Abstract
Purpose of Review
Periprosthetic infection after shoulder arthroplasty is relatively uncommon though associated with severe long-term morbidity when encountered. The purpose of the review is to summarize the recent literature regarding the definition, clinical evaluation, prevention, and management of prosthetic joint infection after reverse shoulder arthroplasty.
Recent Findings
The landmark report generated at the 2018 International Consensus Meeting on Musculoskeletal Infection has provided a framework for diagnosis, prevention, and management of periprosthetic infections after shoulder arthroplasty. Shoulder specific literature with validated interventions to reduce prosthetic joint infection is limited; however existing literature from retrospective studies and from total hip and knee arthroplasty allows us to make relative guidelines. One and two-stage revisions seem to demonstrate similar outcomes; however, no controlled comparative studies exist limiting the ability to make definitive recommendations between the two options.
Summary
We report on recent literature regarding the current diagnostic, preventative, and treatment options for periprosthetic infection after shoulder arthroplasty. Much of the literature does not distinguish between anatomic and reverse shoulder arthroplasty, and further high-level shoulder specific studies are needed to answer questions generated from this review.
Keywords: Prosthetic joint infection, Reverse total shoulder arthroplasty, Anatomic total shoulder arthroplasty, Prevention, Management, Diagnosis
Introduction
Reverse total shoulder arthroplasty (TSA) is a common procedure for rotator cuff arthropathy, but indications have expanded in recent years [1]. These indications include but are not limited to proximal humerus fractures, revision arthroplasty, and glenohumeral arthritis [2]. With expanding indications frequently comes an expanding risk profile with complication rates after reverse TSA ranging from 7 to 25% in the reported literature. [2–7]. Of those complications, prosthetic joint infection (PJI) has an estimated incidence of 3–8% with median hospitalization cost of over 100% of that of the index procedure [2–11].
Despite the recent guidelines establishing a framework for management of PJI after total hip and knee arthroplasty, the diagnosis, prevention, and management of PJI after shoulder arthroplasty is less well-defined. The aim of this paper is to provide an in-depth review of literature published within the last 5 years, detailing evidence-based practices for clinical evaluation, prevention, and management of prosthetic joint infection after reverse total shoulder arthroplasty.
Definition
In 2018, the International Consensus Meeting on Musculoskeletal Infection (ICM) met to establish a set of guidelines for the diagnosis, prevention, and management of periprosthetic joint infections after shoulder arthroplasty [12–15]. These diagnostic criteria were similar to those developed by the Musculoskeletal Infection Society (MSIS) in 2011 on diagnosis of PJI in the hip and knee [16]. The 2018 ICM defined four separate categories within the diagnosis of prosthetic shoulder infection: definite infection, probable infection, possible infection, and unlikely infection, as seen in Table 1. A definite infection is defined by presence by at least one of the following: (1) presence of a sinus tract, (2) gross intra-articular pus, or (3) two positive tissue cultures with phenotypically identical virulent organisms. In addition, a set of minor criteria seen in Table 2 are established with weighted scores as listed for definition of probable infection, possible infection, or unlikely infection. A total score of 6 or greater with an identified organism indicates probable infection. A score of 6 or greater without an identified organism indicates possible infection. A score of fewer than 6 with either a single positive culture with a virulent organism or a score of fewer than 6 with two positive cultures with a low-virulence organism indicates possible infection. A score of fewer than 6 with negative culture or a score of fewer than 6 only single positive culture with a lower-virulence organism indicates unlikely infection [12].
Table 1.
Definition of prosthetic joint infection after shoulder arthroplasty (from Garrigues et al. [12])
| Category | Definition |
|---|---|
| Definite infection |
Presence of a sinus tract from skin surface to the prosthesis OR Gross intra-articular pus OR Two positive tissue cultures with phenotypically identical virulent organisms |
| Probable infection | Minor Criteria score ≥ 6 with an identified organism |
| Possible infection |
Minor Criteria score ≥ 6 without an identified organism OR Minor Criteria score < 6 with 1 positive culture with virulent organism OR Minor Criteria score < 6 with 2 positive cultures with low-virulence organism |
| Unlikely infection |
Minor Criteria score < 6 with negative cultures OR Minor Criteria score < 6 with only 1 positive culture with low-virulence organism |
Table 2.
Minor criteria for diagnosis of probable, possible, or unlikely infection after shoulder arthroplasty (from Garrigues et al.[12])
| Minor Criteria | Weight |
|---|---|
| Unexpected wound drainage | 4 |
| Single positive tissue culture with virulent organism | 3 |
| Single positive tissue culture with low-virulent organism | 1 |
| Second positive tissue culture (identical low-virulence organism) | 3 |
| Humeral loosening | 3 |
| Positive frozen section (5 PMNs in ≥ 5 high-power fields | 3 |
| Positive preoperative aspirate culture (low or high virulence) | 3 |
| Elevated synovial neutrophil percentage (> 80%)* | 2 |
| Elevated synovial WBC count (> 3000 cells/µL)* | 2 |
| Elevated ESR (> 30 mm/h)* | 2 |
| Elevated CRP level (> 10 mg/L) | 2 |
| Elevated synovial ⍺-defensin | 2 |
| Cloudy fluid | 2 |
PMN polymorphonuclear leukocyte, WBC white blood cell, ESR erythrocyte sedimentation rate, CRP C-reactive protein
*Beyond 6 weeks from recent surgery
Patient Risk Factors
There have been numerous studies that suggest that gender plays a role in susceptibility to infection [8, 9, 17, 18]. Men have been found to have a significantly higher colonization of Cutibacterium acnes (C. acnes), formerly known as Propionibacterium acnes, around the shoulder joint with one study reporting a 81.6% C. acnes superficial colonization rate amongst males [19]. Patients younger than age 65 have been found to have a higher risk of PJI after Reverse TSA [9, 17, 20, 21]. The role of BMI as a risk factor for PJI is still unknown. Work done by Richards et al. found no association between BMI and shoulder PJI [18]. Though prior studies have shown that obesity has no impact on postoperative complications, Cogan et al. recently demonstrated in a large cross-sectional analysis of over 100,000 patients that patients with a higher BMI had higher odds of readmission, deep vein thrombosis/pulmonary embolism, superficial infection, and prosthetic joint infection [22, 23]. There have been mixed results on the impact of comorbidities on shoulder PJI. Numerous studies have reported there being no link between diabetes mellitus and PJI [9, 24, 25]. Cancienne et al. reported that wound complications increase as hemoglobin A1c reaches an inflection point of 8.0 mg/dL [26]. Revisional surgery after primary reverse TSA has been found to increase the risk of PJI [27]. Nezwek et al. reported a 6% infection rate with patients who had revision surgery versus a 2% infection rate with those patients who had no revision [27]. Prior ipsilateral shoulder surgery has also been shown to be a risk factor of subsequent PJI after reverse TSA [28, 29]. Gates et al. demonstrated a 45% positive intra-operative culture rate in patients with no clinical signs of infection and a history of prior ipsilateral shoulder surgery undergoing primary shoulder arthroplasty [28]. While the relevance of the cultures may be debated, Florschütz et al. demonstrated an increased risk (relative risk = 4.8) of shoulder PJI in patients with a history of prior non-arthroplasty shoulder surgery, compared to those with no prior ipsilateral shoulder surgery [29].
History and Physical Examination
The history and physical examination for PJI of the shoulder has a wide range of clinical presentations. The spectrum of signs/symptoms includes erythema, limited range of motion, pain at surgical site, edema, stiffness, wound drainage, draining sinus, and/or exudative drainage [13]. Though rarely present, a draining sinus tract is pathognomonic for PJI, as seen in Fig. 1.
Fig. 1.
Clinical photo of draining sinus tract after shoulder arthroplasty
Radiographic Evaluation
The initial imaging modality in suspected prosthetic shoulder infection is plain radiographs (Fig. 2) to assess for any signs of implant loosening, bone erosion, osteolysis, and dislocation. Plain radiographs are not sensitive to infection for shoulder PJI, but it helps guide the surgeon to an accurate diagnosis when the clinical presentation aligns with typical radiographic findings. Computed tomography (CT) is essential for evaluating the shoulder before revisional surgery to assess hardware loosening and soft tissue edema or abscess formation. CT efficacy mirrors that of plain radiographs: not sensitive or specific to infection, although it can demonstrate the structural changes of bone and soft tissue often present in chronic shoulder PJI.
Fig. 2.
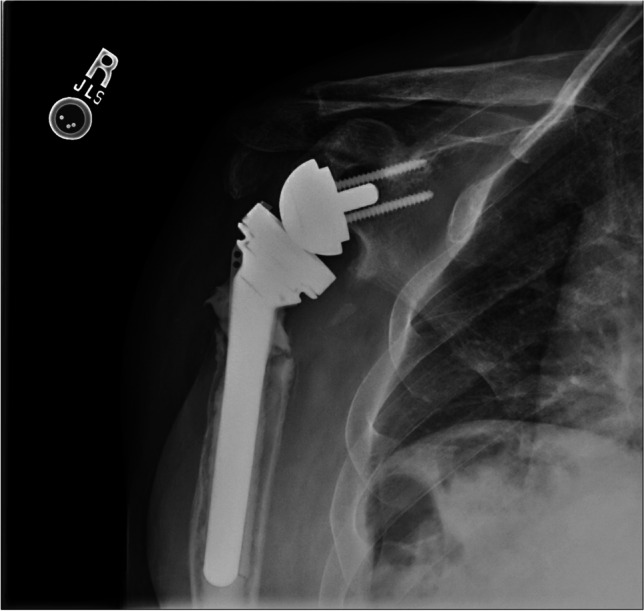
Radiographs of patient 3 years after reverse total shoulder arthroplasty with circumferential radiolucency between bone-cement interface, cortical erosion, and distal cement fracture concerning infection
Laboratory Evaluation
In addition to radiographs, a set of basic labs consisting of a complete white blood cell count (WBC) and inflammatory markers (ESR, CRP) is advised when PJI is suspected [13]. Although this is standard management, numerous studies suggest that these inflammatory markers are not sensitive or specific to shoulder PJI [13, 30]. A retrospective review analyzing the accuracy of ESR and CRP found an overall sensitivity of 16% and 42%, respectively, in the shoulder [31]. Increasingly, serum D-dimer levels are being used to aid in the diagnosis of PJI in hip and knee arthroplasty. Shahi et al., in a prospective study on 245 patients undergoing primary hip and knee arthroplasty, reported a D-dimer level of 850 ng/mL had a sensitivity of 89% and specificity of 93% for diagnosis of PJI [32]. Looking specifically at shoulder arthroplasty, Zmistowski et al. demonstrated elevated D-dimer in patients with definite or probable infections (median 661 ng/mL), compared with those with possible infections or those who were unlikely to have an infection (263 ng/mL). Taken in isolation, the diagnostic value is limited with a D-dimer level of 598 ng/mL, demonstrating 61% sensitivity and 74% specificity for diagnosing a definite or probable infection, according to the ICM definitions. [33] Further research is needed to evaluate the role of D-dimer in combination with other clinical, radiographic, and laboratory diagnostic markers of PJI.
Synovial Fluid Analysis and Microbiology
Synovial fluid analysis may add valuable information in the initial workup for shoulder PJI. The 2018 ICM minor criteria for PJI is synovial WBC > 3000 cells/μL and neutrophil concentration > 80% [13]. Synovial fluid alpha-defensin is a lab value that has been widely studied in the diagnosis of PJI in the after total joint arthroplasty [34, 35]. Frangiamore et al. reported an alpha-defensin shoulder PJI sensitivity and specificity of 63% and 85%, respectively [34]. While this is lower than the reported sensitivity in hip and knee literature, it is still included in the minor criteria of the 2018 ICM definition of PJI [12, 36].
Numerous studies have demonstrated that C. acnes is the main culprit behind shoulder PJI. C. acnes is a gram positive rod found on skin flora and resides on sebum-rich pilosebaceous hair follicles [37]. Its indolent course and ability to make biofilms on prosthetic implants make it hard to detect, requiring cultures to be held for at least 14 days in an anaerobic medium [38]. Studies have implicated C. acnes in 28 to 79% all shoulder PJI [11, 12, 17, 37, 39, 40]. Specifically looking at revisions, Pottinger et al. reported that 70% were associated with C. acnes [20]. In a 2016 systematic review by Nelson et al., it was reported that C. acnes was implicated in 38.9% of all shoulder PJI, followed by Staphylococcus aureus at 14.8% and Staphylococcus epidermidis at 14.5% [41]. It is important to keep in mind that while helpful aspiration may not be negative though, this does not exclude infection of the shoulder.
Prevention
Optimizing Modifiable Risk Factors
As previously discussed, there are multiple risk factors associated with PJI, some of which can be modified to mitigate the risk of PJI. While corticosteroid injections are a common treatment used in the non-operative management of glenohumeral arthritis, use in the perioperative setting has been linked to increased risk of shoulder PJI. Werner et al. showed that patients who received an ipsilateral shoulder corticosteroid injection within 3 months prior to surgery had a 2 times increased risk of PJI. They found no increased risk of infection in patients that received an injection 3–12 months prior to arthroplasty [42].
Diabetes is also a known risk factor for poor wound healing after surgery, including shoulder arthroplasty. Querying a national database, Cancienne et al. reported a nearly 1.5 times odds of deep infection in patients with diabetes and using receiver operating characteristic analysis demonstrated a HbA1c of 8.0 mg/dL was a threshold to markedly increased risk of infection [26]. Despite this, there is still no validated study demonstrating use of a cutoff HbA1c level or evidence that delaying surgery until HbA1c is below a specific cutoff decreases risk of PJI.
Hatta et al. demonstrated that among patients who underwent reverse or anatomic TSA, current and former smokers had significantly higher risk of periprosthetic infection in comparison with non-smokers (hazard ratio [HR], 7.27 and 4.56, respectively) [43]. They defined former smokers as patient who had a documented history of tobacco use, in the form of cigarettes, cigars, or chewing tobacco during his or her lifetime but did not smoke within 1 month before surgery. Though they documented a lower hazard ratio of PJI in a former smoker using non-smokers as the reference, there was no significant difference when using multivariable analysis to directly compare being a former smoker to a current smoker. Overall, the causal effect of smoking cessation remains unclear in limiting PJI risk after TSA.
In terms of intra and post-operative modifiable risk factors, limiting blood loss may have some role in decreasing risk of PJI. Everhart et al. found perioperative blood transfusion increased risk of periprosthetic shoulder infection in a dose-dependent manner, with a relative risk of 1.86 times per unit of packed red blood cells [44]. Grier et al. similarly showed a two times greater odds of infection in patients who received a perioperative blood transfusion [45]. Prior studies have demonstrated treatment of pre-operative anemia before joint arthroplasty can decrease transfusion rates. Kotze et al. found using a protocol of erythropoietin, vitamin B12, or folate supplementation they was able to cut pre-operative anemia prevalence from 26 to 10% before elective total hip or knee arthroplasty [46]. It is not clear whether transfusion itself is associated with the development of shoulder PJI or if it is a proxy for poor surgical hemostasis and hematoma formation following reverse TSA that is the causative factor. Intraoperative use of antifibrinolytic agents, tranexamic acid (TXA), or ε-aminocaproic acid has also been shown to decrease transfusion rates in shoulder arthroplasty patients [47, 48]. Although TXA can pose a theoretical risk of thromboembolism in patients with prior history, it can be delivered topically which may be preferable in these patients and was found to be similarly effective to IV TXA in reducing blood loss and transfusion rates [48]. The 2018 ICM states there is no evidence for routine TXA administration to decrease PJI risk in the shoulder, Hong et al., however, reported lower odds (OR 0.49) of PJI after total hip or knee replacement with administration of TXA on the day of surgery [15, 49]. Further studies are needed to look at the direct efficacy of TXA protocols on shoulder PJI prevention.
Topical Treatments and Skin Preparation
Literature on the use of different topical skin preparation treatments has demonstrated decreased bacterial load, though the efficacy of these treatments to decrease incidence of PJI is still unclear [50–55]. Surgical preparation with chlorhexidine and perioperative administration of cefazolin alone are not capable of eliminating the C. acnes bacterium on the skin because of its unique niche within pilosebaceous glands [55]. Addition of 5% benzoyl peroxide and 3% hydrogen peroxide has both been shown to decrease C. acnes bacterial burden on the skin without significant adverse reactions [50, 52, 55]. Despite this, the 2018 ICM states there is no evidence for or against the use of topical skin treatments to reduce of shoulder PJI; though they may present as a low cost, low-risk adjunct in the prevention of shoulder PJI [11, 15].
In terms of pre-operative scrubs and surgical preparation solution, the 2018 ICM does recommend chlorhexidine gluconate (CHG) showers or cleansing wipes with at least 2 applications decrease the incidence of positive skin culture findings prior to shoulder surgery [15]. Murray et al., in their randomized control trial, demonstrated a lower positive culture rate (66% vs 94%) after use of 2% chlorhexidine no-rinse cloths applied twice prior to shoulder surgery, compared with a control group that only used soap [56]. In addition, based on Level I evidence by Saltzman et al., the 2018 ICM recommended the use of 2% CHG and 70% isopropyl alcohol, such as ChloraPrep (Becton Dickinson, Franklin Lakes, NJ, USA), prior to shoulder arthroplasty [12, 57].
Perioperative Antibiotic Prophylaxis
The 2018 ICM recommended that, for patients undergoing shoulder arthroplasty, a weight-based dose of IV cefazolin be administered within 30–60 min prior to incision; with redosing performed every 4 h, and, post-operative dosing not be extended beyond 24 h. For those with a serious β-lactam allergy, they recommended administration of Vancomycin, 15 mg/kg (max dose 2 g) within 1–2 h prior to incision with post-operative doses not to be given past 24 h [15]. For those with a personal history of MRSA infection or colonization, they recommended both vancomycin and cefazolin [15]. Use of clindamycin as an alternative in the setting severe β-lactam allergy has fallen out of favor after Yian et al. recently demonstrated a 3.5 times increased risk of infection in patients who underwent shoulder arthroplasty and received clindamycin alone, compared to those who received vancomycin or cefazolin [58].
There has been increasing use of vancomycin powder as an adjunct in the prevention of shoulder PJI, as it has been demonstrated in the total hip and knee literature to reduce incidence of PJI [59]. Miquel et al. recently demonstrated that administration of vancomycin powder to a bioartificial shoulder joint model shown to be biomimetic of shoulder PJI, completely eradicated C. acnes colonies analyzed 48 h after administration. Additionally, vancomycin powder had no discernible short-term impact on shoulder capsule cell morphology [60, 61]. Use of povidone-iodine solution lavage has also shown promising results of reduction in skin and soft tissue infections in the spine literature [15, 62, 63]. However, literature for its use in shoulder arthroplasty is deficient and its negative influence on osteoblast proliferation in vitro may limit its use in the setting of greater tuberosity fracture [64]. Furthermore, from a practical standpoint, the oblique orientation of the shoulder field due to modified beach chair positioning tends to preferentially promote lavage distribution to the inferior aspect of the wound. Consensus from the 2018 ICM is that both dilute povidone-iodine and/or vancomycin powder may have a role in patients considered at high risk of PJI, though more shoulder specific research is needed [15].
Blue Light Therapy
In in vitro studies, C. acnes strains isolated from patients with shoulder PJI were found to be highly sensitive to blue light therapy in combination with specific photosensitizers [24]. The 2019 study by Grogan et al. was selected as the inaugural winner of the PJI research grant by the American Shoulder and Elbow Surgeons, though its clinical utilization is not yet widespread. The same research group is currently running a clinical trial on “Efficacy of blue light therapy at reducing bioburden of C. acnes at the deltopectoral interval” [65, 66]. Further investigation is clearly warranted but, if efficacious, it would represent an interesting novel treatment with a limited risk profile.
Management
After diagnostic confirmation, various treatment options including non-operative treatment, one-stage revision, two-stage revision, and or multistage revision with open biopsies have been proposed for the management of shoulder PJI [40, 67, 68]. To help decide between which of these treatment options is the most appropriate one should consider multiple factors including duration of infection, patient overall health and risk profile, and desired functional goals.
Operative Treatment Options
One-stage management includes irrigation and debridement with wide excision of infected tissue and either complete exchange of components or primary component retention. Intravenous antibiotic therapy is prescribed based on pre-operative or intra-operative culture sensitivities and can vary in duration in the literature [69]. Two-stage management includes complete implant removal and placement of an antibiotic spacer with a period of intravenous antibiotics that varies from 10 days to 3 months depending on patient response and responsible pathologic organism [14, 40, 67]. Reported techniques for the first stage of two-stage treatment widely vary in types of cement used, the amount of antibiotics in the cement, the use of prefabricated implants, or the use of intraoperatively handmade implants with or without the use of commercially designed spacer molds. Despite the varying techniques, there is little literature to suggest the superiority of a specific implant design or antibiotic cement regimen [70]. After clinical and laboratory markers suggest eradication of infection, the second stage is performed consisting of removal of the antibiotic spacer and implantation of revision components.
Tseng et al. has also described a three-stage revision protocol. In their protocol, the first stage consists of explant of components, thorough irrigation and debridement, placement of an antibiotic spacer, and a 6-week course of intravenous antibiotics. After completion of antibiotics, patients will undergo a 4-week antibiotic-free interval followed by an intermediate stage open biopsy to confirm eradication of infection. After cultures have been negative for at least 14 days, patients will return for removal of antibiotic spacer and implantation of revision components [71]. Zhang et al. similarly reported on such a technique, though also noted in his protocol if intermediate stage biopsy cultures were positive, then the patient would undergo another formal irrigation and debridement, exchange of the antibiotic spacer, and 6-week course of directed antibiotic therapy [68].
Outcomes from One-stage vs Two-Stage Management
Two-stage management is standard of care for hip and knee PJI and generally considered the most reliable treatment for management of shoulder PJI [14, 40, 67, 72]. Despite this, based on the available evidence, single stage revision has been advocated to achieve similar infection control while minimizing perioperative risks and soft tissue deterioration associated with two stage procedures [69, 73]. In the 2018 ICM, a meta-analysis aggregated 161 cases (12 articles) of PJI, managed with single-stage and 325 cases (27 articles), and managed with 2-stage revision [14]. In their meta-analysis, they found a lower reinfection rate (5.6% vs 11.4%) and lower complication rate (12.7% vs 21.9%) after one-stage management, compared with two-stage management. Final reported functional outcome scores were also similar between groups (Constant-Murley score 49.1 for one-stage and 51.1 for two-exchange) [14].
These aggregated results do not take into timing of infection between acute, subacute, and chronic. This may add additional selection bias, particularly in the setting of more chronic and challenging revision cases where there is a preference towards two-stage procedures. Although there is inconsistent reporting of timing of infection, the majority of studies that report timing of infection classify acute as < 3 months, subacute as 3–12 months, and chronic as > 12 months [14]. Looking specifically at acute PJI, the 2018 ICM found 6 cases were treated with one-stage management, none of whom had reinfection at final follow-up [14]. With such few cases, the committee was unable to make concrete recommendations on management of acute PJI with one- vs two-stage revision.
Regarding management of subacute and chronic PJI, the 2018 ICM found four studies evaluating revision success rate for shoulder PJI with single-stage exchange between subacute or chronic presentation with a reinfection rate of 12.5% for chronic cases and 5.3% for subacute cases. They additionally found three studies specifically looking at success rate for two-stage exchange for sub-acute or chronic PJI with a reinfection rate of 6.3% for chronic cases and 29.4% for subacute cases [14]. They argue that selection bias may have a large role in the discrepancy with more severe infections being treated with two-stage revision [14]. Overall single stage management appears a promising and viable option for treatment of shoulder PJI; however, however there are no studies controlling for various risk factors such as pathogens, timing of infection, and diagnostic features. As such, the 2018 ICM was unable to make a strong recommendation for use of single-stage exchange in place of 2-stage exchange for shoulder PJI [14].
Multiple stage procedures with intermediate stage biopsy has been utilized by Zhang et al. given concerns for latent infections after standard 6-week antibiotic therapy. They demonstrated in their study looking at patients undergoing treatment with their multistage method for shoulder PJI; 22% of patients had evidence of persistent infection during their open biopsy procedure. All 18 patients treated with intermediate stage open biopsy in their study showed no signs of recurrent infection at 24 months after reimplantation [68]. Similarly, Tseng et al. looked at a matched cohort of 27 patients who underwent three-stage revision to RTSA for PJI, as described by Zhang et al., compared with 27 patients who underwent revision to RTSA for aseptic indications. They found no differences between infected and non-infected revisions in range of motion for forward flexion (121° ± 33° vs. 129° ± 30), abduction (117° ± 41° vs. 115° ± 36°), external rotation (29° ± 27° vs. 35° ± 21°), internal rotation (L4 vs. L2), VAS pain score (1.71 ± 1.76 vs. 1.33 ± 1.72), or ASES subjective score at the final follow-up (71.4 ± 22.7 vs. 74.3 ± 14.0)[71].
Overall surgeons must take multiple factors into account when determining treatment protocols including patient comorbidities, the risk of missing subclinical indolent infections, longer hospital stays with more aggressive treatment, and the risk of multiple operative interventions [40, 68].
Single Stage with Implant Retention
Specifically looking at one-stage revision, some surgeons elect to retain the primary implants at time of surgery, though studies demonstrate low rates of overall eradication of infection in both the acute and chronic settings with this method [14]. In the acute setting, the 2018 ICM looked at 4 studies (38 shoulders) of patients treated with I&D and implant retention and found a 50% failure rate [14, 74–77]. They demonstrated similar findings in the case of subacute and chronic PJI with a 47% eradication rate [14]. Despite this, eradication of infection must be weighed with other risks of surgery. A French multicenter study looking at patients with PJI after reverse shoulder arthroplasty reported a 15% complication rate and 54% infection eradication rate after debridement, modular component exchange, and partial component retention. While the risk of residual infection was high, the complication rate was lower than that reported for resection (33%), 1-stage revision (20%), or 2-stage revision (36%) [78]. Overall, component retention should remain an option particularly in physiologically frail patients in whom more aggressive surgery incur significant perio-operatie risk, but clear informed consent between the surgeon and patient on the substantially higher rate of infection recurrence is vital.
Unexpected Positive Culture
Unexpected positive cultures (UPC) at time of revision arthroplasty present a unique challenge with limited literature on outcomes to guide treatment recommendations. Hsu et al. reported on 55-revision shoulder arthroplasties without infection treated with 3 weeks of antibiotics, compared to those with > 2 UPCs treated with 6 months of antibiotics. They demonstrated no difference in pain or functional outcomes [79]. Padegimas also reported on 28 individuals with UPC after revision shoulder arthroplasty, compared to 89 individuals with negative cultures. Individuals were treated with 2 weeks of oral antibiotics followed by 6 weeks of additional antibiotics for those treated for infection. A higher percentage of patients with UPC underwent reoperation (20.2%) than those without (7.1%), but this difference was not statistically significant [80]. Overall, the lack of comparative data on outcomes and the significance of these cultures are still debated, making it difficult to conclusively determine optimal management. Moreover, the unclear clinical significance of UPC makes use of the 2018 ICM criteria a valuable tool in objectively placing the role of positive cultures in a broader context of PJI risk.
Treatment of Low-Demand or High Perioperative Risk Individuals
Definitive treatment with irrigation and debridement, implant removal, and antibiotic spacer placement without plan for reimplantation of arthroplasty components is an option to be considered for select patients. Pelligrini et al. reported no recurrent infections with good pain relief and improvement in outcome scores in 19 patients with shoulder PJI treated definitively with antibiotic spacer [81]. Jawa et al. similarly looked 12 patients who underwent antibiotic spacer placement for shoulder PJI as definitive treatment after declining to proceed with the second stage and found a higher infection recurrence rate of 18% [82]. Though this technique is not without complications, McFarland et al. evaluated outcomes of patients who had antibiotic spacer placed after shoulder PJI and reported 18 complications in 14 patients including glenoid and humeral shaft erosion, spacer fracture or migration, and humerus fractures [83].
Alternatively, one can consider non-operative treatment with a course of intravenous antibiotic therapy followed by chronic oral suppressive therapy. Most of the literature of this technique comes from our understanding of its role in other arthroplasty procedures with the 2018 ICM only identifying 8 total shoulder cases treated with chronic suppressive therapy in their systematic review [14]. Additionally, most studies report on chronic suppressive therapy after initial surgical procedure such as evacuation of abscess or debridement. As such, the 2018 ICM was unable to give a recommendation for the type and duration of suppressive therapy in shoulder PJI but did acknowledge that it may have a role in select cases such as those who have high risk of perioperative complications with revision surgery [14].
Conclusion
Prosthetic joint infection after shoulder arthroplasty is a low-risk complication, though it can lead to significant morbidity for those patients affected. The 2018 International Consensus Meeting on Musculoskeletal Infection established a framework for proper diagnosis and general management; through the efficacy of mitigation protocols, staged versus non-staged surgical treatment, and appropriate choice and duration of antibiotics can be evaluated. Current management strategies for diagnosis and management of shoulder PJI were largely extrapolated from hip and knee arthroplasty literature, although it is becoming increasingly clear that the microbial environment and soft tissue considerations for the shoulder joint are unique. Further shoulder-specific, high-level evidence is needed to better guide future recommendations in the management of prosthetic joint infections.
Declarations
Conflict of Interest
C. Benjamin Ma has received consultant funds from Stryker, research support from Zimmer Biomet National Institutes of Health, Aesculap, and SLACK. Brian T. Feeley has received research support from Orthofix, holds stock options in Bioniks and Kaliber, and has received hospitality payments from Zimmer Biomet. Alexander R. Markes, Joseph Bigham, and Jaicharan J. Iyengar declare that they have no conflicts of interest to report.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Alexander R. Markes, Email: Alexander.Markes@ucsf.edu
Joseph Bigham, Email: josephbigham32@gmail.com.
C. Benjamin Ma, Email: Maben@ucsf.edu.
Jaicharan J. Iyengar, Email: jciyengar@hotmail.com
Brian T. Feeley, Email: Brian.Feeley@ucsf.edu
References
- 1.Rugg CM, Coughlan MJ, Lansdown DA. Reverse total shoulder arthroplasty: biomechanics and indications. Curr Rev Musculoskelet Med. 2019;12:542–53. doi: 10.1007/s12178-019-09586-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheung E, Willis M, Walker M, Clark R, Frankle MA. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2011;19:439–49. [PubMed] [Google Scholar]
- 3.Saltzman BM, Chalmers PN, Gupta AK, Romeo AA, Nicholson GP. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1647–54. doi: 10.1016/j.jse.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Affonso J, Nicholson GP, Frankle MA, Walch G, Gerber C, Garzon-Muvdi J, et al. Complications of the reverse prosthesis: prevention and treatment. Instr Course Lect. 2012;61:157–68. [PubMed] [Google Scholar]
- 5.Ma GC, Bradley KE, Jansson H, Feeley BT, Zhang AL, Ma CB. Surgical complications after reverse total shoulder arthroplasty and total shoulder arthroplasty in the United States. J Am Acad Orthop Surg Glob Res Rev. 2021;5. [DOI] [PMC free article] [PubMed]
- 6.Somerson JS, Hsu JE, Neradilek MB, Matsen FA. Analysis of 4063 complications of shoulder arthroplasty reported to the US Food and Drug Administration from 2012 to 2016. J Shoulder Elbow Surg. 2018;27:1978–86. doi: 10.1016/j.jse.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 7.Wierks C, Skolasky RL, Ji JH, McFarland EG. Reverse total shoulder replacement: intraoperative and early postoperative complications. Clin Orthop. 2009;467:225–34. doi: 10.1007/s11999-008-0406-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kunutsor SK, Barrett MC, Whitehouse MR, Craig RS, Lenguerrand E, Beswick AD, et al. Incidence, temporal trends and potential risk factors for prosthetic joint infection after primary total shoulder and elbow replacement: systematic review and meta-analysis. J Infect. 2020;80:426–36. doi: 10.1016/j.jinf.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Morris BJ, O’Connor DP, Torres D, Elkousy HA, Gartsman GM, Edwards TB. Risk factors for periprosthetic infection after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:161–6. doi: 10.1016/j.jse.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 10.Moeini S, Rasmussen JV, Salomonsson B, Domeij-Arverud E, Fenstad AM, Hole R, et al. Reverse shoulder arthroplasty has a higher risk of revision due to infection than anatomical shoulder arthroplasty: 17 730 primary shoulder arthroplasties from the Nordic Arthroplasty Register Association. Bone Jt J. 2019;101-B:702–7. [DOI] [PubMed]
- 11.Contreras ES, Frantz TL, Bishop JY, Cvetanovich GL. Periprosthetic infection after reverse shoulder arthroplasty: a review. Curr Rev Musculoskelet Med. 2020;13:757–68. doi: 10.1007/s12178-020-09670-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garrigues GE, Zmistowski B, Cooper AM, Green A, Hsu J, Ricchetti E, et al. Proceedings from the 2018 International Consensus Meeting on Orthopedic Infections: the definition of periprosthetic shoulder infection. J Shoulder Elbow Surg. 2019;28:S8–12. doi: 10.1016/j.jse.2019.04.034. [DOI] [PubMed] [Google Scholar]
- 13.Garrigues GE, Zmistowski B, Cooper AM, Green A, Abboud J, Beazley J, et al. Proceedings from the 2018 International Consensus Meeting on Orthopedic Infections: evaluation of periprosthetic shoulder infection. J Shoulder Elbow Surg. 2019;28:S32–66. doi: 10.1016/j.jse.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 14.Garrigues GE, Zmistowski B, Cooper AM, Green A, Abboud J, Beasley J, et al. Proceedings from the 2018 International Consensus Meeting on Orthopedic Infections: management of periprosthetic shoulder infection. J Shoulder Elbow Surg. 2019;28:S67–99. doi: 10.1016/j.jse.2019.04.015. [DOI] [PubMed] [Google Scholar]
- 15.Garrigues GE, Zmistowski B, Cooper AM, Green A. ICM Shoulder Group. Proceedings from the 2018 international consensus meeting on orthopedic infections: prevention of periprosthetic shoulder infection J Shoulder Elbow Surg. 2019 28 S13 31. [DOI] [PubMed]
- 16.Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop. 2011;469:2992–4. doi: 10.1007/s11999-011-2102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Padegimas EM, Maltenfort M, Ramsey ML, Williams GR, Parvizi J, Namdari S. Periprosthetic shoulder infection in the United States: incidence and economic burden. J Shoulder Elbow Surg. 2015;24:741–6. doi: 10.1016/j.jse.2014.11.044. [DOI] [PubMed] [Google Scholar]
- 18.Richards J, Inacio MCS, Beckett M, Navarro RA, Singh A, Dillon MT, et al. Patient and procedure-specific risk factors for deep infection after primary shoulder arthroplasty. Clin Orthop. 2014;472:2809–15. doi: 10.1007/s11999-014-3696-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chuang MJ, Jancosko JJ, Mendoza V, Nottage WM. The incidence of Propionibacterium acnes in shoulder arthroscopy. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2015;31:1702–7. doi: 10.1016/j.arthro.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 20.Pottinger P, Butler-Wu S, Neradilek MB, Merritt A, Bertelsen A, Jette JL, et al. Prognostic factors for bacterial cultures positive for Propionibacterium acnes and other organisms in a large series of revision shoulder arthroplasties performed for stiffness, pain, or loosening. J Bone Joint Surg Am. 2012;94:2075–83. doi: 10.2106/JBJS.K.00861. [DOI] [PubMed] [Google Scholar]
- 21.Singh JA, Sperling JW, Schleck C, Harmsen WS, Cofield RH. Periprosthetic infections after total shoulder arthroplasty: a 33-year perspective. J Shoulder Elbow Surg. 2012;21:1534–41. doi: 10.1016/j.jse.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cogan CJ, Flores SE, Freshman RD, Chi HM, Feeley BT. Effect of obesity on short and long-term complications of shoulder arthroplasty. J Shoulder Elbow Surg. 2022;S1058–2746(22):00687–5. doi: 10.1016/j.jse.2022.07.028. [DOI] [PubMed] [Google Scholar]
- 23.Jiang JJ, Somogyi JR, Patel PB, Koh JL, Dirschl DR, Shi LL. Obesity is not associated with increased short-term complications after primary total shoulder arthroplasty. Clin Orthop. 2016;474:787–95. doi: 10.1007/s11999-015-4584-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McElvany MD, Chan PH, Prentice HA, Paxton EW, Dillon MT, Navarro RA. Diabetes disease severity was not associated with risk of deep infection or revision after shoulder arthroplasty. Clin Orthop. 2019;477:1358–69. doi: 10.1097/CORR.0000000000000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seok H-G, Park J-J, Park S-G. Risk factors for periprosthetic joint infection after shoulder arthroplasty: systematic review and meta-analysis. J Clin Med. 2022;11:4245. doi: 10.3390/jcm11144245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cancienne JM, Brockmeier SF, Werner BC. Association of perioperative glycemic control with deep postoperative infection after shoulder arthroplasty in patients with diabetes. J Am Acad Orthop Surg. 2018;26:e238–45. doi: 10.5435/JAAOS-D-16-00784. [DOI] [PubMed] [Google Scholar]
- 27.Nezwek TA, Dutcher L, Mascarenhas L, Woltemath A, Thirumavalavan J, Lund J, et al. Prior shoulder surgery and rheumatoid arthritis increase early risk of infection after primary reverse total shoulder arthroplasty. JSES Int. 2021;5:1062–6. doi: 10.1016/j.jseint.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gates S, Nguyen I, Del Core M, Nakonezny PA, Bradley H, Khazzam M. Incidence and predictors of positive intraoperative cultures in primary shoulder arthroplasty following prior ipsilateral shoulder surgery. JSES Int. 2020;4:366–71. doi: 10.1016/j.jseint.2019.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Florschütz AV, Lane PD, Crosby LA. Infection after primary anatomic versus primary reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:1296–301. doi: 10.1016/j.jse.2014.12.036. [DOI] [PubMed] [Google Scholar]
- 30.Shields MV, Abdullah L, Namdari S. The challenge of Propionibacterium acnes and revision shoulder arthroplasty: a review of current diagnostic options. J Shoulder Elbow Surg. 2016;25:1034–40. doi: 10.1016/j.jse.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 31.Berbari E, Mabry T, Tsaras G, Spangehl M, Erwin PJ, Murad MH, et al. Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am. 2010;92:2102–9. doi: 10.2106/JBJS.I.01199. [DOI] [PubMed] [Google Scholar]
- 32.Shahi A, Kheir MM, Tarabichi M, Hosseinzadeh HRS, Tan TL, Parvizi J. Serum D-dimer test is promising for the diagnosis of periprosthetic joint infection and timing of reimplantation. J Bone Jt Surg. 2017;99:1419–27. doi: 10.2106/JBJS.16.01395. [DOI] [PubMed] [Google Scholar]
- 33.Zmistowski B, Chang M, Shahi A, Nicholson T, Abboud J, Lazarus M, et al. Is D-dimer a reliable serum marker for shoulder periprosthetic joint infection? Clin Orthop. 2021;479:1447–54. doi: 10.1097/CORR.0000000000001774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frangiamore SJ, Saleh A, Grosso MJ, Kovac MF, Higuera CA, Iannotti JP, et al. α-Defensin as a predictor of periprosthetic shoulder infection. J Shoulder Elbow Surg. 2015;24:1021–7. doi: 10.1016/j.jse.2014.12.021. [DOI] [PubMed] [Google Scholar]
- 35.Lee YS, Koo K-H, Kim HJ, Tian S, Kim T-Y, Maltenfort MG, et al. Synovial fluid biomarkers for the diagnosis of periprosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am. 2017;99:2077–84. doi: 10.2106/JBJS.17.00123. [DOI] [PubMed] [Google Scholar]
- 36.Lee DH, Choi YS, Potter HG, Endo Y, Sivakumaran T, Lim TK, et al. Reverse total shoulder arthroplasty: an imaging overview. Skeletal Radiol. 2020;49:19–30. doi: 10.1007/s00256-019-03275-0. [DOI] [PubMed] [Google Scholar]
- 37.Koh CK, Marsh JP, Drinković D, Walker CG, Poon PC. Propionibacterium acnes in primary shoulder arthroplasty: rates of colonization, patient risk factors, and efficacy of perioperative prophylaxis. J Shoulder Elbow Surg. 2016;25:846–52. doi: 10.1016/j.jse.2015.09.033. [DOI] [PubMed] [Google Scholar]
- 38.Boisrenoult P. Cutibacterium acnes prosthetic joint infection: diagnosis and treatment. Orthop Traumatol Surg Res OTSR. 2018;104:S19–24. doi: 10.1016/j.otsr.2017.05.030. [DOI] [PubMed] [Google Scholar]
- 39.Belay ES, Danilkowicz R, Bullock G, Wall K, Garrigues GE. Single-stage versus two-stage revision for shoulder periprosthetic joint infection: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2020;29:2476–86. doi: 10.1016/j.jse.2020.05.034. [DOI] [PubMed] [Google Scholar]
- 40.Markes AR, Cheung E, Ma CB. Failed reverse shoulder arthroplasty and recommendations for revision. Curr Rev Musculoskelet Med. 2020;13:1–10. doi: 10.1007/s12178-020-09602-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nelson GN, Davis DE, Namdari S. Outcomes in the treatment of periprosthetic joint infection after shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2016;25:1337–45. doi: 10.1016/j.jse.2015.11.064. [DOI] [PubMed] [Google Scholar]
- 42.Werner BC, Cancienne JM, Burrus MT, Griffin JW, Gwathmey FW, Brockmeier SF. The timing of elective shoulder surgery after shoulder injection affects postoperative infection risk in Medicare patients. J Shoulder Elbow Surg. 2016;25:390–7. doi: 10.1016/j.jse.2015.08.039. [DOI] [PubMed] [Google Scholar]
- 43.Hatta T, Werthel J-D, Wagner ER, Itoi E, Steinmann SP, Cofield RH, et al. Effect of smoking on complications following primary shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1–6. doi: 10.1016/j.jse.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 44.Everhart JS, Bishop JY, Barlow JD. Medical comorbidities and perioperative allogeneic red blood cell transfusion are risk factors for surgical site infection after shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1922–30. doi: 10.1016/j.jse.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 45.Grier AJ, Bala A, Penrose CT, Seyler TM, Bolognesi MP, Garrigues GE. Analysis of complication rates following perioperative transfusion in shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1203–9. doi: 10.1016/j.jse.2016.11.039. [DOI] [PubMed] [Google Scholar]
- 46.Kotzé A, Carter LA, Scally AJ. Effect of a patient blood management programme on preoperative anaemia, transfusion rate, and outcome after primary hip or knee arthroplasty: a quality improvement cycle. Br J Anaesth. 2012;108:943–52. doi: 10.1093/bja/aes135. [DOI] [PubMed] [Google Scholar]
- 47.Koutserimpas C, Besiris GT, Giannoulis D, Raptis K, Vlasis K, Dretakis K, et al. Tranexamic acid in shoulder arthroplasty. A comprehensive review. Maedica (Bucur). 2021;16(1):97–101. [DOI] [PMC free article] [PubMed]
- 48.Kuo L-T, Hsu W-H, Chi C-C, Yoo JC. Tranexamic acid in total shoulder arthroplasty and reverse shoulder arthroplasty: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2018;19:60. doi: 10.1186/s12891-018-1972-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hong GJ, Wilson LA, Liu J, Memtsoudis SG. Tranexamic acid administration is associated with a decreased odds of prosthetic joint infection following primary total hip and primary total knee arthroplasty: a national database analysis. J Arthroplasty. 2021;36:1109–13. doi: 10.1016/j.arth.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 50.Kolakowski L, Lai JK, Duvall GT, Jauregui JJ, Dubina AG, Jones DL, et al. Neer Award 2018: Benzoyl peroxide effectively decreases preoperative Cutibacterium acnes shoulder burden: a prospective randomized controlled trial. J Shoulder Elbow Surg. 2018;27:1539–44. doi: 10.1016/j.jse.2018.06.012. [DOI] [PubMed] [Google Scholar]
- 51.Duvall G, Kaveeshwar S, Sood A, Klein A, Williams K, Kolakowski L, et al. Benzoyl peroxide use transiently decreases Cutibacterium acnes load on the shoulder. J Shoulder Elbow Surg. 2020;29:794–8. doi: 10.1016/j.jse.2019.06.026. [DOI] [PubMed] [Google Scholar]
- 52.Stull JD, Nicholson TA, Davis DE, Namdari S. Addition of 3% hydrogen peroxide to standard skin preparation reduces Cutibacterium acnes-positive culture rate in shoulder surgery: a prospective randomized controlled trial. J Shoulder Elbow Surg. 2020;29:212–6. doi: 10.1016/j.jse.2019.09.038. [DOI] [PubMed] [Google Scholar]
- 53.Hernandez P, Sager B, Fa A, Liang T, Lozano C, Khazzam M. Bactericidal efficacy of hydrogen peroxide on Cutibacterium acnes. Bone Jt Res. 2019;8:3–10. doi: 10.1302/2046-3758.81.BJR-2018-0145.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chalmers PN, Beck L, Stertz I, Tashjian RZ. Hydrogen peroxide skin preparation reduces Cutibacterium acnes in shoulder arthroplasty: a prospective, blinded, controlled trial. J Shoulder Elbow Surg. 2019;28:1554–61. doi: 10.1016/j.jse.2019.03.038. [DOI] [PubMed] [Google Scholar]
- 55.Singh AM, Sethi PM, Romeo AA, Anakwenze OA, Abboud JA, Namdari S. Strategies to decolonize the shoulder of Cutibacterium acnes: a review of the literature. J Shoulder Elbow Surg. 2020;29:660–6. doi: 10.1016/j.jse.2019.11.037. [DOI] [PubMed] [Google Scholar]
- 56.Murray MR, Saltzman MD, Gryzlo SM, Terry MA, Woodward CC, Nuber GW. Efficacy of preoperative home use of 2% chlorhexidine gluconate cloth before shoulder surgery. J Shoulder Elbow Surg. 2011;20:928–33. doi: 10.1016/j.jse.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 57.Saltzman MD, Nuber GW, Gryzlo SM, Marecek GS, Koh JL. Efficacy of surgical preparation solutions in shoulder surgery: J Bone Jt Surg-Am Vol. 2009;91:1949–53. [DOI] [PubMed]
- 58.Yian EH, Chan PH, Burfeind W, Navarro RA, Singh A, Dillon MT. Perioperative clindamycin use in penicillin allergic patients is associated with a higher risk of infection after shoulder arthroplasty. J Am Acad Orthop Surg. 2020;28:e270–6. doi: 10.5435/JAAOS-D-19-00168. [DOI] [PubMed] [Google Scholar]
- 59.Iorio R, Yu S, Anoushiravani AA, Riesgo AM, Park B, Vigdorchik J, et al. Vancomycin powder and dilute povidone-iodine lavage for infection prophylaxis in high-risk total joint arthroplasty. J Arthroplasty. 2020;35:1933–6. doi: 10.1016/j.arth.2020.02.060. [DOI] [PubMed] [Google Scholar]
- 60.Miquel J, Huang TB, Athwal GS, Faber KJ, O’Gorman DB. Vancomycin is effective in preventing Cutibacterium acnes growth in a mimetic shoulder arthroplasty. J Shoulder Elbow Surg. 2022;31:159–64. doi: 10.1016/j.jse.2021.06.015. [DOI] [PubMed] [Google Scholar]
- 61.Huang TB, Pena Diaz AM, Faber KJ, Athwal GS, Woolman M, Nygard K, et al. Development of a three-dimensional bioartificial shoulder joint implant mimetic of periprosthetic joint infection. Tissue Eng Part A. 2022;28:175–83. doi: 10.1089/ten.TEA.2021.0081. [DOI] [PubMed] [Google Scholar]
- 62.Tomov M, Mitsunaga L, Durbin-Johnson B, Nallur D, Roberto R. Reducing surgical site infection in spinal surgery with betadine irrigation and intrawound vancomycin powder. Spine. 2015;40:491–9. doi: 10.1097/BRS.0000000000000789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hey HWD, Thiam DW, Koh ZSD, Thambiah JS, Kumar N, Lau L-L, et al. Is intraoperative local vancomycin powder the answer to surgical site infections in spine surgery? Spine. 2017;42:267–74. doi: 10.1097/BRS.0000000000001710. [DOI] [PubMed] [Google Scholar]
- 64.Newton Ede MP, Philp AM, Philp A, Richardson SM, Mohammad S, Jones SW. Povidone-iodine has a profound effect on in vitro osteoblast proliferation and metabolic function and inhibits their ability to mineralize and form bone. Spine. 2016;41:729–34. doi: 10.1097/BRS.0000000000001332. [DOI] [PubMed] [Google Scholar]
- 65.Cotter EJ, Cotter LM, Franczek EB, Godfrey JJ, Hetzel SJ, Safdar N, et al. Efficacy of combinational therapy using blue light and benzoyl peroxide in reducing Cutibacterium acnes bioburden at the deltopectoral interval: a randomized controlled trial. J Shoulder Elbow Surg. 2021;30(12):2671–81. [DOI] [PubMed]
- 66.PJI Research grant - American Shoulder and Elbow Surgeons [Internet]. 2019. Available from: https://www.ases-assn.org/about-ases/pji-research-grant/. Accessed 13 Sept 2022.
- 67.George DA, Volpin A, Scarponi S, Haddad FS, Romanò CL. Does exchange arthroplasty of an infected shoulder prosthesis provide better eradication rate and better functional outcome, compared to a permanent spacer or resection arthroplasty? A Syst Rev. BMC Musculoskelet Disord. 2016;17:52. doi: 10.1186/s12891-016-0901-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang AL, Feeley BT, Schwartz BS, Chung TT, Ma CB. Management of deep postoperative shoulder infections: is there a role for open biopsy during staged treatment? J Shoulder Elbow Surg. 2015;24:e15–20. doi: 10.1016/j.jse.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 69.Klatte TO, Junghans K, Al-Khateeb H, Rueger JM, Gehrke T, Kendoff D, et al. Single-stage revision for peri-prosthetic shoulder infection: outcomes and results. Bone Jt J. 2013;95-B:391–5. [DOI] [PubMed]
- 70.Namdari S, Sudah SY, Menendez ME, Denard PJ. Antibiotic spacers for shoulder periprosthetic joint infection: a review. J Am Acad Orthop Surg. 2022;30:917–24. doi: 10.5435/JAAOS-D-21-00984. [DOI] [PubMed] [Google Scholar]
- 71.Tseng W-J, Lansdown DA, Grace T, Zhang AL, Feeley BT, Hung L-W, et al. Outcomes of revision arthroplasty for shoulder periprosthetic joint infection: a three-stage revision protocol. J Shoulder Elbow Surg. 2019;28:268–75. doi: 10.1016/j.jse.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 72.Fink B, Sevelda F. Periprosthetic joint infection of shoulder arthroplasties: diagnostic and treatment options. BioMed Res Int. 2017;2017:1–10. doi: 10.1155/2017/4582756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beekman PDA, Katusic D, Berghs BM, Karelse A, De Wilde L. One-stage revision for patients with a chronically infected reverse total shoulder replacement. J Bone Joint Surg Br. 2010;92-B:817–22. [DOI] [PubMed]
- 74.Coste JS, Reig S, Trojani C, Berg M, Walch G, Boileau P. The management of infection in arthroplasty of the shoulder. J Bone Joint Surg Br. 2004;86:65–9. [PubMed] [Google Scholar]
- 75.Dennison T, Alentorn-Geli E, Assenmacher AT, Sperling JW, Sánchez-Sotelo J, Cofield RH. Management of acute or late hematogenous infection after shoulder arthroplasty with irrigation, débridement, and component retention. J Shoulder Elbow Surg. 2017;26:73–8. doi: 10.1016/j.jse.2016.05.018. [DOI] [PubMed] [Google Scholar]
- 76.Patel H, Khoury H, Girgenti D, Welner S, Yu H. Burden of surgical site infections associated with select spine operations and involvement of Staphylococcus aureus. Surg Infect. 2017;18:461–73. doi: 10.1089/sur.2016.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ortmaier R, Resch H, Hitzl W, Mayer M, Stundner O, Tauber M. Treatment strategies for infection after reverse shoulder arthroplasty. Eur J Orthop Surg Traumatol Orthop Traumatol. 2014;24:723–31. doi: 10.1007/s00590-013-1251-9. [DOI] [PubMed] [Google Scholar]
- 78.Jacquot A, Sirveaux F, Roche O, Favard L, Clavert P, Molé D. Surgical management of the infected reversed shoulder arthroplasty: a French multicenter study of reoperation in 32 patients. J Shoulder Elbow Surg. 2015;24:1713–22. doi: 10.1016/j.jse.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 79.Hsu JE, Gorbaty JD, Whitney IJ, Matsen FA. Single-stage revision is effective for failed shoulder arthroplasty with positive cultures for propionibacterium. J Bone Jt Surg. 2016;98:2047–51. doi: 10.2106/JBJS.16.00149. [DOI] [PubMed] [Google Scholar]
- 80.Padegimas EM, Lawrence C, Narzikul AC, Zmistowski BM, Abboud JA, Williams GR, et al. Future surgery after revision shoulder arthroplasty: the impact of unexpected positive cultures. J Shoulder Elbow Surg. 2017;26:975–81. doi: 10.1016/j.jse.2016.10.023. [DOI] [PubMed] [Google Scholar]
- 81.Pellegrini A, Legnani C, Macchi V, Meani E. Management of periprosthetic shoulder infections with the use of a permanent articulating antibiotic spacer. Arch Orthop Trauma Surg. 2018;138:605–9. doi: 10.1007/s00402-018-2870-8. [DOI] [PubMed] [Google Scholar]
- 82.Jawa A, Shi L, OʼBrien T, Wells J, Higgins L, Macy J, et al. Prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) use for the treatment of infection after shoulder arthroplasty: J Bone Jt Surg-Am Vol. 2011;93:2001–9. [DOI] [PubMed]
- 83.McFarland EG, Rojas J, Smalley J, Borade AU, Joseph J. Complications of antibiotic cement spacers used for shoulder infections. J Shoulder Elbow Surg. 2018;27:1996–2005. doi: 10.1016/j.jse.2018.03.031. [DOI] [PubMed] [Google Scholar]



