Abstract
In the setting of chronic instability following total hip arthroplasty, implantation of a constrained acetabular liner may be warranted. We report on a patient who sustained a posterior prosthetic hip dislocation out of the constrained acetabular liner component (Stryker Trident [Kalamazoo, MI]), which had been previously replaced 2 months prior, and underwent a successful closed reduction in the emergency department. At 2-year follow-up, the patient’s prosthetic hip has remained stable with no reported issues. To our knowledge, this is the first reported closed reduction of a revised constrained total hip arthroplasty with this implant system, size, and length of follow-up.
Keywords: Closed reduction, Constrained liner, Case report, Revision, Total hip arthroplasty
Introduction
Constrained acetabular liners (CALs) function to promote hip stability by way of a locking mechanism that keeps the femoral head within the acetabular element [1]. Common indications for conversion to a constrained total hip arthroplasty (THA) include recurrent instability, abductor muscle deficiency, and neurologic abnormalities [2]. However, CAL failure over time can occur in the form of acetabular loosening, dislocation, infection, and periprosthetic fracture all of which often warrant surgical intervention [3,4]. Dislocation of a THA with CAL revision has been previously reported by numerous studies in the past, with rates ranging from 10% to 39% [[5], [6], [7]].
Several studies have described successful closed reductions in patients having a constrained THA. These studies include various implants and implant sizes [[8], [9], [10], [11], [12], [13], [14], [15]] along with novel techniques in this situation developed by the authors [13,15]. Although previous studies have described closed reductions of THAs with CALs, most patients have either had short-term follow-up or were lost to follow-up. In addition, none had a previous history of revision of the constrained construct. The purpose of this study is to describe the closed reduction of a tripolar constrained THA without need for revision surgery at 2-year follow-up.
Written informed consent was obtained from the patient’s mother, who is his primary caregiver, power of attorney, and authorized for the publication of this study and accompanying images.
Case history
In 2017, a 45-year-old male with past medical history notable for hepatitis C, drug-induced Parkinsonism, and normal pressure hydrocephalus with cognitive deficits underwent a right primary THA after exhausting nonoperative management of his right hip avascular necrosis. No immediate postoperative complications were noted.
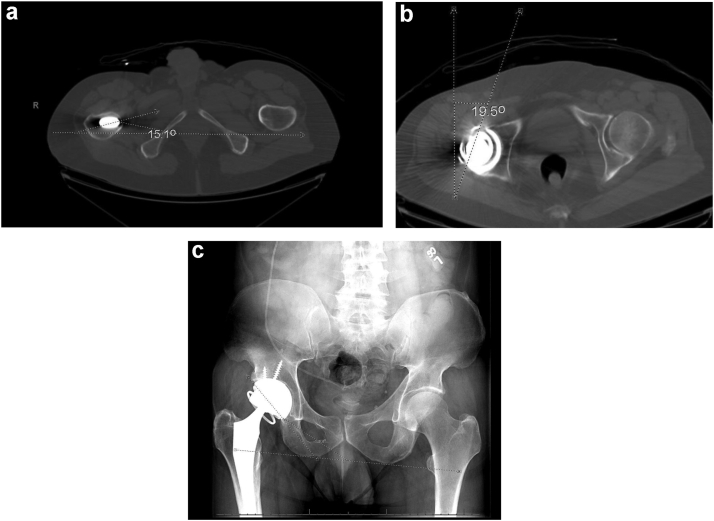
In the second week postoperatively, the patient got up from a low-lying chair and sustained a posterior dislocation of his right THA, which was subsequently closed and reduced in the emergency department (ED) under conscious sedation. Over the next 2 months, the patient sustained 3 more prosthetic hip dislocations, all closed and reduced under conscious sedation in the ED. Considering the patient’s recurrent dislocations, worsening Parkinson’s-related tremors, and cognitive deficits limiting his ability to follow precautions, revision surgery to a constrained THA design was planned based on normal inflammatory markers and an acceptable position of the acetabular and femoral components. A cell count was not performed at the time of revision, but multiple tissue cultures were obtained intraoperatively, which included aerobe and anaerobe cultures that were finalized after 5 days with no growth of bacteria. The implant selected was the Trident (Stryker, Kalamazoo, MI) system. Implant sizing included a 28 mm femoral head with a +4 mm neck length and a 0-degree size F Trident CAL for a size 58 cup. Femoral anteversion was measured to be 15.1 degrees, and the acetabular component was measured to be 19.5 degrees, for a combined version of 34.6 degrees (Fig. 1a and b). Inclination was measured at 45 degrees (Fig. 1c). No immediate postoperative complications were noted.
Figure 1.
(a) Axial computed tomography (CT) scan showing 15.1° of femoral anteversion. (b) Axial CT scan showing 19.5° of acetabular anteversion. (c) Anteroposterior (AP) radiograph showing a CAL with 45° of inclination.
In 2020, the patient was attempting to stand up from a low-seated toilet and fell, dislocating his right THA. Closed reduction in the ED was attempted but was not successful. The patient was taken to the operating room for open reduction and revision of the CAL. Preoperative inflammatory labs were obtained and were not indicative of a prosthetic joint infection. Intraoperatively, minor impressions were noted on the posterior part of the neck. The femoral neck was noted to be solid and intact. Despite these findings, there was no component-to-component impingement observed on intraoperative exam, which included flexion to 90 degrees, adduction to 20 degrees, extension to 10 degrees, 25 degrees of internal rotation, and 60 degrees of external rotation. Otherwise, the implants were intact and had maintained an appropriate and acceptable position and version. Therefore, the patient had the previous implants removed and replaced with the same-sized implants as before (Stryker 28 mm femoral head with neck length of +4 mm, size F Trident 0-degree CAL). Intraoperative cultures were negative. No acute complications were noted postoperatively.
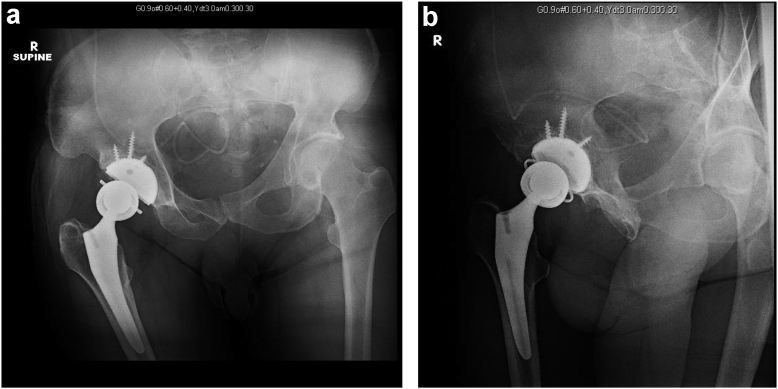
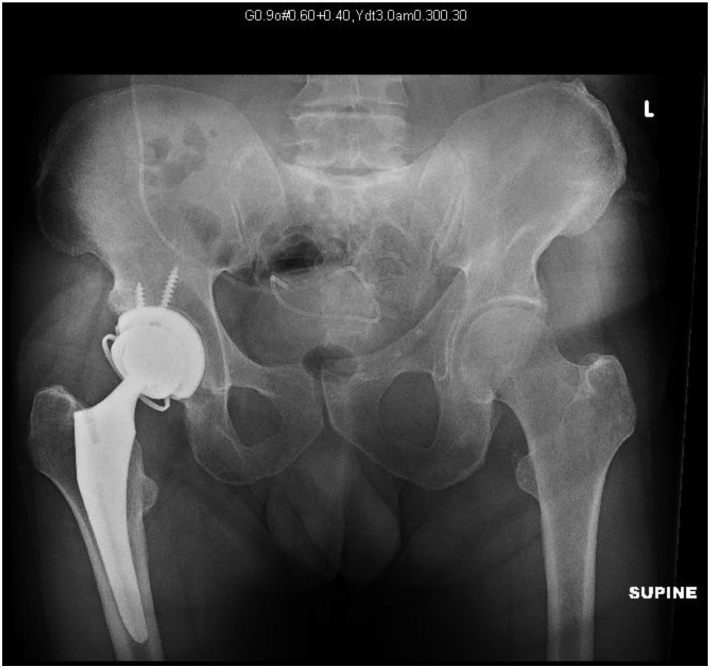
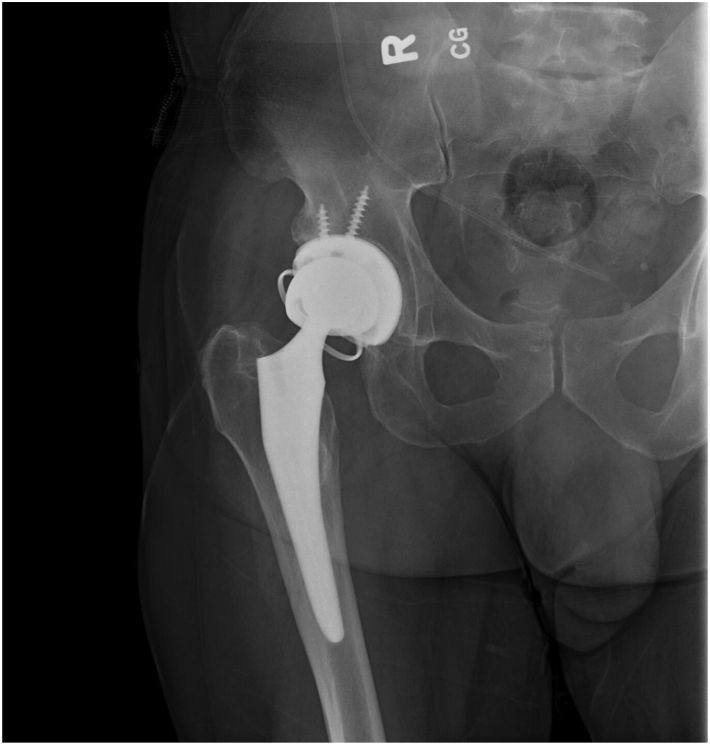
Two months later, the patient presented to the ED again following an attempt to stand up from a low-seated toilet. The patient reported feeling a “pop” in his right hip, followed by an inability to bear weight. On exam, the patient’s right leg was shortened and internally rotated but neurovascularly intact. Plain-film anteroposterior radiograph showed a right total hip dislocation with a constrained liner (Fig. 2). The patient then underwent conscious sedation with propofol performed by ED providers and closed reduction performed by orthopaedic team. A reduction of the hip was attempted by applying traction with the hip adducted and internally rotated. The physician attempting the reduction believed the hip was reduced, but formal postreduction x-rays demonstrated the femoral head perched up against the locking ring and was not entirely reduced (Fig. 3a and b). While the patient was still under conscious sedation, axial compression was applied to the greater trochanter with the hip in approximately neutral rotation and 45 degrees of flexion. Compression was applied approximately in the vector of the femoral neck. Successful closed reduction was achieved and confirmed by x-ray, with no obvious implant breakage (Fig. 4). Hip stability was tested after reduction and was noted to be stable to 90 degrees of flexion, 15 degrees of adduction, and 15 degrees of internal rotation. The patient was subsequently placed in a knee immobilizer. Posterior hip flexion precautions were explained to the patient and his mother. The patient was then discharged home with no ensuing complications. At 1-month follow-up, standing x-rays were taken of the right hip, which showed a properly aligned THA with constrained mechanism (Fig. 5).
Figure 2.
Supine AP radiograph showing a dislocated THA with a constrained liner.
Figure 3.
(a) Supine AP radiograph showing the femoral component perched against the locking ring after initial closed reduction attempt. (b) Lateral radiograph showing a perched femoral component against the locking ring after initial closed reduction attempt.
Figure 4.
Supine AP radiograph showing a successful closed reduction of the THA back into the CAL component with no obvious implant breakage.
Figure 5.
Standing AP radiograph at 1-month follow-up showing an intact THA with CAL.
At 2-year follow-up, there has not been another subsequent dislocation event (Fig. 6). He reports no right hip pain or instability type symptoms but does continue to walk with the aid of assistive devices due to worsening tremors secondary to his Parkinsonism.
Figure 6.
AP radiograph showing an intact THA with a CAL at 2-year follow-up.
Discussion
Dislocation of a constrained THA is the most common complication for patients following the procedure and often requires operative intervention [16]. In order for the femoral head to dislocate in constrained THA designs in the absence of mechanical failure, the crosslinked liner must deform [9,13,15]. Since the plastic liner was able to temporarily distort to allow the femoral head to dislocate, the liner may be able to distort again to allow the femoral head to reenter the acetabular component during a closed reduction attempt [8,14]. This mechanism may permit closed reduction of the dislocation if the CAL implant has not failed, which can occur in one of four locations: the liner-shell interface (Type I failure), the shell-bone interface (Type II failure), the locking ring (Type III failure), or the bipolar-femoral head interface (Type IV failure) [8,[17], [18], [19]]. On x-ray, the only convenient indication that implant failure has not occurred lies with the locking ring [14]. If the locking ring appears to be in the proper position and does not appear fractured, closed reduction of the dislocation may be attempted. However, if there is a belief that failure has occurred at the liner-shell interface or shell-bone interface, closed reduction would not be recommended. Intraprosthetic head dissociation has been described as a complication in dual mobility implants rather than CAL implants, such as the one described in this case [20].
A closed reduction of a THA with a CAL may be attempted under adequate sedation with propofol when there is no evidence of hardware failure on radiographs and the patient has dislocated for the first time since placement of the CAL construct. This may be trialed in the emergency room if adequate sedation and radiograph technicians for flat plate imaging postreduction are available. Otherwise, an attempt at closed reduction in the operating room under anesthesia and with fluoroscopy is also reasonable before attempting open reduction. The authors believe that contraindications to a closed reduction attempt include but are not limited to the presence of a periprosthetic fracture, severely osteoporotic bone, concern for prosthetic joint infection, concern for implant malposition, and recurrent dislocations. These pathologies are likely better treated with revision surgery.
All patients referenced in the available studies in which closed reduction was successful experienced their dislocations with their original CAL implants in place [[8], [9], [10], [11], [12], [13], [14], [15]]. Robertson et al reported on a patient that experienced a dislocation 2 months following a revised CAL implant system but required open reduction and conversion to a bipolar femoral prosthesis [11]. Harman et al’s in vitro study investigated the torque required to dislocate and relocate the femoral head in a constrained THA, which showed a significantly lower amount of torque was required to dislocate the femoral head between initial dislocation and second and third dislocations. Additionally, Harman et al found that the second relocation of the femoral head back into the constrained THA liner required significantly less torque than the initial relocation [13]. These findings suggest that dislocation and reduction of the constrained THA may damage the polyethylene liner, possibly increasing the risk of another dislocation event or causing chronic hip instability. Despite these findings, our patient did not sustain another dislocation event within 2 years of his closed reduction.
Summary
Closed reduction of a dislocated THA with a CAL has been reported in the literature as a viable alternative to surgically invasive treatment when no discernible implant breakage has occurred on prereduction imaging. We report on a case in which closed reduction of the patient’s dislocated THA with a CAL was achieved, even after previous revision of the constrained components. The patient’s combination of femoral head size, implant system, history of revision to the CAL, and time to follow-up add a new dimension to the literature on the utility of closed reduction in this patient population.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2023.101159.
Informed patient consent
The author(s) confirm that written informed consent has been obtained from the involved patient(s) or if appropriate from the parent, guardian, power of attorney of the involved patient(s); and, they have given approval for this information to be published in this case report (series).
Appendix A. Supplementary data
References
- 1.Shrader M.W., Parvizi J., Lewallen D.G. The use of a constrained acetabular component to treat instability after total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2179–2183. doi: 10.2106/00004623-200311000-00019. [DOI] [PubMed] [Google Scholar]
- 2.Lombardi A.V., Jr., Mallory T.H., Kraus T.J., Vaughn B.K. Preliminary report on the S-ROM constraining acetabular insert: a retrospective clinical experience. Orthopedics. 1991;14:297–303. [PubMed] [Google Scholar]
- 3.Khan R.J., Fick D., Alakeson R., Haebich S., de Cruz M., Nivbrant B., et al. A constrained acetabular component for recurrent dislocation. J Bone Joint Surg Br. 2006;88:870–876. doi: 10.1302/0301-620X.88B7.17644. [DOI] [PubMed] [Google Scholar]
- 4.Berend K.R., Lombardi A.V., Jr., Mallory T.H., Adams J.B., Russell J.H., Groseth K.L. The long-term outcome of 755 consecutive constrained acetabular components in total hip arthroplasty examining the successes and failures. J Arthroplasty. 2005;20(7 Suppl 3):93–102. doi: 10.1016/j.arth.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Williams J.T., Jr., Ragland P.S., Clarke S. Constrained components for the unstable hip following total hip arthroplasty: a literature review. Int Orthop. 2007;31:273–277. doi: 10.1007/s00264-006-0191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wetters N.G., Murray T.G., Moric M., Sporer S.M., Paprosky W.G., Della Valle C.J. Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. 2013;471:410–416. doi: 10.1007/s11999-012-2561-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daly P.J., Morrey B.F. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334–1343. [PubMed] [Google Scholar]
- 8.Sonohata M., Waewsawangwong W., Goodman S.B. Successful closed reduction of a dislocated constrained total hip arthroplasty: a case report and literature review. Open Orthop J. 2012;6:211–214. doi: 10.2174/1874325001206010211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flint J.H., Phisitkul P., Callaghan J.J. Closed reduction of a dislocated constrained total hip arthroplasty using a novel technique with a PEG board. Orthopedics. 2010;33:201. doi: 10.3928/01477447-20100129-28. [DOI] [PubMed] [Google Scholar]
- 10.Gaines R.J., Hardenbrook M. Closed reduction of a dislocated total hip arthroplasty with a constrained acetabular component. Am J Orthop (Belle Mead NJ) 2009;38:523–525. [PubMed] [Google Scholar]
- 11.Robertson W.J., Mattern C.J., Hur J., Su E.P., Pellicci P.M. Failure mechanisms and closed reduction of a constrained tripolar acetabular liner. J Arthroplasty. 2009;24:322.e5–322.e11. doi: 10.1016/j.arth.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Birdwell S., Wilke E. Closed reduction of constrained total hip arthroplasty in the ED. J Emerg Med. 2011;40:162–166. doi: 10.1016/j.jemermed.2007.10.069. [DOI] [PubMed] [Google Scholar]
- 13.Harman M.K., Hodge W.A., Banks S.A. Closed reduction of constrained total hip arthroplasty. Clin Orthop Relat Res. 2003;414:121–128. doi: 10.1097/01.blo.0000073342.50837.4a. [DOI] [PubMed] [Google Scholar]
- 14.Miller C.W., Zura R.D. Closed reduction of a dislocation of a constrained acetabular component. J Arthroplasty. 2001;16:504–505. doi: 10.1054/arth.2001.21504. [DOI] [PubMed] [Google Scholar]
- 15.McPherson E.J., Costigan W.M., Gerhardt M.B., Norris L.R. Closed reduction of dislocated total hip with S-ROM constrained acetabular component. J Arthroplasty. 1999;14:882–885. doi: 10.1016/s0883-5403(99)90043-8. [DOI] [PubMed] [Google Scholar]
- 16.Song J.H., Kwon W.H., Oh S.B., Moon K.H. Use of a constrained acetabular liner to prevent and treat recurrent dislocation after total hip replacement arthroplasty. Orthop Surg. 2020;12:2004–2012. doi: 10.1111/os.12811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones C.W., Malahias M.A., Baral E., Wright T., Sculco T.P., Sculco P.K. Catastrophic failure of tripolar constrained liners due to backside wear: a novel failure mode. Arthroplast Today. 2018;4:270–274. doi: 10.1016/j.artd.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooke C.C., Hozack W., Lavernia C., Sharkey P., Shastri S., Rothman R.H. Early failure mechanisms of constrained tripolar acetabular sockets used in revision total hip arthroplasty. J Arthroplasty. 2003;18:827–833. doi: 10.1016/s0883-5403(03)00325-5. [DOI] [PubMed] [Google Scholar]
- 19.Guyen O., Lewallen D.G., Cabanela M.E. Modes of failure of osteonics constrained tripolar implants: a retrospective analysis of forty-three failed implants. J Bone Joint Surg Am. 2008;90:1553–1560. doi: 10.2106/JBJS.G.00317. [DOI] [PubMed] [Google Scholar]
- 20.De Martino I., D'Apolito R., Waddell B.S., McLawhorn A.S., Sculco P.K., Sculco T.P. Early intraprosthetic dislocation in dual-mobility implants: a systematic review. Arthroplast Today. 2017;3:197–202. doi: 10.1016/j.artd.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.