Abstract
Background
Albumin infusion is the primary therapeutic strategy for septic patients with liver cirrhosis. Although recent studies have investigated the efficacy of albumin in the resuscitation stage of septic patients with liver cirrhosis, it remains unclear whether daily albumin administration can improve outcomes. Furthermore, the indications for initiating albumin therapy are not well defined.
Methods
Septic patients with liver cirrhosis were obtained from the Medical Information Mart for Intensive Care (MIMIC-IV 2.0) database. Marginal structural Cox models were employed to investigate the association between daily albumin infusion and 28-day mortality. We also aimed to explore under what circumstances enrolled patients could benefit most from albumin administration, based on the clinical parameters collected on the day of albumin infusion, including serum albumin concentration, serum lactate concentration, mean arterial pressure (MAP), and vasopressor dosage.
Results
A total of 2265 patients were included in the final analysis, of whom 1093 (48.3%) had received albumin treatment at least once. The overall 28-day mortality was 29.6%. After marginal structural modeling, daily albumin infusion was associated with a reduced risk of 28-day death (hazard ratio, 0.76; 95% CI 0.61–0.94). We found that patients benefit most from albumin infusion when initiated on the day of serum albumin concentration between 2.5 and 3.0 g/dL, serum lactate concentration greater than or equal to 2 mmol/L, MAP less than 60 mmHg, or vasopressor dosage between 0.2 and 0.3 mcg/kg/min (norepinephrine equivalent, NEE).
Conclusions
Albumin infusion is associated with a reduction in mortality in septic patients with liver cirrhosis under specific circumstances. Serum albumin concentration, serum lactate, MAP, and vasopressor dosage were found to be modifiers of treatment effectiveness and should be considered when deciding to initial albumin infusion.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-023-04587-3.
Keywords: Sepsis, Liver cirrhosis, Albumin, Time-varying confounder
Background
Sepsis is defined as the dysregulated host response to infection that leads to life-threatening acute organ dysfunction [1, 2]. Liver cirrhotic patients with sepsis have worse outcomes than those without, mainly attributed to its intrinsic characteristics, including portosystemic shunting, gut dysbiosis, increased bacterial translocation, cirrhosis-associated immune dysfunction, and genetic factors [3, 4]. Cirrhotic patients with sepsis constitute a distinct population regarding clinical course and prognosis, mainly characterized by prominent hemodynamic instability, reduced colloid oncotic pressure, and hypoalbuminemia. Thus, albumin infusion is pivotal to improving this population's prognosis, which they are prone to benefit from [5, 6].
Although albumin administration demonstrated its potential beneficial effects for cirrhotic patients with sepsis in several clinical trials [7, 8], and its role in reversing sepsis-induced hypotension is endorsed by current guidelines [9], several controversial and challenging issues remain to be addressed. First, recent studies investigating the efficacy of albumin in septic patients with liver cirrhosis tend to focus on the resuscitation stage, neglecting the impact on the prognosis of dynamic albumin administration throughout the entire clinical course of the illness. Aside from maintaining intravascular oncotic pressure during resuscitation, albumin’s anti-inflammatory, immunomodulating, positive effects on vessel wall integrity, drug-carrying, and nitric oxide scavenging properties can also lead to more favorable outcomes. Second, although limited data pointed out a potential benefit of maintaining serum albumin concentration at more than 30 g per liter in critically ill patients [10, 11], the well-designed ALBIOS trial could not substantiate the advantages of albumin infusion, a conclusion that may partly be attributed to excluding patients with cirrhosis [12]. For septic patients with liver cirrhosis, a specific cutoff for serum albumin concentration has not been established yet, below which initiating albumin administration would be invariably associated with lower mortality and considered a therapeutic necessity. Moreover, whether cutoff values derived from clinical variables other than serum albumin concentration can be used as indications for albumin administration has not been explored thoroughly.
This study focused primarily on patients with sepsis and liver cirrhosis, aiming to investigate dynamic albumin administration's impact on prognosis and clarify potential indications for albumin administration.
Materials and methods
Study design and participants
We conducted a retrospective analysis of the MIMIC-IV (2.0) database, which contains comprehensive and high-granularity information about well-defined and characterized patients admitted to ICUs at Beth Israel Deaconess Medical Center between 2008 and 2019 [13]. Two authors obtained access to the database and were responsible for data extraction (certification numbers 27252652 and 39732765).
Critically ill adult patients with liver cirrhosis who met the Sepsis 3.0 criteria were eligible (Supplemental Method A) [2, 14, 15]. Patients with a hospital length of stay less than 24 h, those who were identified as sepsis 12 h before or 24 h after ICU admission, and patients with an ICU length of stay less than 24 h or more than 100 days were excluded. Furthermore, we analyzed only the first ICU stay for patients who were admitted to the ICU more than once.
Because only third-party anonymized publicly available data were used, the study was considered exempt from human subjects committee review. This study was reported in accordance with the REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement [16].
Variable extraction and data collection
Three sets of data were collected: baseline, daily observations, and outcome. The following data were extracted from the MIMIC-IV database on the first day of ICU admission: age, gender, weight, ethnicity, admission type, comorbidity, Sequential Organ Failure Assessment (SOFA) score, and each component of the SOFA score. Other relevant data, including vital signs, laboratory measurements, and treatment regimens, were obtained daily throughout the ICU stay. If a variable was recorded more than once on one ICU Day, we used the value related to the greatest severity of illness. The selection strategy for variables with multiple measurements is shown in Additional file 1: Table S1. The chart time of measurement and physiologic values were extracted from the database. Based on Townsend et al. [17], we conducted a thorough identification of infection sites based on the ICD-9-CM and ICD-10-CM codes available at discharge (Additional file 1: Table S2). Septic shock was recognized as vasopressor use and a serum lactate concentration > 2 mmol/L. Acute kidney injury was defined according to the clinical practice guidelines of Kidney Disease: Improving Global Outcomes (KDIGO) [18]. Time to antibiotics was determined as the duration from ICU admission to antibiotic administration. Variables with more than 60% missing values were excluded from the analysis (Additional file 1: Table S3, Table S4) [19]. Multiple imputation by weighted predictive mean matching was performed for variables with missing values of less than 60% (Supplemental Method B) [20].
Primary exposure and outcomes
The main exposure of interest was the daily administration of intravenous (IV) albumin throughout the ICU stay. All manners of administering albumin were considered. The infusion time of albumin, solution concentration, and the total amount of albumin administered were extracted from the database.
The primary outcome was 28-day mortality. Secondary outcomes included ICU-free days at day 28, hospital-free days at day 28, and in-hospital mortality, defined as the status of patient survival at the time of hospital discharge.
Statistical analysis
The study population was categorized into those treated with albumin (albumin group) and those who did not receive albumin during the entire ICU stay (non-albumin group). Values are presented as the mean (standard deviation) or median [interquartile range (IQR)] for continuous variables when appropriate and as the total number (percentage) for categorical variables. Comparisons between groups were made using the X2 test or Fisher’s exact test for categorical variables and Student’s t-test or Mann–Whitney U test for continuous variables as appropriate.
Albumin exposure was initially dichotomized as “any dosage versus none” on a daily basis. To estimate the impact of albumin treatment on 28-day mortality from longitudinal observational data, the time-dependent nature of albumin administration was first explored by marginal structural Cox proportional hazards models (MSCM) with inverse probability weighting (Supplemental Method C) [21]. The probability of receiving albumin infusion was weighted by adjusting for baseline confounders (age, gender, admission type, ethnicity, infection site, and serum albumin concentration) and time-varying confounders (SOFA score, serum lactate concentration, PaO2/FiO2 ratio, vasopressor dose, daily UO, and MAP) (Additional file 1: Figure S1). An extended Kaplan–Meier survival analysis was also performed, incorporating the weights derived from the marginal structural models [22]. As the effect of albumin treatment may differ depending on the time of initiation, MSCM with Heaviside functions was utilized to assess how the hazard ratio (HR) for death at 28 days changed over four consecutive weeks [23]. Each follow-up interval was assigned its own HR. Further, the correlation was re-evaluated in a multivariable Cox model with time-fixed and time-dependent covariates for 28-day mortality adding to the model the effect of albumin administration, weighted with marginal structural models [24]. In multivariable MSCM, we avoided multicollinearity by removing highly correlated covariates (Additional file 1: Figure S2, Figure S3) and identified the subset of covariates that gave the lowest -2 log L value by stepwise selection (Additional file 1: Figure S4). At last, extended Cox proportional hazards models with time-varying confounders were adopted to assess the robustness of the results [25].
Sensitivity analysis was executed after eliminating cases of spontaneous bacterial peritonitis. Subgroup evaluations were carried out based on several factors at ICU admission, including age, gender, site of infection, SOFA and MELD scores, the incidence of acute kidney injury, septic shock, platelet count, and the PaO2/FiO2 ratio. For continuous variables, the points of differentiation were obtained from either pre-existing knowledge or the interquartile range.
Second, we estimated the effectiveness of albumin administration using clinical parameters on the day of albumin infusion as indications, which the treating intensivists might have considered to decide whether albumin therapy should be initiated or not, including laboratory measurements (serum albumin concentration, serum lactate concentration), physiologic characteristics (MAP), and specific treatment regimens (NEE equivalent dose). Details about thresholds setting are shown in Additional file 1: Table S5. Schematic illustrations of the sub-cohort establishment are shown in Additional file 1: Figure S5. MSCMs were conducted in each sub-cohort to evaluate the impact of albumin administration on prognosis, weighted by adjusting for the confounding factors as aforementioned.
Third, the effects of albumin infusion were tested within different cutoffs of laboratory measurements. Initially, a data-driven threshold was determined by repeating the models with a 0.1 g/dL increase in the serum albumin threshold until reaching the highest value when albumin infusion was still associated with a reduction in risk of 28-day death. Then, another threshold was determined by repeating the models with a 0.1 mmol/L decrease in serum lactate threshold until reaching the lowest point when albumin infusion was consistently associated with decreased mortality.
Fourth, to further explore the effects of different albumin dosages on 28-day mortality, we stratified daily albumin exposure into five groups: no exposure, ≤ 0.5 g/kg, ≤ 1.0 and > 0.5 g/kg, ≤ 1.5 and > 1.0 g/kg, > 1.5 g/kg. Regression models were fitted using multinom (nnet) to calculate inverse probability weights of multi-groups [21]. We also assessed the treatment effects of different albumin solutions (5% and 25% concentrations) employing the same methodologies.
All statistical analyses were performed using R (version 4.2.2), and P < 0.05 was considered statistically significant. Bonferroni’s correction for multiple comparisons was used where appropriate.
Results
Patient characteristics
A total of 2,265 septic patients with liver cirrhosis were included in the final analysis (Fig. 1). During the 28-day follow-up, 670 patients died (29.6%). Longitudinal data were collected for 12,441 ICU days. Out of this cohort, 1,093 patients (48.3%) received albumin infusion at least once during their ICU stay. Compared with the non-albumin group, patients in the albumin group were more severely ill, with a higher SOFA score (5 [IQR, 3–7] vs. 4 [IQR, 2–5]), a higher likelihood of receiving mechanical ventilation (662 [61%] vs. 647 [55%]), and a higher incidence of septic shock (375 [34%] vs. 182 [16%]). At ICU admission, the occurrence of acute kidney injury (AKI) was noticeably greater in the albumin-administered group compared to those not receiving albumin (854 [78%] vs. 619 [53%]). The group receiving albumin showed a significantly higher 28-day mortality rate than the group that did not (447 [41%] vs. 223 [19%]). Notably, there was no significant difference in serum albumin concentration at ICU admission between treated and untreated patients (Table 1).
Fig. 1.
Flowchart showing patient selection for the study. MIMIC-IV: Medical Information Mart for Intensive Care IV; ICU: intensive care unit
Table 1.
Baseline characteristics and outcomes of patients with and without IV albumin administration during ICU stay
| Variables | Total patients (n = 2265) |
Non-albumin group (n = 1172) |
Albumin group (n = 1093) |
P value |
|---|---|---|---|---|
| Male, [n (%)] | 1453 (64) | 773 (66) | 680 (62) | 0.07 |
| Age, [years, M(IQR)] | 59 (52, 67) | 60 (52, 67) | 58 (51, 66) | 0.002 |
| Weight, [kg, M(IQR)] | 81 (69, 97) | 80.45 (68, 96.3) | 81.8 (69.2, 98.3) | 0.126 |
| Height, [cm, M(IQR)] | 170 (165, 178) | 173 (165, 178) | 170 (163, 178) | 0.185 |
| Admission type*, [n (%)] | < 0.001 | |||
| Elective | 11 (0) | 5 (0) | 6 (1) | |
| Emergency | 1420 (63) | 784 (67) | 636 (58) | |
| Observation | 243 (11) | 93 (8) | 150 (14) | |
| Surgical | 43 (2) | 20 (2) | 23 (2) | |
| Urgent | 548 (24) | 270 (23) | 278 (25) | |
| Infection site, [n (%)] | < 0.001 | |||
| Respiratory | 400 (18) | 167 (14) | 233 (21) | |
| Gastrointestinal | 173 (8) | 62 (5) | 111 (10) | |
| Genitourinary | 186 (8) | 101 (9) | 85 (8) | |
| Others | 1506 (66) | 842 (72) | 664 (61) | |
| Severity of illness | ||||
| CCI, [M(IQR)] | 7 (5, 9) | 7 (5, 9) | 6 (5, 8) | 0.138 |
| APS III, [M(IQR)] | 60 (45, 83) | 51 (40, 68) | 73 (55, 95) | < 0.001 |
| OASIS, [M(IQR)] | 35 (28, 42) | 32 (26, 39) | 37 (31, 44) | < 0.001 |
| GCS, [M(IQR)] | 15 (14, 15) | 15 (14, 15) | 15 (13, 15) | < 0.001 |
| SOFA score, [M(IQR)] | 4 (3, 6) | 4 (2, 5) | 5 (3, 7) | < 0.001 |
| Laboratory measurements | ||||
| WBC, [10^9/L, M(IQR)] | 10.7 (6.9, 16.2) | 9.4 (6.2, 14.3) | 12.2 (7.8, 18.3) | < 0.001 |
| NLR, [M(IQR)] | 8.8 (4.8, 16.0) | 7.7 (4.3, 14.2) | 9.5 (5.3, 17.4) | < 0.001 |
| Chloride, [mmol/L, M(IQR)] | 105 (100, 109) | 106 (101, 110) | 104 (99, 109) | < 0.001 |
| Sodium, [mmol/L, M(IQR)] | 138 (135, 142) | 139 (135, 142) | 138 (133, 141) | < 0.001 |
| Hemoglobin, [g/dL, M(IQR)] | 8.7 (7.5, 10.2) | 9.1 (7.8, 10.6) | 8.4 (7.2, 9.6) | < 0.001 |
| ALT, [U/L, M(IQR)] | 33 (21, 69) | 33 (20, 65) | 34 (21, 73) | 0.06 |
| AST, [U/L, M(IQR)] | 71 (42, 146) | 65 (38, 127) | 78 (44, 170) | < 0.001 |
| Albumin, [g/dL, M(IQR)] | 2.8 (2.4, 3.2) | 2.8 (2.4, 3.2) | 2.8 (2.4, 3.3) | 0.313 |
| Total bilirubin, [mg/dL, M(IQR)] | 2.7 (1.2, 6.6) | 1.8 (0.9, 4) | 4.4 (2, 9.7) | < 0.001 |
| Platelet, [10^9/L, M(IQR)] | 82 (52, 132) | 88 (56, 145) | 75 (48, 120) | < 0.001 |
| INR, [M(IQR)] | 1.7 (1.4, 2.3) | 1.6 (1.3, 1.9) | 2 (1.6, 2.6) | < 0.001 |
| aPTT, [s, M(IQR)] | 39.4 (33, 52.6) | 35.7 (31, 44.7) | 44.3 (36.1, 58.1) | < 0.001 |
| Creatinine, [mg/dL, M(IQR)] | 1.3 (0.9, 2.4) | 1.1 (0.8, 2.1) | 1.6 (1, 2.7) | < 0.001 |
| BUN, [mmol/L, M(IQR)] | 29 (18, 49) | 26 (17, 43) | 33 (20, 54) | < 0.001 |
| BE, [mmol/L, M(IQR)] | − 2 (− 6, 0) | − 1 (− 5, 0) | − 4 (− 8, 0) | < 0.001 |
| Bicarbonate, [mmol/L, M(IQR)] | 20 (17, 23) | 21 (18, 24) | 19 (16, 22) | < 0.001 |
| Lactate, [mmol/L, M(IQR)] | 2.3 (1.6, 3.7) | 2 (1.5, 3) | 2.7 (1.8, 4.4) | < 0.001 |
| PaO2, [mmHg, M(IQR)] | 64 (43, 90) | 67 (44, 94) | 60 (42, 86) | < 0.001 |
| PaCO2, [mmHg, M(IQR)] | 41 (35, 48) | 41 (35, 49) | 41 (34, 48) | 0.039 |
| PaO2/FiO2 ratio [mmHg, M(IQR)] | 185 (112.5, 272.5) | 195 (123.25, 282.5) | 176.67 (104, 262.5) | < 0.001 |
| pH, [M(IQR)] | 7.36 (7.28, 7.42) | 7.37 (7.3, 7.42) | 7.34 (7.26, 7.4) | < 0.001 |
| Vital signs | ||||
| Heart rate, [beats , M(IQR)] | 105 (91, 119) | 104.5 (91, 118) | 107 (93, 120) | 0.016 |
| MAP, [mmHg, M(IQR)] | 56 (49, 63) | 58 (51, 65) | 55 (48, 61) | < 0.001 |
| RR, [ breaths , M(IQR)] | 27 (23, 32) | 27 (23, 31) | 27 (24, 32) | 0.078 |
| Temperature, [℃, M(IQR)] | 37.2 (36.9, 37.6) | 37.2 (36.9, 37.7) | 37.1 (36.9, 37.6) | < 0.001 |
| Organ support components | ||||
| Vasopressor use, [n (%)] | 903 (40) | 360 (31) | 543 (50) | < 0.001 |
| Vasopressor dose, [mcg/kg/min, M(IQR)] | 0 (0, 0.15) | 0 (0, 0.06) | 0 (0, 0.24) | < 0.001 |
| RRT, [n (%)] | 161 (7) | 74 (6) | 87 (8) | 0.149 |
| Mechanical ventilation, [n (%)] | 1309 (58) | 647 (55) | 662 (61) | 0.011 |
| Time to antibiotics, [hour, M(IQR)] | 3.7 (1.8, 11.3) | 3.8 (1.8, 10.8) | 3.6 (1.8, 12.6) | 0.965 |
| Time to sepsis onset, [hour, M(IQR)] | − 1.9 (− 4.8, 0.6) | − 1.8 (− 4.7, 0.6) | − 2.0 (− 4.8, 0.5) | 0.066 |
| Urine output, [mL, M(IQR)] | 1155 (588, 1853) | 1375 (785, 2102.5) | 905 (450, 1575) | < 0.001 |
| Fluid balance, [mL, M(IQR)] | 437 (− 951, 1909) | 93 (− 1198, 1376) | 847 (− 536, 2426) | < 0.001 |
| Spontaneous bacterial peritonitis, [n (%)] | 186 (8) | 33 (3) | 153 (14) | < 0.001 |
| Septic shock, [n (%)] | 557 (25) | 182 (16) | 375 (34) | < 0.001 |
| Acute kidney injury, [n (%)] | 1473 (65) | 619 (53) | 854 (78) | < 0.001 |
| ICU readmission, [n (%)] | 178 (8) | 67 (6) | 111 (10) | < 0.001 |
| 28-day mortality, [n (%)] | 670 (30) | 223 (19) | 447 (41) | < 0.001 |
| 90-day mortality, [n (%)] | 875 (39) | 314 (27) | 561 (51) | < 0.001 |
| Hospital mortality, [n (%)] | 573 (25) | 181 (15) | 392 (36) | < 0.001 |
| Hospital-free days, [days, M(IQR)] | 10 (0, 21) | 18 (0, 23) | 0 (0, 15) | < 0.001 |
| ICU-free days, [days, M(IQR)] | 23.1 (0, 25.9) | 25.0 (19.0, 26.2) | 15.2 (0, 24.6) | < 0.001 |
CCI = Charlson Comorbidity Index; SAPS II = Simplified Acute Physiology Score II; OASIS = Oxford Acute Severity of Illness Score; SOFA = Sequential Organ Failure Assessment; WBC = white blood cells; NLR = neutrophil-to-lymphocyte ratio; ALT = alanine transaminase; AST = aspartate aminotransferase; GCS = Glasgow Coma Scale; INR = international normalized ratio; aPTT = activated partial thromboplastin clotting time; BUN = blood urea nitrogen; MAP = mean arterial pressure; BE = base excess; PaCO2 = partial pressure of carbon dioxide; PaO2/FiO2 ratio = ratio of arterial oxygen partial pressure to fractional inspired oxygen; RR = respiration rate; RRT = renal replacement therapy; ICU = intensive care unit
*The 'AMBULATORY OBSERVATION,' 'DIRECT OBSERVATION,' 'EU OBSERVATION,' and 'OBSERVATION ADMIT' categories were consolidated into a single group labeled ‘observation.’
Vital signs, laboratory measurements, and other time-varying variables presented in this table were collected within 24 h of ICU admission. If a variable was recorded more than once in 24 h, we used the value related to the greatest severity of illness
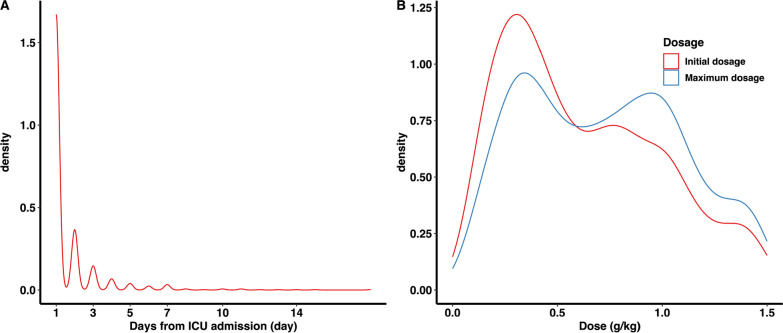
Albumin administration had a median initiation time of 1.0 days (IQR 1.0–2.0) from ICU admission. The initial and maximum daily doses administered were 0.62 g/kg (IQR 0.32–1.03) and 0.82 g/kg (IQR 0.42–1.19), respectively. The duration of albumin treatment was 2.0 days (IQR, 1.0–3.0 days), with a maximum of 25.0 days. Figure 2 shows the time distribution from ICU admission to initiation of albumin administration (Fig. 2A) and the initial and maximum daily dosage of albumin therapy (Fig. 2B).
Fig. 2.
Distribution of time to initiate albumin administration (A) and dosage of albumin therapy (B)
Impact of albumin administration on the risk of 28-day death
According to the results of the marginal structure Cox proportional model, albumin administration was associated with a reduced probability of death across the 28-day follow-up (HR 0.76 [95% CI 0.61–0.94]) (Table 2) (Additional file 1: Figure S6). The distributions of IPW in albumin and non-albumin groups are shown in Additional file 1: Figure S7. However, using Heaviside functions, this association remained significant only in the first week, when evaluated by each week during the 28 days. The results of the multivariate MSCM in the overall population were in accordance with the univariate MSCM (HR 0.64 [95% CI 0.51–0.80]) (Additional file 1: Table S6). Besides, the association was confirmed by the extended Cox proportional hazards model (HR 0.74 [95% CI 0.61–0.89]) (Additional file 1: Table S7).
Table 2.
MSCM for the effect of albumin administration with the trend over the follow-up on 28-day mortality
| Marginal structural cox proportional hazards model for 28-day mortality | ||||||
|---|---|---|---|---|---|---|
| Variable | Overall effect during follow-up | P value | Heaviside step functions | |||
| Week 1 | Week 2 | Week 3 | Week 4 | |||
| Albumin administration | 0.76 (0.61–0.94) | 0.0132 | 0.72 (0.56–0.92)* | 0.79 (0.47–1.32) | 1.08 (0.35–3.30) | 2.52 (0.42–14.96) |
MSCM = Marginal Structural Cox proportional hazards Model
Sensitivity analysis
After the exclusion of patients with spontaneous bacterial peritonitis, 2,079 patients remained. The results of the sensitivity analysis were consistent with the primary analysis: Weighted by MSCM, albumin infusion was associated with reduced 28-day mortality regardless of the univariate (HR 0.72 [95% CI 0.56–0.92]) or multivariate model (HR 0.62 [95% CI 0.49–0.80]) (Additional file 1: Table S8).
Subgroup analysis
Albumin administration was associated with lower 28-day mortality in patients with MELD score ≥ 20 (HR 0·68 [95% CI 0·54–0·84]), septic shock (HR 0·65 [95% CI 0·48–0·89]), and total bilirubin ≥ 3.0 mg/dl (HR 0.61 [95% CI 0·47–0·79]), while no interaction was detected. More importantly, significant interaction relationships were observed among patients with acute kidney injury (HR 0.66 [95% CI 0·52–0·83] vs. HR 0.99 [95% CI 0·59–1.67]; P for interaction = 0.019) and low platelet counts (HR 0.59 [95% CI 0·41–0·83] vs. HR 0.94 [95% CI 0·71–1.25]; P for interaction = 0.018). However, no such interactive effects were found between albumin administration and different infection sites regarding 28-day mortality (Additional file 1: Figure S8).
Indications for albumin administration
The effects of albumin administration were accessed under varying serum albumin concentrations (Fig. 3). We detected that albumin therapy significantly improved outcomes only when initiated in patients with a serum albumin concentration of 2.5–3.0 g/dL, with a hazard ratio for 28-day mortality of 0.49 (0.31 to 0.78). The following hazard ratios for mortality were measured if albumin administration had been initiated according to the other four prespecified thresholds for serum albumin concentration: < 2.5 g/dL, 0.88 (0.55 to 1.40); < 3.5 and ≥ 3.0 g/dL, 0.66 (0.42 to 1.04); < 4.0 and ≥ 3.5 g/dL, 0.71 (0.43 to 1.15); and ≥ 4.0 g/dL, 0.59 (0.31–1.12). Additionally, the highest serum albumin concentration derived as a trigger for albumin administration associated with a reduced risk of death was 2.7 g/dL (Additional file 1: Table S9).
Fig. 3.
Sub-cohort analyses of the association between albumin administration and 28-day mortality using MSCM. HR: hazard ratio; NEE: norepinephrine equivalence
Likewise, when comparing albumin treatment strategies initiated in patients with higher time-dependent serum lactate concentrations to those not receiving albumin treatment, the results suggested albumin therapy significantly improved outcomes only when initiated in patients with a serum lactate concentration of more than or equal to 2.0 mmol/L. Subsequently, we identified that the lowest serum lactate concentration derived as a trigger for albumin administration associated with a reduced risk of death was 2.2 mmol/L (Additional file 1: Table S10). We also observed that albumin therapy significantly increased 28-day survival only when initiated in patients with a MAP of less than 60 mmHg, with a hazard ratio of 0.54 (0.30 to 0.99), regardless of the vasopressor dose. Further, for patients receiving vasopressor regimens, it is optimal to initiate albumin administration when the NEE equivalent dose is between 0.2 and 0.3 mcg/kg/min.
Secondary analysis
Adopting multinomial MSCM weighted for the same covariates as above, the association between different albumin dosages and 28-day mortality was demonstrated. The results revealed that the beneficial effects of albumin infusion were compromised when the daily dose exceeded 1.0 g/kg (daily dose ≤ 1.5 and > 1.0 g/kg: HR 0.81 [95% CI 0.50–1.29]) (Table 3). Additionally, our analysis indicated that both 25% and 5% albumin solution administrations were associated with reduced 28-day mortality (Additional file 1: Table S11).
Table 3.
Association between different albumin dosage strata and 28-day mortality estimated by the MSCM
| Albumin dosage* strata | No. of patients | Hazard ratio | Lower limit of 95% CI | Upper limit of 95% CI | P value |
|---|---|---|---|---|---|
| ≤ 0.5 g/kg | 665 | 0.62 | 0.43 | 0.88 | 0.008 |
| ≤ 1.0 and > 0.5 g/kg | 547 | 0.52 | 0.34 | 0.80 | 0.003 |
| ≤ 1.5 and > 1.0 g/kg | 299 | 0.81 | 0.50 | 1.29 | 0.37 |
| > 1.5 g/kg | 151 | 0.87 | 0.39 | 1.94 | 0.73 |
*The albumin dosage was calculated on a daily basis using the formula: Albumin dosage = [amount A (mL) × concentration A + amount B (mL) × concentration B + …]/weight (kg)
CI = Confidence interval; MSCM = Marginal Structural Cox proportional hazards Model
Discussion
Our study on cirrhotic patients with sepsis has many novel findings that merit further discussion. First, dynamic albumin infusion was associated with a reduced 28-day risk of death, especially during the first week of illness, but only in specific sub-cohorts. Second, in patients when albumin administration was initiated on the day of serum albumin concentration between 2.5 and 3.0 g/dL, serum lactate concentration greater than or equal to 2 mmol/L, MAP less than 60 mmHg, or vasopressor dosage between 0.2 and 0.3 mcg/kg/min (norepinephrine equivalent, NEE), we found that albumin infusion would have been most effective.
Previous studies proved that albumin administration could significantly improve the hemodynamics of septic patients with cirrhosis as a resuscitation fluid, while the sustained benefit of albumin administration was only identified in septic shock in a subgroup analysis of the SAFE study [26]. Our data confirmed the beneficial effects of daily albumin administration in septic patients with cirrhosis, and baseline subgroups suggested that patients with higher severity of illness and more organ dysfunctions would benefit more from albumin infusion. The oncotic properties of albumin are well known. Moreover, human serum albumin displays pivotal secondary functions in patients with cirrhosis, including antioxidant, immune-modulating effects, and positive inotropic effects, which could explain the longitudinal association between albumin infusion and prognosis.
Limited data were available regarding the indications for albumin infusion in septic patients with cirrhosis. Hypoalbuminemia (generally defined as a serum albumin concentration ≤ 30 g/L) was a prognostic biomarker in acutely ill patients, and each 10 g/L decrease in serum albumin concentration was associated with a 137% increase in the odds of death, an 89% increase in morbidity, and a 71% increase in length of hospital stay [11]. Correction of hypoalbuminemia via albumin infusion remains controversial. A pilot study found that maintaining serum albumin of more than 30 g per liter results in improved organ function, a less positive fluid balance, and a better tolerance of enteral feeding in critically ill patients [10]. A meta-analysis of dose-dependency in controlled trials of albumin therapy hypothesized that complication rates might be reduced when the serum albumin level attained during albumin administration exceeds 30 g/L, while no significant survival benefit was demonstrated [11]. The ALBIOS study also declared that in patients with severe sepsis, daily administration of albumin to maintain a serum albumin level of 30 g per liter or more, compared with crystalloids alone, did not improve the survival rate at 28 and 90 days [12]. Our analysis generated a reliable, data-driven threshold for serum albumin concentration at 2.7 g/dL, beneath which the albumin administration corresponded to a diminished 28-day mortality risk. A closer examination of specific sub-cohorts derived from real-time clinical parameters revealed that the employment of albumin was particularly beneficial when commenced in septic patients with liver cirrhosis, exhibiting serum albumin levels between 2.5 and 3.0 g/dL. Nevertheless, we also noted that those with a serum albumin concentration of less than 2.5 g/dL did not experience the same advantageous effects from albumin infusion. The observed divergence can likely be attributed to the circumstance that this specific sub-cohort was not enduring a continuous state of illness—during which the proposed treatment might significantly impact outcomes—but was rather facing a rapid mortality scenario [27]. Furthermore, despite our rigorous efforts to adjust for potential biases, it is possible that some residual confounders were not fully eliminated.
Meanwhile, we also explored the potential indications for albumin infusion except for hypoalbuminemia and declared that albumin infusion would also be effective if provided to selected patients with unstable hemodynamic status, indicating by serum lactate greater than or equal to 2 mmol/L, MAP less than 60 mmHg, or vasopressor dosage between 0.2 and 0.3 mcg/kg/min (NEE), regardless of the serum albumin concentration. Although the beneficial effects of albumin infusion on hemodynamic status have been proved, no clear criteria were available. The present study identified clear criteria using a data-driven approach under real-world conditions.
The systemic and organ inflammation-modulating effect of albumin highly depends on the post-treatment serum albumin concentration, emphasizing the importance of albumin dosage [28, 29]. The three randomized controlled trials so far published assessing the beneficial effects of albumin therapy in cirrhosis patients with non-SBP infection draw similar conclusions that receiving albumin 1.5 g/kg on day 1 and 1 g/kg on day 3 would not improve survival [30–32]. A more troublesome observation was that Thévenot et al. [32] found nine patients who suffered from pulmonary edema following albumin infusion, two of whom died within a short time window after albumin infusion. These findings were validated in our study. The association between different albumin dosages and 28-day mortality suggested that the therapeutic effects of albumin infusion were compromised when the daily dose exceeded 1.0 g/kg. Despite the potential benefits of albumin, its protective oncotic effect may be diminished when capillary permeability increases, a condition well established in cirrhotic patients with sepsis, exacerbated by impaired lymphatic circulation [33–35]. Increased extravasation of albumin from capillaries may result in accumulation within the extravascular spaces, leading to fluid overload subsequently [36]. Overall, from a clinical point of view, we suggested that a large amount of albumin administration should be avoided in patients with prominent pulmonary capillary permeability alterations, or given cautiously after a thorough assessment of cardiac function and volume status.
Several limitations in the present study should be acknowledged. First, this study was based on electronic healthcare records of routine clinical practice with missing data and outliers. To retain statistical power, we used multiple imputation by weighted predictive mean matching to reduce the risk of bias from missing data. Second, the single-database design requires further validation to confirm its beneficial effects. Third, it is imperative to acknowledge that the MIMIC-IV database collects data over a time span of more than a decade. Consequently, our findings might be influenced by changes in the guidelines for sepsis and liver cirrhosis that occurred during this period, which could affect the practical relevance of our results. Fourth, this study included patients who belong to a well-defined and characterized clinical entity. Thus, the threshold may not apply to other patients. Fifth, whether the benefits we observed are primarily attributed to sepsis management, cirrhosis-related complications, or an amalgamation of both remains an essential question that needs to be addressed. The therapeutic effects of albumin between septic patients with and without liver cirrhosis warrant further investigation.
Conclusion
In conclusion, dynamic albumin administration provided a significant survival benefit at 28 days in septic patients with liver cirrhosis, especially in specific sub-cohorts. Serum albumin concentration, serum lactate, MAP, and vasopressor dosage were found to be modifiers of treatment effectiveness and should be considered when deciding to initial albumin infusion. Large amounts of albumin infusion (> 1.0 g/kg) should be cautiously administered in patients with prominent pulmonary capillary permeability alterations. Prospective interventional trials are needed to confirm these findings.
Supplementary Information
Additional file 1: Additional method. Table S1: Selection strategy for variables with multiple measurements. Table S2: Infection category codes from ICD-9-CM to ICD-10-CM. Table S3: Missing rate for demographics and clinical variables extracted from the database during the observation period. Table S4: Missing rate for demographics and clinical variables extracted from the database on the first day. Table S5: Thresholds for clinical variables as albumin therapy indication. Table S6: Multivariable Cox model with time-fixed and time-dependent covariates for 28-day mortality adding to the model the effect of albumin administration, weighted with marginal structural models. Table S7: Association between albumin administration and 28-day mortality estimated by extended Cox regression model with time-varying covariates. Table S8: Univariate and multivariate analyses weighted with MSCM of the association between albumin infusion and 28-day mortality in patients after the exclusion of spontaneous bacterial peritonitis. Table S9: Multivariable Cox model with time-fixed and time-dependent covariates for 28-day mortality adding to the model the effect of albumin administration, weighted with marginal structural models. The analysis was repeated until reaching the highest level of serum albumin concentration, for which the albumin infusion still showed a positive effect on the outcome. Table S10: Multivariable Cox model with time-fixed and time-dependent covariates for 28-day mortality adding to the model the effect of albumin administration, weighted with marginal structural models. The analysis was repeated until reaching the lowest level of serum lactate concentration, for which the albumin infusion still showed a positive effect on the outcome. Table S11: Correlation between the types of albumin solutions administered and 28-day mortality as estimated by the MSCM. Figure S1: Directed acyclic graph (DAG) illustrating the potential actions of confounding covariates on the relation between the administration of albumin according to different albumin concentrations and clinical outcomes. Figure S2: Correlation matrix for time-fixed covariates. Figure S3: Correlation matrix for time-dependent covariates. Figure S4: Variable selection for Cox time-dependent and time-independent model factors associated with 28-day mortality. Figure S5: Schematic illustrations of the sub-cohort establishment. Figure S6: Expanded Kaplan–Meier survival analysis, weighted by marginal structural models. Figure S7: Distribution of inverse probability weight in albumin and non-albumin groups. Figure S8: Adjusted risk of death at 28 days measured by Marginal Structural Cox proportional hazards Model according to baseline subgroups.
Acknowledgements
None.
Abbreviations
- SBP
Spontaneous bacterial peritonitis
- MELD
Model for End-Stage Liver Disease
- HAS
Human albumin solution
- MSCM
Marginal Structural Cox proportional hazards Model
- IPW
Inverse probability weighting
- EHR
Electronic healthcare record
- GCS
Glasgow Coma Scale
- HR
Hazard ratio
- CI
Confidence interval
- ICD
International Classification of Diseases
- ICU
Intensive care unit
- IQR
Interquartile range
- IRB
Institutional review board
- MIMIC-IV
Medical Information Mart for Intensive Care IV
- PaCO2
Partial pressure of carbon dioxide
- PaO2
Arterial partial oxygen pressure
- RRT
Renal replacement therapy
- SOFA
Sequential Organ Failure Assessment
- MICE
Multiple imputations with chained equations
Author contributions
WHH and HC contributed equally to this work. WHH and HC designed the study, conducted the formal analysis, and drafted the manuscript. HC and CCM extracted the data from the MIMIC-IV database. QS, MCY, and JFX guided the manuscript review and editing. YZH instructed the conceptualization. All authors read and approved the final manuscript.
Funding
The present study was supported by the National Natural Science Foundation of China (81971812 and 82272235), Jiangsu Province Key Research and Development Program (Social Development) Special Project (BE2021734), National Key R&D Program of China (2022YFC2304600), and Science Foundation of the Commission of Health of Jiangsu Province (ZDB2020009).
Availability of data and materials
Data are available on reasonable request.
Declarations
Ethics approval and consent to participate
This study was an analysis of the third-party anonymized databases with pre-existing IRB approval.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wenhan Hu and Hui Chen have contributed equally to this work.
Contributor Information
Wenhan Hu, Email: huwenhan@126.com.
Hui Chen, Email: 15905162429@163.com.
Chencheng Ma, Email: machencheng3@163.com.
Qin Sun, Email: sunqin1990seu@126.com.
Meicheng Yang, Email: meicheng@seu.edu.cn.
Haofei Wang, Email: seu_wanghaofei@163.com.
Qingyun Peng, Email: pengqingyun928@126.com.
Jinlong Wang, Email: doctorwang2016@163.com.
Chen Zhang, Email: 15996273508@163.com.
Wei Huang, Email: huangw43@mail2.sysu.edu.cn.
Jianfeng Xie, Email: xie820405@126.com.
Yingzi Huang, Email: yz_huang@126.com.
References
- 1.Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, Angus DC, Reinhart K. Assessment of global incidence and mortality of hospital-treated sepsis current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–272. doi: 10.1164/rccm.201504-0781OC. [DOI] [PubMed] [Google Scholar]
- 2.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3) JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69(2):406–460. [DOI] [PubMed]
- 4.Simonetto DA, Piccolo Serafim L, Gallo de Moraes A, Gajic O, Kamath PS. Management of sepsis in patients with cirrhosis: current evidence and practical approach. Hepatology. 2019;70(1):418–428. doi: 10.1002/hep.30412. [DOI] [PubMed] [Google Scholar]
- 5.Vincent JL, De Backer D, Wiedermann CJ. Fluid management in sepsis: the potential beneficial effects of albumin. J Crit Care. 2016;35:161–167. doi: 10.1016/j.jcrc.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 6.Durand F, Kellum JA, Nadim MK. Fluid resuscitation in patients with cirrhosis and sepsis: a multidisciplinary perspective. J Hepatol. 2023;S0168–8278(23):00113–00117. doi: 10.1016/j.jhep.2023.02.024. [DOI] [PubMed] [Google Scholar]
- 7.Maiwall R, Kumar A, Pasupuleti SSR, Hidam AK, Tevethia H, Kumar G, Sahney A, Mitra LG, Sarin SK. A randomized-controlled trial comparing 20% albumin to plasmalyte in patients with cirrhosis and sepsis-induced hypotension [ALPS trial] J Hepatol. 2022;77(3):670–682. doi: 10.1016/j.jhep.2022.03.043. [DOI] [PubMed] [Google Scholar]
- 8.Philips CA, Maiwall R, Sharma MK, Jindal A, Choudhury AK, Kumar G, Bhardwaj A, Mitra LG, Agarwal PM, Sarin SK. Comparison of 5% human albumin and normal saline for fluid resuscitation in sepsis induced hypotension among patients with cirrhosis (FRISC study): a randomized controlled trial. Hepatol Int. 2021;15(4):983–994. doi: 10.1007/s12072-021-10164-z. [DOI] [PubMed] [Google Scholar]
- 9.Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, McIntyre L, Ostermann M, Prescott HC, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–1247. doi: 10.1007/s00134-021-06506-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dubois MJ, Orellana-Jimenez C, Melot C, De Backer D, Berre J, Leeman M, Brimioulle S, Appoloni O, Creteur J, Vincent JL. Albumin administration improves organ function in critically ill hypoalbuminemic patients: a prospective, randomized, controlled, pilot study. Crit Care Med. 2006;34(10):2536–2540. doi: 10.1097/01.CCM.0000239119.57544.0C. [DOI] [PubMed] [Google Scholar]
- 11.Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg. 2003;237(3):319–334. doi: 10.1097/01.SLA.0000055547.93484.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, Fanizza C, Caspani L, Faenza S, Grasselli G, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med. 2014;370(15):1412–1421. doi: 10.1056/NEJMoa1305727. [DOI] [PubMed] [Google Scholar]
- 13.Johnson AEW, Bulgarelli L, Shen L, Gayles A, Shammout A, Horng S, Pollard TJ, Hao S, Moody B, Gow B, et al. MIMIC-IV, a freely accessible electronic health record dataset. Sci Data. 2023;10(1):1. doi: 10.1038/s41597-022-01899-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reyna MA, Josef CS, Jeter R, Shashikumar SP, Westover MB, Nemati S, Clifford GD, Sharma A. Early prediction of sepsis from clinical data: the physionet/computing in cardiology challenge 2019. Crit Care Med. 2020;48(2):210–217. doi: 10.1097/CCM.0000000000004145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang M, Liu C, Wang X, Li Y, Gao H, Liu X, Li J. An explainable artificial intelligence predictor for early detection of sepsis. Crit Care Med. 2020;48(11):e1091–e1096. doi: 10.1097/CCM.0000000000004550. [DOI] [PubMed] [Google Scholar]
- 16.Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sørensen HT, von Elm E, Langan SM. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Townsend SR, Phillips GS, Duseja R, Tefera L, Cruikshank D, Dickerson R, Nguyen HB, Schorr CA, Levy MM, Dellinger RP, et al. Effects of compliance with the early management bundle (SEP-1) on mortality changes among medicare beneficiaries with sepsis: a propensity score matched cohort study. Chest. 2022;161(2):392–406. doi: 10.1016/j.chest.2021.07.2167. [DOI] [PubMed] [Google Scholar]
- 18.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–184. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Z, Ho KM, Hong Y. Machine learning for the prediction of volume responsiveness in patients with oliguric acute kidney injury in critical care. Crit Care. 2019;23(1):112. doi: 10.1186/s13054-019-2411-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4(2):30. doi: 10.3978/j.issn.2305-5839.2015.12.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van der Wal WM, Geskus RB. ipw: an r package for inverse probability weighting. J Stat Softw. 2011;43(13):1–23. doi: 10.18637/jss.v043.i13. [DOI] [Google Scholar]
- 22.Snapinn SM, Jiang Q, Iglewicz B. Illustrating the impact of a time-varying covariate with an extended Kaplan-Meier estimator. Am Stat. 2005;59(4):301–307. doi: 10.1198/000313005X70371. [DOI] [Google Scholar]
- 23.David G, Kleinbaum MK. Survival analysis: a self-learning text. 3. New York: Springer; 2012. [Google Scholar]
- 24.Martucci G, Schmidt M, Agerstrand C, Tabatabai A, Tuzzolino F, Giani M, Ramanan R, Grasselli G, Schellongowski P, Riera J, et al. Transfusion practice in patients receiving VV ECMO (PROTECMO): a prospective, multicentre, observational study. Lancet Respir Med. 2023;11(3):245–255. doi: 10.1016/S2213-2600(22)00353-8. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Z, Reinikainen J, Adeleke KA, Pieterse ME, Groothuis-Oudshoorn CGM. Time-varying covariates and coefficients in Cox regression models. Ann Transl Med. 2018;6(7):121. doi: 10.21037/atm.2018.02.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350(22):2247–2256. doi: 10.1056/NEJMoa040232. [DOI] [PubMed] [Google Scholar]
- 27.Schwager E, Jansson K, Rahman A, Schiffer S, Chang Y, Boverman G, Gross B, Xu-Wilson M, Boehme P, Truebel H, et al. Utilizing machine learning to improve clinical trial design for acute respiratory distress syndrome. NPJ Digit Med. 2021;4(1):133. doi: 10.1038/s41746-021-00505-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arroyo V, García-Martinez R, Salvatella X. Human serum albumin, systemic inflammation, and cirrhosis. J Hepatol. 2014;61(2):396–407. doi: 10.1016/j.jhep.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Fernández J, Clària J, Amorós A, Aguilar F, Castro M, Casulleras M, Acevedo J, Duran-Güell M, Nuñez L, Costa M, et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019;157(1):149–162. doi: 10.1053/j.gastro.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 30.Fernández J, Angeli P, Trebicka J, Merli M, Gustot T, Alessandria C, Aagaard NK, de Gottardi A, Welzel TM, Gerbes A, et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020;18(4):963–973.e914. doi: 10.1016/j.cgh.2019.07.055. [DOI] [PubMed] [Google Scholar]
- 31.Guevara M, Terra C, Nazar A, Solà E, Fernández J, Pavesi M, Arroyo V, Ginès P. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012;57(4):759–765. doi: 10.1016/j.jhep.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 32.Thévenot T, Bureau C, Oberti F, Anty R, Louvet A, Plessier A, Rudler M, Heurgué-Berlot A, Rosa I, Talbodec N, et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015;62(4):822–830. doi: 10.1016/j.jhep.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 33.Caramelo C, Fernandez-Muñoz D, Santos JC, Blanchart A, Rodriguez-Puyol D, López-Novoa JM, Hernando L. Effect of volume expansion on hemodynamics, capillary permeability and renal function in conscious, cirrhotic rats. Hepatology. 1986;6(1):129–134. doi: 10.1002/hep.1840060125. [DOI] [PubMed] [Google Scholar]
- 34.Ellman H. Capillary permeability in septic patients. Crit Care Med. 1984;12(8):629–633. doi: 10.1097/00003246-198408000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Ribera J, Pauta M, Melgar-Lesmes P, Tugues S, Fernández-Varo G, Held KF, Soria G, Tudela R, Planas AM, Fernández-Hernando C, et al. Increased nitric oxide production in lymphatic endothelial cells causes impairment of lymphatic drainage in cirrhotic rats. Gut. 2013;62(1):138–145. doi: 10.1136/gutjnl-2011-300703. [DOI] [PubMed] [Google Scholar]
- 36.Kumar R, Kumar S, Lata S. Albumin infusion may deleteriously promote extracellular fluid overload without improving circulating hypovolemia in patients of advanced cirrhosis with diabetes mellitus and sepsis. Med Hypotheses. 2013;80(4):452–455. doi: 10.1016/j.mehy.2012.12.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Additional method. Table S1: Selection strategy for variables with multiple measurements. Table S2: Infection category codes from ICD-9-CM to ICD-10-CM. Table S3: Missing rate for demographics and clinical variables extracted from the database during the observation period. Table S4: Missing rate for demographics and clinical variables extracted from the database on the first day. Table S5: Thresholds for clinical variables as albumin therapy indication. Table S6: Multivariable Cox model with time-fixed and time-dependent covariates for 28-day mortality adding to the model the effect of albumin administration, weighted with marginal structural models. Table S7: Association between albumin administration and 28-day mortality estimated by extended Cox regression model with time-varying covariates. Table S8: Univariate and multivariate analyses weighted with MSCM of the association between albumin infusion and 28-day mortality in patients after the exclusion of spontaneous bacterial peritonitis. Table S9: Multivariable Cox model with time-fixed and time-dependent covariates for 28-day mortality adding to the model the effect of albumin administration, weighted with marginal structural models. The analysis was repeated until reaching the highest level of serum albumin concentration, for which the albumin infusion still showed a positive effect on the outcome. Table S10: Multivariable Cox model with time-fixed and time-dependent covariates for 28-day mortality adding to the model the effect of albumin administration, weighted with marginal structural models. The analysis was repeated until reaching the lowest level of serum lactate concentration, for which the albumin infusion still showed a positive effect on the outcome. Table S11: Correlation between the types of albumin solutions administered and 28-day mortality as estimated by the MSCM. Figure S1: Directed acyclic graph (DAG) illustrating the potential actions of confounding covariates on the relation between the administration of albumin according to different albumin concentrations and clinical outcomes. Figure S2: Correlation matrix for time-fixed covariates. Figure S3: Correlation matrix for time-dependent covariates. Figure S4: Variable selection for Cox time-dependent and time-independent model factors associated with 28-day mortality. Figure S5: Schematic illustrations of the sub-cohort establishment. Figure S6: Expanded Kaplan–Meier survival analysis, weighted by marginal structural models. Figure S7: Distribution of inverse probability weight in albumin and non-albumin groups. Figure S8: Adjusted risk of death at 28 days measured by Marginal Structural Cox proportional hazards Model according to baseline subgroups.
Data Availability Statement
Data are available on reasonable request.