Abstract
Craniomaxillofacial trauma (CMFT) is a type of injury that affects the face, neck, and scalp, and includes facial bone fractures, dentoalveolar trauma, and soft tissue injuries. Work, traffic accidents, sports, and daily activities commonly cause these injuries. However, they are widespread in war‐torn countries where armed conflict leads to a high incidence of CMFT. The lack of resources, health care infrastructure, and surgical personnel in these areas result in subpar treatment and poor patient outcomes, contributing to the high mortality and morbidity rates among war victims. The importance of a multidisciplinary approach to CMFT management cannot be overstated, but current obstacles, such as a lack of access to proper medical care and rehabilitation services, impede the development of effective treatments. CMFT treatment is complex and prohibitively expensive for war‐torn nations to afford, necessitating international intervention to provide life‐saving surgical procedures for those suffering from CMFT in conflict zones. Despite efforts to improve CMFT treatments in war‐torn countries, more must be done to improve treatment outcomes. Data collection and research must also be improved in order to develop effective evidence‐based treatment methods.
Keywords: craniomaxillofacial, surgery, trauma, war zones
This submission examines the incidence and management of craniomaxillofacial trauma (CMFT) in war‐affected nations, highlighting the critical gaps in care due to limited resources, health care infrastructure, and surgical personnel. The study emphasizes the importance of a multidisciplinary approach to CMFT management and calls for international intervention to provide life‐saving surgical procedures for those suffering from CMFT in conflict zones. The need for improved data collection and research to develop effective evidence‐based treatment methods is also emphasized.
BACKGROUND
Craniomaxillofacial trauma (CMFT) is an injury to the soft and hard tissues of the face, neck, and scalp. It can occur as a singular entity or in conjunction with injuries to the head, neck, spine, upper and lower limbs, and the intracranial region. Soft tissue injuries, facial bone fractures, and dentoalveolar trauma are a few examples of CMFT. The primary causes of CMFT are work, traffic, sports, and daily activities. 1
Before their wars, most of the war‐torn nations had low‐ and middle‐class incomes and lacked the resources to provide effective emergency, trauma, and surgical care; nevertheless, the wars have only worsened the situation. Massive damage to their health care infrastructure led to the exodus of highly trained medical professionals, particularly surgeons, and economic devastation, making it challenging to uphold traditional health care standards. 2 , 3
Despite having the highest needs, these war victims had the lowest surgical outcomes, necessitating a complex, multidisciplinary team (MDT) approach made up of a range of experts and other nonphysicians. In poor countries with political unrest and military conflict, CMFTs are major global sources of mortality and morbidity. 4
This paper aims to highlight the incidence and implications of CMFT in war‐torn nations and analyze gaps in the management with suggested recommendations.
CMFT CAUSES, INCIDENCE, IMPLICATIONS, AND MORTALITY
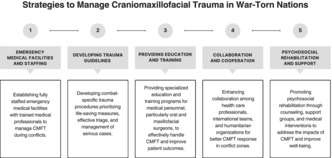
CMFT in a conflict‐trodden region has a number of processes, but the main offenders are bomb explosions and gunfire in these locations (Figure 1). For instance, a case series from Misrata, Libya, examined 154 individuals between February and November 2011 to determine the pathways of injury resulting from CMFT. This was conducted during the Libyan Civil War. Blasts (75.3%), bullets (19.5%), and road‐traffic accidents (3.9%) were the most common sources of injury. 5 Another study 6 documented the CMF wounds sustained during the wars in Afghanistan and Iraq. CMF injuries surmounting 4783 were reported, with penetrating soft tissue injuries (58%) and fractures (27%), with 76% of the fractures being open fractures, which were the most common injuries. These fractures may be sustained on the body globally, with the mandible accounting for 36% of all cases. In 84% of all CMFT instances, explosives were demonstrated to be the main mechanism of injury. In a retrospective study 7 conducted in a Turkish hospital, the majority (90%) of the 80 patients with CMFT were shot victims, and mandibular fractures were the most common type of trauma. These findings support explosions and gunshots as the main etiologies of CMFT trauma. In addition, a study in Iraq indicated that 65% (n = 2630) of the injured patients had CMFT open wounds (Figure 1), with 43,822 servicemen and women injured overall between 2001 and 2011. 8 The slow healing of these open wounds, medical intervention, the presence of foreign bodies, and bacterial and viral infections may all be applied to identify them. 8 Fractures of the CMF skeleton were observed in 44% of patients sustaining war‐inflicted injuries. The high‐velocity explosives were also responsible for a considerable amount of open fractures (75%) in the body. Patients succumbing to facial burns amounted to 10% concurrently, 16% of which comprised ocular burns (Figure 1). 8 About 6% (n = 244) of individuals sustained CMF nerve injuries, with facial nerve injuries accounting for 34% and optic nerve injuries for 15%. The rate of vascular injury was 12%. 8 These CMFT incidents in armed conflict are also consistent with findings from Yemen and Syria, where refugees sustained 40% and 60%, respectively, of all CMFT injuries. 7 , 9
FIGURE 1.
A summary diagram of craniomaxillofacial traumas (CMFTs) in war zones with its causes, clinical picture, and implications.
Retrospective cohort research also assessed the prevalence of CMFT among Israeli soldiers harmed in the Second Lebanon War in the summer of 2006. 10 As many as 36 of the 565 injured troops, or 6.4% of all injured soldiers, had CMF injuries. As CMF injuries account for a major fraction of all trauma cases and have severe consequences such as mortality and disability, addressing them in conflict zones is imperative. In fact, the severity of CMF injuries in places of conflict emphasizes the seriousness of the issue and how urgently high‐quality medical care is warranted. 11 For instance, 7.76% of patients in Iran who received therapy for CMF injury reported issues such as infections, graft movement issues, and necrosis. These sequelae increase the risk of long‐term physical and psychological repercussions such as persistent pain, scarring, and deformity in addition to exacerbating the patients’ issues. 4 , 11 Furthermore, the reported perioperative death due to anesthetic errors emphasizes the moribund consequences of insufficient medical care in conflict zones.
The Syrian Civil War resulted in 13.3% of individuals sustaining CMFT injuries, unfortunately, succumbing to mortality, which had pronounced adverse effects (Figure 1). The war demonstrated how severely the health of the Syrian population had been impacted by such war and how urgently medical attention was necessitated. About 45% of those affected required complex surgical treatments such as facial reconstruction, craniotomies, and the repair of open globe injuries, according to data garnered following the conflicts in Syria and Iraq. 12 With the perioperative death rate being 6%, 12 emphasis on the necessity for individuals with such injuries to have better access to health care and treatment choices needs highlighting. Furthermore, during the Second Lebanon War, CMFTs claimed the lives of 2.8% of military personnel. 10
MANAGEMENT GAPS ON CMFT SURGICAL DELIVERY
Infrastructure
Instability, particularly in the management of CMFT, has a significant negative influence on health care provision in areas affected by war. Effective medical treatment is difficult to provide for those in need, especially in hospitals, due to a shortage of resources. Health care systems are essentially destroyed by war, resulting in more individuals without access to health care, particularly surgical care, and limited access to medical supplies. 2 , 3 Studies demonstrate that insufficient medical infrastructure and knowledge may profoundly impact the service grade. For instance, a study of 607 surgeons conducted in Tripoli, Libya, in 2014 and 2015 revealed that more than 81% of those polled claimed that insufficient hospital equipment made it difficult to successfully treat explosion injuries. 5 A national capacity survey of hospitals offering trauma care in war‐torn Syria was also conducted in 2016. 13 The findings indicated a major underservicing of hospitals and a lowered competence of these hospitals to administer adequate trauma care to achieve the best outcomes. In this poll, 94 hospitals were involved. Of those, 91% claimed to be equipped to perform emergency surgery. However, 16% claimed they lacked inpatient beds for the postoperative care of their patients with trauma. While 70% of hospitals could transfuse whole blood, only 7.4% could sort and bank blood products. Syria's war‐torn medics thus face a number of challenges. Another substantial problem is the lack of energy resources necessary for the operation of clinics and hospitals. Because of multifaceted energy issues, the majority of medical facilities in conflict zones rely on diesel generators to operate. Surgery cannot be performed in these circumstances without surgical lighting; instead, surgeons must rely on flashlights and cell phone illumination. 14 While anesthesiologists must rely on manual breathing and intravenous sedation, nurses must administer body heat to warm intravenous fluids. 14 Given these extreme conditions, trauma surgical care in a war‐torn zone is already tricky.
Despite rehabilitation being an essential component of every trauma patient's treatment process to restore function and improve their quality of life as much as possible after an injury, the bulk of studies have reported substandard or no rehabilitation services and outcomes in these war‐torn countries.
Surgical workforce and other MDTs
Most war‐torn countries suffer from acute staffing shortages, notably in surgical delivery. 5 , 13 , 14 Even in the absence of conflict, many low‐ and middle‐income countries have essentially no practical access to and delivery of surgical treatment. War in these undeveloped countries makes the already pressing demand for specialists to handle patients with complex traumatic CMFT even more pressing. Moreover, nonspecialists manage patients with comparable injuries in several war‐torn countries. 14 , 15 This is a concerning tendency, but it is a natural result of the scarcity of medical resources in war‐torn zones. In the administration of CMFT by nonspecialists, the clinical and educational facets are divided. On the clinical front, nonspecialists are trusted to provide medical care without specialists who are either difficult to locate or unable to reach those in need. This frequently leads to subpar treatment, which produces poor outcomes and increased morbidity. On the educational front, nonspecialists are typically undertrained in the management of CMFT. This lack of training is especially problematic in war zones, where the complexity and urgency of the injuries necessitate specialized knowledge and skills. 13 , 14 , 15
MDT was not employed to treat CMF injuries, according to a recent study of 171 individuals conducted during a military conflict. 15 According to the study, which observed medical professionals typically worked as sole providers (53.6%), orthodontists infrequently participated in CMFT care (23.1%) or consulted concerning patients with trauma (10.7%). 15 These results significantly affect the quality of care for patients with CMF injuries. The tendency of medical professionals to work alone and their absence from interdisciplinary teams may result in worse‐than‐optimum patient outcomes. Another illustration is the conflict in Syria, where a serious shortage of surgeons existed. Physicians for Human Rights 14 estimated that by 2013, 70% of the medical workforce will have fled the country. For instance, in Aleppo, Syria, surgeons have unique challenges. In the city, which had 2.5 million inhabitants and 6000 doctors on staff before the conflict, fewer than 70 doctors are currently employed. 14 After barrel bombs wreaked havoc on the city, only two vascular surgeons and one plastic surgeon were available to manage patients with trauma. One illustration of how the conflict has harmed Syria's health care industry is the country's chronic medical staff shortage. Further, the lack of surgeons significantly burdens the already overburdened surviving health care staff. Lower patient outcomes result from this, and junior residents and medical students are forced to complete duties outside their training scope. 14
Cost and finances
Many of these war‐torn regions have extreme economic challenges and cannot financially support high‐quality medical care (Figure 1). Because of its high cost, the surgical industry demands more financial investments. According to estimates, trauma costs are estimated to be US $400 billion annually, but CMF injuries are predicted to cost US $3.7 million, or approximately US $5000 per patient, in the United States. 16 Although the cost of CMF treatment may be financially less in conflict‐affected countries than in high‐income countries, these domiciles still struggle to recover from years of conflict and tyranny caused by poverty and unemployment. This demonstrates an inability to handle the significant trauma witnessed in war‐torn countries due to a lack of resources and a methodical approach. Individuals, therefore, find it difficult to contribute financially for medical care. 17 Hospital services in war‐torn countries such as Syria and Iraq require central support, as is the case in many other countries internationally. The repercussions of conflict in these areas have necessitated the allocation of a sizable portion of annual budgets to the comprehensive reconstruction of the country. This includes essential infrastructure such as structures, roads, electricity, and gas supplies, frequently resulting in disregarding health care services.
Further, corruption surmounts to a substantial detriment in the said war‐torn countries. Although these nations may possibly afford better health care treatments, including CMF services, their governments have recently grappled with corruption. Budgetary allocations consequently do not seem to be allocated to their expected sectors, which has resulted in a recent decline in the innovation and quality of health care services. Surgery and trauma care costs are prohibitive for underdeveloped nations, even those that have just experienced war. Because of the complexity of the issues at hand, the management of patients with CMFT may be extortionate. For instance, it has been demonstrated that the expenditure of CMF surgery for Syrian conflict victims in Hatay, Turkey, may reach US $4192 per patient. This price may be highly burdensome for those who require it and their families. The complexity of the surgical procedure, the necessity for specialized tools and materials, and the degree of experience necessary to perform these surgeries all contribute to the said high cost. 7
The high cost of CMFT surgery may potentially hinder some for the economy. The government, charities, and other organizations may be able to assist individuals who are affected. At the same time, the economy may be impacted and funds may be diverted from other essential requirements as a result. Furthermore, if the cost of CMF surgery becomes exponential, it may discourage patients from seeking treatment, which could result in longer‐term, more significant health issues and higher health care costs.
Huge research gaps need to be addressed
When investigating this topic, there are apparent gaps in the literature. Finding statistics on CMFTs across many war‐torn countries is exceedingly difficult. 9 , 10 Despite CMFT being frequently observed in places of conflict, reliable data on these injuries are difficult to come by. Moreover, limited resources and labor further hinder recordkeeping and data acquisition. 5 , 9 , 10 , 13 Health care providers in these areas prioritize immediate care for injured patients over data collection for research. 9
In certain scenarios, the matter of migration poses a noteworthy concern, given the constant movement of individuals. Consequently, effectively monitoring and establishing contact with patients, as well as gathering valuable data, become exceedingly challenging. 18
The inability to gather data on CMFTs in conflict zones has severe implications for developing best practices and suggestions for treating these wounds. Without exact data, health care professionals and academics find it difficult to grasp the scope of the problem, identify areas that require improvement, and develop evidence‐based treatment techniques. Because of this, insufficient knowledge may jeopardize the quality of care provided to people with CMF injuries in conflict zones.
THE INTERNATIONAL COMMUNITY’S SIGNIFICANT ROLE NEEDS TO BE COMMENDED
Providing life‐saving surgical procedures has long been important to humanitarian relief efforts during violent times. Examples are Aid to the Church in Need (ACN) and Medecins Sans Frontières (MSF), which are two organizations that excel at providing aid to the most vulnerable citizens of war‐torn countries. 19 , 20 MSF, for instance, has participated in 125 missions in 20 different countries, performing a staggering 64,000 surgical interventions. 19 ACN, by contrast, has also helped 3835 people in Syria, many of whom needed emergency care and trauma surgery. 20
It is also admirable that neighboring countries are attempting to provide surgical delivery, which is crucial for preserving life and improving the general prognosis for conflict‐associated injury victims. 7 , 9 Despite the challenges this possess, several countries are committed to providing care to individuals who have endured CMFTs in a war‐torn zone. For instance, the Turkey Borders Hospitals provide medical care to displaced individuals and refugees at the Turkish–Syrian border. However, despite challenging and oftentimes dangerous conditions, these hospitals are committed to providing high‐quality healthcare, including treatment for CMF injuries. 18
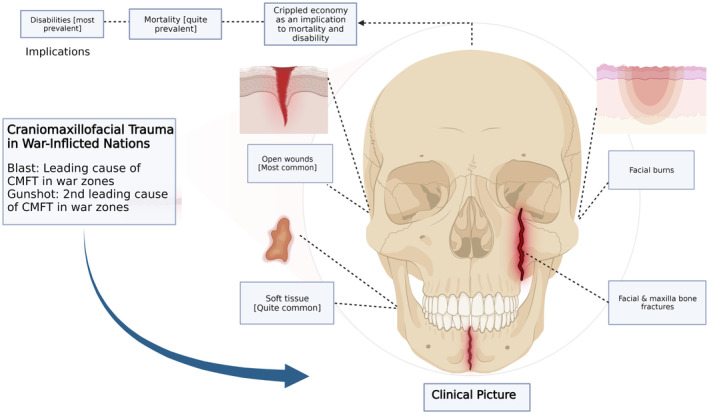
STRATEGIES FOR ADDRESSING CMFT IN WAR‐TORN NATIONS
Several crucial strategies must be implemented to adequately manage CMFT during periods of conflict. First and foremost, it is essential to construct emergency medical facilities that are fully staffed with qualified medical professionals, such as surgeons and nurses with CMFT management training (Figure 2). 21 In addition, it is critical to develop trauma procedures that are specific to environments engrossed in military combat. According to Ogilvie et al., 22 these guidelines should give priority to measures that save lives, pertain to effective triage, and manage serious cases (Figure 2).
FIGURE 2.
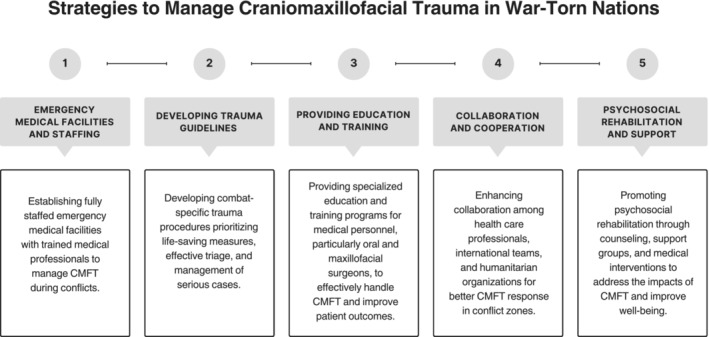
Strategies to manage craniomaxillofacial trauma (CMFT) in war‐torn nations.
Moreover, it is paramount that complimentary education is provided to medical personnel, especially oral and maxillofacial surgeons, to effectively handle CMFT (Figure 2). To strengthen local capacity and improve patient outcomes, specialized programs that encompass trauma care concepts, patient assessment, wound management, fracture fixation, and soft tissue repair are vital. 21 In addition, it is essential to promote cooperation and collaborations between regional health care professionals, international medical teams, and humanitarian organizations (Figure 2). 23 , 24 Further, supporting psychosocial rehabilitation is fundamental when addressing the psychological and social impacts of CMFT. Providing counseling, support groups, and access to reconstructive surgeries or prosthetic devices aid in the coping of patients, restores functionality, and improves self‐esteem. 23 , 24
Lastly, documenting and reporting CMFT cases is substantial for advocacy, resource allocation, and policy development. Collaboration between international organizations and local health care providers is warranted to collect data on cases, treatment outcomes, and rehabilitation needs. 23 This information drives policy changes and enhances the overall response to CMFT in conflict zones.
CONCLUSION
The management of CMFT in war‐torn nations presents formidable challenges precipitated by limited resources, damaged infrastructure, and a dearth of skilled surgical professionals. Financial constraints further hinder access to quality care, while gaps in research impede approaches and advances in evidence‐based treatment. To address these gaps, a multifaceted approach is needed, including rebuilding health care infrastructure, increasing skilled surgical professionals, countering financial constraints, and promoting international collaborations. These efforts can improve CMFT management, enhance care quality, and reduce mortality rates.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: Not applicable.
Informed consent: Not applicable.
Registry and the registration no. of the study/trial: Not applicable.
Animal studies: Not applicable.
ACKNOWLEDGEMENTS
The authors have nothing to report.
Adebusoye FT, Awuah WA, Alshareefy Y, Wellington J, Mani S, Ahmad AO, et al. Craniomaxillofacial trauma in war‐torn nations: Incidence, management gaps, and recommendations. Acute Med Surg. 2023;10:e877. 10.1002/ams2.877
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Kraft A, Abermann E, Stigler R, Zsifkovits C, Pedross F, Kloss F, et al. Craniomaxillofacial trauma: synopsis of 14,654 cases with 35,129 injuries in 15 years. Craniomaxillofac Trauma Reconstr. 2012;5(1):41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wireko AA, Adebusoye FT, Wellington J, Bel‐Nono KN, Abdul‐Rahman T, Ovechkin D, et al. Appraising war's impacts on neurosurgical delivery in Ukraine. Int J Health Plann Manage. 2023;38:1071–1075. 10.1002/hpm.3633 [DOI] [PubMed] [Google Scholar]
- 3. Awuah WA, Mehta A, Kalmanovich J, Yarlagadda R, Nasato M, Kundu M, et al. Inside the Ukraine war: health and humanity. Postgrad Med J. 2022;98(1160):408–410. 10.1136/postgradmedj-2022-141801 [DOI] [PubMed] [Google Scholar]
- 4. Ghanem AM, Borg TM, Sadigh P, Myers S, Smith DJ, Holmes S. Craniomaxillofacial trauma management in austere and war zone environments‐a role for composite tissue allotransplantation? Ann Burns Fire Disasters. 2019;32(4):308–320. [PMC free article] [PubMed] [Google Scholar]
- 5. Qmro.qmul.ac.uk . Craniomaxillofacial War Injuries in Misrata, Libya. [Cited 2023 Feb 6]. Available from: https://qmro.qmul.ac.uk/xmlui/bitstream/handle/123456789/68687/Zaggut_Craniomaxillofacial%20War%20Injuries%20in%20Misrata_Published_2020.pdf?sequence=2
- 6. Lew TA, Walker JA, Wenke JC, Blackbourne LH, Hale RG. Characterization of craniomaxillofacial battle injuries sustained by United States service members in the current conflicts of Iraq and Afghanistan. J Oral Maxillofac Surg. 2010;68(1):3–7. [DOI] [PubMed] [Google Scholar]
- 7. Arlı C, Özkan M, Karakuş A. Incidence, etiology, and patterns of maxillofacial traumas in Syrian patients in Hatay, Turkey: a 3 year retrospective study. Ulus Travma Acil Cerrahi Derg. 2019;25(1):29–33. [DOI] [PubMed] [Google Scholar]
- 8. Chan RK, Siller‐Jackson A, Verrett AJ, Wu J, Hale RG. Ten years of war: a characterization of craniomaxillofacial injuries incurred during operations enduring freedom and Iraqi freedom. J Trauma Acute Care Surg. 2012;73(6):S453–S458. [DOI] [PubMed] [Google Scholar]
- 9. Daniels JS, Albakry I, Braimah RO, Samara MI, Albalasi RA, Al‐Rayshan SM. Management of maxillofacial gunshot injuries with emphasis on damage control surgery during the Yemen civil war. Review of 173 victims from a level 1 trauma Hospital in Najran, Kingdom of Saudi Arabia. Craniomaxillofac Trauma Reconstr. 2022;15(1):58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Levin L, Zadik Y, Peleg K, Bigman G, Givon A, Lin S. Incidence and severity of maxillofacial injuries during the second Lebanon war among Israeli soldiers and civilians. J Oral Maxillofac Surg. 2008;66(8):1630–1633. [DOI] [PubMed] [Google Scholar]
- 11. Hennocq Q, Bennedjaï A, Simon F, Testelin S, Devauchelle B, Tulasne JF, et al. Maxillofacial surgery in wartime Middle‐East: Paul Tessier's missions to Iran. J Craniomaxillofac Surg. 2019;47(9):1449–1455. [DOI] [PubMed] [Google Scholar]
- 12. Neubauer DC, Camacho M, O'Reilly EB, Brice M, Gurney JM, Martin MJ. The new face of war: craniofacial injuries from operation inherent resolve. J Trauma Acute Care Surg. 2022;93(2S):S49–S55. [DOI] [PubMed] [Google Scholar]
- 13. Mowafi H, Hariri M, Alnahhas H, Ludwig E, Allodami T, Mahameed B, et al. Results of a nationwide capacity survey of hospitals providing trauma care in war‐affected Syria. JAMA Surg. 2016;151(9):815–822. [DOI] [PubMed] [Google Scholar]
- 14. Sahloul MZ, Monla‐Hassan J, Sankari A, Kherallah M, Atassi B, Badr S, et al. War is the enemy of health. Pulmonary, critical care, and sleep medicine in war‐torn Syria. Ann Am Thorac Soc. 2016;13(2):147–155. [DOI] [PubMed] [Google Scholar]
- 15. Maj BC, Col MS, Capt MA. The Orthodontist's role in post‐battlefield craniomaxillofacial trauma reconstruction. Mil Med. 2022;usac102. [DOI] [PubMed] [Google Scholar]
- 16. Moses H, Powers D, Keeler J, Erdmann D, Marcus J, Puscas L, et al. Opportunity cost of surgical management of craniomaxillofacial trauma. Craniomaxillofac Trauma Reconstr. 2016;9(1):76–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Al Bayati MJ, Samaha GJ, Al Bayati AJ, Kummoona R, Habal MB, Thaller SR. Trauma in Iraq's wars: assessment and management of craniofacial injury. J Craniofac Surg. 2020;31(5):1434–1437. [DOI] [PubMed] [Google Scholar]
- 18. Ucak M. Incidence and severity of maxillofacial injuries during the Syrian civil war in Syrian soldiers and civilians. J Craniofac Surg. 2019;30(4):992–995. [DOI] [PubMed] [Google Scholar]
- 19. Chu K, Rosseel P, Trelles M, Gielis P. Surgeons without Borders: a brief history of surgery at Médecins Sans Frontières. World J Surg. 2009;34(3):411–414. 10.1007/s00268-009-0187-z [DOI] [PubMed] [Google Scholar]
- 20. Przepiórka Ł, Boguszewski M, Smuniewski C, Kujawski S. Medical aid to war victims in Syria in 2019: a report of organized healthcare support from a charity organization. BMC Health Serv Res. 2022;22(1):1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dubose J, Rodriguez C, Martin M, Nunez T, Dorlac W, King D, et al. Eastern Association for the Surgery of trauma military ad hoc committee. Preparing the surgeon for war: present practices of US, UK, and Canadian militaries and future directions for the US military. J Trauma Acute Care Surg. 2012;73(6 Suppl 5):S423–S430. 10.1097/TA.0b013e3182754636 [DOI] [PubMed] [Google Scholar]
- 22. Ogilvie MP, Pereira BM, Ryan ML, Panthaki ZJ. Emergency department assessment and management of facial trauma from war‐related injuries. J Craniofac Surg. 2010;21(4):1002–1008. [DOI] [PubMed] [Google Scholar]
- 23. Chen J. A paradigm of medical humanitarianism: the case of Medecins sans Frontieres (doctors without Borders) in Africa. Online J Afr Aff. 2014;3(6):87–94. [Google Scholar]
- 24. Coupland RM, Parker PJ, Gray RC. Triage of war wounded: the experience of the International Committee of the Red Cross. Injury. 1992;23(8):507–510. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


