Abstract
Background/Objective
After years of war, political instability and natural catastrophes high rates of PTSD and depression have been found in the Afghan population. On this background, it was investigated whether religious beliefs (trust in higher guidance; TIHG) moderated the association between PTSD symptoms and/or depression and suicidal ideation.
Method
A total of 279 Afghan university students (61.6% women; aged 18 to 30 years) took part in this cross-sectional study between July and November 2022. Self-report measures of PTSD, depression, suicidal ideation, trust in higher guidance were used.
Results
Severe PTSD symptoms were reported by 58.4%, clinically relevant depression symptoms were reported by 55.2% and current suicidal ideation was reported by 44.4% of the sample. TIHG moderated the impact of PTSD symptoms, on suicidal ideation. TIHG and depression were unrelated.
Conclusion
PTSD symptoms, depression and suicidal ideation show an alarmingly high prevalence in this specific sample of Afghan students. TIHG seems to be a resilience factor of special importance.
Keywords: Afghanistan, Depression, PTSD, Suicidal ideation, Religious beliefs
Introduction
After 20 years of war with the US and its allies, the Taliban regained control of Afghanistan in August 2021. The Taliban took over at a time when the economic and humanitarian situation in Afghanistan was already shattered by four decades of war, years of substantial drought and the COVID-19 pandemic (www.cfr.org; www.wfp.org). The collapse of the country's economy has led to deepening poverty, food insecurity, malnutrition and displacement. Afghanistan is one of the world's poorest countries (UNDP, 2022) and according to the UNHCR there are 24 million Afghans in need of vital humanitarian relief: In consequence, Afghans constitute one of the largest refugee populations worldwide (www.unhcr.org).
In a nationwide survey (N = 4474) conducted between April and October 2017 (Kovess-Masfety et al., 2021), 64.67% of the Afghan population reported to have personally experienced at least one traumatic event; about 5% of the population suffered from probable posttraumatic stress disorder (PTSD) and about 12% from probable Major Depression. Furthermore, 2.2% reported suicidal ideation in the past 12 month and 3.4% reported a lifetime suicide attempt (Sabawoon et al., 2022). An even greater mental load was reported by Cardozo et al. (2004) based on a national multistage, cluster, population- based mental health survey conducted in 2002: Using established cut-off scores, 67.7% of the participants suffered from significant depression and 42.1% from posttraumatic stress (see also Kurt et al., 2022; Neyazi et al., 2023a; Panter-Brick et al., 2009; Rahimi et al., 2023; Scholte et al., 2004). High rates of mental disorders were also reported in the immediate aftermath of the Taliban take-over: In a sample of adolescents recruited from high schools in Kabul between November and December 2021, half of participants met criteria for probable posttraumatic stress disorder (PTSD, 51.6%) and depression (48.9%; Ahmadi et al., 2022). In a sample of predominantly female university students recruited between August and November 2021, severe posttraumatic stress disorder symptoms and clinically relevant depression symptoms were reported by about 70% of the participants; furthermore, 6.6% reported a lifetime suicide attempt and 41.3% reported suicidal ideation within the past 12 month (Naghavi et al., 2022). Though prevalence rates vary considerably depending on the time of assessment and sample, all studies point to the significant burden faced by the Afghan population.
In view of these burdens, the present study focuses on the question which factors might confer resilience against suicidal ideation - as an expression of deepest despair - in Afghan students. Naghavi et al. (2022) found that neither social support nor positive mental health – two established cross-cultural resilience factors (Johnson et al., 2011; Siegmann et al., 2018; Teismann et al., 2022) – buffered the effects of PTSD and depression on suicide risk in Afghan students. Only posttraumatic growth, i.e. positive psychological changes after adverse life events, was shown to buffer the effect of depression (but not PTSD) on suicide risk. Naghavi et al. (2022) suspect that a crucial resilience factor – religion – was not taken into account in their study. In line with this reasoning, Scholte et al. (2004) found that religion was the main resource of Afghan residents when feeling sad, worried or tensed.
In general, suicide rates have been shown to be lower in Muslim countries than in comparative countries (Gearing & Alonzo, 2018; Lester, 2006). Furthermore, studies tend to support the premise that religion provides protection against suicide risk (Lawrence et al., 2016; Wu et al., 2015). In this regard, studies have shown that religious affiliation (Dervic et al., 2004) and religious service attendance (Kleiman & Liu., 2014) are negatively associated with suicide attempts and suicide. Moreover, an inverse relationship between religious commitment and suicide ideation has been reported (Stack & Lester, 1991). Finally, Teismann et al. (2017) found trust in higher guidance (TIHG), that is an individual's spiritual and/or religious reliance on a transcendent source of support, which is believed to carry the individual through hardship (Büssing, 2010; Büssing et al., 2022), to moderate the association between depressive symptoms and suicidal ideation in a non-clinical and a clinical sample of German adults. Still, it is unclear, whether religious beliefs, also buffer the effect of PTSD and depression on suicidal ideation in Afghan students.
On this background, the current study aimed to investigate the association between religious beliefs, i.e. TIHG, and suicidal ideation in Afghan students one year after the Taliban take-over. In an attempt to understand factors that differentiate those who consider suicide from those who make suicide attempt (Klonsky and May 2015), it was furthermore investigated whether TIHG differentiates participants suffering from concurrent suicide that have or have not attempted suicide in their lifetime (cf., Teismann et al., 2019). Finally, it was studied whether TIHG moderates the associations between depression as well as PTSD and suicidal ideation.
Materials and methods
Participants and procedure
The sample consists of 279 university students (61.6.% women; age: 18–21 years: 43%; 22–24: 36.6%; 25–27: 6.5%; 28–30: 14%) affiliated with Herat University, Eshragh University, Jami University and Ghaleb University in Afghanistan. Participants were recruited via personal invitations or invitations forwarded via social media between July and November 2022. The study invitation indicated that the survey would address traumatic experiences. The Ethics Committee of the Faculty of Psychology, Ruhr-Universität Bochum approved the implementation of the present study (790/2022). All participants were properly instructed and provided their informed consent to participate online. In case of severe current stress, participants were advised to visit the universitarian counselling center.
Measures
PTSD checklist
(PCL-5; Blevins et al., 2015; Farsi version: Sadeghi et al., 2016). The PCL-5 assessed symptoms of PTSD (e.g., intrusion, avoidance, cognitive and mood alteration, arousal) with 20 items (e.g., “In the past month, how much were you been bothered by: Having strong negative feelings such as fear, horror, anger, guilt, or shame?”) that are rated on a 5-point Likert-type scale (0=not at all, 4=extremely). The higher the sum score, the higher the sypmtoms of PTSD. A score ≥ 33 is indicative of probable PTSD. Internal consistency was α=0.905 in the current sample.
Patient health questionnaire
(PHQ-9; Kroenke et al., 2001; Farsi version: Ardestani et al., 2019). The Patient Health Questionnaire (PHQ-9) assesses symptoms of depression (e.g., lack of interest, feeling down, poor appetite) with nine items (e.g., “Over the last two weeks, how often have you been bothered by any of the following problems: Little interest or pleasure in doing things?”) that are rated on a 4-point Likert-type scale (0=not at all, 3=nearly every day). With a cut-off score of 10, the scale can detect major depression with sensitivity and specificity of 88%, respectively (Manea et al., 2012). Internal consistency was α=0.880 in the current sample. The suicide item (Item 9) was excluded from the PHQ-sum score in all regression analyses to avoid overlapping and thus part-whole correlations with the Suicide Ideation and Behavior Scale (Teismann et al., 2021). The PHQ-8 (leaving out Item 9) has been shown to have excellent validity and reliability and has been recommended for screening purposes (Wells et al., 2013).
Suicide ideation and behavior scale
(SIBS; Teismann et al., 2021). The SIBS comprises six items assessing (passive/active) suicidal ideation, suicidal intent, suicidal impulses and suicide planning within the last 4 weeks. Items are rated on a 6-point Likert-type scale (0= never, 5=many times a day). Three further items assess the occurrence of a suicide attempt within the last four weeks as well as occurrence/frequency of lifetime suicide attempts. The questionnaire was translated to Farsi according to common guidelines regarding the cross-cultural validation of questionnaires (Wild et al., 2005). Excellent internal consistency has been demonstrated in German samples: α=0.873. Internal consistency was α=0.875 in the current sample.
Spirituality and religiousness in dealing with illness – trust in higher guidance subscale
(SpREUK-TIHG; Büssing, 2010). The SpREUK-TIHG is a 5-item self-report scale designed to measure a patient's religious and/or spiritual conviction to be connected with a transcendent source (“Whatever happens, I will trust in a higher power which carries me through”; “I have faith in the spiritual guidance in my life”; “In my mind I am connected with a “higher source”). Scores on each item range from 0 to 4, with higher scores indicating greater trust in higher guidance. The questionnaire was translated to Farsi according to common guidelines regarding the cross-cultural validation of questionnaires (Wild et al., 2005). Good convergent validity as well as internal consistency (Cronbach's α = 0.91) have been demonstrated in a sample of German patients (Büssing, 2010). Internal consistency was α=0.724 in the current sample.
Statistical analyses
Statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS 28) and the macro Process version 4.0 (www.processmacro.org/index.html; Hayes, 2021). After descriptive analyses, we assessed the association between the main investigated variables by the calculation of zero-order bivariate correlation analyses. To assess gender-related differences of the investigated variables, a multiple analysis of variance (MANOVA) was calculated. Since the Box's test was non-significant, Pillai's trace served as multivariate test. A t-test for independent samples was used to investigate differences between current suicide ideators with vs. without lifetime suicide attempts regarding TIHG. Next, two moderation analyses (Process: model 1) were run to investigate whether TIHG buffers the effect of symptoms of PTSD or symptoms of depression on suicidal ideation. Both analyses included TIHG as moderator and suicidal ideation as outcome, controlling for gender as covariate because of the rather female composition of the sample. In the first analysis, symptoms of PTSD served as predictor and symptoms of depression were included as a further covariate. In the second analysis, symptoms of depression served as predictor and symptoms of PTSD were included as a further covariate. The moderation effect was assessed by the bootstrapping procedure (10.000 samples) that provides percentile bootstrap confidence intervals (CI 95%). The results were Bonferroni corrected. A priori conducted power analyses (G*Power program, version 3.1) revealed that the sample size was sufficient for valid results (power>0.80, α=0.05, effect size f2=0.15).
Results
Table 1 presents the descriptive statistics of the investigated variables and their correlations. The proportion of those who are above the cut-off values for clinically relevant symptoms is high: Severe posttraumatic stress disorders symptoms (PCL ≥ 33) were reported by 58.4% of the sample, clinically relevant depression symptoms (PHQ-9 ≥ 10) were reported by 55.2% of the sample. A lifetime suicide attempt was reported by 12.9% (Range: 1 to 6 attempts), 44.4% reported suicidal ideation within the past 4 weeks (SSEV > 1).
Table 1.
Descriptive statistics and correlations of the investigated variables.
| M (SD) | Min–Max | (2) | (3) | (4) | |
|---|---|---|---|---|---|
| (1) PCL | 36.60 (15.83) | 2–80 | .732⁎⁎ | .390⁎⁎ | .000 |
| (2) PHQ-9 | 10.58 (6.46) | 0–24 | .404⁎⁎ | −0.082 | |
| (3) SIBS | 2.83 (5.06) | 0–30 | −0.170⁎⁎ | ||
| (4) TIHG | 13.75 (4.25) | 0–20 |
Notes. PCL=PTSD-Checklist; PHQ-9=Patient Health Questionnaire; SIBS= Suicidal Ideation and Behavior Scale; TIHG = Trust in Higher Guidance; M=Mean, SD=Standard Deviation, Min=Minimum, Max=Maximum.
p<001.
Association between study variables
Symptoms of PTSD, symptoms of depression and suicidal ideation were significantly positively correlated (see Table 1). TIHG was inversely correlated with suicidal ideation.
A MANOVA was used to investigate gender-specific differences: Pillai's trace was significant, V = 0.048, F (5273) = 2.775, p = .018, ηp2 = 0.048, demonstrating significant differences between both groups. Results revealed that there were no gender-specific differences regarding suicidal ideation, F(1, 277) = 0.158, p = .692, lifetime suicide attempts, F(1, 277) = 2.804, p =. 095, and TIHG, F(1, 277) = 3.091, p = .080. Yet, women showed heightened levels of posttraumatic stress disorder symptoms, F(1, 277) = 5.324, p = 0.022, and depression, F(1, 277) = 7.243, p = .008, compared to men.
Furthermore current suicide ideators without lifetime suicide attempts (n = 91; TIHG: M = 14.098, SD= 3.893) reported more TIHG than current ideators with lifetime suicide attempts (n = 36; TIHG: M = 11.939, SD= 4.649), t(122) = 2.589, p = .011.
Moderation effects of trust in higher guidance
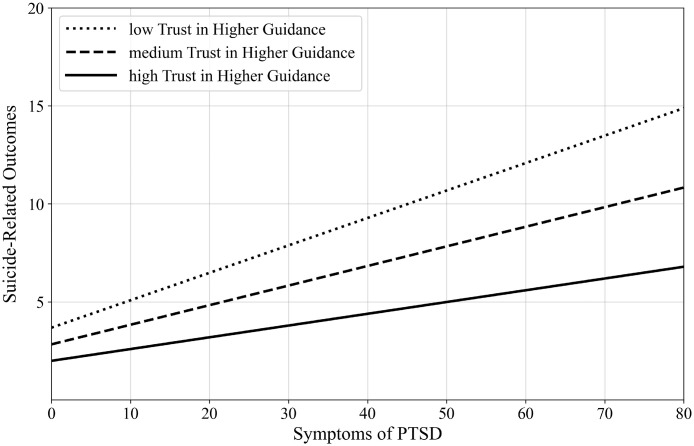
The first moderation model that included symptoms of PTSD as predictor was noted to be statistically significant, R2=0.205, F(5273)=14.101, p<.001. As shown in Table 2, the significant interaction between symptoms of PTSD and TIHG revealed that the association between symptoms of PTSD and suicidal ideation was moderated by TIHG. The simple slopes tests showed that the positive link between symptoms of PTSD and suicidal ideation was significant for low and medium level of TIHG. The link was stronger for low than for medium level of TIHG. However, the association between symptoms of PTSD and suicidal ideation was not significant for high level of TIHG. Thus, the higher the TIHG level, the less close the relationship between symptoms of PTSD and suicidal ideation (see Table 2). Fig. 1 visualizes the moderation effect.
Table 2.
Moderation analyses (outcome: suicidal ideation).
| ß | SE | t | p | 95% CI | |
|---|---|---|---|---|---|
| Moderation Model 1 | |||||
| PCL | .100 | .025 | 3.975 | < 0.001 | [.050, 0.149] |
| TIHG | −0.198 | .065 | −3.039 | .003 | [−0.327, −0.070] |
| Interaction: PCL*TIHG | −0.010 | .004 | −2.389 | .018 | [−0.018, −0.002] |
| Control variables: | |||||
| Gender | −0.207 | .573 | −0.362 | .718 | [−1.335, 0.920] |
| PHQ-8 | .099 | .068 | 1.448 | .149 | [−0.036, 0.233] |
| TIHG: | |||||
| Low (one SD below mean=−4.255) | .141 | .031 | 4.518 | < 0.001 | [.080, 0.203] |
| Medium (mean=0) | .100 | .025 | 3.975 | < 0.001 | [.050, 0.149] |
| High (one SD above mean=4.255) | .058 | .030 | 1.966 | .050 | [−0.001, 0.117] |
| Moderation Model 2 | |||||
| PHQ-8 | .110 | .069 | 1.603 | .110 | [−0.025, 0.246] |
| TIHG | −0.192 | .066 | −2.908 | .004 | [−0.322, −0.062] |
| Interaction: PHQ-8*TIHG | −0.007 | .010 | −0.624 | .533 | [−0.027, 0.014] |
| Control variables: | |||||
| Gender | −0.208 | .579 | −0.359 | .720 | [−1.347, 0.931] |
| PCL | .096 | .025 | 3.787 | < 0.001 | [.046, 0.146] |
Notes. PCL=PTSD-Checklist; PHQ-8=Patient Health Questionnaire; TIHG = Trust in Higher Guidance; ß = standardized coefficient beta; SE = Standard Error; t=t-test; p = significance; CI = Confidence Interval.
Fig. 1.
Moderation effect of trust in higher guidance (TIHG; moderator) on symptoms of PTSD (predictor) to suicide-related outcomes (outcome). (N=279 Afghan students)
Notes. PTSD=Post-Traumatic Stress Disorder.
The second moderation model that included symptoms of depression as moderator was statistically significant, R2=0.190, F(5273)=12.790, p<.001. However, the interaction between symptoms of depression and TIHG was not significant (see Table 2). Thus, the relationship between symptoms of depression and suicidal ideation was not moderated by TIHG.
Discussion
This study shows a high prevalence of probable depression (55%) and PTSD (58%) in a sample of Afghan students. Prevalence rates were somewhat lower than in a comparable study conducted right after the Taliban take-over in August 2021 (Naghavi et al., 2022). Yet, they are comparable to those of other studies conducted in Afghanistan (Ahmadi et al., 2022; Panter-Brick et al., 2009; Scholte et al., 2004) and show the extreme mental strain under which the Afghan population suffers. Suicidal ideation within the last 4 weeks was experienced by 44% of participants and lifetime suicide attempts were reported by about 13%. The rate of lifetime suicide attempts was comparable to that found by Naghavi et al. (2022) but nearly four times higher than in a nationwide Afghan study conducted in 2017 (3.4%; Sabawoon et al., 2022). Differences in sample composition and in the assessment of suicidal ideation/behavior might underlie these differing prevalence rates. However, it might also be that suicide attempts have become more frequent due to the political shift in 2021 and/or due to the COVID pandemic (cf. Brailovskaia et al., 2021, Cheung et al., 2021). Regardless of possible causes, it is an alarmingly high rate of people suffering from suicidal thoughts and/or suicide attempts.
In line with previous studies, PTSD symptoms were positively associated with suicidal ideation (Kovess-Masfety et al., 2021; Panagioti et al., 2012; Naghavi et al., 2022), whereas TIHG was inversely associated with suicidal ideation (Teismann et al., 2017). Furthermore, trust in higher guidance differentiated between current suicide ideators with or without lifetime suicide attempts. This is a relevant finding, as only few variables have been shown to differentiate between ideators and attempters (May & Klonsky, 2016). One might speculate that TIHG protects suicide ideators from a transition to suicidal behavior - a possibility that should be investigated in further studies using larger samples. Finally, TIHG moderated the association between PTSD symptoms and suicidal ideation: Those participants who reported high levels of TIHG were less likely to experience suicidal ideation even at higher levels of PTSD symptoms. These results complement previous findings, showing that religious commitment is negatively associated with suicide risk (Dervic et al., 2004; Lawrence et al., 2016), that TIHG buffers the impact of a risk factor on suicidal ideation (Teismann et al., 2017) and that religion is an especially relevant resource for Afghan residents (Schotte et al., 2004). The importance of TIHG is further underscored by the fact that in the study by Nagahvi et al. (2022), none of the protective factors examined (i.e. social support, posttraumatic growth, positive mental health) buffered the impact of PTSD symptoms on suicidal ideation/behavior. Of note, TIHG did not buffer the effect of depression on suicidal ideation. In fact, no significant relationship was shown between depression and trust in higher guidance in the current study.
The current findings point to the urgent necessity to keep mental health treatment services available in Afghanistan (Saleem et al., 2021). Shoib et al. (2022a) propose to “provide psychological first aid through a toll-free hotline, training non-medical professionals to deliver simple, cost-effective psychological interventions, providing online counselling through data-free connections, and telepsychiatry services for first-contact health workers to obtain expert opinion” (p. 1046). Online services offered from abroad have proven to be effective during the armed conflict in Iraq (Knaevelsrud et al., 2015). Furthermore, synchronous teletherapy has been shown to be as effective as in-person therapy (Batastini et al., 2021; Lin et al., 2022; see also Cuijpers et al., 2022; Khoja et al., 2016). Therefore, psychological aid provided by counsellors in Iran, Pakistan and Tajikistan, who speak Afghan languages and dialects might be a viable option. In addition positive experiences have been made with training lay person in conducting trauma-focused therapy (Ertl et al., 2011), interpersonal group therapy for depression (Bolten et al., 2003) or problem-solving therapy (Chibanda et al., 2016). Finally, a combination of regular contacts and safety planning was shown to be effective in reducing suicidal behaviour in Sri Lankan refugees residing in camps in India (Vijayakumar et al., 2017). In all these contexts it might be advisable to assess TIHG in addition to risk factors, when screening individuals for suicide risk.
There are several limitations to the present study. First, this study was based on self-report of mental health problems. Since there is evidence that self-report measurements might yield overestimated prevalence rates (Charlson et al., 2019), the prevalence data given here should be evaluated critically. At the same time, a prevalence estimate based on cut-off values rather than on clinical interviews is common in studies in crisis areas (cf. Ahmadi et al., 2022; Kovess-Masfety et al., 2021; Rahimi et al., 2023). Second, a generalization of the results to age or social groups other than university students is not possible, as the study focused only on this highly educated group. It should be emphasized, however, that it is this group of young, well-educated people whose way of life is – among others - substantially threatened by the Taliban's seizure of power (Shoib et al., 2022b). In fact, the Taliban banned women from continuing to study at universities in December 2022 (Neyazi et al., 2023b) which, at a societal level, leads to a further exacerbation of poverty and a further reduction in the accessibility and quality of health-care services (Essar et al., 2023); it can be speculated that the significantly increased risk of suicide among Afghan women is related to this (Tharwani et al., 2022). Third, only a single facet of religious/spiritual experience, that is TIHG, was investigated in the present study. TIHG seems to be a cross-cultural resilience factor against suicidal ideation/behavior (Teismann et al., 2017). Nonetheless future studies should strive to conduct a more comprehensive assessment of religious beliefs and practices (cf. Lawrence et al., 2016). Finally, given the cross-sectional nature of the data, conclusions about causality inevitably involve a degree of speculation.
Conclusion
To conclude, the present study demonstrated a high prevalence of PTSD symptoms, depression, suicidal ideation and suicide attempts in Afghan students in the year after the Taliban take-over. In dealing with PTSD symptoms, TIHG seems to be an important resilience factor within young Afghans.
Declarations
Financial disclosure
None.
Availability of data and material
The datasets are available from the corresponding author on reasonable request.
Code availability
The codes are available from the corresponding author on reasonable request.
Ethic approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Contribution
All authors contributed to the conception and design of the study as well as the interpretation of the data. MEA and MSA conducted the acquisition of data, JB and TT conducted the data analysis. AM, AN and TT drafted a first version of the article and finalized the revised version All authors listed have approved the publication of the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
References
- Ahmadi S.J., Jobson L., Earnest A., McAvoy D., Musavi Z., Samim N., et al. Prevalence of poor mental health among adolescents in Kabul, Afghanistan, as of November 2021. JAMA Network Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.18981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardestani M.S., Ashtiani R.D., Rezaei Z., Vasegh S., Gudarzi S.S. Validation of Persian version of PHQ-9 for diagnosis of major depressive episode in psychiatric wards in IRAN. Journal of Applied Behavior Science. 2019;5:1–8. [Google Scholar]
- Batastini A.B., Paprzycki P., Jones A.C.T., MacLean N. Are video conferenced mental and behavioral health services just as good as in-person? A meta-analysis of a fast-growing practice. Clinical Psychology Review. 2021;83 doi: 10.1016/j.cpr.2020.101944. [DOI] [PubMed] [Google Scholar]
- Blevins C.A., Weathers F.W., Davis M.T., Witte T.K., Domino J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015;28:489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bolton P., Bass J., Neugebauer R., Verdeli H., Clougherty K.F., Wickramaratne P., et al. Group interpersonal psychotherapy for depression in rural Uganda: A randomized controlled trial. JAMA. 2003;289:3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Brailovskaia J., Teismann T., Friedrich S., Schneider S., Margraf J. Suicide ideation during the COVID-19 outbreak in German university students: Comparison with pre-COVID 19 rates. Journal of Affective Disorders Report. 2021;6 doi: 10.1016/j.jadr.2021.100228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Büssing A. Spirituality as a resource to rely on in chronic illness: The SpREUK questionnaire. Religions. 2010;1:9–17. [Google Scholar]
- Büssing A., Baumann K., Surzykiewicz J. Loss of faith and decrease in trust in a higher source during COVID-19 in Germany. Journal of Religion and Health. 2022;61:741–766. doi: 10.1007/s10943-021-01493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardozo B.L., Bilukha O.O., Crawford C.A., Shaikh I., Wolfe M.I., Gerber M.L., et al. Mental health, social functioning, and disability in postwar Afghanistan. JAMA. 2004;292:575–584. doi: 10.1001/jama.292.5.575. [DOI] [PubMed] [Google Scholar]
- Charlson F., van Ommeren M., Flaxman A., Cornett J., Whiteford H., Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet. 2019;394:240–248. doi: 10.1016/S0140-6736(19)30934-1. (London, England) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung T., Lam S.C., Lee P.H., Xiang Y.T., Yip P.S.F., International Research Collaboration on COVID-19 Global imperative of suicidal ideation in 10 countries amid the COVID-19 pandemic. Frontiers Psychiatry. 2021;11 doi: 10.3389/fpsyt.2020.588781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibanda D., Weiss H.A., Verhey R., Simms V., Munjoma R., Rusakaniko S., et al. Effect of a primary care–based psychological intervention on symptoms of common mental disorders in Zimbabwe: A randomized clinical trial. JAMA. 2016;316:2618–2626. doi: 10.1001/jama.2016.19102. [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Heim E., Abi Ramia J., Burchert S., Carswell K., Cornelisz I., et al. Effects of a WHO-guided digital health intervention for depression in Syrian refugees in Lebanon: A randomized controlled trial. PLOS Medicine. 2022;19(6) doi: 10.1371/journal.pmed.1004025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dervic K., Oquendo M.A., Grunebaum M.F., Ellis S., Burke A.K., Mann J.J. Religious affiliation and suicide attempt. American Journal of Psychiatry. 2004;161:2302–2308. doi: 10.1176/appi.ajp.161.12.2303. [DOI] [PubMed] [Google Scholar]
- Ertl V., Pfeiffer A., Schauer E., Elbert T., Neuner F. Community-implemented trauma therapy for former child soldiers in Northern Uganda: A randomized controlled trial. JAMA. 2011;306:503–512. doi: 10.1001/jama.2011.1060. [DOI] [PubMed] [Google Scholar]
- Essar M.Y., Raufi N., Head M.G., Nemat A., Bahez A., Blanchet K., et al. Afghan women are essential to humanitarian NGO work. The Lancet Global Health. 2023;11:e497–e498. doi: 10.1016/S2214-109X(23)00048-7. [DOI] [PubMed] [Google Scholar]
- Gearing R.E., Alonzo D. Religion and suicide: New findings. Journal of Religion and Health. 2018;57:2478–2499. doi: 10.1007/s10943-018-0629-8. [DOI] [PubMed] [Google Scholar]
- Hayes A. Guilford Press; New York: 2021. Introduction to mediation, moderation, and conditional process analysis. [DOI] [PubMed] [Google Scholar]
- Johnson J., Wood A.M., Gooding P., Taylor P.J., Tarrier N. Resilience to suicidality: The buffering hypothesis. Clinical Psychology Review. 2011;31:563–591. doi: 10.1016/j.cpr.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Khoja S., Scott R., Husyin N., Durrani H., Arif M., Faqiri F., et al. Impact of simple conventional and telehealth solutions on improving mental health in Afghanistan. Journal of Telemedicine and Telecare. 2016;22:495–498. doi: 10.1177/1357633X16674631. [DOI] [PubMed] [Google Scholar]
- Kleiman E.M., Liu R.T. Prospective prediction of suicide in a nationally representative sample: Religious service attendance as a protective factor. British Journal of Psychiatry. 2014;204:262–266. doi: 10.1192/bjp.bp.113.128900. [DOI] [PubMed] [Google Scholar]
- Knaevelsrud C., Brand J., Lange A., Ruwaard J., Wagner B. Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: Randomized controlled trial. Journal of Medical Internet Research. 2015;17:E71. doi: 10.2196/jmir.3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovess-Masfety V., Keyes K., Karam E., Sabawoon A., Sarwari B.A. A national survey on depressive and anxiety disorders in Afghanistan: A highly traumatized population. BMC Psychiatry. 2021;21:314. doi: 10.1186/s12888-021-03273-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9. Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurt G., Ventevogel P., Ekhtiari M., Ilkkursun Z., Erşahin M., Akbiyik N., et al. Estimated prevalence rates and risk factors for common mental health problems among Syrian and Afghan refugees in Türkiye. BJPsych open. 2022;8:E167. doi: 10.1192/bjo.2022.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence R.E., Oquendo M.A., Stanley B. Religion and suicide risk: A systematic review. Archives of Suicide Research. 2016;20:121. doi: 10.1080/13811118.2015.1004494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester D. Suicide and islam. Archives of Suicide Research. 2006;10:77–97. doi: 10.1080/13811110500318489. [DOI] [PubMed] [Google Scholar]
- Lin T., Heckman T.G., Anderson T. The efficacy of synchronous teletherapy versus in-person therapy: A meta-analysis of randomized clinical trials. Clinical Psychology Science & Practice. 2022;29:167–178. doi: 10.1037/cps0000056. [DOI] [Google Scholar]
- Manea L., Gilbody S., McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): A meta-analysis. CMAJ Canadian Medical Association journal. 2012;184:191–196. doi: 10.1503/cmaj.110829. = journal de l'Association Medicale Canadienne. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May A.M., Klonsky E.D. What distinguishes suicide attempter from suicide ideators? A meta-analysis of potential factors. Clinical Psychology Science & Practice. 2016;23:5–20. doi: 10.1111/cpsp.12136. [DOI] [Google Scholar]
- Naghavi A., Afsharzada M.S., Brailovskaia J., Teismann T. Mental health and suicidality in Afghan students after the Taliban takeover in 2021. Journal of Affective Disorders. 2022;307:178–183. doi: 10.1016/j.jad.2022.04.001. [DOI] [PubMed] [Google Scholar]
- Neyazi A., Haidarzada A.S., Rangelova V., Erfan A., Bashiri B., Neyazi M., et al. Prevalence and predictors of depression among women in Afghanistan: A cross-sectional study. Discover Psychology. 2023;3:7. doi: 10.1007/s44202-023-00068-4. [DOI] [Google Scholar]
- Neyazi A., Padhi B., Sah R., members of the Global Centre for Public Health Collaborators Girls' education and the future of healthcare in Afghanistan. BMJ. 2023;380:561. doi: 10.1136/bmj.p561. (Clinical research ed.) [DOI] [PubMed] [Google Scholar]
- Panagioti M., Gooding P.A., Tarrier N. A meta-analysis of the association between posttraumatic stress disorder and suicidality: The role of comorbid depression. Comprehensive Psychiatry. 2012;53:915–930. doi: 10.1016/j.comppsych.2012.02.009. [DOI] [PubMed] [Google Scholar]
- Panter-Brick C., Eggerman M., Gonzalez V., Safdar S. Violence, suffering, and mental health in Afghanistan: A school-based survey. Lancet. 2009;374:807–816. doi: 10.1016/S0140-6736(09)61080-1. (London, England) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahimi M.P., Wafa M.H., Stanikzai M.H., Rahimi B.A. Post-traumatic stress disorder (PTSD) probability among parents who live in Kandahar, Afghanistan and lost at least a child to armed conflict. Scientific Reports. 2023;13:3994. doi: 10.1038/s41598-023-31228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabawoon A., Keyes K.M., Karam E., Kovess-Masfety V. Associations between traumatic event experiences, psychiatric disorders, and suicidal behavior in the general population of Afghanistan: Findings from Afghan national mental health survey. Injury Epidemiology. 2022;9:31. doi: 10.1186/s40621-022-00403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeghi M., Taghva A., Goudarzi N., Rah Nejat A. Validity and reliability of Persian version of “post-traumatic stress disorder scale” in war veterans. Iranian Journal of War & Public Health. 2016;8:243–249. http://ijwph.ir/article-1-596-en.html [Google Scholar]
- Saleem S.M., Shoib S., Dazhamyar A.R., Chandradasa M. Afghanistan: Decades of collective trauma, ongoing humanitarian crises, Taliban rulers, and mental health of the displaced population. Asian Journal of Psychiatry. 2021;65 doi: 10.1016/j.ajp.2021.102854. [DOI] [PubMed] [Google Scholar]
- Scholte W.F., Olff M., Ventevogel P., de Vries G.J., Jansveld E., Cardozo B.L., et al. Mental health symptoms following war and repression in eastern Afghanistan. JAMA. 2004;292:585–593. doi: 10.1001/jama.292.5.585. [DOI] [PubMed] [Google Scholar]
- Shoib S., Essar M.Y., Saleem S.M., Legris Z., Chandradasa M. The children of Afghanistan need urgent mental health support. Lancet. 2022;399:1045–1046. doi: 10.1016/S0140-6736(22)00155-6. (London, England) [DOI] [PubMed] [Google Scholar]
- Shoib S., Saeed F., Dazhamyar A.R., Armiya'u A.Y., Badawy M.M., Shah J., et al. Women in Afghanistan: A call for action. The lancet Psychiatry. 2022;9:342–343. doi: 10.1016/S2215-0366(22)00039-6. [DOI] [PubMed] [Google Scholar]
- Siegmann P., Teismann T., Fritsch N., Forkmann T., Glaesmer H., Zhang X.C., et al. Resilience to suicide ideation: A cross-cultural test of the buffering hypothesis. Clinical Psychology and Psychotherapy. 2018;25(1):e1–e9. doi: 10.1002/cpp.2118. [DOI] [PubMed] [Google Scholar]
- Stack S., Lester D. The effect of religion on suicide ideation. Social Psychiatry & Psychiatric Epidemiology. 1991;26:168–170. doi: 10.1007/bf00795209. [DOI] [PubMed] [Google Scholar]
- Teismann T., Forkmann T., Glaesmer H., Juckel G., Cwik J.C. Skala Suizidales Erleben und Verhalten (SSEV): Faktorstruktur und psychometrische Eigenschaften. Diagnostica. 2021;67:115–125. doi: 10.1026/0012-1924/a000269. [DOI] [Google Scholar]
- Teismann T., Naghavi A., Asgari Z., Grundei L., Brailovskaia J. Posttraumatic stress disorder symptoms and suicidal ideation/behavior: The moderating effects of positive mental health and social support among Iranian and German students. Current Psychology. 2022 doi: 10.1007/s12144-022-03187-8. [DOI] [Google Scholar]
- Teismann T., Paashaus L., Siegmann P., Nyhuis P., Wolter M., Willutzki U. Suicide attempters, suicide ideators and non-ideators: Differences in protective factors. Crisis. 2019;40:294–297. doi: 10.1027/0227-5910/a000554. [DOI] [PubMed] [Google Scholar]
- Teismann T., Willutzki U., Michalak J., Siegmann P., Nyhuis P., Wolter M., et al. Religious beliefs buffer the impact of depression on suicide ideation. Psychiatry Research. 2017;257:276–278. doi: 10.1016/j.psychres.2017.07.060. [DOI] [PubMed] [Google Scholar]
- Tharwani Z.H., Essar M.Y., Farahat R.A., Shah J. The urgency of suicide prevention in Afghanistan: Challenges and recommendations. The Lancet Regional Health Southeast Asia. 2022;8 doi: 10.1016/j.lansea.2022.100082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNDP (United Nations Development Programme) & OPHI (Oxford Poverty and Human Development Initiative) (2022). Global multidimensional poverty index (MPI): Unpacking deprivation bundles to reduce multidimensional poverty. New York.
- Vijayakumar L., Mohanraj R., Kumar S., Jeyaseelan V., Sriram S., Shanmugam M. CASP - An intervention by community volunteers to reduce suicidal behaviour among refugees. The International Journal of Social Psychiatry. 2017;63:589–597. doi: 10.1177/0020764017723940. [DOI] [PubMed] [Google Scholar]
- Wells T.S., Horton J.L., LeardMann C.A., Jacobson I.G., Boyko E.J. A comparison of the PRIME-MD PHQ-9 and PHQ-8 in a large military prospective study, the Millennium Cohort Study. Journal of Affective Disorders. 2013;15:77–83. doi: 10.1016/j.jad.2012.11.052. [DOI] [PubMed] [Google Scholar]
- Wild D., Grove A., Martin M., Eremenco S., McElroy S., Verjee-Lorenz A., et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR task force for translation and cultural adaptation. Value In Health. 2005;8:94–104. doi: 10.1111/j.1524-4733.2005.04054.x. , the journal of the International Society for Pharmacoeconomics and Outcomes Research. [DOI] [PubMed] [Google Scholar]
- Wu A., Wang J.Y., Jia C.X. Religion and completed suicide: A meta-analysis. PloS One. 2015;10 doi: 10.1371/journal.pone.0131715. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets are available from the corresponding author on reasonable request.