Abstract
The cognitive abilities of older persons vary greatly, even among those with similar amounts of Alzheimer disease (AD) pathology, suggesting differences in neural reserve. Although its neurobiologic basis is not well understood, reserve may reflect differences in the ability to compensate for the deleterious effects of pathology by recruiting alternative or additional brain networks to perform a specific task. If this is an effective compensatory strategy, then involvement of additional cognitive systems may help maintain function in other cognitive systems despite the accumulation of pathology.
Objective: We tested the hypothesis that processing resources, specifically perceptual speed and working memory, modify the associations of AD pathology with other cognitive systems.
Method: A total of 103 older participants of the Rush Memory and Aging Project underwent detailed annual clinical evaluations and brain autopsy. Five cognitive systems including perceptual speed, working memory, semantic memory, visuospatial abilities, and episodic memory were assessed proximate to death, and AD pathology including tau tangles and amyloid load were quantified postmortem.
Results: In multiple regression models adjusted for age, sex, and education, processing resources reduced the associations of tangles with other cognitive systems, such that persons with higher levels of perceptual speed and working memory performed better on semantic memory and visuospatial abilities despite the burden of tangles. Perceptual speed also reduced the associations of amyloid with semantic memory, visuospatial abilities, and episodic memory.
Conclusion: These findings suggest that processing resources may help compensate for the deleterious effects of Alzheimer disease pathology on other cognitive systems in older persons.
The concept of reserve applies to many physiologic systems and is an important determinant of health outcomes. Reserve also applies to brain function, including cognition.1 Numerous clinical-pathologic studies of older persons have reported only modest associations between the degree of neuropathology and the level of impairment prior to death.2–5 Many persons without clinical dementia meet pathologic criteria for Alzheimer disease (AD)2,3 and AD pathology is frequently observed in persons known to have had only mild or no cognitive impairment prior to death,5–8 suggesting that some form of reserve protects the brain from expressing pathology as impairment or clinically evident disease.1
The neurobiologic basis of reserve is not well understood. Neural reserve may reflect differences in brain reserve capacity or the threshold of susceptibility to pathology.9 Thus, persons with larger brains or more neurons or synapses may be able to withstand a greater amount of pathology prior to the manifestation of cognitive impairment. A related idea is that neural reserve reflects differences in the ability of the brain to actively respond to challenges.1,10–13 For example, there may be differences in neural efficiency, such that some persons have highly efficient and flexible neural networks that are less susceptible to disruption from pathology. Alternatively, there may be differences in the ways in which brains compensate in response to pathology. The compensation hypothesis10,11 posits that some persons actively recruit alternative or additional neural networks not normally involved in a specific task to compensate for the disruption of other networks by pathology. In prior work from our group using this and another cohort, we identified several factors that modified the relation of AD pathology to cognition, consistent with this hypothesis12,13 (e.g., education and social networks).
There is reason to think that some cognitive systems, such as processing resources, may also alter the relation of AD pathology to other cognitive systems. Cognitive function reflects the output of several relatively dissociable neural networks that subserve different aspects of cognition. Whereas some cognitive systems are relatively functionally and neuroanatomically specific, others are required for multiple cognitive functions and are subserved by widely distributed neural networks.14 If recruitment of alternative or additional brain networks is an effective compensatory mechanism, then the recruitment of alternative or additional cognitive systems may help compensate for the deleterious effects of pathology on other cognitive systems. For example, processing resources such as perceptual speed and working memory enhance virtually all other cognitive systems and reflect the output of extensive neural networks.15–17 Processing resources therefore may buffer or reduce the negative effect of pathology on other systems. Although processing resources are considered an important determinant of cognitive aging,16–19 we are not aware of any prior study that has examined whether processing resources provide a compensatory benefit by altering the association of pathology with other cognitive systems. We used data from the Rush Memory and Aging Project,20 a large longitudinal clinical-pathologic investigation of common conditions of old age, to test the hypothesis that processing resources modify the association of AD pathology with other cognitive systems.
METHODS
Participants and procedures.
Participants were from the Rush Memory and Aging Project,20 an ongoing longitudinal clinical-pathologic study of common chronic conditions of old age. Participants were recruited from approximately 40 senior residential facilities and social service agencies throughout the Chicago metropolitan area and provided written informed consent in accordance with the Declaration of Helsinki and an anatomic gift act. The study was approved by the Institutional Review Board of Rush University Medical Center. More than 1,100 persons have completed the baseline clinical assessment. The overall annual follow-up rate of survivors exceeds 90% and the autopsy rate exceeds 85%. These analyses were based on the first 103 persons (38 without cognitive impairment, 36 with mild cognitive impairment, and 29 with AD) for whom postmortem data were available.
All participants underwent structured clinical assessments including medical history interviews, neurologic examination, and neuropsychological assessment, as previously described.20–22 Annual follow-up assessments were identical in all essential details to the baseline and were conducted by examiners shielded to previously collected data.
Assessment of cognitive function.
Cognitive function was assessed via a battery of 21 tests, as previously described. 20,23 Scores on 19 tests were used to create summary indices of the following five specific cognitive domains: episodic memory, semantic memory, working memory, perceptual speed, and visuospatial ability. The cognitive tests were grouped, a priori, to represent five cognitive systems. We then conducted a factor analysis with varimax rotation of the 19 tests. Loadings of 0.50 or greater were assigned to a group. The relations between the hypothesized groupings and the empirically derived groupings were examined using the Rand statistic.24 Our data yielded a Rand statistic of 0.79 (p < 0.001), indicating a good fit consistent with the hypothesized cognitive systems. Next, in order to combine the scores from different tests, we converted the raw scores on each of the tests to z-scores using the baseline mean and SD of the entire cohort and averaged the z-scores of tests within a given system to yield a domain score.
Neuropathologic evaluation.
Brains were removed in standard fashion and cut coronally using a Plexiglas jig into 1-cm slabs, as previously described.12,13,20 Slabs from one hemisphere were fixed in 4% paraformaldehyde for 72 hours. Multiple tissue blocks from entorhinal cortex proper, hippocampus (CA1/subiculum), superior frontal cortex, dorsolateral prefrontal cortex, inferior temporal cortex, angular gyrus cortex, anterior cingulate cortex, and calcarine cortex were embedded in paraffin and cut into 20 μm sections. Amyloid-β was labeled with an N-terminus directed monoclonal antibody (10D5, courtesy Elan Pharmaceuticals; 1:1,000), and immunohistochemistry was performed as previously described.12,13 PHF tau was labeled with an antibody specific for phosphorylated tau, AT8 (Innogenetics, San Ramon, CA, 1:1,000). Quantification of amyloid-β load was done via an automated, multistage computational image analysis protocol that uses an algorithm with the addition of a defective pixel removal procedure to exclude faulty pixels, as previously described.12,13 Mean fraction (% area) per region and per subject were computed. Quantification of tangle density per mm2 was performed, as previously described.12,13
Hypothesis testing required the use of continuous quantitative measures of amyloid and tangles with adequate metric properties. Thus, for these analyses, we used composite measures which were computed by averaging the amyloid measures and the tangle counts across all regions. The approach is supported by Cronbach coefficient α, factor analysis, and intercorrelations, as described previously in this and another cohort.12,13
Statistical analysis.
We first examined the simple associations of the measures of AD pathology with cognitive function via linear regression analyses; these and all subsequent models controlled for age, sex, and education. Next, multiple regression analyses were used to test examine whether perceptual speed and working memory modified the associations of AD pathology with the other cognitive systems. The initial models included terms for the main effects of the relevant measure of AD pathology and perceptual speed or working memory, respectively. Then, to explicitly test the hypothesis that perceptual speed and working memory modify (or, more specifically, reduce) the associations of AD pathology with other cognitive systems, we repeated the initial models with additional terms for the interaction of each processing resource measure with the relevant measure of AD pathology. In these tests of effect modification,25 the interaction term directly examines the extent to which a unit increase in the processing resource reduces the effect of a unit of pathology on the level of function in another cognitive system; thus, interaction terms are the primary focus of the results. In secondary analyses, we examined the extent to which the other cognitive systems modified the associations of AD pathology with each other and with the processing resource measures. Unadjusted regression coefficients are presented in data tables. Models were validated graphically and analytically and analyses were carried out using SAS/STAT software version 8.26
RESULTS
The mean age of participants was about 87 years at the time of death, and the sample was predominantly female, white, and non-Hispanic (table 1). The average interval from the last clinical interview to autopsy was 6.8 months (SD = 4.2). The mean amyloid load was 3.7% (SD = 4.2) and the mean number of neurofibrillary tangles per mm2 was 6.4 (SD = 8.2).
Table 1 Sample characteristics of deceased participants

Associations of AD pathology with cognitive function.
We first examined the associations of AD pathology with the level of function in the cognitive systems that serve as the outcomes in our core models; these and all subsequent models controlled for age, sex, and education. In separate linear regression models, a greater burden of tangle and amyloid pathology was associated with a lower level semantic memory (for tangles = −0.082, p < 0.001, for amyloid = −0.063, p = 0.028) and episodic memory (for tangles = −0.096, p < 0.001, for amyloid = −0.063, p = 0.002). A greater burden of tangle pathology was associated with a lower level of visuospatial abilities (= −0.053, p < 0.001) but the association of amyloid with visuospatial abilities was not significant (= −0.021, p = 0.464).
Does perceptual speed modify the associations of AD pathology with other cognitive systems?
We constructed a series of models to examine cognition as a function of each measure of AD pathology and perceptual speed. For these analyses, we first examined the main effects of the relevant measure of pathology and perceptual speed, and subsequently added a term for their interaction. The interaction term directly examines the extent to which a unit increase in perceptual speed reduces the effect of a unit of pathology on the level of function in the cognitive system. Semantic memory was the outcome in the first analysis. In the initial model, each tangle per mm2 was associated with about a 0.04 (p < 0.001) unit lower semantic memory score, and each unit increase in perceptual speed was associated with about a 0.6 (p < 0.001) unit increase in semantic memory (table 2, semantic memory, model 1, tangles). We then added a term for the interaction of tangles with perceptual speed. In this model, the effect of each tangle on the level of semantic memory was reduced by about 50% (p = 0.023) for a one unit increase in perceptual speed (table 2, semantic memory, model 2, tangles). Next, we repeated the models above but replaced tangles with amyloid. In the initial model, each 1% increase in amyloid was associated with about a 0.04 (p = 0.065) unit lower semantic memory score, and each unit increase in perceptual speed was associated with about a 0.7 (p < 0.001) unit increase in semantic memory (table 2, semantic memory, model 1, amyloid). In the model with the additional interaction term, the effect of a percent increase in amyloid on the level of semantic memory was reduced by more than 100% (p = 0.006) for a one unit increase in perceptual speed (table 2, semantic memory, model 2, amyloid). These findings suggest that perceptual speed reduces the association of tangles and amyloid with semantic memory, such that persons with higher levels of perceptual speed function better on semantic memory despite the burden of AD pathology.
Table 2 Cognitive performance as a function of Alzheimer disease pathology, perceptual speed, and their interactions
A similar series of analyses was conducted with visuospatial abilities as the outcome. In the first model, each tangle was associated with about a 0.02 (p = 0.089) unit lower visuospatial ability score, and perceptual speed was associated with about a 0.5 (p < 0.001) unit increase in visuospatial abilities (table 2, visuospatial abilities model 1, tangles). In the model with the additional interaction term, the effect of each tangle on level of visuospatial abilities was reduced by more than 100% (p < 0.001) for a one unit increase in perceptual speed (table 2, visuospatial abilities, model 2, tangles). The corresponding models for amyloid are also presented in table 2. Although the interaction term with amyloid also was significant (p = 0.010), the finding must be interpreted with caution since the basic association of amyloid with visuospatial abilities was not significant.
Finally, we repeated these analyses with episodic memory as the outcome. Each tangle was associated with about a 0.07 (p < 0.001) unit lower episodic memory score, and each unit increase in perceptual speed was associated with about a 0.4 (p < 0.001) unit increase in episodic memory (table 2, episodic memory, model 1, tangles). However, the interaction of tangles with perceptual speed was not significant (table 2, episodic memory, model 2, tangles). In the initial corresponding model for amyloid, each 1% increase in amyloid was associated with about a 0.09 (p < 0.001) unit lower episodic memory score and each unit increase in perceptual speed was associated with about a 0.6 (p < 0.001) unit increase in episodic memory (table 2, episodic memory, model 1, amyloid). In the model with the additional interaction term, the effect of a percent increase in amyloid on the level of episodic memory was reduced by about 50% (p = 0.009) for a one unit increase in perceptual speed (table 2, episodic memory, model 2, amyloid).
Does working memory modify the associations of AD pathology with other cognitive systems?
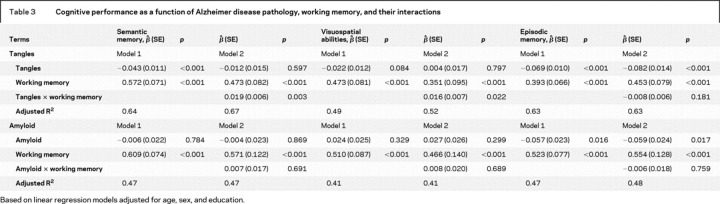
To test the hypothesis that working memory may also modify the association of AD pathology with other cognitive systems, we repeated the models above but replaced perceptual speed with working memory. Notably, the interaction model showed that the effect of each tangle on the level of semantic memory was reduced by about 50% (p = 0.003) for a one unit increase in working memory (table 3, semantic memory, model 2, tangles), suggesting that persons with higher levels of working memory perform better on semantic memory despite the burden of tangles. No such effect was found for amyloid.
Table 3 Cognitive performance as a function of Alzheimer disease pathology, working memory, and their interactions
When examining visuospatial abilities as the outcome, the interaction model showed that effect of each tangle on the level of visuospatial abilities was reduced by about 75% (p = 0.022) for a one unit increase in working memory (table 3, visuospatial abilities, model 2, tangles). The corresponding model for amyloid is presented in table 3 but should be interpreted with caution since the basic association of amyloid with visuospatial abilities was not significant.
Finally, in the models with episodic memory as the outcome (table 3, episodic memory, model 1, tangles and amyloid), the interactions of working memory with tangles and amyloid were not significant (table 3, episodic memory, model 2, tangles and amyloid).
Examining the effects for other cognitive systems.
In order to determine whether the findings were specific for processing resources or reflected more general associations between cognitive systems, we next examined whether the level of function in semantic memory, visuospatial abilities, and episodic memory modified the associations of AD pathology with each other and with processing resources (table 4). Episodic memory reduced the associations of tangles with semantic memory (p < 0.001), visuospatial abilities (p < 0.001), and working memory (p = 0.002), and amyloid with semantic memory (p < 0.001). By contrast, semantic memory and visuospatial abilities did not reduce the associations of tangles or amyloid with each other or with the processing resources.
Table 4 Cognitive performance as a function of the interactions of Alzheimer disease pathology with episodic memory, semantic memory and visuospatial abilities
Additional analyses.
Because the measures of AD pathology were skewed and we were concerned about the potential influence of outliers, we conducted several secondary analyses to further examine the robustness of these findings. First, we repeated all models using a square-root transformation of the pathology variables. Second, we repeated all models after excluding those persons with the top 2.5%, 5%, and 10%, respectively, of values on each of the pathology measures. The main findings persisted in both sets of analyses and estimates were essentially unchanged (data not shown).
DISCUSSION
In more than 100 well-characterized older persons in whom multiple cognitive abilities were assessed proximate to death and AD pathology was quantified postmortem, we found that processing resources modified the associations of AD pathology with other cognitive systems. Specifically, perceptual speed and working memory reduced the associations of tangles with semantic memory and visuospatial abilities. Perceptual speed also reduced the associations of amyloid with semantic memory, visuospatial abilities, and episodic memory. In secondary analyses, episodic memory reduced the associations of tangles with semantic memory, visuospatial abilities, and working memory, and amyloid with semantic memory. These findings suggest that processing resources and, to some degree, episodic memory help compensate for the deleterious effects of AD pathology in older persons by reducing the effect of pathology, especially neurofibrillary tangles, on other cognitive systems.
It is widely recognized that the modest association between the degree of neuropathology and the level of cognitive impairment suggests individual differences in neural reserve.2–5 Neural reserve may reflect the threshold of susceptibility to injury, the ability to use pre-existing neural networks efficiently, or the ability of the brain to actively compensate for pathology by recruiting alternative or additional neural networks to perform a specific task.9–13,27,28 Support for a compensatory response comes from neuroimaging studies which have shown that older persons activate larger brain volumes than younger persons to perform cognitive tasks.29–31 Often, the degree of brain activation is related to task proficiency,13,28,31–33 suggesting that increased activation is associated with maintenance of cognitive function. Activation of regions not typically involved in a task may represent a functional reorganization of the brain in an attempt to compensate in response to pathology.
Importantly, although neuroimaging data provide strong evidence of a potential compensatory response, neuropathology cannot yet be directly measured via neuroimaging. Clinical-pathologic studies have the potential to complement imaging studies by examining whether involvement of alternative functional neural systems promotes maintenance of cognitive function as pathology accumulates. We are unaware of any prior study that has attempted to examine neural reserve in this manner. Our hypothesis was that processing resources, which are integral to most other cognitive functions and reflect the output of distributed brain networks, reduce the association of AD pathology with other cognitive systems. Processing resources are considered an important determinant of cognitive aging.16–18,34–36 Perceptual speed refers to the speed with which mental comparisons are made, and working memory involves the ability to hold and manipulate information in short-term memory stores.15,17,18,34–36 Both are essential for information processing and are considered indicators of mental capacity.19,34,36 We suspect that processing resources optimize other cognitive systems because they promote efficient information transfer and reduce demand on other systems. Additionally, processing resources appear to rely on complex brain networks that involve multiple brain regions.14,34–36 Processing resources therefore may be available to support function in other systems that have been compromised by pathology.
In addition to processing resources, we also found that episodic memory reduced the association of AD pathology with semantic memory, visuospatial abilities, and working memory. Some data suggest that episodic memory may support other cognitive functions.14,37 Our findings may suggest that it provides compensatory benefit when preserved.
Notably, the beneficial effects of processing resources and episodic memory were most evident in analyses with tangles as compared to amyloid. Tangles are more strongly associated with cognitive function,38 and the modifying effects may have been greatest for tangles for this reason. We have found similar dissociations with other factors that modify the associations of amyloid but not tangles with cognition in a separate cohort.13 In addition, it is possible that the temporal and regional pattern of the progression of AD pathology affects the extent to which specific cognitive systems are able to provide compensatory benefit in the face of accumulating pathology. AD pathology is thought to begin in the mesial temporal region and affect the neocortex later. Thus, semantic memory and visuospatial abilities, primarily subserved by domain-specific neocortical association areas, are relatively less profoundly affected by AD pathology and may be more amenable to facilitation by a higher level of processing resources, particularly early in the disease. By contrast, the hippocampal formation, a small region highly vulnerable to AD pathology early in the disease, is critical to the formation of episodic memory and may be less amenable to facilitation by processing resources once compromised. Future studies that compare persons with differing degrees of cognitive impairment or across diagnostic groups may provide important information regarding how the regional and temporal progression of AD pathology affects neural reserve. In addition, it will be important to further examine how other AD-related pathologic changes and diverse pathologies that degrade cognitive function in aging influence reserve.
Although the results of this study are consistent with compensation, this may not be the only mechanism by which processing resources are linked to neural reserve. Persons with greater processing resources may benefit from a higher threshold of brain reserve capacity and have more efficient neural networks, which may increase their ability to maintain function despite pathology. It is difficult to directly study the neurobiologic basis of reserve, as the factors that contribute to reserve are not mutually exclusive. In addition, processing resources themselves are considered indicators of fluid ability.39 Although we did not directly assess fluid ability in this study, if we reconceptualize processing resources as indicators of fluid ability in the present study and semantic memory resources as indicators of crystallized ability, then our data suggest that fluid ability serves as a better modifier of the effect of AD pathology on other cognitive systems than crystallized ability. Thus, processing resources or fluid ability may show greater plasticity and offer particular compensatory benefit in response to the accumulation of AD pathology in aging. Most notably, however, our findings support those of imaging studies in which recruitment of additional brain regions is associated with maintenance of cognitive function and suggest that some form of compensation also works at the level of the cognitive systems.
This study has several strengths, including the linking of quantitative measures of AD pathology with cognition proximate to death in more than 100 well-characterized community-based persons. In addition, data come from a single cohort with high rates of follow-up and autopsy, and uniform structured procedures were followed with blinding of postmortem data to clinical data.
ACKNOWLEDGMENT
The authors thank the Illinois residents from the following facilities for participating in the Memory and Aging Project: Fairview Village, Downers Grove; The Holmstead, Batavia; Covenant Village, Northbrook; Wyndemere, Wheaton; Francis Manor, Des Plaines; Friendship Village, Schaumberg; Peace Village, Palos Park; Washington Jane Smith, Chicago; Garden House Apartments, Calumet City; Victorian Village, Homer Glen; King Bruwaert, Burr Ridge, The Breakers of Edgewater; The Imperial, Chicago; Victory Lakes, Lindenhurst; Windsor Park Manor, Carol Stream; Fanciscan Village, Lemont; Renaissance, Chicago; Alden of Waterford, Aurora; Elgin Housing Authority; The Oaks, Oak Park; Bethlehem Woods, LaGrange Park; Luther Village, Arlington Heights; St. Paul's Home, Chicago; Marion Village, Home Glen; Holland Home, South Holland; Village Woods, Crete; Laurence Manor, Matteson; Trinity, Chicago; St. Andrew's Phoenix, Phoenix; The Moorings, Arlington Heights; Mayslake, Oak Brook; The Birches, Clarendon Hills; Cedar Village, Arlington Heights; Kingston Manor, Chicago; Community Renewal Senior Ministry, Chicago; and the residents of the Chicago metropolitan area. The authors also thank Traci Colvin, MPH, Tracy Hagman, and Tracy Nowakowski for study coordination, Pam Smith, Barbara Eubeler, Karen Lowe Graham, and Mary Futrell for study recruitment, George Dombrowski and Greg Klein for data management, Zhaotai Cui for statistical programming, and the staff of the Rush AD Center.
Glossary
- AD
Alzheimer disease.
Footnotes

e-Pub ahead of print on March 19, 2008, at www.neurology.org.
Supported by National Institute on Aging grants R01AG17917 and K23 AG23040.
Disclosure: The authors report no conflicts of interest.
Received July 23, 2007. Accepted in final form December 5, 2007.
REFERENCES
- 1.Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc 2002;8:448–460. [PubMed] [Google Scholar]
- 2.Katzman R, Terry R, DeTeresa R, et al. Clinical, pathological, and neurochemical changes in dementia: a subgroup with preserved mental status and numerous neocortical plaques. Ann Neurol 1988;23:138–141. [DOI] [PubMed] [Google Scholar]
- 3.Crystal HA, Dickson DW, Sliwinski MJ, et al. Pathological markers associated with normal aging and dementia in the elderly. Ann Neurol 1993;34:566–573. [DOI] [PubMed] [Google Scholar]
- 4.Riley KP, Snowdon DA, Markesbery WR. Alzheimer's neurofibrillary pathology and the spectrum of cognitive function: findings from the Nun Study. Ann Neurol 2002;51:567–577. [DOI] [PubMed] [Google Scholar]
- 5.Knopman DS, Parisi JE, Salviati A, et al. Neuropathology of cognitively normal elderly. J Neuropathol Exp Neurol 2003;62:1087–1095. [DOI] [PubMed] [Google Scholar]
- 6.Hulette CM, Welsh-Bohmer KA, Murray MG, et al. Neuropathological and neuropsychological changes in “normal” aging: evidence for preclinical Alzheimer disease in cognitively normal individuals. J Neuropathol Exp Neurol 1998;57:1168–1174. [DOI] [PubMed] [Google Scholar]
- 7.Petersen RC, Pareisi JE, Dickson DW, et al. Neuropathologic features of amnestic mild cognitive impairment. Arch Neurol 2006;63:665–672. [DOI] [PubMed] [Google Scholar]
- 8.Bennett DA, Schneider JA, Arvanitakis Z, et al. Neuropathology of older persons without cognitive impairment from two community-based studies. Neurology 2006;66:1837–1844. [DOI] [PubMed] [Google Scholar]
- 9.Satz P. Brain reserve capacity and symptom onset after brain injury: a formulation and review of evidence for threshold theory. Neuropsychology 1993;7:273–295. [Google Scholar]
- 10.Cabeza R, McIntosh AR, Tulvinv E, et al. Age-related differences in effective neural connectivity during encoding and recall. Neuroreport 1997;8:3479–3483. [DOI] [PubMed] [Google Scholar]
- 11.Cabeza R, Anderson ND, Locantore JK, McIntosh AR. Aging gracefully: compensatory brain activity in high-performing older adults. NeuroImage 2002;17:1394–1402. [DOI] [PubMed] [Google Scholar]
- 12.Bennett DA, Schneider JA, Tang Y, et al. The effect of social networks on the relation between Alzheimer's disease pathology and level of cognitive function in old people: a longitudinal cohort study. Lancet Neurol 2006;5:406–412. [DOI] [PubMed] [Google Scholar]
- 13.Bennett DA, Schneider JA, Wilson RS, et al. Education modifies the association of amyloid but not tangles with cognitive function. Neurology 2005;65:953–955. [DOI] [PubMed] [Google Scholar]
- 14.Cabeza R, Nyberg L. Imaging cognition II: an empirical review of 275 PET and fMRI studies. J Cogn Neurosci 2000;2:1047. [DOI] [PubMed] [Google Scholar]
- 15.Baddley A. Working Memory. New York: Oxford University Press; 1986. [Google Scholar]
- 16.Salthouse T. Resource-reduction interpretation of cognitive aging. Dev Rev 1998;8:238–272.
- 17.Salthouse T. The role of processing resources in cognitive aging. In: Howe ML, Brainerd CJ, eds. Cognitive Development in Adulthood. New York: Springer-Verlag; 1998: 185–239. [Google Scholar]
- 18.Salthouse T. Aging and measures of processing speed. Biol Psychol 2000;54:35–54. [DOI] [PubMed] [Google Scholar]
- 19.Deary IJ, Bastin ME, Pattie A, et al. White matter integrity and cognition in childhood and old age. Neurology 2006;66:505–512. [DOI] [PubMed] [Google Scholar]
- 20.Bennett DA, Schneider JA, Buchman AS, et al. The Rush Memory and Aging Project: study design and baseline characteristics of the study cohort. Neuroepidemiology 2005;25:163–175. [DOI] [PubMed] [Google Scholar]
- 21.Bennett DA, Schneider JA, Aggarwal NT, et al. Decision rules guiding the clinical diagnosis of Alzheimer's disease in two community-based cohort studies compared to standard practice in a clinic-based cohort study. Neuroepidemiology 2006;27:169–176. [DOI] [PubMed] [Google Scholar]
- 22.McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer's disease: Report of the NINCDS/ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology 1984;34:939–944. [DOI] [PubMed] [Google Scholar]
- 23.Wilson RS, Barnes LL, Krueger KR, et al. Early and late-life cognitive activity and cognitive systems in old age. JINS 2005;11:400–407. [PubMed] [Google Scholar]
- 24.Rand WM. Objective criteria for the evaluation of clustering methods. J Am Stat Assoc 1971;66:846–850. [Google Scholar]
- 25.Hennekens CH, Buring JE. Epidemiology in Medicine. Boston: Little, Brown; 1987. [Google Scholar]
- 26.SAS Institute Inc. SAS/STAT User's Guide, Version 8. Cary, NC: SAS Institute Inc., 2000. [Google Scholar]
- 27.Cabeza R, Grady CL, Nyberg L, et al. Age-related differences in neural activity during memory encoding and retrieval: a positron emission tomography study. J Neurosci 1997;17:391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reuter-Lorenz PA, Stanczak L, Miller AC. Neural recruitment and cognitive aging: Two hemispheres are better than one, especially as you age. Psychol Sci 1999;10:494–500. [Google Scholar]
- 29.McIntosh AR, Sekuler AB, Penpeci C, et al. Recruitment of unique neural systems to support visual memory in normal aging. Curr Biol 1999;9:1275–1278. [DOI] [PubMed]
- 30.Grady CL, McIntosh AR, Beig S, et al. Evidence from functional neuroimaging of a compensatory prefrontal network in Alzheimer's disease. J Neurosci 2003;23:986–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cabeza R. Hemispheric asymmetry reduction in old adults: The HAROLD model. Psychol Aging 2002;17:85–100. [DOI] [PubMed] [Google Scholar]
- 32.Marcom AM, Good CD, Frackowiak RS, Rugg MD. Age effects on the neural correlates of successful memory encoding. Brain 2003;126:213–229. [DOI] [PubMed] [Google Scholar]
- 33.Stern Y, Habeck C, Moeller, et al. Brain networks associated with cognitive reserve in healthy young and old adults. Cereb Cortex 2005;15:394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salthouse T. The processing-speed theory of adult age differences in cognition. Psychol Rev 1996;103:403–428. [DOI] [PubMed] [Google Scholar]
- 35.Earles JA, Kersten AW. Processing speed and adult age differences in activity memory. Exp Aging Res 1999;25:243–253. [DOI] [PubMed] [Google Scholar]
- 36.Kail R, Salthouse TA. Processing speed as a mental capacity. Acta Psychol 1994;86:199–225. [DOI] [PubMed] [Google Scholar]
- 37.Piccinin AM, Rabbitt PM. Contribution of cognitive abilities to performance and improvement on a substitution coding task. Psychol Aging 1999;14:539–551. [DOI] [PubMed] [Google Scholar]
- 38.Giannakopoulos P, Herrmann FR, Bussire T, et al. Tangle and neuron numbers, but not amyloid load, predict cognitive status in Alzheimer's disease. Neurology 2003;60:1495–1500. [DOI] [PubMed] [Google Scholar]
- 39.Salthouse T, Davis HP. Organization of cognitive abilities and neuropsychological variables across the lifespan. Dev Rev 2006;26:31–54. [Google Scholar]