, enhances the water uptake of the hydrogel, while PLA, a biodegradable polymer, controls the degradation rate of the hydrogel. By incorporating multiple polymer chains, multipolymer hydrogels offer a broader range of properties compared to single polymer-based hydrogels. The combination of different polymers allows for the fine-tuning of mechanical strength, degradation rates, biocompatibility, and other characteristics [63,113,114]. This versatility makes multipolymer hydrogels suitable for various applications, including tissue engineering, drug delivery, and biomedical implants.
Interpenetrating network (IPN) hydrogels are a type of hydrogel composed of two or more polymer networks that are interlocked at a molecular level. The polymer networks can consist of their homopolymer or copolymer [40,209,215]. The formation of an IPN hydrogel involves the polymerization or crosslinking of the different networks either sequentially or simultaneously. One of the key advantages of IPN hydrogels is their unique combination of properties that arise from the interpenetration of the polymer networks [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,215]. By selecting appropriate polymer combinations, the properties of the resulting hydrogel can be tailored to meet specific requirements. For example, the incorporation of different polymers can lead to an improved biocompatibility, mechanical strength, stability, and permeability. The sequential polymerization method involves the formation of one polymer network first, followed by the introduction of the second polymer system, which infiltrates the spaces between the chains of the first network [40,209,215]. In simultaneous polymerization, different monomers or pre-polymers are polymerized together to form the interpenetrating networks. The crosslinking of the polymer networks further strengthens the structure of the IPN hydrogel. IPN hydrogels have a wide range of applications in the biomedical field. In drug delivery systems, IPN hydrogels offer the controlled and sustained release of drugs due to their unique structure and properties. They are also extensively used in tissue engineering, where their enhanced mechanical properties and biocompatibility support cell growth and tissue regeneration [40,209]. IPN hydrogels have shown promise in wound healing applications by providing a moist and favorable environment for tissue repair. Furthermore, their versatility makes them suitable for the development of biosensors that can detect specific analytes or biomarkers. Due to their versatility, IPN hydrogels have a wide range of applications in the biomedical field, including drug delivery, tissue engineering, wound healing, and biosensors [11,17,40,215].
3.1.3. Classification of Polymer-Based Hydrogels Based on Ionic Charge
Polymer-based hydrogels can also be classified based on their ionic charge. These hydrogels can be classified into three types: neutral [129], ionic [216,217], and ampholytic hydrogels [79].
Neutral polymer-based hydrogels are hydrogels that lack an ionic charge. They are composed of polymers that contain hydrophilic groups, such as hydroxyl or amide groups, which enable them to absorb and retain water [11,129]. These neutral polymer-based hydrogels are typically synthesized through the crosslinking polymerization of monomers such as acrylates, methacrylates, or vinyl monomers. These hydrogels offer several advantages in biomedical applications [13,17,129]. Firstly, they are biocompatible and non-toxic, making them suitable for use in contact with biological systems [23,129]. This biocompatibility reduces the risk of adverse reactions or toxicity when the hydrogels are implanted or administered in vivo. Additionally, neutral polymer-based hydrogels can be designed to have specific mechanical properties, such as elasticity or stiffness, which can be tailored to match the requirements of the target tissue or application [11,17,23]. The versatility of neutral hydrogels allows for a wide range of applications in the biomedical field. In drug delivery, they can provide the sustained release of drugs, protecting them from degradation and ensuring their controlled release over time. In tissue engineering, neutral hydrogels can provide a scaffold for cell growth and tissue regeneration, mimicking the natural extracellular matrix [11,17,23]. They can also be used in wound healing to create a moist and protective environment that promotes healing and tissue regeneration.
Ionic polymer-based hydrogels are a type of hydrogel that contain charged functional groups within their polymer structure, such as carboxyl, amine, or sulfonate groups [124,216]. They are responsible for imparting an ionic charge to the hydrogel. When the hydrogel is immersed in water or an aqueous environment these charged groups can dissociate, releasing charged ions into the surrounding solution [174,194,217]. The presence of these charged ions enables interactions with oppositely charged species in the environment. Ionic polymer-based hydrogels can be classified into two main types: cationic polymer-based hydrogels and anionic polymer-based hydrogels, based on the type of charged functional groups they possess [194,216,217]. The cationic polymer-based hydrogels contain positively charged functional groups, typically amine groups. These hydrogels have a propensity to interact with negatively charged molecules present in the environment, such as proteins, nucleic acids, or polysaccharides [17,23]. The electrostatic interactions between the positively charged hydrogel and the negatively charged molecules can be utilized in various applications [11,17]. For example, cationic polymer-based hydrogels have been explored for drug delivery systems, where the charged hydrogel can bind and deliver negatively charged drug molecules or interact with the negatively charged components of the biological environment. They have also found applications in wound healing and tissue engineering, where the interactions with negatively charged biomolecules play a role in promoting cellular adhesion and tissue engineering. On the other hand, anionic polymer-based hydrogels contain negatively charged functional groups such as carboxyl or sulfonate groups [206,216,217]. These hydrogels can interact with positively charged molecules, such as metal ions or proteins containing basic amino acid residues. The electrostatic interactions between the anionic hydrogel and the positively charged species can be harnessed for various applications [23,124,206]. The anionic polymer-based hydrogels have been investigated for drug delivery systems, where they can bind and release positively charged drugs or interact with positively charged proteins to modulate drug release [11,23]. They have also been explored in tissue engineering applications, where the interactions with positively charged molecules can influence cell behavior and tissue regeneration processes [174,217]. The presence of ionic charges in these hydrogels introduces unique properties and functionalities. The electrostatic interactions between the charged hydrogel and the surrounding environment can affect the swelling behavior, mechanical properties, and the release kinetics of encapsulated drugs or bioactive molecules. The ability to selectively interact with oppositely charged species provides opportunities for precise control over drug delivery, molecular recognition, and cellular interactions.
Ampholytic polymer-based hydrogels, also known as zwitterionic hydrogels, are a type of polymer-based hydrogel that contains both positively and negatively charged groups within the polymer chains [11,17,23,79]. These charged groups can be in the form of acidic and basic functional groups, such as carboxyl and amino groups. The presence of both positive and negative charges imparts amphoteric properties to the hydrogel, meaning it can exhibit acidic or basic behavior depending on the pH of the surrounding environment. The pH responsiveness of ampholytic polymer-based hydrogels arises from the ionization of the charged groups in response to changes in pH [218,219]. When the pH of the surrounding medium changes, the charged groups within the hydrogel can either gain or lose protons, leading to alterations in the overall charged density of the polymer-based hydrogel network [191,193,194]. This change in charged density affects the electrostatic interactions within the hydrogel and influences its swelling behavior and mechanical properties. As a result, ampholytic polymer-based hydrogels can undergo significant volume changes or alterations in their crosslinking density in response to pH variations [77,119,129]. The pH responsiveness of ampholytic polymer-based hydrogels makes them attractive for various applications. In drug delivery, these hydrogels can be designed to respond to specific pH conditions, such as those found in different regions of the body, to trigger drug release. For example, an ampholytic hydrogel with a lower critical solution temperature (LCST) above physiological pH can undergo a volume phase transition and release a loaded drug when exposed to acidic conditions, such as those in tumor microenvironments [76,77,218,219]. In tissue engineering, the pH responsiveness of ampholytic hydrogels can be exploited to modulate cell adhesion, proliferation, and differentiation by creating pH-tunable microenvironments that mimic native tissue conditions. Additionally, the ability of ampholytic hydrogels to interact with biomolecules due to their charged nature makes them suitable for biosensor applications, where they can selectively bind or detect specific analytes based on pH changes [78,119,130,131]. Ampholytic polymer-based hydrogels offer advantages such as enhanced stability, improved biocompatibility, and reduced nonspecific interactions compared to ionic hydrogels. The presence of both positive and negative charges in the hydrogel network can provide a balanced response to pH variations, allowing for precise control over their properties and behavior.
3.1.4. Classification of Polymer-Based Hydrogels Based on Pore Size
Polymer-based hydrogels can exhibit different structural features, including pore size and interstitial domains. Pore size refers to the void spaces or cavities within the hydrogel structure that are interconnected and allow for the diffusion of solvents, gases, or other molecules [11,23]. Pores are typically defined as openings or channels that can be accessed by molecules, and their size is often characterized by the diameter of the opening. On the other hand, interstitial domains refer to the spaces between the polymer chains or networks within the hydrogel structure. These domains are not necessarily interconnected and may not provide direct pathways for molecule diffusion [17,220]. Instead, they contribute to the overall structure and integrity of the hydrogel. It is important to note that not all hydrogels exhibit well-defined or interconnected pores. Some hydrogels may have a more homogeneous structure with minimal or no discernible pores. In such cases, the transport of molecules occurs primarily through the interstitial domains, where the polymer chains create a network with sufficient space for solvent or molecule diffusion. The interstitial domains provide a pathway for molecular transport within the hydrogel, although they may not be explicitly characterized as “pores” due to their lack of well-defined openings or channels [11,17,23].
Polymer-based hydrogels can be engineered to have a specific pore size, which can influence their properties and applications. The presence of pores in polymer-based hydrogels is not a universal feature and depends on the specific manufacturing process used to produce the hydrogel. This means not all polymer-based hydrogels are necessarily porous, although all hydrogels are swellable [220,221]. Pores can be intentionally introduced during the hydrogel fabrication process through various methods such as solvent evaporation, freeze-drying, or templating techniques. These methods create void spaces or cavities within the hydrogel structure, resulting in a porous matrix [28,29,30,31,90,189]. Porous hydrogels have distinct advantages compared to non-porous hydrogels. The presence of pores provides increased surface area, which can enhance the diffusion of molecules, promote cell infiltration, and support tissue integration in biomedical applications [220,221]. Porous hydrogels can also facilitate the loading and release of drugs or bioactive agents, making them useful for drug delivery systems [89,202]. However, it is important to note that not all hydrogels require porosity to fulfill their intended functions. Many hydrogels are designed for applications where swelling and gel formation are the primary requirements, such as in contact lenses, wound dressings, or as matrices for tissue engineering scaffolds [28,29,30,31,89,90]. In these cases, the absence of pores does not hinder the performance of polymer-based hydrogels. The control of pore size in hydrogels is crucial for regulating the transport of molecules, cells, and fluids within the gel matrix. Here are three types of polymer-based hydrogels based on their pore size:
Macroporous polymer-based hydrogels are hydrogels that possess a three-dimensional network with relatively large, interconnected pores [90]. The macroporous structure allows for the easy flow of fluids, transport of cells, and tissue ingrowth. These hydrogels have pore sizes ranging from tens to hundreds of micrometers, providing ample space for the infiltration of cells, nutrients, and oxygen [11,23]. There are several methods to create macroporous structures in polymer-based hydrogels such as salt leaching, gas foaming, or solvent casting/particulate leaching. For the salt leaching technique, a water-soluble salt (e.g., sodium chloride) is mixed with the hydrogel precursor solution. After gelation, the salt particles create void spaces within the hydrogel matrix [11,17,90]. Subsequent leaching with water or a suitable solvent dissolves the salt particles, leaving behind a macroporous structure. Gas foaming involves the incorporation of a gas-generating agent (e.g., sodium bicarbonate) into the hydrogel precursor solution. When the hydrogel is crosslinked, the gas-generating agent releases gas bubbles, leading to the formation of macropores [11,23,90]. The bubbles can be stabilized by controlling the crosslinking process, resulting in a stable macroporous structure. For the solvent casting/particulate leaching method, a mixture of the hydrogel precursor and porogen particles (e.g., sugar particles or gelatin microspheres) is cast into a mold. After gelation, the porogen particles are selectively removed by leaching with a suitable solvent, leaving behind interconnected macropores. Macroporous polymer-based hydrogels have a wide range of applications, particularly in tissue engineering [11,17,90]. The large pore size facilitates cell infiltration, nutrient and oxygen transport, and the removal of waste products. The macroporous structure mimics the extracellular matrix, providing a favorable environment for cell adhesion, proliferation, and tissue regeneration [23,90]. These hydrogels can serve as scaffolds for various tissues, including bone, cartilage, skin, and vascular tissues. Additionally, macroporous hydrogels can be utilized in drug delivery systems, where the large pores enable the encapsulation and sustained release of therapeutic agents.
Mesoporous polymer-based hydrogels are a type of hydrogel that incorporate mesopores within their structure. Mesopores are defined as pores with diameters in the range of 2 to 50 nm [89,189]. These polymer-based hydrogels exhibit a high surface area and pore volume, providing unique properties and applications [17,23,89]. The synthesis of mesoporous polymer-based hydrogels typically involves the use of templating agents or self-assembly techniques with two commonly employed methods of template-assisted synthesis and self-assembly [11,189]. In templating agents or the self-assembly method, a sacrificial template, such as micelles or colloidal particles, is dispersed within the hydrogel precursor solution. After gelation, the template is selectively removed, leaving behind a network of interconnected mesopores [11,17,89]. The size and structure of the mesopores can be controlled by adjusting the size and characteristics of the template. On the other hand, self-assembly methods utilize the spontaneous organization of amphiphilic molecules or block copolymers to form mesostructures within the hydrogel matrix [23,189]. By controlling the self-assembly process, the formation of mesopores can be achieved. Hydrophilic–hydrophobic interactions and the arrangement of polymer chains dictate the mesopore structure [89,189]. The presence of mesopores in polymer-based hydrogels offers several advantages. The high surface area and pore volume allow for the efficient loading and release of molecules, making them promising for drug delivery systems. The mesoporous structure enables the controlled and sustained release of therapeutic agents [11,23]. Additionally, the mesopores can serve as reservoirs for bioactive molecules, growth factors, or cells, promoting tissue regeneration in tissue engineering applications. The properties and applications of mesoporous polymer-based hydrogels are diverse. They can be utilized for controlled drug release, biosensing, catalysis, and environmental remediation. The tailored mesoporous structure provides a platform for precise control over molecular diffusion, interactions, and reactions within the hydrogel matrix [11,17,23,189].
Microporous polymer-based hydrogels are a type of hydrogel that possess a network of interconnected micropores within their structure. Micropores are defined as pores with diameters typically less than 2 nm [23,202,221]. These hydrogels exhibit a high surface area and can absorb and retain a significant amount of fluid. The synthesis of microporous polymer-based hydrogels involves the introduction of porogens or porogenic agents during the polymerization process. These porogens are later removed, leaving behind a porous structure [11,17,23,221]. Various techniques can be employed to generate micropores, including solvent casting and particulate leaching and gas foaming. The solvent casting and particulate leaching method involves casting a mixture of polymer and porogenic particles, such as salt crystals or sugar particles, into a mold. After solidification, the porogens are dissolved or leached out, creating micropores in the hydrogel [11,23,202]. In the gas-foaming approach, a gas, such as nitrogen or carbon dioxide, is dissolved in the hydrogel precursor solution under high pressure. Upon rapid depressurization, the gas forms bubbles within the hydrogel, resulting in a microporous structure upon gelation [202,221]. Microporous polymer-based hydrogels offer several advantages due to their unique pore characteristics. The presence of micropores enhances the mechanical properties of the hydrogel, including its compressibility and flexibility [11,17,23]. The high surface area and porosity enable the efficient absorption and release of fluids, making them suitable for applications such as wound dressings, tissue engineering scaffolds, and biosensors [23,221]. These hydrogels can also be functionalized with specific chemical groups or bioactive molecules within the micropores, allowing for targeted drug delivery or the controlled release of therapeutic agents. The small pore size of microporous hydrogels can regulate the diffusion of molecules, providing tunable release profiles and prolonged drug delivery [11,202]. Furthermore, microporous polymer-based hydrogels can be designed to mimic the extracellular matrix (ECM) of biological tissues, facilitating cell adhesion, proliferation, and tissue regeneration. The micropores serve as pathways for cell migration, nutrient transport, and waste removal, promoting cell growth and tissue integration [11,17,23,202,221].
3.1.5. Classification of Polymer-Based Hydrogels Based on Physical Appearance
Actually, the classification of polymer-based hydrogels based on physical appearance is unrelated to the polymerization technique. It refers to the different forms that the polymer-based hydrogels can take depending on their shape and structure. Here are the common classifications of polymer-based hydrogels based on their physical appearance:
Matrix polymer-based hydrogels, also known as bulk hydrogels, are three-dimensional networks composed of a polymer matrix that swells in the presence of water or biological fluids. These hydrogels are formed through the polymerization of monomers or the crosslinking of pre-polymers to create a continuous polymeric structure [40,51,198]. The polymer matrix provides structural integrity to the hydrogel while allowing for the absorption and retention of water within its network [73,73]. Matrix polymer-based hydrogels have a homogeneous structure throughout and occupy a relatively large volume. They can be soft and gel-like or have a more solid-like consistency, depending on the crosslinking density and composition of the polymer network [54,95,100]. The polymer chains within the hydrogel matrix are typically hydrophilic and contain hydrophilic functional groups, such as hydroxyl or amide groups, that facilitate water absorption. The properties of matrix polymer-based hydrogels can be tailored by selecting specific polymers, crosslinking methods, and polymerization conditions [185,189,198]. These hydrogels can exhibit various characteristics, including a high water content, biocompatibility, biodegradability, and mechanical properties that can range from soft and elastic to stiff and rigid [40,185]. The swelling behavior of matrix polymer-based hydrogels can be controlled by adjusting the crosslinking density and polymer composition. Matrix polymer-based hydrogels find a wide range of applications in areas such as tissue engineering, drug delivery, wound healing, and biosensing [40,51,73]. They can be used as scaffolds to support cell growth and tissue regeneration, as matrices for the controlled release of drugs or bioactive molecules, and as biomimetic materials to mimic the extracellular matrix. The versatility of matrix polymer-based hydrogels makes them valuable for developing advanced biomaterials for biomedical applications.
Film polymer-based hydrogels, also known as thin film, are hydrogel materials that are fabricated in form of thin films or coatings [64,90,188]. Unlike bulk hydrogels, which have a three-dimensional network structure, film hydrogels are typically two-dimensional and have a flat, sheet-like morphology. These hydrogels are composed of polymers that can absorb and retain water, similar to other hydrogel types [90,163]. Film polymer-based hydrogels are often prepared by casting, deposition techniques, or by using electrospinning techniques, where a solution or dispersion of hydrogel precursors is spread onto a substrate and then subjected to a crosslinking process to form a solid film [88,89]. The crosslinking can be achieved through various methods, such as chemical crosslinking, physical crosslinking, or photo-polymerization, depending on the specific polymer system used [64,163,188]. The thickness of film hydrogels can vary depending on the application requirements and the desired properties. They can range from a few micrometers to several millimeters in thickness. The composition of the polymer matrix can also be tailored to achieve specific properties such as mechanical strength, swelling behavior, and biocompatibility [23,64,90]. Film polymer-based hydrogels offer several advantages in various applications. Their thin and flexible nature allows for easy handling and conformability to different surfaces, making them suitable for coating medical devices, implants, or wound dressings. They can provide a protective barrier, promote moisture retention, and deliver bioactive substances to the target site. Film hydrogels also find applications in biosensing, where they can be utilized as thin films on sensor surfaces to detect specific analytes or biomarkers [11,17,163]. The film polymer-based hydrogels offer versatility and customization possibilities, making them attractive for a wide range of applications that require thin, flexible, and water-absorbent materials.
Microsphere polymer-based hydrogels are a type of hydrogel material that combine the properties of both microspheres and hydrogels [161,222]. These hydrogels are composed of small, spherical particles called microspheres that are made of a crosslinked polymer network. The microspheres are typically in the micrometer size range, ranging from a few micrometers to hundreds of micrometers in diameter [96,148]. The microspheres in microsphere polymer-based hydrogels can be made from a variety of polymers, such as natural polymers (e.g., gelatin or alginate) or synthetic polymers (e.g., polyvinyl alcohol or poly(lactic-co-glycolic acid)) [11,23,160]. These polymers are crosslinked to form a three-dimensional network within each microsphere, creating a porous structure. The pores within the microspheres can absorb and retain water or other aqueous solutions, giving them hydrogel-like properties [96,159,222]. Microsphere polymer-based hydrogels offer several advantages in different applications. The microspheres provide a high surface-area-to-volume ratio, allowing for the efficient encapsulation and delivery of bioactive molecules, such as drugs or growth factors [23,161]. The porous structure of the microspheres allows for the controlled release of the encapsulated substances, providing sustained and localized delivery over time. These hydrogels are also useful in tissue engineering and regenerative medicine [11,96,160]. The microspheres can serve as scaffolds or carriers for cells, facilitating their proliferation and differentiation. The porous structure of the microspheres allows for cell infiltration and nutrient exchange, supporting tissue growth and regeneration [96,148,161]. Microsphere polymer-based hydrogels can be prepared using various techniques, including emulsion methods, solvent evaporation, or spray drying. The size, porosity, and mechanical properties of the microspheres can be tailored by adjusting the polymer composition, crosslinking method, and processing parameters [17,222]. Microsphere polymer-based hydrogels provide a versatile platform for drug delivery, tissue engineering, and other biomedical applications [11,23,161]. Their unique combination of microsphere and hydrogel properties allows for precise control over drug release kinetics and cellular behavior, making them valuable in the development of advanced therapeutic and regenerative strategies.
Nanoparticle polymer-based hydrogels are hydrogel materials that incorporate nanoparticles within their polymer network [166,167,168]. These hydrogels combine the properties of both hydrogels and nanoparticles, offering unique characteristics and functionalities. The nanoparticles in nanoparticle polymer-based hydrogels can be either organic or inorganic in nature [77,78,82,150]. Examples of organic nanoparticles include polymeric nanoparticles, liposomes, micelles, or dendrimers, while inorganic nanoparticles may include metallic, magnetic, or quantum dot nanoparticles [14,38]. These nanoparticles are typically dispersed or embedded within the hydrogel matrix during the fabrication process. The presence of nanoparticles in the hydrogel network can impart several advantages to the material [20,42,64]. First, nanoparticles can enhance the mechanical properties of hydrogels, improving their strength, elasticity, and stability [62,124,126]. This is particularly important in applications where robustness is required, such as tissue engineering or drug delivery [153,163,166,167,168]. Second, the incorporation of nanoparticles can provide additional functionalities to the hydrogel [11,23]. For instance, magnetic nanoparticles can enable magnetic targeting or imaging capabilities, while fluorescent nanoparticles can facilitate the imaging and tracking of the hydrogel in biological systems [150,162]. Similarly, nanoparticles with specific surface chemistry can enable controlled drug release, enhance biocompatibility, or promote cellular interactions. Furthermore, nanoparticles within the hydrogel network can influence the release kinetics of encapsulated drugs or therapeutic agents [14,77,82]. The size, shape, and surface properties of the nanoparticles can affect the diffusion and release behavior, allowing for controlled and sustained drug delivery. Nanoparticle polymer-based hydrogels can be fabricated using various techniques, such as in situ polymerization, co-precipitation, self-assembly, or the surface modification of pre-synthesized nanoparticles followed by their incorporation into the hydrogel matrix [23,78,126]. The choice of fabrication method depends on the desired nanoparticle properties, compatibility with the hydrogel matrix, and the targeted application. Applications of nanoparticle polymer-based hydrogels span various fields. They have been used in drug delivery systems for the targeted and controlled release of therapeutics, as scaffolds for tissue engineering and regenerative medicine, as biosensors for the detection and monitoring of biomarkers, and in imaging and diagnostic technologies [23,150]. Nanoparticle polymer-based hydrogels offer a versatile platform that combines the unique properties of both nanoparticles and hydrogels. Their tunable properties, enhanced functionalities, and diverse applications make them attractive for a wide range of biomedical and technological advancements.
Polymer-based hydrogel beads, also known as gel beads, are small spherical particles made of hydrogel materials [180,223]. These beads are typically composed of crosslinked polymer networks that can absorb and retain large amounts of water or biological fluids. These hydrogel beads are often prepared through a process called suspension polymerization or emulsion polymerization. In this method, the monomers and crosslinking agents are dispersed in a continuous phase, such as water or an organic solvent, along with a surfactant or stabilizer to prevent aggregation. Polymerization is then initiated to form a three-dimensional network of interconnected polymer chains, resulting in the hydrogel structure of the beads [11,23,119,180]. The size of the beads can be controlled by adjusting the polymerization conditions, such as the concentration of monomers, crosslinking density, or stirring speed. Polymer-based hydrogel beads have various applications across different fields. In drug delivery, they can be used as carriers for the controlled and targeted release of drugs or therapeutic agents [17,223]. The porous structure of the beads allows for the encapsulation of drugs within the hydrogel matrix, and the release kinetics can be modulated by adjusting the polymer composition and crosslinking density. Additionally, the beads can be functionalized with specific ligands or targeting moieties to enhance their binding affinity to specific cells or tissues [11,180]. In biotechnology and diagnostics, polymer-based hydrogel beads are used for applications such as enzyme immobilization, protein separation, cell encapsulation, and biosensing [11,17,119]. The large surface area and high porosity of the beads facilitate efficient enzyme loading or protein binding, enabling enhanced catalytic activity or the effective separation of biomolecules. They can also serve as a matrix for encapsulating cells in tissue engineering or regenerative medicine applications [23,180]. Polymer-based hydrogel beads can also find use in cosmetics, agriculture, and environmental engineering. For example, they can be employed in personal care products for the controlled release of active ingredients or as absorbent materials for moisture management [23]. In agriculture, hydrogel beads can improve water retention in soil and facilitate the controlled release of fertilizers [11]. In environmental applications, they can be utilized for water treatment, the adsorption of pollutants, or controlled release of chemicals for environmental remediation [11,23].
There are other physical appearances that hydrogels can take, depending on the manufacturing technique and intended application.
3.1.6. Classification of Polymer-Based Hydrogels Based on Crystallinity
Polymer-based hydrogels can be classified based on their crystallinity, which relates to the degree of structural order in the polymer network. Crystallinity influences the physical and mechanical properties of hydrogels, including their strength, stiffness, and swelling behavior. In terms of crystallinity, hydrogels can be broadly categorized into two types, with amorphous polymer-based hydrogels [224,225] and semi-crystalline polymer-based hydrogels [17,23,226].
Amorphous polymer-based hydrogels are hydrogels that lack long-range structural order or crystallinity in their polymer network [23,224,225]. The polymer chains in these hydrogels are randomly distributed, resulting in a more disordered and non-crystalline structure [224]. Amorphous polymer-based hydrogels are characterized by the absence of well-defined crystalline domains, which distinguishes them from crystalline hydrogels [225]. Without the presence of ordered polymer segments, amorphous hydrogels exhibit different physical and mechanical properties [23,224]. Amorphous polymer-based hydrogels find applications in various fields, including drug delivery systems, wound dressings, tissue engineering scaffolds, and biosensors [11,23]. Their flexibility and high water absorption capacity make them suitable for conformal contact with biological tissues, while their transparency and biocompatibility are advantageous for biomedical applications [11,23,225]. It is worth noting that the distinction between amorphous and crystalline hydrogels is not always absolute, as some hydrogels may exhibit a combination of amorphous and crystalline regions to varying degrees [224]. The degree of crystallinity in a hydrogel can be influenced by factors such as the choice of polymer, synthesis conditions, and post-processing treatments [23,225].
Semi-crystalline polymer-based hydrogels are hydrogels that exhibit a combination of amorphous and crystalline regions within their polymer network [11,23,226]. Unlike amorphous polymer-based hydrogels that lack long-range structural order, semi-crystalline polymer-based hydrogels contain regions where the polymer chains arrange themselves in an ordered, crystalline manner, interspersed with amorphous regions [11,17]. The presence of crystalline regions in semi-crystalline hydrogels introduces additional structural organization and can significantly influence the material properties [226]. The development of semi-crystalline polymer-based hydrogels involves careful control of the synthesis and processing conditions to promote the formation of crystalline regions [23]. Factors such as polymer selection, crystallization temperature, and annealing can influence the degree of crystallinity within the hydrogel [23,226]. The unique combination of crystalline and amorphous regions in semi-crystalline hydrogels offers advantages in various applications. For instance, their enhanced mechanical properties make them suitable for load-bearing tissue engineering scaffolds [11,17], while their thermal stability is advantageous for applications requiring exposure to higher temperatures [17,23]. The balance between crystallinity and amorphousness can be tailored to achieve the desired properties for specific applications [11,23].
The degree of crystallinity in a polymer-based hydrogel can be controlled by adjusting the polymerization conditions, such as temperature, pH, and the concentration of the polymer and crosslinking agent [23,226].
3.1.7. Classification of Polymer-Based Hydrogels Based on Crosslinking
Polymer-based hydrogels can indeed be classified based on the type of crosslinking they employ. The crosslinking mechanism is crucial in determining the structure, properties, and performance of the hydrogel. The two main types of crosslinking in polymer-based hydrogels are physical crosslinking [58,227,228] and chemical crosslinking [23,58,173,228].
Chemical crosslinking involves the formation of covalent bonds between the polymer chains, resulting in a three-dimensional network structure [23,228]. Chemical crosslinking methods include radical polymerization, Michael addition, Schiff base reaction, and epoxy crosslinking, among others [58,173]. This process typically requires the use of crosslinking agents or the incorporation of functional groups in the polymer chains that can react and form covalent bonds [228]. Chemical crosslinking reactions can be initiated by various methods such as heat, light, or chemical initiators [11,23]. Once the crosslinks are formed, they are permanent and stable. Chemically crosslinked hydrogels often exhibit excellent mechanical strength, stability, and resistance to dissolution [58,173]. However, the crosslinking process may involve harsh conditions or toxic chemicals, which can limit their applications in certain sensitive environments or in biomedical applications [11,23,228].
Physical crosslinking relies on reversible, non-covalent interactions between polymer chains to form a network structure [227,228]. These interactions can include hydrogen bonding, hydrophobic interactions, electrostatic interactions, or the physical entanglement of polymer chains [11,23]. Physical crosslinking methods offer advantages such as mild processing conditions and the ability to tune the network structure and properties by altering the environmental conditions [17,227]. Common physical crosslinking methods include temperature-induced gelation, pH-induced gelation, ion-induced gelation, and self-assembly, among others [23,228]. Physically crosslinked hydrogels can exhibit stimuli-responsive behavior, such as swelling/deswelling in response to environmental changes, due to the reversible nature of the interactions [228]. However, physically crosslinked hydrogels generally have lower mechanical strength compared to chemically crosslinked hydrogels and can be sensitive to changes in environmental conditions [227,228].
The choice between chemical and physical crosslinking depends on the desired properties and applications of the hydrogel. Chemically crosslinked hydrogels are often preferred when high mechanical strength, stability, and resistance to degradation are required [11,23]. They are commonly used in load-bearing applications, tissue engineering scaffolds, and long-term drug delivery systems. On the other hand, physically crosslinked hydrogels are advantageous when stimuli-responsive behavior, injectability, or biodegradability are desired [23,58,227,228]. They find applications in drug delivery, tissue engineering, and regenerative medicine, where the ability to respond to specific triggers or undergo controlled degradation is beneficial.
3.1.8. Classification of Polymer-Based Hydrogels Based on External Stimuli Response
Polymer-based hydrogels can be classified based on their responsiveness to external stimuli, which is an important characteristic that enables their use in various applications. These stimuli-responsive polymer-based hydrogels, also known as smart hydrogels or intelligent hydrogels, exhibit changes in their structure, properties, or behavior in response to specific external stimuli [11,23]. This responsiveness is a result of the specific design and incorporation of responsive components or functional groups within the hydrogel network.
Temperature-responsive polymer-based hydrogels are a type of hydrogel that exhibit changes in their swelling behavior or sol–gel transition in response to changes in temperature [74,75,131,192,193]. These hydrogels are designed to undergo a volume phase transition at a specific temperature, known as the lower critical solution temperature (LCST) or an upper critical solution temperature (UCST) [23,192,193]. The transition can be reversible or irreversible, depending on the specific polymer and formulation used. Temperature-responsive polymer-based hydrogels typically consist of a polymer network that incorporates thermo-responsive components, such as N-isopropylacrylamide (NIPAAm), poly(N-isopropylacrylamide) (PNIPAAm), or polyethylene glycol (PEG). These polymers have LCSTs close to physiological temperatures, making them suitable for biomedical applications [23,74,75]. Below the LCST, temperature-responsive polymer-based hydrogels are in a swollen state, allowing for the absorption and retention of water. As the temperature increases beyond the LCST, the hydrogel undergoes a phase transition and collapses, resulting in a decrease in swelling and an increase in mechanical strength [17,131]. The LCST of temperature-responsive hydrogels can be adjusted by varying the polymer composition, molecular weight, and crosslinking density. This allows for the fine-tuning of the hydrogel properties to match specific application requirements. Temperature-responsive polymer-based hydrogels have a wide range of applications, particularly in drug delivery systems and tissue engineering [11,23,192,193]. They can be used as carriers for controlled drug release, where the drug is released at a higher rate above the LCST due to the collapse of the hydrogel. In tissue engineering, these hydrogels can serve as scaffolds for cell culture, where the ability to switch between a swollen and collapsed state can mimic dynamic cellular environments and facilitate cell attachment, proliferation, and differentiation [17,23,74,75].
pH-responsive polymer-based hydrogels are a type of hydrogel that exhibit changes in their swelling behavior or properties in response to variations in pH [76,77,78,129,130,131]. These hydrogels can contain pH-sensitive functional groups within their polymer networks, allowing them to respond to acidic or basic conditions. The pH-responsive behavior of these hydrogels arises from the ionization or deionization of the functional groups within the polymer network as the pH of the surrounding environment changes [119,120]. Common pH-sensitive functional groups used in the design of pH-responsive hydrogels include carboxylic acid (COOH), amino groups (NH2), and imidazole groups (imidazole). At certain pH values, these functional groups can either be ionized or deionized, leading to changes in the charge density and hydrophilicity of the hydrogel. This, in turn, affects the swelling or collapse of the hydrogel network [119,120]. For example, in an acidic environment (low pH), hydrogels containing ionizable carboxylic acid groups will be in a collapsed or shrunken state due to increased protonation of the acidic groups. As the pH increases towards neutrality or becomes basic, the carboxylic acid groups deprotonate, leading to an increase in hydrogel swelling [191,193,194]. The pH-responsive behavior of these hydrogels can be fine-tuned by modifying the type and concentration of the pH-sensitive functional groups, as well as the crosslinking density of the polymer network [218,219]. This allows for precise control over the pH range at which the hydrogel exhibits responsive behavior. pH-responsive polymer-based hydrogels have numerous applications, particularly in drug delivery systems and biosensors. In drug delivery, these hydrogels can be used to release drugs in a pH-dependent manner, where the hydrogel swells or collapses in response to the pH of the target site, leading to controlled release kinetics [129,130,131]. In biosensors, pH-responsive polymer-based hydrogels can serve as sensing elements that undergo changes in their optical or electrical properties in response to pH variations, enabling the detection of pH-related analytes or environmental changes [76,77,78]. The pH-responsive nature of these hydrogels makes them highly versatile and valuable in biomedical and biotechnological applications, providing a platform for responsive materials that can be tailored to the specific pH conditions encountered in biological systems.
Light-responsive polymer-based hydrogels, also known as photoresponsive or photosensitive hydrogels, are a type of hydrogel that can undergo changes in their properties or behavior upon exposure to light [121,122,123]. These hydrogels contain light-sensitive components or photoactive molecules that can be activated or deactivated by specific wavelengths of light [121]. Light-responsive polymer-based hydrogels can be classified into two main categories of photothermal-responsive polymer-based hydrogels and photoresponsive polymer-based hydrogels [122]. The first one exhibits a response to light in the form of heat generation. They are typically composed of polymers or nanoparticles that can convert light energy into heat through processes such as plasmonic absorption or photothermal conversion [123]. The heat generated can trigger changes in the swelling, sol–gel transition, or mechanical properties of the hydrogel. The second one undergoes changes in their structure, shape, or properties upon exposure to light, without involving heat generation [23]. This response is achieved through the incorporation of photoresponsive molecules, such as photochromic compounds or light-sensitive crosslinkers, into the polymer network [11]. These molecules undergo reversible photoisomerization or photodimerization reactions when illuminated with specific wavelengths of light, leading to conformational changes or crosslinking/de-crosslinking of the polymer network [23,122]. Light-responsive polymer-based hydrogels offer precise spatiotemporal control over their properties and functionalities, making them valuable in various applications such as drug delivery systems, tissue engineering, actuators and soft robotics, and optical sensors and imaging [121,122,123]. The choice of photoactive molecules and the design of the hydrogel network can be tailored to achieve the desired light responsiveness, such as specific light wavelengths, intensity, and response kinetics. This versatility allows for the development of smart materials with controlled and tunable photoresponsive properties for a wide range of applications [11,23,121,122,123].
Electric-field-responsive polymer-based hydrogels, also known as electroactive hydrogels, are a type of hydrogel that can undergo changes in their properties or behavior in the presence of an electric field [229,230]. These hydrogels contain electrically conductive components or responsive polymers that can be influenced by the application of an electric field [30,216]. The response of electric-field-responsive hydrogels can be attributed to several underlying mechanisms of electromechanical effect, electroosmosis, and electrically triggered release [70,229]. The response of electric-field-responsive hydrogels can be controlled by adjusting parameters such as the electric field strength, frequency, or waveform [216,230]. This allows for the precise modulation of the hydrogel’s behavior and functionality. Electric-field-responsive hydrogels find applications in various fields such as tissue engineering, sensors and actuators, and drug delivery [229,230]. The specific design and composition of electric-field-responsive hydrogels can vary depending on the desired application and the targeted response [30,70]. By integrating electrically responsive components into the hydrogel matrix, these materials offer unique opportunities for the development of advanced functional systems with electrically tunable properties [23,216,229,230].
Magnetic-field-responsive polymer-based hydrogels are a type of hydrogel that can exhibit changes in in their properties or behavior in the presence of a magnetic fields [126,127,128]. These hydrogels contain magnetic particles or responsive polymers that can be influenced by magnetic forces [222,223]. The response of magnetic-field-responsive hydrogels is attributed to the interaction between the embedded magnetic components and the applied magnetic field [126,222]. The magnetic particles or polymers within the hydrogel can respond to the magnetic field in several ways including magnetic actuation, thermal effects, and magnetic resonance imaging (MRI) contrast agents [127,223]. The response of magnetic-field-responsive hydrogels can be tuned by adjusting parameters such as the strength and orientation of the magnetic field, as well as the concentration and properties of the magnetic components within the hydrogel [126,127,128,223]. They have potential applications in drug delivery, tissue engineering, biomedical devices, and magnetic resonance imaging [222,223]. Magnetic-field-responsive polymer-based hydrogels offer unique advantages in terms of remote control, non-invasiveness, and tunability. Their ability to respond to magnetic fields opens up opportunities for various biomedical applications where external manipulation or control is desired [126,127,128,222,223].
Classifications of polymer-based hydrogels are listed in Table 3 as follows:
Table 3.
Classifications of polymer-based hydrogels in different ways.
| No. | Classifications of Polymer-Based Hydrogels | Type of Polymer-Based Hydrogels |
|---|---|---|
| 01 | Classification of polymer-based hydrogels based on origin data | Natural polymer-based hydrogels |
| Synthetic polymer-based hydrogels | ||
| Hybrid polymer-based hydrogels | ||
| 02 | Classification of polymer-based hydrogels based on composition | Homopolymer polymer-based hydrogels |
| Copolymer polymer-based hydrogels | ||
| Multipolymer polymer-based hydrogels | ||
| Interpenetrating network (IPN) polymer-based hydrogels | ||
| 03 | Classification of polymer-based hydrogels based on ionic charge | Neutral polymer-based hydrogels |
| Ionic polymer-based hydrogels | ||
| Ampholytic polymer-based hydrogels | ||
| 04 | Classification of polymer-based hydrogels based on pore size | Macroporous polymer-based hydrogels |
| Mesoporous polymer-based hydrogels | ||
| Microporous polymer-based hydrogels | ||
| 05 | Classification of polymer-based hydrogels based on physical appearance | Matrix polymer-based hydrogels |
| Film polymer-based hydrogels | ||
| Microsphere polymer-based hydrogels | ||
| Nanoparticle polymer-based hydrogels | ||
| Polymer-based hydrogel beads | ||
| 06 | Classification of polymer-based hydrogels based on crystallinity | Amorphous polymer-based hydrogels |
| Semi-crystalline polymer-based hydrogels | ||
| 07 | Classification of polymer-based hydrogels based on crosslinking | Chemical crosslinking polymer-based hydrogels |
| Physical crosslinking polymer-based hydrogels | ||
| 08 | Classification of polymer-based hydrogels based on external stimuli response | Temperature-responsive polymer-based hydrogels |
| pH-responsive polymer-based hydrogels | ||
| Light-responsive polymer-based hydrogels | ||
| Electric-field-responsive polymer-based hydrogels | ||
| Magnetic-field-responsive polymer-based hydrogels |
These classifications are not mutually exclusive, and a hydrogel can belong to more than one category depending on its properties and composition.
3.2. Main Engineering Properties of Polymer-Based Hydrogels’ Influence on DDSs
3.2.1. Swelling Property with Most Important Role in DDSs
Swelling is one of the most important characteristics of polymer-based hydrogels. Swelling in polymer-based hydrogels occurs when a solvent permeates and diffuses through the interstitial space within the hydrogel network [5,24,25,26]. The interstitial space is defined by the arrangement and density of the polymer chains, which are determined by the crosslinking process kinetics and conditions [45,55]. Several metrics are commonly used to quantify the characteristics of the interstitial space in a polymer-based hydrogel network [120,130]. The first is the molecular weight between crosslinks, referring to the average distance between two adjacent crosslinks along a polymer chain. A higher molecular weight between crosslinks corresponds to a larger distance, resulting in a more extended polymer network and larger interstitial spaces [169,170,171]. The second is mesh size, which represents the average distance between adjacent polymer chains within the hydrogel network. It determines the size of the gaps or voids available for solvent penetration [5,23]. A larger mesh size indicates larger interstitial spaces and higher swelling capacity. The last one is crosslink density where the number of crosslinks per unit volume in the hydrogel network is quantified [11,55]. A lower crosslink density leads to a more loosely packed polymer network, creating larger interstitial spaces and promoting higher swelling capabilities [17,120]. These metrics play a crucial role in understanding and predicting the swelling behavior of hydrogels [23]. By manipulating the crosslinking conditions, such as polymer concentration, crosslinker concentration, and reaction time, it is possible to control the interstitial space and subsequently the swelling properties of the polymer-based hydrogel [11,23,169,170,171].
Polymer-based hydrogels have a unique ability to absorb and retain large amounts of water due to the presence of hydrophilic groups in their polymer chains [5,23]. The swelling behavior of hydrogels is influenced by several factors, such as the chemical composition of the hydrogel, crosslinking density, and the properties of the solvent. It can be described by parameters such as equilibrium swelling ratio (Q), swelling kinetics, and diffusion coefficients [11,120].
| (1) |
Ws is the weight of the swollen hydrogel.
Wd is the hydrogel’s weight before swelling with water.
The equilibrium swelling ratio (Q) is a parameter that quantifies the extent of swelling exhibited by a polymer-based hydrogel. It is defined as the ratio of the weight or swollen volume of the hydrogel to its dry weight or volume in equilibrium with the surrounding solvent [23,24,25,26]. Q is a function of the crosslinking density, degree of ionization of the functional groups, temperature, and pH of the surrounding medium. Q provides information about the capacity of the hydrogel to absorb and retain water, and it is influenced by the polymer structure, crosslinking density, and interactions with the solvent [45,55].
Swelling kinetics refers to the time-dependent process of hydrogel swelling. It involves the absorption of solvent molecules into the hydrogel network and the subsequent equilibrium establishment [11,45]. The kinetics can be influenced by factors such as the diffusivity of the solvent, the presence of barriers or hindrances within the hydrogel structure, and the availability of swelling sites [23,130]. Understanding the swelling kinetics is important for optimizing hydrogel performance in applications where controlled swelling or the release of substances is desired [24,25,26,169,170,171].
Diffusion coefficients are parameters that describe the rate at which solutes can diffuse within the hydrogel network. They provide information about the mobility of solute molecules within the hydrogel and their ability to traverse the polymer chains or interstitial spaces [11,23,24,25,26]. Diffusion coefficients are affected by the porosity of the hydrogel, polymer chain density, and interactions between the solute and the hydrogel matrix [45,45]. Knowledge of diffusion coefficients is essential for designing the hydrogels used in drug delivery systems, as it influences the release kinetics of encapsulated substances.
The swelling properties of hydrogels make them attractive for various applications such as drug delivery, tissue engineering, and biosensors [11,23]. In drug delivery, the swelling properties of hydrogels can be utilized to control the release of drugs by adjusting the crosslinking density and the degree of ionization of the functional groups [23,24,25,26,120]. In tissue engineering, hydrogels can provide a three-dimensional matrix for cell growth and proliferation due to their ability to mimic the extracellular matrix of natural tissues [169,170,171]. In biosensors, hydrogels can be used as a transducer to convert biological signals into measurable signals by incorporating enzymes or antibodies into the hydrogel network [5,11,120,130]. There are several factors that can affect the swelling properties of hydrogels, including:
Chemical composition: The chemical composition of the hydrogel polymer can affect the swelling properties. Hydrogels with more hydrophilic groups (such as hydroxyl, amide, or carboxyl groups) tend to have higher swelling ratios than those with fewer hydrophilic groups [5,23].
Crosslinking density: The degree of crosslinking of the hydrogel network affects the swelling properties. Hydrogels with a higher crosslinking density tend to have a lower swelling ratio, as there are fewer available spaces for water molecules to enter and swell the hydrogels [11,23,24,25,26].
pH and ionic strength: Changes in the pH and ionic strength of the surrounding environment can affect the swelling properties of hydrogels. For example, acidic environments can protonate amine groups on the polymer chains, leading to a decrease in swelling. On the other hand, basic environments can deprotonate carboxylic acid groups on the polymer chains, leading to an increase in swelling [11,17,23,169,170,171].
Temperature: Temperature can affect the swelling properties of some hydrogels. For example, some thermo-responsive hydrogels can swell or shrink in response to changes in temperature [5,23,24,25,26].
Presence of other molecules: The presence of other molecules in the surrounding environment, such as salts or other solvents, can affect the swelling properties of hydrogels. These molecules can compete with water molecules for space within the hydrogel network, leading to changes in swelling [5,11,17].
3.2.2. Permeation Property in Biomedical Applications
The permeation property of polymer-based hydrogels refers to their ability to allow the transport of molecules and ions through their three-dimensional network structure [23,166]. Polymer-based hydrogels can exhibit different permeation characteristics depending on their composition, crosslinking density, pore size, and other factors [11,48]. Understanding and controlling the permeation properties of hydrogels are crucial for their applications in fields such as drug delivery, tissue engineering, and biosensing [23,172]. The permeation behavior of polymer-based hydrogels is influenced by several factors, such as molecular size, pore size, crosslinking density, and chemical composition [11,17,23,172].
Molecular size: Hydrogels can selectively permeate molecules based on their size. Smaller molecules, such as gases, ions, and small hydrophilic compounds, can diffuse more easily through the hydrogel network [23]. In contrast, larger molecules, such as proteins or macromolecules, face greater resistance and may have limited permeability [11,23,48].
Pore size: The pores are characteristic of the porous polymer-based hydrogels. This is to make it clear that not all polymer-based hydrogels are porous. With the porous polymer-based hydrogels, it is the size of the pores which plays a significant role in determining the permeation properties [11,23]. Hydrogels with larger pore sizes generally exhibit higher permeability, allowing for the easier passage of molecules through the network [166,172]. The pore size can be controlled by adjusting the crosslinking density or by incorporating porogens during hydrogel synthesis [23,48].
Crosslinking density: The degree of crosslinking within the hydrogel network can affect permeation. A higher crosslinking density can lead to smaller pore sizes and reduced permeability, while lower crosslinking density can result in larger pores and increased permeability [11,23,166].
Chemical Composition: The chemical composition of the hydrogel, including the polymer type and functional groups, can influence permeation. Hydrogels made from polymers with charged functional groups may interact with charged molecules, affecting their permeation. Additionally, the presence of specific functional groups can be utilized to design hydrogels with selective permeation properties for targeted applications [11,23,172].
Controlling the permeation properties of polymer-based hydrogels allows for the design of materials with specific transport characteristics [23,48]. For example, hydrogels can be engineered to selectively allow the passage of certain molecules while restricting the permeation of others [48,172]. This control is essential in applications such as drug delivery, where controlled release kinetics and targeted delivery are desired. In tissue engineering, permeable hydrogels can facilitate nutrient and oxygen transport to support cell growth and viability [11,23,166]. The permeation properties of hydrogels can be tailored to meet specific needs for drug delivery, tissue engineering, and other applications.
3.2.3. Mechanical Properties with a Crucial Role in Drug Delivery Systems
The mechanical properties of polymer-based hydrogels play a crucial role in drug delivery systems. These properties determine the stability, integrity, and functionality of the hydrogel as it interacts with biological tissues and releases drugs in a controlled manner [38,174,190,191,231]. Several key mechanical properties of hydrogels are relevant to drug delivery systems.
Elasticity and flexibility: The elasticity and flexibility of hydrogels influences their ability to conform to the surrounding tissue and withstand mechanical stresses [190,191,231]. Hydrogels with appropriate elasticity can adhere to irregular surfaces, such as wound sites, or be implanted in specific locations. This property ensures good contact with the target site and prevents the premature degradation or disintegration of the hydrogel [23,38,231].
Chemical composition: The chemical composition of the hydrogel can also affect its mechanical properties [11,190,191]. For example, hydrogels made from poly(acrylic acid) are generally brittle and have poor mechanical strength [232] while hydrogels made from poly(ethylene glycol) are more elastic and flexible [205]. Additionally, the presence of functional groups, such as double bonds, can also enhance the mechanical properties of hydrogels [23,231].
Swelling behavior: The swelling behavior of hydrogels is important in drug delivery systems. Swelling affects the release rate and diffusion of drugs from the hydrogel matrix. Controlled swelling can provide sustained release over an extended period [11,23]. Additionally, the extent of swelling can impact the mechanical stability of the hydrogel, affecting its ability to retain shape and integrity during drug release [17,231].
Viscoelasticity: The viscoelastic nature of hydrogels refers to their ability to exhibit both elastic and viscous behavior under mechanical stress [11]. Viscoelasticity is relevant in drug delivery systems as it affects the hydrogel’s ability to absorb and dissipate mechanical forces [23]. A suitable balance of elasticity and viscosity allows hydrogels to accommodate mechanical deformations, such as tissue movements or compression, without compromising their structural integrity [23,191].
Adhesion and cohesion: Adhesion and cohesion properties influence the interaction between the hydrogel and the surrounding tissue [11,17]. Adequate adhesion promotes close contact between the hydrogel and the target tissue, enhancing drug delivery efficiency. Cohesion is essential to maintain the integrity of the hydrogel and prevent drug leakage or migration [23,231].
The mechanical strength of hydrogels determines their ability to maintain structural integrity under mechanical forces. Hydrogels should possess sufficient strength to withstand handling during fabrication, implantation, and drug release [17,38]. Mechanical strength prevents structural failure and ensures the hydrogel remains intact throughout the drug delivery process [174]. The mechanical properties of polymer-based hydrogels can be tailored through various strategies, including adjusting the polymer composition, crosslinking density, and incorporating reinforcing materials or fillers [190,191]. By carefully controlling these mechanical properties, drug delivery systems can be optimized to achieve the desired drug release kinetics, improve tissue compatibility, and enhance therapeutic efficacy [23,191]. It is important to note that the mechanical properties of hydrogels used in drug delivery systems should be carefully optimized to ensure they meet the specific requirements of the application [231]. For instance, hydrogels for implantable devices or injectable systems may have different mechanical considerations than hydrogels used in topical or transdermal drug delivery [17]. Therefore, a thorough understanding of the mechanical behavior and requirements of the drug delivery system is crucial for a successful translation and implementation in biomedical applications.
3.2.4. Biological Properties of Polymer-Based Hydrogels for DDSs
Polymer-based hydrogels used in drug delivery systems possess various biological properties that are important for their performance and effectiveness [3,8]. These properties enable hydrogels to interact with biological systems and facilitate controlled drug release [11,12]. Some key biological properties of polymer-based hydrogels for drug delivery systems include the following:
Biocompatibility refers to the ability of a material to coexist with living tissues without causing adverse reactions or toxicity [41,233]. Polymer-based hydrogels intended for drug delivery systems should exhibit high biocompatibility to minimize immune responses, inflammation, or tissue damage upon implantation or administration [101]. Biocompatible hydrogels ensure safe and well-tolerated drug delivery within the body [102].
Bioadhesion is the ability of hydrogels to adhere to biological tissues or surfaces. This property is particularly relevant for local drug delivery applications, where the hydrogel needs to adhere to the target site, such as wounds or mucosal membranes [23,233]. Bioadhesive hydrogels can prolong drug residence time, enhance drug penetration into tissues, and provide sustained drug release at the site of action [101,102].
Cell interaction and the tissue integration of polymer-based hydrogels meet in certain drug delivery applications, such as tissue engineering or regenerative medicine, where hydrogels are designed to interact with cells and support tissue growth and integration [234]. Hydrogels with appropriate biological properties can promote cell adhesion, proliferation, and differentiation, facilitating tissue regeneration and healing processes [235].
Controlled biodegradability is an important property for polymer-based hydrogels in drug delivery systems, as it allows for the gradual degradation and clearance of the hydrogel after drug release [2,11]. Controlled biodegradability ensures that the hydrogel is metabolized or eliminated from the body without causing harm or leaving residues. The degradation rate can be tailored to match the desired drug release kinetics and the tissue healing timeline [23,66].
The immunomodulation of polymer-based hydrogels influences the immune response at the site of drug delivery [11]. Depending on the application, hydrogels can be designed to stimulate or suppress immune reactions to optimize therapeutic outcomes. Immunomodulatory hydrogels can help promote tissue healing, prevent immune rejection, or enhance the effectiveness of immunotherapeutic drugs [17,23].
Drug stability and protection: Polymer-based hydrogels can provide protection to encapsulated drugs from degradation or inactivation [12,125]. They can shield drugs from enzymatic degradation, pH variations, or other harsh conditions in the body, preserving their stability and therapeutic activity until release [80,129]. This property is particularly important for sensitive drugs that require protection during transit to the target site [11,23].
By considering these biological properties, polymer-based hydrogels can be tailored to achieve an optimal drug delivery performance, ensuring compatibility with biological systems, the controlled release of therapeutic agents, and minimization of adverse effects [41]. The selection of appropriate polymer materials, fabrication techniques, and formulation strategies plays a crucial role in achieving the desired biological properties for drug delivery systems [23,101,102].
3.3. Applications of Polymer-Based Hydrogels in Drug Delivery Systems
Polymer-based hydrogels have been widely investigated for drug delivery applications due to their unique properties such as a high water content, biocompatibility, and the ability to respond to various stimuli [11,23]. Some of the applications of hydrogels in drug delivery systems include the following:
Controlled drug release: Polymer-based hydrogels can be used to control the release of drugs by varying the swelling behavior of the hydrogel. By altering the chemical composition or crosslinking density of the hydrogel, the release rate of the drug can be controlled [29,134].
Targeted drug delivery: Polymer-based hydrogels can be designed to specifically target certain tissues or cells. By incorporating targeting moieties such as antibodies or peptides into the hydrogel, the drug can be delivered to a specific site within the body [16,105].
Oral drug delivery: Polymer-based hydrogels can be used to improve the oral bioavailability of drugs. By encapsulating the drug within a hydrogel matrix, the drug can be protected from degradation in the gastrointestinal tract and released in a controlled manner [8,9,16].
Transdermal drug delivery: Polymer-based hydrogels can be used for transdermal drug delivery by incorporating the drug into the hydrogel matrix. The hydrogel can then be applied topically to the skin, and the drug will be released in a controlled manner over time [136,236].
Implantable drug delivery systems: Polymer-based hydrogels can be used as implantable drug delivery systems, where the hydrogel is placed within the body and releases the drug over an extended period of time. These systems can be used for the treatment of chronic diseases or for the delivery of long-acting drugs [69,108].
Gene delivery: Polymer-based hydrogels can also be used for the delivery of genetic material such as DNA or RNA. By incorporating the genetic material into the hydrogel matrix, the material can be protected from degradation and delivered to specific cells or tissues [115,237].
The unique properties of polymer-based hydrogels make them a promising candidate for drug delivery applications, and ongoing research in this area is expected to lead to the development of new and innovative drug delivery systems. There are common hydrogel-based products known as biotene, Simpurity™ Hydrogel (SupremeMed, Van Nuys City, City of Los Angeles, CA, USA), Soflens daily disposable, Nicorette®( Johnson & Johnson, Stockholm, Sweden), Neutrogena® Hydro Boost® (Johnson & Johnson, City of Los Angeles, CA, USA), Sericin (Huzhou Shengtao Biotech, Zhejiang, China), Suprasorb® G (Lohmann & Rauscher, Rengsdorf, Germany) and others.
3.3.1. Biotene Products
Biotene is an oral moisturizing agent that is commonly used for treating dry mouth. The product is manufactured by GlaxoSmithKline (London, United Kingdom) and contains a mixture of ingredients, including carbomer and hydroxyethyl cellulose, which are hydrogels that have the ability to absorb water and retain it within their three-dimensional structures. These hydrogels provide a sustained release of moisture in the oral cavity, relieving the symptoms of dry mouth and promoting oral health. Biotene is also available in other formulations, including mouthwash, toothpaste, and oral gel, and is recommended for individuals with dry mouth caused by medication, radiation therapy, or Sjogren’s syndrome [57].
3.3.2. SimpurityTM Hydrogel
Simpurity™ (from SupremeMed, Van Nuys City, City of Los Angeles, United States) Hydrogel from Safe n’ Simple is a hydrogel product that is used to treat skin burns, dry wounds, and dry scabs. The product is made from a combination of polyethylene oxide (PEO), polyvinyl alcohol (PVA), acrylate, polyurethane, and pure water to create absorbent sheets. The hydrogel is designed to provide a moist environment for wound healing and can also help to reduce pain and inflammation. It is a widely used product for wound care and is known for its effectiveness in promoting wound healing [232].
3.3.3. Soflens Daily Disposable
Soflens daily disposable from Bausch & Lomb (New York, NY, USA) is a contact lens product used to correct short- and long-sightedness. The hydrogel material used in this product allows for a high water content and oxygen permeability, making the lenses comfortable for extended wear. The hydrogel also helps to maintain moisture around the lens, preventing dryness and discomfort for the wearer [194].
3.3.4. Nicorette® Hydrogel
Nicorette® hydrogel from GlaxoSmithKline (London, UK) is a chewing gum used as a smoking cessation aid. It contains hydroxypropyl methylcellulose as one of its components. The hydrogel in the chewing gum acts as a carrier for the nicotine and helps to release it slowly over time, providing a controlled release of nicotine to help with cravings and withdrawal symptoms during the quitting process [57].
3.3.5. Neutrogena® Hydro Boost® Hydrogel
Neutrogena® Hydro Boost® is a hydrogel-based face mask from Johnson and Johnson (City of Los Angeles, CA, USA)) that is used to provide the skin with immediate and long-lasting moisture. The key ingredient in the mask is hyaluronic acid, which is a naturally occurring polysaccharide that can hold up to 1000 times its weight in water. The hydrogel mask is designed to adhere to the skin and slowly release the hydrating ingredients over time, leaving the skin feeling soft, supple, and moisturized [85].
3.3.6. Sericin Hydrogel
Sericin (Huzhou Shengtao Biotech, Zhejiang, China) has also been investigated for its potential use in drug delivery systems. In one study, sericin was used as a carrier for an optically trackable drug delivery system for malignant melanoma. The sericin nanoparticles loaded with the drug were shown to effectively deliver the drug to cancer cells and inhibit their growth, indicating its potential as a promising drug delivery system for cancer therapy [238].
3.3.7. Suprasorb® G Hydrogel
Suprasorb G (Lohmann & Rauscher, Rengsdorf, Germany) hydrogel is a wound dressing that is used for the management of various types of wounds such as lower leg ulcers, pressure ulcers, first- and second-degree burns, and scalds. The hydrogel is composed of a blend of acrylic polymers, polyethylene (PE), and phenoxyethanol, and contains 70% water. The hydrogel provides a moist environment for the wound, which promotes wound healing by facilitating the migration of cells and promoting the formation of granulation tissue. The water content of the hydrogel also helps to cool the wound, reducing pain and inflammation. Suprasorb G hydrogel is easy to apply and remove and can be used on both dry and exuding wounds [46].
3.4. Current and Future Trends of Research on Polymer-Based Hydrogels Applied in Drug Delivery Systems
The increasing number of research articles on polymer-based hydrogels, particularly in the field of drug delivery, reflects the growing interest and recognition of the potential of hydrogel-based systems in biomedical applications [11,23,101,102,233]. The unique properties of hydrogels, such as their high water content, biocompatibility, and tunable mechanical properties, make them highly suitable for drug delivery applications [11,23,142,143,144,145,146]. The graph in Figure 2 illustrates the significant growth in research publications related to polymer-based hydrogels from 2000 to 2022. The number of publications has steadily increased over the years, indicating the expanding research efforts in this field. In 2005, there were less than 1000 publications per year on polymer-based hydrogel materials in general, with less than 400 publications per year specifically focused on polymer-based hydrogels for drug delivery, accounting for less than 35% of the total. Between 2005 and 2015, there was a steady increase in research publications. In 2015, the number of publications on polymer-based hydrogel materials reached nearly 4000, with around 1650 articles specifically dedicated to polymer-based hydrogels for drug delivery, accounting for approximately 38% of the total publications in the field. From 2015 to the present, there has been a remarkable jump in research related to hydrogels. For instance, in 2022, the number of publications on polymer-based hydrogel materials surpassed 12,000, with more than 5000 articles specifically focused on polymer-based hydrogels for drug delivery, accounting for over 42% of the total publications. This upward trend signifies the increasing recognition of hydrogels as a promising platform for drug delivery applications. The continuous growth in research indicates the ongoing exploration of novel hydrogel formulations, synthesis methods, drug encapsulation techniques, and delivery mechanisms. As researchers uncover new insights and address existing challenges, the field of hydrogel-based drug delivery is expected to further expand in the future, leading to the development of more advanced and efficient drug delivery systems.
Figure 2.
Increasing number of publications related to polymer-based hydrogels and polymer-based hydrogels for drug delivery systems from 2000 to 2022.
Current and future research on polymer-based hydrogels applied in drug delivery systems is focused on advancing the field by addressing existing challenges and exploring innovative approaches. In the future, it is predicted that the key trends and areas of research in the polymer-based hydrogels applied for drug delivery systems will include the following:
Advanced drug release strategies: Researchers are developing novel drug release strategies that offer precise control over the release rate and duration of therapeutic agents. This includes the development of stimuli-responsive polymer-based hydrogels that can release drugs in response to specific triggers such as pH, temperature, enzymes, or light. Additionally, efforts are being made to incorporate drug delivery mechanisms such as sustained release, pulsatile release, and on-demand release into polymer-based hydrogel systems.
Targeted and site-specific delivery: Enhancing the targeting efficiency and specificity of drug delivery systems is a major focus. Researchers are exploring the incorporation of targeting ligands, such as antibodies, peptides, or aptamers, into polymer-based hydrogels to improve the delivery of drugs to specific cells, tissues, or organs. The use of external stimuli, such as magnetic fields or ultrasound, to guide the polymer-based hydrogel to the target site is also being investigated.
Combination therapy: Polymer-based hydrogels are being studied for their potential to deliver multiple therapeutic agents simultaneously, enabling combination therapy. This includes the co-delivery of drugs with different mechanisms of action or the incorporation of drugs and biological molecules, such as growth factors or gene therapies, within the polymer-based hydrogel matrix. Combination therapy can enhance therapeutic efficacy, reduce side effects, and overcome drug resistance.
Bioactive polymer-based hydrogels: Researchers are incorporating bioactive molecules, such as peptides or growth factors, into hydrogels to promote tissue regeneration and healing. These bioactive polymer-based hydrogels can provide a suitable microenvironment for cells, promote cell adhesion and proliferation, and support tissue integration. Such polymer-based hydrogels hold promise for applications in wound healing, tissue engineering, and regenerative medicine.
Nanotechnology and nanoparticles: Nanoparticles and nanotechnology are being integrated into polymer-based hydrogel systems to enhance drug loading, stability, and release. Nanoparticles, such as liposomes, polymeric nanoparticles, or inorganic nanoparticles, can be incorporated within the polymer-based hydrogel matrix or used as carriers to encapsulate drugs. These nanoparticles can provide controlled release profiles, protect drugs from degradation, and enable targeted delivery.
3D printing and additive manufacturing: Advances in 3D printing and additive manufacturing techniques have opened new avenues for the fabrication of complex and customized hydrogel-based drug delivery systems. Researchers are exploring the use of 3D printing to create patient-specific implants, scaffolds, or drug-loaded structures with precise control over shape, architecture, and drug distribution.
Smart polymer-based hydrogels and sensors: The integration of smart polymer-based hydrogels with sensing capabilities is an emerging area of research. These hydrogels can detect and respond to specific biological or environmental cues, such as pH changes, enzyme activity, or the presence of specific biomarkers. By incorporating sensors into polymer-based hydrogels, the real-time monitoring of drug release, therapeutic efficacy, or disease progression can be achieved.
Biodegradability and sustainability: Researchers are focusing on developing biodegradable hydrogels that can degrade in a controlled manner, eliminating the need for surgical removal. The use of biocompatible and sustainable materials, such as natural polymers or biomimetic materials, is also gaining attention to reduce the environmental impact of hydrogel-based drug delivery systems.
The future of research into polymer-based hydrogels for drug delivery systems lies in designing more sophisticated, targeted, and patient-specific approaches. The integration of advanced technologies, materials, and knowledge from various disciplines will continue to drive innovation in this field, leading to improved therapeutic outcomes and personalized medicine.
4. Conclusions
Polymer-based hydrogels have emerged as a promising class of materials for drug delivery systems, offering unique properties that make them highly suitable for biomedical applications. Their high water content, soft and elastic texture, and biocompatibility make them well suited for interacting with biological systems. Throughout this review, we have explored various hydrogel-based drug delivery systems and highlighted their advantages. One key advantage is ability of hydrogels to achieve sustained drug release, ensuring a controlled and prolonged delivery of therapeutic agents. This is particularly beneficial for drugs that require a specific release profile or long-term treatment. Another advantage is the potential for targeted drug delivery. By incorporating targeting moieties or modifying the polymer-based hydrogel’s properties, drugs can be delivered specifically to a desired site within the body, minimizing systemic exposure and reduced toxicity. Moreover, the increasing number of publications on polymer-based hydrogels in the past two decades indicates the growing interest and importance of these materials in the biomedical field. This active research and development contributes to the continuous improvement of polymer-based hydrogel properties and functionalities. It is expected that further advancements will lead to new and innovative applications of polymer-based hydrogels in the future. Beyond drug delivery, polymer-based hydrogels have shown potential in tissue engineering, wound healing, and biosensing applications. Their biocompatibility and ability to mimic the extracellular matrix make them valuable scaffolds for tissue regeneration and repair. Additionally, polymer-based hydrogels can be designed to respond to specific biological signals, enabling their use in biosensors for the detection and monitoring of biomarkers. Polymer-based hydrogels for drug delivery systems hold great promise in revolutionizing the treatment of various diseases and medical conditions. By improving drug efficacy, reducing side effects, and enhancing patient compliance, polymer-based hydrogels have the potential to significantly improve healthcare outcomes. Additionally, their versatility and wide range of applications make them an exciting area of research and development with promising opportunities to advance medical science.
Acknowledgments
We would like to thank Ho Chi Minh City University of Food Industry for their support.
Author Contributions
Conceptualization, N.H.T. and T.B.C.; methodology, N.H.T.; software, D.X.C.; validation, N.H.T., T.B.C. and D.X.C.; formal analysis, N.H.T.; investigation, N.H.T.; resources, N.H.T.; data curation, N.H.T.; writing—original draft preparation, N.H.T.; writing—review and editing, N.H.T.; visualization, D.X.C.; supervision, N.H.T.; project administration, D.X.C.; funding acquisition, N.H.T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Hubbell J.A. Hydrogel systems for barriers and local drug delivery in the control of wound healing. J. Control. Release. 1996;39:305–313. doi: 10.1016/0168-3659(95)00162-X. [DOI] [Google Scholar]
- 2.Hubbell J.A. Synthetic biodegradable polymers for tissue engineering and drug delivery. Curr. Opin. Solid State Mater. Sci. 1998;3:246–251. doi: 10.1016/S1359-0286(98)80098-3. [DOI] [Google Scholar]
- 3.Perrie Y., Rades T. Pharmaceutics—Drug Delivery and Targeting. 2nd ed. Pharmaceutical Press; London, UK: 2009. pp. 1–240. [Google Scholar]
- 4.Wang Y., Malcolm D.W., Benoit D.S.W. Controlled and sustained delivery of siRNA/NPs from hydrogels expedites bone fracture healing. Biomaterials. 2017;139:127–138. doi: 10.1016/j.biomaterials.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brazel C.S., Peppas N.A. Dimensionless analysis of swelling of hydrophilic glassy polymers with subsequent drug release from relaxing structures. Biomaterials. 1999;20:721–732. doi: 10.1016/S0142-9612(98)00215-4. [DOI] [PubMed] [Google Scholar]
- 6.Campea M., Lofts A., Xu F., Yeganeh M., Kostashuk M., Hoare T. Disulfide-Cross-Linked Nanogel-Based Nanoassemblies for Chemotherapeutic Drug Delivery. ACS Appl. Mater. Interfaces. 2023;15:25324–25338. doi: 10.1021/acsami.3c02575. [DOI] [PubMed] [Google Scholar]
- 7.Qiu Y. Environment-sensitive hydrogels for drug delivery. Adv. Drug Deliv. Rev. 2012;64:49–60. doi: 10.1016/j.addr.2012.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Chien Y. Novel Drug Delivery Systems. 2nd ed. CRC Press; Boca Raton, FL, USA: 1991. [Google Scholar]
- 9.Caló E. Biomedical applications of hydrogels: A review of patents and commercial products. Eur. Polym. J. 2014;65:252–267. doi: 10.1016/j.eurpolymj.2014.11.024. [DOI] [Google Scholar]
- 10.Das D., Pal S. Modified biopolymer-dextrin based crosslinked hydrogels: Application in controlled drug delivery. RSC Adv. 2015;5:25014–25050. doi: 10.1039/C4RA16103C. [DOI] [Google Scholar]
- 11.Ghosal A., Kaushik A.K. Intelligent Hydrogels in Diagnostics and Therapeutics. CRC Press; Boca Raton, FL, USA: 2020. [Google Scholar]
- 12.Knipe J.M., Chen F., Peppas N.A. Enzymatic Biodegradation of Hydrogels for Protein Delivery Targeted to the Small Intestine. Biomacromolecules. 2015;16:962–972. doi: 10.1021/bm501871a. [DOI] [PubMed] [Google Scholar]
- 13.He Y.J., Young D.A., Mededovic M., Li K., Li C., Tichauer K., Venerus D., Papavasiliou G. Protease-Sensitive Hydrogel Biomater with Tunable Modulus and Adhesion Ligand Gradients for 3D Vascular Sprouting. Biomacromolecules. 2018;19:4168–4181. doi: 10.1021/acs.biomac.8b00519. [DOI] [PubMed] [Google Scholar]
- 14.Yin Y., Papavasilion G., Zaborina O.Y., Alverdy J.C., Teymour F. Synthesis and Functional Analysis of Polyphosphate-Loaded Poly(Ethylene) Glycol Hydrogel Nanoparticles Targeting Pyocyanin and Pyoverdin Production in Pseudomonas aeruginosa as a Model Intestinal Pathogen. Ann. Biomed. Eng. 2017;45:1058–1068. doi: 10.1007/s10439-016-1740-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Porter T.L., Stewart R., Reed J., Morton K. Models of hydrogel swelling with applications to hydration sensing. Sensors. 2007;7:1980–1991. doi: 10.3390/s7091980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bindu Sri M., Ashok V., Arkendu C. As A Review on Hydrogels as Drug Delivery in the Pharmaceutical Field. Int. J. Pharm. Chem. Sci. 2012;1:642–661. [Google Scholar]
- 17.Ottenbrite R.M., Park K., Okano T. Biomedical Applications of Hydrogels Handbook. Springer; New York, NY, USA: 2010. p. 204. [Google Scholar]
- 18.Licht C., Rose J.C., Anarkoli A.O., Blondel D., Roccio M., Haraszti T., Gehlen D.B., Hubbell J.A., Lutolf M.P., De Laporte L. Synthetic 3D PEG-Anisogel Tailored with Fibronectin Fragments Induce Aligned Nerve Extension. Biomacromolecules. 2019;20:4075–4087. doi: 10.1021/acs.biomac.9b00891. [DOI] [PubMed] [Google Scholar]
- 19.Serra L., Doménech J., Peppas N.A. Drug transport mechanisms and release kinetics from molecularly designed poly(acrylic acid-g-ethylene glycol) hydrogels. Biomaterials. 2006;27:5440–5451. doi: 10.1016/j.biomaterials.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 20.Stano A., Scott E.A., Dane K.Y., Swartz M.A., Hubbell J.A. Tunable T cell immunity towards a protein antigen using polymersomes vs. solid-core nanoparticles. Biomaterials. 2013;34:4339–4346. doi: 10.1016/j.biomaterials.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 21.Clegg J.R., Peppas N.A. Design of Synthetic Hydrogel Compositions for Noncovalent Protein Recognition. ACS Appl. Mater. Interfaces. 2023. in press . [DOI] [PubMed]
- 22.McCall J.D., Lin C.C., Anseth K.S. Affinity Peptides Protect Transforming Growth Factor Beta during Encapsulation in Poly(ethylene glycol) Hydrogels. Biomacromol. 2011;14:1051–1057. doi: 10.1021/bm101379v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thakur V.K., Thakur M.K., editors. Hydrogels. Springer; Singapore: 2018. [Google Scholar]
- 24.Flemming M., Peppas N.A. Complexation graft copolymer networks: Swelling properties, calcium binding and proteolytic enzyme inhibition. Biomaterials. 1999;20:1701–1708. doi: 10.1016/s0142-9612(99)00071-x. [DOI] [PubMed] [Google Scholar]
- 25.Ganji F., Vasheghani-Farahani S., Vasheghani-Farahani E. Theoretical Description of Hydrogel Swelling: A Review. Iranian Pol. J. 2010;19:375–398. [Google Scholar]
- 26.Fraser D., Nguyen T., Kotelsky A., Lee W., Buckley M., Benoit D.S.W. Hydrogel Swelling-Mediated Strain Induces Cell Alignment at Dentin Interfaces. ACS Biomater. Sci. Eng. 2022;8:3568–3575. doi: 10.1021/acsbiomaterials.2c00566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang H., Dong Z., Ren X., Jia B., Li G., Zhou S., Zhao X., Wang W. High-strength hydrogels: Fabrication, reinforcement mechanisms, and applications. Nano Res. 2023;16:3475–3515. doi: 10.1007/s12274-022-5129-1. [DOI] [Google Scholar]
- 28.Caldwell A.S., Rao V.V., Golden A.C., Anseth K.S. Porous bio-click microgel scaffolds control hMSC interactions and promote their secretory properties. Biomaterials. 2020;232:119725. doi: 10.1016/j.biomaterials.2019.119725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mastropietro D.J., Omidian H., Park K. Drug delivery applications for superporous hydrogels. Expert Opin. Drug Deliv. 2012;9:71–89. doi: 10.1517/17425247.2012.641950. [DOI] [PubMed] [Google Scholar]
- 30.Xie S., Ren T., Chen G., Zhou Z., Li Z., Wu W., Huang L. High-performance porous copolymer hydrogel for oceanic electricity generation. Chem. Eng. J. 2023;456:140983. doi: 10.1016/j.cej.2022.140983. [DOI] [Google Scholar]
- 31.Foudazi R., Zowada R., Manas-Zloczower I., Feke D.L. Porous Hydrogels: Present Challenges and Future Opportunities. Langmuir. 2023;39:2092–2111. doi: 10.1021/acs.langmuir.2c02253. [DOI] [PubMed] [Google Scholar]
- 32.Wei S.-Y., Chen T.-H., Kao F.-S., Hsu Y.-J., Chen Y.-C. Strategy for improving cell-mediated vascularized soft tissue formation in a hydrogen peroxide-triggered chemically-crosslinked hydrogel. J. Tissue Eng. 2022;13:1–20. doi: 10.1177/20417314221084096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weiss A.M., Hossainy S., Rowan S.J., Hubbell J.A., Esser-Kahn A.P. Immunostimulatory Polymers as Adjuvants, Immunotherapies, and Delivery Systems. Macromolecules. 2022;55:6913–6937. doi: 10.1021/acs.macromol.2c00854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kavimandan N.J., Losi E., Peppas N.A. Novel delivery system based on complexation hydrogels as delivery vehicles for insulin–transferrin conjugates. Biomaterials. 2006;27:3846–3854. doi: 10.1016/j.biomaterials.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 35.Elbert D.L., Hubbell J.A. Conjugate Addition Reactions Combined with Free-Radical Cross-Linking for the Design of Materials for Tissue Engineering. Biomacromolecules. 2001;2:430–441. doi: 10.1021/bm0056299. [DOI] [PubMed] [Google Scholar]
- 36.Blatchley M.R., Anseth K.S. Middle-out methods for spatiotemporal tissue engineering of organoids. Nat. Rev. Bioeng. 2023;1:329–345. doi: 10.1038/s44222-023-00039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li H., Li B., Lv D., Li W., Lu Y., Luo G. Biomater releasing drug responsively to promote wound healing via regulation of pathological microenvironment. Adv. Drug. Deliv. Rev. 2023;196:114778. doi: 10.1016/j.addr.2023.114778. [DOI] [PubMed] [Google Scholar]
- 38.Zhou R., Zhou Q., Ling G., Zhang P. A cross-linked hydrogel of bismuth sulfide nanoparticles with excellent photothermal antibacterial and mechanical properties to combat bacterial infection and prompt wound healing. Colloids Surf. A Physicochem. Eng. Asp. 2023;660:130832. doi: 10.1016/j.colsurfa.2022.130832. [DOI] [Google Scholar]
- 39.Yang J., Wang S. Polysaccharide-Based Multifunctional Hydrogel Bio-Adhesives for Wound Healing: A Review. Gels. 2023;9:138. doi: 10.3390/gels9020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang W., Dai J., Huang Y., Li X., Yang J., Zheng Y., Shi X. Extracellular matrix mimicking dynamic interpenetrating network hydrogel for skin tissue engineering. Chem. Eng. J. 2023;457:141362. doi: 10.1016/j.cej.2023.141362. [DOI] [Google Scholar]
- 41.Halstenberg S., Panitch A., Rizzi S., Hall H., Hubbell J.A. Biologically Engineered Protein-graft-Poly(ethylene glycol) Hydrogels: A Cell Adhesive and Plasmin-Degradable Biosynthetic Material for Tissue Repair. Biomacromolecules. 2002;3:710–723. doi: 10.1021/bm015629o. [DOI] [PubMed] [Google Scholar]
- 42.Ma X., Luan Z., Li J. Inorganic Nanoparticles-Based Systems in Biomedical Applications of Stem Cells: Opportunities and Challenges. Int. J. Nanomed. 2023;18:143–182. doi: 10.2147/IJN.S384343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lin X., Wang J., Wu X., Luo Y., Wang Y., Zhao Y. Marine-Derived Hydrogels for Biomedical Applications. Adv. Funct. Mater. 2023;33:2211323. doi: 10.1002/adfm.202211323. [DOI] [Google Scholar]
- 44.Ahmed E.M. Hydrogel: Preparation, characterization, and applications: A review. J. Adv. Res. 2015;6:105–121. doi: 10.1016/j.jare.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang T. Mechanical and Swelling Properties of Hydrogels. KTH Chemical Science and Engineering, Uppsala University; Stockholm, Sweden: 2012. [Google Scholar]
- 46.Nguyen M.H., Le T.T.N., Nguyen T.A., Le H.N.T., Pham T.T. Biomedical materials for wound dressing: Recent advances and applications. RSC Adv. 2023;13:5509–5528. doi: 10.1039/D2RA07673J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Parent M., Baradari H., Champion E., Damia C., Viana-Trecant M. Design of calcium phosphate ceramics for drug delivery applications in bone diseases: A review of the parameters affecting the loading and release of the therapeutic substance. J. Control. Release. 2017;252:1–17. doi: 10.1016/j.jconrel.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 48.Barbosa A.I., Lima S.A.C., Yousef I., Reis S. Evaluating the Skin Interactions and Permeation of Alginate/Fucoidan Hydrogels Per Se and Associated with Different Essential Oils. Pharmaceutics. 2023;15:190. doi: 10.3390/pharmaceutics15010190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kita K., Dittrich C. Drug delivery vehicles with improved encapsulation efficiency: Taking advantage of specific drug-carrier interactions. Expert Opin. Drug Deliv. 2011;8:329–342. doi: 10.1517/17425247.2011.553216. [DOI] [PubMed] [Google Scholar]
- 50.Günay K.A., Chang T.L., Skillin N.P., Rao V.V., Macdougall L.J., Alicia A.C., Jason S.S., Tobin E.B., Zhang C., Yu C.Y., et al. Photo-expansion microscopy enables super-resolution imaging of cells embedded in 3D hydrogels. Nat. Mater. 2023;22:777–785. doi: 10.1038/s41563-023-01558-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rizzi S.C., Hubbell J.A. Recombinant Protein-co-PEG Networks as Cell-Adhesive and Proteolytically Degradable Hydrogel Matrixes. Part I: Development and Physicochemical Characteristics. Biomacromolecules. 2005;6:1226–1238. doi: 10.1021/bm049614c. [DOI] [PubMed] [Google Scholar]
- 52.Winblade N.D., Nikolic I.D., Hoffman A.S., Hubbell J.A. Blocking Adhesion to Cell and Tissue Surfaces by the Chemisorption of a Poly-l-lysine-graft-(poly(ethylene glycol); phenylboronic acid) Copolymer. Biomacromolecules. 2000;1:523–533. doi: 10.1021/bm000040v. [DOI] [PubMed] [Google Scholar]
- 53.Cai J., Guo J., Wang S. Application of Polymer Hydrogels in the Prevention of Postoperative Adhesion: A Review. Gels. 2023;9:98. doi: 10.3390/gels9020098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Halimeh A., Baradar K.A., Nosratollah Z. A dual synergistic effect of titanium and curcumin co-embedded on extracellular matrix hydrogels of decellularized bone: Potential application in osteoblastic differentiation of adipose-derived mesenchymal stem cells. J. Biomater. Sci. Polym. Ed. 2023;34:372–397. doi: 10.1080/09205063.2022.2123216. [DOI] [PubMed] [Google Scholar]
- 55.Park H., Guo X., Temenoff J.S., Tabata Y., Caplan A.I., Kasper F.K., Mikos A.G. Effect of swelling ratio of injectable hydrogel composites on chondrogenic differentiation of encapsulated rabbit marrow mesenchymal stem cells in vitro. Biomacromolecules. 2009;10:541–546. doi: 10.1021/bm801197m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li H., Hao Z., Zhang S., Li B., Wang Y., Wu X., Hu Y., Chen R., Chen T., Li J. “Smart” Stimuli-responsive Injectable Gels for Bone Tissue Engineering Application. Macromol. Biosci. 2023;23:2200481. doi: 10.1002/mabi.202200481. [DOI] [PubMed] [Google Scholar]
- 57.Jacob S., Nair A.B., Shah J., Sreeharsha N., Gupta S., Shinu P. Emerging role of hydrogels in drug delivery systems, tissue engineering and wound management. Pharmaceutics. 2021;13:357. doi: 10.3390/pharmaceutics13030357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xue X., Hu Y., Wang S., Chen X., Jiang Y., Su J. Fabrication of physical and chemical crosslinked hydrogels for bone tissue engineering. Bioact. Mater. 2022;12:327–339. doi: 10.1016/j.bioactmat.2021.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Anseth K.S., Klok H.A. Click Chemistry in Biomater, Nanomedicine, and Drug Delivery. Biomacromolecules. 2016;17:1–3. doi: 10.1021/acs.biomac.5b01660. [DOI] [PubMed] [Google Scholar]
- 60.Yang Q., Wang K., Nie J., Du B., Tang G. Poly(N-vinylpyrrolidinone) Microgels: Preparation, Biocompatibility, and Potential Application as Drug Carriers. Biomacromolecules. 2014;15:2285–2293. doi: 10.1021/bm5004493. [DOI] [PubMed] [Google Scholar]
- 61.Koehler K.C., Anseth K.S., Bowman C.N., Diels A. Mediated Controlled Release from a Poly(ethylene glycol) Based Hydrogel. Biomacromolecules. 2013;14:538–547. doi: 10.1021/bm301789d. [DOI] [PubMed] [Google Scholar]
- 62.Roth A., Murschel F., Latreille P.L., Martinez V.A., Liberelle B., Banquy X., De Crescenzo G.C.C. Affinity-Based Systems for the Controlled Release of Biofunctionalized Gold Nanoparticles from Alginate Hydrogels. Biomacromolecules. 2019;20:1926–1936. doi: 10.1021/acs.biomac.9b00137. [DOI] [PubMed] [Google Scholar]
- 63.Baranello M.P., Bauer L., Benoit D.S.W. Poly(styrene-alt-maleic anhydride)-Based Diblock Copolymer Micelles Exhibit Versatile Hydrophobic Drug Loading, Drug-Dependent Release, and Internalization by Multidrug Resistant Ovarian Cancer Cells. Biomacromolecules. 2014;15:2629–2641. doi: 10.1021/bm500468d. [DOI] [PubMed] [Google Scholar]
- 64.Nichols D., Pimentel M.B., Borges F.T.P., Hyoju S.K., Teymour F., Hong S.H., Zaborina O.Y., Alverdy J.C., Papavasiliou G. Sustained Release of Phosphates from Hydrogel Nanoparticles Suppresses Bacterial Collagenase and Biofilm Formation In Vitro. Front. Bioeng. Biotechnol. 2019;7:153. doi: 10.3389/fbioe.2019.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yan S., Wu S., Zhang J., Zhang S., Huang Y., Zhu H., Li Y., Qi B. Controlled release of curcumin from gelatin hydrogels by the molecular-weight modulation of an oxidized dextran cross-linker. Food Chem. 2023;418:135966. doi: 10.1016/j.foodchem.2023.135966. [DOI] [PubMed] [Google Scholar]
- 66.Yamamoto M., Tabata Y., Hong L., Miyamoto S., Hashimoto N., Ikada Y. Bone regeneration by transforming growth factor β1 released from a biodegradable hydrogel. J. Control. Release. 2000;64:133–142. doi: 10.1016/S0168-3659(99)00129-7. [DOI] [PubMed] [Google Scholar]
- 67.Chapa-Villarreal F.A., Miller M., Rodriguez-Cruz J.J., Pérez-Carlos D., Peppas N.A. Self-assembled block copolymer Biomater for oral delivery of protein therapeutics. Biomaterials. 2023;300:122191. doi: 10.1016/j.biomaterials.2023.122191. [DOI] [PubMed] [Google Scholar]
- 68.Al Badri Y.N., Chaw C.S., Elkordy A.A. Insights into Asymmetric Liposomes as a Potential Intervention for Drug Delivery Including Pulmonary Nanotherapeutics. Pharmaceutics. 2023;15:294. doi: 10.3390/pharmaceutics15010294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cong Y.Y., Fan B., Zhang Z.Y., Li G.Y. Implantable sustained-release drug delivery systems: A revolution for ocular therapeutics. Int. Ophthalmol. 2023. in press . [DOI] [PubMed]
- 70.Ahmadi S., Fatahi Y., Safarkhani M., Rabiee M., Warkiani M.E., Rabiee N. Electric-Responsive Materials: Properties, Design, and Applications, Stimuli-Responsive Materials for Biomedical Applications. ACS Symp. Ser. Am. Chem. Soc. 2023;1436:31–52. [Google Scholar]
- 71.Scott R.A., Nicholas A.P. Highly crosslinked, PEG-containing copolymers for sustained solute delivery. Biomaterials. 1999;20:1371–1380. doi: 10.1016/S0142-9612(99)00040-X. [DOI] [PubMed] [Google Scholar]
- 72.Rizzi S.C., Ehrbar M., Halstenberg S., Raeber G.P., Schmoekel H.G., Hagenmüller H., Müller R., Weber F.E., Hubbell J.A. Recombinant Protein-co-PEG Networks as Cell-Adhesive and Proteolytically Degradable Hydrogel Matrixes. Part II: Biofunctional Characteristics. Biomacromolecules. 2006;7:3019–3029. doi: 10.1021/bm060504a. [DOI] [PubMed] [Google Scholar]
- 73.Mereness J.A., Piraino L., Chen C.Y., Moyston T., Song Y., Shubin A., DeLouise L.A., Ovitt C.E., Benoit D.S.W. Slow hydrogel matrix degradation enhances salivary gland mimetic phenotype. Acta Biomater. 2023. in press . [DOI] [PMC free article] [PubMed]
- 74.Pan Z., Yang X., Liang Y., Lyu M., Huang Y., Zhou H., Wen G., Yu H., He J. Chromium-containing wastewater reclamation via forward osmosis with sewage sludge ash temperature-sensitive hydrogel as draw agent. J. Water Process. Eng. 2023;51:103422. doi: 10.1016/j.jwpe.2022.103422. [DOI] [Google Scholar]
- 75.Liu Z., Li J., Zhang Z., Liu J., Wu C., Yu Y. Incorporating self-healing capability in temperature-sensitive hydrogels by non-covalent chitosan crosslinkers. Eur. Polym. J. 2023;182:111728. doi: 10.1016/j.eurpolymj.2022.111728. [DOI] [Google Scholar]
- 76.Knipe J.M., Strong L.E., Peppas N.A. Enzyme- and pH-Responsive Microencapsulated Nanogels for Oral Delivery of siRNA to Induce TNF-α Knockdown in the Intestine. Biomacromolecules. 2016;17:788–797. doi: 10.1021/acs.biomac.5b01518. [DOI] [PubMed] [Google Scholar]
- 77.Tian B., Hua S., Liu J. Multi-functional chitosan-based nanoparticles for drug delivery: Recent advanced insight into cancer therapy. Carbohydr. Polym. 2023;315:120972. doi: 10.1016/j.carbpol.2023.120972. [DOI] [PubMed] [Google Scholar]
- 78.Sharpe L.A., Vela R., Julia E., Haddadin O.M., Ross K.A., Narasimhan B., Peppas N.A. pH-Responsive Microencapsulation Systems for the Oral Delivery of Polyanhydride Nanoparticles. Biomacromolecules. 2018;19:793–802. doi: 10.1021/acs.biomac.7b01590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tani Y., Yonenuma R., Mori H. Clusterization-triggered emission of poly(vinyl amine)-based ampholytic block and random copolymers. React. Funct. Polym. 2023;184:105518. doi: 10.1016/j.reactfunctpolym.2023.105518. [DOI] [Google Scholar]
- 80.Rice M.A., Sanchez-Adams J., Kristi S. Exogenously Triggered, Enzymatic Degradation of Photopolymerized Hydrogels with Polycaprolactone Subunits: Experimental Observation and Modeling of Mass Loss Behavior. Biomacromolecules. 2006;7:1968–1975. doi: 10.1021/bm060086+. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Durán-Lobato M., Carrillo-Conde B., Khairandish Y., Peppas N.A. Surface-Modified P(HEMA-co-MAA) Nanogel Carriers for Oral Vaccine Delivery: Design, Characterization, and In Vitro Targeting Evaluation. Biomacromolecules. 2014;15:2725–2734. doi: 10.1021/bm500588x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Paul W., Sharma C.P. Woodhead Publishing Series in Biomaterials, Biointegration of Medical Implant Materials. Woodhead Publishing; Sawston, UK: 2010. 8—Inorganic nanoparticles for targeted drug delivery; pp. 204–235. [Google Scholar]
- 83.Ackun-Farmmer M.A., Overby C.T., Haws B.E., Choe R., Benoit D.S.W. Biomaterials for orthopedic diagnostics and theranostics. Curr. Opin. Biomed. Eng. 2021;19:100308. doi: 10.1016/j.cobme.2021.100308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sharma P., Baisoya D., Chauhan D., Mishra D., Sharma M., Chandra A. Recent Progress, Therapeutic Concepts and Pharmaceutical Challenges of Dendrimer Based Drug Delivery System. J. Pharm. Negat. Results. 2022;13:6865–6873. [Google Scholar]
- 85.Altay Benetti A., Tarbox T., Benetti C. Current Insights into the Formulation and Delivery of Therapeutic and Cosmeceutical Agents for Aging Skin. Cosmetics. 2023;10:54. doi: 10.3390/cosmetics10020054. [DOI] [Google Scholar]
- 86.John G.W. Encyclopedia of Medical Devices and Instrumentation. 2nd ed. Wiley-Interscience; Hoboken, NJ, USA: 2006. [Google Scholar]
- 87.Waresindo W.X., Luthfianti H.R., Priyanto A., Hapidin D.A., Edikresnha D., Aimon A.H., Suciati T., Khairurrijal K. Freeze–thaw hydrogel fabrication method: Basic principles, synthesis parameters, properties, and biomedical applications. Mater. Res. Express. 2023;10:024003. doi: 10.1088/2053-1591/acb98e. [DOI] [Google Scholar]
- 88.Sedighi M., Shrestha N., Mahmoudi Z., Khademi Z., Ghasempour A., Dehghan H., Talebi S.F., Toolabi M., Préat V., Chen B., et al. Multifunctional Self-Assembled Peptide Hydrogels for Biomedical Applications. Polymers. 2023;15:1160. doi: 10.3390/polym15051160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sordi M.B., Fredel M.C., da Cruz A.C.C., Sharpe P.T., de Souza Magini R. Enhanced bone tissue regeneration with hydrogel-based scaffolds by embedding parathyroid hormone in mesoporous bioactive glass. Clin. Oral Investig. 2023;27:125–137. doi: 10.1007/s00784-022-04696-3. [DOI] [PubMed] [Google Scholar]
- 90.Tolstova T., Drozdova M., Popyrina T., Matveeva D., Demina T., Akopova T., Andreeva E., Markvicheva E. Preparation and In Vitro Evaluation of Chitosan-g-Oligolactide Based Films and Macroporous Hydrogels for Tissue Engineering. Polymers. 2023;15:907. doi: 10.3390/polym15040907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wallace S.J., Li J., Nation R.L., Boyd B.J. Drug release from nanomedicines: Selection of appropriate encapsulation and release methodology. Drug Deliv. Transl. Res. 2012;2:284–292. doi: 10.1007/s13346-012-0064-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lin C.C., Anseth K.S. Glucagon-Like Peptide-1 Functionalized PEG Hydrogels Promote Survival and Function of Encapsulated Pancreatic β-Cells. Biomacromolecules. 2009;10:2460–2467. doi: 10.1021/bm900420f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mabry K.M., Lawrence R.L., Anseth K.S. Dynamic stiffening of poly(ethylene glycol)-based hydrogels to direct valvular interstitial cell phenotype in a three-dimensional environment. Biomaterials. 2015;49:47–56. doi: 10.1016/j.biomaterials.2015.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Biswal A., Purohit S.S., Swain S.K. Chitosan based composite scaffolds in skin wound repair: A review. J. Drug Deliv. Sci. Technol. 2023;84:104549. doi: 10.1016/j.jddst.2023.104549. [DOI] [Google Scholar]
- 95.Wei Q., Liu D., Chu G., Yu Q., Liu Z., Li J., Meng Q., Wang W., Han F., Li B. TGF-β1-supplemented decellularized annulus fibrosus matrix hydrogels promote annulus fibrosus repair. Bioact. Mater. 2023;19:581–593. doi: 10.1016/j.bioactmat.2022.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lin F., Li Y., Cui W. Injectable hydrogel microspheres in cartilage repair. Biomed. Technol. 2023;1:18–29. doi: 10.1016/j.bmt.2022.11.002. [DOI] [Google Scholar]
- 97.Wen X., Xi K., Tang Y., Bian J., Qin Y., Xiao W., Pan T., Cheng X., Ge Z., Cui W. Immunized Microspheres Engineered Hydrogel Membrane for Reprogramming Macrophage and Mucosal Repair. Small. 2023;19:2207030. doi: 10.1002/smll.202207030. [DOI] [PubMed] [Google Scholar]
- 98.Cerritelli S., Velluto D., Hubbell J.A. PEG-SS-PPS: Reduction-Sensitive Disulfide Block Copolymer Vesicles for Intracellular Drug Delivery. Biomacromolecules. 2007;8:1966–1972. doi: 10.1021/bm070085x. [DOI] [PubMed] [Google Scholar]
- 99.Jiang Y., Lyu Z., Ralahy B., Liu J., Roussel T., Ding L., Tang J., Kosta A., Giorgio S., Tomasini R., et al. Dendrimer nanosystems for adaptive tumor-assisted drug delivery via extracellular vesicle hijacking. Proc. Natl. Acad. Sci. USA. 2023;120:e2215308120. doi: 10.1073/pnas.2215308120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cui P., Pan P., Qin L., Wang X., Chen X., Deng Y., Zhang X. Nanoengineered hydrogels as 3D biomimetic extracellular matrix with injectable and sustained delivery capability for cartilage regeneration. Bioact. Mater. 2023;19:487–498. doi: 10.1016/j.bioactmat.2022.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Xu J., Li Y., Yang J., Zhou S., Situ W. Plasma etching effect on the molecular structure of chitosan-based hydrogels and its biological properties. Int. J. Biol. Macromol. 2023;230:123257. doi: 10.1016/j.ijbiomac.2023.123257. [DOI] [PubMed] [Google Scholar]
- 102.Norahan M.H., Pedroza-González S.C., Sánchez-Salazar M.G., Álvarez M.M., de Santiago G.T. Structural and biological engineering of 3D hydrogels for wound healing. Bioact. Mater. 2023;24:197–235. doi: 10.1016/j.bioactmat.2022.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Williams T.J., Jeevarathinam A.S., Jivan F., Baldock V., Kim P., McShane M.J., Alge D.L. Glucose biosensors based on Michael addition crosslinked poly(ethylene glycol) hydrogels with chemo-optical sensing microdomains. J. Mater. Chem. B. 2023;11:1749–1759. doi: 10.1039/D2TB02339C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nel J., Elkhoury K., Velot E., Bianchi A., Acherar S., Francius G., Tamayol A., Grandemange S., Arab-Tehrany E. Functionalized liposomes for targeted breast cancer drug delivery. Bioact. Mater. 2023;24:401–437. doi: 10.1016/j.bioactmat.2022.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhang H., Wu S., Chen W., Hu Y., Geng Z., Su J. Bone/cartilage targeted hydrogel: Strategies and applications. Bioact. Mater. 2023;23:156–169. doi: 10.1016/j.bioactmat.2022.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Aubry G., Lee H.J., Lu H. Applications in Diagnostics and Therapeutics. Anal. Chem. 2023;95:444–467. doi: 10.1021/acs.analchem.2c04562. [DOI] [PubMed] [Google Scholar]
- 107.Park J., Lee S., Lee M., Kim H.-S., Lee J.Y. Injectable Conductive Hydrogels with Tunable Degradability as Novel Implantable Bioelectrodes. Small. 2023;19:2300250. doi: 10.1002/smll.202300250. [DOI] [PubMed] [Google Scholar]
- 108.del Olmo J.A., Pérez-Álvarez L., Martínez V.S., Cid S.B., Ruiz-Rubio L., González R.P., Vilas-Vilela J.L., Alonso J.M. Multifunctional antibacterial chitosan-based hydrogel coatings on Ti6Al4V biomaterial for biomedical implant applications. Int. J. Biol. Macromol. 2023;231:123328. doi: 10.1016/j.ijbiomac.2023.123328. [DOI] [PubMed] [Google Scholar]
- 109.Bellotti D., D’Accolti M., Pula W., Huang N., Simeliere F., Caselli E., Esposito E., Remelli M. Calcitermin-Loaded Smart Gels Activity against Candida albicans: A Preliminary In Vitro Study. Gels. 2023;9:165. doi: 10.3390/gels9020165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Qi X., Yuan Y., Zhang J., Bulte J.W.M., Dong W. Oral Administration of Salecan-Based Hydrogels for Controlled Insulin Delivery. J. Agric. Food Chem. 2018;66:10479–10489. doi: 10.1021/acs.jafc.8b02879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hussain M., Rehan T., Ul-Islam M., Shehzad O., Khan A., Ullah M.W., Baig A., Yang G., Shah N. Poly(2-acrylamido-2-methylpropane sulfonic acid)@butyl methacrylate latex anchored into polyethylene glycol diacrylate-based hydrogel composite for drug loading and controlled release studies. Adv. Compos. Hybrid. Mater. 2023;6:58. doi: 10.1007/s42114-022-00600-5. [DOI] [Google Scholar]
- 112.Reza Rezaie H., Esnaashary M., Aref arjmand A., Öchsner A. A Review of Biomaterials and Their Applications in Drug Delivery. Springer; Singapore: 2018. Classification of Drug Delivery Systems; pp. 9–25. [Google Scholar]
- 113.Jose J., Athira V.P., Michel H., Hafeela A.R., Bhat S.G., Thomas S., Maria L.P. Chapter 1—Hydrogels: An overview of the history, classification, principles, applications, and kinetics. In: Thomas S., Sharma B., Jain P., Shekhar S., editors. Sustainable Hydrogels. Elsevier; Amsterdam, The Netherlands: 2023. pp. 1–22. [Google Scholar]
- 114.Akram M.U., Abbas N., Farman M., Manzoor S., Khan M.I., Osman S.M., Luque R., Shanableh A. Tumor micro-environment sensitive release of doxorubicin through chitosan based polymeric nanoparticles: An in-vitro study. Chemosphere. 2023;313:137332. doi: 10.1016/j.chemosphere.2022.137332. [DOI] [PubMed] [Google Scholar]
- 115.Nam S.H., Park J., Koo H. Recent advances in selective and targeted drug/gene delivery systems using cell-penetrating peptides. Arch. Pharm. Res. 2023;46:18–34. doi: 10.1007/s12272-022-01425-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Scott E.A., Stano A., Gillard M., Maio-Liu A.C., Swartz M.A., Hubbell J.A. Dendritic cell activation and T cell priming with adjuvant- and antigen-loaded oxidation-sensitive polymersomes. Biomaterials. 2012;33:6211–6219. doi: 10.1016/j.biomaterials.2012.04.060. [DOI] [PubMed] [Google Scholar]
- 117.Richbourg N.R., Peppas N.A. Solute diffusion and partitioning in multi-arm poly(ethylene glycol) hydrogels. J. Mater. Chem. B. 2023;11:377–388. doi: 10.1039/D2TB02004A. [DOI] [PubMed] [Google Scholar]
- 118.Zhang K., Han Q., Feng L., Zhang L. A novel Solution-Diffusion-Flory-Rehner model to predict flux behavior during forward osmosis with thermo-responsive hydrogel as draw agent. J. Membr. Sci. 2023;675:121553. doi: 10.1016/j.memsci.2023.121553. [DOI] [Google Scholar]
- 119.Wang L., Gang X., Xiao X., Ren Y., Wang J., Niu B., Li W. Sodium Alginate/carboxymethyl chitosan-CuO hydrogel beads as a pH-sensitive carrier for the controlled release of curcumin. Eur. Polym. J. 2023;192:112069. doi: 10.1016/j.eurpolymj.2023.112069. [DOI] [Google Scholar]
- 120.Zhu C., Zhang X., Gan J., Geng D., Bian X., Cheng Y., Tang N. A pH-sensitive hydrogel based on carboxymethylated konjac glucomannan crosslinked by sodium trimetaphosphate: Synthesis, characterization, swelling behavior and controlled drug release. Int. J. Biol. Macromol. 2023;232:123392. doi: 10.1016/j.ijbiomac.2023.123392. [DOI] [PubMed] [Google Scholar]
- 121.Wei X., Xue Y., Sun Y., Chen L., Zhang C., Wu Q., Peng S., Ma C., Liu Z., Jiang S., et al. A robust anisotropic light-responsive hydrogel for ultrafast and complex biomimetic actuation via poly(pyrrole)-coated electrospun nanofiber. Chem. Eng. J. 2023;452:139373. doi: 10.1016/j.cej.2022.139373. [DOI] [Google Scholar]
- 122.Li D., Qian X., Huang R., Li C. Preparation of PNIPAM-Azo by RAFT polymerization and their application in thermo- and light-responsive hydrogel. J. Polym. Res. 2023;30:155. doi: 10.1007/s10965-023-03541-9. [DOI] [Google Scholar]
- 123.Kolahdoozan M., Rahimi T., Taghizadeh A., Aghaei H. Preparation of new hydrogels by visible light cross-linking of dextran methacrylate and poly(ethylene glycol)-maleic acid copolymer. Int. J. Biol. Macromol. 2023;227:1221–1233. doi: 10.1016/j.ijbiomac.2022.11.309. [DOI] [PubMed] [Google Scholar]
- 124.Veisi H., Varshosaz J., Rostami M., Mirian M. Thermosensitive TMPO-oxidized lignocellulose/cationic agarose hydrogel loaded with deferasirox nanoparticles for photothermal therapy in melanoma. Int. J. Biol. Macromol. 2023;238:124126. doi: 10.1016/j.ijbiomac.2023.124126. [DOI] [PubMed] [Google Scholar]
- 125.Kobayashi D., Uchida H., Ishibane M., Kurita E., Kirihara M., Kotsuchibashi Y. Fabrication of thermally cross-linked poly(methacrylic acid)-based sponges with nanolayered structures and their degradation. Polym. J. 2023;55:163–170. doi: 10.1038/s41428-022-00721-0. [DOI] [Google Scholar]
- 126.Zhou C., Wang C., Xu K., Niu Z., Zou S., Zhang D., Qian Z., Liao J., Xie J. Hydrogel platform with tunable stiffness based on magnetic nanoparticles cross-linked GelMA for cartilage regeneration and its intrinsic biomechanism. Bioact. Mater. 2023;25:615–628. doi: 10.1016/j.bioactmat.2022.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shrivastava P., Vishwakarma N., Gautam L., Vyas S.P. Chapter 5—Magnetically responsive polymeric gels and elastomeric system(s) for drug delivery. In: Vyas S.P., Agrawal U., Sharma R., editors. Smart Polymeric Nano-Constructs in Drug Delivery. Academic Press; Cambridge, MA, USA: 2023. pp. 129–150. [Google Scholar]
- 128.Ganguly S., Margel S. 3D printed magnetic polymer composite hydrogels for hyperthermia and magnetic field driven structural manipulation. Prog. Polym. Sci. 2022;131:101574. doi: 10.1016/j.progpolymsci.2022.101574. [DOI] [Google Scholar]
- 129.Liu J., Chai J., Yuan Y., Zhang T., Saini R.K., Yang M., Shang X. Dextran sulfate facilitates egg white protein to form transparent hydrogel at neutral pH: Structural, functional, and degradation properties. Food Hydrocoll. 2022;122:107094. doi: 10.1016/j.foodhyd.2021.107094. [DOI] [Google Scholar]
- 130.Hocine S., Ghemati D., Aliouche D. Synthesis, characterization and swelling behavior of pH-sensitive polyvinylalcohol grafted poly(acrylic acid-co-2-acrylamido-2-methylpropane sulfonic acid) hydrogels for protein delivery. Polym. Bull. 2023. in press .
- 131.Yu Y., Feng R., Yu S., Li J., Wang Y., Song Y., Yang X., Pan W., Li S. Nanostructured lipid carrier-based pH and temperature dual-responsive hydrogel composed of carboxymethyl chitosan and poloxamer for drug delivery. Int. J. Biol. Macromol. 2018;114:462–469. doi: 10.1016/j.ijbiomac.2018.03.117. [DOI] [PubMed] [Google Scholar]
- 132.Chen N., Chang B., Shi N., Yan W., Lu F., Liu F. Cross-linked enzyme aggregates immobilization: Preparation, characterization, and applications. Crit. Rev. Biotechnol. 2023;43:369–383. doi: 10.1080/07388551.2022.2038073. [DOI] [PubMed] [Google Scholar]
- 133.Dalei G., Das S., Jena S.R., Jena D., Nayak J., Samanta L. In situ crosslinked dialdehyde guar gum-chitosan Schiff-base hydrogels for dual drug release in colorectal cancer therapy. Chem. Eng. Sci. 2023;269:118482. doi: 10.1016/j.ces.2023.118482. [DOI] [Google Scholar]
- 134.Zhu W., Zhao Y., Wu Z., Lv F., Zhang Y., Guo S. Application of UV responsive SiO2/PVP composite hydrogels as intelligent controlled drug release patches. Polymer. 2023;264:125535. doi: 10.1016/j.polymer.2022.125535. [DOI] [Google Scholar]
- 135.Li Y., Yang D., Wu Z., Gao F.-L., Gao X.-Z., Zhao H.-Y., Li X., Yu Z.-Z. Self-adhesive, self-healing, biocompatible and conductive polyacrylamide nanocomposite hydrogels for reliable strain and pressure sensors. Nano Energy. 2023;109:108324. doi: 10.1016/j.nanoen.2023.108324. [DOI] [Google Scholar]
- 136.Li Y., Yao M., Luo Y., Li J., Wang Z., Liang C., Qin C., Huang C., Yao S. Polydopamine-Reinforced Hemicellulose-Based Multifunctional Flexible Hydrogels for Human Movement Sensing and Self-Powered Transdermal Drug Delivery. ACS Appl. Mater. Interfaces. 2023;15:5883–5896. doi: 10.1021/acsami.2c19949. [DOI] [PubMed] [Google Scholar]
- 137.Nelson B.R., Kirkpatrick B.E., Miksch C.E., Davidson M.D., Skillin N.P., Hach G.K., Khang A., Hummel S.N., Fairbanks B.D., Burdick J.A., et al. Photoinduced Dithiolane Crosslinking for Multiresponsive Dynamic Hydrogels. Adv. Mater. 2023. p. 2211209. in press . [DOI] [PMC free article] [PubMed]
- 138.Gennaro A.R. Remington: The Science and Practice of Pharmacy. Lippincott Williams & Wilkins; Baltimore, MD, USA: 2000. [Google Scholar]
- 139.Mamidi N., González-Ortiz A., Romo I.L., Barrera E.V. Development of Functionalized Carbon Nano-Onions Reinforced Zein Protein Hydrogel Interfaces for Controlled Drug Release. Pharmaceutics. 2019;11:621. doi: 10.3390/pharmaceutics11120621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Pang H., Huang J., Li X., Yi K., Li S., Liu Z., Zhang W., Zhang C., Liu S., Gu Y. Enhancing quorum quenching media with 3D robust electrospinning coating: A novel biofouling control strategy for membrane bioreactors. Water Res. 2023;234:119830. doi: 10.1016/j.watres.2023.119830. [DOI] [PubMed] [Google Scholar]
- 141.Basu S., Pacelli S., Paul A. Self-healing DNA-based injectable hydrogels with reversible covalent linkages for controlled drug delivery. Acta Biomater. 2020;105:159–169. doi: 10.1016/j.actbio.2020.01.021. [DOI] [PubMed] [Google Scholar]
- 142.Reza Rezaie H., Esnaashary M., Aref arjmand A., Öchsner A. A Review of Biomaterials and Their Applications in Drug Delivery. Springer; Singapore: 2018. The History of Drug Delivery Systems; pp. 1–8. [Google Scholar]
- 143.Vashist A., Vashist A., Gupta Y.K., Ahmad S. Recent advances in hydrogel based drug delivery systems for the human body. J. Mater. Chem. B. 2014;2:147–166. doi: 10.1039/C3TB21016B. [DOI] [PubMed] [Google Scholar]
- 144.Anselmo A.C., Mitragotri S. An overview of clinical and commercial impact of drug delivery systems. J. Control. Release. 2014;190:15–28. doi: 10.1016/j.jconrel.2014.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Karaz S., Senses E. Liposomes Under Shear: Structure, Dynamics, and Drug Delivery Applications. Adv. NanoBiomed Res. 2023;3:2200101. doi: 10.1002/anbr.202200101. [DOI] [Google Scholar]
- 146.Kotta S., Aldawsari H.M., Badr-Eldin S.M., Nair A.B., Yt K. Progress in Polymeric Micelles for Drug Delivery Applications. Pharmaceutics. 2022;14:1636. doi: 10.3390/pharmaceutics14081636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ghezzi M., Pescina S., Padula C., Santi P., Del Favero E., Cantù L., Nicoli S. Polymeric micelles in drug delivery: An insight of the techniques for their characterization and assessment in biorelevant conditions. J. Control. Release. 2021;332:312–336. doi: 10.1016/j.jconrel.2021.02.031. [DOI] [PubMed] [Google Scholar]
- 148.Kim K.K., Pack D.W. BioMEMS and Biomedical Nanotechnology. Springer; Boston, MA, USA: 2006. Microspheres for Drug Delivery; pp. 19–50. [Google Scholar]
- 149.Zhang Q., Kuang G., Zhang L., Zhu Y. Nanocarriers for platinum drug delivery. Biomed. Technol. 2023;2:77–89. doi: 10.1016/j.bmt.2022.11.011. [DOI] [Google Scholar]
- 150.Ghosn Y., Kamareddine M.H., Tawk A., Elia C., El Mahmoud A., Terro K., El Harake N., El-Baba B., Makdessi J., Farhat S. Inorganic Nanoparticles as Drug Delivery Systems and Their Potential Role in the Treatment of Chronic Myelogenous Leukaemia. Technol. Cancer Res. Treat. 2019;18:1533033819853241. doi: 10.1177/1533033819853241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Liu S., Wang Z., Chen X., Han M., Xu J., Li T., Yu L., Qin M., Long M., Li M., et al. Multiscale Anisotropic Scaffold Integrating 3D Printing and Electrospinning Techniques as a Heart-on-a-Chip Platform for Evaluating Drug-Induced Cardiotoxicity. Adv. Healthcare Mater. 2023. p. 2300719. in press . [DOI] [PubMed]
- 152.Koochaki A., Shahgholi M., Sajadi S.M., Babadi E., Inc M. Investigation of the mechanical stability of polyethylene glycol hydrogel reinforced with cellulose nanofibrils for wound healing: Molecular dynamics simulation. Eng. Anal. Bound. Elem. 2023;151:1–7. doi: 10.1016/j.enganabound.2023.02.055. [DOI] [Google Scholar]
- 153.Zhang R., Zhang Y., Yu J., Gao Y., Mao L. Enhanced freeze-thawing stability of water-in-oil Pickering emulsions stabilized by ethylcellulose nanoparticles and oleogels. Carbohydr. Polym. 2023;312:120814. doi: 10.1016/j.carbpol.2023.120814. [DOI] [PubMed] [Google Scholar]
- 154.Başyiğit B., Altun G., Yücetepe M., Karaaslan A., Karaaslan M. Locust bean gum provides excellent mechanical and release attributes to soy protein-based natural hydrogels. Int. J. Biol. Macromol. 2023;231:123352. doi: 10.1016/j.ijbiomac.2023.123352. [DOI] [PubMed] [Google Scholar]
- 155.Chiani E., Beaucamp A., Hamzeh Y., Azadfallah M., Thanusha A.V., Collins M.N. Synthesis and characterization of gelatin/lignin hydrogels as quick release drug carriers for Ribavirin. Int. J. Biol. Macromol. 2023;224:1196–1205. doi: 10.1016/j.ijbiomac.2022.10.205. [DOI] [PubMed] [Google Scholar]
- 156.Patterson J., Hubbell J.A. Enhanced proteolytic degradation of molecularly engineered PEG hydrogels in response to MMP-1 and MMP-2. Biomaterials. 2010;31:7836–7845. doi: 10.1016/j.biomaterials.2010.06.061. [DOI] [PubMed] [Google Scholar]
- 157.Metters A., Hubbell J. Network Formation and Degradation Behavior of Hydrogels Formed by Michael-Type Addition Reactions. Biomacromolecules. 2005;6:290–301. doi: 10.1021/bm049607o. [DOI] [PubMed] [Google Scholar]
- 158.Mawazi S.M., Al-Mahmood S.M.A., Chatterjee B., Hadi H.A., Doolaanea A.A. Carbamazepine Gel Formulation as a Sustained Release Epilepsy Medication for Pediatric Use. Pharmaceutics. 2019;11:488. doi: 10.3390/pharmaceutics11100488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Boury F., Marchais H., Benoit J.P., Proust J.E. Surface characterization of poly(α-hydroxy acid) microspheres prepared by a solvent evaporation/ extraction process. Biomaterials. 1997;18:125–136. doi: 10.1016/S0142-9612(96)00102-0. [DOI] [PubMed] [Google Scholar]
- 160.Rastogi V., Shukla S., Singh R., Lal N., Yadav P. Microspheres: A promising drug carrier. J. Drug. Deliv. Ther. 2016;6:18–26. doi: 10.22270/jddt.v6i3.1196. [DOI] [Google Scholar]
- 161.Ingle T.G., Pande S.D., Sawarkar R., Padole D. The Current Trends in Microspheres: A Review. J. Drug. Deliv. Ther. 2023;13:183–194. doi: 10.22270/jddt.v13i1.5915. [DOI] [Google Scholar]
- 162.Vadlamudi S., Nichols D., Papavasiliou G., Teymour F. Phosphate-Loaded Hydrogel Nanoparticles for Sepsis Prevention Prepared via Inverse Miniemulsion Polymerization. Macromol. React. Eng. 2018;13:1800066. doi: 10.1002/mren.201800066. [DOI] [Google Scholar]
- 163.Khairan K., Hasan M., Idroes R., Diah M. Fabrication and Evaluation of Polyvinyl Alcohol/Corn Starch/Patchouli Oil Hydrogel Films Loaded with Silver Nanoparticles Biosynthesized in Pogostemon cablin Benth Leaves’ Extract. Molecules. 2023;28:2020. doi: 10.3390/molecules28052020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Pérez-Carrión M.D., Posadas I. Dendrimers in Neurodegenerative Diseases. Processes. 2023;11:319. doi: 10.3390/pr11020319. [DOI] [Google Scholar]
- 165.Ghosh T.K., Rojanasakul Y., Jasti B.R., Singh J., Svensson C.K., Hughes J., Jambhekar S.S., Li X., Bashaw E.D., De Villiers M.M., et al. Theory and Practice of Contemporary Pharmaceutics. CRC Press; Boca Raton, FL, USA: 2004. [Google Scholar]
- 166.Rapalli V.K., Tomar Y., Sharma S., Roy A., Singhvi G. Apremilast loaded lyotropic liquid crystalline nanoparticles embedded hydrogel for improved permeation and skin retention: An effective approach for psoriasis treatment. Biomed. Pharmacother. 2023;162:114634. doi: 10.1016/j.biopha.2023.114634. [DOI] [PubMed] [Google Scholar]
- 167.Cardia M.C., Carta A.R., Caboni P., Maccioni A.M., Erbì S., Boi L., Meloni M.C., Lai F., Sinico C. Trimethyl Chitosan Hydrogel Nanoparticles for Progesterone Delivery in Neurodegenerative Disorders. Pharmaceutics. 2019;11:657. doi: 10.3390/pharmaceutics11120657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Fabiano A., Piras A.M., Guazzelli L., Storti B., Bizzarri R., Zambito Y. Impact of Different Mucoadhesive Polymeric Nanoparticles Loaded in Thermosensitive Hydrogels on Transcorneal Administration of 5-Fluorouracil. Pharmaceutics. 2019;11:623. doi: 10.3390/pharmaceutics11120623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sievers J., Sperlich K., Stahnke T., Kreiner C., Eickner T., Martin H., Guthoff R.F., Schünemann M., Bohn S., Stachs O. Determination of hydrogel swelling factors by two established and a novel non-contact continuous method. J. Appl. Polym. Sci. 2021;138:e50326. doi: 10.1002/app.50326. [DOI] [Google Scholar]
- 170.Blanco A., González G., Casanova E., Pirela M., Briceño A. Mathematical Modeling of Hydrogels Swelling Based on the Finite Element Method. Appl. Math. 2013;4:161–170. doi: 10.4236/am.2013.48A022. [DOI] [Google Scholar]
- 171.Jozaghkar M.R., Sepehrian Azar A., Ziaee F. Preparation, Characterization, and swelling study of N,N′-dimethylacrylamide/acrylic acid amphiphilic hydrogels in different conditions. Polym. Bull. 2022;79:5183–5195. doi: 10.1007/s00289-021-03760-4. [DOI] [Google Scholar]
- 172.Burdick J.A., Lovestead T.M., Anseth K.S., Kinetic C. Lengths in Highly Cross-Linked Networks Formed by the Photoinitiated Polymerization of Divinyl Monomers: A Gel Permeation Chromatography Investigation. Biomacromolecules. 2003;4:149–156. doi: 10.1021/bm025677o. [DOI] [PubMed] [Google Scholar]
- 173.Gadziński P., Froelich A., Jadach B., Wojtyłko M., Tatarek A., Białek A., Krysztofiak J., Gackowski M., Otto F., Osmałek T. Ionotropic Gelation and Chemical Crosslinking as Methods for Fabrication of Modified-Release Gellan Gum-Based Drug Delivery Systems. Pharmaceutics. 2023;15:108. doi: 10.3390/pharmaceutics15010108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wang M., Yin Z., Sun W., Zhong Q., Zhang Y., Zeng M. Microalgae play a structuring role in food: Effect of spirulina platensis on the rheological, gelling characteristics, and mechanical properties of soy protein isolate hydrogel. Food Hydrocoll. 2023;136:108244. doi: 10.1016/j.foodhyd.2022.108244. [DOI] [Google Scholar]
- 175.Polizzotti B.D., Fairbanks B.D., Anseth K.S. Three-Dimensional Biochemical Patterning of Click-Based Composite Hydrogels via Thiolene Photopolymerization. Biomacromolecules. 2008;9:1084–1087. doi: 10.1021/bm7012636. [DOI] [PubMed] [Google Scholar]
- 176.Heidari B.S., Ruan R., Vahabli E., Chen P., De-Juan-Pardo E.M., Zheng M., Doyle B. Natural, synthetic and commercially-available biopolymers used to regenerate tendons and ligaments. Bioact. Mater. 2023;19:179–197. doi: 10.1016/j.bioactmat.2022.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Islam M.R., Rahman M.M., Dhar P.S., Nowrin F.T., Sultana N., Akter M., Rauf A., Khalil A.A., Gianoncelli A., Ribaudo G. The Role of Natural and Semi-Synthetic Compounds in Ovarian Cancer: Updates on Mechanisms of Action, Current Trends and Perspectives. Molecules. 2023;28:2070. doi: 10.3390/molecules28052070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Bercea M., Plugariu I.-A., Gradinaru L.M., Avadanei M., Doroftei F., Gradinaru V.R. Hybrid Hydrogels for Neomycin Delivery: Synergistic Effects of Natural/Synthetic Polymers and Proteins. Polymers. 2023;15:630. doi: 10.3390/polym15030630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li T., Wei H., Zhang Y., Wan T., Cui D., Zhao S., Zhang T., Ji Y., Algadi H., Guo Z., et al. Sodium alginate reinforced polyacrylamide/xanthan gum double network ionic hydrogels for stress sensing and self-powered wearable device applications. Carbohydr. Polym. 2023;309:120678. doi: 10.1016/j.carbpol.2023.120678. [DOI] [PubMed] [Google Scholar]
- 180.Wu Z., Han Y., Zan F., Ye Y., Ren Y., Han K., Liu D., Jiang W. Highly efficient removal of phosphate by La–diatomite and sodium alginate composite hydrogel beads. Environ. Sci. Water Res. Technol. 2023;9:1205–1215. doi: 10.1039/D2EW00864E. [DOI] [Google Scholar]
- 181.Do N.H.N., Pham T.H., Le P.K., Ha A.C. Thermo-responsive Chitosan/β-glycerophosphate hydrogels directly post-loading anti-inflammatory diclofenac sodium. J. Sol Gel Sci. Technol. 2023;105:451–460. doi: 10.1007/s10971-022-06020-7. [DOI] [Google Scholar]
- 182.Zheng Y., Wang X., Zhang C., Zong L. Synthesis, characterization, and swelling behaviors of chitosan-g-poly (acrylic acid-co-acrylamide) superabsorbent using tetraallylammonium bromine as crosslinker. Polym. Bull. 2023;80:4443–4458. doi: 10.1007/s00289-022-04289-w. [DOI] [Google Scholar]
- 183.Heidarian P., Kouzani A.Z. A self-healing nanocomposite double network bacterial nanocellulose/gelatin hydrogel for three dimensional printing. Carbohydr. Polym. 2023;313:120879. doi: 10.1016/j.carbpol.2023.120879. [DOI] [PubMed] [Google Scholar]
- 184.Hipwood L., Clegg J., Weekes A., Davern J.W., Dargaville T.R., Meinert C., Bock N. Semi-Synthetic Click-Gelatin Hydrogels as Tunable Platforms for 3D Cancer Cell Culture. Gels. 2022;8:821. doi: 10.3390/gels8120821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Turturro M.V., Christenson M.C., Larson J.C., Young D.A., Eric M.B., Georgia P. MMP-Sensitive PEG Diacrylate Hydrogels with Spatial Variations in Matrix Properties Stimulate Directional Vascular Sprout Formation. PLoS ONE. 2013;8:e58897. doi: 10.1371/journal.pone.0058897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Turturro M.V., Papavasiliou G. Generation of Mechanical and Biofunctional Gradients in PEG Diacrylate Hydrogels by Perfusion-Based Frontal Photopolymerization. J. Biomater. Sci. Polym. Ed. 2012;23:917–939. doi: 10.1163/092050611X566450. [DOI] [PubMed] [Google Scholar]
- 187.Barbero C.A. Functional Materials Made by Combining Hydrogels (Cross-Linked Polyacrylamides) and Conducting Polymers (Polyanilines)—A Critical Review. Polymers. 2023;15:2240. doi: 10.3390/polym15102240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bhusari S., Kim J., Polizzi K., Sankaran S., del Campo A. Encapsulation of bacteria in bilayer Pluronic thin film hydrogels: A safe format for engineered living materials. Biomater. Adv. 2023;145:213240. doi: 10.1016/j.bioadv.2022.213240. [DOI] [PubMed] [Google Scholar]
- 189.Roudsari F.P., Mehrnia M.R., Honarparvaran A., Kaghazian H. Facile Capture of Recombinant Human Erythropoietin on Mesoporous Affinity Hydrogel Matrix Functionalized with Azoboronate. Appl. Biochem. Biotechnol. 2023;195:3456–3476. doi: 10.1007/s12010-022-04303-x. [DOI] [PubMed] [Google Scholar]
- 190.Anseth K.S., Bowman C.N., Brannon-Peppas L. Mechanical properties of hydrogels and their experimental determination. Biomaterials. 1996;17:1647–1657. doi: 10.1016/0142-9612(96)87644-7. [DOI] [PubMed] [Google Scholar]
- 191.Wang T., Qin Y., Cui C., Ji N., Dai L., Wang Y., Xiong L., Shi R., Sun Q. The effects of pH and iron ions on the mechanical properties of pea starch hydrogels. Int. J. Biol. Macromol. 2023;224:1228–1235. doi: 10.1016/j.ijbiomac.2022.10.208. [DOI] [PubMed] [Google Scholar]
- 192.Liu X., Zhang L., El Fil B., Díaz-Marín C.D., Zhong Y., Li X., Lin S., Wang E.N. Unusual Temperature Dependence of Water Sorption in Semicrystalline Hydrogels. Adv. Mater. 2023;35:2211763. doi: 10.1002/adma.202211763. [DOI] [PubMed] [Google Scholar]
- 193.Saraydın D., Işıkver Y. Calculations of the magnitude of responsivities in pH-, temperature- and ion- responsive hydrogels. Mater. Today Commun. 2022;31:103253. doi: 10.1016/j.mtcomm.2022.103253. [DOI] [Google Scholar]
- 194.Ahn J., Choi M. The pH-induced physical properties of ionic contact lens material. Heliyon. 2023;9:e12996. doi: 10.1016/j.heliyon.2023.e12996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Li J., Song W., Li F. Polymeric DNA Hydrogels and Their Applications in Drug Delivery for Cancer Therapy. Gels. 2023;9:239. doi: 10.3390/gels9030239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Ooi S.Y., Ahmad I., Amin M.C.I.M. Cellulose nanocrystals extracted from rice husks as a reinforcing material in gelatin hydrogels for use in controlled drug delivery systems. Ind. Crops Prod. 2016;93:227–234. doi: 10.1016/j.indcrop.2015.11.082. [DOI] [Google Scholar]
- 197.Dutta S., Gupta R.S., Pathan S., Bose S. Interpenetrating polymer networks for desalination and water remediation: A comprehensive review of research trends and prospects. RSC Adv. 2023;13:6087–6107. doi: 10.1039/D2RA07843K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Fraser D., Nguyen M.T., Benoit D.S. Matrix Control of Periodontal Ligament Cell Activity Via Synthetic Hydrogel Scaffolds. Tissue Eng. A. 2021;27:733–747. doi: 10.1089/ten.tea.2020.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Sokic S., Christenson M.C., Larson J.C., Appel A.A., Brey E.M., Papavasiliou G. Evaluation of MMP substrate concentration and specificity for neovascularization of hydrogel scaffolds. Biomater. Sci. 2014;2:1343–1354. doi: 10.1039/C4BM00088A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.McKinnon D.D., Brown T.E., Kyburz K.A., Kiyotake E.A., Kristi S. Design and Characterization of a Synthetically Accessible, Photodegradable Hydrogel for User-Directed Formation of Neural Networks. Biomacromolecules. 2014;15:2808–2816. doi: 10.1021/bm500731b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Aimetti A.A., Tibbitt M.W., Anseth K.S. Human Neutrophil Elastase Responsive Delivery from Poly(ethylene glycol) Hydrogels. Biomacromolecules. 2009;10:1484–1489. doi: 10.1021/bm9000926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Widener A.E., Roberts A., Phelps E.A. Single versus dual microgel species for forming guest-host microporous annealed particle PEG-MAL hydrogel. J. Biomed. Mater. Res. 2023. pp. 1–11. in press . [DOI] [PMC free article] [PubMed]
- 203.Yi Y., Chiao M., Mahmoud K.A., Wu L., Wang B. Preparation and characterization of PVA/PVP conductive hydrogels formed by freeze–thaw processes as a promising material for sensor applications. J. Mater. Sci. 2022;57:8029–8038. doi: 10.1007/s10853-022-07179-8. [DOI] [Google Scholar]
- 204.Zhong G., Qiu M., Zhang J., Jiang F., Yue X., Huang C., Zhao S., Zeng R., Zhang C., Qu Y. Fabrication and characterization of PVA@PLA electrospinning nanofibers embedded with Bletilla striata polysaccharide and Rosmarinic acid to promote wound healing. Int. J. Biol. Macromol. 2023;234:123693. doi: 10.1016/j.ijbiomac.2023.123693. [DOI] [PubMed] [Google Scholar]
- 205.Lutolf M.P., Hubbell J.A. Synthesis and Physicochemical Characterization of End-Linked Poly(ethylene glycol)-co-peptide Hydrogels Formed by Michael-Type Addition. Biomacromolecules. 2003;4:713–722. doi: 10.1021/bm025744e. [DOI] [PubMed] [Google Scholar]
- 206.Gu J., Clegg J.R., Heersema L.A., Peppas N.A., Smyth H.D.C. Optimization of Cationic Nanogel PEGylation to Achieve Mammalian Cytocompatibility with Limited Loss of Gram-Negative Bactericidal Activity. Biomacromolecules. 2020;21:1528–1538. doi: 10.1021/acs.biomac.0c00081. [DOI] [PubMed] [Google Scholar]
- 207.Rosales A.M., Mabry K.M., Nehls E.M., Anseth K.S. Photoresponsive Elastic Properties of Azobenzene-Containing Poly(ethylene-glycol)-Based Hydrogels. Biomacromolecules. 2015;16:798–806. doi: 10.1021/bm501710e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Sridhar B.V., Anseth K.S. Stress Relaxation and Composition of Hydrazone-Crosslinked Hybrid Biopolymer-Synthetic Hydrogels Determine Spreading and Secretory Properties of MSCs. Adv. Healthc. Mater. 2022;11:2270082. doi: 10.1002/adhm.202200393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Hu N., Shi L., Ji S., Wang W., Lei L., Fan H., Müller-Buschbaum P., Zhong Q. Adhesive Hybrid Interpenetrating Network Hydrogel-Based Detector to Monitor Solar Radiation Dose Required for Plant Growth. Adv. Eng. Mater. 2023;25:2201118. doi: 10.1002/adem.202201118. [DOI] [Google Scholar]
- 210.Ju Y.-X., Hu R.-Z., Wang P.-Y., Shen Y.-S., Shuang F.-F., Wang J., Song P., Zhao W.-G., Yao X.-H., Zhang D.-Y., et al. Strong Silk Fibroin/PVA/Chitosan Hydrogels with High Water Content Inspired by Straw Rammed Earth Brick Structures. ACS Sustain. Chem. Eng. 2022;10:13070–13080. doi: 10.1021/acssuschemeng.2c03255. [DOI] [Google Scholar]
- 211.Borges F.T.P., Papavasiliou G., Teymour F. Characterizing the Molecular Architecture of Hydrogels and Crosslinked Polymer Networks beyond Flory–Rehner. II: Experiments. Biomacromolecules. 2023;24:1585–1603. doi: 10.1021/acs.biomac.2c01339. [DOI] [PubMed] [Google Scholar]
- 212.Borges F.T.P., Papavasiliou G., Teymour F. Characterizing the Molecular Architecture of Hydrogels and Crosslinked Polymer Networks beyond Flory–Rehner—I. Theory. Biomacromolecules. 2020;21:5104–5118. doi: 10.1021/acs.biomac.0c01256. [DOI] [PubMed] [Google Scholar]
- 213.Mahfufah U., Sultan N.A.F., Fitri A.M.N., Elim D., Mahfud M.A.S., Wafiah N., Friandini R.A., Chabib L., Aliyah, Permana A.D. Application of multipolymers system in the development of hydrogel-forming microneedle integrated with polyethylene glycol reservoir for transdermal delivery of albendazole. Eur. Polym. J. 2023;183:111762. doi: 10.1016/j.eurpolymj.2022.111762. [DOI] [Google Scholar]
- 214.Xu B., Wang H., Luo Z., Yang J., Wang Z. Multi-material 3D Printing of Mechanochromic Double Network Hydrogels for On-Demand Patterning. ACS Appl. Mater. Interfaces. 2023;15:11122–11130. doi: 10.1021/acsami.2c22564. [DOI] [PubMed] [Google Scholar]
- 215.Lin Q., Hu Y., Qiu C., Li X., Sang S., McClements D.J., Chen L., Long J., Xu X., Wang J., et al. Peanut protein-polysaccharide hydrogels based on semi-interpenetrating networks used for 3D/4D printing. Food Hydrocoll. 2023;137:108332. doi: 10.1016/j.foodhyd.2022.108332. [DOI] [Google Scholar]
- 216.Yang S., Tao X., Chen W., Mao J., Luo H., Lin S., Zhang L., Hao J. Ionic Hydrogel for Efficient and Scalable Moisture-Electric Generation. Adv. Mater. 2022;34:2200693. doi: 10.1002/adma.202200693. [DOI] [PubMed] [Google Scholar]
- 217.Labelle M.-A., Ispas-Szabo P., Tajer S., Xiao Y., Barbeau B., Mateescu M.A. Anionic and High-Amylose Starch Derivatives as Excipients for Pharmaceutical and Biopharmaceutical Applications: Structure-Properties Correlations. Pharmaceutics. 2023;15:834. doi: 10.3390/pharmaceutics15030834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Liang Y., Zhao X., Ma P.X., Guo B., Du Y., Han X. pH-responsive injectable hydrogels with mucosal adhesiveness based on chitosan-grafted-dihydrocaffeic acid and oxidized pullulan for localized drug delivery. J. Colloid Interface Sci. 2019;536:224–234. doi: 10.1016/j.jcis.2018.10.056. [DOI] [PubMed] [Google Scholar]
- 219.Huang J., Deng Y., Ren J., Chen G., Wang G., Wang F., Wu X. Novel in situ forming hydrogel based on xanthan and chitosan re-gelifying in liquids for local drug delivery. Carbohydr. Polym. 2018;186:54–63. doi: 10.1016/j.carbpol.2018.01.025. [DOI] [PubMed] [Google Scholar]
- 220.Zhang S., Song L., Liu B., Zhao Y.-D., Chen W. Poly(ethylene glycol) diacrylate based hydrogel filled micropore with enhanced sensing capability. Anal. Chim. Acta. 2023;1251:341000. doi: 10.1016/j.aca.2023.341000. [DOI] [PubMed] [Google Scholar]
- 221.Tang H., Guo C., Xu Q., Zhao D. Boosting Evaporative Cooling Performance with Microporous Aerogel. Micromachines. 2023;14:219. doi: 10.3390/mi14010219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Chen X., Fan M., Tan H., Ren B., Yuan G., Jia Y., Li J., Xiong D., Xing X., Niu X., et al. Magnetic and self-healing chitosan-alginate hydrogel encapsulated gelatin microspheres via covalent cross-linking for drug delivery. Mater. Sci. Eng. C. 2019;101:619–629. doi: 10.1016/j.msec.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 223.Supramaniam J., Adnan R., Mohd Kaus N.H., Bushra R. Magnetic nanocellulose alginate hydrogel beads as potential drug delivery system. Int. J. Biol. Macromol. 2018;118:640–648. doi: 10.1016/j.ijbiomac.2018.06.043. [DOI] [PubMed] [Google Scholar]
- 224.Alamdarnejad G., Kokabi M. Shape memory behavior of polyacrylate-based amorphous nanocomposite hydrogel under uniaxial tension: Modeling and experimental. Compos. B Eng. 2023;252:110501. doi: 10.1016/j.compositesb.2023.110501. [DOI] [Google Scholar]
- 225.Xiao Y., Li Q., Yao X., Bai R., Hong W., Yang C. Fatigue of amorphous hydrogels with dynamic covalent bonds. Extrem. Mech. Lett. 2022;53:101679. doi: 10.1016/j.eml.2022.101679. [DOI] [Google Scholar]
- 226.Driest P.J., Dijkstra D.J., Stamatialis D., Grijpma D.W. Structure–property relations in semi-crystalline combinatorial poly(urethane-isocyanurate)-type hydrogels. Polym. Int. 2022;71:1055–1061. doi: 10.1002/pi.6427. [DOI] [Google Scholar]
- 227.Apartsin E., Caminade A.-M. Single-Component Physical Hydrogels of Dendritic Molecules. J. Compos. Sci. 2023;7:26. doi: 10.3390/jcs7010026. [DOI] [Google Scholar]
- 228.Yang T., Wang L., Wu W.-H., Wei S., Zhang W.-B. Orchestrating Chemical and Physical Cross-Linking in Protein Hydrogels to Regulate Embryonic Stem Cell Growth. ACS Macro Lett. 2023;12:269–273. doi: 10.1021/acsmacrolett.2c00741. [DOI] [PubMed] [Google Scholar]
- 229.Sharma A., Panwar V., Mondal B., Prasher D., Bera M.K., Thomas J., Kumar A., Kamboj N., Mandal D., Ghosh D. Electrical stimulation induced by a piezo-driven triboelectric nanogenerator and electroactive hydrogel composite, accelerate wound repair. Nano Energy. 2022;99:107419. doi: 10.1016/j.nanoen.2022.107419. [DOI] [Google Scholar]
- 230.Torres F.G., Troncoso O.P., De-la-Torre G.E. Hydrogel-based triboelectric nanogenerators: Properties, performance, and applications. Int. J. Energy Res. 2022;46:5603–5624. doi: 10.1002/er.7585. [DOI] [Google Scholar]
- 231.Sun P., Li Q. Tension-Responsive Graphene Oxide Conductive Hydrogel with Robust Mechanical Properties and High Sensitivity for Human Motion Monitoring. Macromol. Mater. Eng. 2023;308:2200529. doi: 10.1002/mame.202200529. [DOI] [Google Scholar]
- 232.Yu S., An S.J., Kim K.J., Lee J.H., Chi W.S. High-Loading Poly(ethylene glycol)-Blended Poly(acrylic acid) Membranes for CO2 Separation. ACS Omega. 2023;8:2119–2127. doi: 10.1021/acsomega.2c06143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Nowak J.F., Kerns A., Patel P., Batzinger K., Tong X., Samuel J. The Construction of Biologically Relevant Fiber-Reinforced Hydrogel Geometries Using Air-Assisted Dual-Polarity Electrospinning, ASME. J. Biomech. Eng. 2023;145:011009. doi: 10.1115/1.4055038. [DOI] [PubMed] [Google Scholar]
- 234.Mabry K.M., Payne S.Z., Anseth K.S. Microarray analyses to quantify advantages of 2D and 3D hydrogel culture systems in maintaining the native valvular interstitial cell phenotype. Biomaterials. 2016;74:31–41. doi: 10.1016/j.biomaterials.2015.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Chang G., Chen Y., Li Y., Li S., Huang F., Shen Y., Xie A. Self-healable hydrogel on tumor cell as drug delivery system for localized and effective therapy. Carbohydr. Polym. 2015;122:336–342. doi: 10.1016/j.carbpol.2014.12.077. [DOI] [PubMed] [Google Scholar]
- 236.Naeem A., Yu C., Zang Z., Zhu W., Deng X., Guan Y. Synthesis and Evaluation of Rutin–Hydroxypropyl β-Cyclodextrin Inclusion Complexes Embedded in Xanthan Gum-Based (HPMC-g-AMPS) Hydrogels for Oral Controlled Drug Delivery. Antioxidants. 2023;12:552. doi: 10.3390/antiox12030552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Wang Y., Zheng C., Wu Y., Zhang B., Hu C., Guo C., Kong Q., Wang Y. An injectable and self-strengthening nanogel encapsuled hydrogel gene delivery system promotes degenerative nucleus pulposus repair. Compos. B Eng. 2023;250:110469. doi: 10.1016/j.compositesb.2022.110469. [DOI] [Google Scholar]
- 238.Lie W.-R., Steiner H., Williams S., Banerjee M., Saporita A., Gilliam B., Xiao Q. Abstract 5298: Multiplex immunoassay characterization of 48 cytokines, chemokines, and growth factors in colorectal cancer. Cancer Res. 2023;83:5298. doi: 10.1158/1538-7445.AM2023-5298. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are contained within the article.