Abstract
Allergic rhinitis (AR) is a highly prevalent respiratory condition that carries a heavy burden and can have a significant impact on patient quality of life. AR is caused by seasonal or perennial exposure to outdoor pollens and molds as well as indoor allergic triggers. In this review article, we discuss the factors associated with the development of AR throughout the year and the fact that patients with AR need continuous treatment rather than seasonal treatment. Conventionally, AR has been mainly categorized into seasonal AR and perennial AR, but these classes do not seem to be well-adapted. Climate changes, temperature changes, and high carbon dioxide (CO2) concentration affect the growth of plants and increase the length of pollen seasons and pollen allergenicity. Air pollution aggravates allergic sensitization symptoms in AR sensitized individuals. Due to increased air pollution and indefinite pollen seasons AR symptoms are present throughout the year. Patients with AR often need continuous treatment, which should be considered while making the strategy for treating allergic rhinitis sufferers. Management of AR involves avoiding the allergen, medications for symptomatic relief, anti-inflammatory therapies, and allergy immunotherapy. Although the first-generation H1-antihistamines reduce AR symptoms, they cause sedation and impair cognitive functions; thus, second-generation antihistamines (ie, levocetirizine, loratadine, bilastine, fexofenadine) are preferred. The efficacy and safety of fexofenadine for the treatment of seasonal allergic rhinitis (SAR) symptoms have been demonstrated by numerous clinical studies, irrespective of the season and underlying allergen. In this review, we discuss the allergic rhinitis classification, the role of climate change, air pollution, and factors contributing to year-round symptoms in patients with AR and the need for continuous pharmacological treatment for management.
Keywords: Allergic rhinitis, Antihistaminic, Fexofenadine, Pollens, Climatic change and allergy, Air pollution and allergy
Introduction
Allergic rhinitis (AR) is a chronic, immunoglobulin E (IgE) mediated inflammation of the nasopharynx occurring in response to inhaled environmental allergens.1,2 It is a highly prevalent respiratory condition that affects 20–30% of adults and 40% of children.3 The symptoms of AR include nasal pruritus, sneezing, rhinorrhea, and nasal obstruction.4, 5, 6 Non-nasal symptoms are also observed, which consist of ocular signs such as tearing, redness, swollen/puffy, itchy eyes, itchy palate, and itchy ears.6,7 Further, this disease carries a heavy burden, can have a significant negative impact on patient quality of life, can cause interference with sleep and poor performance at work or school, and is associated with comorbidities including asthma.6,8
Allergens causing AR could be outdoor pollens (tree, grass and weed, including ragweed), molds and indoor allergens (eg, house dust mites, animals, molds).9 AR is caused by seasonal or perennial exposure to these triggers and is influenced by various risk factors, including genetic predisposition, differences of lifestyle and environmental exposure.10,11 Climate, geography, and vegetation affect the allergenic content of the atmosphere.12 In pollen monosensitized patients, symptoms last only during the spring, while in polysensitized patients the symptoms are present for several months or throughout the year.12
Management of AR involves avoiding the allergen, medications for symptomatic relief, anti-inflammatory therapies, and allergy immunotherapy.3 Symptoms of AR can be treated with oral antihistamines.13, 14, 15 Fexofenadine is a selective histamine type 1 (H1)-receptor antagonist indicated for symptomatic relief in seasonal allergic rhinitis (SAR) and chronic idiopathic urticaria (CIU) in children and adults.13 In this review article we discuss the factors associated with the development of AR throughout the year. Further, we also discuss the fact the AR patients need a continuous treatment rather than seasonal.
Allergic rhinitis classification redefined
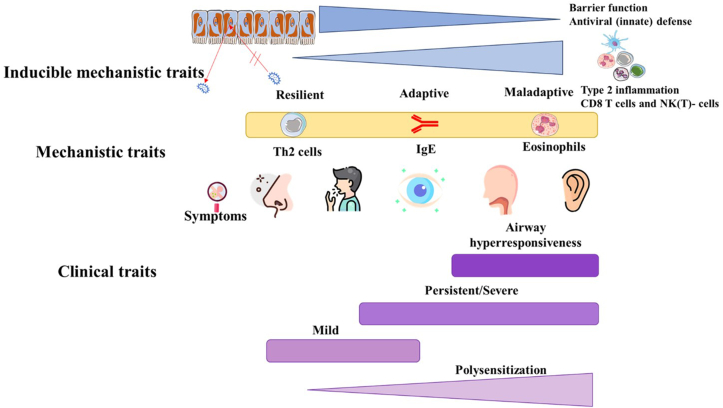
Conventionally, AR has been mainly categorized into SAR and perennial allergic rhinitis (PAR),4,16 based on the time of exposure. SAR is caused by outdoor allergens occurring during a specific season; consequently, its symptoms occur with the pollen season. PAR is caused by indoor allergens; thus, its symptoms occur throughout the year. However, this distinction does not seem to be well adapted for many reasons. In many areas, pollens and molds are perennial allergens such as grass pollen allergy in southern California and Florida in the United States or Parietaria pollen allergy in the Mediterranean area. Some patients sensitized to perennial allergens may not show symptoms throughout the year but only a few weeks per year, for example, patients allergic to house dust mites suffering only from mild or moderate/severe intermittent AR. Further, many patients are sensitized to various types of allergens and can present symptoms throughout the year. Some patients could be allergic to both pollens and molds so it becomes difficult to clearly define the pollen season while others who are sensitized to a single pollen species could have symptoms throughout the year.17 Patients with AR show a heterogeneity ranging from monosensitization to polysensitization for various allergens combined with mild-to-persistent and/or moderate rhinitis, including comorbidities characteristic for asthma, such as airway hyperresponsiveness (Fig. 1).18 Furthermore, climate change has also increased the production of various aeroallergens and changes in their geographical distribution. Changes in the flowering season due to climate changes have extended allergenic seasons with consequent increases in human exposure.19 Non-specific irritants such as air pollution may aggravate symptoms in symptomatic patients and induce symptoms in asymptomatic patients with nasal inflammation. Lastly, seasonal allergens in one region or country can be perennial in another country and vice versa. Consequently, the organization Allergic Rhinitis and its Impact on Asthma (ARIA) proposed and adopted replacing seasonality classes with intermittent and persistent rhinitis based on the frequency and severity of AR.17,20 In intermittent AR the symptoms last for less than 4 days a week or less than 4 consecutive weeks, whereas in persistent AR the symptoms last for more than 4 days a week and more than 4 consecutive weeks.20 This is really important as the burden of disease will decide the management and treatment of patients.
Fig. 1.
Heterogeneity of allergic rhinitis: Inducible mechanistic traits. Adapted from Gerth van Wijk and Smits, 202118 CD8, cluster of differentiation 8; NK, natural killer; Th2, Type 2 helper. Allergic rhinitis patients exhibit heterogeneous clinical traits, including monosenstization to polysensitization for various allergens combined with mild-to-persistent and/or moderate typical rhinitis complaints, together with comorbidities for asthma, such as airway hyperresponsiveness
Causes of allergic rhinitis
Allergic rhinitis is caused by exposure to indoor and outdoor triggers. Common allergens that can trigger AR symptoms include pollens.
Pollens
Pollen grains (2.5–10 μm), male reproductive structures of plants, are a major causal agent of respiratory allergy.21,22 These plant-derived pauci-micronic components include stem particles, trichome parts, plant debris and carry allergens which can produce allergic symptoms.22 They enter the human body via upper respiratory tract mucosa and cause allergic sensitization. D'Amato et al proposed that these allergen-bearing minute particles originate from dispersion of plant debris, such as Ubish bodies.12,23,24 The pollen count, pollen abundance, dispersal, and allergenicity are the parameters that are affected by the local climate, geography, vegetation.25 Pollens that cause allergic reactions originate mainly from grasses, weeds, and trees.
Various sensitizing predominant pollens are ragweed in North America; Gramineae in Europe; tree plants in Austria, New Zealand and Japan; Bermuda, timothy, humulus in Guangdong (southern China).26 In Japan, Japanese cedar (Cryptomeria japonica) is the major allergen causing SAR. It is dispersed over long distances and can remain airborne for more than 12 h; thus, patients experience severe symptoms during allergy season (between February and April). Pollens from Japanese cypress (Chamaecyparis obtusa) is dispersed in April and May; thus, pollen season lasts from February to May in Japan.27 In Mexico, pollens from the species Fraxinus, Cupressaceae, Alnus, and Poaceae are the most common.28 In the region covering the continental United States and southern Canada, Quercus and Cupressaceae are the most abundant allergenic pollen taxa. Sub-regional data show that tree pollen was the dominant pollen type in Washington (95.8%; abundant taxa: Cupressaceae and Alnus), California (94%; Ulmus and Olea), Ontario, Canada (81%; Morus), and Texas (Quercus, Cupressaceae).29 In Australia, grass pollens are the major allergens, and these grasses vary in different climatic zones. Subtropical Brisbane is dominated by subtropical Bahia grass (Paspalum notatum) and Bermuda grass (Cynodon dactylon) and temperate Sydney, Canberra, Melbourne, and Hobart are dominated by the temperate Ryegrass (Lolium perenne).30 The most common pollen grains in Greece are from olive, oak/beech, grasses, and cypress. Various studies have shown significant correlations between olive, grass, and Parietaria pollens and symptoms scores in AR patients.31
Tree pollens produced by birch (Betula) in north, central, and eastern Europe, olive (Olea europaea) and cypress (Cupressus) are very allergenic. In the United States and southern Canada region, for a long time, pine pollen was considered a non-allergenic pollen due mainly to the large size of the grain and its low levels of proteins. However, recent findings show that pine pollen can be considered as allergenic overall in those geographical areas where the presence of pines is high. There is a high degree of cross-reactivity among the pollen of the different pine species. Additional studies are needed to better understand the contribution of certain factors, such as diesel exhaust particles (DEPs), in the increase of the allergenic potency of pollen.32 Cross-reacting allergens present in fruits, vegetables, roots, and nuts may trigger IgE-mediated allergic reactions in Birch pollen allergic patients. Pollens usually peak 1–3 weeks after the start of the flowering season, which begins by the end of March in western Europe, beginning to middle of April in central and eastern Europe, and by late April to late May in northern Europe. The duration of this main flowering season fluctuates from 2 to 8 weeks depending upon temperature. Further various regions of Europe show shorter or longer periods, with yearly alternating low and high pollen production causing cross-reactivity and sequential pollen seasons of birch-related allergens thus extending the period of symptoms of allergy in many patients.12 In central and northern Europe, many trees such as Corylaceae trees, hazel, and alder show early pollination (December to April) followed by birch, hornbeam and hop hornbeam. Due to this allergenic cross-reactivity, hazel and alder can act as primers of allergic sensitization to Betulaceae pollen allergens and thus the symptoms become more noticeable during the birch-pollen season.12 In the Mediterranean region, Oleaceae olive (Olea europaea) pollen is an important cause of respiratory allergic disease whereas in Spain, southern Italy, Greece, and Turkey, olive pollen is an important cause of pollinosis. It is cross reactive with several trees pollinating from winter to summer in the Mediterranean area (privet (Ligustrum vulgare) and Phillyrea angustifolia a common bush) and other parts of Europe (ash tree).33 Cupressaceae can pollinate from mid-November to April. Cypress produces a large amount of anemophilous pollen and has increased pollinosis in several Mediterranean countries like Israel, France, and Spain.34, 35, 36 In the continental United States and southern Canada pollen start date. Quercus starts producing pollen in mid-February in Houston and early-May in New York, showing almost a three-month difference in start date due to latitudinal difference. Similarly, the duration of the main pollen season varies according to the region (Quercus pollinates for 23 days in Seattle and 103 days in California). This indicates that higher altitudinal regions have a later start date and a shorter pollen season.29
Grass pollens comprise of Poa pratensis, Poa annua, and Lolium perenne and show peak 1–2 months after the start of the main flowering season; in Europe grass flowering peaks in June. Due to the reduction in grasslands, there is a decrease in total grass pollen count but the frequency of allergic sensitization to grass pollen has not shown any decrease.12
A retrospective cross-sectional study involving 894 patients with SAR from Bahía Blanca, Argentina suggests a high frequency of sensitization to grass pollen extracts from the Poaceae family among these patients. A sensitization to the Pooideae (86.8%) sub-family being the most common, having highest frequency with Phalaris arundinacea (62.2%) and lower responses with Chloridoideae (Cynodon dactylon) and Panicoideae (Paspalum notatum, Sorghum halepense) subfamily allergens.37 Another study quantifying pollen grains of Poaceae family in the atmosphere of Curitiba, Brazil, compared the pollen distribution curve with data from the 1980s–1990s. The study classified the daily concentration of grass pollen according to the National Allergy Bureau (NAB) and showed a change in the grass pollen season. Historically, only 2 peaks of Poaceae pollen dispersion were being observed over the years, however, with this study, grass pollens were observed in other months of the year as well, provoking symptoms upon exposure outside the previously established grass pollen seasons.38 Subtropical grass species like Cynodon dactylon (Bermuda grass) and Paspalum notatum (Bahia grass) became prominent due to their invasiveness and ubiquity as reported by Vieira et al.39
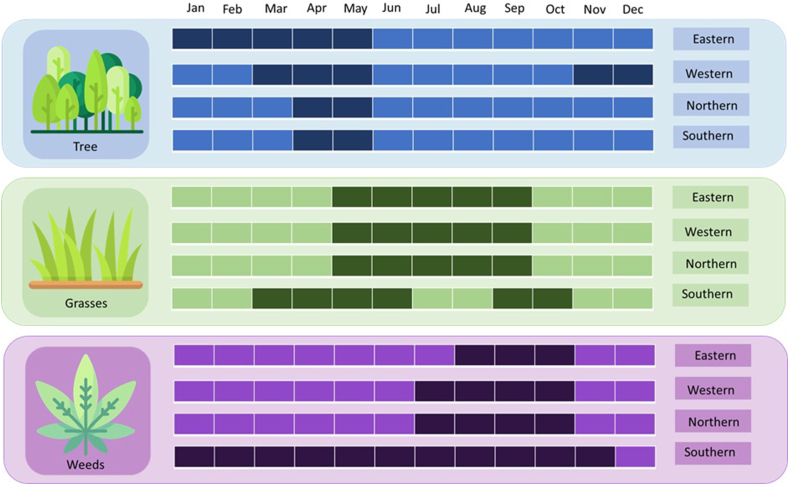
Among weed pollens, ragweed which includes both Artemisia (A.) artemisiifolia (short or common ragweed), and A. trifida (giant ragweed) cause AR. The pollen of A. artemisifolia are small (18–22 μm), so, they often travel long distance and are produced in enormous amounts from one single plant alone.12,22,40 Ragweed and mugwort have identical flowering seasonal periods and high degree of cross-reactivity.41 Parietaria pollen causes multi-seasonal symptomatology in the Mediterranean area due to its long persistence in the atmosphere.12 The Amaranthaceae (Chenopodium, Salsola, and Amaranthus), common weeds, are triggers of allergy and major sources of pollinosis in southern Europe.12 Ambrosia pollinates in late summer and early fall and it ends late at the lower altitudes. It is the most abundant weed pollen in Ontario, Canada, occurring in mid-August to mid-September.29 Overall, pollen seasons are not well precise, and pollen sensitive individuals are exposed to the different pollens round the year in the different European countries. Fig. 2 shows a pollen calendar with the most common allergenic pollen species in different European zones.
Fig. 2.
Pollen peaks in Europe. Darker boxes indicate the presence of pollen season
Climate changes and extended pollen allergy seasons
The Intergovernmental Panel on Climate Change (IPSS) reports have documented the indication of increased carbon dioxide (CO2)concentrations and other greenhouse gases leading to a higher frequency of extreme climate events.23 Earth's temperature has increased by 1.0 °C since the pre-industrial levels. Climate changes have led to higher global temperatures and heatwaves, rising sea levels, altered precipitation patterns, altered plant growth seasons, increased frequency or intensity of extreme weather events, droughts, and changes in the distribution of infectious vectors.23,24,42 Further, the increase in global temperature and high CO2 concentration has modified the duration of pollen seasons, time of pollen release, amount of pollen produced, pollen composition, and allergenicity. Various studies have shown that increased CO2 concentrations lead to increased allergenicity of ragweed pollen and higher prevalence of seasonal allergic disease.43,44 A recent meta-analysis by Ziska et al reported increased allergenic pollen levels in 71% study sites and lengthening of pollen seasons in 65% of the sites. This study further demonstrated a significant increase in pollen season duration over time, increasing by 0.9 days per year on average.45 Manangan et al investigated the localized trends in pollen concentrations and pollen phenology over time and the effect of seasonal climate variations in Atlanta, Georgia (1992–2018). The study reported that allergenic pollen concentrations for several types of pollen are increasing and trending towards an earlier pollen release in Atlanta. Warmer temperatures preceding the pollen season were associated with the earlier pollen release.46 Start date of some of the allergic pollen season was seen to be negatively correlated with total pollen duration in some regions; this indicates, in low altitudes, though the season start early, it lasts for longer than the higher altitudes (Quercus). This suggests the involvement of other factors such as temperature, rain, wind, and sun which might have contributed to the longer pollen season.29
Air pollution and interaction with pollen allergens
Air pollution is defined as an alteration in the levels of quality and purity of air owing to the natural or anthropogenic emissions of chemical and biological substances. Various factors affect the composition of indoor air including outdoor pollutants, the quality/quantity of ventilation, indoor allergens, and activities such as smoking, heating, and cooking. Air pollution increases pollen allergenicity and contributes to the onset and aggravation of chronic respiratory diseases including AR and asthma.23 Over the past decades various activities such as burning of fossil fuels, primary emissions from industries and vehicles, secondary emissions and photochemical oxidation, and the concentrations of pollutants like reactive trace gases and aerosols such as ozone, nitrogen, sulfur oxides, and soot have increased drastically and have affected air pollution.22 The amount and allergenicity of pollen grains produced by plants, and the number of allergens per pollen grain has increased by outdoor pollution. Additionally, various studies have shown that aeroallergens can become chemically modified by outdoor pollutants and aggravate allergic symptoms.47, 48, 49, 50 Some air pollutants have a direct effect on the respiratory system, and they also interact with plants and fungi to enhance the production and allergenicity of pollen, such as ragweed or cypress, and of fungal spores. For example, ragweed grew faster and produced more pollens in an urban area with high CO2 concentrations as compared to ragweed grown in rural areas.23 Environmental CO2 may also affect the amount of pollen produced; for example, Ambrosia produced more pollen (allergenic) under increased CO2 levels.29,51 Further, climate changes and global warming have increased the outdoor air pollution, pollen exposure and extreme weather conditions leading to increased risk of developing or exacerbating allergic-atopic disorders, respiratory health, and infection susceptibility.
Management of allergic rhinitis
The approaches used for the management of AR include avoiding the allergen, pharmacotherapy for symptomatic relief, and allergen immunotherapy.9 The pharmacological therapy includes H1-antihistamines (oral, intranasal), intranasal corticosteroids (INS), leukotriene receptor antagonists, and combination therapy.9 Oral antihistamines and INS are the first line treatment options. For patients with persistent or moderate to severe AR symptoms, intranasal corticosteroids such as beclomethasone, budesonide, ciclesonide, fluticasone propionate, fluticasone furoate, mometasone furoate, and triamcinolone acetonide alone or in combination with intranasal anti-H1 are therapeutic options.52 They have local anti-inflammatory effect on nasal mucosal cells.9 Leukotriene receptor antagonists used for treatment of AR includes montelukast and zafirlukast.
Histamine is the key mediator of the allergic reactions, and its clinical effects are mainly mediated via the H1-receptor.53 H1-antihistamines block the action of histamine on H1-receptors and are commonly used in the treatment of AR. Their benefits include once-a day administration, low cost, and rapid effective action.9 Although first-generation H1-antihistamine drugs, such as diphenhydramine, reduce AR symptoms effectively, their anticholinergic properties and, induced sedation limit their use.53
Second-generation oral antihistamines are preferred and include cetirizine, levocetirizine, loratadine, desloratadine, bilastine, mizolastine, rupatadine, and fexofenadine. It is beyond the scope of this article to discuss all second-generation antihistamines and thus fexofenadine is presented as representative of the effectiveness of this class of drugs for the treatment of AR. Fexofenadine shows similar effectiveness as the first-generation without any sedation effect or risk profile as it does not cross the blood brain barrier.1,53 Fexofenadine is a non-sedating H1-antihistamine, indicated for the treatment of symptoms associated with AR and CIU in adults,13 and children aged 6 months and older for CIU and 2 years and over for AR.60 Fexofenadine is currently being marketed in approximately 100 countries worldwide. The efficacy and safety of fexofenadine for the treatment of SAR symptoms has been consistently demonstrated in various clinical studies (Table 1), irrespective of season and underlying allergen.54, 55, 56, 57, 58
Table 1.
Summary of efficacy and safety of fexofenadine from various clinical studies
| Reference | Study population | Treatment arm | Efficacy data | Safety data |
|---|---|---|---|---|
| Howarth PH et al. 199949 | Seasonal AR | Fexofenadine HCl 120 mg QD; n = 211 Fexofenadine HCl 180 mg QD; n = 202 Cetirizine 10 mg QD; n = 207 Placebo; n = 201 |
|
|
| Ellis AK et al. 202151 | Seasonal AR | Fexofenadine HCl 180 mg; n = 126 Placebo; n = 125 |
|
|
| Casale TB et al. 199952 | Seasonal AR | Fexofenadine HCl 120 mg QD; n = 287 Fexofenadine 180 mg QD; n = 282 Placebo; n = 292 |
|
|
| Nathan RA et al. 199953 | Healthy volunteers | 6-month study Fexofenadine 60 mg BID; n = 217 Placebo; n = 211 12-month study Fexofenadine 240 mg QD; n = 234 Placebo; n = 235 |
NA (Safety studies) |
|
AR, allergic rhinitis; AUC2-12, area under the curve from baseline to 12h; BID, twice daily; CI, confidence interval; HCl, hydrochloride; n, number of subjects; NA,: not applicable; QD, once a day; TEAE, treatment-emergent adverse event.
A meta-analysis including 8 randomized, controlled clinical trials showed an overall beneficial effect of fexofenadine on the symptoms of SAR as measured by TSS and individual nasal symptoms scores.55 Further, various studies have reported favourable AE profile of fexofenadine, supporting the satisfactory safety profile of fexofenadine at the recommended dosages.58 Moreover, a recent study by Ellis et al demonstrated that fexofenadine improves AR pollen symptoms aggravated by air pollutants.56
Summary/discussion
Allergic rhinitis is a common respiratory allergy which carries a high burden both for the individual and the society. It impairs the daily activities, quality of sleep, and work performance significantly and could also lead to comorbidities such as asthma. Guidelines emphasize on the early detection and optimal treatment of this disorder.6,44 Traditionally, AR has been classified into SAR and PAR, but these classes do not seem to be straightforward due to various whys and wherefores. On the one hand, some patients may be sensitized to many types of allergens and exhibit symptoms throughout the year, while on the other hand some patients could be sensitized only to a single pollen and still have symptoms round the year. Further, in some areas pollens and molds are perennial allergens and if a person is allergic to both it is difficult to clearly define the pollen season. Upon travelling, allergic patients may be exposed to the sensitizing allergens in different times of the year.
Over the recent decades, higher levels of vehicular emissions, urbanization, and westernized lifestyles are associated with the increased frequency of pollen-induced respiratory allergies in urban areas as compared to that in rural areas. The increase in global temperature and CO2 concentration has caused climate changes which has further increased the duration of pollen seasons, time of pollen release, amount of pollen produced, and increased pollen allergenicity. Aerobiological and allergology studies have shown that the pollen map of Europe is changing also as a result of cultural factors (for example, importation of plants such as birch and cypress for urban parklands), greater international travel (eg, colonization by ragweed in France, northern Italy, Austria, Hungary, etc), and climate change. In this regard, the higher frequency of weather extremes, such as thunderstorms and increasing episodes of long-range transport of allergenic pollen represent new challenges for researchers. Changes in the flowering season due to climate change has extended allergenic seasons with consequent increases in human exposure. Furthermore, in the last few years, experimental data on pollen and sub-pollen-particles structure, the pathogenetic role of pollen, and the interaction between pollen and air pollutants have given new insights into the mechanisms of respiratory allergic diseases.12
Over the past decades, the concentrations of pollutants such as reactive trace gases, ozone, nitrogen, sulfur oxides, and soot have increased and have affected air pollution. These components of air pollution modify not only the morphology of the pollens but also their allergenic potential. Air pollutants also interact with airborne allergens and further augment risk of allergic sensitization and exacerbation of symptoms in sensitized individuals.42
Increased and longer pollen seasons and allergen exposure have led to a continuous antihistaminic drug use, not limited to a pollen season (eg, tree) only but also extended to others pollen seasons (grass, weed). All these reasons, combined with the AR patients’ polysensitization who present symptoms due to different pollen families (tree, grass, weed) around the year, combined to indoor allergens sensitization and symptoms aggravation provoked by air pollutants, rationalize the continuous use of antihistamine drugs like fexofenadine which has been proven effective in relieving AR symptoms and has a good long-term safety profile as demonstrated in controlled clinical trials. Continuous treatment is not needed when air pollution levels are low and in geographical locations where the pollen seasons are well-defined; however, continuous treatment is needed when pollens are present even if the level of air pollution is low.
Further, there is a need to treat AR on time, from the appearance of first symptoms, to avoid exacerbations or comorbidities and decrease the spread of viral infections, and second-generation antihistamines such as fexofenadine are preferred.53, 54, 55, 56, 57, 58
Conclusions
To conclude, AR classification does not seem to be well adapted. Climate changes, changes in temperature, and high CO2 concentration affect the growth of plants, increase the length of pollen seasons and pollen allergenicity. Air pollution exacerbates allergic sensitization symptoms in AR sensitized individuals. Due to increased air pollution and vague pollen seasons AR symptoms are present throughout the year. AR patients need continuous treatment, which should be considered in making the strategy on treating AR sufferers. Consequently, an optimal treatment should be used continuously not only during spring but throughout the year when pollens are present, even when the air pollution level is low, according to the severity and duration of symptoms.
Abbreviations
AR, allergic rhinitis; ARIA, Allergic Rhinitis and its Impact on Asthma; CIU, chronic idiopathic urticaria; CUSSC, Continental USA and Southern Canada; H1, histamine type 1; IgE, immunoglobulin E; PAR, perennial allergic rhinitis; SAR, seasonal allergic rhinitis.
Funding
This work was supported by Sanofi. The authors received editorial/writing support in the preparation of this manuscript.
Availability of data and materials
Not applicable.
Author contributions
All authors were involved in the conception of the work, critically revising the manuscript, and take full accountability for the work, for all content and editorial decisions. All authors approved the final version to be published.
Ethics approval
This manuscript is a review. It did not involve human or animal subject.
Authors’ consent for publication
The authors provide their consent for the publication of the review article.
Declaration of competing interest
GDA, DAM, and IJA do not have conflict of interest for the present work. MMA is an employee of Sanofi and may hold shares or stock options in the company.
Acknowledgement
Writing and editorial support was provided by Nany Gulati, PhD, and Sambasiva Kolati, M.S from Sanofi.
Footnotes
Full list of author information is available at the end of the article
References
- 1.Schuler Iv C.F., Montejo J.M. Allergic rhinitis in children and adolescents. Pediatr Clin North Am. Oct 2019;66(5):981–993. doi: 10.1016/j.pcl.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Dykewicz M.S., Wallace D.V., Baroody F., et al. Treatment of seasonal allergic rhinitis: an evidence-based focused 2017 guideline update. Ann Allergy Asthma Immunol. Dec 2017;119(6):489–511.e41. doi: 10.1016/j.anai.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 3.Hoyte F.C.L., Nelson H.S. Recent advances in allergic rhinitis. F1000Res. 2018;7 doi: 10.12688/f1000research.15367.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meng Y., Wang C., Zhang L. Advances and novel developments in allergic rhinitis. Allergy. Dec 2020;75(12):3069–3076. doi: 10.1111/all.14586. [DOI] [PubMed] [Google Scholar]
- 5.Canonica G.W., Mullol J., Pradalier A., Didier A. Patient perceptions of allergic rhinitis and quality of life: findings from a survey conducted in europe and the United States. World Allergy Organ J. Sep 2008;1(9):138–144. doi: 10.1097/WOX.0b013e3181865faf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scadding G.K., Durham S.R., Mirakian R., et al. BSACI guidelines for the management of allergic and non-allergic rhinitis. Clin Exp Allergy. Jan 2008;38(1):19–42. doi: 10.1111/j.1365-2222.2007.02888.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scadding G.K., Kariyawasam H.H., Scadding G., et al. BSACI guideline for the diagnosis and management of allergic and non-allergic rhinitis (Revised Edition 2017; First edition 2007) Clin Exp Allergy. Jul 2017;47(7):856–889. doi: 10.1111/cea.12953. [DOI] [PubMed] [Google Scholar]
- 8.Meltzer E.O. Allergic rhinitis: burden of illness, quality of life, comorbidities, and control. Immunol Allergy Clin North Am. May 2016;36(2):235–248. doi: 10.1016/j.iac.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Bousquet J., Anto J.M., Bachert C., et al. Allergic rhinitis. Nat Rev Dis Primers. Dec 3 2020;6(1):95. doi: 10.1038/s41572-020-00227-0. [DOI] [PubMed] [Google Scholar]
- 10.Wahn U. What drives the allergic march? Allergy. Jul 2000;55(7):591–599. doi: 10.1034/j.1398-9995.2000.00111.x. [DOI] [PubMed] [Google Scholar]
- 11.Murrison L.B., Brandt E.B., Myers J.B., Hershey G.K.K. Environmental exposures and mechanisms in allergy and asthma development. J Clin Invest. Apr 1 2019;129(4):1504–1515. doi: 10.1172/jci124612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D'Amato G., Cecchi L., Bonini S., et al. Allergenic pollen and pollen allergy in Europe. Allergy. Sep 2007;62(9):976–990. doi: 10.1111/j.1398-9995.2007.01393.x. [DOI] [PubMed] [Google Scholar]
- 13.Simpson K., Jarvis B. Fexofenadine: a review of its use in the management of seasonal allergic rhinitis and chronic idiopathic urticaria. Drugs. Feb 2000;59(2):301–321. doi: 10.2165/00003495-200059020-00020. [DOI] [PubMed] [Google Scholar]
- 14.Linton S., Burrows A.G., Hossenbaccus L., Ellis A.K. Future of allergic rhinitis management. Ann Allergy Asthma Immunol. Aug 2021;127(2):183–190. doi: 10.1016/j.anai.2021.04.029. [DOI] [PubMed] [Google Scholar]
- 15.May J.R., Dolen W.K. Management of allergic rhinitis: a review for the community pharmacist. Clin Ther. Dec 2017;39(12):2410–2419. doi: 10.1016/j.clinthera.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Brożek J.L., Bousquet J., Agache I., et al. Allergic rhinitis and its impact on asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol. Oct 2017;140(4):950–958. doi: 10.1016/j.jaci.2017.03.050. [DOI] [PubMed] [Google Scholar]
- 17.Demoly P., Allaert F.A., Lecasble M., Bousquet J. Validation of the classification of ARIA (allergic rhinitis and its impact on asthma) Allergy. Jul 2003;58(7):672–675. doi: 10.1034/j.1398-9995.2003.t01-1-00202.x. [DOI] [PubMed] [Google Scholar]
- 18.Gerth van Wijk R., Smits H.H. Heterogeneity in allergic rhinitis: explained by inducible mechanistic traits? J Allergy Clin Immunol. Aug 2021;148(2):358–360. doi: 10.1016/j.jaci.2021.06.011. [DOI] [PubMed] [Google Scholar]
- 19.D'Amato G., Chong-Neto H.J., Monge Ortega O.P., et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy. Sep 2020;75(9):2219–2228. doi: 10.1111/all.14476. [DOI] [PubMed] [Google Scholar]
- 20.Bousquet J., Van Cauwenberge P., Khaltaev N. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. Nov 2001;108(5 Suppl):S147–S334. doi: 10.1067/mai.2001.118891. [DOI] [PubMed] [Google Scholar]
- 21.Kim K.R., Han M.J., Oh J.W. Forecast for pollen allergy: a review from field observation to modeling and services in korea. Immunol Allergy Clin North Am. Feb 2021;41(1):127–141. doi: 10.1016/j.iac.2020.09.011. [DOI] [PubMed] [Google Scholar]
- 22.Singh A.B., Mathur C. Climate change and pollen allergy in India and south asia. Immunol Allergy Clin North Am. Feb 2021;41(1):33–52. doi: 10.1016/j.iac.2020.09.007. [DOI] [PubMed] [Google Scholar]
- 23.D'Amato G., Holgate S.T., Pawankar R., et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J. 2015;8(1):25. doi: 10.1186/s40413-015-0073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Da M., Cecchi L., Annesi-Maesano I., Da G. News on climate change, air pollution, and allergic triggers of asthma. J Investig Allergol Clin Immunol. 2018;28(2):91–97. doi: 10.18176/jiaci.0228. [DOI] [PubMed] [Google Scholar]
- 25.Ariano R., Canonica G.W., Passalacqua G. Possible role of climate changes in variations in pollen seasons and allergic sensitizations during 27 years. Ann Allergy Asthma Immunol. Mar 2010;104(3):215–222. doi: 10.1016/j.anai.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Wang X.Y., Ma T.T., Wang X.Y., et al. Prevalence of pollen-induced allergic rhinitis with high pollen exposure in grasslands of northern China. Allergy. Jun 2018;73(6):1232–1243. doi: 10.1111/all.13388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yamada T., Saito H., Fujieda S. Present state of Japanese cedar pollinosis: the national affliction. J Allergy Clin Immunol. Mar 2014;133(3):632–639.e5. doi: 10.1016/j.jaci.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 28.Calderón-Ezquerro M.C. First airborne pollen calendar for Mexico City and its relationship with bioclimatic factors. Aerobiologia. 2016;32(2):225–244. doi: 10.1007/s10453-015-9392-4. 0000 2016;v. v.32 no.2. [DOI] [Google Scholar]
- 29.Lo F., Bitz C.M., Battisti D.S., Hess J.J. Pollen calendars and maps of allergenic pollen in North America. Aerobiologia. 2019;35(4):613–633. doi: 10.1007/s10453-019-09601-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beggs P.J., Katelaris C.H., Medek D., et al. Differences in grass pollen allergen exposure across Australia. Aust N Z J Public Health. Feb 2015;39(1):51–55. doi: 10.1111/1753-6405.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Katotomichelakis M., Nikolaidis C., Makris M., et al. The clinical significance of the pollen calendar of the Western Thrace/northeast Greece region in allergic rhinitis. Int Forum Allergy Rhinol. Dec 2015;5(12):1156–1163. doi: 10.1002/alr.21623. [DOI] [PubMed] [Google Scholar]
- 32.Gastaminza G., Lombardero M., Bernaola G., et al. Allergenicity and cross-reactivity of pine pollen. Clin Exp Allergy Suppl. Sep 2009;39(9):1438–1446. doi: 10.1111/j.1365-2222.2009.03308.x. [DOI] [PubMed] [Google Scholar]
- 33.Bousquet J., Guérin B., Hewitt B., Lim S., Michel F.B. Allergy in the Mediterranean area. III: cross reactivity among Oleaceae pollens. Clin Allergy. Sep 1985;15(5):439–448. doi: 10.1111/j.1365-2222.1985.tb02293.x. [DOI] [PubMed] [Google Scholar]
- 34.Geller-Bernstein C., Waisel Y., Lahoz C. Environment and sensitization to cypress in Israel. Allerg Immunol (Paris) Mar 2000;32(3):92–93. [PubMed] [Google Scholar]
- 35.Charpin D. Epidemiology of cypress allergy. Allerg Immunol (Paris) Mar 2000;32(3):83–85. [PubMed] [Google Scholar]
- 36.Subiza J., Jerez M., Jiménez J.A., et al. Allergenic pollen pollinosis in Madrid. J Allergy Clin Immunol. Jul 1995;96(1):15–23. doi: 10.1016/s0091-6749(95)70028-5. [DOI] [PubMed] [Google Scholar]
- 37.Ramon G.D., Barrionuevo L.B., Viego V., et al. Sensitization to subtropical grass pollens in patients with seasonal allergic rhinitis from Bahia Blanca, Argentina. World Allergy Organ J. Sep 2019;12(9) doi: 10.1016/j.waojou.2019.100062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Camargo J.F., Godoi R.H.M., Rosário C.S., Rosario N.A. Seasonal changes in Poaceae pollen counts in Curitiba, south of Brazil. Arq Asma Alerg Imunol. 2022;6(3):354–359. doi: 10.5935/2526-5393.20220040. [DOI] [Google Scholar]
- 39.Vieira F.A.M. Gramíneas tropicais alergênicas: Cynodon dactylon e Paspalum notatum- uma visão para o trópico brasileiro. Rev Bras Alerg Imunopatol. 2012;35:40–41. [Google Scholar]
- 40.Mandrioli P., Di Cecco M., Andina G. Ragweed pollen: the aeroallergen is spreading in Italy. Aerobiologia. 1998/03/01 1998;14(1):13. doi: 10.1007/BF02694590. [DOI] [Google Scholar]
- 41.Asero R., Wopfner N., Gruber P., Gadermaier G., Ferreira F. Artemisia and Ambrosia hypersensitivity: co-sensitization or co-recognition? Clin Exp Allergy. May 2006;36(5):658–665. doi: 10.1111/j.1365-2222.2006.02477.x. [DOI] [PubMed] [Google Scholar]
- 42.D'Amato G., Pawankar R., Vitale C., et al. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res. Sep 2016;8(5):391–395. doi: 10.4168/aair.2016.8.5.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singer B.D., Ziska L.H., Frenz D.A., Gebhard D.E., Straka J.G. Research note: increasing Amb a 1 content in common ragweed (Ambrosia artemisiifolia) pollen as a function of rising atmospheric CO(2) concentration. Funct Plant Biol. Aug 2005;32(7):667–670. doi: 10.1071/fp05039. [DOI] [PubMed] [Google Scholar]
- 44.Wayne P., Foster S., Connolly J., Bazzaz F., Epstein P. Production of allergenic pollen by ragweed (Ambrosia artemisiifolia L.) is increased in CO2-enriched atmospheres. Ann Allergy Asthma Immunol. Mar 2002;88(3):279–282. doi: 10.1016/s1081-1206(10)62009-1. [DOI] [PubMed] [Google Scholar]
- 45.Ziska L.H., Makra L., Harry S.K., et al. Temperature-related changes in airborne allergenic pollen abundance and seasonality across the northern hemisphere: a retrospective data analysis. Lancet Planet Health. Mar 2019;3(3):e124–e131. doi: 10.1016/s2542-5196(19)30015-4. [DOI] [PubMed] [Google Scholar]
- 46.Manangan A., Brown C., Saha S., et al. Long-term pollen trends and associations between pollen phenology and seasonal climate in Atlanta, Georgia (1992-2018) Ann Allergy Asthma Immunol. Oct 2021;127(4):471–480.e4. doi: 10.1016/j.anai.2021.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Choi Y.J., Lee K.S., Oh J.W. The impact of climate change on pollen season and allergic sensitization to pollens. Immunol Allergy Clin North Am. Feb 2021;41(1):97–109. doi: 10.1016/j.iac.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 48.Sénéchal H., Visez N., Charpin D., et al. A review of the effects of major atmospheric pollutants on pollen grains, pollen content, and allergenicity. Sci World J. 2015;2015 doi: 10.1155/2015/940243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schiavoni G., D'Amato G., Afferni C. The dangerous liaison between pollens and pollution in respiratory allergy. Ann Allergy Asthma Immunol. Mar 2017;118(3):269–275. doi: 10.1016/j.anai.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 50.Baldacci S., Maio S., Cerrai S., et al. Allergy and asthma: effects of the exposure to particulate matter and biological allergens. Respir Med. Sep 2015;109(9):1089–1104. doi: 10.1016/j.rmed.2015.05.017. [DOI] [PubMed] [Google Scholar]
- 51.Ziska L.H., Gebhard D.E., Frenz D.A., Faulkner S., Singer B.D., Straka J.G. Cities as harbingers of climate change: common ragweed, urbanization, and public health. J Allergy Clin Immunol. Feb 2003;111(2):290–295. doi: 10.1067/mai.2003.53. [DOI] [PubMed] [Google Scholar]
- 52.Bousquet J., Schunemann H.J., Togias A., et al. Next-generation allergic rhinitis and its impact on asthma (ARIA) guidelines for allergic rhinitis based on grading of recommendations assessment, development and evaluation (GRADE) and real-world evidence. J Allergy Clin Immunol. Jan 2020;145(1):70–80 e3. doi: 10.1016/j.jaci.2019.06.049. [DOI] [PubMed] [Google Scholar]
- 53.Golightly L.K., Greos L.S. Second-generation antihistamines: actions and efficacy in the management of allergic disorders. Drugs. 2005;65(3):341–384. doi: 10.2165/00003495-200565030-00004. [DOI] [PubMed] [Google Scholar]
- 54.Howarth P.H., Stern M.A., Roi L., Reynolds R., Bousquet J. Double-blind, placebo-controlled study comparing the efficacy and safety of fexofenadine hydrochloride (120 and 180 mg once daily) and cetirizine in seasonal allergic rhinitis. J Allergy Clin Immunol. Nov 1999;104(5):927–933. doi: 10.1016/s0091-6749(99)70070-9. [DOI] [PubMed] [Google Scholar]
- 55.Compalati E., Baena-Cagnani R., Penagos M., et al. Systematic review on the efficacy of fexofenadine in seasonal allergic rhinitis: a meta-analysis of randomized, double-blind, placebo-controlled clinical trials. Int Arch Allergy Immunol. 2011;156(1):1–15. doi: 10.1159/000321896. [DOI] [PubMed] [Google Scholar]
- 56.Ellis A.K., Murrieta-Aguttes M., Furey S., Picard P., Carlsten C. Effect of fexofenadine hydrochloride on allergic rhinitis aggravated by air pollutants. ERJ Open Res. Apr 2021;7(2) doi: 10.1183/23120541.00806-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Casale T.B., Andrade C., Qu R. Safety and efficacy of once-daily fexofenadine HCl in the treatment of autumn seasonal allergic rhinitis. Allergy Asthma Proc. May-Jun 1999;20(3):193–198. doi: 10.2500/108854199778553046. [DOI] [PubMed] [Google Scholar]
- 58.Nathan R.A., Mason J., Bernstein D.I., et al. Long-term tolerability of fexofenadine in healthy volunteers. Clin Drug Invest. 1999/10/01 1999;18(4):317–328. doi: 10.2165/00044011-199918040-00008. [DOI] [Google Scholar]
- 60.Meltzer E.O., Rosario N.A., Van Bever H., et al. Fexofenadine: review of safety, efficacy and unmet needs in children with allergic rhinitis. Allergy Asthma Clin Immunol. 2021;17:113. doi: 10.1186/s13223-021-00614-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.