Abstract
Background
Forward Head Posture (FHP), which refers to the head being more forward than the shoulder, is one of the most common postural defects of all ages. Therefore, in this study, we aimed to compare the effectiveness of exercise therapy and electroacupuncture in patients with FHP and myofascial pain syndrome (MPS).
Methods
The present study was an open-label randomized clinical trial. A total of 61 patients with FHP and MPS who were referred to the physical medicine clinic of Besat Hospital between 2020 and 2021 were analyzed. Patients in one group were treated with electroacupuncture, and another one was treated with exercise therapy. The primary outcomes were FHP angles (CVA, CA, and shoulder angle), pain intensity (VAS), and quality of life (SF-12). Paired t-test was used to compare the results obtained in the pre-test and post-test. To detect differences over time, the analysis of variance models was used to repeat the observations. If the p-test result is less than the test significance level of 0.05, the null hypothesis is not confirmed.
Results
The rate of final CVA and increase in CVA in the exercise therapy group were significantly higher than in the electroacupuncture group (P < 0.001). The average shoulder angle in the exercise therapy group increased from 47.1° ± 3.0° to 51.9° ± 3.3° (P < 0.001) and in the electroacupuncture group from 47.9° ± 3.1° to 51.0° ± 2.8° (P < 0.001). A significant difference was observed between the two groups in terms of pain intensity changes during the study.
Conclusion
Overall, the results of this study showed that both exercise therapy and electroacupuncture significantly improved patients' posture, reduced pain intensity, and increased quality of life in FHP patients with MPS; But exercise therapy was more effective in improving FHP angles and electroacupuncture was more successful in reducing patients' pain intensity.
Keywords: Exercise Therapy, Electroacupuncture, Myofascial Pain Syndrome, Forward Head Posture
↑What is “already known” in this topic:
We aimed to compare of the effectiveness of exercise therapy and electroacupuncture in patients with forward head abnormalities and myofascial pain syndrome.
→What this article adds:
The rate of final CVA and increase in CVA in the exercise therapy group were significantly higher than in the electroacupuncture group.
Introduction
Forward head posture (FHP), which refers to the head being more forward than the shoulder, is one of the most common postural defects of all ages(1, 2). In this anomaly, the head and neck areas deviate forward relative to the sagittal reference line, which increases the flexion of the cervical vertebrae and the tendency of the head to move forward and down (3-7).
A number of previous studies have shown FHP to be associated with other musculoskeletal disorders such as neck and shoulder pain, fibromyalgia, temporomandibular joint (TMJ) disorders, masticatory muscle disorders, and myofascial pain syndrome (MPS) (8-11). Disorders in the position of the joints and changes in muscle activity cause stress on the muscles in this area and cause trigger points and musculoskeletal pain in these patients (12). All of these cases reduce the quality of life and dysfunction of patients (13). Therefore, it is necessary to develop correct posture habits to correct defective posture and achieve proper spinal function.
The goals of treatment to correct postural problems include improving the range of motion, increasing flexibility, and increasing the strength of weak muscles (14). Manipulation, postural retraining, use of kinesio tape and orthoses, and exercise therapy are some of the most common treatments for FHP (15-18). Exercise therapy, especially resistance and stretching exercises, stretches the shortened upper trapezius, sternocleidomastoid muscle (SCM), and scapular muscles and increases the strength of the deep cervical flexor muscles; Therefore, they are associated with improving the position of the head and shoulders (18, 19). However, due to differences in the results and protocols of exercise therapy used in different studies, more studies are still needed to determine the effectiveness of exercise therapy and compare it with other modern methods. However, due to differences in the results and protocols of exercise therapy used in different studies, more studies are still needed to determine the effectiveness of exercise therapy and compare it with other modern methods. Many previous studies have shown the usefulness of acupuncture in improving a wide range of musculoskeletal problems (20). Acupuncture stimulates points on the body manually or electrically by inserting a needle to modulate pain perception or alter physiological functions (21) In electroacupuncture, an electric current passes through the needle and appears to be slightly more effective in relieving pain than acupuncture (22). Electroacupuncture relieves pain by activating a range of bioactive chemicals through peripheral mechanisms, the spinal cord, and the central nervous system (23).
Opioids that reduce the sensitivity of peripheral pain receptors and reduce proinflammatory cytokines in the environment and in the spinal cord and serotonin and norepinephrine that reduce the phosphorylation of the N-methyl-D-aspartate GluN1 subunit, including These are chemicals (24-27). Although there is no quality evidence and studies in support of the trigger point electroacupuncture method, it seems to be a low-complication and effective therapeutic intervention in patients with neck and musculoskeletal pain (28).
The aim of this study was to compare the effectiveness of exercise therapy and electroacupuncture in improving the condition and pain in patients diagnosed with MPS and FHP. It is hoped that the results of this study will lead to better treatment and increased quality of life for patients with FHP.
Methods
The present study was a parallel open-label randomized clinical trial. This study was performed between 2020 and 2021 in the physical medicine clinic of Besat Hospital and Neshat Rehabilitation Clinic, affiliated with Hamadan University of Medical Sciences, Hamedan, Iran. The study was approved by the Local Ethics Committee of Hamedan University of Medical Sciences, Hamedan, Iran and registered in the Iranian Registry of Clinical Trials (IRCT.ir); ID number: IRCT20151123025202N17. In this study, informed consent was received from all participants and their partners.
Population/Patients
A total of 65 patients with FHP and MPS who referred to the physical medicine clinic of Besat Hospital between 2020 and 2021 were included. A sample size of 61 patients in two groups was estimated to detect a CVA difference of 2.5 (2.6) in the exercise therapy group and 0.5 (2.3) in the control group (based on Rivo et al.) (18), with 85% power, 95% confidence interval, and considering 15% drop out rate. A total of 65 patients with FHP and MPS who referred to the physical medicine clinic of Besat Hospital between 2020 and 2021. One of the patients was excluded from the study due to unwillingness to continue treatment. One case was excluded from the study due to physiotherapy 1 month before enrollment. Two patients were excluded from the study with a history of radicular pain and MRI based on cervical disc herniation despite abnormal posture (Figure 1).
Figure 1.
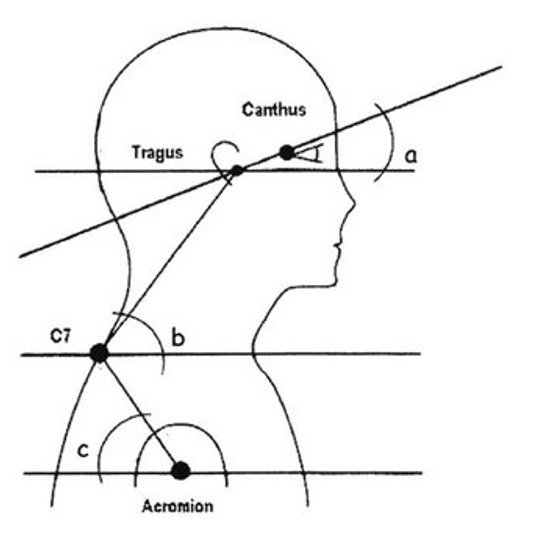
FHP angles were measured in this study. A: CA angle or sagittal head tilt angle, B: CVA angle, C: shoulder angle
The inclusion criteria were as follows; diagnosis of FHP based on standard clinical criteria, diagnosis of MPS with at least 1 trigger point in the neck or shoulder girdle, and age 65-18 years. Patients were excluded if they had shoulder surgery, pregnancy, history of cervical vertebral fractures, peripheral vascular disease (PVD), cardiac pacemaker, taking anticoagulants and bleeding disorders, treating skin disease, other diseases of the cervical spine (scoliosis fracture, symptomatic disc herniation ...), nervous and motor disorders (stroke, Parkinson’s, ...), and any pharmacological or non-pharmacological treatment for neck pain.
Randomization
Participants were randomly assigned to two groups by means of a computer-generated random number.
Data collection method
Diagnostic criteria based on the criteria of Simons et al. And Gerwin et al. Were used to diagnose MPS.
❖ Existence of a stretched band in the muscle
❖ The presence of a super-sensitive lightning point in the drawn tape
❖ Have a quick contraction response package
❖ At trigger point compression, the patient has the same typical referral or localized pain
❖ The presence of spontaneous pain in a specific radicular pattern familiar to the patient.
According to previous studies and assessments, there is no standard and definitive treatment for this disease, so in this study, patients were not deprived of standard treatment in either group. All patients underwent a complete physical examination as soon as they entered the study. A complete history was taken of the patient and then initial examinations including neurological examinations and musculoskeletal examinations, were performed. After confirmation, the checklist of demographic information (age, gender, ethnicity, occupation) and clinical information (signs and symptoms, duration of symptoms, etc.) was filled out.
Main Outcomes
The primary outcomes included FHP angles (CVA, CA, and shoulder angle), pain intensity (VAS), and quality of life (SF-12). The amount of head-forward angle was measured using the body profile imaging method and similar to the protocol presented in the study of Ruivo et al. (18). First, the authors identified and marked the three anatomical features of the ear tragus and the protrusion of the right acromion, as well as the thorny appendage of the C7 vertebra. The patients were then asked to stand at a designated location next to the wall (at a distance of 23 cm) with their left arm facing the wall. Then, the tripod on which the digital camera was installed was placed at a distance of 265 cm from the wall and its height was adjusted to the level of the patient's right shoulder. In such a condition, the patients were asked to bend forward three times and raise their arms over head three times, then stand completely comfortably and naturally and look at a hypothetical point on the opposite wall (eyes in line Horizon). Then, after a five-second pause, the authors took a photo of the body profile. Finally, the image was transferred to a computer and using ImageJ software, the angle of the line between the canthus of the eye and the tragus with the horizon (CA, angle a), the angle of the line of the tragus and C7 with the horizon (neck angle or CVA, angle b) and the angle of the connecting line C7 and the acromion with the horizon line (shoulder angle, angle C) were measured according to Figure 1.
The VAS pain visual acuity scale was used to assess the severity of neck and shoulder girdle pain in patients. The standardized questionnaire SF-12 was used to assess the quality of life. The above variables were measured at the beginning of the study and after the end of the study (twelfth week).
Interventions
The duration of treatment in this study was 3 months (12 weeks). Group A patients underwent exercise therapy. Exercise therapy sessions were performed once a week for 20 to 30 minutes under the supervision of a therapist. The exercise therapy protocol of this study is similar to the study of Ruivo et al. (18).Three stretching exercises and four strength exercises were performed with the aim of correcting the neck and shoulders. Strength training is designed for the activity of the rotator cuff, especially the fear minor, infraspinatus, scapular stabilizing muscles (upper and lower trapezius), rhomboids, and deep neck flexors. Stretching exercises were designed to stretch the shortened pectoralis minor muscles, the SCM neck muscles, and the scapula lift. Each session of the exercise program was performed under the direct supervision of the therapist to ensure the correctness of the exercises. To increase patients' resistance, all exercises were started lightly, including 2 sets of 15, and gradually the intensity, the number of sets and the repetition of movements were increased. The average duration of exercise was 20 to 30 minutes and the exercise sequence was random.
For patients in group B, electroacupuncture was performed (first, neck, and shoulder girdle muscles including the trapezius, SCM, sub-occipital, scapula, pectoralis major, and infraspinatus and rhomboid). The detection of trigger points was consistent with the criteria of Simons et al. (29), and Gerwin et al. (30). The identified trigger point was marked for each patient at the anatomical site.
For electroacupuncture, patients were asked to lie in a comfortable bed in a calm room for 20 minutes. Procedure and faint symptoms of weakness, dizziness, shortness of breath, and nausea were reported to the patient. In each session, the previous meal was taken and the patient did not fast for a long time. The patient's skin was checked for cleanness and free of lotion oil and perspiration. Electroacupuncture after sterilization of the position by inserting a steel acupuncture needle with a diameter of 0.25 mm and a length of 40 mm in the identified trigger point (ashi points) and routine points of acupuncture neck pain with pinching needle insertion technique and establishing electricity by the device SDZ-II 2013 was performed.
Fixed stimulus points in group B patients include 15 points, which according to the results of previous studies in a study conducted in China in 2019 as the most effective electroacupuncture points in reducing neck pain patients: GB-20, GB- 21, GB-12, SI-14 SI-15 SI-3, SI-11, BL-10, BL-11, LI-10, LI-16, DU-14, SJ-3, SJ-15, LU- 7
The EA device was set up with the following specifications for the therapeutic session duration of 20 minutes and maximum stimulation intensity with mild pain determined by the patient's thorax. Frequency 5 to 100 Hz and the selected wave pattern Dense disperse (a combination of high and low-frequency waves and the patient does not adapt to stimulation). As in group A, treatment sessions in this group were once a week for 12 weeks.
Statistical analyses
After collecting data, the relevant data were analyzed in SPSS software version 20. Mean and standard deviation was used to describe quantitative variables and frequency and percentage were used to describe qualitative variables. Parametric analyzes (t-test and ANOVA) were used to analyze the variables with normal distribution and non-parametric analyzes (Mann-Whitney U and Chi-square) were used to analyze the variables with abnormally distributed. Paired t-test was used to compare the results obtained in the pre-test and post-test. To detect differences over time, an analysis of variance models was used to repeat the observations. If the p-test result is less than the test significance level of 0.05, the null hypothesis is not confirmed.
Results
Demographic profile
A total of 61 patients with MPS and FHP were analyzed.31 patients in the exercise therapy group and 30 patients in the electroacupuncture group were analyzed (Figure 2). 16 patients (51.6%) of the exercise therapy group and 17 patients (56.7%) of the electroacupuncture group were female (P = 0.692). The mean age of patients in the exercise therapy group was 39.9 ± 11.1, and in the electroacupuncture group was 37.2 ± 8.2 (P = 0.383). The demographic and clinical characteristics of patients in this study by group therapy are shown in Table 1. As can be seen, the condition of the patients in the two groups at the beginning of the study was similar in terms of body mass index, FHP angles (CA, CVA and shoulder angle), pain intensity and quality of life.
Figure 2.
CONSORT flow diagram
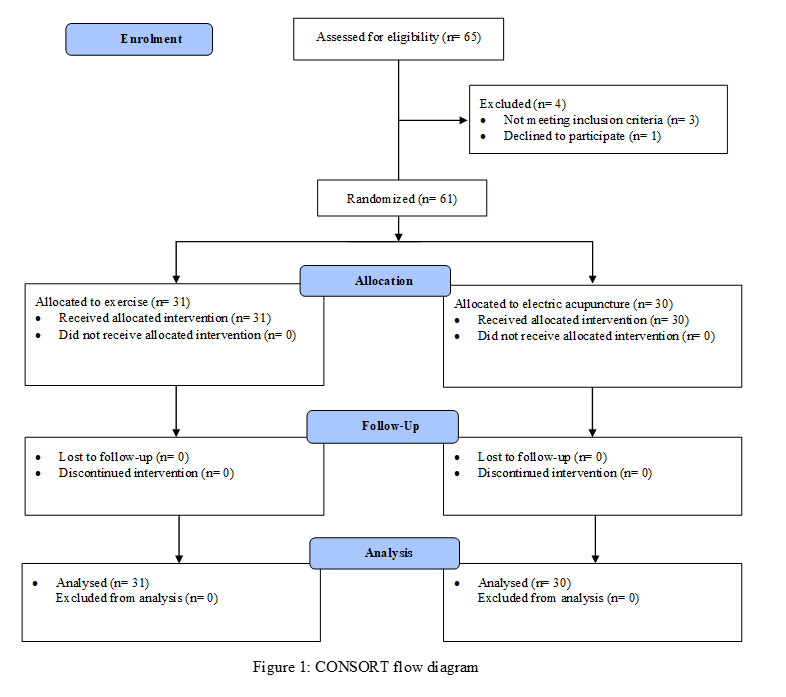
Table 1. Baseline characteristics of patients in this study at the time of enrollment.
| Variable | Exercise therapy group (N=31) | Electric acupuncture group (N=30) | P-value |
|---|---|---|---|
| Age | 39.9 ± 11.1 | 37.7 ± 8.2 | 0.383 |
|
Sex
Male Female |
16 (51.6 %) 15 (48.4 %) |
17 (56.7 %) 13 (43.3 %) |
0.692 |
| BMI | 26.8 ± 3.3 | 27.5 ± 4.1 | 0.529 |
|
FHP angles
CA CVA Shoulder angle |
40.2 ± 2.9 44.1 ± 2.9 47.1 ± 3.0 |
40.4 ± 3.6 44.8 ± 2.9 47.9 ± 3.1 |
0.804 0.372 0.267 |
| Intensity of pain | 8.8 ± 1.0 | 9.0 ± 1.0 | 0.382 |
| Quality of Life | 63.7 ± 14.2 | 60.1 ± 12.5 | 0.305 |
Comparison of two groups in terms of CA changes
The mean CA in the exercise therapy group increased from 40.2 ± 2.9 degrees to 49.0 ± 3.5 degrees (P <0.001), and in the electroacupuncture group from 40.4 ± 3.6 degrees to 43.9 ± 3.8 degrees (P < 0.001) (Figure 3). CA changes in exercise therapy and electroacupuncture groups are compared in Table 2. As can be seen, the final CA (P < 0.001) and the increase in CA (P <0.001) in the exercise therapy group were significantly higher than in the electroacupuncture group. The difference between groups remained significant even after adjustment for baseline CA was applied (mean difference [95% CI]: 5.3 [3.8-6.7], P < 0.001).
Figure 3.
Mean CA changes during the study period
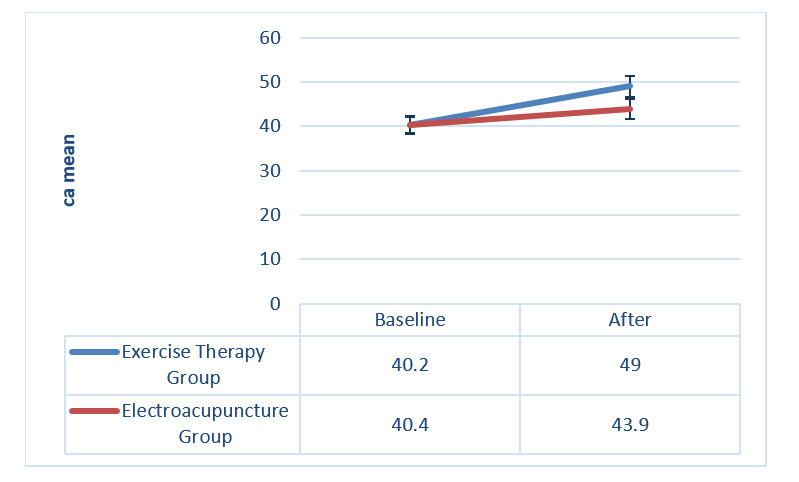
Table 2. Comparison of CA changes in the exercise therapy and electroacupuncture groups.
| Variable | Exercise therapy group (N=31) | Electric Acupuncture Group (N=30) | P-value (Comparison between groups) |
|---|---|---|---|
| CA mean in baseline | 40.2 ± 2.9 | 40.4 ± 3.6 | 0.804 |
| Final CA mean (Month 3) | 49.0 ± 3.5 | 43.9 ± 3.8 | <0.001 |
| Mean (95% confidence interval) CA changes | 8.7 (7.4 – 10.1) | 3.4 (2.7 – 4.2) | <0.001 |
| P-value (intragroup comparison) | <0.001 | <0.001 | - |
| Adjusted final CAa mean (SE) | 49.0 (0.5) | 43.8 (0.5) | <0.001 |
a Adjusted for baseline CA using ANCOVA analysis.
Comparison of two groups in terms of CVA changes
The mean CVA size in the exercise therapy group increased from 44.1 ± 2.9 degrees to 52.6 ± 2.2 degrees (P < 0.001) and in the electroacupuncture group from 44.8 ± 2.9 degrees to 48.6 ± 3.4 degrees (P < 0.001) (Figure 4). The CVA changes in the two groups of exercise therapy and electroacupuncture are compared in Table 3. The rate of final CVA (P < 0.001) and increase in CVA (P < 0.001) in the exercise therapy group were significantly higher than in the electroacupuncture group (Table 3). The difference between groups remained significant even after adjustment for baseline CVA was applied (mean difference [95% CI]: 4.5 [3.5-5.5], P < 0.001).
Figure 4.
Changes in the mean CVA during the study period
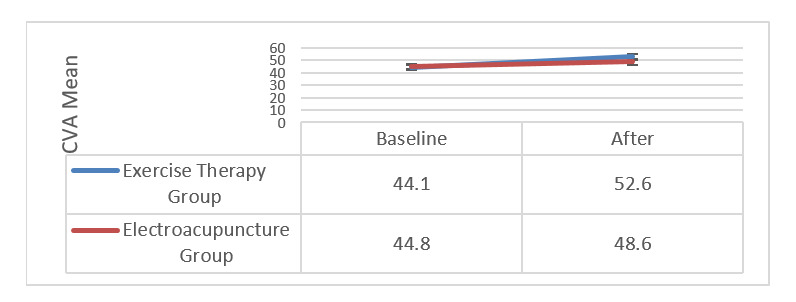
Table 3. Comparison of CVA changes in the exercise therapy and electroacupuncture groups.
| Variable | Exercise therapy group (N=31) | Electric Acupuncture Group (N=30) | P-value (Comparison between groups) |
|---|---|---|---|
| CVA Study time | 44.1 ± 2.9 | 44.8±2.9 | 0.372 |
| Final CVA (Month 3) | 52.6 ± 2.2 | 48.6 ± 3.4 | <0.001 |
| Mean (95% confidence interval) CVA changes | 8.5 (7.6 – 9.3) | 3.8 (3.2 – 4.4) | <0.001 |
| P-value (intragroup comparison) | <0.001 | <0.001 | - |
| Adjusted final CVAa mean (SE) | 52.8 (0.3) | 48.4 (0.4) | <0.001 |
a Adjusted for baseline CVA using ANCOVA analysis.
Comparison of two groups in terms of shoulder angle changes
The average shoulder angle in the exercise therapy group increased from 47.1 ± 3.0 degrees to 51.9 ± 3.3 degrees (P < 0.001), and in the electro-acupuncture group from 47.9 ± 3.1 degrees to 51.0 ± 2.8 degrees (P < 0.001) (Figure 5). Shoulder angle changes in the two groups of exercise therapy and electro-acupuncture are compared in Table 4. There was no significant difference between the two groups in this study in terms of the final amount of shoulder angle (P = 0.254). However, when adjusted for baseline shoulder angle was applied using ANCOVA analysis, the final shoulder angle in the exercise therapy group was significantly higher than the electroacupuncture group (mean difference [95% CI]: 1.6 [0.5-2.6], P = 0.004). The increase in shoulder angle in the exercise therapy group was significantly higher than in the electroacupuncture group (P = 0.002).
Figure 5.
Changes in the average shoulder angle during the study period
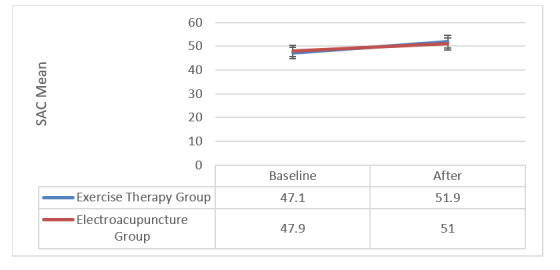
Table 4. Comparison of shoulder angle changes in the two groups of exercise therapy and electro-acupuncture.
| Variable | Exercise therapy group (N=31) | Electric Acupuncture Group (N=30) | P-value (Comparison between groups) |
|---|---|---|---|
| Shoulder angle Study time | 47.1 ± 3.0 | 47.9 ± 3.1 | 0.267 |
| Final shoulder angle (Month 3) | 51.9±3.3 | 51.0 ± 2.8 | 0.254 |
| Mean (95% confidence interval) shoulder angle changes | 4.8 (3.9 – 5.8) | 3.1 (2.5 – 3.6) | 0.002 |
| P-value (intragroup comparison) | <0.001 | <0.001 | - |
| Adjusted final shoulder angleamean (SE) | 52.2 (0.4) | 50.7 (0.4) | 0.004 |
a Adjusted for baseline shoulder angle using ANCOVA analysis.
Comparison of changes in pain intensity between the two groups
Changes in pain intensity during the study in the two groups of exercise therapy and electroacupuncture are shown in Table 5.
Table 5. Comparison of pain intensity changes in the two groups of exercise therapy and electroacupuncture.
| Thickness after Anserina | Exercise therapy group (N=31) | Electric Acupuncture Group (N=30) | P-value (Comparison between groups) |
|---|---|---|---|
| First Visit | 8.8 ± 1.0 | 9.0 ± 1.0 | 0.382 |
| One month after the intervention | 6.8±1.0 | 3.8±1.7 | <0.001 |
| Changes since the first visit | -1.8 (-1.2; -2.5) | -5.3 (-4.6; -5.9) | <0.001 |
| P-value (intragroup comparison) | <0.001 | <0.001 | |
| Two months after the intervention | 6.4±1.4 | 3.1±1.5 | <0.001 |
| Changes since the first visit | -2.4 (-1.7; -3.1) | -6.0 (-5.3; -6.7) | <0.001 |
| P-value (intragroup comparison) | <0.001 | <0.001 | |
| Changes compared to the first month | -0.6 (-0.02; -1.1) | -0.7 (-0.1; -1.3) | 0.321 |
| P-value (intragroup comparison) | 0.036 | 0.008 | |
| Three months after the intervention | 5.4±1.7 | 2.1±1.5 | <0.001 |
| changes from the first visit | -3.4 (-2.7; -4.2) | -6.4 (-5.7; -7.2) | <0.001 |
| P-value (intragroup comparison) | <0.001 | <0.001 | |
| Changes compared to the first month | -1.6 (-0.9; -2.3) | -1.2 (-0.4; -1.9) | 0.558 |
| P-value (intragroup comparison) | <0.001 | <0.001 | |
| Changes compared to the second month | -1.0 (-0.4; -1.6) | -0.5 (-1.0; -0.1) | 0.803 |
| P-value (intragroup comparison) | <0.001 | 0.165 |
Then, using Repeated Measures ANOVA, we compared the trend of pain intensity changes during the study. Due to the non-confirmation of the spatial hypothesis of the Machuli test (P = 0.021), Greenhouse-Geisser line statistics were considered.
According to the results of the RM-ANOVA test, the effect of time was significant (F = 332.3, P < 0.001). This finding means that patients' pain intensity was significantly reduced during the study. Also, group-time interaction was significant (F = 49.1, P < 0.001). This result indicates a significant difference between the two groups of exercise therapy and electroacupuncture in terms of pain intensity changes during the study. Then, using Bonferroni post hoc test, we compared the changes in pain intensity during the study within each group and compared between groups (Table 5). In both exercise therapy and electroacupuncture groups, pain intensity was significantly reduced in the first, second and third months after the intervention compared to baseline (P < 0.001); But this reduction in pain intensity in the electroacupuncture group was significantly better than the exercise therapy group (P < 0.001). In the electroacupuncture group, no significant difference was found between the pain intensity between the second and third months of the intervention (P = 0.165) (Table 5).
Comparison of quality-of-life changes between the two groups
Changes in the quality-of-life score during the study period in the two groups of exercise therapy and electro-acupuncture are shown in Table 6. Using the RM-ANOVA test, we compared the trend of changes in quality-of-life scores during the study. Due to the non-confirmation of the sphericity of the Machuli test (P <0.001), the Greenhouse-Geisser line statistics were considered. According to the results of the RM-ANOVA test, the effect of time was significant (F = 141.3, P < 0.001). This finding means that quality of life scores increased significantly during the study. Also, group-time interaction was significant (F = 3.9, P = 0.027). This result indicates a significant difference between the two groups of exercise therapy and electroacupuncture in terms of changes in quality of life scores during the study period. Then, using Bonferroni post hoc test, we compared the changes in pain intensity during the study within each group and compared between groups (Table 6). In both exercise therapy and electroacupuncture groups, the mean scores of quality of life in the first, second and third months after the intervention increased significantly compared to the initial visit (P < 0.001). The mean quality of life scores only in the second month after the intervention were significantly different between the two groups (P = 0.024), so the quality of life scores in the electro-acupuncture group were higher than the exercise therapy group. In the electroacupuncture group, no significant difference was found between the quality-of-life scores between the second and third months of the intervention (P = 0.156).
Table 6. Comparison of quality-of-life score changes in the two groups of exercise therapy and electro-acupuncture.
| Thickness after Anserina | Exercise therapy group (N=31) | Electric Acupuncture Group (N=30) | P-value (Comparison between groups) |
|---|---|---|---|
| First Visit | 63.7 ± 14.2 | 60.1 ± 12.5 | 0.305 |
| One month after the intervention | 76.5 ± 10.3 | 79.4 ± 10.5 | 0.269 |
| Changes since the first visit | 12.7 (7.3 – 18.2) | 19.3 (13.9 – 24.8) | 0.024 |
| P-value (intragroup comparison) | <0.001 | <0.001 | - |
| Two months after the intervention | 80.6 ± 9.2 | 85.1 ± 6.7 | 0.032 |
| Changes since the first visit | 16.8 (10.7 – 23.1) | 25 (18.8 – 31.2) | 0.014 |
| P-value (intragroup comparison) | <0.001 | <0.001 | - |
| Changes compared to the first month | 4.1 (0.4 – 7.8) | 5.7 (2.0 – 9.4) | 0.408 |
| P-value (intragroup comparison) | 0.022 | 0.001 | - |
| Three months after the intervention | 84.9 ± 6.5 | 87.1 ± 7.0 | 0.221 |
| changes from the first visit | 21.2 (14.9 – 27.6) | 27 (20.6 – 33.3) | 0.086 |
| P-value (intragroup comparison) | <0.001 | <0.001 | - |
| Changes compared to the first month | 8.5 (4.3 – 12.7) | 7.6 (3.5 – 11.8) | 0.702 |
| P-value (intragroup comparison) | <0.001 | <0.001 | - |
| Changes compared to the second month | 4.4 (2.0 – 6.7) | 1.9 (0.4 – 4.3) | 0.480 |
| P-value (intragroup comparison) | <0.001 | 0.156 | - |
Discussion
MPS is one of the most common musculoskeletal disorders in patients with anterior head deformity (10, 12). MPS is characterized by the presence of trigger points, which is a sensitive area with a taut band. These points are painful when pressed or stretched and cause pain with non-dermatomal and non-myotomy referral patterns and autonomic symptoms (31). In this study, we compared the effectiveness of exercise therapy and electroacupuncture in improving body condition, pain, and quality of life in patients with MPS and FHP. As observed in the previous chapter, after the end of the treatment period, body posture (FHP angles) in patients in the exercise therapy group was significantly better than in the electroacupuncture group. Although patients in both groups reported a significant reduction in pain intensity during the study period, the reduction in pain intensity was greater in the electroacupuncture group than in the exercise therapy group. Both exercise therapy and electroacupuncture significantly improved patients' quality of life.
As in our study, many previous studies have reported the effectiveness of exercise therapy in improving posture, especially CVA correction in patients with a diagnosis of FHP (15, 18, 32, 33). Different studies have published different results on the effectiveness of stretching and strength exercises on CA changes; While a group of studies such as ours showed improvement in CA (18), another group of studies did not report a significant change for CA following exercise therapy (34). The results of a systematic review and meta-analysis of 7 clinical trials involving 627 participants diagnosed with FHP showed that exercise therapy could significantly improve CVA angle and have a moderate and significant effect on neck pain in patients, but Its effect on CA is not significant (25). Exercise therapy, especially strength and stretching exercises, is considered as a non-invasive treatment option to improve pain and function in patients with MPS (35). Exercise therapy in patients with FHP and MPS In this study, in addition to dramatically improving FHP angles. It also improved patients' pain intensity. It seems that exercise therapy reduces the pressure on the muscles by improving the position of the head and neck and therefore reduces the pain intensity of patients.
In the present study, the effect of electroacupuncture on improving patients' pain was more pronounced than its effect on improving their posture. Although CA, CVA, and shoulder angles in patients in this group were statistically significantly better than at baseline, the final CA and CVA were much lower than in the exercise therapy group and showed no clinical correction of FHP angles in patients in this group. In contrast, patients receiving electroacupuncture reported early and dramatic improvement in trigger point pain following treatment, which was more pronounced than in the exercise therapy group. The highest reduction in pain was observed in the first month of the intervention in these patients and the pain intensity in the second and third months after the intervention was not significantly reduced compared to the first month of the intervention. As in our study, the usefulness of electroacupuncture to improve trigger point pain has been demonstrated in a number of other studies (26, 36). Dr. Ismailian et al. At Tabriz University of Medical Sciences, in a clinical trial study comparing the effectiveness of electroacupuncture and biofeedback in improving pain intensity (VAS), neck disability index (NDI), neck range of motion (ROM) and compressive pain threshold (PPT) in Patients with cervical MPS (37). The results of this study showed that electroacupuncture was more successful than biofeedback in improving NDI, VAS, ROM extension and lateral-bending and PPT of the left upper trapezius (37). In our study, the authors of this study reported an early reduction in pain in patients in the electroacupuncture group after 6 sessions of treatment (37). It seems that the release of trigger points and a taut band by inserting a needle in the target points is the basis of the effectiveness of this treatment in patients with neck MPS. In another study conducted by Dr. Eftekharsadat et al. In Tabriz, the effectiveness of aerobic exercise with acupuncture compared to acupuncture alone in improving pain intensity, NDI, PPT and quality of life (SF-36) in patients with MPS was evaluated (38). The results of this study showed that there was no significant difference between the two groups in terms of evaluated variables (38). This finding could mean that the addition of exercise protocol to the treatment of MPS patients has no additive effect in terms of improving pain intensity in these patients.
Conclusion
Overall, the results of this study showed that both exercise therapy and electroacupuncture significantly improved patients' posture, reduced pain intensity, and increased quality of life in FHP patients with MPS; But exercise therapy was more effective in improving FHP angles, and electroacupuncture was more successful in reducing patients' pain intensity.
Authors' contribution
L.M., Z.K., B.A., and M.R.N: conception and design, L.M. and M.R.N: acquisition of data, or analysis and interpretation of data. L.M., Z.K., B.A. and M.R.N: drafting the article or revising it critically for important intellectual content. All authors approved the final version to be submitted for publication.
Ethical approval
This study was ethically approved by the local EthicsCommittee of Hamedan University of MedicalSciences (IR.UMSHA.REC.1399.924).
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as : Majidi L, Kargar Z, Alaei B, Nikoo MR. Comparison of The Effectiveness of Exercise Therapy and Electroacupuncture in Patients with Forward Head Abnormalities and Myofascial Pain Syndrome: A Randomized Clinical Trial. Med J Islam Repub Iran. 2023 (8 Apr);37:34. https://doi.org/10.47176/mjiri.37.34
References
- 1.Gangnet N, Pomero V, Dumas R, Skalli W, Vital JM. Variability of the spine and pelvis location with respect to the gravity line: a three-dimensional stereoradiographic study using a force platform. Surg Radiol Anat. 2003;25(5-6):424. doi: 10.1007/s00276-003-0154-6. [DOI] [PubMed] [Google Scholar]
- 2.Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther. 1992;72(6):425. doi: 10.1093/ptj/72.6.425. [DOI] [PubMed] [Google Scholar]
- 3.Yeganeh M, Baradaran HR, Qorbani M, Moradi Y, Dastgiri S. The effectiveness of acupuncture, acupressure and chiropractic interventions on treatment of chronic nonspecific low back pain in Iran: a systematic review and meta-analysis. Complement Ther Clin Pract. 2017 May 1;27:11. doi: 10.1016/j.ctcp.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 4.Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther. 1992;72(6):425. doi: 10.1093/ptj/72.6.425. [DOI] [PubMed] [Google Scholar]
- 5.Quek J, Pua YH, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther. 2013;18(1):65–71. doi: 10.1016/j.math.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Szeto GP, Straker L, Raine S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl Ergon. 2002;33(1):75–84. doi: 10.1016/s0003-6870(01)00043-6. [DOI] [PubMed] [Google Scholar]
- 7.Vázquez-Delgado E, Cascos-Romero J, Gay-Escoda C. Myofascial pain syndrome associated with trigger points: a literature review. (I): Epidemiology, clinical treatment and etiopathogeny. Med Oral Patol Oral Cir Bucal. 2009;14(10):E494. doi: 10.4317/medoral.14.e494. [DOI] [PubMed] [Google Scholar]
- 8.Desai MJ, Saini V, Saini S. Myofascial pain syndrome: a treatment review. Pain Ther. 2013;2(1):21–36. doi: 10.1007/s40122-013-0006-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lau KT, Cheung KY, Chan KB, Chan MH, Lo KY, Chiu TT. Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man Ther. 2010;15(5):457. doi: 10.1016/j.math.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, Gerwin RD, Pareja JA. Trigger points in the suboccipital muscles and forward head posture in tension-type headache. Headache. 2006;46(3):454. doi: 10.1111/j.1526-4610.2006.00288.x. [DOI] [PubMed] [Google Scholar]
- 11.Armijo-Olivo S, Rappoport K, Fuentes J, Gadotti IC, Major PW, Warren S. et al. Head and cervical posture in patients with temporomandibular disorders. J Orofac Pain. 2011;25(3):199–209. [PubMed] [Google Scholar]
- 12.Fernández-de-Las-Peñas C, Simons D, Cuadrado ML, Pareja J. The role of myofascial trigger points in musculoskeletal pain syndromes of the head and neck. Curr Pain Headache Rep. 2007;11(5):365. doi: 10.1007/s11916-007-0219-z. [DOI] [PubMed] [Google Scholar]
- 13.Abbasi AH, Aslam M, Ashraf T, Malik AN. Evaluation of the Forward Head Posture, its association with Neck Pain & Quality of life of Female DPT Students. J Riphah Coll Rehabili Sci. 2016;4(2):59–64. [Google Scholar]
- 14.Dommerholt J, Grieve R, Hooks T, Layton M. A critical overview of the current myofascial pain literature - October 2015. J Bodyw Mov Ther. 2015;19(4):736. doi: 10.1016/j.jbmt.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an Exercise Program to Improve Forward Head Posture in Normal Adults: A Randomized, Controlled 10-Week Trial. J Man Manip Ther. 2005;13(3):163. [Google Scholar]
- 16.Fathollahnejad K, Letafatkar A, Hadadnezhad M. The effect of manual therapy and stabilizing exercises on forward head and rounded shoulder postures: a six-week intervention with a one-month follow-up study. BMC Musculoskelet Disord. 2019;20(1):86. doi: 10.1186/s12891-019-2438-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miecznikowski W, Kiczmer P, Seńkowska AP, Cygan K, Świętochowska E. Comparison of two methods of cervical spine pain manual therapy using clinical and biochemical pain markers. Med Res J. 2019;4(3):163. [Google Scholar]
- 18.Ruivo RM, Pezarat-Correia P, Carita AI. Effects of a Resistance and Stretching Training Program on Forward Head and Protracted Shoulder Posture in Adolescents. J Manipulative Physiol Ther. 2017;40(1):1–10. doi: 10.1016/j.jmpt.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br J Sports Med. 2010;44(5):376. doi: 10.1136/bjsm.2009.066837. [DOI] [PubMed] [Google Scholar]
- 20.Yuan Q-L, Wang P, Liu L, Sun F, Cai YS, Wu WT. et al. Acupuncture for musculoskeletal pain: A meta-analysis and meta-regression of sham-controlled randomized clinical trials. Sci Rep. 2016;6:30675. doi: 10.1038/srep30675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pomeranz B, Berman B. Scientific basis of acupuncture. Basics of acupuncture: Springer; 2003
- 22.Wang TQ, Li YT, Wang LQ, Shi GX, Tu JF, Yang JW. et al. Electroacupuncture versus manual acupuncture for knee osteoarthritis: a randomized controlled pilot trial. Acupunct Med. 2020;38(5):291–300. doi: 10.1177/0964528419900781. [DOI] [PubMed] [Google Scholar]
- 23.Zhang R, Lao L, Ren K, Berman BM. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. 2014;120(2):482–503. doi: 10.1097/ALN.0000000000000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65(4):653. [PubMed] [Google Scholar]
- 25.Sheikhhoseini R, Shahrbanian S, Sayyadi P, O'Sullivan K. Effectiveness of Therapeutic Exercise on Forward Head Posture: A Systematic Review and Meta-analysis. J Manipulative Physiol Ther. 2018;41(6):530. doi: 10.1016/j.jmpt.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 26.Aranha MF, Alves MC, Bérzin F, Gavião MB. Efficacy of electroacupuncture for myofascial pain in the upper trapezius muscle: a case series. Revista brasileira de fisioterapia (Sao Carlos (Sao Paulo, Brazil)) 2011;15(5):371. doi: 10.1590/s1413-35552011005000022. [DOI] [PubMed] [Google Scholar]
- 27.Campa-Moran I, Rey-Gudin E, Fernández-Carnero J, Paris-Alemany A, Gil-Martinez A, Lerma Lara. et al. Comparison of Dry Needling versus Orthopedic Manual Therapy in Patients with Myofascial Chronic Neck Pain: A Single-Blind, Randomized Pilot Study. Pain Res Treat. 2015;2015:327307. doi: 10.1155/2015/327307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim J, Kim S, Shim J, Kim H, Moon S, Lee N. et al. Effects of McKenzie exercise, Kinesio taping, and myofascial release on the forward head posture. J Phys Ther Sci. 2018;30(8):1103. doi: 10.1589/jpts.30.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Travell JG, Simons DG. Lippincott Williams & Wilkins;; 1983. Myofascial pain and dysfunction: the trigger point manual. [Google Scholar]
- 30.Gerwin RD, Shannon S, Hong C-Z, Hubbard D, Gevirtz R. Interrater reliability in myofascial trigger point examination. Pain. 1997;69(1-2):65–73. doi: 10.1016/s0304-3959(96)03248-4. [DOI] [PubMed] [Google Scholar]
- 31.Gerwin RD. Classification, epidemiology, and natural history of myofascial pain syndrome. Curr Pain Headache Rep. 2001;5(5):412. doi: 10.1007/s11916-001-0052-8. [DOI] [PubMed] [Google Scholar]
- 32.Lee SM, Lee CH, O'Sullivan D, Jung JH, Park JJ. Clinical effectiveness of a Pilates treatment for forward head posture. J Phys Ther Sci. 2016;28(7):2009. doi: 10.1589/jpts.28.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seidi F, Rajabi R, Ebrahimi I, Alizadeh MH, Minoonejad H. The efficiency of corrective exercise interventions on thoracic hyper-kyphosis angle. J Back Musculoskelet Rehabil. 2014;27(1):7–16. doi: 10.3233/BMR-130411. [DOI] [PubMed] [Google Scholar]
- 34.Mulet M, Decker KL, Look JO, Lenton PA, Schiffman EL. A randomized clinical trial assessing the efficacy of adding 6 x 6 exercises to self-care for the treatment of masticatory myofascial pain. J Orofac Pain. 2007;21(4):318. [PubMed] [Google Scholar]
- 35.Mata Diz, de Souza, Leopoldino AAO, Oliveira VC. Exercise, especially combined stretching and strengthening exercise, reduces myofascial pain: a systematic review. J Physiother. 2017;63(1):17–22. doi: 10.1016/j.jphys.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 36.Aranha MFM, Müller CEE, Gavião MBD. Pain intensity and cervical range of motion in women with myofascial pain treated with acupuncture and electroacupuncture: a double-blinded, randomized clinical trial. Braz J Phys Ther. 2015;19(1):34–43. doi: 10.1590/bjpt-rbf.2014.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eslamian F, Jahanjoo F, Dolatkhah N, Pishgahi A, Pirani A. Relative Effectiveness of Electroacupuncture and Biofeedback in the Treatment of Neck and Upper Back Myofascial Pain: A Randomized Clinical Trial. Arch Phys Med Rehabil. 2020;101(5):770. doi: 10.1016/j.apmr.2019.12.009. [DOI] [PubMed] [Google Scholar]
- 38.Eftekharsadat B, Porjafar E, Eslamian F, Shakouri SK, Fadavi HR, Raeissadat SA. et al. Combination of Exercise and Acupuncture Versus Acupuncture Alone for Treatment of Myofascial Pain Syndrome: A Randomized Clinical Trial. J Acupunct Meridian Stud. 2018;11(5):315. doi: 10.1016/j.jams.2018.04.006. [DOI] [PubMed] [Google Scholar]


