Abstract
There is a strong association between family meals and child and adolescent health. To systematically understand the associations between family meals with a variety of health and risk outcomes, we developed and conducted a validation study of child- and parent-versions of the Family Dinner Index (FDI; FDI-C/FDI-P). We validated the measures with a national sample of 2,090 parent–child dyads. Using factor analysis, we reduced the initial FDIs each to eight items representing communication, enjoyment, and digital distractions; the FDI-C also included meal logistics and the FDI-P, family bonding. Using multivariable log-binomial regression models, we examined the relationships between FDI scores and substance use, violence, weight perception, weight control intention, and health indicators. Children who scored ≥21 on the FDI-C had a significantly lower average prevalence of a ‘negative outcome’ composite, as well as a lower prevalence of each of the individual behaviors. Children of parents who scored ≥24 on the FDI-P had a significantly lower average prevalence of the ‘negative outcome’ composite, as well as a lower prevalence of substance use indicators, negative weight perception and intentions to lose weight, less than daily fruit and vegetable consumption, and not meeting guidelines for physical activity. The FDI measures provide support for face and content validity, as well as concurrent criterion validity and construct validity. Further validation with these measures using a longitudinal design will allow for the establishment of predictive validity. Currently, the FDI measures may help researchers and practitioners identify points of emphasis for tailoring family-based prevention programs accordingly.
Keywords: Family dinner, Measure, Psychometric, Child and adolescent health, Risk and protective factors and parental practices
1. Introduction
The positive relationship between family meals and adolescent health and wellbeing has been widely studied (Goldfarb et al., 2015, Harrison et al., 2015, Skeer and Ballard, 2013). In general, young people who frequently eat meals with their parents/guardians (termed ‘parents’ herein) are more likely to have healthier exercise (Pyper et al., 2016) and eating habits (Hammons and Fiese, 2011), including increased fruit and vegetable consumption (Christian et al., 2013, Pyper et al., 2016), and are less likely to engage in a variety of risk behaviors (Fulkerson et al., 2006, Goldfarb et al., 2015, Haghighatdoost et al., 2017, Harrison et al., 2015, Skeer and Ballard, 2013), such as substance use (Fulkerson et al., 2006), violence (Fulkerson et al., 2006, Yockey et al., 2021), and having a negative body weight perception (Marques et al., 2018). Because of these associations, family meals have been promoted as interventions for preventing issues such as higher weight (Harbec and Pagani, 2018) and substance use (Skeer et al., 2022), as well as enhancing academic and social adjustment among lower age groups (Harbec and Pagani, 2018). While it has been hypothesized that family meals may serve as protective factors through familial engagement, communication, and connection (Skeer and Ballard, 2013), details on the underlying mechanisms of these consistent associations remain less well understood.
In prior work (Skeer and Ballard, 2013, Skeer et al., 2018), we described the two primary challenges with the extant literature on family meals. First, the frequency-centric measurement of family meals fails to incorporate other important dimensions that could be protective—or harmful—for youth. Second, given the unidimensional nature, the methods of measuring meal frequency are quite heterogeneous with respect to time frame (i.e., ever, past year, past month, past week) and mealtime (i.e., inquiring about ‘meals’ in general compared to ‘dinner’ specifically). Such heterogeneity threatens the validity of the associations, intensifying the difficulty in comparing results across studies.
There is a need for a standardized multi-dimensional measure to systematically understand the associations between family meals and different health and risk outcomes (Middleton et al., 2020). Previous public health interventions such as Project EAT (Eating Among Teens) (University of Minnesota, n.d.) and the McMaster Mealtime Interaction Coding System (MICS) (Mitchell et al., 2009) have focused on measuring the nutritional outcomes from family meal promotion. We therefore sought to fill gaps in the literature by developing and establishing face and content validity, as well as criterion and construct validity (DeVellis and Thorpe, 2021) of child and parent versions of the Family Dinner Index (FDI; FDI-C and FDI-P, respectively). More specifically, criterion validity assesses a measure in comparison with a current standard used in the literature (in this case, frequency of family dinners) and construct validity assesses how the measure is associated with other constructs that it should be related to (or not associated with ones it should not relate to) (DeVellis and Thorpe, 2021), including the aforementioned health and risk-related outcomes.
The current research was carried out in three phases. For Phase I (already concluded (Skeer et al., 2018)) we conducted qualitative research through individual interviews and developed the FDI instruments. Briefly, we conducted one-on-one interviews with 37 children aged 6–16 years and with their parent separately on various aspects of family meals (Skeer et al., 2018). To ensure content validity (DeVellis and Thorpe, 2021), expert opinion was obtained on the likely items of child and parent versions of a family dinner index. Three investigators (MS, KS, SF) discussed relevant themes and proposed content of the indices and subsequently created lists of scale items for children and parents. We found three prevailing themes: parents and children generally enjoyed spending time with their families during meals; mealtime is conducive to both mundane and serious conversations; and technology use during mealtimes, when allowed, often hindered communication among those present. Additionally, almost all participants reported that dinner was the meal they ate together most frequently, which led us to focus the measure on dinner. The initial set of items for the FDI-C and FDI-P reflected these themes. The generation of scale items also addressed the issue of face validity, the property that a scale, at face value, measures the latent variable it is created to capture (DeVellis and Thorpe, 2021).
For Phase II, we conducted cognitive interviews on the quantitative items for the survey, pilot tested the questions with a sample of 142 parent–child dyads, and preliminarily assessed concurrent criterion validity and construct validity of the instruments (see Supplementary material). For Phase III, the focus of this manuscript, we performed a factor analysis in a large, nationally diverse sample that approximately matches the ethnic and racial distribution of the US. The purpose of the current paper is to present the results of Phase III, which aimed to assess concurrent criterion validity and construct validity of the FDIs.
2. Materials and methods
2.1. FDI development and cognitive interviews
The process of developing and validating the FDI scales consisted of Phase I (Skeer et al., 2018) (qualitative research and FDI development) and Phase II [cognitive interviews (Willis, 2004) and preliminary FDI validation]. For Phase II, first, between June and October 2015, we conducted cognitive interviews with children in the target age range (8–16) and parents to determine the wording of the questions, resulting in the set of questions in the FDI-C and FDI-P that we tested in the ensuing quantitative study. Second, between February 2016 and August 2017, we conducted a quantitative pilot study with the FDI-C and FDI-P to reduce the items to create the most parsimonious set of questions, develop a score for the measures, and assess preliminary concurrent criterion validity and construct validity of the final FDI measures (see Supplementary materials). Between October 2021 and February 2022, we carried out a large, national study to validate the instruments.
2.2. Quantitative surveys
2.2.1. Participants and procedures
To validate the instruments developed and pilot tested in Phase II (n = 142), we collected data from a national online sample of 2,090 parent–child dyads. Inclusion criteria were: able to speak, read, and understand English well enough to complete study procedures; parents were living with their children at least half-time, and children were aged 12–17. This age range aligns with the National Survey on Drug Use and Health (SAHMSA, 2020) and was chosen to provide sufficient variation in the risk and prevention continuum and allow us to determine the appropriate age for the subsequent administration of the FDI-C.
Recruitment took place through the Qualtrics software company, which has panels of potential adult participants across the United States who have been recruited through various strategies and have agreed to be contacted to participate in surveys for which they are eligible. Qualtrics sent a survey invitation to potentially eligible panelists. Respondents were screened and if eligible, were invited to complete the survey. Qualtrics has systems in place to ensure the quality of responses—that they come from real people, that one person does not take the survey multiple times, and that respondents are attentive to the survey questions.
Participating parents receive the survey link, which contained surveys for both them and the child in the study with them. They consent for themselves and for their children to participate in the study. Once the parent completes their part of the survey, they are prompted to have the child complete theirs, after the child provides assent. Parents and children are asked to take their surveys in private, separately, and not share their answers. Child responses are not shared with the parent, and vice versa. Each survey took approximately 15 minutes, was done online, and participants were compensated according to the Qualtrics protocols, which includes a point system that equaled monetary value. All study procedures were approved by the Principal Investigator’s Institutional Review Board and met guidelines for the protection of human subjects concerning safety and privacy accordingly.
2.3. Measures
Demographic variables included age, gender, ethnicity, race, and, for parents only, education, household income, and census region place of residence.
Family Dinner Frequency. The following question came from the qualitative study: ‘During a typical week during the school year, how many dinners do you eat with your (child or parent)?’ Response options were 0–7.
The following ten outcome measures, which came from the 2021 Youth Risk Behavior Survey Middle School and National Youth versions (CDC, 2021), were administered to child participants for the analyses related to construct validity.
2.3.1. Substance use
Alcohol use (lifetime) was measured through asking participants: ‘During your life, on how many days have you had at least one drink of alcohol?’ Alcohol was defined as ‘drinking beer, wine, wine coolers, and liquor such as rum, gin, vodka, or whiskey… (this) does not include drinking a few sips of wine for religious purposes.’ Because the prevalence of alcohol use is lower for this age range, the categorical variable was dichotomized to zero days compared to one or more.
Cigarette smoking (lifetime) was measured by asking participants if they have ‘ever tried cigarette smoking, even one or two puffs?’ (dichotomized).
E-cigarette (electronic vapor products, such as blu, NJOY, or Starbuzz) use (lifetime) was assessed through one question: ‘Have you ever used an electronic vapor product?’ (dichotomized). Electronic vapor products were defined to include e-cigarettes, vapes, vape pens, e-cigars, e-hookahs, hookah pens, and mods.
Marijuana (grass, weed, pot) use (lifetime) was measured by asking participants how many times they have used marijuana, and as with alcohol, responses were dichotomized to zero days compared to one or more.
2.3.2. Violence
Violence was assessed through the question: ‘Have you ever been in a physical fight?’ (dichotomized).
2.3.3. Weight status perception
Perception of weight status was assessed by asking participants how they describe their weight (five levels ranging from ‘very underweight’ to ‘very overweight’), which was dichotomized as ‘overweight’ (slightly or very overweight) and ‘not overweight’ (about the right weight, or slightly or very underweight).
2.3.4. Weight control intention
Weight control intention was assessed by asking participants what they are trying to do about their weight (lose weight, gain weight, stay the same weight, or not trying to do anything about their weight). Responses were dichotomized as ‘trying to lose weight’ and ‘not trying to lose weight’.
2.3.5. Health indicators
Fruit consumption was assessed through the question: ‘During the past 7 days, how many times did you eat fruit? (Do not count fruit juice.)’ Response options included: None, one to three times, four to six times, one time per day, two times per day, three times per day, and four or more times per day, which was dichotomized to fruit consumption less than daily and at least daily.
Vegetable consumption was assessed through a question that was a combination of several questions related to vegetables on the YRBS: ‘During the past 7 days, how many times did you eat vegetables (for example, green salad, carrots – do not include French fries or potato chips)?’ Response options included: None, one to three times, four to six times, one time per day, two times per day, three times per day, and four or more times per day, which was dichotomized to vegetable consumption less than daily and at least daily.
Physical activity was assessed through the question: ‘During the past 7 days, on how many days were you physically active for a total of at least 60 min per day?’ Response options included one through seven and we dichotomized the variable at seven for meeting physical activity guidelines (U.S. Department of Health and Human Services, 2018) and anything less than seven as not.
2.4. Statistical analysis
2.4.1. Item reduction
A total of 2,090 child-parent dyads completed the survey consisting of 22 questions related to family dinners in the child survey and 19 in the parent survey. Table 1 lists the dinner and family mechanics items and child and parent family dinner items with response options that were used in the factor analysis.
Table 1.
Dinner and family mechanics and child and parent family dinner items used in factor analysis with response options.
| Question/Label | Response Options |
|---|---|
| Dinner and Family Mechanics | |
|
0, 1, 2, 3, 4, 5, 6, 7 |
|
15 min or less 30 min 45 min An hour or more |
|
2, 3, 4, 5, 6, 7, 8, 9, 10 or more |
| Child Items | |
|
Never Rarely Sometimes Often Always |
|
Not at all A little Somewhat A lot Very much |
| Parent Items | |
|
Never Rarely Sometimes Often Always |
|
Not at all A little Somewhat A lot Very much |
The final versions of the child and parent FDIs were developed using the following steps: First, an exploratory factor analysis with varimax rotation and Kaiser normalization was used to assess the level of loading of the family dinner questions onto constructs (i.e., factors or latent variables) and to assess their orthogonality. In the factor analysis, family dinner questions with an absolute loading above 0.5 were considered for selection for a particular construct and items were eliminated if they loaded on multiple factors. The factor analysis yielded four constructs for children and four for parents. Children and parents each had factors related to ‘communication’, ‘enjoyment’, and ‘digital distractions’. Children had an additional factor on helping with ‘meal logistics’ and parents had an additional factor related to ‘family bonding’. Second, the number of items was further reduced by selecting the two family dinner questions within each construct that the study team deemed to best characterize these constructs, based on their knowledge of the previous work (Skeer et al., 2018). We chose to retain two items to capture the essence of the constructs while limiting respondent burden (Drolet and Morrison, 2001). Finally, Cronbach’s alpha was used to quantify the level of internal consistency of the resulting constructs. The sum of the eight items in both the FDI-C and FDI-P ranged from 0 to 32. This process was first done in the pilot sample (n = 142) and then in the larger sample (n = 2,090), resulting in the same items for both indices. To assess the applicability of the FDI-C and FDI-P in different subgroups in the national sample, stratified confirmatory factor analyses were conducted to assess whether the constructs in the larger samples persisted across the categories of children’s age, children’s sex, parent’s ethnicity and race, and census region of residence (presented in Supplementary material).
2.4.2. Validity testing
Following development, the FDI was assessed for concurrent criterion validity by estimating the Pearson correlation between the FDI scores and frequency, the current, pervasively used measure of family dinners. Family dinner frequency was selected as the criterion (DeVellis and Thorpe, 2021, Eisenberg et al., 2004). Using multivariable log-binomial regression models, we examined the relationships between FDI scores (dichotomized at the median split for the children and the parents separately) and each of the outcome variables, which included topics of substance use, violence, weight perception, weight control intention, and health indicators. The results were summarized in terms of prevalence ratios (PR) with 95% confidence intervals. In addition, the FDI scores were related to an overall composite of ‘negatives outcomes’ by using a multilevel log-binomial regression model, which simultaneously considered all outcomes as dependent variables. All models were adjusted for the following factors: children’s age category, parent’s ethnicity and race, and census region. SAS 9.4 was used for all analyses and results with p-values < 0.05 were deemed to be statistically significant.
3. Results
3.1. Quantitative survey
Table 2 displays the demographic characteristics of the children and parents in the national sample (n = 2,090). The mean (sd) age of children was 14.9 (1.7) years, 48.7% were female, and their racial/ethnic breakdown was: 52.5% non-Hispanic white, 14.5% black or African American, and 21.2% Hispanic. The mean (sd) age of the parents was 40.5 (6.6) years, 68.7% were female, 76.0% had college or higher education, 53.7% had household incomes exceeding $50,000 and their racial/ethnic breakdown was: 58.9% non-Hispanic white, 14.7% black or African American, and 18.6% Hispanic.
Table 2.
Descriptive Statistics of Children and Parents from the U.S. Based Sample (n = 2090); October 2021-February 2022.
| Children | |
|---|---|
| Age in years, mean (sd) | 14.9 (1.7) |
| Age category, n (%) | |
| 12 to 12.9 years | 341 (16.3) |
| 13 to 13.9 years | 395 (18.9) |
| 14 to 14.9 years | 363 (17.4) |
| 15 to 15.9 years | 366 (17.5) |
| 16 to 16.9 years | 317 (15.2) |
| 17 to 17.9 years | 308 (14.7) |
| Gender, n (%) | |
| Female | 1019 (48.7) |
| Male | 1036 (49.6) |
| Non-Binary | 35 (1.7) |
| Ethnicity and race, n (%) | |
| Hispanic or Latino | 444 (21.2) |
| White, Non-Hispanic | 1097 (52.5) |
| Black, Non-Hispanic | 302 (14.5) |
| Asian/Other/Multi, Non-Hispanic | 247 (11.8) |
| Parents | |
| Age in years, mean (sd) | 40.5 (6.6) |
| Age category, n (%) | |
| 25 to 34.9 years | 403 (19.3) |
| 35 to 44.9 years | 1231 (58.9) |
| 45 to 79.9 years | 456 (21.8) |
| Gender, n (%) | |
| Female | 1437 (68.7) |
| Male | 641 (30.7) |
| Non-Binary | 12 (0.6) |
| Ethnicity and race, n (%) | |
| Hispanic or Latino | 389 (18.6) |
| White, Non-Hispanic | 1232 (58.9) |
| Black, Non-Hispanic | 307 (14.7) |
| Asian/Other/Multi, Non-Hispanic | 162 (7.8) |
| Education level, n (%) | |
| High school or less | 501 (24.0) |
| College | 908 (43.4) |
| University | 681 (32.6) |
| Household income, n (%) | |
| $0 to $25,999 | 463 (22.1) |
| $26,000 to $49,999 | 505 (24.2) |
| $50,000 to $74,999 | 371 (17.8) |
| $75,000 or more | 751 (35.9) |
| Census region place of residence, n (%) | |
| Northeast | 442 (21.2) |
| Midwest | 335 (16.0) |
| South | 952 (45.5) |
| West | 361 (17.3) |
Among children in the sample, the average prevalence of the ten negative outcomes was 30.2%. The prevalence of substance use was: 21.1% for drinking alcohol, 12.5% for smoking cigarettes, 17.8% for vaping, and 15.4% for using marijuana. Further, 28.9% of the children reported having been in a fight. A total of 22.7% of the children perceived themselves as overweight and 16.4% were trying to lose weight. Finally, 48.0% of the children had less than daily fruit consumption, 46.6% had less than daily vegetable consumption, and 72.8% did not meet guidelines for daily physical activity.
3.2. Final FDI items
The following results were initially found in the pilot sample and then reproduced with the same outcomes in the larger sample. The item reduction procedure resulted in eight items each for the FDIs. The individual items loaded strongly and orthogonally on each of the four factors in the FDI-C and FDI-P; all factor loadings were above 0.7 with very little cross-contamination of items across different factors. The items forming the FDI-C and FDI-P, within each factor, are displayed in Table 3, Table 4. Of note, the factors and items did not change between the pilot sample and larger sample, demonstrating robust results. The stratified confirmatory factor analyses showed consistent construct factor loadings across the categories of demographic variables, including by children’s age group, children’s gender, parent’s race and ethnicity, and census region of residence (see Supplementary material).
Table 3.
Child Results from the Exploratory Factor Analysis from the U.S. Based Sample (n = 2090); October 2021-February 2022.
| Item | Mean (sd) | Factor 1a | Factor 2a | Factor 3a | Factor 4a |
|---|---|---|---|---|---|
| In general, how much do people talk to each other during family dinners? | 3.90 (0.96) | 0.90 | 0.18 | −0.04 | 0.03 |
| How much do you participate in the conversation during family dinners? | 3.69 (1.01) | 0.80 | 0.29 | 0.01 | 0.23 |
| How much do you like being with your parent/guardian during family dinners? | 4.14 (0.92) | 0.22 | 0.88 | −0.03 | 0.15 |
| How much do you like being with members of your family during family dinners? | 4.01 (0.97) | 0.25 | 0.85 | 0.02 | 0.23 |
| How often are people allowed to talk, send messages, or watch something during family dinners using personal devices (for example, phones)? | 2.72 (1.31) | 0.04 | −0.01 | 0.90 | 0.06 |
| How often do people actively watch shows, movies, or sports games during family dinners (when it is not just on in the background)? | 2.65 (1.24) | −0.08 | −0.01 | 0.89 | 0.08 |
| How much do you like chores that go along with dinners (for example, setting or clearing the table, washing the dishes) during family dinners? | 2.56 (1.35) | 0.12 | 0.07 | 0.15 | 0.86 |
| How much do you like helping with cooking during family dinners? | 3.37 (1.32) | 0.10 | 0.30 | −0.01 | 0.78 |
Proportion of variance explained by the two bolded items: Communication = 24.9%; Enjoyment = 26.6%; Digital Distractions = 25.1%;Dinner Logistics = 23.4%.
Cronbach’s Alpha of the two bolded items: Communication = 0.75; Enjoyment = 0.82; Digital Distractions = 0.75; Dinner Logistics = 0.64.
Factor 1 = Communication; Factor 2 = Enjoyment; Factor 3 = Digital Distractions; Factor 4 = Dinner Logistics.
Table 4.
Parent Results from the Exploratory Factor Analysis from the U.S. Based Sample (n = 2090); October 2021-February 2022.
| Item | Mean (sd) | Factor 1a | Factor 2a | Factor 3a | Factor 4a |
|---|---|---|---|---|---|
| In general, how much do people talk to each other during family dinners? | 3.93 (0.88) | 0.89 | 0.13 | −0.03 | 0.19 |
| How much does your child participate in the conversation during family dinners? | 3.93 (0.93) | 0.82 | 0.34 | −0.01 | 0.12 |
| How much do you think your child enjoys family dinners in general (note: this does not include the food being served)? | 3.96 (0.98) | 0.22 | 0.90 | 0.02 | 0.20 |
| How much do you think your child likes having dinner with you? | 4.06 (0.96) | 0.23 | 0.89 | −0.01 | 0.20 |
| How often are people allowed to talk, send messages, or watch something during family dinners using personal devices (for example, phones)? | 2.79 (1.26) | 0.03 | −0.01 | 0.89 | −0.03 |
| How often do people actively watch shows, movies, or sports games during family dinners (when it not just on in the background)? | 2.74 (1.18) | −0.06 | 0.02 | 0.88 | −0.05 |
| How important is time to speak with your child a reason for eating family dinners with your child? | 4.44 (0.80) | 0.13 | 0.16 | −0.06 | 0.87 |
| How important is building or maintaining stability in the family a reason for eating family dinners with your child? | 4.46 (0.79) | 0.17 | 0.20 | −0.03 | 0.85 |
Proportion of variance explained by the two bolded items: Communication = 24.5%; Enjoyment = 27.2%; Digital Distractions = 23.9%;Family Bonding = 24.4%.
Cronbach’s Alpha of the two bolded items: Communication = 0.77; Enjoyment = 0.88; Digital Distractions = 0.73; Family Bonding = 0.74.
Factor 1 = Communication; Factor 2 = Enjoyment; Factor 3 = Digital Distractions; Factor 4 = Family Bonding.
An overall score for the FDI-C and the FDI-P were calculated by reverse-coding the Digital Distraction items (Digital Distractions) and then summing the scores from the eight questions, yielding an overall score ranging from 0 to 32. Cronbach’s alpha for the FDI-C and FDI-P ranged from 0.66 and 0.88 (see footnote in Table 3, Table 4).
3.3. Criterion and construct validity
The Pearson correlation between the overall FDI scores and frequency of family dinners in the sample (test for criterion validity) was 0.33 for children (p < 0.001) and 0.29 for parents (p < 0.001). The mean (sd) overall scores for the child and parent FDIs were 20.3 (4.9) and 23.2 (4.5), respectively, with scores ranging from 3 to 32 and 6 to 32, respectively, out of a possible maximum of 32 (higher scores representing more positive family meal atmospheres).
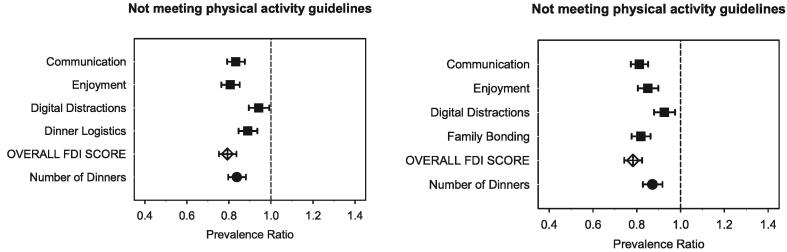
Table 5 presents the associations between dichotomized FDI scores and health and risk-related outcomes for children and parents, which provide evidence of construct validity (graphically displayed in Fig. 1). Overall, children who scored greater than or equal to 21 or had parents who scored greater than or equal to 24 had lower prevalence of the negative outcomes. Children who scored ≥21 on the FDI-C had a significantly lower negative outcome composite (PR: 0.77; 95% CI: 0.72–0.81; p < 0.001) and had significant reductions in each individual negative outcome (PR ranging from 0.67 to 0.87). Parents who scored ≥24 on the FDI-P had children who had a significantly lower negative outcome composite score (PR: 0.80; 95% CI: 0.76–0.84; p < 0.001) and had significant reductions in almost all of the individual negative outcomes (PR ranging from 0.76 to 0.81), with the exception of vaping, violence, and weight intentions.
Table 5.
Evidence of Construct Validity: Adjusted Prevalence and Adjusted Prevalence Ratios of Health and Risk-Related Outcomes by Children and Parents Dichotomized FDI Scores from the U.S. Based Sample (n = 2090); October 2021-February 2022.
| Children |
Parents |
|||||||
|---|---|---|---|---|---|---|---|---|
| Outcomes | FDI > 21a (N = 1021)n (%) |
FDI < 21a (N = 1069)n (%) |
Prevalence Ratio (95% CI) |
P-value | FDI > 24b (N = 1068)n (%) |
FDI < 24b (N = 1022)n (%) |
Prevalence Ratio (95% CI) |
P-value |
| Negative outcome composite c | 2629/10210 (24.9) |
3687/10690 (32.5) |
0.77 (0.72 to 0.81) |
< 0.001 | 2852/10680 (25.5) |
3464/10220 (31.9) |
0.80 (0.76 to 0.84) |
< 0.001 |
| Substance use | ||||||||
| Ever had at least one drink of alcohol | 177 (13.8) | 264 (17.7) | 0.78 (0.66 to 0.92) |
0.003 | 192 (14.2) | 249 (17.5) | 0.81 (0.69 to 0.95) |
0.009 |
| Ever tried cigarette smoking | 108 (7.8) | 153 (9.8) | 0.79 (0.63 to 0.99) |
0.046 | 115 (7.8) | 146 (9.8) | 0.79 (0.63 to 0.99) |
0.045 |
| Ever used an electronic vapor product | 156 (10.9) | 217 (13.2) | 0.83 (0.69 to 0.99) |
0.039 | 176 (11.4) | 197 (12.7) | 0.90 (0.75 to 1.07) |
0.22 |
| Ever used marijuana | 130 (9.6) | 192 (12.5) | 0.77 (0.63 to 0.93) |
0.008 | 138 (9.7) | 184 (12.5) | 0.78 (0.64 to 0.95) |
0.012 |
| Violence: ever been in physical fight | 269 (26.6) | 335 (30.6) | 0.87 (0.76 to 0.99) |
0.040 | 302 (28.1) | 302 (29.0) | 0.97 (0.85 to 1.10) |
0.62 |
| Weight perception | ||||||||
| Describe oneself as overweight | 196 (18.3) | 278 (24.3) | 0.75 (0.64 to 0.89) |
0.001 | 211 (18.6) | 263 (24.1) | 0.77 (0.66 to 0.91) |
0.001 |
| Weight intention | ||||||||
| Trying to lose weight | 147 (13.3) | 196 (16.7) | 0.80 (0.66 to 0.97) |
0.025 | 158 (13.5) | 185 (16.4) | 0.82 (0.68 to 1.01) |
0.051 |
| Health indicators | ||||||||
| < Daily fruit consumption | 392 (36.0) | 612 (53.6) | 0.67 (0.61 to 0.74) |
< 0.001 | 444 (38.8) | 560 (51.2) | 0.76 (0.69 to 0.83) |
< 0.001 |
| < Daily vegetable consumption | 394 (36.1) | 579 (50.6) | 0.71 (0.65 to 0.78) |
< 0.001 | 432 (37.7) | 541 (49.5) | 0.76 (0.69 to 0.84) |
< 0.001 |
| Not meeting guidelines for physical activity | 660 (66.4) | 861 (83.7) | 0.79 (0.75 to 0.84) |
< 0.001 | 684 (66.0) | 837 (84.3) | 0.78 (0.74 to 0.82) |
< 0.001 |
Child FDI range: 0 to 32.
Parent FDI range: 0 to 32.
Multivariate analysis from a multilevel linear mixed model which simultaneously considered all negative outcomes as dependent variables. All estimates adjusted for children’s age category, parent’s ethnicity and race, and census region.
Fig. 1.
Relationships between Dichotomized Child and Parent FDI Scores and Child Health- and Risk-Related Outcomes.
Fig. 2 graphically displays how each factor relates to the different outcomes and to the number of family dinners, demonstrating the relative importance of the factors to the outcomes.
Fig. 2.
Relationships Between the FDI Constructs for Children and Parents and Number of Family Dinners with Each Child Health/Risk-Related Outcome.
4. Discussion
In an initial phase, we used qualitative methods to develop a new set of measures that go beyond frequency and help elucidate mechanisms for the observed associations between family dinners and adolescent health and wellbeing (Boateng et al., 2018). Here, we present the finalized versions of the FDI and provide evidence of concurrent criterion validity and construct validity.
Using factor analysis, we identified eight items representing four constructs, including ‘communication’, ‘enjoyment’, and ‘digital distractions’ for both children and parents, as well as ‘meal logistics’ for children and ‘family bonding ‘for parents. These items have face validity and align with mechanisms that other researchers have speculated as causal factors in the relationship between family meals and adolescent health outcomes (Fulkerson et al., 2006, Goldfarb et al., 2015, Haghighatdoost et al., 2017, Harrison et al., 2015, Skeer and Ballard, 2013). Further support for the items we identified is provided by a recent meta-analysis, which found a consistent positive association between child nutritional outcomes and three of the family meal characteristics related to those included in the FDIs: a positive family meal atmosphere was associated with healthier nutritional outcomes, as was having the television off during meals and meal preparation (Dallacker et al., 2019).
Each set of items demonstrated moderate to strong internal consistency reliability. With respect to validity, FDI scores had moderate correlations with frequency of family dinners in the sample, providing some evidence of concurrent criterion validity, while also indicating that the FDI adds more complexity than the measure of frequency alone. While no absolute gold standard exists, in future studies FDI scores can be compared against coded video-recordings of family meals (Berge, 2021, Berge et al., 2014, Skeer et al., 2022) to further evaluate concurrent criterion validity. The results are also suggestive of construct validity based on the cross-sectional associations between child scores on the indices and an associated reduced risk of all of the studied outcomes, as well as between child scores on the indices and an associated reduced risk of alcohol, cigarette, and marijuana use, as well as negative weight perception, trying to lose weight, not eating fruit and vegetables at least one time per day, and not meeting guidelines for physical activity. As a next step, these associations can be evaluated longitudinally to establish predictive criterion validity.
The FDI-C and FDI-P have the potential to expand the family meal literature and help researchers and practitioners tailor family-based prevention programs accordingly. For example, these indices may eventually be used in larger, longitudinal epidemiologic studies to establish evidence for mechanisms in the relationship between family dinners and youth risk- and health-related outcomes. The brevity of the measures allows for their ready integration into a battery of study questionnaires to be able to address various questions. These data may ultimately be used to develop new and innovative prevention interventions specifically around family dinners.
This study has several strengths. We adhered to best practices for measure development (Boateng et al., 2018) and conducted each of the appropriate steps, starting with extensive qualitative work and starting with a pilot study. Additionally, the cognitive interviews, preliminary validity testing, and validity testing with a large, national sample were done in samples that had racial/ethnic diversity, and likely have some ability to cross cultures; and with range of education levels, suggesting good comprehension of the items across levels of education.
There are important limitations to note. First, the age range limited the ability to examine associations with certain risk factors that are more prevalent among older youth (e.g., substance use). Second, we limited participation to those who were able to speak, read, and understand English well enough to complete study procedures. It is therefore necessary to examine the psychometric properties of the FDIs with populations with different language capabilities and literacy levels. Third, while Qualtrics had processes in place to verify participants, it was not possible to prevent parents from responding for their child. However, the distribution of risk-related behaviors (e.g., substance use, violence) in our sample approximated a nationally representative survey of 12–17-year-olds from the National Survey on Drug Use and Health (SAMHSA, 2021), providing confidence that this did not threaten the validity of the sample. Finally, the study was cross-sectional, so we are not able to determine the directionality of the associations. However, as behaviors in the family environment, such as eating dinner together, often occur before the onset of many of the risk behaviors addressed in this study, we have confidence about the associations. As noted, our results provide support for concurrent criterion validity and construct validity, but do not definitively establish either. Future studies with longitudinal data collection and analysis are warranted to assess criterion validity more fully, based on the promise demonstrated in this study. Further assessment of validity is warranted.
5. Conclusions
Family meals are consistently associated with healthier habits and outcomes among youth, yet the underlying protective mechanisms remain poorly understood. By developing and validating a brief, multi-dimensional measure of family dinners, the present study fills a critical research gap and will allow for greater consistency and collaboration among researchers focusing on range of adolescent health outcomes. Elucidating these mechanisms is of particular public health interest given the potential for an extended health impact linked to this single behavior. Future studies should examine associations between dimensions of family dinners and adolescent health- and risk-related outcomes, helping researchers and practitioners to identify points of emphasis and to tailor family-based prevention programs accordingly.
CRediT authorship contribution statement
Margie R. Skeer: Conceptualization, Methodology, Investigation, Resources, Data curation, Writing – original draft, Supervision, Project administration, Funding acquisition. Misha Eliasziw: Methodology, Formal analysis, Writing – original draft, Visualization. Kendrin R. Sonneville: Investigation, Resources, Writing – review & editing, Project administration. Sara C. Folta: Investigation, Resources, Writing – original draft, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The team would like to thank the Weiner Hailey family for their support and commitment to substance use prevention research. We would also like to acknowledge Drs. Olohirere Ezomo and Ebuwa Igho-Osagie for their work on Phase II of this research; Grace Hajinazarian, Rachael Sabelli, and Jinan Moumneh for their work on editing the manuscript; and Drs. Kenneth Chui and Kimberly Dong Breen for their thoughtful review.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102318.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Berge J.M. Families, Food, and Parenting. Springer; 2021. Mixed-Methods Assessment of Childhood Obesity: Parental and Familial Factors; pp. 115–137. [Google Scholar]
- Berge J.M., Rowley S., Trofholz A., Hanson C., Rueter M., MacLehose R.F., Neumark-Sztainer D. Childhood obesity and interpersonal dynamics during family meals. Pediatrics. 2014;134(5):923–932. doi: 10.1542/peds.2014-1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boateng G.O., Neilands T.B., Frongillo E.A., Melgar-Quiñonez H.R., Young S.L. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front. Public Health. 2018;6:149. doi: 10.3389/fpubh.2018.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2021). Youth Risk Behavior Survey Questionnaire. Centers for Disease Control and Prevention. Available at: www.cdc.gov/yrbs.
- Christian M.S., Evans C.E., Hancock N., Nykjaer C., Cade J.E. Family meals can help children reach their 5 A Day: a cross-sectional survey of children's dietary intake from London primary schools. J. Epidemiol. Community Health. 2013;67(4):332–338. doi: 10.1136/jech-2012-201604. [DOI] [PubMed] [Google Scholar]
- Dallacker M., Hertwig R., Mata J. Quality matters: A meta-analysis on components of healthy family meals. Health Psychol. 2019;38(12):1137. doi: 10.1037/hea0000801. [DOI] [PubMed] [Google Scholar]
- DeVellis R.F., Thorpe C.T. Sage Publications; 2021. Scale Development: Theory and Applications. [Google Scholar]
- Drolet A.L., Morrison D.G. Do we really need multiple-item measures in service research? J. Serv. Res. 2001;3(3):196–204. doi: 10.1177/109467050133001. [DOI] [Google Scholar]
- Eisenberg M.E., Olson R.E., Neumark-Sztainer D., Story M., Bearinger L.H. Correlations between family meals and psychosocial well-being among adolescents. Arch. Pediatr. Adolesc. Med. 2004;158(8):792–796. doi: 10.1001/archpedi.158.8.792. [DOI] [PubMed] [Google Scholar]
- Fulkerson J.A., Story M., Mellin A., Leffert N., Neumark-Sztainer D., French S.A. Family dinner meal frequency and adolescent development: relationships with developmental assets and high-risk behaviors. J. Adolesc. Health. 2006;39(3):337–345. doi: 10.1016/j.jadohealth.2005.12.026. [DOI] [PubMed] [Google Scholar]
- Goldfarb S.S., Tarver W.L., Locher J.L., Preskitt J., Sen B. A systematic review of the association between family meals and adolescent risk outcomes. J. Adolesc. 2015;44(1):134–149. doi: 10.1016/j.adolescence.2015.07.008. [DOI] [PubMed] [Google Scholar]
- Haghighatdoost F., Kelishadi R., Qorbani M., Heshmat R., Motlagh M.E., Ardalan G., Azadbakht L. Family dinner frequency is inversely related to mental disorders and obesity in adolescents: the CASPIAN-III study. Arch. Iran. Med. 2017;20(4) [PubMed] [Google Scholar]
- Hammons, A. J., Fiese, B. H. (2011). Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics, 127(6), e1565-e1574. [DOI] [PMC free article] [PubMed]
- Harbec M.-J., Pagani L.S. Associations between early family meal environment quality and later well-being in school-age children. J. Dev. Behav. Pediatr. 2018;39(2):136–143. doi: 10.1097/DBP.0000000000000520. [DOI] [PubMed] [Google Scholar]
- Harrison M.E., Norris M.L., Obeid N., Fu M., Weinstangel H., Sampson M. Systematic review of the effects of family meal frequency on psychosocial outcomes in youth. Can. Fam. Physician. 2015;61(2):e96–e106. [PMC free article] [PubMed] [Google Scholar]
- Marques, A., Naia, A., Branquinho, C. S. d. S., Matos, M. (2018). Adolescents’ eating behaviours and its relationship with family meals, body mass index and body weight perception. Nutrición Hospitalaria, 35(3), 550-556. [DOI] [PubMed]
- Middleton G., Golley R., Patterson K., Le Moal F., Coveney J. What can families gain from the family meal? A mixed-papers systematic review. Appetite. 2020;153 doi: 10.1016/j.appet.2020.104725. [DOI] [PubMed] [Google Scholar]
- Mitchell M., Piazza-Waggoner C., Modi A., Janicke D. Examining short-term stability of the Mealtime Interaction Coding System (MICS) J. Pediatr. Psychol. 2009;34(1):63–68. doi: 10.1093/jpepsy/jsn043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyper E., Harrington D., Manson H. The impact of different types of parental support behaviours on child physical activity, healthy eating, and screen time: a cross-sectional study. BMC Public Health. 2016;16(1):1–15. doi: 10.1186/s12889-016-3245-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAHMSA . Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; Rockville, MD: 2020. 2020 National Survey on Drug Use and Health Public Use File Codebook. [Google Scholar]
- SAMHSA. (2021). Center for Behavioral Health Statistics and Quality. 2021 National Survey on Drug Use and Health. Table 2.26B – Alcohol Use in Past Year: Among People Aged 12 or Older; by Age Group and Demographic Characteristics, Percentages. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt39441/NSDUHDetailedTabs2021/NSDUHDetailedTabs2021/NSDUHDetTabsSect2pe2021.htm#tab2.25b.
- Skeer M.R., Ballard E.L. Are family meals as good for youth as we think they are? A review of the literature on family meals as they pertain to adolescent risk prevention. J. Youth Adolesc. 2013;42(7):943–963. doi: 10.1007/s10964-013-9963-z. [DOI] [PubMed] [Google Scholar]
- Skeer, M. R., Sabelli, R. A., Rancaño, K. M., Lee-Bravatti, M., Ryan, E. C., Eliasziw, M., Spirito, A. (2022). Randomized controlled trial to test the efficacy of a brief, communication-based, substance use preventive intervention for parents of adolescents: Protocol for the SUPPER Project (Substance Use Prevention Promoted by Eating family meals Regularly). PLoS One, 17(2), e0263016. [DOI] [PMC free article] [PubMed]
- Skeer M.R., Sonneville K.R., Deshpande B.R., Goodridge M.C., Folta S.C. Going beyond frequency: A qualitative study to explore new dimensions for the measurement of family meals. J. Child Fam. Stud. 2018;27(4):1075–1087. [Google Scholar]
- U.S. Department of Health and Human Services. (2018). Physical Activity Guidelines for Americans, 2nd edition. Washington, DC: U.S. Department of Health and Human Services.
- University of Minnesota. (n.d.). Project EAT (Eating and Activity over Time). Available at:https://www.sph.umn.edu/research/projects/project-eat/.
- Willis, G. B. (2004). Cognitive Interviewing: A Tool for Improving Questionnaire Design. Sage Publications.
- Yockey R.A., King K.A., Vidourek R.A. Family factors and parental correlates to adolescent conduct disorder. J. Fam. Stud. 2021;27(3):356–365. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.