Abstract
Lactate is an important metabolic substrate for sustaining brain energy requirements when glucose supplies are limited. Recurring exposure to hypoglycemia (RH) raises lactate levels in the ventromedial hypothalamus (VMH), which contributes to counterregulatory failure. However, the source of this lactate remains unclear. The current study investigates whether astrocytic glycogen serves as the major source of lactate in the VMH of RH rats. By decreasing the expression of a key lactate transporter in VMH astrocytes of RH rats, we reduced extracellular lactate concentrations, suggesting excess lactate was locally produced from astrocytes. To determine whether astrocytic glycogen serves as the major source of lactate, we chronically delivered either artificial extracellular fluid or 1,4-dideoxy-1,4-imino-d-arabinitol to inhibit glycogen turnover in the VMH of RH animals. Inhibiting glycogen turnover in RH animals prevented the rise in VMH lactate and the development of counterregulatory failure. Lastly, we noted that RH led to an increase in glycogen shunt activity in response to hypoglycemia and elevated glycogen phosphorylase activity in the hours following a bout of hypoglycemia. Our data suggest that dysregulation of astrocytic glycogen metabolism following RH may be responsible, at least in part, for the rise in VMH lactate levels.
Article Highlights
Astrocytic glycogen serves as the major source of elevated lactate levels in the ventromedial hypothalamus (VMH) of animals exposed to recurring episodes of hypoglycemia.
Antecedent hypoglycemia alters VMH glycogen turnover.
Antecedent exposure to hypoglycemia enhances glycogen shunt activity in the VMH during subsequent bouts of hypoglycemia.
In the immediate hours following a bout of hypoglycemia, sustained elevations in glycogen phosphorylase activity in the VMH of recurrently hypoglycemic animals contribute to sustained elevations in local lactate levels.
Introduction
Hypoglycemia remains a serious complication for patients with type 1 and, increasingly, those with type 2 diabetes on insulin therapy (1,2). Recurring exposure to hypoglycemia (RH) impairs the sympathoadrenal response to subsequent bouts of hypoglycemia, which, in turn, leads to hypoglycemia unawareness—a condition referred to as hypoglycemia-associated autonomic failure. Asymptomatic awareness of hypoglycemia increases the risk for severe hypoglycemic events. Although the mechanisms leading to hypoglycemia unawareness remain unclear, it has been suggested that increased utilization of alternate fuel substrates by the brain prevents glucose responsive neurons from sensing falling glucose levels (3). Lactate is an important metabolic substrate and signaling molecule in the brain, especially when glucose is low. Previous studies showed that increased extracellular lactate concentrations in the ventromedial hypothalamus (VMH), a major glucose sensing region of the brain, following RH may contribute to the development of hypoglycemia-associated autonomic failure (3).
Brain lactate is primarily derived either from the periphery or locally from the metabolism of glucose or glycogen. In the brain, glycogen is mainly stored in astrocytes and is thought to serve a protective role ensuring a supply of fuel to neurons when glucose availability is limited. Glycogen stores can be mobilized to produce lactate during hypoglycemia and replenished when glucose levels recover to normal. While astrocytes are believed to be the major cells in the brain that produce lactate, it remains unclear whether astrocytic glycogen is the source of elevated lactate levels in the VMH following RH. Therefore, the current study investigates whether astrocytic glycogen serves as the major source of lactate in the VMH of RH rats and how glycogen metabolism is affected by RH.
Research Design and Methods
Animals and Ethics Statement
Male Sprague-Dawley rats (Charles River Laboratories) weighing ∼275 g were housed in temperature- (22–23°C) and humidity-controlled rooms with access to chow and water. They were acclimated to a 12-h light cycle (lights on: 0700 h) for 1 week before experimental manipulation. All studies were approved by the Institutional Animal Care and Use Committee at the University of Utah.
Study 1: Identifying the Major Source of VMH Lactate in RH Rats
To establish whether elevated VMH lactate levels in RH animals are derived locally from astrocytes or taken up from the periphery, rats were inoculated with an adeno-associated viral vector to express a siRNA against monocarboxylic acid transporter 1 (MCT1) under the control of a glial fibrillary acidic protein (GFAP) promoter for 3 weeks and sacrificed. The control vector expressed a scrambled RNA sequence under the control of a GFAP promoter. Specificity of the AAV was validated using immunohistochemistry and the antibodies listed in Table 1. A subset of animals was microinjected with either the scrambled or MCT1 siRNA adeno-associated viral (AAV) (GeneDetect Ltd, Auckland, New Zealand) and implanted with microdialysis-microinjection guide cannulas that targeted the VMH. Two weeks later, vascular catheters were implanted, and, 3 days after the surgery, the animals underwent the RH treatment regimen (Supplementary Materials and Methods) before undergoing a microdialysis procedure to quantify basal VMH lactate concentrations the day after the final bout of treatment.
Table 1.
Antibodies used in the current study
| Antibody | Vendor | Catalogue no. | Use | Dilution |
|---|---|---|---|---|
| GFAP | Invitrogen | A6455 | IF | 1:500 |
| GFP | Millipore | MAB2510 | IF | 1:500 |
| Donkey Anti-Rabbit | Invitrogen | A21206 | IF | 1:300 |
| Goat Anti-Mouse | Invitrogen | A11003 | IF | 1:500 |
| GP | Abcam | 154969 | IB | 1:1,000 |
| GS | Cell Signal | 3893S | IB | 1:1,000 |
| β-actin | Sigma | A5316 | IB | 1:5,000 |
| Anti-rabbit | Perkin-Elmer | NEF812001EA | IB | 1:5,000 |
| Anti-mouse | Sigma | A9044 | IB | 1:10,000 |
IF, immunofluorescence; IB, immunoblots.
Study 2: To Establish Whether Glycogen Serves as the Major Source of Lactate in the VMH of RH Rats
To determine whether astrocytic glycogen is the major source of lactate in the VMH, we used mini-osmotic pumps to deliver 1,4-dideoxy-1,4-imino-d-arabinitol (DAB) (300 μmol/L) into the VMH of a subgroup of RH animals to inhibit glycogen turnover (Supplementary Fig. 1) (4).
Surgery
Rats were implanted with vascular catheters, VMH intracranial infusion sets connected to osmotic pumps, and microdialysis-microinjection guide cannulas. Three days later, the animals underwent the RH treatment protocol before undergoing the hypoglycemic clamp procedure the next day. We evaluated the following groups: recurrent saline + aECF (Control-Hypoglycemia [C-H]), RH+aECF (RH), and RH+DAB. To control for the effects of insulin on glycogen deposition (5), we conducted hyperinsulinemic- (50 mU/kg/min) euglycemic clamps in a subgroup of control animals where blood glucose was maintained between 100 and 120 mg/dL (Control-Euglycemia [C-E]). These animals were compared with a saline-infused group (Control-Saline [C-S]). Following the clamp, the animals were euthanized, and the brains were removed and frozen in liquid nitrogen in <30 s. VMH micropunches were collected to assess glycogen content.
Hormone and Microdialysate Lactate Analysis
Plasma glucagon, catecholamine, and microdialysate lactate concentrations were analyzed using commercial kits (Supplementary Table 1).
Tissue Glycogen
Glycogen content was quantified in frozen VMH micropunches using a commercial glycogen assay kit and normalized to the tissue weight of each sample.
Study 3: VMH Glycogen Turnover Following Recovery From Hypoglycemia
Control and RH rats were sacrificed 24 h after the final day of treatment, and immunoblots were used to quantify glycogen synthase (GS) and phosphorylase (GP) enzyme expression in VMH micropunches (Supplementary Fig. 2). The BIORAD ChemiDoc Imaging System was used to capture the images, and ImageLab software was used for densitometric analysis.
GS and GP enzyme activity were evaluated to assess glycogen turnover in VMH micropunches collected immediately after the final acute bout of hypoglycemia (AH) or after the third episode of hypoglycemia in RH rats (0 h) or 6 and 24 h later when glucose levels were normalized, as described previously (Supplementary Fig. 3) (6,7). Additionally, we sacrificed a group of rats 3 h after an intraperitoneal saline injection to determine basal GS and GP activity in the absence of hypoglycemia.
Statistical Analysis
Data are expressed as mean ± SEM and analyzed using GraphPad Prism 9.5. Group comparisons were performed using one- or two-way ANOVA for independent or repeated measures as appropriate. Comparisons of two groups were performed using Student’s t test for unpaired data. Statistical significance was assumed at P < 0.05.
Data and Resource Availability
The data sets generated during and/or analyzed in the current study are not publicly available but are available from the corresponding author on reasonable request.
Results
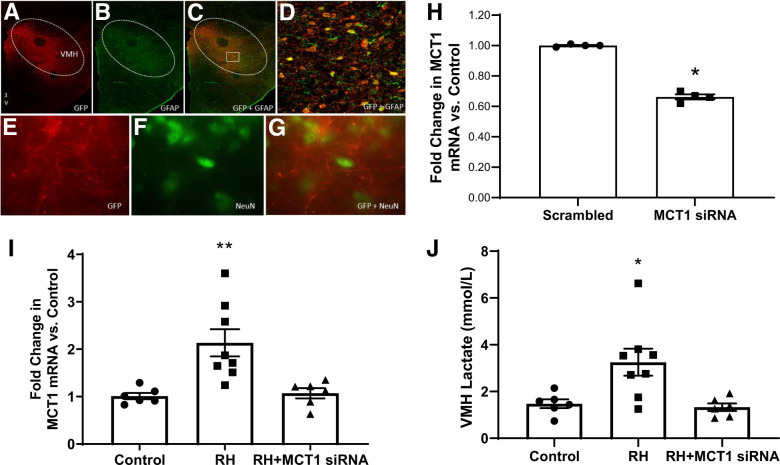
MCT1 Knockdown Prevented the Increase of VMH Lactate Production in RH Rats
The AAV vector specifically targeted astrocytes and not neurons, as demonstrated by colocalization of the green fluorescent protein (GFP) reporter with GFAP, and not NeuN (Fig. 1A–G). MCT1 expression in the VMH was decreased by ∼35% compared with controls receiving the scrambled RNA (P < 0.05) (Fig. 1H). Reducing astrocytic MCT1 mRNA expression in RH animals decreased extracellular lactate levels in the VMH (Fig. 1I and J).
Figure 1.
(A–G) Immunohistochemical staining demonstrating cellular specificity of the AAV vector for targeting astrocytes in VMH sections. A and E show labeling of the AAV’s GFP reporter gene in red. B and F show the labeling of GFAP, an astrocyte marker or NeuN, a neuronal marker, in green. C and G are the merged images showing colocalization of the GFP signal with GFAP on top and distinct labeling of the GFP reporter and neurons (NeuN) on the bottom, indicating the AAV vector specifically targets expression to astrocytes and not neurons. D is a magnified image of the area outlined in C that more clearly shows the colocalization. (H) Quantitative RT-PCR analysis showing the MCT1 siRNA-expressing AAV (MCT1 siRNA; n = 4) decreased the expression of MCT1 mRNA in the VMH by ∼35% (*P < 0.05) compared with controls receiving the AAV expressing the scrambled RNA (Scrambled; n = 4). (I) Quantitative RT-PCR showing an increase in MCT1 mRNA expression in RH rats (squares; N = 8) compared with controls (circles; N = 6) and normalization of MCT1 mRNA levels in the VMH of RH animals using the astrocyte targeting AAV (RH+MCT1 siRNA; triangles; N = 6). (J) Extracellular lactate concentrations in the VMH were elevated in RH animals (squares), and these levels were restored to normal following knockdown of MCT1 (RH + MCT1 siRNA; triangles). RH increased extracellular lactate concentrations (squares) compared with hypoglycemia-naïve control animals (circles). Reducing astrocytic MCT1 expression in the VMH of recurrently hypoglycemic rats (triangles) decreased extracellular lactate levels to normal. Data are presented as mean ± SEM. *P < 0.05, **P < 0.01 vs. Scrambled/Control and RH+MCT1 siRNA; 3V, 3rd ventricle.
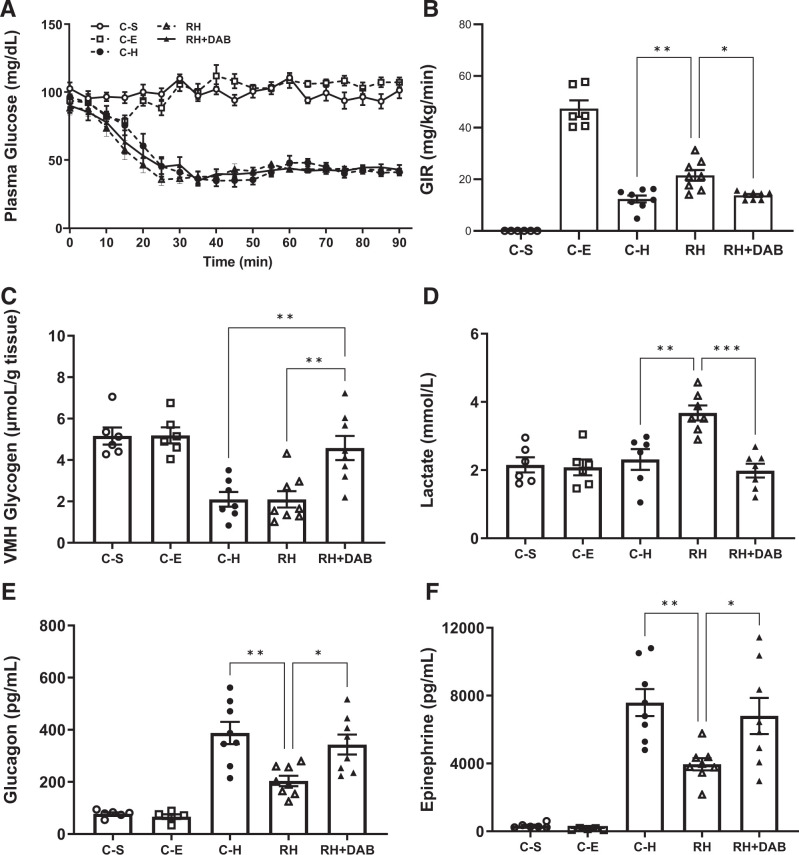
DAB Treatment Reduced Exogenous Glucose Requirements and Prevented Impairment of the Hormone Responses in RH Rats
Despite matched plasma glucose levels (Fig. 2A), exogenous glucose infusion rates were significantly higher in the RH group compared with controls (Fig. 2B). Treatment with DAB significantly reduced glucose requirements in RH rats back to normal. As expected, glucose infusion rates in the C-E group during the euglycemic clamps were higher than in the groups undergoing the hypoglycemic clamp.
Figure 2.
(A) Plasma glucose concentrations of all treatment groups during the glucose clamp procedure. Plasma glucose concentrations were well matched between animals either receiving a saline infusion or undergoing the hyperinsulinemic-euglycemic clamp. Plasma glucose concentrations were matched for groups undergoing the hypoglycemic clamp as well. (B) Average glucose infusion rates (GIR) during the last 20 min of the clamp procedure for all treatment groups. (C) VMH glycogen levels following the clamping procedure. (D) Basal extracellular lactate concentrations in the VMH. (E) Peak plasma glucagon concentrations during the clamping procedure. (F) Peak plasma epinephrine concentrations during the clamping procedure. C-S: N = 6; C-E: N = 6; C-H: N = 8; RH: N = 8; RH+DAB: N = 8. Data are presented as mean ± SEM. *P < 0.05, **P < 0.01, and ***P < 0.001.
Since VMH glycogen content was evaluated at the end of the clamp, we were unable to determine baseline glycogen levels for each individual animal. Instead, we compared VMH glycogen levels from all the treatment groups with glycogen levels measured in a group of rats that received a saline infusion under similar sampling conditions (C-S) whose average glycogen content was 5.2 ± 0.4 μmol/g tissue (Fig. 2C). This is similar to values previously reported in the rat brain using 13C nuclear magnetic resonance spectroscopy and high-power microwave fixation (8,9), indicating the surgical and blood sampling procedures did not significantly affect brain glycogen content and, more importantly, that the rapid removal and freezing of the brain in liquid nitrogen prevented postmortem breakdown of VMH glycogen content. Insulin-induced hypoglycemia significantly reduced VMH glycogen content, by 55% in the C-H group and by 57% in the RH group, but not in RH+DAB rats, indicating 300 μmol/L DAB effectively prevented depletion of glycogen stores in RH animals.
While RH dramatically increased basal VMH extracellular lactate levels (Fig. 2D), inhibiting VMH glycogen turnover prevented the rise in VMH lactate levels, suggesting lactate is predominantly derived from glycogen in RH rats.
As expected, compared with controls, RH attenuated glucagon and epinephrine responses by 47–48% during the hypoglycemic clamp. Inhibiting VMH glycogen turnover restored these responses to normal (Fig. 2E and F).
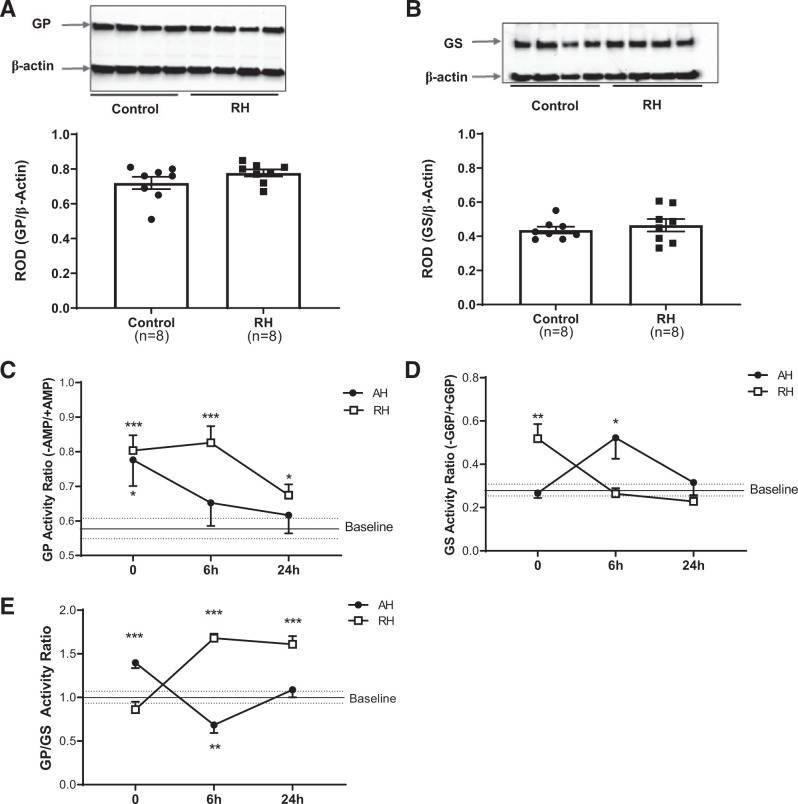
RH Did Not Affect VMH GP and GS Protein Expression, but It Did Affect Glycogen Turnover
Although no significant differences in GP or GS expression were observed between control and RH rats (Fig. 3A and B), there were notable differences in enzyme activity. GP activity increased in AH animals in response to hypoglycemia (Fig. 3C) but returned to baseline within 6 h. In contrast, GP activity in RH animals increased in response to hypoglycemia and remained significantly elevated for 24 h. VMH GS activity in AH animals remained at baseline levels during hypoglycemia (Fig. 3D), increased by 6 h after the bout of hypoglycemia, when blood glucose concentrations were normal, and returned to baseline levels by 24 h. In contrast, RH led to significant increases in GS activity during hypoglycemia, which quickly returned to baseline levels within 6 h.
Figure 3.
Immunoblot analysis of (A) GP and (B) GS protein levels in the VMH of hypoglycemia-naïve controls (Control; N = 8) and RH (N = 8) animals. (Top) Representative immunoblot images of GP, GS and B-actin bands. (Bottom) Densitometric analysis of the immunoblots standardized to the B-actin loading controls. (C) GP and (D) GS activity in the VMH of rats exposed to a single acute bout of hypoglycemia (AH; N = 8 per time point) or after the final bout of RH (N = 8 per time point). Baseline GP and GS activity levels in the VMH were determined in a group of hypoglycemia-naïve animals (N = 8) and are demarcated by the solid line, with SEM indicated by the dotted lines. The time points indicate the amount of time proceeding the last episode of hypoglycemia. (E) The ratio of GP to GS activity standardized to that of the baseline hypoglycemia-naïve animals. Data are presented as mean ± SEM. *P < 0.05, **P < 0.01, and ***P < 0.001 vs. baseline.
The GP/GS activity ratio shows a normal transition from glycogenolysis, at the end of an AH, toward glycogen synthesis before normalization of glycogen turnover by 24 h. Interestingly, the GP/GS ratio at the end of hypoglycemia remained at baseline levels in RH, despite significant elevations in both GP and GS activity, suggesting there is an increase in glycogen shunt activity in RH animals in response to hypoglycemia and greater glycogenolytic capacity in the hours proceeding a bout of hypoglycemia.
Discussion
Astrocytic glycogen is an important energy reserve supplying neurons with lactate when brain glucose supplies are limited (10,11). As expected, RH led to significant increases in VMH lactate levels compared with controls, and this rise was associated with a blunted counterregulatory hormone response (3). The current study showed lactate is locally produced from glycogen stores in astrocytes, as the knockdown of astrocytic MCT1 led to significant reductions in VMH lactate in RH animals.
In the brain, glycogen is stored almost exclusively in astrocytes and is preferentially converted into lactate because of low glucose-6-phosphatase and pyruvate dehydrogenase activity, as well as the preferential conversion of pyruvate to lactate by lactate dehydrogenase 5 (12–15). To establish whether glycogen is the major source of lactate in RH, we inhibited glycogen turnover in the VMH with DAB, which successfully prevented the rise in lactate and the development of counterregulatory failure in RH rats, suggesting astrocytic glycogen is likely the major supplier of lactate to the VMH following RH. Though brain glycogen stores are finite, during hypoglycemia, limited glucose supply to the brain reduces both synaptic activity and glucose utilization (16), and, therefore, glycogen stores can potentially support brain energy metabolism for slightly longer periods. Alternatively, glycogen “supercompensation” during hypoglycemia recovery can result in excess glycogen stores, which can sustain brain metabolism during subsequent bouts of hypoglycemia, potentially masking the ability of glucose responsive neurons to detect hypoglycemia (9,17). To determine how RH affects the metabolism of this important fuel store, we examined metrics of glycogen turnover in the VMH.
While no significant differences in VMH GP or GS protein levels exist between RH and control rats, differences in enzyme activity were observed in response to hypoglycemia and during the recovery phase. Hypoglycemia-naïve rats showed an increase in GP activity during hypoglycemia that reduced VMH glycogen content. In the hours following hypoglycemia, as glucose levels recovered, GS activity predominated to restore glycogen levels back to normal.
In contrast, RH animals exhibited vastly different enzyme activity profiles compared with controls; both GP and GS activity in the VMH were increased during hypoglycemia, indicating some of the entering glucose is directed toward glycogen synthesis, concurrent with an increase in glycogen breakdown, indicating increased glycogen shunt activity in response to hypoglycemia (18), which is a novel observation. Interestingly, once glucose levels recovered to normal, GS activity returned to baseline more rapidly than in the hypoglycemia-naïve controls. However, GP activity remained elevated, suggesting greater breakdown of the glycogen pool in the hours after hypoglycemia. This is an intriguing observation given that VMH glycogen content at 6 h posthypoglycemia was similar between the control and RH groups (Supplementary Fig. 4), suggesting there may be an increase in glycogen deposition that occurs in the immediate hours following hypoglycemia (between 0 and 6 h), as glucose levels recover, that is brought down to normal within 6 h by higher GP activity. At 24 h, GP activity remained elevated, which could explain the sustained rise in lactate production in RH rats.
Regulation of the two glycogen metabolic enzymes in astrocytes is complex and multifactorial in nature, being influenced by insulin, norepinephrine, glutamate, and AMPK (19–22). Normally, during insulin-induced hypoglycemia, a rise in insulin enhances GS activity (19), whereas glutamate, a stimulatory neurotransmitter that is released in the VMH in response to hypoglycemia, enhances glucose uptake in primary cultured astrocytes (23). Additionally, activation of AMPK and release of norepinephrine in the VMH in response to hypoglycemia both enhance glycogen breakdown (21,24). Together, these stimuli coordinate a response that normally inhibits GS activity and enhances GP activity to increase breakdown of the astrocytic glycogen pool during hypoglycemia. As glucose levels recover, inactivation of stimulatory neurotransmitters and AMPK promotes glycogen storage until both GS and GP activity eventually return to baseline levels.
In contrast, RH adversely affects the regulation of both GS and GP activity in the VMH. RH decreases the expression of AMPK α1 and α2 subunits in the VMH (25); hence, astrocytic AMPK activity may be reduced or desensitized following RH. A decrease in astrocytic AMPK activation in response to hypoglycemia may augment GS activity. In contrast, noradrenergic activation, coupled with loss of glutamatergic neurotransmission and possibly oxidation in RH, may augment GP activity during hypoglycemia. Although this mechanism is still speculative, the interaction between these important regulators of astrocytic glycogen metabolism warrants further investigation.
In conclusion, our data demonstrate that glycogen serves as the major supplier of lactate in RH animals, as the inhibition of glycogen turnover in the VMH prevents the rise in extracellular lactate. The increase in GP activity both during and in the hours following a bout of hypoglycemia contribute to the enhanced breakdown and lactate production; however, the mechanisms that lead to this dysregulation remain unknown but are likely multifactorial in nature.
Article Information
Acknowledgments. The authors would like to thank Drs. Xiang Wang and Michael J. Bridge from the University of Utah’s Cell Imaging Core (Salt Lake City, UT) for their assistance with image acquisition on the Zeiss 700 confocal microscope.
Funding. This work was generously supported by research grants from the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK099315), the University of Utah's Undergraduate Research Opportunity Program, and the Native American Research Internship Program in Diabetes, Obesity and Metabolism (R25 DK109894).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. G.S., R.F., A.K.L., K.C.-N., and I.E.N. researched the data. G.S. wrote the manuscript. G.S. and O.C. contributed to protocol development and reviewed/edited the manuscript. All authors reviewed and approved the manuscript. O.C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.22928423.
References
- 1. Gehlaut RR, Dogbey GY, Schwartz FL, Marling CR, Shubrook JH. Hypoglycemia in type 2 diabetes - more common than you think: a continuous glucose monitoring study. J Diabetes Sci Technol 2015;9:999–1005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cryer PE. Severe iatrogenic hypoglycemia in type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab 2007;3:4–5 [DOI] [PubMed] [Google Scholar]
- 3. Chan O, Paranjape SA, Horblitt A, Zhu W, Sherwin RS. Lactate-induced release of GABA in the ventromedial hypothalamus contributes to counterregulatory failure in recurrent hypoglycemia and diabetes. Diabetes 2013;62:4239–4246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Walls AB, Sickmann HM, Brown A, et al. Characterization of 1,4-dideoxy-1,4-imino-d-arabinitol (DAB) as an inhibitor of brain glycogen shunt activity. J Neurochem 2008;105:1462–1470 [DOI] [PubMed] [Google Scholar]
- 5. Heni M, Hennige AM, Peter A, et al. Insulin promotes glycogen storage and cell proliferation in primary human astrocytes. PLoS One 2011;6:e21594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thomas JA, Schlender KK, Larner J. A rapid filter paper assay for UDPglucose-glycogen glucosyltransferase, including an improved biosynthesis of UDP-14C-glucose. Anal Biochem 1968;25:486–499 [DOI] [PubMed] [Google Scholar]
- 7. Gilboe DP, Larson KL, Nuttall FQ. Radioactive method for the assay of glycogen phosphorylases. Anal Biochem 1972;47:20–27 [DOI] [PubMed] [Google Scholar]
- 8. Herzog RI, Chan O, Yu S, Dziura J, McNay EC, Sherwin RS. Effect of acute and recurrent hypoglycemia on changes in brain glycogen concentration. Endocrinology 2008;149:1499–1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Choi IY, Seaquist ER, Gruetter R. Effect of hypoglycemia on brain glycogen metabolism in vivo. J Neurosci Res 2003;72:25–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dienel GA. Brain glucose metabolism: integration of energetics with function. Physiol Rev 2019;99:949–1045 [DOI] [PubMed] [Google Scholar]
- 11. Rich LR, Harris W, Brown AM. The role of brain glycogen in supporting physiological function. Front Neurosci 2019;13:1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dienel GA, Nelson T, Cruz NF, Jay T, Crane AM, Sokoloff L. Over-estimation of glucose-6-phosphatase activity in brain in vivo. Apparent difference in rates of [2-3H]glucose and [U-14C]glucose utilization is due to contamination of precursor pool with 14C-labeled products and incomplete recovery of 14C-labeled metabolites. J Biol Chem 1988;263:19697–19708 [PubMed] [Google Scholar]
- 13. Gotoh J, Itoh Y, Kuang TY, Cook M, Law MJ, Sokoloff L. Negligible glucose-6-phosphatase activity in cultured astroglia. J Neurochem 2000;74:1400–1408 [DOI] [PubMed] [Google Scholar]
- 14. Bittar PG, Charnay Y, Pellerin L, Bouras C, Magistretti PJ. Selective distribution of lactate dehydrogenase isoenzymes in neurons and astrocytes of human brain. J Cereb Blood Flow Metab 1996;16:1079–1089 [DOI] [PubMed] [Google Scholar]
- 15. Laughton JD, Charnay Y, Belloir B, Pellerin L, Magistretti PJ, Bouras C. Differential messenger RNA distribution of lactate dehydrogenase LDH-1 and LDH-5 isoforms in the rat brain. Neuroscience 2000;96:619–625 [DOI] [PubMed] [Google Scholar]
- 16. Suda S, Shinohara M, Miyaoka M, Lucignani G, Kennedy C, Sokoloff L. The lumped constant of the deoxyglucose method in hypoglycemia: effects of moderate hypoglycemia on local cerebral glucose utilization in the rat. J Cereb Blood Flow Metab 1990;10:499–509 [DOI] [PubMed] [Google Scholar]
- 17. Canada SE, Weaver SA, Sharpe SN, Pederson BA. Brain glycogen supercompensation in the mouse after recovery from insulin-induced hypoglycemia. J Neurosci Res 2011;89:585–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shulman RG, Hyder F, Rothman DL. Cerebral energetics and the glycogen shunt: neurochemical basis of functional imaging. Proc Natl Acad Sci USA 2001;98:6417–6422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hamai M, Minokoshi Y, Shimazu T. L-glutamate and insulin enhance glycogen synthesis in cultured astrocytes from the rat brain through different intracellular mechanisms. J Neurochem 1999;73:400–407 [DOI] [PubMed] [Google Scholar]
- 20. Voss CM, Pajęcka K, Stridh MH, Nissen JD, Schousboe A, Waagepetersen HS. AMPK activation affects glutamate metabolism in astrocytes. Neurochem Res 2015;40:2431–2442 [DOI] [PubMed] [Google Scholar]
- 21. Walls AB, Heimbürger CM, Bouman SD, Schousboe A, Waagepetersen HS. Robust glycogen shunt activity in astrocytes: effects of glutamatergic and adrenergic agents. Neuroscience 2009;158:284–292 [DOI] [PubMed] [Google Scholar]
- 22. Swanson RA, Yu AC, Chan PH, Sharp FR. Glutamate increases glycogen content and reduces glucose utilization in primary astrocyte culture. J Neurochem 1990;54:490–496 [DOI] [PubMed] [Google Scholar]
- 23. Chowdhury GMI, Wang P, Ciardi A, et al. Impaired glutamatergic neurotransmission in the ventromedial hypothalamus may contribute to defective counterregulation in recurrently hypoglycemic rats. Diabetes 2017;66:1979–1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Coggan JS, Keller D, Calì C, et al. Norepinephrine stimulates glycogenolysis in astrocytes to fuel neurons with lactate. PLOS Comput Biol 2018;14:e1006392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McCrimmon RJ, Fan X, Cheng H, et al. Activation of AMP-activated protein kinase within the ventromedial hypothalamus amplifies counterregulatory hormone responses in rats with defective counterregulation. Diabetes 2006;55:1755–1760 [DOI] [PubMed] [Google Scholar]