Abstract
Background
Bipolar hemiarthroplasty is the standard of care for transcervical fracture in the elderly. Stainless steel being cheaper is preferred over titanium in developing nations for implants and prostheses. This study was conducted for assessing the short-term outcomes of uncemented bipolar hemiarthroplasty done using hydroxyapatite-coated stainless steel prosthesis.
Methods
Sixty-five patients, >60 year of age operated between 2018 and 2020 at tertiary care centre with stainless steel (316L) completely coated with hydroxyapatite bipolar hemiarthroplasty implants were retrospectively followed up. Radiological outcomes were assessed based on pedestal formation, stem position, radiological limb length discrepancy, sinkage of stem, spot welds and stress shielding. Clinical and functional outcomes were assessed based on mean Harris Hip score.
Results
Mean Harris Hip score at baseline, 3-week follow-up, 6-week follow-up, 3-month follow-up and 1-year follow-up was 45.9 (SD 2.5), 63.2 (SD 6.5), 75.1 (SD 9.9), 83.9 (SD 9.8) and 87.1 (SD 9.9), respectively. Excellent, good, fair, poor results were seen in 32.31, 40, 18.46, 9.23 of the patients, respectively. Valgus, central and varus stem position was seen in 49.23, 40, 10.77 percent of the patients, respectively. Pedestal formation, radiological limb length discrepancy, sinkage, spot welds, stress shielding was seen in 6.15, 32.31, 3.07, 53.85, 40 percent of the patients, respectively.
Conclusion
Short-term outcomes of this study provides evidence that using a more affordable fully hydroxyapatite-coated stainless steel prosthesis for uncemented bipolar hemiarthroplasty is an appropriate treatment option for the transcervical femur fracture.
Keywords: Uncemented, Bipolar hemiarthroplasty, Stainless steel, Hydroxyapatite, Pedestal, Spot welds
Introduction
Femur neck fractures are chief contributors to morbidity and mortality in elderly patients. These fractures are notorious due to non-union because of fracture anatomy (intracapsular fracture) and trauma to blood vessels supplying the femoral head. Management of transcervical femur fractures in the elderly has been a topic of controversy [1]. Surgical treatment is the established gold standard; exact surgical procedure depends on various factors, most importantly, being the age. Although fixation is an option in young patients, hemiarthroplasty is the most viable option in elderly patients as it allows immediate weight bearing, return to activity, and reduced chance of reoperation as compared to fixation. Bipolar hemiarthroplasty, either cemented or uncemented, is the standard of care for the elderly [1]. The decision of cementing depends on canal dimensions according to Dorr’s ratio. Cementing carries the risk of cement reaction leading to hemodynamic and cardiopulmonary complications. An uncemented prosthesis has been said to have a longer lifespan due to intrinsic bony ingrowth, which provides a long-lasting fixation in comparison to fixation by bone–cement–metal bond, which tends to loosen. Stainless steel (SS) 316L is one of the biomaterials that has been used as an implant material due to its corrosion resistance, better biocompatibility, and excellent mechanical properties. However, research conducted on recovered implants from unsuccessful cases indicated that over 90% of the instances where 316L SS-implants failed was caused by localized electrochemical cells that led to either pitting corrosion or crevice corrosion. The corrosion products that arise from this process can trigger a nearby inflammatory reaction, which ultimately culminates in the termination of bone growth, synovitis, and the dislodgement of implants. As a result, it is necessary to improve the corrosion resistance of the implants. One common method to achieve this is by applying hydroxyapatite (HA) coatings onto the implants. The gradual improvement in the implants’ resistance to corrosion that occurs after applying HA coating is due to the non-reactive nature of HA, which is a ceramic material. Consequently, the HA coating acts as a barrier, preventing the release of ions from the substrate and providing effective protection against a corrosive environment [2].
During the late 1970s, porous coatings were introduced to the surfaces of implants to assist with osteointegration. However, it was observed that there was a higher occurrence of thigh pain, shedding of beads, and dislodgement of implants. Additionally, the process of osteointegration with these coatings was lengthy, and the surgical technique required was demanding [3]. The quest for a coating that could improve the osseointegration of implants continued and ultimately led to a heightened interest in calcium phosphate ceramic. Amongst the calcium phosphate ceramics, Hydroxyapatite (HA) was preferred because of its chemical properties and its prominence as a major constituent of bone mineral content. The Leiden Biomaterials Research Group’s Gloot and Geesing [4] were pioneers in using HA as an osteoconductive material in orthopaedics to enhance osseointegration of implants, leading to better long-term survival rates. Currently, HA-coated implants have been utilized for almost 30 years, yielding outstanding outcomes. Multiple studies regarding outcomes of uncemented hemiarthroplasty using titanium HA-coated implants have been done and are available in the literature, but there are very few documented studies in literature where fully coated stainless steel implants are used for uncemented bipolar hemiarthroplasty [1, 5, 6]. A study mentioned better osteointegration using HA-coated titanium implants as compared to HA-coated stainless steel implants [6]. Stainless steel being cheaper, is preferred over titanium in developing nations for implants and prostheses. Hence, in light of the above-mentioned data, the present study was conducted with the aim of assessing the short-term clinical and radiological outcomes of uncemented bipolar hemiarthroplasty done using HA-coated stainless steel implants.
Materials and Methods
Study Design
Retrospective Cohort Study
Study Size
Target population was patients with transcervical fracture of femur presented to us between March 2018 and March 2020 at a tertiary care centre. 110 patients presented to us during the specified time period. 86 patients satisfied all the inclusion criteria’s, gave consent and were included in the study. All patients presented to emergency department were attended by a senior resident and later on admitted in the ward. Surgery was planned for the earliest slot according to anaesthesia fitness. 21 of them lost follow-up after surgery due to death. Therefore, 65 patients completed the follow-up. We also used the formula for sample size for before–after study (using the paired T-test) [2] to calculate the number of patients to be included for our study.
The sample size was also calculated based on a similar study conducted by Figved et al. [5] that compared the Harris Hip Score (HHS) after 12 months in patients treated with cemented or uncemented bipolar hemiarthroplasties in displaced femoral neck fractures. At baseline, the mean ± SD HHS for the uncemented group was 84.6 ± 15.1 while that at 3 months was 72.1 ± 19.7.
Also considering, type I error (two-tailed) = 0.05; type II error = 0.2; effect size = 0.83 and standard deviation = 3.02, we calculated a sample size of 65 patients.
Formula:
The standard normal deviate for
The standard normal deviate for
Setting
After complete informed consent and ethics committee clearance, a study was started. 86 postoperative patients of more than 60 years of age with transcervical fracture of femoral neck managed with uncemented bipolar hemiarthroplasty using fully HA-coated stainless steel prosthesis between March 2018 and March 2020 were included. Femoral bone quality lying within Dorr Type A, Type B and Type C (depending on intra-operative findings) were retrospectively observed over a period of 1 year in a tertiary medical centre. Patients with pathological transcervical fracture of femur, with associated skeletal abnormalities, with lower life expectancy because of some chronic ailment and patients in which the same proximal femur was previously operated on which led to poor osteointegration were excluded from the study. All the patients were operated in a tertiary medical centre by the same team of surgeons with a standard posterior approach. Stainless steel (316L) completely HA-coated stem by Orthotech India was used. Post-op physiotherapy was done under supervision of same group of physiotherapists for each patient. Quadriceps, glutei and hamstring strengthening was emphasised mainly and weight bearing was allowed only after strengthening the quadriceps such that there was no extension lag. All patients started full weight bearing mobilisation within a week of surgery. All the patients were co-operative with physiotherapy.
Patients were followed up in OPD at 3 weeks, 6 weeks, 3 month, 6 months and 1 year for assessing outcomes.
Participants
Inclusion Criteria:
All post-operative patients of transcervical fracture of femur managed with uncemented bipolar hemiarthroplasty using fully HA-coated stainless steel prosthesis between March 2018 and March 2020.
Age of the patient >60 years.
Patients with femoral bone quality lying within Dorr Type A, Type B and Type C (depending on intra-operative findings).
Exclusion Criteria:
Patients with pathological transcervical fracture of femur.
Patients with associated skeletal abnormalities.
Patients with lower than normal life expectancy because of chronic ailments (e.g. cancer).
Patients in which the same proximal femur was previously operated on which led to poor osteointegration.
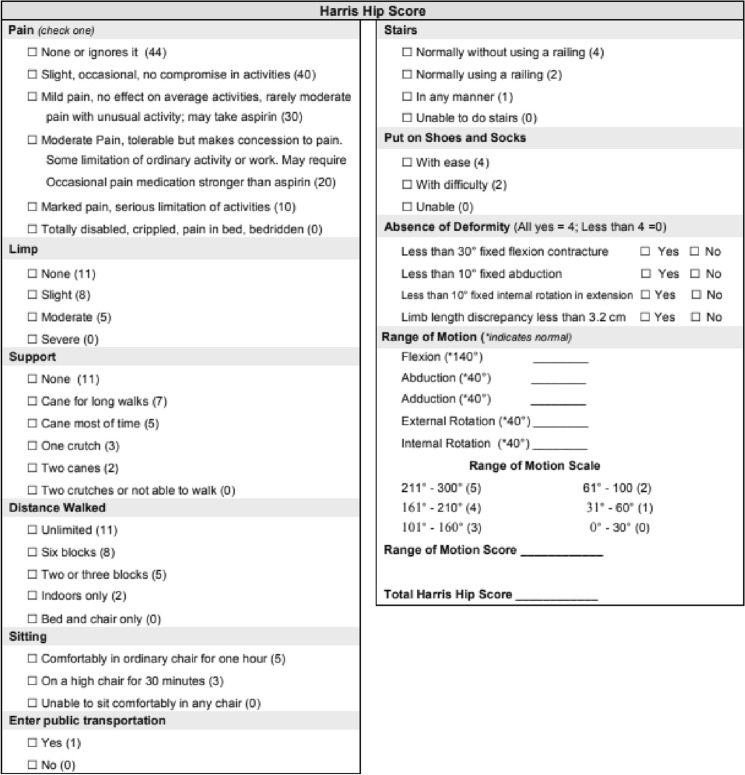
Data collection was done on admission of patient as well as in follow-up visits as per the case record form. Clinical outcome was assessed by mean Harris Hip Score (HHS) [7, 8] which is a dependent variable in our study. HHS was developed for the assessment of the outcomes of hip surgeries. It was devised in 1969 by Harris WH. There are ten items covering four domains. The domains are pain, function, absence of deformity, and range of motion (Fig. 1). Patients were followed up in OPD at 3 weeks, 6 weeks, 3 month, 6 months and 1 year for assessing outcomes.
Fig. 1.
Questionnaire for calculating HHS
(source: https://www.scribd.com/document/368551978/Harris-Hip-Score-pdf)
The radiological outcome was assessed by authors (Orthopaedic surgeons) by doing repeated radiological assessment postoperatively at 3 weeks, 6 weeks, 3 months, 6 months and 1 year thereafter for assessing outcomes. All the radiological parameters considered were dependent variables in our study. The following parameters were considered:
Pedestal formation: the formation of sclerosis at the distal end of an uncemented femoral component, spanning across the medullary canal, is known as a bone pedestal. The relationship between this frequently discovered phenomenon and the dislodgement of the femoral component is uncertain.
Stem position: ideally, the position of the femoral stem on an AP view should be seen in line with the anatomical axis of the femoral shaft and the tip of the stem should be in the centre of the shaft. Valgus position of the stem is still acceptable. Numerous research works have indicated that improper placement of the femoral stem in varus malalignment results in stem failure, although it does not affect cases of uncemented stems.
Radiological limb length discrepancy: the radiological limb length discrepancy is measured by drawing a transverse line connecting the inferior borders of the acetabular teardrops, the pelvic reference line. The lesser trochanters are used as the femoral reference points. Perpendicular lines are drawn from the pelvic reference line to the femoral reference points; the difference between the distances is the leg length discrepancy. Limb length discrepancy is common after hip replacement; an allowance of around 1 cm discrepancy is generally acceptable. Mild to moderate differences can typically be addressed through the use of a shoe orthotic.
Sinkage of stem: quantified with radiological subsidence seen on follow-up X-rays.
Spot welds/integration of stem: the process of spot welding involves the growth of fresh bone from the innermost surface towards the prosthesis, and is predominantly observed in uncemented femoral stems. This is a robust indication of stability and generally negates any concerns regarding instability.
Stress shielding: stress shielding is the phenomenon whereby the natural load on the femoral neck and intertrochanteric region is diverted towards the proximal femoral diaphysis due to the impact of the hip implant on mechanical forces. This typically leads to bone loss on the lateral side of the proximal femur, which is most frequently observed in Gruen zone 1, while bone hypertrophy occurs on the medial side of the proximal femur. This process signifies stability and should not be misinterpreted as a sign of instability.
Bias
All the patients were operated in a tertiary medical centre by the same team of surgeons with a standard posterior approach.
Statistical Method
The findings were documented in a Microsoft Excel spreadsheet and subsequently scrutinized using SPSS software. To determine their level of significance, statistical tests such as the Chi-square, Student t-test, and ANOVA were conducted.
Data collection was done according to all the parameters as mentioned in Table 2 at the time of surgery, discharge and in subsequent follow-up visits by authors.
Table 2.
Comparison of our results for some parameters with results of studies done by other authors—Azeem et al. [9], Bashir et al. [10], Kumar et al. [11]
| Parameter | Our study | Azeem et al. | Bashir et al. | Kumar et al. |
|---|---|---|---|---|
| Age (year) (mean) | 72.5 | 70 | 67.1 | – |
| Gender (percent) | ||||
| Male | 36.2 | 24.62 | 40 | 40 |
| Female | 63.8 | 75.38 | 60 | 60 |
| Mode of injury | ||||
| Trivial fall | 92.31 | 82.5 | 90 | 70 |
| Type of fracture | – | |||
| Garden IV | 49.23 | 61.9 | 60 | |
| Mean duration of surgery (min) | 88.5 | 54 | 130.6 | – |
| Mean blood loss (ml) | 193.2 | 300 | 256.33 | – |
| Mean hospital stay (days) | 13.2 | – | 13.7 | – |
| Mean HHS at final follow-up | 87.1 | – | 88.97 | – |
Results
24.44 percent of patients (21 patients) lost follow-up because of death. This study contains data from only those patients who could follow-up for a minimum of 1 year. Of the 21 patients who died postoperatively within 1 year, eight died in 6 months; six died between 6 and 8 months, and seven died between 8 and 11 months. All the patients died of causes not related to surgery. Of all the patients who died, 85.71 percent of patients were with associated comorbidities.
38.4 percent of the patients were of the age group of more than 75 years. 30.77 percent of the patients belonged to the age group of 71–75 years. The mean age of the patients was 72.5 years. 63.08 percent of the patients were females, while the remaining 36.92 percent were males. In 56.92 percent of the patients, the left side was involved, while in the remaining 43.08 percent, the right side was involved. In 92.31 percent of the patients, the mode of injury was Trauma (slipping or tripping while in the remaining 7.63 percent; the mode of injury was a road traffic accident. In 49.23 percent of the patients, the type of fracture was Garden type IV, while in 30.77 percent of the patients, the type of fracture was Garden type III. Type I and type II fractures were seen in 7.69 percent and 12.31 percent of the patients, respectively. The mean duration of surgery was 88.5 ± 11.29 min. Mean blood loss in surgery was 193.2 ± 11.67 ml. The mean hospital stay was 13.2 ± 1.62 days.
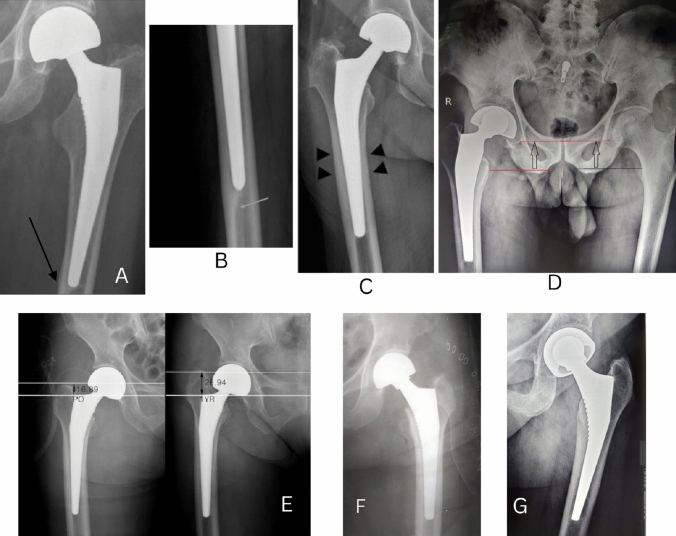
Mean Harris Hip score at baseline, 3 week follow-up, 6 week follow-up, 3 month follow-up, and 1-year follow-up was 45.9 (SD 2.5), 63.2 (SD 6.5), 75.1 (SD 9.9), 83.9 (SD 9.8) and 87.1 (SD 9.9), respectively. Significant results were obtained while comparing the mean Harris Hip score at different time intervals (Fig. 2).
Fig. 2.
Comparison of Harris Hip score at different follow-up
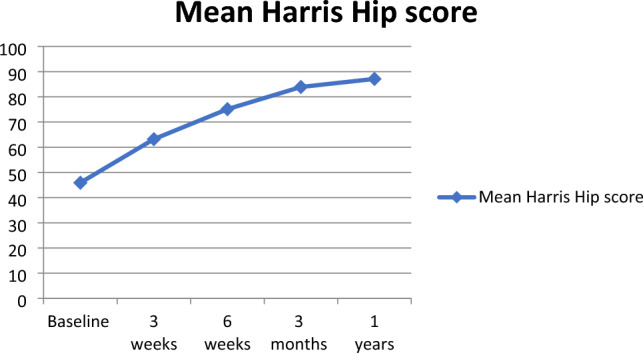
Excellent results were seen in 32.31 percent of the patients, while good results were seen in 40 percent of the patients. 18.46 percent of the patients showed fair results, while poor results were seen in 9.23 percent of the patients. Of the six patients with a poor score, five patients had associated comorbidities who could not follow physiotherapy protocols postoperatively. One patient suffered from a cerebrovascular event 1 month after the operative procedure (Fig. 3).
Fig. 3.
Outcome according to Harris Hip score at 1-year follow-up
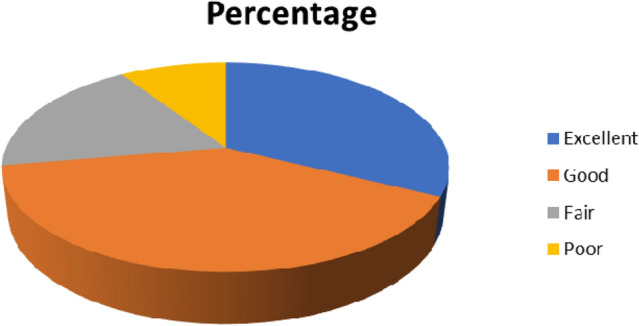
Superficial infection and loosening of the stem were seen in 1.54 percent of the patients, respectively. Limb length discrepancy was seen in 15.38 percent of the patients. Noticed clinical limb length discrepancy was less than 2.5 cm and was not significantly affecting the clinical outcome for all the patients. No cases of dislocation and periprosthetic fracture were noted in our study (Table 1; Fig. 4).
Table 1.
Radiological outcome
| Radiological outcome | Number of patients | Percentage |
|---|---|---|
| Pedestal formation | 4 | 6.15 |
| Stem position | ||
| Valgus | 32 | 49.23 |
| Central position | 26 | 40 |
| Varus | 7 | 10.77 |
| Radiological limb length discrepancy | 21 | 32.31 |
| Sinkage of stem | 2 | 3.07 |
| Spot welds/integration of stem | 35 | 53.85 |
| Stress shielding | 26 | 40 |
Fig. 4.
A Pedestal formation seen in 76-year-old female at 2-year postop, B pedestal formation, C endosteal bone formation in a 68-year-old female after 1-year post-op, D technique to determine radiological limb length discrepancy, E sinkage of the stem (subsidence)—quantified by measuring the distance from greater trochanter tip to fixed point on the stem, F, G immediate post-op X-ray of a 72-year-old female, 1-year post-op X-ray, showing stress shielding, thickened medial cortex and lucency seen towards the trochanteric area
Discussion
Bipolar hemiarthroplasty is the treatment of choice for transcervical femur fracture in elderly. Uncemented prosthesis are used in patients with good bone stock and in accordance with the Dorr’s ratio. Stainless steel implants are preferred in public health hospitals in developing countries due to affordability. We studied the outcomes of HA-coated stainless steel prostheses used for uncemented bipolar hemiarthroplasty. Our results were consistent with those achieved by prior researchers, who documented comparable results, as depicted in Table 2. Bipolar hemiarthroplasty using stainless steel fully HA-coated uncemented bipolar prosthesis for transcervical fracture of femur has a satisfactory outcome and more rapid return to pre-injury activity with an acceptable complication rate. The end functional results also depend on the associated comorbidity and optimum postoperative rehabilitation. The short-term outcome of this study provides evidence that using a more affordable fully HA-coated stainless steel prosthesis for uncemented bipolar hemiarthroplasty is an appropriate treatment option for the transcervical femur fracture especially in public health sector.
The incidence of transcervical fracture of femur is more common in the elderly female group. Females in their advanced age are at a higher risk of experiencing a femoral neck fracture owing to their diminished bone mineral density. Trivial trauma remains the main mode of injury in our study as well other studies by Azeem et al. [9], Bashir et al. [10] and Kumar et al. [11]. In 49.23 percent of the patients, the type of fracture was Garden type IV, while in 30.77 percent of the patients, the type of fracture was Garden type III. Type I and type II fractures were seen in 7.69 percent and 12.31 percent of the patients, respectively. The mean duration of surgery was 88.5 min. In the studies conducted by Calder et al. [12] and Blomfeldt et al. [13], the mean duration of hospital stay was 10.8 days and 11.4 days, respectively. Mean Harris Hip score at baseline, 3 week follow-up, 6 week follow-up, 3 month follow-up, and 1-year follow-up was 45.9, 63.2, 75.1, 83.9 and 87.1, respectively. Noteworthy outcomes were observed when assessing the average Harris Hip score across various time frames. In another study conducted by Bashir et al., the mean Harris Hip score at baseline and final follow-up were 32.93 and 88.97, respectively [10]. Mean Harris Hip scores at the final follow-up in the studies conducted by Narayan et al. [14] and Lestrange et al. [15] were 86.93 and 82.6, respectively. Excellent results were seen in 32.31 percent of the patients, while good results were seen in 40 percent of the patients. 18.46 percent of the patients showed fair results, while poor results were seen in 9.23 percent of the patients. In a study conducted by Kumar et al. [11], excellent, good, fair and poor results were seen in 30 percent, 45 percent, 10 percent and 15 percent of the patients, respectively. Lestrange et al. [15], in another study, reported the presence of excellent, good, fair and poor results in 39.6 percent, 31.2 percent, 15.3 percent and 13.9 percent of the patients, respectively. Moshein et al. [16] reported excellent, good and poor results in 40 percent, 25 percent and 12 percent of the patients, respectively.
In a previous study conducted by Marya et al. [17], 29 patients with transcervical femur fractures who underwent cementless bipolar hemiarthroplasty were followed up over a 2-year period. Mean age was 83 years with range of 71–102 years. The average follow-up was 36 months with range of 26–49 months. The average duration of surgery and blood loss was 28 min with range being 20–50 min and 260 ml with range being 95–535 ml, respectively. The average blood transfusion was 1.4 units with range from 0 to 4 units. The mean duration of hospital stay was 11.9 days with range of 7–26 days. They had no perioperative events or deaths. Twenty-four patients were successfully followed till last follow-up of 36 months; with range being 26–49 months. All the patients were ambulatory and had no complaints of pain; the mean Harris Hip score was 85, range being 69–96. Uncemented bipolar hemiarthroplasty done to address transcervical femur fractures in elderly patients facilitates a prompt return to their pre-injury lifestyle and is not linked to any adverse cardiac events in the perioperative phase.
Pedestal formation was seen in 6.15 percent of the patients, which has an unclear association with loosening of the stem. Valgus stem position was seen in 49.23 percent, while central stem position was seen in 40 percent of the patients. Varus stem position was seen in 10.77 percent, which is acceptable in uncemented hemiarthroplasty with good stem integration. Radiological limb length discrepancy was seen in 32.31 percent of the patients, which was less than 2.5 cm in every case and did not affect clinical outcomes. Sinkage of the stem was seen in 3.07 percent of patients. Spot welds were seen in 53.85 percent of the patients. Stress shielding was seen in 40 percent of the patients. Both spot welds and stress shielding signifies the integration of stem. Superficial infection and loosening of the stem were seen in 1.54 percent of the patients, respectively. Limb length discrepancy was seen in 15.38 percent of the patients, which was less than 2.5 cm and did not affect clinical outcomes in all cases. Dislocation and periprosthetic fractures were not seen in our study. Azeem et al., in a similar study, reported dislocation of prosthesis, superficial infection, limb shortening and loosening of the stem in 3.1 percent, 4.6 percent, 9.2 percent and 4.6 percent of the patients, respectively. Bashir et al. reported hypotension, superficial infection, pressure sores, limb shortening and periprosthetic fracture as common complications [9, 10]. Sadiq et al. [18] assessed the outcome of transcervical femur fracture with bipolar hemiarthroplasty. The mean age of the subjects was 71.6 years, with 12 (34.28%) being male and 23 (65.71%) being female. The study’s conclusion involved a 1-year evaluation utilizing the Harris Hip score. Out of the 35 participants, 32 (91.43%) reported little to no pain, 31 (88.57%) had a mild to no limp, 29 (82.59%) used no aid or a single cane for walking, and 30 (85.71%) could walk unrestricted or for distances greater than 500 m. Between 161 and 300 degrees of motion was observed in 32 (91.43%) of the participants. The final Harris Hip Score ranged from 59 to 97, with an average score of 82.17. Of the participants, 9 (25.7%) achieved an excellent Harris Hip Score, 15 (42.9%) scored good, 7 (20%) rated fair, and 4 (11.4%) achieved a poor score. No noteworthy radiological irregularities were detected. The use of bipolar hemiarthroplasty resulted in improved motion range, effective pain relief, and a high level of mobility with minimal complications. As such, it was determined that bipolar hemiarthroplasty represents a viable approach for treating transcervical fracture of femur in elderly individuals.
24.44 percent of patients lost follow-up because of death. This study contains data from only those patients who could follow-up for a minimum of 1 year. Of the 21 patients who died postoperatively within 1 year, eight died in 6 months; six died between 6 and 8 months, and seven died between 8 and 11 months. All the patients died of causes not related to surgery. Of all the patients who died, 85.71 percent of patients were with associated comorbidities.
Our study successfully states that using stainless steel prosthesis is cost effective as well as durable option for bipolar hemiarthroplasty and this technique can be practiced in public health sector in developing nations.
Limitations of the study
Small sample size to start with and attrition due to death of 21 patients is one of the limitation. A prospective randomised controlled study would have given results with more statistical significance. Also, multicentric study instead of carrying it out at a single tertiary care centre would have been better.
Strength of the study
All the patients were operated by same surgical team and followed up by them which minimised interobserver error. Outcomes of fully HA-coated stainless steel prosthesis used for uncemented bipolar hemiarthroplasty were not studied previously by many researchers making our study impactful.
Acknowledgements
We have not received any external funding for the research underlying our paper, so there is no funding body we could acknowledge.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Nikhil G. Karwande. The first draft of the manuscript was written by Nikhil G. Karwande and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Principal author—Nikhil G. Karwande: data curation, writing—original draft preparation, writing—reviewing and editing. Co-authors—Shaligram S. Purohit: conceptualization, methodology, supervision. Shivaprasad S. Kolur: visualization. Animesh S. Sawarbandhe: software, validation. Sahil S. Lombar: investigation. Shubham Dakhode: formal analysis.
Data Availability
All data supporting the findings of this study are available within the paper and its supplementary information.
Declarations
Conflict of interest
There are no conflict of interest between the authors. No funding was received to assist with the preparation of this manuscript. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. Informed consent was obtained from all individual participants included in the study. The participants have consented to the submission of the study to the journal.
Ethical approval
Study was started with complete informed consent from the patients and Institutional ethics committee approval. Approval letter number being IEC(2)/OUT/362/2021. The research has been carried out following the ethical guidelines outlined in the 2013 Declaration of Helsinki.
Footnotes
The original online version of this article was revised: Correction to the name of Dr. Shivaprasad S. Kolur.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
7/24/2023
A Correction to this paper has been published: 10.1007/s43465-023-00957-9
References
- 1.Bezwada HP, Shah AR, Harding SH, Baker J, Johanson NA, Mont MA. Cementless bipolar hemiarthroplasty for displaced femoral neck fractures in the elderly. The Journal of Arthroplasty. 2004;19(7):73–77. doi: 10.1016/j.arth.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 2.Mhaede M, Ahmed A, Wollmann M, Wagner L. Evaluating the effects of hydroxyapatite coating on the corrosion behavior of severely deformed 316ti SS for surgical implants. Materials Science and Engineering C. 2015;50:24–30. doi: 10.1016/j.msec.2015.01.093. [DOI] [PubMed] [Google Scholar]
- 3.Camron HU, Pilliar RM, Macnab I. The rate of bone ingrowth into porous metal. Journal of Biomedical Materials Research. 1976;10(2):295–302. doi: 10.1002/jbm.820100210. [DOI] [PubMed] [Google Scholar]
- 4.Geesink RGT, De Groot K, Klein CPAT. Chemical implant fixation using hydroxyl-apatite coatings. Clinical Orthopaedics and Related Research. 1987;225:147–170. [PubMed] [Google Scholar]
- 5.Figved W, Opland V, Frihagen F, Jervidalo T, Madsen JE, Nordsletten L. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clinical Orthopaedics and Related Research. 2009;467(9):2426–2435. doi: 10.1007/s11999-008-0672-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Popkov D, Popkov AV, Gorbach EN, Kononovich NA, Tverdokhlebov SI, Shesterikov EV. Bioactivity and osteointegration of hydroxyapatite-coated stainless steel and titanium wires used for intramedullary osteosynthesis. Strategies in Trauma and Limb Reconstruction. 2017;12(2):107–113. doi: 10.1007/s11751-017-0282-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris, WH. (1969). Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end‐result study using a new method of result evaluation. Journal of Bone and Joint Surgery, 51, 737–755. [PubMed]
- 8.Frihagen F, Grotle M, Madsen JE, Wyller TB, Mowinckel P, Nordsletten L. Outcome after femoral neck fractures: A comparison of Harris Hip Score, Eq-5d and Barthel Index. Injury. 2008;39:1147–1156. doi: 10.1016/j.injury.2008.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Azeem MA, Rajkumar K. Bipolar hemi-arthroplasty (uncemented) in the elderly: A study in a tertiary care hospital. Indian Journal of Orthopaedics Surgery. 2016;2(4):415–419. [Google Scholar]
- 10.Ringshawl, Z. Y., Bashir, Z. (2020). Functional outcome of uncemented modular bipolar hemiarthroplasty using modified Harris hip score for fractures of femoral neck in elderly patients. Journal of Medical Science and Clinical Research, 08(09).
- 11.Kumar RK. Prospective study of hemiarthroplasty for intracapsular fracture neck of femur using modular bipolar prosthesis. International Journal of Orthopaedics Sciences. 2018;4(4):92–95. doi: 10.22271/ortho.2018.v4.i4b.20. [DOI] [Google Scholar]
- 12.Calder J. Evolution of hip hemiarthroplasty. Annales Chirurgiae et Gynaecologiae. 1996;71:103. [Google Scholar]
- 13.Blomfeldt, R., Törnkvist, H., Eriksson, K., Söderqvist, A., Ponzer, S., Tidermark, J. (2007). A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. The Journal of Bone and Joint Surgery British Volume, 89-B(2), 160–165. [DOI] [PubMed]
- 14.Narayan KK, George T. Functional outcome of fracture neck of femur treated with total hip replacement versus bipolar arthroplasty in a South Asian population. Archives of Orthopaedic and Trauma Surgery. 2006;126(8):545–548. doi: 10.1007/s00402-006-0182-x. [DOI] [PubMed] [Google Scholar]
- 15.Lestrange NR. Bipolar arthroplasty for 496 hip fractures. Clinical Orthopaedics and Related Research. 1990;251:7–19. doi: 10.1097/00003086-199002000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Moshein J, Alter AH, Elconin KB, Adams WW, Isaacson J. Transcervical fractures of the hip treated with the Bateman bipolar prosthesis. Clinical Orthopaedics and Related Research. 1990;251:48–53. doi: 10.1097/00003086-199002000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Marya SK, Thukral R, Hasan R, Tripathi M. Cementless bipolar hemiarthroplasty in femoral neck fractures in elderly. Indian Journal of Orthopaedics. 2011;45(3):236–242. doi: 10.4103/0019-5413.80042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sadiq M, Mohammed Nayeemuddin DM. A study of intracapsular fracture neck femur treated with bipolar prosthesis. European Journal of Molecular & Clinical Medicine. 2021;7(11):8894–8902. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data supporting the findings of this study are available within the paper and its supplementary information.