Abstract
Purpose
Enchondromas are primary, benign bone neoplasms that arise from intramedullary proliferation of hyaline cartilage cells. Slow and progressive in growth, enchondromas can lead to bone destruction, deformities, and fractures. The treatment of enchondromas remains controversial. We hereby describe the technique for bone fixation using headless intramedullary screws (HISs) after enchondroma resection in the long bones of the hand.
Methods
From January 2018 to June 2021, all patients treated with HISs after the resection of enchondroma of the hand were retrospectively assessed and included in the study. The series comprised four patients with a minimum postoperative follow-up period of 12 months. Postoperative functional results were measured according to Takigawa criteria and postoperative radiographic results were graded according to the Tordai system.
Results
After tumor resection and screw fixation, one patient had autologous bone grafting from the iliac crest, and another had the defect filled with calcium phosphate cement. All patients were followed up for at least 12 months, and the mean healing time of the pathologic fracture was 5 weeks. There were neither complications related to the procedure nor the need for a second surgery.
Conclusions
We describe the technique of intramedullary headless screws for bone fixation after enchondroma resection in the long bones of the hand, as well as the excellent functional, cosmetic, and radiographic results of four patients treated with the technique presented herewith.
Type of study/level of evidence
Therapeutic IV.
Key words: Enchondroma, Headless screws, Metacarpal fracture, Minimally invasive procedure, Phalangeal fracture
Enchondromas are primary benign neoplasms of bone arising from intramedullary proliferation of hyaline cartilage cells. Therefore, they can be considered hamartomas that originate from persistent cartilaginous islands of the growth plate. Enchondromas are lesions commonly found within the long bones of the hand, representing the most frequent benign bone tumor in this location, which is approximately 90% of cases.1
Having slow and progressive growth, enchondromas can lead to bone destruction, deformities, and fractures. They present typical radiographic features, which show up as lytic lesions with or without calcifications inside, and are most commonly located within the metaphysis of the proximal phalanx or metacarpals of the ulnar fingers.2, 3, 4 On magnetic resonance images, they are visualized as lesions with high signal intensity on T1-weighted images and increased signal intensity regarding the muscle on T2-weighted images. These clinical and radiologic features make biopsy analysis unnecessary for diagnosis and treatment, and it is indicated only for aggressive or atypical lesions.4
The treatment of enchondromas remains controversial. Asymptomatic lesions, usually incidental findings, can be followed without the need for surgery. For large and symptomatic lesions, when there is a risk of fracture or when the enchondroma is diagnosed through a pathologic fracture, the most accepted approach is surgical treatment, with curettage and complete removal of the tumor lesion, which may be associated with adjuvant techniques, with or without filling of the cavity with bone graft or bone cement, and subsequent bone fixation.5,6 Several methods of bone fixation after enchondroma treatment have been described, including intramedullary fixation with K-wires, use of plate and screws, and even external fixation.5
In recent years, there has been a great increase in the use of headless intramedullary screws (HISs) in the treatment of long bone fractures of the hand. Therefore, following these good results, their use has also been extrapolated for the treatment of fracture complications, as in malunion and pseudoarthrosis.7
We hereby describe the technique for bone fixation using HISs after enchondroma resection in the long bones of the hand. A small case series of patients is presented with results and complications.
Materials and Methods
From January 2018 to June 2021, all patients treated with HISs after the resection of enchondroma of the hand were retrospectively assessed and included in the study. The series comprised four patients with a minimum postoperative follow-up period of 12 months. All patients had been investigated with radiographs and magnetic resonance imaging scans before the surgery.
Postoperative functional results were measured according to Takigawa8 criteria, on the basis of the following three factors to classify the patients: (1) appearance (acceptable or not), (2) range of motion (greater than 80% in comparison with the contralateral side), and (3) grip strength (greater than 80% in comparison to the contralateral side); satisfactory results were considered when all three factors were graded as positive.
Postoperative radiographic results were graded according to the Tordai9 system. This system grades patients into the following three groups according to the size of bone defects after tumor resection: (1) group 1, the presence of a bone defect of less than 3 mm in diameter; (2) group 2, bone defect of 4–10 mm in diameter; and (3) group 3, bone defect larger than 10 mm with signs of enchondroma recurrence or persistence.
This study obtained approval of the Institutional Review Board at our institution, and informed consent was collected from each subject.
Results
Surgical technique
With the patient in supine position, a pneumatic tourniquet was applied at the proximal region of the arm, and the upper limb was lain on the hand table. Brachial plexus block and sedation were used for anesthesia.
The procedure was started with a skin incision on the dorsum of the hand, centered on the enchondroma. In eccentric metaphyseal intramedullary lesions, one can choose the approach on the side where most of the tumor is located or through dorsolateral incisions.
Next, a careful dissection was performed to preserve the superficial dorsal veins and sensory nerve branches. On reaching the affected bone, a rectangular window in the cortical bone was made at the tumor site. The exact location can be defined with the help of image intensification. On access to the intramedullary space, tumor tissue removal was carefully performed with the help of straight and curved curettes. The help of image intensification may be warranted at this stage to determine whether the entire lesion has been resected. After the curettage of the medullary canal, some adjuvant methods may be used.
Subsequently, the fracture was reduced, and the HIS guide wire was positioned according to standard fixation technique.10, 11, 12, 13, 14 The largest possible screw should be used to create more stability, following the principle of treatment with intramedullary devices used in other long bones. If a bone graft is chosen, it should be applied after complete curettage of the cavity and fracture fixation. Image intensification is used during guide passage, canal tapping, and implant positioning.
After the procedure, a plaster splint was applied to the affected limb. The first postoperative evaluation for dressing change was scheduled to occur at approximately the fifth postoperative day. The immobilization was removed at approximately the third week and replaced by buddy taping, in which active and passive motion exercises are prescribed and encouraged. Monthly follow-up visits and radiographs occured until the fourth month after surgery, and then, every 3 months, until 1 year of follow-up was completed. After radiographic- and clinically-verified bone healing, the patient was released for normal daily living and physical activities.
Case Series
Case 1
A 54-year-old female patient presented with pain, swelling, and deformity of the little finger of her left hand after a low-energy trauma. Radiographs, magnetic resonance imaging, and computed tomography showed a pathologic fracture caused by an enchondroma of the fifth metacarpal (Fig. 1). Surgical treatment was performed with curettage through a dorsoulnar cortical window, using image intensification to confirm the complete resection of the tumor (Fig. 2). Cauterization was used as an adjuvant and the fracture was fixated with two 3-mm diameter HISs inserted retrograde through the metacarpophalangeal joint. The correct position of the screws could be confirmed through the bone window used for the resection of the tumor. After 4 weeks, complete healing was demonstrated on radiographs with proper functional recovery and satisfactory wound healing (Fig. 3).
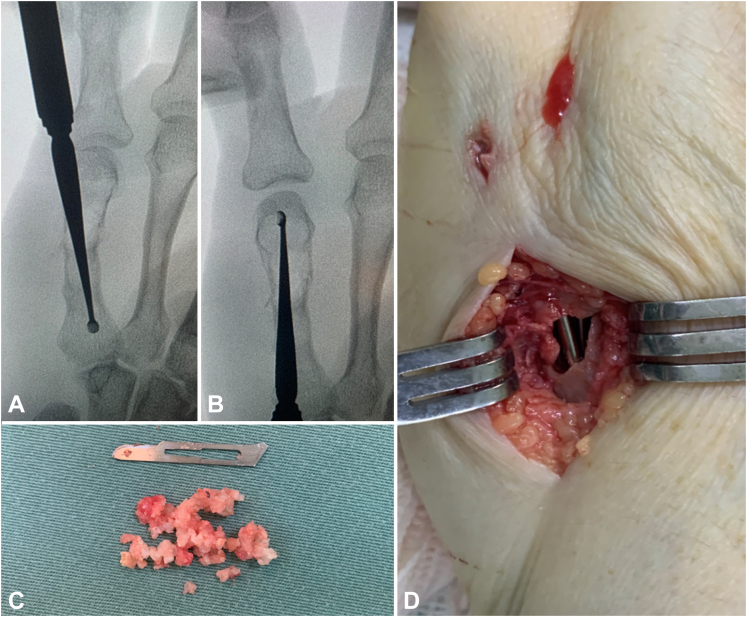
Figure 1.
A A 54-year-old female patient presented with pain, swelling, and deformity of the little finger of her left hand after a low energy trauma, with B, C radiographs, D magnetic resonance imaging, and E computed tomography images showing a pathologic fracture caused by enchondroma of the fifth metacarpal.
Figure 2.
A, B With the aid of an image intensifier, the patient underwent C tumor curettage through a cortical window and D fixation with intramedullary screw.
Figure 3.
A Adequate positioning of the screws is confirmed by perioperative image intensification. B After 4 weeks, satisfactory scar appearance C and radiographic bone healing is evident.
Case 2
A 28-year-old female patient presented with pain and swelling of the little finger of her left hand after a low-energy trauma. Imaging showed a characteristic pathologic fracture of the proximal phalanx caused by an enchondroma located within the proximal metaphysis (Fig. 4). Surgical treatment was performed with a dorsal approach, creation of a window at the dorsal cortex, and subsequent curettage. Cauterization and phenol application followed as an adjuvant treatment, and then, the fracture was treated with a 3-mm anterograde HIS (Fig. 5). The fracture healed uneventfully after 5 weeks.
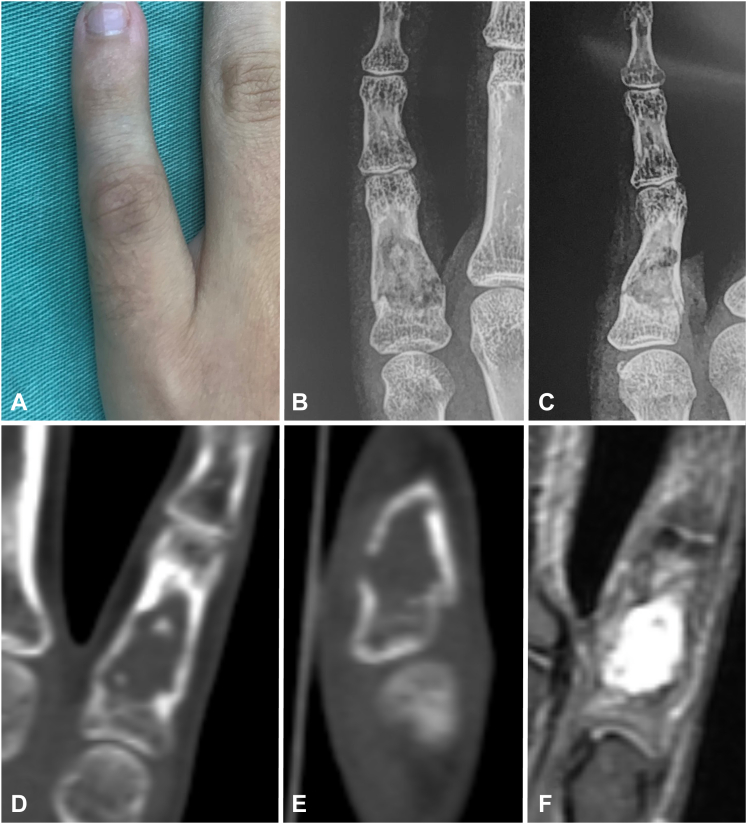
Figure 4.
A A 28-year-old female patient presented with pain and swelling of the little finger of her left hand after a low energy trauma. B, C Radiographs, D, E computed tomography images, and F magnetic resonance imaging show the characteristic appearance of a pathologic fracture at the proximal phalanx caused by enchondroma within the proximal metaphysis.
Figure 5.
Surgical treatment with dorsal extensor transtendon access, in which a window onto the dorsal cortex and subsequent curettage are made. A Image intensification control shows good screw positioning before guidewire removal and B, C, D extensor mechanism repair after E complete removal of the lesion. F, G Final imaging control demonstrates adequate reduction and screw positioning.
Case 3
A 35-year-old male patient presented after a metal object fell on the middle finger of his left hand. The patient reported local pain and swelling for 3 years. Radiographs, computed tomography scans, and magnetic resonance imaging confirmed the presence of a pathologic fracture from an enchondroma of the base of the proximal phalanx (Fig. 6). Fracture fixation was performed with a 2.0-mm HIS along with bone graft harvested from the iliac crest (Fig. 7). After 7 weeks, complete bone healing was evident with good cosmetic appearance of the scar and satisfactory digital motion (Fig. 8).
Figure 6.
A, B radiographic, C magnetic resonance, and D, E computed tomography images of a 35-year-old male patient who sought consultation after a metal object fell on the middle finger of his left hand.
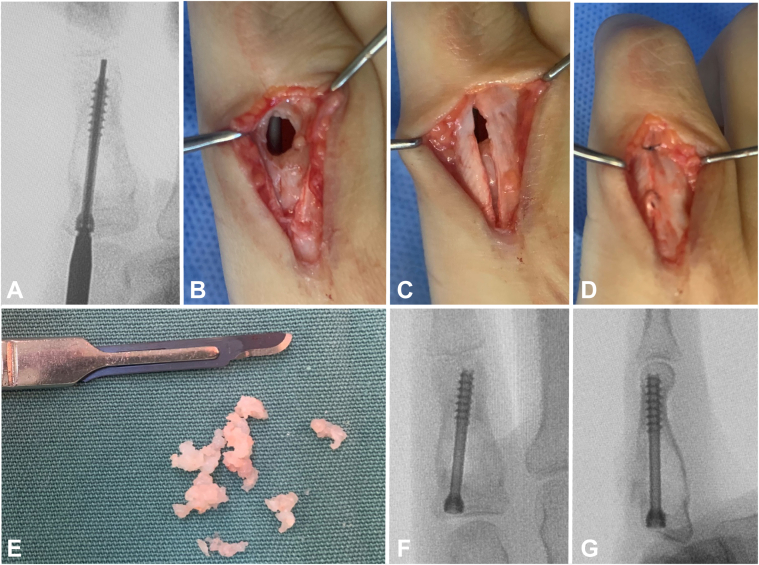
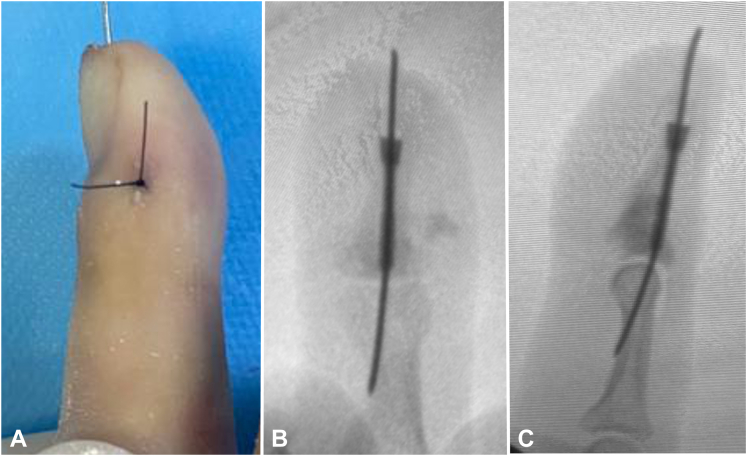
Figure 7.
A Curettage of the enchondroma through a cortical window. B, C After autologous iliac crest bone grafting, intraoperative image intensification demonstrates good defect filling and adequate fixation with a 2.0-mm intramedullary screw.
Figure 8.
A, B After 7 weeks, radiographic images show bone healing. C, D Cosmetic appearance and function are satisfactory after the surgery.
Case 4
A 48-year-old female patient presented with pain and swelling on the middle finger of her right hand after a mild trauma. Radiographs showed an enchondroma-related, pathologic fracture of the base of the distal phalanx. Surgical treatment was performed with curettage through a dorsoradial cortical window, followed by fixation with a 1.7-mm retrograde HIS and cavity filling with liquid calcium phosphate cement (Fig. 9). The patient remained immobilized for 20 days, and the fracture healed at 4 weeks after surgery.
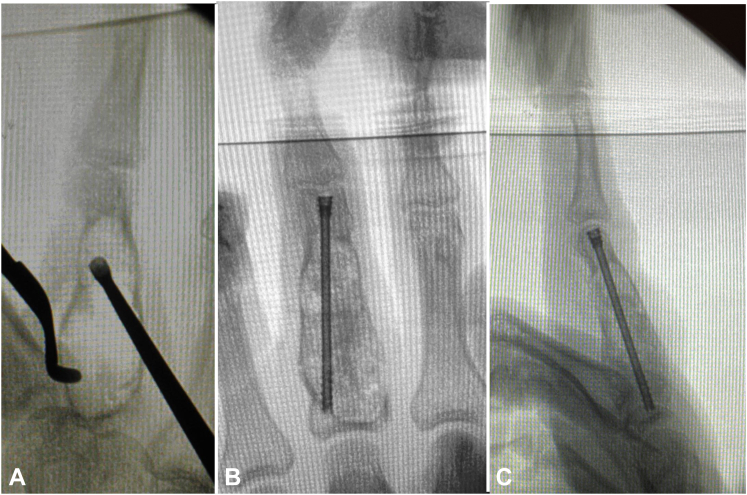
Figure 9.
A 48-year-old female patient who presented with pain and swelling on the middle finger of the right hand after a minor trauma. Radiographs show a pathologic fracture with an enchondroma of the base of the distal phalanx. A Surgical treatment included curettage through a dorsoradial cortical window, B followed by 1.7 mm retrograde HIS and C cavity filling with liquid calcium phosphate cement.
We have treated four patients with enchondroma of the long bones of the hand using HISs after tumor resection. Two cases involved proximal phalanges; one case, the metacarpal bone; and one case had the distal phalanx affected. All patients had a pathologic fracture. Patients’ data are summarized in Table 1.
Table 1.
Patient Surgical and Demographic Data.
| Patient | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Sex | M | M | M | M |
| Side | E | E | D | E |
| Affected ray | 5 | 5 | 3 | 5 |
| Affected bone | Metacarpal | Proximal phalanx | Proximal phalanx | Distal phalanx |
| Adjuvant | Cauterization | Cauterization | Cauterization | Cauterization |
| Filling | No | No | Iliac autograft | Calcium phosphate cement |
| Implant | 3.0 mm headless screw | 3.0 mm headless screw | 2.0 mm headless screw | 1.7 headless screw |
| Time to consolidation, wk | 9 | 8 | 12 | 8 |
After tumor resection and screw fixation, one patient had autologous bone grafting from the iliac crest, and another had the defect filled with calcium phosphate cement.
All patients were followed up for at least 12 months, and the mean healing time of the pathologic fracture was 5 weeks. There were neither complications related to the procedure nor the need for a second surgery.
According to Takigawa8 criteria, all four patients were graded with satisfactory appearance, having range of motion of at least 80% in comparison with the contralateral side and grip strength of at least 80% in comparison with the contralateral side. In conformity with Tordai9 criteria, all four patients were graded as group 1 (Table 2).
Table 2.
| Patient | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Tordai | Group 1 | Group 1 | Group 1 | Group 1 |
| Appearance (Takigawa) | Satisfactory | Satisfactory | Satisfactory | Satisfactory |
| Mobility (Takigawa) | >80% | >80% | >80% | >80% |
| Grip strength (Takigawa) | >80% | >80% | >80% | >80% |
Discussion
Enchondromas are benign, slow-growing tumors formed by hyaline cartilage. They occur more frequently in the third and fourth decades of life and have a predilection for the tubular bones on the ulnar side of the hand. They are most often isolated lesions but can occur as multiple lesions, as seen in Ollier disease and Maffucci syndrome.15 Most patients with hand enchondromas have no symptoms, and their diagnosis is made by an x-ray performed for another reason; therefore, it is an incidental finding in many cases. However, lesions can also create nonspecific symptoms, such as pain and localized swelling. In 40%–60% of patients, the diagnosis is made after a pathologic fracture from a minor trauma.2,3
The treatment of pathologic fractures in the long bones of the hand caused by enchondromas remains controversial with similar results from different techniques.15 Some advocate initial conservative treatment of the fracture, reserving surgery for tumor resection to be performed after bone healing.16 However, others report that patients who were operated and had the fracture treated surgically during the acute phase tended to have better outcomes. A single-stage treatment seemed to shorten the recovery time and the financial impact caused by the patient’s absence from work.17
There is no evidence for the need for autologous bone grafts, allograft, or any synthetic substance, such as methyl methacrylate or calcium phosphate, to fill the remaining cavity after tumor resection. These materials seem to offer some mechanical benefit for bone stabilization. However, such benefits can be replaced by some type of rigid osteosynthesis. In our series, even with stable bone fixation with HISs, we used a bone graft in one patient and calcium phosphate in another. As previously described, we have observed that the functional outcome and bone healing time are similar either with or without using bone grafting. Moreover, graft harvest offers the possibility of pain and complications related to the donor area, not to mention the increased time and added complexity of the procedure.18
To decrease the risk of tumor lesion recurrence, several adjuvant treatment techniques have been described. One study compared application of phenol with the use of a high-speed burr as an adjuvant to curettage and found comparable results.19 In any case, extensive evidence in the literature suggests that an adjuvant treatment is neither necessary nor advisable because tumor removal is sufficient.14
Different methods of bone fixation have been described for the treatment of pathologic hand fractures due to enchondromas, including intramedullary fixation with K-wires, plate and screws, and external fixators. Decramer and Leclerc20 used a Suzuki external fixator in one case, with satisfactory functional and radiologic results. Zheng17 described a technique of simultaneous treatment for the fracture and the tumor by fixation with plate and screws, promoting early mobility, with good results.
The use of HISs for the treatment of phalangeal and metacarpal fractures has become a routine, producing good clinical results; because it is a minimally invasive method, it creates less damage to healthy tissues and low risk of complications caused by the hardware, such as stiffness and adhesions.7 We have been using this method of fixation for the treatment of enchondromas, and we, to our knowledge, believe that this is the first reported patient series using this method.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly to this article.
References
- 1.Lubahn J.D., Bachoura A. Enchondroma of the hand: evaluation and management. J Am Acad Orthop Surg. 2016;24(9):625–633. doi: 10.5435/JAAOS-D-15-00452. [DOI] [PubMed] [Google Scholar]
- 2.Yue K.C., Lans J., Castelein R.M., et al. Benign hand tumors (part I): cartilaginous and bone tumors. Hand (N Y) 2022;17(2):346–353. doi: 10.1177/1558944720922921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaulke R., Suppelna G. Solitary enchondroma at the hand. Long-term follow-up study after operative treatment. J Hand Surg Br. 2004;29:64–66. doi: 10.1016/j.jhsb.2003.08.003. B(1) [DOI] [PubMed] [Google Scholar]
- 4.Sullivan C.W., Kazley J.M., Murtaza H., Cooley M., Jones D., Dicaprio M.R. Team approach: evaluation and management of low-grade cartilaginous lesions. JBJS Rev. 2020;8(1):e0054. doi: 10.2106/JBJS.RVW.19.00054. [DOI] [PubMed] [Google Scholar]
- 5.Lin S.Y., Huang P.J., Huang H.T., Chen C.H., Cheng Y.M., Fu Y.C. An alternative technique for the management of phalangeal enchondromas with pathologic fractures. J Hand Surg Am. 2013;38(1):104–109. doi: 10.1016/j.jhsa.2012.08.045. [DOI] [PubMed] [Google Scholar]
- 6.Bauer R.D., Lewis M.M., Posner M.A. Treatment of enchondromas of the hand with allograft bone. J Hand Surg Am. 1988;13(6):908–916. doi: 10.1016/0363-5023(88)90269-9. [DOI] [PubMed] [Google Scholar]
- 7.del Piñal F., Moraleda E., Rúas J.S., de Piero G.H., Cerezal L. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am. 2015;40(4):692–700. doi: 10.1016/j.jhsa.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 8.Takigawa K. Chondroma of the bones of the hand. A review of 110 cases. J Bone Joint Surg Am. 1971;53(8):1591–1600. [PubMed] [Google Scholar]
- 9.Tordai P., Hoglund M., Lugnegård H. Is the treatment of enchondroma in the hand by simple curettage a rewarding method? J Hand Surg Br. 1990;15(3):331–334. doi: 10.1016/0266-7681_90_90013-t. [DOI] [PubMed] [Google Scholar]
- 10.Aita M.A., Mos P.A.C., de Paula Cardoso Marques Leite G., et al. Minimally invasive surgical treatment for unstable fractures of the proximal phalanx: intramedullary screw. Rev Bras Ortop. 2016;51(1):16–23. doi: 10.1016/j.rboe.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aguilera R.J., Melibosky F., Brunelli J.P.F., et al. Headless Compression Screw for metacarpal nonunion: description of a new technique and report of 4 cases. Tech Hand Up Extrem Surg. 2022;26(4):232–239. doi: 10.1097/BTH.0000000000000390. [DOI] [PubMed] [Google Scholar]
- 12.Giesen T., Gazzola R., Poggetti A., Giovanoli P., Calcagni M. Intramedullary headless screw fixation for fractures of the proximal and middle phalanges in the digits of the hand: a review of 31 consecutive fractures. J Hand Surg Eur Vol. 2016;41(7):688–694. doi: 10.1177/1753193416641330. [DOI] [PubMed] [Google Scholar]
- 13.Ruchelsman D.E., Puri S., Feinberg-Zadek N., Leibman M.I., Belsky M.R. Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. J Hand Surg Am. 2014;39(12):2390–2395. doi: 10.1016/j.jhsa.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 14.Boulton C.L., Salzler M., Mudgal C.S. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am. 2010;35(8):1260–1263. doi: 10.1016/j.jhsa.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 15.Sassoon A.A., Fitz-Gibbon P.D., Harmsen W.S., Moran S.L. Enchondromas of the hand: factors affecting recurrence, healing, motion, and malignant transformation. J Hand Surg Am. 2012;37(6):1229–1234. doi: 10.1016/j.jhsa.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Wessel LE, Christ AB, Athanasian EA. Impact of patient and tumor characteristics on range of motion and recurrence following treatment of enchondromas of the hand. J Hand Surg Am. Published online January 31, 2022. https://doi.org/10.1016/j.jhsa.2021.11.027 [DOI] [PMC free article] [PubMed]
- 17.Zheng H., Liu J., Dai X., Schilling A.F. Modified technique for one-stage treatment of proximal phalangeal enchondromas with pathologic fractures. J Hand Surg Am. 2014;39(9):1757–1760. doi: 10.1016/j.jhsa.2014.06.131. [DOI] [PubMed] [Google Scholar]
- 18.Sekiya I., Matsui N., Otsuka T., Kobayashi M., Tsuchiya D. The treatment of enchondromas in the hand by endoscopic curettage without bone grafting. J Hand Surg Br. 1997;22(2):230–234. doi: 10.1016/s0266-7681(97)80070-8. [DOI] [PubMed] [Google Scholar]
- 19.Cha S.M., Shin H.D., Kim K.C., Park I.Y. Extensive curettage using a high-speed burr versus dehydrated alcohol instillation for the treatment of enchondroma of the hand. J Hand Surg Eur Vol. 2015;40(4):384–391. doi: 10.1177/1753193413517204. [DOI] [PubMed] [Google Scholar]
- 20.Decramer A., Leclercq C. Treatment of a fractured juxta-articular enchondroma of the middle phalanx with a suzuki external fixator: a case report. 2015;19(1):46–49. doi: 10.1097/BTH.0000000000000074. [DOI] [PubMed] [Google Scholar]