Abstract
The use of radiological images is widespread in the emergency department (ED) as physicians commonly rely on them during initial evaluations to confirm diagnoses, contributing to prolonged waiting times. This study aimed to determine the relationship between commonly gathered triage data and the need for radiological imaging. Data were collected from electronic charts that contained routinely collected hospital data at the time of triage in the King Abdulaziz Medical City (KAMC) in Riyadh ED. The binary logistic regression results demonstrated a statistically significant relationship between age and radiological imaging ordered in the ED. Each one-unit increase in age corresponded to a 0.983-fold increase in the likelihood of ordering radiological imaging (odds ratio: 0.983, 95% confidence interval: 0.972-0.995, p = 0.004). In contrast, hypertension, diabetes, and heart failure were independent predictors of the need for radiological imaging in the ED (p >0.05). Patient data that are immediately available during ED triage can be used to predict the need for radiological imaging during ED visits. Such models can identify patients who may require radiological imaging during ED visits and expedite patient disposition.
Keywords: hospital stay, emergency evaluation, radiological image, triage data, emergency department
Introduction
The utilization of imaging techniques, particularly CT scans, has witnessed a significant rise in the emergency department (ED) in recent years. The primary reason for this surge is the ability of CT scans to effectively confirm or exclude a diagnosis [1-2]. However, the use of these advanced radiological studies is associated with increased ED stay lengths [3-4]. Moreover, ED crowding increases mortality rates in patients [5-6]. Therefore, the development of a physician triage model aimed at improving ED performance by expediting workups while patients are in the waiting area may contribute to decreasing the length of stay and allow ER physicians to see more patients promptly [7]. Such a model can also reduce physician-related factors that were found to play a crucial role in selecting the type of imaging study in the ED [8].
In many cases, radiographic imaging is required for the rapid diagnosis and management of life-threatening diseases. This method is commonly used to establish the disease process and finalize the diagnosis of large groups of patients who present to the ED during their initial evaluations [9-10]. However, there are limited studies regarding the use of immediately available triage data, such as patient age, comorbidities, chief complaints, and number of ER visits, to predict the necessity of emergency imaging studies. The development of such a model can contribute to rapid and informed decisions regarding the need for imaging in the ED [10-11]. Therefore, this study aimed to investigate the relationship between commonly gathered triage data and the need for radiographic imaging in the King Abdulaziz Medical City (KAMC) in Riyadh ED. Discovering such a relationship could expedite the time between patient arrival and imaging studies, ultimately leading to a reduction in the ED length of stay.
Materials and methods
Study design
This retrospective electronic chart review study used hospital data that had been routinely collected at the time of triage to predict the possibility of admission to the ED.
Study setting and population
This study was approved by the King Abdullah Medical Research Center (KAIMRC) (reference number: RYD-23-419812-70139) and was conducted in the ED of the KAMC in Riyadh. This is the largest ED in the Middle East. The KAMC in Riyadh is a tertiary-care hospital and level I trauma center. The estimated annual number of adult ED visits at the KAMC in Riyadh is 200,000 patients. Ethical consent was not required for this study, as the research was based on data from an electronic medical system.
Study protocol
All adult patients who visited the KAMC in Riyadh ED between January 2018 and December 2019 were included (146,000 patients in total). Patients who were under 14 years old, absconded, triaged away, died on arrival at the ED, or were admitted directly to the general ward or intensive care unit were excluded. Patients with missing data were also excluded.
Patient record numbers were randomly collected using a computer program (the dplyr CRAN package in R, version 1.0.5). Data for each patient were extracted from the Hospital Clinical Information System (BestCare, version 2.0, Korea, ezCaretech), including the triage level determined according to the Canadian Triage and Acuity Scale (CTAS), age, sex, arrival mode, day of presentation, comorbidities, previous ED visits, and previous hospital admissions with the same complaints. All data were collected and coded using Microsoft Excel (Microsoft, Washington, USA). A sample size calculator was used to determine the sample sizes for both datasets at a 5% level (α = 0.01) [12]. The chosen confidence interval (CI) was 95%, the population size was 146,000, and the margin of error was 3%. Furthermore, an ideal sample size of 1,166 was used. The sample size for the derivation dataset was 696 patients (60% of the total sample) while that for the validation dataset was 464 patients (40% of the total sample).
Statistical analysis
All analyses were performed using the SPSS Statistics version 26 (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp.). The normality of continuous variables was assessed using the Kolmogorov-Smirnov test. Continuous variables were reported as mean ± standard deviation, while categorical variables were reported as proportions. The chi-square test was used to compare categorical variables, and the independent sample t-test was used for continuous variables. Binary logistic regression was used to identify the relationship between the need for radiological imaging and the associated risk factors. Odds ratios (OR) and 95% CIs were also determined. Additionally, a decision tree analysis was performed. Statistical significance was defined at p <0.05.
Results
This study included 1,166 individuals, with a mean age of 46.09 ± 17.04 years. Women constituted a higher proportion (58.60%) than men did (41.40%). Among the participants, 89.60% were Saudi citizens. The previous year’s admissions accounted for 17.4% of the total (Table 1).
Table 1. Demographic characteristics of the individuals included in the study.
| Variables | Scale | Total (n=1166) n (%) |
| Age (years), mean±SD | 46.09±17.04 | |
| Gender | Male | 483(41.40) |
| Female | 683(58.60) | |
| Nationality | Saudi | 1045(89.60) |
| Non-Saudi | 61(10.40) | |
| Arrival mode | Ambulance | 82(7.00) |
| Referral | 3(0.30) | |
| Walk in | 1042(89.40) | |
| Triage level/patient acuity | I | 5(0.40) |
| II | 77(6.60) | |
| III | 541(46.40) | |
| IV | 399(34.20) | |
| V | 68(5.80) | |
| Need for radiological imaging | 630(54.00) | |
| Admissions in the past 1 year | 203(17.40) | |
| Result of visit | Admission | 221(19.00) |
| Discharge | 942(80.78) |
Regarding the need for radiological imaging, statistically significant differences were observed between the two groups in terms of age, sex, nationality, total admissions in the previous year, travel mode, triage level, and visit outcomes (p <0.05) (Table 2).
Table 2. Comparison between demographic characteristics and the need for radiological imaging in the ED.
| Variables | Scale | Need for radiological imaging | p-value | |
| Yes N (%) | No N (%) | |||
| Age (years), mean±SD | 47.37±21.55 | 39.32±16.18 | 0.001 | |
| Gender | Male | 280(58.00) | 203(42.00) | 0.023 |
| Female | 350(51.20) | 333(48.80) | ||
| Nationality | Saudi | 596(57.00) | 449(43.00) | 0.001 |
| Non-Saudi | 34(28.10) | 87(71.90) | ||
| Admission in the last 1 year | Yes | 128(63.10) | 75(36.90) | 0.010 |
| Arrival mode | Ambulance | 74(90.20) | 8(9.80) | 0.001 |
| Referral | 2(66.70) | 1(33.30) | ||
| Walk in | 541(51.90) | 501(48.10) | ||
| Triage level | 1 | 3(60.00) | 2(40.00) | 0.001 |
| 2 | 71(92.20) | 6(7.80) | ||
| 3 | 335(61.90) | 206(38.10) | ||
| 4 | 165(41.40) | 234(58.60) | ||
| 5 | 15(22.10) | 53(77.90) | ||
| Result of visit | Admission | 172(77.80) | 49(22.20) | 0.001 |
| Discharge | 456(48.40) | 486(51.60) | ||
The comparison of comorbidities in relation to the need for radiological imaging revealed a significant difference between the groups that needed radiological imaging and those that did not, particularly with respect to hypertension, diabetes, chronic obstructive pulmonary disease (COPD), and heart failure in the ED. The need for radiological imaging was significantly higher in patients with hypertension and diabetes (36% and 32.5%, respectively, p <0.05), whereas this need was lower in patients with COPD and asthma (1% and 5.4%, respectively) (Table 3).
Table 3. Comparison between comorbidities and the need for radiological imaging in the ED.
COPD, chronic obstructive pulmonary disease; DLP, dyslipidemia
| Variables | Scale | Need for radiological imaging | p-value | |
| Yes N (%) | No N (%) | |||
| Diabetic | Yes | 205(32.5) | 104(19.4) | 0.001 |
| No | 425(67.5) | 432(80.6) | ||
| Hypertension | Yes | 227(36) | 103(19.2) | 0.001 |
| No | 403(64) | 433(80.8) | ||
| COPD | Yes | 6(1.0) | 0(0) | 0.023 |
| No | 624(99) | 536(100) | ||
| Heart failure | Yes | 50(7.9) | 13 (2.4) | 0.001 |
| No | 580(92.1) | 523(97.6) | ||
| Asthma | Yes | 34(5.4) | 34(6.3) | 0.492 |
| No | 596(94.6) | 502(93.7) | ||
| DLP | Yes | 100(15.9) | 58(10.8) | 0.12 |
| No | 530(94.1) | 478(89.2) | ||
The comparison of chief complaints with the need for radiological imaging in the ED revealed a significant association between the need for radiological imaging and specific symptoms, including chest pain, fever, sore throat, and vaginal bleeding (p <0.05). Among the patients, 88.9% had chest pain, 66.2% had a fever, 17.9% had a sore throat, and 30.8% had vaginal bleeding requiring radiological imaging in the ED (Table 4).
Table 4. Comparison between chief complaints and the need for radiological imaging in the ED.
| Variables | Scale | Need for radiological imaging | p-value | |
| Yes N (%) | No N (%) | |||
| Chest pain | Yes | 64(88.9) | 8(11.1) | 0.001 |
| No | 566(51.7) | 528(48.3) | ||
| Back pain | Yes | 11(45.8) | 13(54.2) | 0.416 |
| No | 619(54.2) | 523(45.8) | ||
| Fever | Yes | 49(66.2) | 25(33.8) | 0.030 |
| No | 581(53.2) | 511(46.8) | ||
| Epigastric pain | Yes | 13(48.1) | 14 (51.9) | 0.535 |
| No | 617(54.2) | 522(45.8) | ||
| Sore throat | Yes | 7(17.9) | 32(82.1) | 0.001 |
| No | 623(55.3) | 504(44.7) | ||
| Vaginal bleeding | Yes | 8(30.8) | 18(69.2) | 0.016 |
| No | 622(54.6) | 518(45.4) | ||
| Palpitation | Yes | 7(41.2) | 10(58.8) | 0.284 |
| No | 623(54.2) | 526(45.8) | ||
The binary logistic regression results demonstrated a statistically significant relationship between age and radiological imaging ordered in the ED. For every one-unit increase in age (OR: 0.983, 95% CI: 0.972-0.995, p = 0.004), there was a 0.983-fold increase in the likelihood of radiological imaging being ordered in the ED. In contrast, hypertension, diabetes, and heart failure were independent predictors of the need for radiological imaging in the ED (p >0.05) (Table 5).
Table 5. Predictor variables for the need for radiological imaging based on the binary logistic regression results.
OR, odds ratio; CI, confidence interval
| Variable | OR | (95% CI) | p-value | |
| Age | 0.983 | (0.972-0.995) | 0.004 | |
| Hypertension | Yes | 1.286 | (0.755-2.192) | 0.354 |
| Diabetes | Yes | 1.116 | (0.684-1.820) | 0.661 |
| Heart failure | Yes | 0.534 | (0.273- 1.044) | 0.182 |
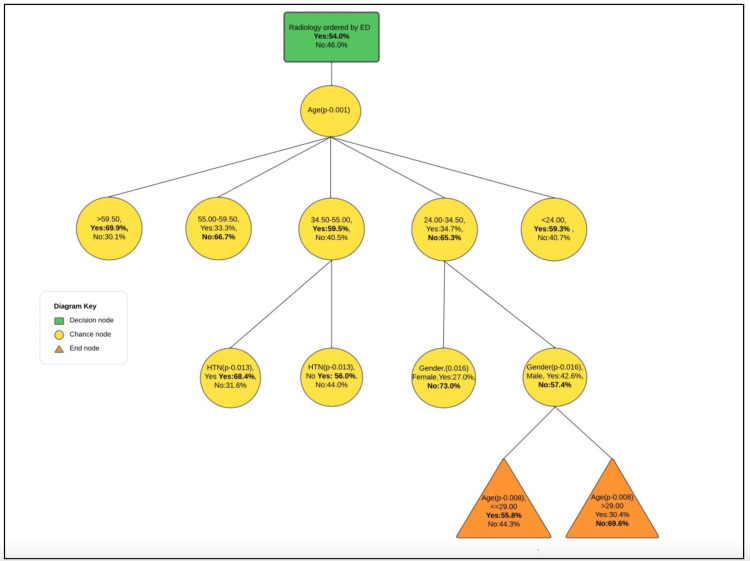
According to the decision tree analysis, age (p = 0.001, χ² = 84) was the most significant factor in determining the need for radiological imaging in the ED. As we examine the branches of the tree, we observe that hypertension became the next crucial factor for individuals aged 35.50-55.00 years who required radiological imaging (p = 0.013, χ² = 6), and sex was important for those aged 24.00-34.50 years. Notably, age was the most significant factor for men (Figure 1). The classification table summarizes the percentages of correct classification, indicating that the model correctly classified 85.90% of the individuals who required radiological imaging. However, it also indicates that 38.10% of those who did not require imaging were incorrectly classified. Overall, our predictions were accurate for 63.90% of the cases (Table 6).
Table 6. Classification results of the decision tree analysis.
Observed; underwent radiological imaging with hypertension and individuals aged 35.50-55.00
| Observed | Predicted | ||
| Yes | No | Percent correct | |
| Yes | 541 | 89 | 85.90% |
| No | 332 | 204 | 38.10% |
| Overall percentage | 74.90% | 25.10% | 63.90% |
Figure 1. Decision tree analysis diagram.
Discussion
In this study, data commonly provided by patients in the triage phase was used to predict the need for radiological imaging. By developing a decision tree diagram, we identified age as the most significant factor in determining the need for radiological imaging in the ED, followed by hypertension for those aged 35.50-55.00 years (p = 0.013, χ² = 6) and sex for those aged 24.00-34.50 years. Notably, age was the most significant factor for men. The decision tree, developed using administrative triage data collected during the initial interaction with the ED, proved to be a valuable tool for predicting outcomes. This predictive model has the potential to contribute to the reduction of length of stay and alleviate ED crowding. By assisting physicians in making rapid decisions regarding the need for radiological imaging, the model can expedite the diagnostic process and facilitate timely interventions.
Numerous efforts have been made to reduce the utilization of imaging in the ED. The National Council on Radiation Protection and Measurements [12] and the American College of Radiology have developed guidelines to help physicians in deciding the best radiological modality for each specific clinical case, thereby improving the quality of care [13]. However, these guidelines primarily depend on physician assessments. In our study, we aimed to expedite the process of predicting radiological needs using administrative triage data. Our findings align with other studies, indicating that as age increases, the likelihood of requiring radiological imaging also increases. Furthermore, our study revealed a higher likelihood of imaging needs among patients triaged as CTAS 1 and 2, compared to that in patients triaged as CTAS 3-5 [14-15].
This study had some limitations. First, this study was confined to a single center in a capital city for one year, which can make generalizing the results to other centers difficult. It is important to note that different hospitals may not have similar administrative triage data or electronic record systems during the triage phase. Second, the sample size used for developing the decision tree was limited due to the exclusion of data from absconded patients. This small sample size may impact the reliability and generalizability of the results. Third, the study did not investigate the specific reasons for patients needing imaging or differentiate between different types of radiological imaging. Fourth, as a retrospective study, there is a possibility of selection bias and unmeasured confounding factors that were not accounted for. Lastly, the study was unable to determine whether patients were offered radiological imaging and whether they accepted or refused.
Conclusions
In this study, we developed a decision tree diagram to help predict the eventual use of radiological imaging using only the information gathered during ED triaging, including patients’ demographic data, general medical information, and chief complaints. We found out that age is the most significant factor followed by hypertension. This decision tree can aid in predicting the need for radiological imaging, allowing for timely referral to the radiology department and potentially reducing ED waiting times.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Diagnostic imaging trends in the emergency department: an extensive single-center experience. Juliusson G, Thorvaldsdottir B, Kristjansson JM, Hannesson P. Acta Radiol Open. 2019;8:2058460119860404. doi: 10.1177/2058460119860404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CT in the emergency department: a real-time study of changes in physician decision making. Pandharipande PV, Reisner AT, Binder WD, et al. Radiology. 2016;278:812–821. doi: 10.1148/radiol.2015150473. [DOI] [PubMed] [Google Scholar]
- 3.Long length of stay at the emergency department is mostly caused by organisational factors outside the influence of the emergency department: a root cause analysis. Driesen BE, van Riet BH, Verkerk L, Bonjer HJ, Merten H, Nanayakkara PW. PLoS One. 2018;13:0. doi: 10.1371/journal.pone.0202751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Length of stay in the emergency department and its associated factors at Jimma Medical Center, Southwest Ethiopia. Ahmed AA, Ibro SA, Melkamu G, Seid SS, Tesfaye T. Open Access Emerg Med. 2020;12:227–235. doi: 10.2147/OAEM.S254239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The effect of emergency department crowding on clinically oriented outcomes. Bernstein SL, Aronsky D, Duseja R, et al. Acad Emerg Med. 2009;16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 6.Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the emergency department. Olshaker JS, Rathlev NK. J Emerg Med. 2006;30:351–356. doi: 10.1016/j.jemermed.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 7.A long-term analysis of physician triage screening in the emergency department. Rogg JG, White BA, Biddinger PD, Chang Y, Brown DF. Acad Emerg Med. 2013;20:374–380. doi: 10.1111/acem.12113. [DOI] [PubMed] [Google Scholar]
- 8.Use of Imaging in the emergency department: do individual physicians contribute to variation? Valtchinov VI, Ip IK, Khorasani R, Schuur JD, Zurakowski D, Lee J, Raja AS. AJR Am J Roentgenol. 2019;213:637–643. doi: 10.2214/AJR.18.21065. [DOI] [PubMed] [Google Scholar]
- 9.Radiation exposure from CT scanning in the resuscitative phase of trauma care: a level one trauma centre experience. Beatty L, Furey E, Daniels C, Berman A, Tallon JM. CJEM. 2015;17:617–623. doi: 10.1017/cem.2014.61. [DOI] [PubMed] [Google Scholar]
- 10.Advanced radiology utilization in a tertiary care emergency department from 2001 to 2010. Ahn S, Kim WY, Lim KS, et al. PLoS One. 2014;9:0. doi: 10.1371/journal.pone.0112650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Optimizing diagnostic imaging in the emergency department. Mills AM, Raja AS, Marin JR. Acad Emerg Med. 2015;22:625–631. doi: 10.1111/acem.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National conference on dose reduction in CT, with an emphasis on pediatric patients. Linton OW, Mettler FA Jr. AJR Am J Roentgenol. 2003;181:321–329. doi: 10.2214/ajr.181.2.1810321. [DOI] [PubMed] [Google Scholar]
- 13.About the ACR appropriateness criteria. [ May; 2023 ]. https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria/About-the-ACR-AC https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria/About-the-ACR-AC
- 14.Advanced diagnostic imaging utilization during emergency department visits in the United States: a predictive modeling study for emergency department triage. Zhang X, Kim J, Patzer RE, Pitts SR, Chokshi FH, Schrager JD. PLoS One. 2019;14:0. doi: 10.1371/journal.pone.0214905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National trends in CT use in the emergency department: 1995-2007. Larson DB, Johnson LW, Schnell BM, Salisbury SR, Forman HP. https://pubmed.ncbi.nlm.nih.gov/21115875/ Radiology. 2011;258:164–173. doi: 10.1148/radiol.10100640. [DOI] [PubMed] [Google Scholar]