Rubor et tumor cum calore et dolore—the cardinal signs of inflammation—first described by Cornelius Celsus—is far from a new concept. Even Galen understood that the balance of health and disease hinged on the body's response to exposures. Inflammation is a response to harmful stimuli and an essential component of the immune response that enables host survival to infection. When systemic immune system activation is overexuberant, any organ system can be adversely impacted. In the cardiovascular system, the impact of inflammation ranges broadly from the initiation or promotion of atherosclerosis to vasculitis, myocarditis, pericarditis, and even heart failure. 1 , 2 Recognizing this, along with recent clinical trials showing cardiovascular benefit when targeting the inflammatory pathways (interleukin‐1 inhibition in cardiovascular disease, CANTOS: Canakinumab Anti‐Inflammatory Thrombosis Outcome Study, 3 and pericarditis, RHAPSODY: Rilonacept Inhibition of Interleukin‐1 Alpha and Beta for Recurrent Pericarditis: A Pivotal Symptomatology and Outcomes Study 4 ), as well as upcoming and future trials testing this hypothesis (interleukin‐6 inhibition in atherosclerotic disease in ZEUS: A Research Study to Look at How Ziltivekimab Works Compared to Placebo in People With Cardiovascular Disease, Chronic Kidney Disease, and Inflammation 5 ), the time has come to define an evolving subspecialty focused on the intersection of the dysregulated immune response, inflammation, and cardiovascular system—termed cardio‐rheumatology. The expansion of the breadth and depth of cardiovascular medicine has led to an increase in subspecialization. Cardio‐oncology is one of the best examples of a growing field within the past decade, 6 with new emerging areas such as cardio‐obstetrics and cardio‐diabetology. 7 The concept of cardio‐rheumatology is not new, and clinical programs exist at a few academic centers, but we are now at a crossroad where it has come to the forefront. 8
What is cardio‐rheumatology, and what does it encompass? We propose that cardio‐rheumatology is a subspeciality that focuses on the impact of inflammation on the cardiovascular system. Other terms such as “cardio‐inflammation” could similarly be used, but the core features are the same. It includes understanding the cardiovascular impact of immune‐mediated inflammatory diseases, such as myo/pericarditis in systemic lupus erythematosus and early atherosclerosis observed in systemic lupus erythematosus and rheumatoid arthritis (RA) as well as inflammatory conditions typically managed by cardiology, including idiopathic recurrent pericarditis. Cardio‐rheumatology also includes familiarity with anti‐inflammatory strategies encompassing both the treatment and potential complications of targeting inflammation.
Autoimmune diseases are vast, and many are understudied in cardiovascular risk. A recent large study from the United Kingdom that examined 19 of the most common autoimmune disorders demonstrated that depending on the autoimmune conditions, patients may be up to 40% to >3 times more likely to develop cardiovascular disease, similar to the risk of type 2 diabetes. 9 Sarcoidosis is another multiorgan systemic inflammatory disease with cardiac involvement in up to 5% to 10% of affected patients. Cardiac involvement can be extensive and include cardiomyopathy/heart failure, atrioventricular conduction disease, or arrythmias and often requires advanced heart failure specialists and electrophysiology. Some referral institutions have separate dedicated programs to fulfill this multidisciplinary niche. 10
Cardiologists are comfortable prescribing statins and antiplatelet and heart failure therapies, but up until recently, therapies targeting the immune system for cardiovascular conditions have been limited. However, in 2020, the first US Food and Drug Administration–labeled biologic medication for recurrent pericarditis was approved with the interleukin‐1 trap receptor, rilonacept. 4 While this class of medication has been a mainstay in rheumatology, the cardio‐rheumatologist is uniquely positioned to anchor this overlapping area. At our centers, cardio‐rheumatology includes referred patients with refractory pericarditis, and many will then initiate interleukin‐1 inhibition therapy. In addition to pericarditis in which interleukin‐1 inhibition is now US Food and Drug Administration approved for a cardiac indication, there is an expanding body of work emerging on the role of interleukin‐1 and interleukin‐6 inhibition in atherosclerotic cardiovascular disease. 3 , 5 , 11 Approved therapies include targeting interleukin‐1 and interleukin‐6 for RA and systemic juvenile idiopathic arthritis, and interleukin‐6 is also used in large‐vessel vasculitis. 12 CANTOS was the first large‐scale proof of principle randomized control trial to test the inflammatory hypothesis in the general population for atherosclerosis using canakinumab (anti‐interleukin‐1β) and demonstrated an overall 15% reduction in cardiovascular events in patients with prior myocardial infarction and elevated high‐sensitivity C‐reactive protein (high‐sensitivity C‐reactive protein >2 mg/dL). 3 Further analysis demonstrated that the magnitude of interleukin‐6 reduction associated with reduction in major adverse cardiovascular events 13 which has led to the ongoing randomized double‐blind placebo‐controlled trial ZEUS, 5 focused on patients with chronic kidney disease and elevated high‐sensitivity C‐reactive protein to determine if ziltivekimab, a humanized monoclonal antibody that blocks interleukin‐6 ligand, compared with placebo reduces cardiovascular event rates. Although the similarities between pathways are important to recognize, the complexity of these biologics is essential to understand mechanistically, as ziltivekimab has not been studied in RA and whether interleukin‐6 inhibition will preferentially mitigate cardiovascular risk in patients with RA at higher cardiovascular risk compared with more standard conventional RA treatments is not known.
As the armamentarium of immunotherapies and biologics expand within rheumatology, knowledge of how these drugs affect the cardiovascular system is of increasing importance. It is important that the cardio‐rheumatologist understands both the short‐term effects (ie, lipid alterations) and the longer‐term outcomes of these therapies on cardiovascular health. One example is an increase in total cholesterol, including low‐density lipoprotein cholesterol and triglycerides, that can occur in a patient beginning therapy with tocilizumab, which could prompt initiation of a statin to control hyperlipidemia. The cardio‐rheumatologist can work with the rheumatologist to control the elevation in lipids as the optimal therapeutic regimen is found to control the inflammatory disease activity. Furthermore, the cardio‐rheumatologist will work closely with the rheumatologist in guiding the appropriate therapeutic selection for cardiovascular manifestations, such as in systemic lupus erythematosus myocarditis, and particularly in conditions that incorporate advanced cardiac imaging (eg, cardiac magnetic resonance imaging, cardiac positron emission tomography) in the longitudinal monitoring. This is not dissimilar to the awareness of checkpoint inhibitor–induced myocarditis within cardio‐oncology. 14 For example, in response to findings from the ORAL (Oral Rheumatoid Arthritis Trial) Surveillance, the US Food and Drug Administration issued a black box warning on the use of Janus kinase inhibitors for rheumatoid arthritis due to a safety signal for major adverse cardiovascular events and all‐cause death. 15 Now, as cardiologists, when we are asked to assist with assessing or managing cardiovascular risk in RA, a common autoimmune disorder with increased cardiovascular risk, we must also be aware that some disease‐modifying antirheumatic drugs may carry higher cardiovascular risk than others. One example is a patient referred to cardio‐rheumatology for cardiac risk stratification in the setting of Janus kinase inhibition, which is a frequent referral at our institution. Often, these medications are prescribed when others have failed. A patient on a Janus kinase inhibitor who is found to have high cardiovascular risk after cardiovascular risk stratification testing, such as severe calcium score identified on computed tomographic chest imaging would not only warrant initiation of aggressive primary cardiovascular prevention therapies but may warrant a discussion with the patient and the referring rheumatologist on other therapeutic options for RA.
Whether these various immunotherapies affect the cardiovascular system and cardiovascular risk similarly is still not known and a crucial area of scientific investigation moving forward. This will require mechanistic studies as well as longer‐term outcome studies. Given the rarity of these conditions compared with the general population, randomized control trials powered for cardiovascular outcomes are often not feasible, and this is where the expanding role of cardiovascular imaging biomarkers as a surrogate of cardiovascular risk and outcomes is well suited. Harnessing these imaging technologies could allow us to identify subclinical risk that can be treated before the development of a cardiovascular event.
We believe that cardiovascular risk prevention is at the forefront of cardio‐rheumatology. Equally important to treating the underlying inflammation process (eg, recurrent pericarditis, myocarditis, vasculitis) is the recognition of the increased risk of cardiovascular disease, particularly atherosclerotic disease, among patients with systemic inflammatory disorders. Patient awareness and education is a key component to prevention. Many academic centers embed the cardio‐rheumatology programs within cardiovascular prevention. However, as this field continues to grow, it could become a separate program or at least allow the programmatic structure for complex medical decision making across multiple different specialties with a footprint in cardiology and rheumatology. It is important for the cardiologist to recognize that our standard risk calculators do not adequately capture risk in these individuals. This has been most studied in RA, found to underestimate at least 2‐fold in women. In fact, the American College of Cardiology/American Heart Association 2019 updated guidelines to the atherosclerotic cardiovascular disease risk score highlight this by adding systemic inflammatory conditions as a risk enhancer that can be used in shared decision making for those at intermediate risk. Improved risk stratification is needed and is the ongoing area of multiple research efforts and an area where cardiovascular imaging tools may help to advance the field. One example is the recognition of the increased prevalence of coronary microvascular dysfunction in patients with systemic inflammatory conditions detected by cardiac myocardial perfusion positron emission tomography imaging or the prevalence of high‐risk plaque features in psoriatic disease detected by coronary computed tomography. 16 , 17 , 18 Cardiac imaging also plays an important role in cardiovascular inflammatory conditions such as cardiac magnetic resonance imaging in recurrent pericarditis or cardiac fluorodeoxyglucose positron emission tomography in inflammatory conditions that affect the myocardium and vasculature. 19 , 20 Furthermore, novel imaging markers and modalities are on the horizon; awareness and understanding of the use of these imaging modalities will be critical to the cardio‐rheumatology field moving forward to best enable the diagnosis, prognostication, and monitoring over time of these conditions. The field of cardio‐rheumatology could also adapt and learn from subspecialties such as cardio‐oncology for trial design and management. As the field evolves, we envision integrated multidisciplinary patient care models across cardiology, rheumatology, and immunology, similar to cardio‐oncology, to optimize management and preventive strategies and harmonize guidelines for treatment monitoring. Early detection and initiation of cardioprotective agents or even the choice of the biologic agent could be optimized. As the biologic landscape grows in rheumatology, the balance between the optimal treatment regimen for the disease versus the cardiovascular risk could be different, and these unanswered questions will certainly require future study with adaptative and innovative trial design. One example would be routine protocols of surveillance, such as the application of routine echocardiographic imaging with global longitudinal strain monitoring to detect subclinical myocardial dysfunction and initiation of cardioprotective therapies.
Similar to fields that have emerged within cardiology, cardio‐rheumatology will continue to grow, and incorporation of aspects of rheumatology clinical training in the use of targeted immune‐based therapies within cardiovascular training programs will be an important component. The field is expanding rapidly, but continued larger‐scale mechanistic studies and long‐term follow‐up data will be critical (Figure). We must move forward with caution and be aware that the immune system is complex and the dysregulated immune axis within each organ system may have different effects on the cardiovascular system. We must reach beyond the simple dichotomy of innate and adaptive immunity and dive deeper with the advancing tools available to disentangle the complicated relationship of “inflammation” and cardiovascular disease to improve the health of patients who also span these two fields.
Figure . Conceptual model of the individual components required to advance the evolving field of cardio‐rheumatology.
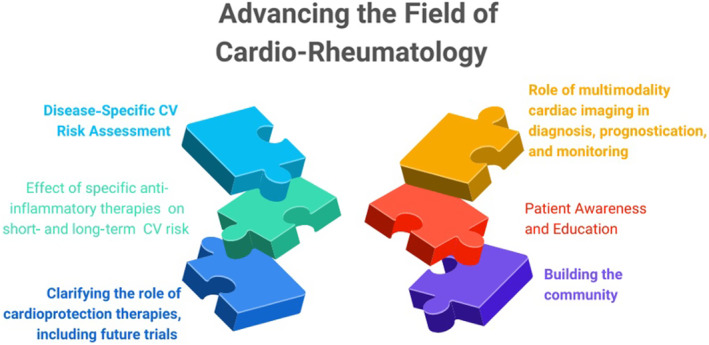
Shown are the key building blocks for advancing the care of patients with systemic inflammatory disorders. CV indicates cardiovascular.
Sources of Funding
Dr Weber is supported, in part, by National Heart, Lung, and Blood Institute K23 HL159276‐01 and American Heart Association Career Development Grant (Dallas, TX) 21CDA851511. American Society of Nuclear Cardiology Institute for the Advancement of Nuclear Cardiology Research Award. Dr Garshick is supported, in part, by a National Heart, Lung, and Blood Institute K23 HL152013 career development award and an unrestricted Pfizer Research Grant.
Disclosures
The authors have reported that they have no conflict‐of‐interest relationships relevant to the contents of this article to disclose. The author financial disclosures include: Dr Di Carli reports grants from Gilead Sciences and Spectrum Dynamics, and personal consulting fees from Janssen and Bayer, outside the submitted work. Dr Weber reports personal consulting fees from Horizon Therapeutics, Novo Nordisk, and Kinisika, outside of the submitted work. Dr Garshick reports personal consulting fees from Horizon Therapeutics and Abbvie.
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
This manuscript was sent to Kwok Leung Ong, PhD, Guest Editor, for review by expert referees, editorial decision, and final disposition.
For Sources of Funding and Disclosures, see page 4.
REFERENCES
- 1. Libby P, Hansson GK. Inflammation and immunity in diseases of the arterial tree: players and layers. Circ Res. 2015;116:307–311. doi: 10.1161/circresaha.116.301313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mason JC, Libby P. Cardiovascular disease in patients with chronic inflammation: mechanisms underlying premature cardiovascular events in rheumatologic conditions. Eur Heart J. 2014;36:482–489. doi: 10.1093/eurheartj/ehu403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914 [DOI] [PubMed] [Google Scholar]
- 4. Klein AL, Imazio M, Cremer P, Brucato A, Abbate A, Fang F, Insalaco A, LeWinter M, Lewis BS, Lin D, et al. Phase 3 trial of interleukin‐1 trap rilonacept in recurrent pericarditis. N Engl J Med. 2021;384:31–41. doi: 10.1056/NEJMoa2027892 [DOI] [PubMed] [Google Scholar]
- 5. Ridker PM. From RESCUE to ZEUS: will interleukin‐6 inhibition with ziltivekimab prove effective for cardiovascular event reduction? Cardiovasc Res. 2021;117:e138–e140. doi: 10.1093/cvr/cvab231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hayek SS, Ganatra S, Lenneman C, Scherrer‐Crosbie M, Leja M, Lenihan DJ, Yang E, Ryan TD, Liu J, Carver J, et al. Preparing the cardiovascular workforce to care for oncology patients: JACC review topic of the week. J Am Coll Cardiol. 2019;73:2226–2235. doi: 10.1016/j.jacc.2019.02.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rosenblit PD, Lepor NE, Wong ND. The emergence of cardiodiabetology. Cardiovasc Endocrinol. 2017;6:3–7. doi: 10.1097/xce.0000000000000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yoo BW. Embarking on a career in cardio‐rheumatology. J Am Coll Cardiol. 2020;75:1488–1492. doi: 10.1016/j.jacc.2020.02.021 [DOI] [PubMed] [Google Scholar]
- 9. Conrad N, Verbeke G, Molenberghs G, Goetschalckx L, Callender T, Cambridge G, Mason JC, Rahimi K, McMurray JJV, Verbakel JY. Autoimmune diseases and cardiovascular risk: a population‐based study on 19 autoimmune diseases and 12 cardiovascular diseases in 22 million individuals in the UK. Lancet. 2022;400:733–743. doi: 10.1016/S0140-6736(22)01349-6 [DOI] [PubMed] [Google Scholar]
- 10. Giblin GT, Murphy L, Stewart GC, Desai AS, Di Carli MF, Blankstein R, Givertz MM, Tedrow UB, Sauer WH, Hunninghake GM, et al. Cardiac sarcoidosis: when and how to treat inflammation. Card Fail Rev. 2021;7:e17. doi: 10.15420/cfr.2021.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Weber B, Weisenfeld D, Seyok T, Huang SS, Massarotti E, Barrett L, Bibbo CF, Solomon D, Plutzky J, Bolster M, et al. The relationship between ascvd risk, inflammation, and coronary microvascular dysfunction in rheumatoid arthritis. J Am Coll Cardiol. 2022;79:1207. doi: 10.1016/S0735-1097(22)02198-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Choy EH, De Benedetti F, Takeuchi T, Hashizume M, John MR, Kishimoto T. Translating IL‐6 biology into effective treatments. Nat Rev Rheumatol. 2020;16:335–345. doi: 10.1038/s41584-020-0419-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ridker PM, Libby P, MacFadyen JG, Thuren T, Ballantyne C, Fonseca F, Koenig W, Shimokawa H, Everett BM, Glynn RJ. Modulation of the interleukin‐6 signalling pathway and incidence rates of atherosclerotic events and all‐cause mortality: analyses from the Canakinumab Anti‐Inflammatory Thrombosis Outcomes Study (CANTOS). Eur Heart J. 2018;39:3499–3507. doi: 10.1093/eurheartj/ehy310 [DOI] [PubMed] [Google Scholar]
- 14. Mahmood SS, Fradley MG, Cohen JV, Nohria A, Reynolds KL, Heinzerling LM, Sullivan RJ, Damrongwatanasuk R, Chen CL, Gupta D, et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71:1755–1764. doi: 10.1016/j.jacc.2018.02.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Khosrow‐Khavar F, Kim SC, Lee H, Lee SB, Desai RJ. Tofacitinib and risk of cardiovascular outcomes: results from the Safety of TofAcitinib in Routine care patients with Rheumatoid Arthritis (STAR‐RA) study. Ann Rheum Dis. 2022;81:798–804. doi: 10.1136/annrheumdis-2021-221915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Weber BN, Stevens E, Perez‐Chada LM, Brown JM, Divakaran S, Bay C, Bibbo C, Hainer J, Dorbala S, Blankstein R, et al. Impaired coronary vasodilator reserve and adverse prognosis in patients with systemic inflammatory disorders. JACC Cardiovasc Imaging. 2021;14:2212–2220. doi: 10.1016/j.jcmg.2020.12.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Feher A, Boutagy NE, Oikonomou EK, Liu Y‐H, Miller EJ, Sinusas AJ, Hinchcliff M. Association between impaired myocardial flow reserve on 82rubidium positron emission tomography imaging and adverse events in patients with autoimmune rheumatic disease. Circ Cardiovasc Imaging. 2021;14:e012208. doi: 10.1161/circimaging.120.012208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lerman JB, Joshi AA, Chaturvedi A, Aberra TM, Dey AK, Rodante JA, Salahuddin T, Chung JH, Rana A, Teague HL, et al. Coronary plaque characterization in psoriasis reveals high‐risk features that improve after treatment in a prospective observational study. Circulation. 2017;136:263–276. doi: 10.1161/CIRCULATIONAHA.116.026859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chetrit M, Xu B, Kwon DH, Ramchand J, Rodriguez RE, Tan CD, Jellis CL, Johnston DR, Renapurkar RD, Cremer PC, et al. Imaging‐guided therapies for pericardial diseases. JACC Cardiovasc Imaging. 2020;13:1422–1437. doi: 10.1016/j.jcmg.2019.08.027 [DOI] [PubMed] [Google Scholar]
- 20. Martineau P, Grégoire J, Harel F, Pelletier‐Galarneau M. Assessing cardiovascular infection and inflammation with FDG‐PET. Am J Nucl Med Mol Imaging. 2021;11:46–58. [PMC free article] [PubMed] [Google Scholar]


