Abstract
Introduction
Penile fracture is very uncommon urological condition. Sexual intercourse in most areas remains the major causative entity. Diagnosis is merely through clinical history, signs and symptoms. Surgical management has emerged as the gold standard option for penile fracture.
Case presentation
we present a case of a young man who sustained penile fracture during sexual intercourse. It involved the left corpora cavernosum and early surgical repair was done successfully.
Discussion
Penile fracture during sexual intercourse is due to impaction of erected penis against the female perineum. It's mostly unilateral but also bilateral with or without involvement of urethra. Investigations such as retrograde urethrogram, ultrasound, MRI and urethrocystoscopy can be done for assessment of severity of the injury. Early surgical repair of the injury has yield better outcome in both sexual and voiding function.
Conclusion
Penile fracture being rare urological condition but sexual intercourse has remained the major risk factor. Early surgical intervention is gold standard for its management as it’s associated with very minimal long term complication.
Keywords: Penile fracture, Tanzania
Highlights
-
•
Penile fracture is a very rare urological condition.
-
•
Sexual intercourse still the leading cause of penile fracture.
-
•
Diagnosis is mainly by clinical sign and symptoms, other investigations are for severity assessment.
-
•
Early surgical exploration and repair is the gold standard in management.
1. Introduction
Penile fracture is uncommon urological surgical condition. It’s defined as a the rupture of the tunica albuginea of the corpus cavernosum due to trauma during rigid erection [1]. Tunica albuginea is very thin and not flexible during erection which predispose to easy rupture [2].
There are several causes but Sexual intercourse due to impaction of erected penis against the female perineum remain the major cause and others being masturbation and falling off the bed or fighting [2].
The usual classical presentations include cracking sound during rigid erection followed by immediate pain, rapid detumescence and then rapid swelling and later with or without ecchymosis. The diagnosis of PF is usually done by thorough clinical presentation and physical examination though some investigations such us penile ultrasound, MRI and Urethroscopy or urethrogram can also be done in some cases [3,4].
Early surgical exploration with closure of tunica albuginea has remained the best option to prevent post-operative complications such as sexual and voiding dysfunction [5,6]. We report the case with a literature review. This manuscript was prepared in accordance with the SCARE 2020 guidelines [7].
2. Case presentation
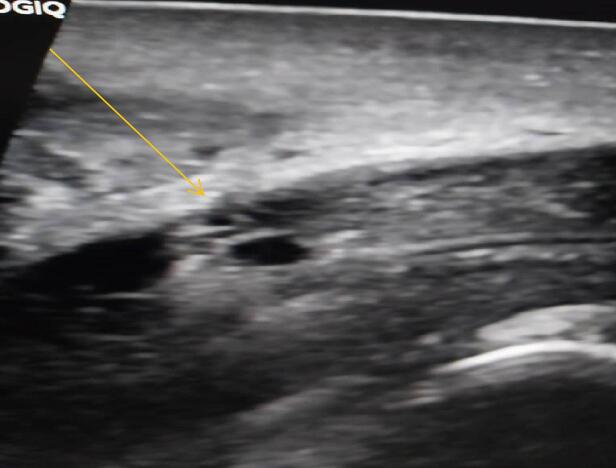
We report a case of a 27-year-old male who was referred to our facility from a secondary care hospital, he presented to the emergency department 34 h after sustaining injury to the penis during sexual intercourse with his wife. During intercourse he felt an abrupt pop sensation in the penis which was painful initially but the pain subsided immediately afterwards, it was associated with detumescence and gradual swelling of the penis and scrotum. He was voiding normally and there was no blood in urine. The review of systems was normal and the past medical history was uneventful. On examination the penis was swollen particularly in the proximal part, it was deviated to the left side, non-tender, the rolling sign was present on the right side of the penile shaft (Fig. 1). A penile ultrasound was performed which revealed a tear in the left proximal lateral corpus carvenosus with a subcutaneous hematoma (Fig. 2).
Fig. 1.
Swollen penis with rolling sign.
Fig. 2.
Tear in the left proximal lateral corpus carvenosus with hematoma.(yellow arrow).
The patient was taken to the theater for emergency penile exploration and repair of the tear which was performed by a urologist. Circumferential Sub coronal degloving incision was made, hematoma was evacuated, tunica albuginea tear of the left lateral corpus cavernosus was noted and urethra was intact (Fig. 3). The tear was repaired with vicryl 20 interrupted suture technique (Fig. 4). Urethral catheter was inserted and skin was closed with vicryl 30.
Fig. 3.

Tunica albuginea tear of the left lateral corpus cavernosus (black arrow).
Fig. 4.

Repaired tear with interrupted suture.
Post operatively the patient was kept on antibiotics and analgesia. Urethral catheter was removed on the third day postoperative. Wound was clean and he was discharge with oral antibiotics for next 7 days. During 6 months follow up the patient reported normal voiding and sexual function (Fig. 5).
Fig. 5.

Well healed penis 6 months post repair.
3. Discussion
Penile injury is very uncommon in urology with global incidence of 1 to 175,000 [8]. This is due to anatomical position protection and due to flexibility of genitalia. Penile fracture involves tearing of tunica albuginea in the erect state. In flaccid state, the penis in its position is well protected against the blunt trauma and the tunica albuginea thickness is 2 mm. In erect state, the tunica albuginea becomes thin to 0.25 mm making it very easy to rupture in case of abrupt penile trauma [2,6].
Sexual intercourse trauma as it's also for this case as is the most cause for penile fracture. This was reported in many studies done in Europe and USA as the study done by Leandro et al. in 2010 sexual trauma was main etiologic factor with 93.3 %(140) followed by masturbation 10(6.7 %) cases. Sex position such as woman on top and reverse cowgirl styles has been attributed as a major cause for severe penile fracture which is the same to this case report [[9], [10], [11]].
Diagnosis of penile fracture is easily made from patient thorough clinical history and physical examination to determine duration and site of injury and presence of fracture. No need of further tests in most cases as however some investigations are being added for further confirmation of the diagnosis and sometimes assessing the severity of the injury [12]. Penile ultrasound is widely used as it easily assessable in most areas but results can be operator dependent especially in assessing the carvenosus severity. Retrograde Urethrogram is also being advocated for these patients as it helps to show any involvement of the urethral injury. This can also be assessed with urgent urethrocystoscopy. MRI of the penis can also be done as it shows to be more accurate for assessing soft tissue disruption especially those involving corpora carvenosus. It also helps to give details on vascular pattern of both corpora carvenosus and tunica albuginea hence giving accurate diagnosis [6]. But MRI being expensive and unavailable in most of our hospital facilities it's not usually done.
Management of penile fracture has been some with controversy with conservative management and early surgical repair being the options available. Conservative management involves compression dressing, urethral catheterization, antibiotics and anti-inflammatory drugs, and erection suppression drugs being advised in patient confirmed with low corpora carvenosus injury involvement and also depending on Ultrasound findings. It’s associated with severe post injury penile curvature, persistent hematoma, abscess and erectile dysfunction [2,4,5]. Early penile surgical exploration and repair of tunica albuginea is now the gold standard option for management of PF to avoid long term complications. This involves subcorona degloving incision of the penis which gives better view of the corpora bodies and location of the tunica albuginea tear, with easy hematoma evacuation, assessment of urethral injury and hence easy surgical repair [4,8].
4. Conclusion
Penile fracture being rare urological condition a rapid diagnosis by history and clinical examination with or without other investigations remain important part and surgical intervention is key for management. Early surgical intervention is the best option as its associated with significantly fewer complications.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Patient consent
Written informed consent was obtained from the patient's parents/ legal guardian for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical Approval was provided from our institution.
Funding
The author received no financial support for this article.
Authorship contribution
Vitus Kajerero; involved in surgery, study concept and design, literature review and manuscript writing Okoa Sukunala: Supervision;writing-review and editing; Remigius A. Rugakingira: Writing-review and editing Reuben Mkinga: writing-review and editing. Ogeness J. Mbwambo: Writing-review and editing. Emmanuel Tairo: Writing-review and editing.
Guarantor
Vitus Kajerero
Registration of research studies
-
1.
Name of the registry:
-
2.
Unique identifying number or registration ID:
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Conflict of interest statement
There are no conflicts of interest.
References
- 1.Kozacıoğlu Z., Ceylan Y., Aydoğdu Ö., Bolat D., Günlüsoy B., Minareci S. An update of penile fractures: long-term significance of the number of hours elapsed till surgical repair on long-term outcomes. Turk. Urol. Derg. 2017;43(1):25–29. doi: 10.5152/tud.2016.39129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Taher A.M., Aboul-Ella H.A., Sayed M.A., Gaafar A.A. Management of penile fracture. J. Trauma – Inj. Infect. Crit. Care. 2004;56(5):1138–1140. doi: 10.1097/01.ta.0000033140.73750.14. [DOI] [PubMed] [Google Scholar]
- 3.Kati B., Akin Y., Demir M., Boran OF, Gumus K., Ciftci H. Penile fracture and investigation of early surgical repair effects on erectile dysfunction. Urol. J. 2019;86(4):207–210. doi: 10.1177/0391560319844657. [DOI] [PubMed] [Google Scholar]
- 4.Koifman L., Barros R., Jnior R.A.S., Cavalcanti A.G., Favorito L.A. Penile fracture: diagnosis, treatment and outcomes of 150 patients. Urology. 2010;76(6):1488–1492. doi: 10.1016/j.urology.2010.05.043. [DOI] [PubMed] [Google Scholar]
- 5.Zargooshi J. Sexual function and tunica albuginea wound healing following penile fracture: an 18-year follow-up study of 352 patients from Kermanshah, Iran. J. Sex. Med. 2009;6(4):1141–1150. doi: 10.1111/j.1743-6109.2008.01117.x. [DOI] [PubMed] [Google Scholar]
- 6.Bozzini G., Albersen M., Otero J.R., et al. Delaying surgical treatment of penile fracture results in poor functional outcomes: results from a large retrospective multicenter European study. Eur. Urol. Focus. 2018;4(1):106–110. doi: 10.1016/j.euf.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus surgical case report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 8.Amer T., Wilson R., Chlosta P., et al. Penile fracture: a meta-analysis. Urol. Int. 2016;96(3):315–329. doi: 10.1159/000444884. [DOI] [PubMed] [Google Scholar]
- 9.Barros R., Schulze L., Ornellas A.A., Koifman L., Favorito L.A. Relationship between sexual position and severity of penile fracture. Int. J. Impot. Res. 2017;29(5):207–209. doi: 10.1038/ijir.2017.24. [DOI] [PubMed] [Google Scholar]
- 10.Garofalo M., Bianchi L., Gentile G., et al. Sex-related penile fracture with complete urethral rupture: a case report and review of the literature. Arch. Ital. Urol. Androl. 2015;87(3):260–261. doi: 10.4081/aiua.2015.3.260. [DOI] [PubMed] [Google Scholar]
- 11.Jagodič K., Erklavec M., Bizjak I., Poteko S., Korošec Jagodič H. A case of penile fracture with complete urethral disruption during sexual intercourse: a case report. J. Med. Case Rep. 2007;1:1–3. doi: 10.1186/1752-1947-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barros R., Hampl D., Cavalcanti A.G., Favorito L.A., Koifman L. Lessons learned after 20 years’ experience with penile fracture. Int. Braz. J. Urol. 2020;46(3):409–416. doi: 10.1590/S1677-5538.IBJU.2019.0367. [DOI] [PMC free article] [PubMed] [Google Scholar]