Abstract
Microglia are the main human immunodeficiency virus (HIV) reservoir in the central nervous system and most likely play a major role in the development of HIV dementia (HIVD). To characterize human adult microglial chemokine receptors, we analyzed the expression and calcium signaling of CCR5, CCR3, and CXCR4 and their roles in HIV entry. Microglia expressed higher levels of CCR5 than of either CCR3 or CXCR4. Of these three chemokine receptors, only CCR5 and CXCR4 were able to transduce a signal in microglia in response to their respective ligands, MIP-1β and SDF-1α, as recorded by single-cell calcium flux experiments. We also found that CCR5 is the predominant coreceptor used for infection of human adult microglia by the HIV type 1 dementia isolates HIV-1DS-br, HIV-1RC-br, and HIV-1YU-2, since the anti-CCR5 antibody 2D7 was able to dramatically inhibit microglial infection by both wild-type and single-round luciferase pseudotype reporter viruses. Anti-CCR3 (7B11) and anti-CXCR4 (12G5) antibodies had little or no effect on infection. Last, we found that virus pseudotyped with the DS-br and RC-br envelopes can infect cells transfected with CD4 in conjunction with the G-protein-coupled receptors APJ, CCR8, and GPR15, which have been previously implicated in HIV entry.
Human immunodeficiency virus (HIV) dementia (HIVD) is a central nervous system (CNS) complication that affects 20 to 30% of individuals infected with HIV and is a defining condition for AIDS (24). The underlying cause of HIVD is unknown, but since productive HIV infection in the CNS occurs mostly in microglia, or brain macrophages, it is generally thought that these cells play a key role in the development of neurological abnormalities. HIVD might then be caused by neuronal damage or dysfunction resulting from the release of putative neurotoxic products by infected microglia or, alternatively, by neuronal interaction with viral proteins released or expressed by the infected cells.
The propensity for certain viral isolates to infect the CNS and mediate neuronal damage is one of the major unanswered questions of HIVD. A proportion of HIV isolates replicate in cultured microglia (44), resulting in prominent syncytial formation, which is an important signature of HIV replication in the CNS (39). This cytopathology is presumably the result of membrane fusion between microglia mediated by HIVD envelope proteins.
Cellular entry by HIV is now known to require at least two cell membrane proteins, CD4, and one of several seven-transmembrane domain G-protein-coupled receptors (GPCRs), principally CXCR4, an α-chemokine receptor, and CCR5, whose natural ligands are β-chemokines (7). CXCR4 mediates infection of T-tropic HIV strains, i.e., those, that replicate in T-cell lines, whereas CCR5 is the most important coreceptor for M-tropic strains, which replicate both in monocyte-derived macrophages (MDM) and in microglia. Studies with cultured fetal and adult microglia have shown that CCR5 is sufficient for HIV entry (19, 43). The role of CCR3, another β-chemokine receptor, is more controversial. Several HIVD isolates isolated from the CNS can use CCR3 to enter cells dually transfected with CCR3 and CD4 and to enter fetal microglia, which express CCR3 on their cell surface. However, studies that examined the inhibition of microglial infection by anti-CCR3 antibodies or the CCR3 ligand eotaxin have yielded conflicting results (16, 19). Microglia also express CXCR4 in vivo and in vitro (27), but in general T-tropic strains do not replicate very well in microglia or MDM (42, 48). Whether microglial GPCRs can respond to their natural chemokine ligands, and what role signal transduction may play in HIV infection of microglia or CNS pathogenesis, is thus far unknown.
Recent studies have demonstrated that HIV and simian immunodeficiency virus (SIV) envelopes can also use other GPCRs, besides CCR5, CCR3, and CXCR4, for viral entry and fusion. Among these are CCR8 (21, 40), the receptor for I309, and the orphan receptors GPR1 (8, 12), GPR15 (6, 8, 12), STRL33 (6, 8, 29), and APJ (3, 10). The mRNAs for GPR1 (31) and APJ (3, 32, 36) are expressed in the brain, but their cellular localization is unknown. Choe and colleagues have recently demonstrated that APJ is not utilized by the HIVD isolates JrFL and YU-2 (3), although JrFL has been reported to use STRL33 (29) and YU-2 utilizes GPR15 (6, 12). Little else is known regarding the ability of HIVD envelopes to use CCR8 or orphan receptors as HIV coreceptors. However, it is quite conceivable that preferential replication in the brain is a consequence of the utilization of one or more of these alternate coreceptors by HIV isolates.
To begin to develop a more detailed understanding of the role of each of the established coreceptors (CCR5, CCR3, and CXCR4) in HIV entry into adult microglia, we have assayed their surface expression by flow cytometry. We have also addressed the functionality of these GPCRs by determining the microglial response to α- and β-chemokines. To determine whether viruses obtained from the brain can use CCR5, CCR3, or CXCR4 as a coreceptor, we have looked at infection with pseudotyped viruses expressing the luciferase reporter gene, as well as with wild-type viruses.
MATERIALS AND METHODS
Cells.
Microglial cultures were prepared as previously described from fresh adult human brain tissue obtained during temporal lobectomy for medication-resistant epilepsy (1, 43, 44, 49). Microglia were cultured in 10% Dulbecco modified Eagle medium (DMEM; GIBCO-BRL) with 5% heat-inactivated fetal calf serum (FCS; Atlanta Biologicals, Norcross, Ga.), 5% Giant Cell Tumor Supernatant (Fisher), 50 μg of gentamicin (GIBCO-BRL)/ml, and 1 mM sodium pyruvate. 293T and U87 cells were cultured in DMEM with 10% FCS (43).
Detection of cell surface CCR5 and CCR3.
Microglial cells were cultured for 5 to 7 days prior to staining for CCR5 or CCR3. All staining steps were performed on ice. For each staining condition, 8 × 105 cells were washed with 1× phosphate-buffered saline (PBS), without Ca2+ or Mg2+ (GIBCO-BRL), and detached by treatment with 0.5 mM EDTA and mechanical dissociation. Cells were immediately diluted 15-fold in DMEM with 10% FCS and then centrifuged for 5 min at 1,000 rpm in a Beckman tabletop centrifuge. The supernatant was removed; the cells were resuspended in staining buffer with blocking solution (PBS with 0.1% bovine serum albumin [BSA], 0.02% sodium azide, and 8% rabbit serum), divided into staining tubes (Robbins Scientific, Sunnyvale, Calif.), and washed; and 50 μl of primary antibody was added per tube. Cells were incubated on ice for 45 min with the following primary antibodies diluted in staining buffer (PBS with 0.1% BSA and 0.02% sodium azide): 807.09 isotype control (17), 7B11 (anti-CCR3) (20), and 2D7 (anti-CCR5) (47) (all at 5 μg/ml) and a 1:10 dilution of an anti-major histocompatibility complex MHC class I monoclonal antibody (MAb) supernatant (W6/32) (11, 37). Cells were washed with staining buffer without rabbit serum and were resuspended in 1 drop of heat-inactivated FCS, 25 μl of secondary antibody (10 μg of rabbit anti-mouse biotin/ml) was added per tube (Dako, Carpinteria, Calif.), and the mixture was incubated on ice for 30 min. Cells were washed and resuspended in 25 μl of 1.3 μg of streptavidin/ml coupled to fluorescein isothiocyanate (Dako), incubated on ice for 30 min, washed, and fixed with 300 μl of freshly prepared 2% paraformaldehyde diluted in PBS. U87 and 293T cells transiently transfected with CCR5 and CCR3 plasmids (as described below) were used as controls. All flow cytometry analysis was performed on the FACScan (Becton Dickinson) by using CellQuest flow cytometry (Cancer Center, University of Pennsylvania).
Quantification of CCR5, CCR3, and CXCR4 antibody binding sites on microglia.
Quantitative flow cytometry was performed by converting the mean channel fluorescence into the number of antibody binding sites, or the number of target molecules per cell (if antibody-binding valency is known), by using a standardized microbead kit (Quantum Simply Cellular Microbeads Kit; Sigma, St. Louis, Mo.). This is a mixture of five microbead populations of uniform size, coated with goat anti-mouse antibodies, that have differing abilities to bind mouse antibodies (one bead population has no specific ability to bind mouse immunoglobulin G and is included as a baseline control). Each MAb is then added at saturating amounts to approximately 100,000 beads. After a 1-h incubation, the beads were washed and stained with secondary antibodies in a manner identical to that used for microglia. The beads were then analyzed by using the same instrument settings as those for the microglia. The binding capacities of the stained microbeads were then regressed against the corresponding geometric mean of each bead population. Subsequently, the mean fluorescence intensity of the antigen analyzed on microglia can be converted to the number of antibody binding sites per cell by comparison with the regression curve generated. The parameters of the regression curve permit a determination of the linear deviation and hence provide an estimate of the degree of confidence one should have in the values generated. Regression curves are acceptable only if r > 0.995 and the deviation from linearity (average residual percent) is less than 5%.
Microglial response to chemokines.
All intracellular calcium level ([Ca2+]i) measurement procedures were performed at room temperature (23 to 25°C). Microglia (2 × 104 to 4 × 104) were plated on 22- by 22-mm coverslips and cultured for 2 days (as described above); coverslips were then inverted and attached to the upper side of a perfusion chamber (RC-21B; Warner Instrument Corp., Hamden, Conn.) that was mounted on the stage of an upright microscope (Optiphot; Nikon, Tokyo, Japan) equipped for epifluorescence. The microglia were then loaded with 5 μM fura-2/AM in 0.02% Pluronic F-127 in standard recording medium for 30 min (22). Excess fura-2/AM was washed out of the chamber, and the cells were maintained in standard recording medium for an additional 15 min in order to hydrolyze loaded fura-2/AM completely. Microglial cells were exposed to 30 to 150 nM eotaxin, 60 nM macrophage inflammatory protein 1β (MIP-1β), or 60 nM stromal cell-derived factor 1α (SDF-1α) (Peprotech, Rocky Hill, N.J.) while being alternatively illuminated by a 75-W Xe arc lamp through 340- and 380-nm excitation filters controlled by a computer-assisted filter changing device (LAMBDA-10; Sutter Instrument Co., Novato, Calif.). Emission fluorescence images through a 20× objective lens (CF Fluor DL; numerical aperture, 0.75; Nikon) and a 510-nm barrier filter were collected with a SIT camera (C2400-08; Hamamatsu Photonics K. K., Hamamatsu City, Japan) and converted to digital data by an image-processing system (ARGUS-50; Hamamatsu Photonics K. K.). Each frame of a digital image consisted of 512 by 382 pixels. Every frame was stored in a PC-based computer and converted to single-cell temporal 510-nm emission plots.
Preparation of luciferase reporter virus pseudotyped with high-expression HIVD envelope clones.
The HIVD env genes DS-br (clone C17), RC-br (clone 56), KJ-br (clone A1), and YU-2 (clone A10) were obtained from viruses from individuals with HIVD or encephalopathy (15, 28). Prior to cloning, these viruses were obtained from brains by cocultivation with MDM (14, 15). They were expanded by a single additional culture in MDM prior to cloning of their envelopes (43). The previously cloned envelopes in pCR3.1-Uni (Invitrogen) (43) were subcloned into pEXV3, a eukaryotic expression plasmid with a simian virus 40 (SV40) promoter (a gift from N. Harel) (34). pEXV3 was linearized by digestion with SmaI (New England Biolabs), and the HIVD envelope genes were removed from pCR3.1-Uni by digestion with PmeI. The HIVD envelope genes were blunt ligated into pEXV3 and cotransfected with pNL-4-3-LucR+E− into 293T cells to generate one-round infectious pseudotype virus as previously described (5, 43). Other envelopes (BaL and NL43) were obtained from J. Moore (Aaron Diamond AIDS Research Center), and SIVmac251 was obtained from A. Edinger (8).
Infection of U87 cells expressing chemokine and orphan coreceptors.
U87 cells (3 × 105/well) were transiently transfected in a six-well plate with 2 μg of pT4 (30), which expresses the CD4 molecule, in each well and 3 μg of a plasmid expressing CCR3 (40), CCR5 (5), CXCR4 (13), APJ (10), CCR8 (40, 41), GPR1 or GPR15 (9, 31), or STRL33 (9) in each well by using a calcium phosphate transfection kit (5 Prime→3 Prime, Boulder, Colo.) as previously described (43). The following day, 7.5 × 103 transfected cells per well were plated in 96-well plates, incubated overnight, and infected with pseudotype virus in the presence of 8 μg of Polybrene (Sigma)/ml. Cultures were exposed to the inocula overnight at 37°C and refed with 200 μl of medium. Three days after infection, the cells were lysed with 60 μl of luciferase assay buffer (Promega). Luciferase activity was measured by adding 50 μl of luciferase assay substrate (Promega) to 50 μl of lysate and reading light activity in a Wallac 1450 Microbeta luminometer detector. The light activity is reported as relative light units (RLU) per second.
Infection of microglia with HIVD envelope-pseudotyped viruses in the presence of anti-chemokine receptor antibodies.
Microglial cells were cultured in 96-well plates for 2 to 7 days and were then pretreated with anti-CCR5 (2D7), anti-CCR3 (7B11), or anti-CXCR4 (12G5; a gift from J. Hoxie) at 20 μg/ml for 45 min at 4°C. The cells were then infected with 200 μl of pseudotyped virus for 16 h at 37°C, the medium was replaced, the cells were lysed 4 to 5 days postinfection with 100 μl of lysis buffer, and then 40 μl of the lysate was combined with 100 μl of luciferase substrate, and the chemiluminescence was read as indicated above.
Inhibition of virus infection of microglia with anti-chemokine receptor antibodies.
Microglia were preincubated with anti-chemokine receptor antibodies, as described above, and then infected with HIV-1DS-br, HIV-1RC-br (14, 15), HIV-1YU-2(RF-1) (originally cloned by Li et al. [28] and obtained from R. Fouchier [University of Pennsylvania]), or the microglia-passaged virus HIV-1BORI-20 (44) at 4 ng of p24gag per well. The next day the inocula were removed, the cells were washed, and medium was replaced with 5 μg of the corresponding antibody/ml. A 2D7 antibody with no azide and low endotoxin levels (Pharmingen) was used in these experiments. The cell cultures were observed for cytopathicity, and the supernatants were assayed for viral p24gag antigen at intervals of several days with maintenance of antibody throughout (43).
Expression and infection of U87 cells transfected with chemokine receptors (CCR5, CCR3, and CXCR4).
U87 cells were transiently transfected with 2 μg of CD4 and a total of 1.5 to 2.0 μg of pCDNA3.1 and the chemokine receptor CCR5, CCR3, or CXCR4 or a combination of CCR5 plus CXCR4, CCR5 plus CCR3, or CCR3 plus CXCR4. pCDNA3.1 was used to equilibrate the quantity of total DNA used in each transfection. The cells were plated, cultured overnight, infected with HIV env/pNL-4-3-LucR+E− pseudotyped viruses, constructed with the HIVD envs from HIV-1YU-2 and HIV-1DS-br, lysed, and analyzed by a luciferase assay.
RESULTS
Chemokine receptor expression on adult microglia.
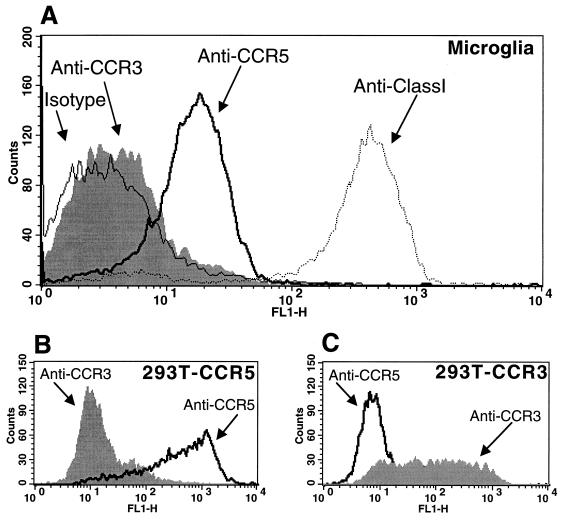
To determine whether there were detectable levels of CCR5 or CCR3 on the surfaces of microglia, we used flow cytometry analysis. Microglia were cultured for 5 to 7 days under the conditions described in Materials and Methods and were stained with MAbs directed against each of the chemokine receptors. As shown in Fig. 1A, there was a prominent shift in the fluorescence profile with a MAb against CCR5 (2D7) in comparison with an isotype-matched control. CCR3 expression was considerably lower or undetectable in four experiments performed with different microglial preparations. The histogram in Fig. 1A is a representative experiment where there was a slight shift with the anti-CCR3 MAb (7B11). CXCR4 expression has been shown previously in similar microglial preparations (27). Figures 1B and C are antibody controls using cells transfected with CCR5 and CCR3 plasmids, respectively.
FIG. 1.
Surface expression of chemokine receptors CCR3 and CCR5 on microglia. (A) Adult human microglia were cultured for 6 days, detached, stained with a MAb for CCR5 (2D7) or CCR3 (7B11), an isotype-matched monoclonal control (807.09), or an anti-class I hybridoma supernatant, and analyzed by flow cytometry as described in Materials and Methods. Microglia were positive for CCR5, whereas levels of CCR3 staining were low or undetectable. Similar staining patterns were seen in microglia from three other donors. (B and C) As positive controls, 293T cells transiently transfected with CCR5 (B) and CCR3 (C) were stained with the same chemokine receptor MAbs.
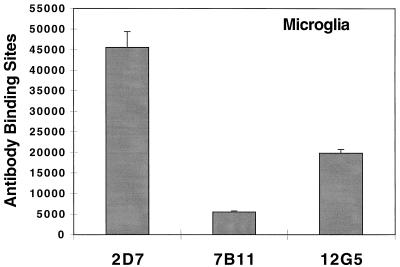
To quantify the expression of CCR3 on microglial cells, and to eliminate any potential effects of the culture conditions on chemokine receptor expression, we used a flow cytometry assay, as described in Materials and Methods. Microglia were stained less than 24 h after isolation, and the numbers of antibody binding sites for CCR3, CCR5, and CXCR4 were calculated. Figure 2 demonstrates that the findings with this assay were consistent with the data shown in Fig. 1 and furthermore that microglia express high levels of CCR5 before prolonged culture. The levels of CCR5 found in these microglia are comparable to those seen in MDM cultured in macrophage colony-stimulating factor (data not shown).
FIG. 2.
Anti-chemokine receptor antibody binding sites on microglia cultured less than 24 h. To determine the number of antibody binding sites per cell, microglia were stained and analyzed with the MAbs 2D7 (anti-CCR5), 7B11 (anti-CCR3), and 12G5 (anti-CXCR4), as described in Materials and Methods. Error bars indicate the deviations from linearity obtained from the linear regression curve. The CCR3 quantification was repeated on microglia that had been cultured for 11 days with similar results.
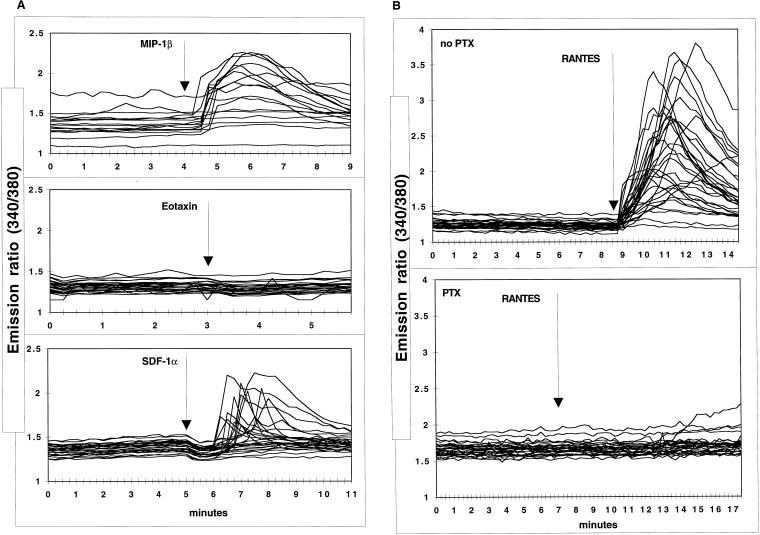
Microglial calcium signaling in response to MIP-1β, eotaxin, SDF-1α, and RANTES.
To determine whether the chemokine receptors present on adult microglia could transduce a calcium flux in response to their chemokine ligands, changes in intracellular calcium levels were measured in single-cell experiments using a calcium-sensitive dye (Fig. 3). Following stimulation with 60 nM MIP-1β, which binds CCR5, the majority of the microglial cells in the culture responded with a marked change in the ratio of emission (recorded at 510 nm) at 340- and 380-nm excitation wavelengths (Fig. 3A). In contrast to the results with MIP-1β, we were unable to detect a response after exposure to eotaxin (30 to 150 nM), a chemokine that transduces signals through CCR3 (Fig. 3A), in five different experiments with microglia from four different donors. To control for potential generalized unresponsiveness of some of the cells, ATP was used in experiments where there was no response to ligands, since microglia have metabotropic ATP receptors (35). There was a marked response to ATP (data not shown).
FIG. 3.
Exposure to chemokines triggers changes in microglial intracellular free [Ca2+]. Microglia cultured for 5 to 10 days (3 × 104/coverslip) were loaded with 2.5 μM fura-2/AM and prepared for single-cell calcium flux experiments as described in Materials and Methods. (A) Cells were exposed to 60 nM MIP-1β, 60 nM eotaxin, or 60 nM SDF-1α for 5 min, and changes in free Ca2+ were expressed as the emission ratio, at 510 nm, following excitation at 340 and 380 nm. These results are representative of experiments repeated multiple times with different microglial preparations. (B) Microglia that were or were not pretreated with 0.5 to 1.0 μg of pertussis toxin (PTX)/ml were exposed to 60 nM RANTES.
Since CXCR4 was also detected in these microglial preparations (Fig. 2) (27), we performed experiments with SDF-1α, its natural ligand. As shown in the representative curve in Fig. 3A (bottom panel), a proportion of the cells responded with a change in the emission ratio after excitation of the fura-2. In four separate experiments, 10 to 50% of the cells demonstrated this phenomenon. These signaling data reinforce the receptor expression analysis, as the microglia responded to the ligands whose receptors are most readily detected on the cell surface. CCR3, on the other hand, demonstrated no response to its ligand.
RANTES, a potent β-chemokine that binds and signals through several receptors, was also used to stimulate signal transduction in microglia. As shown in Fig. 3B (top panel), there was a strong response to this chemokine when it was used at concentrations ranging from 60 to 80 nM. Since microglia had low levels of CCR3 and high levels of CCR5 on their surfaces, it is likely that the changes in free calcium concentration were due to an interaction between RANTES and CCR5, although signaling through other receptors cannot be ruled out. Microglia pretreated with 0.5 to 1.0 μg of pertussis toxin/ml did not respond to RANTES, indicating that the microglia respond to these chemokines by the pertussis toxin-sensitive GPCR pathway (Fig. 3B, bottom panel).
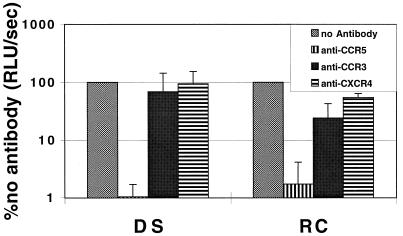
Inhibition of infection with antibodies: envelope-pseudotyped viruses.
We have previously shown that envelope proteins derived from microglia-tropic virus strains used CCR5, and, to a lesser extent, CCR3 and CXCR4 to infect transfected cells (43). To determine which of the receptors can mediate entry of these HIVD isolates into microglia, we exposed microglia to pseudotyped viruses in the presence of chemokine receptor antibodies. Pretreatment of microglia with the anti-CCR5 antibody 2D7 consistently inhibited, by 2 log units, infection by virus pseudotyped with envelopes obtained from HIV-1DS-br and HIV-1RC-br (Fig. 4). In contrast, antibodies against either CCR3 or CXCR4 showed either very slight or no inhibition of infection by the same pseudotypes (Fig. 4). Pseudotypes prepared with the envelope from HIV-1YU-2 did not result in as high a signal as pseudotypes made with other envelopes, particularly that from HIV-1DS-br. Nevertheless, the YU-2 pseudotypes followed the general trend of marked reduction in the signal with anti-CCR5 and much less pronounced effects with anti-CCR3 or anti-CXCR4 antibody. As a control, the anti-CCR3 antibody inhibited infection of DS-br and RC-br pseudotype viruses in CCR3-transfected U87 cells (data not shown).
FIG. 4.
Inhibition of env-pseudotyped virus infection of microglia with antibodies to chemokine receptors. Microglia were preincubated with MAb to CCR5 (2D7), CCR3 (7B11), or CXCR4 (12G5) at a concentration of 20 μg/ml for 45 min at 4°C and were then infected with pseudotyped viruses. Cells were lysed 4 to 5 days postinfection, and infection was measured as luciferase activity (RLU per second). Data are expressed as percentages of luciferase activity obtained in the absence of antibody. DS, envelope from HIV-1DS-br; RC, envelope from HIV-1RC-br.
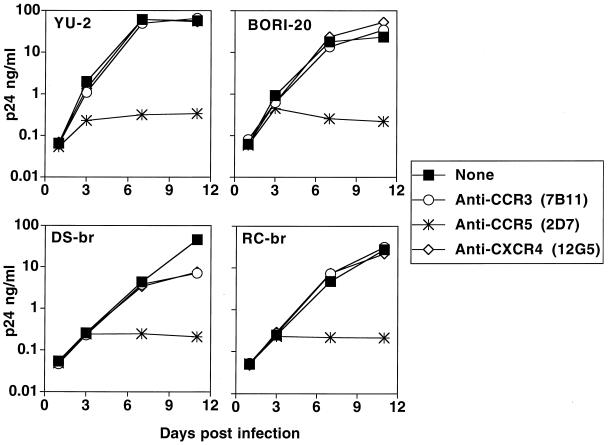
Inhibition of infection with antibodies: wild-type viruses.
In the next series of infections we used wild-type viruses. In agreement with the single-round pseudotype infection data (Fig. 4), when microglia were pretreated with anti-CCR5 MAb, there was a marked reduction in the production of p24gag antigen after infection with several HIV isolates. Figure 5 shows representative growth curves from isolates HIV-1YU-2, HIV-1BORI-20, HIV-1DS-br, and HIV-1RC-br. All viral inocula were normalized by p24gag antigen concentration, and peak viral outputs in five similar experiments were consistent. Infections performed after preincubation with anti-CCR3 or anti-CXCR4 antibody demonstrated low or no inhibition of viral replication in four of five experiments. In one experiment there was significant (100- to 1,000-fold) diminution in p24gag output by two other isolates, HIV-1BORI and HIV-189.6, after pretreatment with anti-CCR3 and less inhibition of HIV-1BORI-20 (data not shown).
FIG. 5.
Inhibition of HIVD isolate infection of microglia in the presence of antibodies to chemokine receptors. Microglia were preincubated with MAb to CCR3 (7B11), CCR5 (2D7), or CXCR4 (12G5) at a concentration of 20 μg/ml for 45 min at 4°C and were then infected with 4 ng of p24gag of HIV-1YU-2, HIV-1BORI-20, HIV-1DS-br, or HIV-1RC-br. The following day, the inocula were removed, the cells were washed, and medium was replaced with the appropriate antibody (5 μg/ml). Infected cultures were maintained with the appropriate MAb at a constant concentration. Supernatants were collected over the course of infection and assayed for viral p24gag antigen, expressed in nanograms per milliliter.
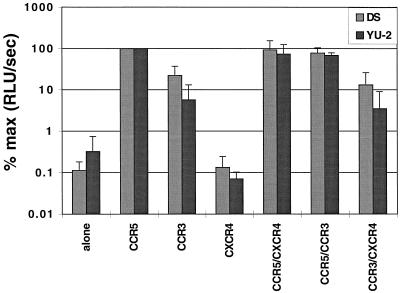
Analysis of HIVD envelope utilization of cells transfected with two chemokine receptors.
We used a double chemokine receptor system to determine whether two chemokine receptors present together on the surface of a cell, which we assume occurs in microglia, could have either a synergistic or an inhibitory role in HIV entry, since such a scenario has been proposed for this cell type (19). 293T cells transiently transfected with CD4 and various combinations of the CCR5, CCR3, and CXCR4 plasmids (Fig. 6) were infected with pseudotypes expressing the HIV-1DS-br and HIV-1YU-2 envelopes, and single-cycle infection was measured by chemiluminescence. As shown in the summary of several experiments in Fig. 6, the presence of two receptors was not synergistic, and maximum entry was achieved with CCR5 alone. The addition of either CCR3 or CXCR4 had no effect on pseudotype entry. Since the degree of CD4 expression may affect the importance of chemokine receptor concentration (38), similar experiments were performed with different levels of CD4 expression. The results were comparable to those depicted in Fig. 6 (data not shown).
FIG. 6.
HIVD env-pseudotyped virus infection of 293T cells transfected with two chemokine receptors. 293T cells were transiently transfected with CD4 alone or with CD4 and CCR5, CCR3, CXCR4, CCR5 plus CXCR4, CCR5 plus CCR3, or CCR3 plus CXCR4. pCDNA3.1 was used to equalize the quantity of DNA in each well. Data are expressed as percentages of infection of 293T cells with CD4 and CCR5. Error bars, standard deviations. DS, envelope from HIV-1DS-br; YU-2, envelope from HIV-1YU-2.
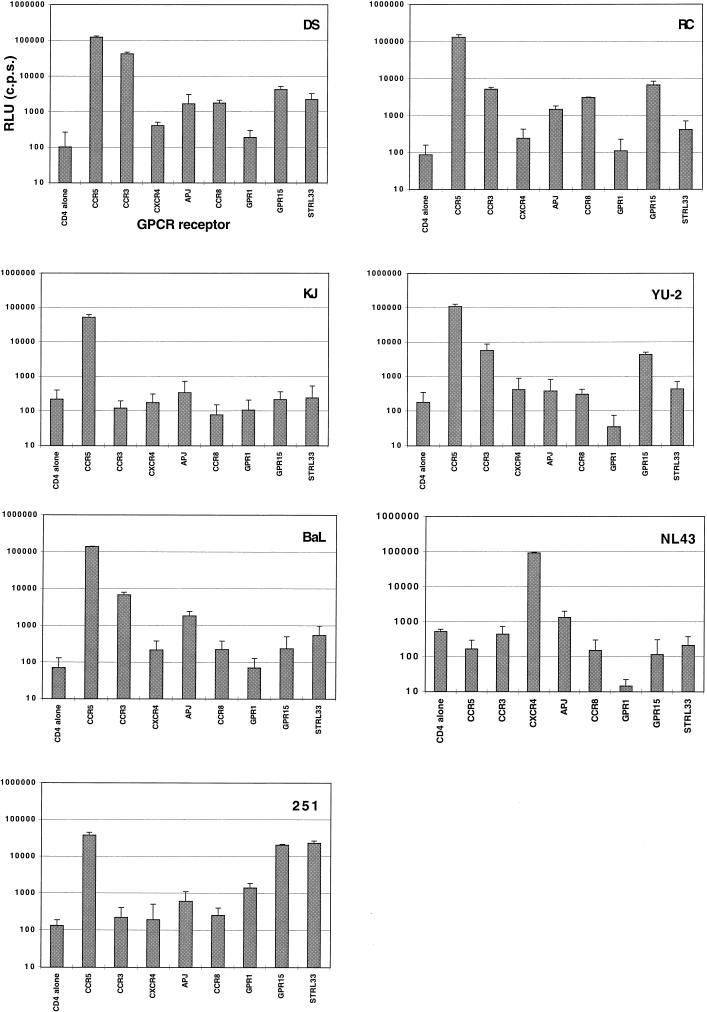
HIVD envelope utilization of alternate coreceptors.
We recently studied the ability of HIVD envelope-pseudotyped virus to infect transiently transfected cells through CCR5-, CCR3-, and CXCR4 (CD4-dependent)-mediated entry pathways, and we concluded that all HIVD envelopes tested used CCR5, with some evidence for low-level CCR3 and CXCR4 use by some of the envelope clones (43). To improve expression, HIVD envelopes were cloned into EXV3, an SV40 expression vector (34). Luciferase reporter virus was then pseudotyped with the EXV3-based HIVD envelope clones DS, RC, KJ, and YU-2. Virus pseudotypes were also generated with the BaL, NL43, and SIVmac251 envelopes to ensure that adequate expression of the various coreceptors was obtained. These pseudotyped viruses were tested in triplicate on U87 cells transiently transfected with plasmids encoding CD4 and either CCR5, CCR3, CXCR4, APJ, CCR8, GPR1, GPR15, or STRL33 (Fig. 7). A signal 10 times over background (CD4 only) was considered to be positive. In agreement with our previous report (43), HIVD envelope-pseudotyped viruses predominantly used CCR5, with some other coreceptors being used less efficiently. These data are depicted graphically in Fig. 7 and summarized in Table 1. Because reagents are not available, except for CCR5, CXCR4, and CCR3 (see Fig. 1), we could not quantify the level of expression of the alternate receptors. Several envelopes used CCR3 and GPR15, albeit at lower levels than CCR5. There was also some use of APJ, CCR8, and STRL33, particularly by the DS envelope. The KJ envelope, cloned from a virus isolated from a pediatric encephalitic case, used CCR5 only. DS-br, the pseudotyped virus with the highest luciferase activity, was unable to use any of the coreceptors tested when CD4 was not coexpressed (data not shown).
FIG. 7.
Alternative coreceptor use by HIVD viral envelopes. Pseudotyped viruses prepared with HIV envelopes DS-br, RC-br, and KJ-br and control envelopes YU-2, BaL, NL-43, and SIVmac251 were assayed for infectivity as measured by luciferase activity (in RLU per second) on U87 cells transiently transfected with CD4 and CCR5, CCR3, CXCR4, APJ, CCR8, GPR1, GPR15, or STRL33. Infections were performed in triplicate. Error bars, standard deviations.
TABLE 1.
CCR5, CCR3, and orphan receptor use by HIVD envelope-pseudotyped viruses
| Virus | Level of infectiona with receptor:
|
|||||||
|---|---|---|---|---|---|---|---|---|
| CCR5 | CCR3 | CXCR4 | APJ | CCR8 | GPR1 | GPR15 | STRL33 | |
| DS | +++ | ++ | − | + | + | − | + | + |
| RC | +++ | + | − | + | + | − | + | − |
| KJ | ++ | − | − | − | − | − | − | − |
| YU-2 | +++ | + | − | − | − | − | + | − |
| BaL | +++ | + | − | + | − | − | − | − |
| NL43 | − | − | ++ | − | − | − | − | − |
| 251 | ++ | − | − | − | − | − | ++ | ++ |
Infection was measured in RLU per second. −, less than 1 log unit over background; +, 1 log unit over background; ++, 2 log units over background; +++, 3 log units over background. Background, infection with CD4 alone and no chemokine receptor (see text for details).
DISCUSSION
Microglia are the cells primarily responsible for viral load in the CNS, where they probably play a role in the development of HIVD, and because of poor penetration of antiretrovirals into the CNS, they may serve as a potential “sanctuary” site for the virus (4). Since virus replication can differ between microglia and MDM (44), understanding the virus-cell biology in microglia is critical for the development of strategies to treat HIVD. The discovery that chemokine receptors act as HIV coreceptors has been a major advance in delineating tropism, and the role of these receptors in microglial entry and replication has been the subject of recent publications (16, 19, 43). Here we have shown that three major chemokine receptors implicated in HIV entry, CCR5, CCR3, and CXCR4, are expressed on adult microglial cells, albeit at different levels (Fig. 2). Two of these, CCR5 and CXCR4, are functional chemokine receptors, as measured by their abilities to mediate signal transduction after stimulation with their respective ligands. In these experiments we noted robust Ca2+ responses with chemokine concentrations within the same range as (or lower than) those used for stimulation of MDM (20a, 42). Although we did not detect eotaxin-mediated calcium signaling, it is formally possible that CCR3 could mediate a signal in the absence of changes in intracellular calcium levels, as such signaling has been reported with other GPCRs (45). While our primary interest in chemokine receptors on human microglia relates to their role in HIV infection, these and future experiments will help us understand the roles of chemokine receptors in a number of inflammatory conditions involving microglia (2, 33).
Our results demonstrating that SDF-1α, MIP-1β, and RANTES induced internal calcium fluxes in microglia are not entirely unexpected, insomuch as MDM and microglia share many of the same phenotypes, with some notable differences (44). Two groups have demonstrated MDM signaling in response to treatment with SDF-1α (20a, 42), and a recent report by Herbein and colleagues demonstrated that MDM signal in response to the CCR5 ligands MIP-1β and RANTES (20a). However, there are other differences between microglia and MDM, including the time course of expression of chemokine receptors and differences in the replication potential among different isolates. Furthermore, whereas the responses of MDM and microglia were qualitatively similar, we cannot make any quantitative statements based on our data.
Depending on the assay, several viruses isolated from individuals with HIVD can use CCR5, CCR3, and, to some extent, CXCR4 as coreceptors for entry into cells transfected with plasmids expressing these receptors (43). Theoretically, HIV could utilize any of these chemokine receptors for entry into microglial cells, and He et al. have proposed that CCR3 and CCR5 function as coreceptors for fetal microglia (19). Using antibodies, we demonstrated that CCR5 is the predominant coreceptor involved in HIVD virus infection of adult microglia, with antibodies against either CCR3 or CXCR4 having only a modest or no effect on viral replication. Results with pseudotyped or wild-type viruses were quite congruent with each other and previous data (43). It is possible that the isolates utilize the CCR3 or CXCR4 on microglia inefficiently simply because of the low number of chemokine receptor molecules on the cell surface or, alternatively, because CCR3 and CXCR4 are not presented in the right context. For example, there may be an optimal CD4/coreceptor ratio that can be achieved only with a coreceptor that is expressed at high levels, such as CCR5 (25, 38). Another possibility is that a virion could simultaneously use two coreceptors complexed together, e.g., CCR5 and CCR3, and that under some circumstances antibodies against the coreceptor present in the lower concentration (CCR3) could partially block entry. This would explain why we see some inhibition with anti-CCR3 antibodies but have not been able to infect microglia with a pseudotyped virus that uses CCR3 but not CCR5 (20b). Therefore, CCR3 and CXCR4 may play roles in microglial entry, but for an infection of microglia to occur at relevant levels, HIV must use CCR5, which is both necessary and sufficient for infection.
Additionally, we found that envelopes from several HIVD isolates can mediate infection of cells transfected with other GPCRs previously described as HIV coreceptors. But they do so with apparently reduced efficiency in comparison with CCR5, at least within the constraints of this assay system, which did not quantify the level of expression of each of the coreceptors on the transfected cell surface. This area will need further clarification when antibodies against these alternative coreceptors become available.
We have previously suggested that direct amplification of envelope genes from HIV-infected brains may clarify the potential role of these other coreceptors, since it does not introduce the selection bias associated with viral isolation (43). For infection of microglia, it is also quite possible that CCR3, CXCR4, and other coreceptors are expressed at higher levels in the CNS of individuals with HIVD and that under those circumstances they play a more significant role in HIV entry.
In contrast to microglia, which can be infected soon after isolation (43a), undifferentiated monocytes are relatively resistant to infection on day 1 after isolation (46). Monocytes have low levels of CCR5 until cultured, whereas microglia have high levels of CCR5 soon after purification from brain tissue (Fig. 2). These high levels of CCR5 may explain why the CNS is infected early during the course of HIV infection, at a time when most viruses use CCR5 as a coreceptor, and why virus is present in the brains of many patients with or without HIVD (23). Chemokine receptor levels may also contribute to the differences we have previously noted between replication in MDM and in microglia (44). Given the detectable levels of CXCR4 present in microglia, it is somewhat surprising that more CXCR4-using viruses have not been isolated from brains, particularly since these isolates are particularly prominent in the late stages of HIV disease, when HIVD is more prevalent. In MDM, blocks to replication beyond the entry step have been identified for some HIV strains (42, 48), and further experimentation may clarify this issue in microglia. Alternatively, parenchymal microglia may become infected only after the CNS perivascular population of macrophages/microglia has been infected (26). This perivascular population, which may be phenotypically different with regard to HIV infection, may act as a filter, allowing only viruses using a certain coreceptor repertoire to infect the parenchymal microglia, which are used in our experimental system (18).
ACKNOWLEDGMENTS
J.T.C.S. and A.V.A. contributed equally to this work.
This work was supported in part by NS-27405, NS-35743, and MH-58958.
We thank Wei Cao for excellent technical assistance and Benjamin Doranz, Trevor Hoffman, Aimee Edinger, and Joseph Rucker from the R.W.D. laboratory for sharing reagents and for helpful discussions. Sarina Berger (F.G.-S. laboratory) helped clone the KJ-br envelope, and Julie Turner (J. Hoxie laboratory) provided advice on flow cytometry. The anti-chemokine receptor antibodies were obtained from the AIDS Reagent Program. Suzanne Gartner (Johns Hopkins University) kindly provided the HIVD viral isolates.
REFERENCES
- 1.Albright A V, Strizki J, Harouse J M, Lavi E, O’Connor M, González-Scarano F. HIV-1 infection of cultured human adult oligodendrocytes. Virology. 1996;217:211–219. doi: 10.1006/viro.1996.0108. [DOI] [PubMed] [Google Scholar]
- 2.Benveniste E N. Role of macrophages/microglia in multiple sclerosis and experimental allergic encephalomyelitis. J Mol Med. 1997;75:165–173. doi: 10.1007/s001090050101. [DOI] [PubMed] [Google Scholar]
- 3.Choe H, Farzan M, Konkel M, Martin K, Sun Y, Marcon L, Cayabyab M, Berman M, Dorf M E, Gerard N, Gerard C, Sodroski J. The orphan seven-transmembrane receptor Apj supports the entry of primary T-cell-line-tropic and dualtropic human immunodeficiency virus type 1. J Virol. 1998;72:6113–6118. doi: 10.1128/jvi.72.7.6113-6118.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen J. AIDS therapies: exploring how to get at—and eradicate—hidden HIV. Science. 1998;279:1854. doi: 10.1126/science.279.5358.1854. [DOI] [PubMed] [Google Scholar]
- 5.Deng H, Liu R, Ellmeier W, Choe S, Unutmaz D, Burkhart M, Di Marzio P, Marmon S, Sutton R E, Hill C M, Davis C B, Peiper S C, Schall T J, Littman D R, Landau N R. Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996;381:661–666. doi: 10.1038/381661a0. [DOI] [PubMed] [Google Scholar]
- 6.Deng H K, Unutmaz D, KewalRamani V N, Littman D R. Expression cloning of new receptors used by simian and human immunodeficiency viruses. Nature. 1997;388:296–300. doi: 10.1038/40894. [DOI] [PubMed] [Google Scholar]
- 7.Doms R W, Peiper S C. Unwelcomed guests with master keys: how HIV uses chemokine receptors for cellular entry. Virology. 1997;235:179–190. doi: 10.1006/viro.1997.8703. [DOI] [PubMed] [Google Scholar]
- 8.Edinger A L, Mankowski J L, Doranz B J, Margulies B J, Lee B, Rucker J, Sharron M, Hoffman T L, Berson J F, Zink M C, Hirsch V M, Clements J E, Doms R W. CD4-independent, CCR5-dependent infection of brain capillary endothelial cells by a neurovirulent simian immunodeficiency virus strain. Proc Natl Acad Sci USA. 1997;94:14742–14747. doi: 10.1073/pnas.94.26.14742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edinger A L, Hoffman T L, Sharron M, Lee B, O’Dowd B, Doms R W. Use of GPR1, GPR15, and STRL33 as coreceptors by diverse HIV-1 and SIV envelope proteins. Virology. 1998;249:367–378. doi: 10.1006/viro.1998.9306. [DOI] [PubMed] [Google Scholar]
- 10.Edinger A L, Hoffman T L, Sharron M, Lee B, Yi Y, Choe W, Kolson D L, Mitrovic B, Zhou Y, Faulds D, Collman R G, Hesselgesser J, Horuk R, Doms R W. An orphan seven-transmembrane domain receptor expressed widely in the brain functions as a coreceptor for human immunodeficiency virus type 1 and simian immunodeficiency virus. J Virol. 1998;72:7934–7940. doi: 10.1128/jvi.72.10.7934-7940.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Endres M J, Clapham P R, Marsh M, Ahuja M, Turner J D, McKnight A, Thomas J F, Stoebenau-Haggerty B, Chose S, Vance P J, Wells T N C, Power C A, Landau N R, Hoxie J A. CD4-independent infection of HIV-2 is mediated by fusin/CXCR4. Cell. 1996;87:745–756. doi: 10.1016/s0092-8674(00)81393-8. [DOI] [PubMed] [Google Scholar]
- 12.Farzan M, Choe H, Martin K, Marcon L, Hofmann W, Karlsson G, Sun Y, Barrett P, Marchand N, Sullivan N, Gerard N, Gerard C, Sodroski J. Two orphan seven-transmembrane segment receptors which are expressed in CD4-positive cells support simian immunodeficiency virus infection. J Exp Med. 1997;186:405–411. doi: 10.1084/jem.186.3.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feng Y, Broder C C, Kennedy P E, Berger E A. HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996;272:872–877. doi: 10.1126/science.272.5263.872. [DOI] [PubMed] [Google Scholar]
- 14.Gartner S, Popovic M. Macrophage tropism of HIV-1. AIDS Res Hum Retroviruses. 1990;6:1017–1021. doi: 10.1089/aid.1990.6.1017. [DOI] [PubMed] [Google Scholar]
- 15.Gartner S, McDonald R A, Hunter E A, Bouwman F, Liu Y, Popovic M. gp120 sequence variation in brain and in T-lymphocyte human immunodeficiency virus type 1 primary isolates. J Hum Virol. 1997;1:3–18. [PubMed] [Google Scholar]
- 16.Ghorpade A, Xia M Q, Hyman B T, Persidsky Y, Nukuna A, Bock P, Che M, Limoges J, Gendelman H E, Mackay C R. Role of the β-chemokine receptors CCR3 and CCR5 in human immunodeficiency virus type 1 infection of monocytes and microglia. J Virol. 1998;72:3351–3361. doi: 10.1128/jvi.72.4.3351-3361.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.González-Scarano F, Shope R E, Calisher C E, Nathanson N. Characterization of monoclonal antibodies against the G1 and N proteins of LaCrosse and Tahyna, two California serogroup bunyaviruses. Virology. 1982;120:42–53. doi: 10.1016/0042-6822(82)90005-8. [DOI] [PubMed] [Google Scholar]
- 18.González-Scarano F, Strizki J M, Albright A, Shieh J. Use of primary CNS cultures to investigate HIV neurotropism. J Neurovirol. 1997;3:S11–S13. [PubMed] [Google Scholar]
- 19.He J, Chen Y, Farzan M, Choe H, Ohagen A, Gartner S, Busciglio J, Yang X, Hoffman W, Newman W, Mackay C R, Sodroski J, Gabuzda D. CCR3 and CCR5 are coreceptors for HIV-1 infection of microglia. Nature. 1997;385:645–649. doi: 10.1038/385645a0. [DOI] [PubMed] [Google Scholar]
- 20.Heath H, Qin S, Rao P, Wu L, LaRosa G, Kassam N, Ponath P D, Mackay C R. Chemokine receptor usage by human eosinophils. The importance of CCR3 demonstrated using an antagonistic monoclonal antibody. J Clin Investig. 1997;99:178–184. doi: 10.1172/JCI119145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20a.Herbein G, Mahlknecht U, Batliwalla F, Gregersen P, Pappas T, Butler J, O’Brien W A, Verdin E. Apoptosis of CD8+ T cells is mediated by macrophages through interaction of HIV gp120 with chemokine receptor CXCR4. Nature. 1998;395:189–194. doi: 10.1038/26026. [DOI] [PubMed] [Google Scholar]
- 20b.Hoffman, T., and J. Shieh. Unpublished data.
- 21.Horuk R, Hesselgesser J, Zhou Y, Faulds D, Halks-Miller M, Harvey S, Taub D, Samson M, Parmentier M, Rucker J, Doranz B J, Doms R W. The CC chemokine I-309 inhibits CCR8-dependent infection by diverse HIV-1 strains. J Biol Chem. 1998;273:386–391. doi: 10.1074/jbc.273.1.386. [DOI] [PubMed] [Google Scholar]
- 22.Itoh, T., A. Itoh, K. Horiuchi, and D. Pleasure. AMPA receptor-mediated excitotoxicity in human NT2-N neurons results from loss of intracellular Ca2+ homeostasis following marked elevation of intracellular Na2+. J. Neurochem., in press. [DOI] [PubMed]
- 23.Johnson R T, Glass J D, McArthur J C, Chesebro B W. Quantitation of human immunodeficiency virus in brains of demented and nondemented patients with acquired immunodeficiency syndrome. Ann Neurol. 1996;39:392–395. doi: 10.1002/ana.410390319. [DOI] [PubMed] [Google Scholar]
- 24.Kolson D L, Lavi E, González-Scarano F. The effects of human immunodeficiency virus in the central nervous system. Adv Virus Res. 1998;50:1–47. doi: 10.1016/s0065-3527(08)60804-0. [DOI] [PubMed] [Google Scholar]
- 25.Kozak S L, Platt E J, Madani N, Ferro F E, Peden K, Kabat D. CD4, CXCR-4, and CCR-5 dependencies for infections by primary patient and laboratory-adapted isolates of human immunodeficiency virus type 1. J Virol. 1997;71:873–882. doi: 10.1128/jvi.71.2.873-882.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lane J H, Sasseville V G, Smith M O, Vogel P, Pauley D R, Heyes M P, Lackner A A. Neuroinvasion by simian immunodeficiency virus coincides with increased numbers of perivascular macrophages/microglia and intrathecal immune activation. J Neurovirol. 1996;2:423–432. doi: 10.3109/13550289609146909. [DOI] [PubMed] [Google Scholar]
- 27.Lavi E, Strizki J M, Ulrich A M, Zhang W, Fu L, Wang Q, O’Connor M, Hoxie J A, González-Scarano F. CXCR-4 (Fusin), a co-receptor for the type 1 human immunodeficiency virus (HIV-1), is expressed in the human brain in a variety of cell types, including microglia and neurons. Am J Pathol. 1997;151:1035–1042. [PMC free article] [PubMed] [Google Scholar]
- 28.Li Y, Kappes J C, Conway J A, Price R W, Shaw G M, Hahn B H. Molecular characterization of human immunodeficiency virus type 1 cloned directly from uncultured human brain tissue: identification of replication-competent and -defective viral genomes. J Virol. 1991;65:3973–3985. doi: 10.1128/jvi.65.8.3973-3985.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liao F, Alkhatib G, Peden K W, Sharma G, Berger E A, Farber J M. STRL33, a novel chemokine receptor-like protein, functions as a fusion cofactor for both macrophage-tropic and T cell line-tropic HIV-1. J Exp Med. 1997;185:2015–2023. doi: 10.1084/jem.185.11.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maddon P J, Dalgleish A G, McDougal J S, Clapham P R, Weiss R A, Axel R. The T4 gene encodes the AIDS virus receptor and is expressed in the immune system and the brain. Cell. 1986;47:333–348. doi: 10.1016/0092-8674(86)90590-8. [DOI] [PubMed] [Google Scholar]
- 31.Marchese A, Docherty J M, Nguyen T, Heiber M, Cheng R, Heng H H, Tsui L C, Shi X, George S R, O’Dowd B F. Cloning of human genes encoding novel G protein-coupled receptors. Genomics. 1994;23:609–618. doi: 10.1006/geno.1994.1549. [DOI] [PubMed] [Google Scholar]
- 32.Matsumoto M, Hidaka K, Akiho H, Tada S, Okada M, Yamaguchi T. Low stringency hybridization study of the dopamine D4 receptor revealed D4-like mRNA distribution of the orphan seven-transmembrane receptor, APJ, in human brain. Neurosci Lett. 1996;219:119–122. doi: 10.1016/s0304-3940(96)13198-0. [DOI] [PubMed] [Google Scholar]
- 33.McRae A, Dahlstrom A, Ling E A. Microglia in neurodegenerative disorders: emphasis on Alzheimer’s disease. Gerontology. 1997;43:95–108. doi: 10.1159/000213838. [DOI] [PubMed] [Google Scholar]
- 34.Miller J, Germain R N. Efficient cell surface expression of class II MHC molecules in the absence of associated invariant chain. J Exp Med. 1986;164:1478–1489. doi: 10.1084/jem.164.5.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moeller T, Nolte C, Burger R, Verkhratsky A, Kettenmann H. Mechanisms of C5a and C3a complement fragment-induced [Ca2+]i signaling in mouse microglia. J Neurosci. 1997;17:615–624. doi: 10.1523/JNEUROSCI.17-02-00615.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Dowd B F, Heiber M, Chan A, Heng H H, Tsui L C, Kennedy J L, Shi X, Petronis A, George S R, Nguyen T. A human gene that shows identity with the gene encoding the angiotensin receptor is located on chromosome 11. Gene. 1993;136:355–360. doi: 10.1016/0378-1119(93)90495-o. [DOI] [PubMed] [Google Scholar]
- 37.Parham P, Barnstable C J, Bodmer W F. Use of a monoclonal antibody (W6/32) in structural studies of HLA-A,B,C antigens. J Immunol. 1979;123:342–349. [PubMed] [Google Scholar]
- 38.Platt E J, Wehrly K, Kuhmann S E, Chesebro B, Kabat D. Effects of CCR5 and CD4 cell surface concentrations on infections by macrophagetropic isolates of human immunodeficiency virus type 1. J Virol. 1998;72:2855–2864. doi: 10.1128/jvi.72.4.2855-2864.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Price R W, Brew B, Sidtis J, Rosenblum M, Scheck A C, Cleary P. The brain in AIDS: central nervous system HIV-1 infection and AIDS dementia complex. Science. 1988;239:586–592. doi: 10.1126/science.3277272. [DOI] [PubMed] [Google Scholar]
- 40.Rucker J, Edinger A L, Sharron M, Samson M, Lee B, Berson J F, Ti Y, Margulies B, Collman R G, Doranz B J, Parmentier M, Doms R W. Utilization of chemokine receptors, orphan receptors, and herpesvirus-encoded receptors by diverse human and simian immunodeficiency viruses. J Virol. 1997;71:8999–9007. doi: 10.1128/jvi.71.12.8999-9007.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Samson M, Stordeur P, Labbe O, Soularue P, Vassart G, Parmentier M. Molecular cloning and chromosomal mapping of a novel human gene, ChemR1, expressed in T lymphocytes and polymorphonuclear cells and encoding a putative chemokine receptor. Eur J Immunol. 1996;26:3021–3028. doi: 10.1002/eji.1830261230. [DOI] [PubMed] [Google Scholar]
- 42.Schmidtmayerova H, Alfano M, Nuovo G, Bukrinsky M. Human immunodeficiency virus type 1 T-lymphotropic strains enter macrophages via a CD4- and CXCR4-mediated pathway: replication is restricted at a postentry level. J Virol. 1998;72:4633–4642. doi: 10.1128/jvi.72.6.4633-4642.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shieh J T C, Albright A V, Sharron M, Gartner S, Strizki J, Doms R W, González-Scarano F. Chemokine receptor utilization by human immunodeficiency virus type 1 isolates that replicate in microglia. J Virol. 1998;72:4243–4249. doi: 10.1128/jvi.72.5.4243-4249.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43a.Shieh, J. T. C. Unpublished data.
- 44.Strizki J M, Albright A V, Sheng H, O’Connor M, Perrin L, González-Scarano F. Infection of primary human microglia and monocyte-derived macrophages with human immunodeficiency virus type 1 isolates: evidence of differential tropism. J Virol. 1996;70:7654–7662. doi: 10.1128/jvi.70.11.7654-7662.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Turner L, Ward S G, Westwick J. RANTES-activated human T lymphocytes. A role for phosphoinositide 3-kinase. J Immunol. 1995;155:2437–2444. [PubMed] [Google Scholar]
- 46.Tuttle D L, Harrison J K, Anders C, Sleasman J W, Goodenow M M. Expression of CCR5 increases during monocyte differentiation and directly mediates macrophage susceptibility to infection by human immunodeficiency virus type 1. J Virol. 1998;72:4962–4969. doi: 10.1128/jvi.72.6.4962-4969.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu L, Paxton W A, Kassam N, Ruffing N, Rottman J B, Sullivan N, Choe H, Sodroski J, Newman W, Koup R A, Mackay C R. CCR5 levels and expression pattern correlate with infectability by macrophage-tropic HIV-1, in vitro. J Exp Med. 1997;185:1681–1691. doi: 10.1084/jem.185.9.1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yi Y, Rana S, Turner J D, Gaddis N, Collman R G. CXCR-4 is expressed by primary macrophages and supports CCR5-independent infection by dual-tropic but not T-tropic isolates of human immunodeficiency virus type 1. J Virol. 1998;72:772–777. doi: 10.1128/jvi.72.1.772-777.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yong V W, Antel J P. Culture of glial cells from human brain biopsies. In: Fedoroff S, Richardson A, editors. Protocols for neural cell culture. Totowa, N.J: Humana Press; 1992. pp. 81–96. [Google Scholar]