Abstract
Objectives
Chronic pain (CP) is a poorly recognised and frequently inadequately treated condition affecting one in five adults. Reflecting on sociodemographic disparities as barriers to CP care in Canada was recently established as a federal priority. The objective of this study was to assess sex and gender differences in healthcare utilisation trajectories among workers living with CP.
Design
Retrospective cohort study.
Participants
This study was conducted using the TorSaDE Cohort which links the 2007–2016 Canadian Community Health Surveys and Quebec administrative databases (longitudinal claims). Among 2955 workers living with CP, the annual number of healthcare contacts was computed during the 3 years after survey completion.
Outcome
Group-based trajectory modelling was used to identify subgroups of individuals with similar patterns of healthcare utilisation over time (healthcare utilisation trajectories).
Results
Across the study population, three distinct 3-year healthcare utilisation trajectories were found: (1) low healthcare users (59.9%), (2) moderate healthcare users (33.6%) and (3) heavy healthcare users (6.4%). Sex and gender differences were found in the number of distinct trajectories and the stability of the number of healthcare contacts over time. Multivariable analysis revealed that independent of other sociodemographic characteristics and severity of health condition, sex—but not gender—was associated with the heavy healthcare utilisation longitudinal trajectory (with females showing a greater likelihood; OR 2.6, 95% CI 1.6 to 4.1).
Conclusions
Our results underline the importance of assessing sex-based disparities in help-seeking behaviours, access to healthcare and resource utilisation among persons living with CP.
Keywords: EPIDEMIOLOGY, Organisation of health services, Quality in health care, PAIN MANAGEMENT, Sexual and gender disorders, STATISTICS & RESEARCH METHODS
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Healthcare trajectories were modelled using group-based trajectory modelling, an objective and person-centred statistical approach.
Use of an exhaustive database harnessing the strengths of longitudinal claim data linked to patient-reported outcomes.
The analysis was conducted in a community sample and included people with little or no contact with the healthcare system, which increases the external validity of the results.
A gender measure was only available among participants having worked in the past year.
Medical claims do not allow reliable identification of chronic pain-related healthcare contacts/visit. All-cause healthcare visits were thus studied.
Introduction
Defined as persistent or recurrent pain lasting over 3 months,1 chronic pain (CP) affects 23% of females and 16% of males in Canada,2 seriously impacting physical functioning, emotional well-being and quality of life.3–8 It also constitutes a significant economic burden for patients, the healthcare system and third-party payers.9–11 In Canada, direct healthcare costs and loss of productivity due to CP amount to US$38.3–US$40.4 billion per year.12 This number was estimated to reach US$560–US$635 billion in the USA, exceeding the societal cost of heart disease, diabetes or cancer.13 Despite decades of research on CP and its treatment, the management of this condition remains suboptimal. Indeed, CP is characterised as poorly recognised, underdiagnosed and inadequately treated.12 14–17 CP should be managed in the primary care setting (family physicians, pharmacists, nurses) and more complex cases referred to multidisciplinary pain clinics in the secondary and tertiary care sectors before being redirected to community-based services. Unfortunately, the current situation does not reflect such trajectories. In the universal healthcare coverage context of Canada, for example, major shortcomings persist and render the healthcare system inefficient, such as numerous gaps in primary care CP management,14 too many patients ending up in the emergency room (a setting that is not conducive to the management of CP),18 19 ill-equipped healthcare professionals,14 insufficient access to pain clinics due to a lack of resources, long waiting lists or the absence of such clinics in certain regions20 and the absence of a measurement culture that makes it difficult to quantify the impact of our interventions (need for outcome measures and descriptors that are standardised from one care setting to another21). Implementing favourable healthcare trajectories for CP, from primary care to multidisciplinary specialised care teams and reversing sociodemographic disparities as barriers to CP care are priorities emanating from consultations conducted among patients and stakeholders.12
One may wonder if women, men and gender-diverse people living with CP share similar healthcare utilisation. Sex can be defined as a set of biological attributes associated with physical and physiological features.22 It has intrigued pain researchers for decades; differences between males and females are found in pain sensitivity, CP prevalence, medication use, response to treatment, drug side effects, pain beliefs and attitudes towards people living with CP.16 23–34 Conversely, gender refers to socially constructed roles, behaviours, expressions and identities.22 Although equally important, it is a complex and challenging construct to measure that is often overlooked.35 Without proper measurement and consideration of gender, it is unclear the extent to which sex differences are explained by biological factors or indirect measurement of social factors.
While sex differences have been found in healthcare utilisation among people living with CP,36 37 few has considered gender in their analysis38 or explored how sex and gender intersect with regard to healthcare utilisation. Furthermore, to our knowledge, none has delved into the related patterns of healthcare utilisation over time (trajectories). A better understanding of the determinants of healthcare utilisation has the potential to guide the prevention of adverse trajectories and reduction of pain inequities. This study thus aimed to examine sex and gender differences in healthcare utilisation trajectories.
Methods
Data source
This retrospective cohort study was conducted using data from the TorSaDE Cohort.39 This cohort of 102 148 participants links five cycles of Statistics Canada’s Canadian Community Health Survey (CCHS; 2007–2008, 2009–2010, 2011–2012, 2013–2014 and 2015–2016 cross-sectional questionnaires) and Quebec administrative databases (1996 to 2016 longitudinal health insurance claims).
Canadian Community Health Survey
Statistics Canada’s CCHS is designed to collect health data on a representative sample of Canadians aged 12 years and older (probability sampling).40 Not included are on-reserve Indigenous people, full-time members of the Canadian Armed Forces, institutionalised individuals or persons living in the Quebec regions of Nunavik and Terres-Cries-de-la-Baie-James (altogether <3% of Canadians). Standardised questionnaires are used and data quality is maximised through a variety of methods, including rigorous interviewer training and various control measures.40 Response rates are high (69.8%–78.9%, depending on cycles41) and the test–retest reliability of responses to several questions has been demonstrated.42 As part of the CCHS, participants give informed consent to Statistics Canada allowing the provinces to link their responses to provincial administrative databases.
Quebec administrative databases
The Régie de l’assurance maladie du Québec (RAMQ) administers the provincial universal health insurance,43 which covers the cost of medical visits, emergency department visits, hospitalisations and medical procedures for all Quebec residents.44 The TorSaDE Cohort, whose implementation is detailed elsewhere,39 is unique in Canada and contains a rich set of sociodemographic variables not included in administrative databases when used alone for healthcare service research.
Patient and public involvement
In this study, a person with lived experience of CP (NM) was involved in the grant application, formulation of research objectives and interpretation of results.
Selection criteria and study population
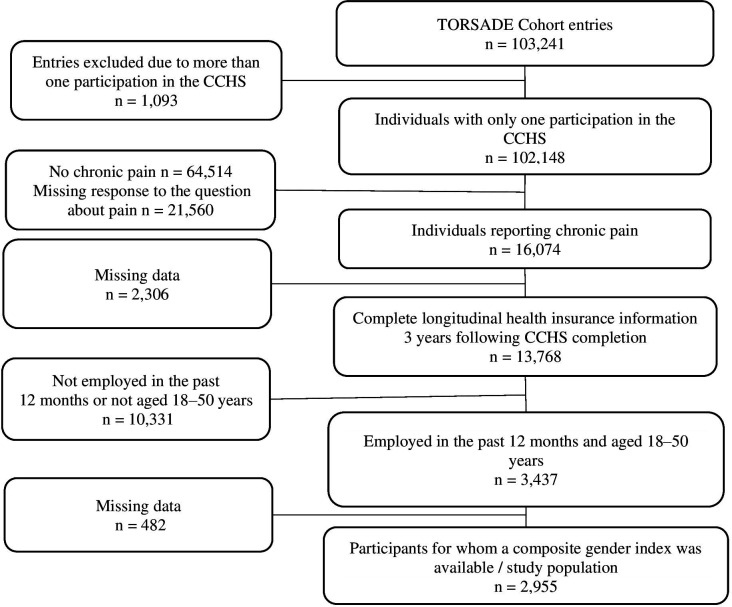
The TorSaDE Cohort includes 102 148 participants who completed 103 241 entries (participants could take part in more than one CCHS cycle). As shown in figure 1, our study sample, of 2955 individuals, was created using four criteria: (1) For participants with more than one CCHS entry, only the most recent entry was retained. (2) Participants reporting CP (having answered ‘No’ to the CCHS question ‘Are you usually free of pain or discomfort?’). While this definition may differ from commonly used definitions of chronicity based on the duration of symptoms,1 45–47 it has been used in many CP epidemiology studies2 8 48–52 and provides prevalence estimates comparable to studies using more traditional definitions.53 (3) Participants with complete longitudinal health insurance information for 3 years following CCHS completion (since longitudinal administrative data are available in the TorSaDE Cohort up until 2016, participants of the 2015–2016 CCHS cycle were not included). (4) Participants for whom a composite gender index54 was available. In the TorSaDE Cohort, a gender measure (see the Study variables section) is only available among participants having worked in the past year (all types of occupations taken together) and for whom work variables were measured by Statistics Canada (participants aged 18–50 years). For this reason, this study is centred on workers only.
Figure 1.
Study population selection. CCHS, Canadian Community Health Survey.
Study variables
Healthcare utilisation trajectories
Using administrative data, all hospitalisations, physician visits and emergency department visits were considered. The number of healthcare contacts per participant per year was modelled into 3-year healthcare utilisation trajectories using group-based trajectory modelling (GBTM), a statistical approach to grouping participants with similar patterns of outcomes over time55–59 (see full description in online supplemental file 1). Trajectory group membership was then used as a categorical dependent variable.
bmjopen-2022-070509supp001.pdf (115.7KB, pdf)
Sex and gender
Sex and gender were the independent variables of interest. In the 2007–2016 CCHS cross-sectional questionnaires, sex was measured as a self-reported dichotomous variable (male vs female). Gender was not directly available in the CCHS questionnaire, but measured using a composite index previously developed by our group using gender-related CCHS variables, namely the GENDER Index.54 Higher scores on the 0–100 index represent more feminine characteristics. Face and construct validity of the GENDER Index scores were demonstrated in the TorSaDE Cohort population.54 When looking at the distribution of GENDER Index scores in males and females in the TorSaDE Cohort, sex and GENDER Index scores appeared related but partly independent (eg, incomplete histogram overlap, variability of gender scores within each sex group).54 The index was deemed multidimensional and includes variables related to various gender constructs such as gender identity (how individuals see themselves—eg, man, woman, non-binary, two-spirited), gender roles (behavioural norms applied to males and females that influence everyday actions, expectations and experiences), gender relationships (how individuals interact with and are treated by others based on their ascribed gender) and institutionalised gender (distribution of power between men and women in societal institutions).60 As underlined, work-related variables appeared to be paramount in the development of our gender measure (conceptually60 61 and based on the iterative statistical analysis54). Thus, the gender index could only be calculated among participants aged 18–50 years who reported having worked in the past year in the CCHS and for whom work variables were measured by Statistics Canada (figure 1).
Covariables
CCHS data enabled consideration of the following self-reported variables: socioeconomic factors, pain intensity (mild/moderate/severe), pain interference (none/a few/some/most activities prevented), self-reported back pain (except fibromyalgia and arthritis), self-reported arthritis (except fibromyalgia), perceived general health (excellent/very good/good/fair/poor), alcohol consumption in the past year, smoking, physical activity (regular/occasional, rare), lifestyle (active/moderately active/inactive, according to Statistics Canada’s index of physical activity) and reporting having a regular physician. Further, the following was derived from administrative data: public prescription drug insurance status at time of CCHS completion (about 45% of the Quebec population is covered: people who are not eligible for private drug insurance with their employer or their spouse’s employer, who are ≥65 years old or who receive last-resort financial assistance44), combined Charlson Comorbidity Index and Elixhauser Comorbidity Index62 calculated in the year before CCHS completion (accounting for various non-pain comorbidities that can show sex differences) and use of a pain clinic (medical claims associated with a pain clinic establishment code (4×1) or professional activities billed for services rendered in a pain clinic (anaesthesia services coded 41055, 41056, 41057, 41058 and 41059)).
Statistical analysis
A sex-based and gender-based analysis was conducted,63–65 including stratified statistics, statistical significance of sex, gender and their interaction term in multivariable models, and reporting of negative findings (statistically non-significant results). First, the characteristics of the whole study population were summarised using descriptive statistics. As mentioned earlier, GBTM was applied to model 3-year healthcare utilisation trajectories and classify participants into trajectory groups (online supplemental file #1). This analysis was conducted for the whole study sample, and then repeated among the following strata to assess sex and gender differences in the number and patterns of healthcare utilisation trajectories: males, females and three strata formed using the GENDER Index tertiles (0–100 values were ordered and the distribution was separated into three equal parts/groups to reflect masculine, androgynous or undifferentiated, and feminine gender). A multivariable logistic regression model was then used across the study sample to assess the association between sex, gender (independent variables) and dichotomised trajectory group membership (dependent variable), while accounting for covariables. In the regression model, trajectory group membership was dichotomised to predict participants with the heaviest healthcare utilisation over time (the healthcare utilisation trajectory the most likely to be unfavourable66). All variables considered are detailed in table 1. Intersectional factors and potential confounders to be considered in the model were selected a priori based on intersectionality-based research65 67 and Andersen’s (1995) model,68 which is widely used in healthcare utilisation studies.69 Multicollinearity was tested according to variance inflation factors70 and no multiple imputation was applied as missing data proportion was low across variables of interest (<3.8%). Statistical interaction between sex and gender was tested, and all analyses were conducted using SAS (V.9.4).
Table 1.
Study population characteristics
| Characteristics* (n=2 955) |
No (%) of participants† | |
| Sociodemographic profile | ||
| Age (years)—mean±SD | 37.31 | ±9.02 |
| Sex | ||
| Females | 1659 | (56.14) |
| Males | 1296 | (43.86) |
| Gender Index (0–100)—mean±SD | 0.50 | ±0.26 |
| Masculine (tertile #1 scores 0.01–0.42) | 984 | (33.30%) |
| Androgynous or undifferentiated (tertile #2 scores 0.43–0.64) | 986 | (33.47%) |
| Feminine (tertile #3 scores 0.65–0.99) | 985 | (33.33%) |
| White self-identified race | ||
| Yes | 2705 | (91.54) |
| Indigenous self-identification | ||
| Yes | 67 | (2.36) |
| Country of birth | ||
| Canada | 2734 | (92.52) |
| Other | 221 | (7.48) |
| Education level | ||
| No secondary diploma | 270 | (9.16) |
| Secondary diploma | 322 | (10.92) |
| College diploma/registered apprenticeship or other trades certificate or diploma | 1618 | (54.88) |
| University education diploma | 738 | (25.03) |
| Marital status | ||
| In a relationship | 1655 | (56.35) |
| Not in a relationship | 1290 | (43.65) |
| Household income ($C) | ||
| <20 000 | 160 | (5.41) |
| 20 000–39 999 | 582 | (19.70) |
| 40 000–59 999 | 633 | (21.42) |
| 60 000–79 999 | 551 | (18.65) |
| ≥80 000 | 1029 | (34.82) |
| Region of residence | ||
| Remote | 657 | (22.23) |
| Non-remote | 2298 | (77.77) |
| Geographical area | ||
| Urban | 2136 | (72.28) |
| Rural | 819 | (27.72) |
| Public drug insurance status | ||
| Covered | 753 | (25.48) |
| Not covered | 2202 | (74.52) |
| Pain symptoms | ||
| Pain intensity | ||
| Mild | 964 | (32.74) |
| Moderate | 1568 | (53.26) |
| Severe | 412 | (13.99) |
| Pain interference (activities prevented) | ||
| None | 1257 | (42.61) |
| A few | 1183 | (40.10) |
| Some | 348 | (11.80) |
| Most | 162 | (5.49) |
| Self-reported back pain (except fibromyalgia and arthritis) | ||
| Yes | 1261 | (42.79) |
| Self-reported arthritis (except fibromyalgia) | ||
| Yes | 414 | (14.06) |
| General health and lifestyle profile | ||
| Combined comorbidity index of Charlson and Elixhauser—mean±SD | 0.12 | ±0.68 |
| Perceived general health | ||
| Excellent or very good | 1291 | (43.72) |
| Good | 1245 | (42.16) |
| Fair or bad | 417 | (14.12) |
| Alcohol consumption in the past 12 months | ||
| Regular | 2280 | (77.26) |
| Occasional | 400 | (13.55) |
| Has not drunk | 271 | (9.18) |
| Smoking | ||
| Regular | 762 | (25.79) |
| Occasional | 190 | (6.43) |
| Never | 2003 | (67.78) |
| Physical activity | ||
| Regular | 1822 | (61.66) |
| Occasional | 596 | (20.17) |
| Rare | 537 | (18.17) |
| Lifestyle | ||
| Active | 583 | (19.73) |
| Moderately active | 737 | (24.94) |
| Inactive | 1635 | (55.33) |
| Healthcare | ||
| Use of a pain clinic | ||
| Yes | 162 | (5.49) |
| Having a regular physician | ||
| Yes | 2215 | (74.98) |
*Proportion of missing data across presented variables ranged between 0 and 3.76%. Listwise deletion was thus applied for the subsequent phases of the analysis.
†Unless stated otherwise.
Results
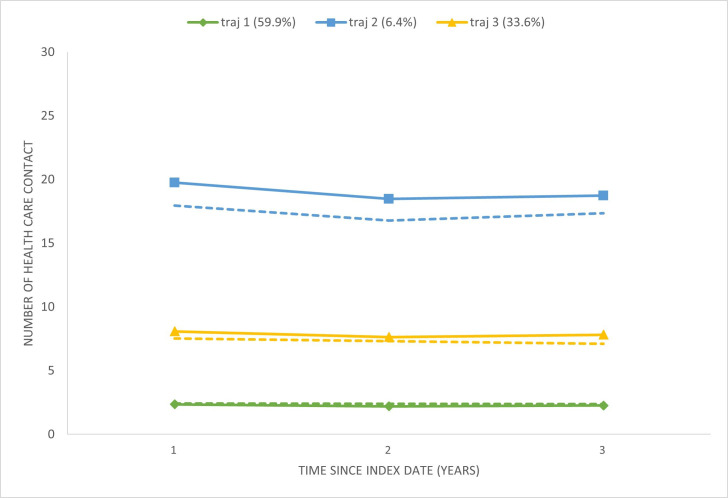
The analysis was conducted among 2955 workers living with CP (figure 1), whose characteristics are shown in table 1. Mean age was 37.3±9.0 years old (range: 18–50) and 56.1% were female. In total, GBTM led to the testing of 29 models with differences in the number of healthcare utilisation trajectories (between 1 and 4) and trajectory shape (linear or linear and quadratic components). Model fit indices for each model tested are shown in online supplemental file #1. The best fit for the data, guaranteeing a minimum of 5% of participants belonging to the smallest trajectory was a three-trajectory model (figure 2): (1) low healthcare users (trajectory #1: 59.9% of the sample; the mean number of healthcare contacts varied from 2.1±2.1 to 2.3±2.2 per year), (2) heavy healthcare users (trajectory #2: 6.4% of the sample; 19.0±10.8 to 20.6±12.6 contacts per year) and (3) moderate healthcare users (trajectory #3: 33.6% of the sample; 7.9±4.7 to 8.4±5.0 contacts per year). According to the graph (figure 2), healthcare utilisation (number of healthcare contacts per year) appeared stable across the 3-year time window.
Figure 2.
Healthcare utilisation trajectories in the whole study sample. Plain line: observed mean number of healthcare contacts. Interrupted line: estimated number of healthcare contacts by the GBTM. GBTM, group-based trajectory modelling.
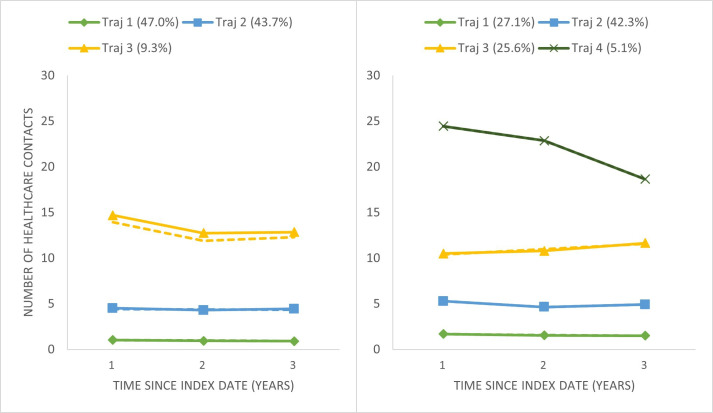
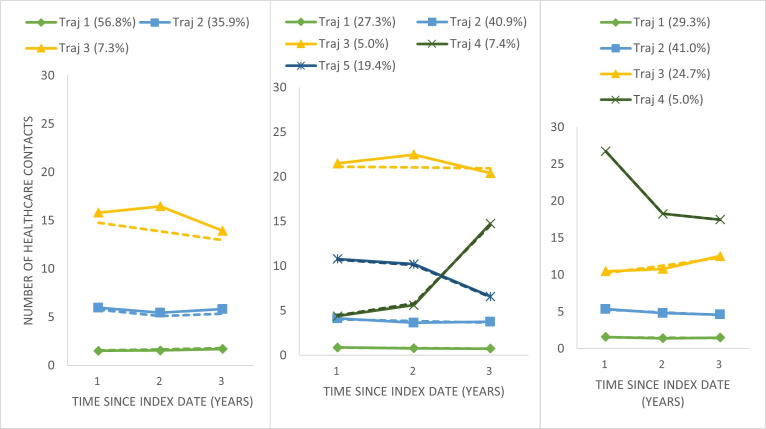
When GBTM was repeated among sex (males and females) and gender (GENDER Index tertiles) strata (see online supplemental file #1 for model fit indices), a three-trajectory model best fit the data for males, and a four-trajectory model best fitted the data for females (shown, respectively, in the left and right panels of figure 3). The first three healthcare utilisation trajectories (low, moderate and substantial healthcare users) were characterised by stable number of healthcare contacts over time and were similar between males and females. However, a fourth group of females (5.4%) displayed a decreasing curve of heavy healthcare use. Also, the number and pattern of healthcare utilisation trajectories varied across gender strata (figure 4), with feminine persons showing a decreasing curve of heavy healthcare use.
Figure 3.
Healthcare utilisation trajectories in males (left) and females (right). Plain line: observed mean number of healthcare contacts. Interrupted line: estimated number of healthcare contacts by the GBTM. GBTM, group-based trajectory modelling.
Figure 4.
Healthcare utilisation trajectories in first (left), second (centre) and third (right) tertiles of gender index. Plain line: observed mean number of healthcare contacts. Interrupted line: estimated number of healthcare contacts by the GBTM. GBTM, group-based trajectory modelling.
The complete results of the multivariable logistic regression model used to assess the association between sex, gender and a heavy healthcare trajectory while adjusting for sociodemographic status, pain characteristics and health profile are presented in online supplemental file #2. Sex—but not gender—was associated with a heavy healthcare trajectory (females having a greater likelihood than males; OR 2.6, 95% CI 1.6 to 4.1). The same result was reached whether gender was used as a continuous or categorical variable (groups formed by tertiles). No statistical interaction was found between sex and gender. Other factors associated with a heavy healthcare utilisation trajectory in the multivariable model were greater pain intensity, pain interference, and comorbidity, poorer perceived general health, use of a pain clinic and having a regular physician.
Discussion
This study aimed to examine sex and gender differences in healthcare utilisation trajectories given the growing recognition of the importance of examining these differences when studying the experience of pain28 33 35 and health outcomes in general.71–73 Sex and gender differences were found in the number and shape of healthcare utilisation trajectories. Females had a greater likelihood of falling into the heavy healthcare utilisation trajectory independent of social factors measured by the GENDER Index, pain severity and non-pain comorbidities.
To our knowledge, not one previous study has focused on sex-based and gender-based differences in healthcare utilisation longitudinal trajectories among people living with CP. An earlier Canadian study by Antaky et al36 failed to find a multivariable association between sex and heavy healthcare use among CP patients (defined as individuals in the highest 1-year direct healthcare costs quartile). However, their definition of heavy healthcare, statistical approach and time window were different, and they did not consider gender. Having adjusted for many covariables, our results are likely to reflect true sex-based differences. As there are no tenable access barriers to healthcare driven exclusively by biological sex, differences in healthcare utilisation trajectories between the males and females of our study may be explained by intersecting behavioural and social factors not captured by the GENDER Index or covariables that could be related to healthcare utilisation (eg, help-seeking tendencies,74 health literacy75).
Implications for knowledge users
For clinicians
It will be important for clinicians to be aware of their clientele who are heavy healthcare users. Be vigilant about the presence of sex disparities versus inequities is relevant. Disparities are not undesirable as such, unless they result in unfairness and injustice. On the other side, inequities are undesirable and should be subject to moral criticism as they imply unfairness and injustice.76 77 One may wonder, for example, if males receive similar medical follow-up and prescription opportunities as females do to manage their pain. Our results provide valuable information to identify, early on, patients who are more likely to experience heavy healthcare utilisation—that is, females—and adapt healthcare services accordingly (eg, assess if heavy healthcare use is useful and necessary).
For patients
It will be important to raise awareness among persons living with CP, especially women, regarding the trends found in this study. Partnership with patients and the public could help explore the causes and potential solutions.
For policy-makers
We would suggest all federal and provincial survey and patient registry developers to plan the measurement of sex at birth, gender identity (which was not available in our data), in addition to gender-related variables (eg, responsibility for caring for children, occupation, number of hours of work). The inclusion of such measures would allow for more relevant, equitable, diversified, and inclusive future research.
For researchers
Our results underline the importance of considering both sex and gender in CP healthcare utilisation research. This approach allows for a better understanding of whether differences are explained by biological factors or indirect measurement of social factors, and consequently helps identify modifiable risk factors for unfavourable outcomes. Although the non-pain-related medical literature abounds with findings demonstrating the tendency of females to have more health service contacts,74 our study is novel as it represents a first step in demystifying distinct subgroups of healthcare users among females and males living with CP. Future studies should build on our work and enhance and diversify the operationalisation of healthcare utilisation and care trajectories. For example, they could focus on a specific type of visits (eg, emergency department visits), examine transitions between different care sectors (primary, secondary, tertiary) or analyse sequences of care events over time (eg, sequence analysis59). Further studies should also examine the reasons for sex differences (eg, qualitative studies allowing an in-depth understanding of the behaviours and experiences specific to people living with CP).
Strengths and limitations
Selection bias and external validity
The TorSaDE Cohort, a unique database harnessing the strengths of longitudinal claim data from Canadian universal healthcare coverage linked to cross-sectional patient-reported outcomes, allowed to increase the generalisability of our results to various persons living with CP in Canada and possibly in countries with a similar gender norms and healthcare system. In fact, probability sampling and diversity of profiles are strengths of the CCHS. Also, CCHS allowed to work with a community sample and include people with little or no contact with the healthcare system, as compared with studies using administrative databases alone, studies using medical charts or studies involving clinic-based recruitment. A limitation is, however, that the GENDER Index was only available to workers54 limiting our capacity to study older adults who are more likely to have CP. Still, various socioeconomic and health impairment profiles (eg, participants reporting severe pain) could be taken into account in the multivariable analysis.
Information bias
Available data did not allow us to apply the new accepted definition of CP (persistent or recurrent pain lasting over 3 months).1 However, our CCHS-based CP definition has been used in many epidemiology studies2 8 48–52 and provides prevalence estimates comparable to studies using more traditional definitions.53 In our study, the index date (defined as CCHS date of completion) was not related to a significant event in the care trajectory of CP patients (eg, first diagnosis). Consequently, trajectories modelled in this study represent a random picture of a part of the life course of participants, and patterns of healthcare utilisation were quite stable over time. A limitation of our study is also that we had to study all-cause healthcare visits (as medical claims do not allow reliable identification of CP-related healthcare contacts/visits).78 79 Nevertheless, this allows the patient journey to be viewed as a whole, which could also be seen as a strength. Next relevant aspect, gender was assessed using the GENDER Index, which was computed using cross-sectional CCHS variables. Although some Canadians may have participated multiple times in the CCHS, our sample was limited to only one CCHS participation (figure 1), and we could not accommodate change in gender over time in the analysis. Overall, the strengths of using the TorSaDe Cohort clearly outweigh the disadvantages since, to our knowledge, at the time of this study, no pain-specific Canadian data source outside tertiary care settings links self-reported data from thousands of patients to longitudinal administrative databases (the only way to study biopsychosocial determinants of healthcare trajectories).
Confounding
The use of multivariable analysis in a large sample of participants and the availability of many potential confounders chosen according to recognised models65 67–69 allowed us to control confounding.
Conclusion
Our results underline the importance of deepening our understanding of sex-based disparities and inequities in terms of help-seeking, access to healthcare and resource utilisation among persons living with CP. Studies exploring the experience and perception of patients would be a good follow-up to this study in order to identify priorities to reduce the burden of pain and pain inequities in Canada.
Supplementary Material
Acknowledgments
We would like to thank members of the TorSaDE Cohort Working Group for exchange and methodological sharing activities. We thank Mélissa Gosselin and Adriana Angarita-Fonseca who helped with the literature review. We would also like to thank Emily-Jayn Rubec, who provided linguistic revision services for this paper.
Footnotes
Collaborators: TorSaDE Cohort Working Group : Past and current members of the TorSaDE Cohort Working Group are as follows: Alain Vanasse (outgoing director), Alexandre Lebel, Amélie Quesnel-Vallée, Anaïs Lacasse (incoming director), André Néron, Anne-Marie Cloutier, Annie Giguère, Benoit Lamarche, Bilkis Vissandjee, Catherine Hudon, Danielle St-Laurent, David Buckeridge, Denis Roy, Geneviève Landry, Gillian Bartlett, Guillaume Blanchet, Hermine Lore Nguena Nguefack, Isabelle Leroux, Jaime Borja, Jean-François Ethier, Josiane Courteau, Lucie Blais, Manon Choinière, Marc Dorais, Marc-André Blanchette, Marc-Antoine Côté-Marcil, Marie-Josée Fleury, Marie-Pascale Pomey, Mike Benigeri, Mireille Courteau, Nadia Sourial, Pasquale Roberge, Pier Tremblay, Pierre Cambon, Roxanne Dault, Sonia Jean, Sonia Quirion, Stéphanie Plante, Thomas Poder, Valérie Émond.
Contributors: Each author listed in the manuscript has participated actively and sufficiently in this study to fulfill all authorship criteria of the International Committee of Medical Journal Editors (ICMJE). AL, GP, MC, OMS, JK and NM conceptualised the project and secured funding. AL led the study, wrote the statistical analysis plan and drafted the manuscript. HLNN conducted the statistical analysis and assisted in drafting the manuscript. NM, BV and MZ contributed to the interpretation of data. All authors revised the manuscript critically, gave final approval of the version to be published and agreed to act as guarantors of the work.
Funding: This work was supported by the Canadian Institutes of Health Research (CIHR) (Personalised Health Catalyst Grants—Development of predictive analytic models: #PCG155479) and the Fondation de l’Université du Québec en Abitibi-Témiscamingue (FUQAT; no funding #). The implementation of the TorSaDE Cohort was funded by the Quebec SUPPORT Unit (Support for People and Patient-Oriented Research and Trials; no funding #), an initiative funded by the CIHR, the Ministry of Health and Social Services of Québec, and the Fonds de recherche du Québec—Santé (FRQS). During this study, GP and AL were, respectively, Junior 1 and Junior 2 research scholars from the FRQS. JK is supported by a CIHR Research Chair in health psychology. This research received no specific grant from the commercial sector.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Collaborators: on behalf of the TorSaDE Cohort Working, Alain Vanasse, Alexandre Lebel, Amélie Quesnel-Vallée, Anaïs Lacasse, André Néron, Anne-Marie Cloutier, Annie Giguère, Benoit Lamarche, Bilkis Vissandjee, Catherine Hudon, Danielle St-Laurent, David Buckeridge, Denis Roy, Geneviève Landry, Gillian Bartlett, Guillaume Blanchet, Hermine LoreNguena Nguefack, Isabelle Leroux, Jaime Borja, Jean-François Ethier, Josiane Courteau, Lucie Blais, Manon Choinière, Marc Dorais, Marc-André Blanchette, Marc-Antoine Côté-Marcil, Marie-Josée Fleury, Marie-Pascale Pomey, Mike Benigeri, Mireille Courteau, Nadia Sourial, Pasquale Roberge, Pier Tremblay, Pierre Cambon, Roxanne Dault, Sonia Jean, Sonia Quirion, Stéphanie Plante, Thomas Poder, and Valérie Émond
Data availability statement
Data may be obtained from a third party and are not publicly available. TorSaDE Cohort data links Statistics Canada’s Canadian Community Health Survey (CCHS) data and Quebec Health Ministry data that are not publicly available. Access must be granted by the Institut de la statistique du Québec (ISQ) (data holder) and the Commission d’accès à l’information du Québec. Programming codes can be obtained directly from the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and deidentified TorSaDE Cohort data was accessed through the Institut de la statistique du Québec (ISQ) secure virtual server (data holder). Ethical approval was obtained from the Commission d’accès à l’information du Québec (#1013990) and relevant university Research Ethics Boards (Université du Québec en Abitibi-Témiscamingue: # 2018-02-Lacasse, A.; Centre hospitalier universitaire de Sherbrooke (CHUS): #2017-1504). CCHS participants gave informed consent for their anonymized data to be used for research purposes.
References
- 1.Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease.The IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain 2019;160:19–27. 10.1097/j.pain.0000000000001384 [DOI] [PubMed] [Google Scholar]
- 2.Reitsma M, Tranmer JE, Buchanan DM, et al. The epidemiology of chronic pain in Canadian men and women between 1994 and 2007: longitudinal results of the national population health survey. Pain Res Manag 2012;17:166–72. 10.1155/2012/875924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashburn MA, Staats PS. Management of chronic pain. Lancet 1999;353:1865–9. 10.1016/S0140-6736(99)04088-X [DOI] [PubMed] [Google Scholar]
- 4.Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry 2003;60:39–47. 10.1001/archpsyc.60.1.39 [DOI] [PubMed] [Google Scholar]
- 5.Gureje O, Von Korff M, Simon GE, et al. Persistent pain and well-being: a world health organization study in primary care. JAMA 1998;280:147–51. 10.1001/jama.280.2.147 [DOI] [PubMed] [Google Scholar]
- 6.Smith BH, Elliott AM, Chambers WA, et al. The impact of chronic pain in the community. Fam Pract 2001;18:292–9. 10.1093/fampra/18.3.292 [DOI] [PubMed] [Google Scholar]
- 7.Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. EurJ Pain 2006;10:287. 10.1016/j.ejpain.2005.06.009 [DOI] [PubMed] [Google Scholar]
- 8.Hogan ME, Taddio A, Katz J, et al. Health utilities in people with chronic pain using a population-level survey and linked health care administrative data. Pain 2017;158:408–16. 10.1097/j.pain.0000000000000776 [DOI] [PubMed] [Google Scholar]
- 9.Kronborg C, Handberg G, Axelsen F. Health care costs, work productivity and activity impairment in non-malignant chronic pain patients. Eur J Health Econ 2009;10:5–13. 10.1007/s10198-008-0096-3 [DOI] [PubMed] [Google Scholar]
- 10.Guerriere DN, Choinière M, Dion D, et al. The Canadian STOP-PAIN project - part 2: what is the cost of pain for patients on waitlists of multidisciplinary pain treatment facilities Can J Anaesth 2010;57:549–58. 10.1007/s12630-010-9306-4 [DOI] [PubMed] [Google Scholar]
- 11.Lalonde L, Choinière M, Martin E, et al. Costs of moderate to severe chronic pain in primary care patients - a study of the ACCORD program. J Pain Res 2014;7:389–403. 10.2147/JPR.S55388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Campbell M, Hudspith M, Choinière M, et al. Working together to better understand, prevent and, manage chronic pain: what we heard. Ottawa: Report by the Canadian Pain Task Force – Health Canada, 2020. [Google Scholar]
- 13.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain 2012;13:715–24. 10.1016/j.jpain.2012.03.009 [DOI] [PubMed] [Google Scholar]
- 14.Lalonde L, Choinière M, Martin E, et al. Priority interventions to improve the management of chronic non-cancer pain in primary care: a participatory research of the ACCORD program. J Pain Res 2015;8:203–15. 10.2147/JPR.S78177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kress H-G, Aldington D, Alon E, et al. A holistic approach to chronic pain management that involves all stakeholders: change is needed. Curr Med Res Opin 2015;31:1743–54. 10.1185/03007995.2015.1072088 [DOI] [PubMed] [Google Scholar]
- 16.Lacasse A, Choinière M, Connelly J-A. Knowledge, beliefs, and attitudes of the Quebec population toward chronic pain: where are we now Can J Pain 2017;1:151–60. 10.1080/24740527.2017.1369849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Campbell M, Hudspith M, Anderson M, et al. Chronic pain in Canada: laying a foundation for action. Ottawa: Report by the Canadian Pain Task Force – Health Canada, 2019. [Google Scholar]
- 18.Poulin PA, Nelli J, Tremblay S, et al. Chronic pain in the emergency department: a pilot mixed-methods cross-sectional study examining patient characteristics and reasons for presentations. Pain Res Manag 2016;2016:3092391. 10.1155/2016/3092391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dépelteau A, Racine-Hemmings F, Lagueux É, et al. Chronic pain and frequent use of emergency department: a systematic review. Am J Emerg Med 2020;38:358–63. 10.1016/j.ajem.2019.158492 [DOI] [PubMed] [Google Scholar]
- 20.Choinière M, Peng P, Gilron I, et al. Accessing care in multidisciplinary pain treatment facilities continues to be a challenge in Canada. Reg Anesth Pain Med 2020;45:943–8. 10.1136/rapm-2020-101935 [DOI] [PubMed] [Google Scholar]
- 21.Campbell M, Hudspith M, Choinière M, et al. An action plan for pain in Canada. Ottawa: Report by the Canadian Pain Task Force – Health Canada; 2021. [Google Scholar]
- 22.CIHR . How to integrate sex and gender into research. Ottawa: Institute of Gender and Health, Canadian Institutes of Health Research; 2018. Available: http://www.cihr-irsc.gc.ca/e/50836.html [Google Scholar]
- 23.Racine M, Tousignant-Laflamme Y, Kloda LA, et al. A systematic literature review of 10 years of research on sex/gender and experimental pain perception - part 1: are there really differences between women and men Pain 2012;153:602–18. 10.1016/j.pain.2011.11.025 [DOI] [PubMed] [Google Scholar]
- 24.Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 2013;111:52–8. 10.1093/bja/aet127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fillingim RB, Gear RW. Sex differences in opioid analgesia: clinical and experimental findings. Eur J Pain 2004;8:413–25. 10.1016/j.ejpain.2004.01.007 [DOI] [PubMed] [Google Scholar]
- 26.Leresche L. Defining gender disparities in pain management. Clin Orthop Relat Res 2011;469:1871–7. 10.1007/s11999-010-1759-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paller CJ, Campbell CM, Edwards RR, et al. Sex-based differences in pain perception and treatment. Pain Med 2009;10:289–99. 10.1111/j.1526-4637.2008.00558.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pieretti S, Di Giannuario A, Di Giovannandrea R, et al. Gender differences in pain and its relief. Ann Ist Super Sanita 2016;52:184–9. 10.4415/ANN_16_02_09 [DOI] [PubMed] [Google Scholar]
- 29.Smitherman TA, Ward TN. Psychosocial factors of relevance to sex and gender studies in headache. Headache 2011;51:923–31. 10.1111/j.1526-4610.2011.01919.x [DOI] [PubMed] [Google Scholar]
- 30.Hurley RW, Adams MCB. Sex, gender, and pain: an overview of a complex field. Anesth Analg 2008;107:309–17. 10.1213/01.ane.0b013e31816ba437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samulowitz A, Gremyr I, Eriksson E, et al. “Brave men" and "emotional women": a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain”. Pain Res Manag 2018;2018:6358624. 10.1155/2018/6358624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richardson J, Holdcroft A. Gender differences and pain medication. Womens Health (Lond) 2009;5:79–90. 10.2217/17455057.5.1.79 [DOI] [PubMed] [Google Scholar]
- 33.Fillingim RB, King CD, Ribeiro-Dasilva MC, et al. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain 2009;10:447–85. 10.1016/j.jpain.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nguena Nguefack HL, Gabrielle Pagé M, Guénette L, et al. Gender differences in medication adverse effects experienced by people living with chronic pain. Front Pain Res (Lausanne) 2022;3:830153. 10.3389/fpain.2022.830153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boerner KE, Chambers CT, Gahagan J, et al. Conceptual complexity of gender and its relevance to pain. Pain 2018;159:2137–41. 10.1097/j.pain.0000000000001275 [DOI] [PubMed] [Google Scholar]
- 36.Antaky E, Lalonde L, Schnitzer ME, et al. Identifying heavy health care users among primary care patients with chronic non-cancer pain. Can J Pain 2017;1:22–36. 10.1080/24740527.2017.1326088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sagy I, Friger M, Sagy TP, et al. Gender-based differences in the management of low back pain. Harefuah 2014;153:380–4. [PubMed] [Google Scholar]
- 38.LaGrange SJ. Gender influences on help seeking among men and women with chronic pain [PhD thesis]. Indiana University, 2014 [Google Scholar]
- 39.Vanasse A, Chiu YM, Courteau J, et al. Cohort profile: the care trajectories-enriched data (TorSaDE) cohort. Int J Epidemiol 2021;50:1066h. 10.1093/ije/dyaa167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Canadian community health survey - annual component (CCHS) - detailed information for 2012. Ottawa: Statistics Canada; 2012. Available: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=135927 [Google Scholar]
- 41.Sanmartin C, Decady Y, Trudeau R, et al. Linking the Canadian community health survey and the Canadian mortality database: an enhanced data source for the study of mortality. Health Rep 2016;27:10–8. [PubMed] [Google Scholar]
- 42.Raina P, Bonnett B, Waltner-Toews D, et al. How reliable are selected scales from population-based health surveys? An analysis among seniors. Can J Public Health 1999;90:60–4. 10.1007/BF03404102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Régie de l’assurance maladie du Québec . La Régie de L'Assurance Maladie Du Québec. 2017. Available: http://www.ramq.gouv.qc.ca/fr/regie/Pages/mission.aspx
- 44.Régie de l’assurance maladie du Québec . Rapport Annuel de Gestion 2017-2018. Québec, Qc: Gouvernement Du Québec; 2018. Available: http://www.ramq.gouv.qc.ca/SiteCollectionDocuments/citoyens/fr/rapports/rappann1718.pdf [Google Scholar]
- 45.Bouhassira D, Lantéri-Minet M, Attal N, et al. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain 2008;136:380–7. 10.1016/j.pain.2007.08.013 [DOI] [PubMed] [Google Scholar]
- 46.Boulanger A, Clark AJ, Squire P, et al. Chronic pain in Canada: have we improved our management of chronic Noncancer pain? Pain Res Manag 2007;12:39–47. 10.1155/2007/762180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moulin DE, Clark AJ, Speechley M, et al. Chronic pain in Canada--prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag 2002;7:179–84. 10.1155/2002/323085 [DOI] [PubMed] [Google Scholar]
- 48.Ramage-Morin PL, Gilmour H. Chronic pain at ages 12 to 44. Health Rep 2010;21:53–61. [PubMed] [Google Scholar]
- 49.Reitsma ML, Tranmer JE, Buchanan DM, et al. The prevalence of chronic pain and pain-related interference in the Canadian population from 1994 to 2008. Chronic Dis Inj Can 2011;31:157–64. [PubMed] [Google Scholar]
- 50.Gilmour H. Chronic pain, activity restriction and flourishing mental health. Health Rep 2015;26:15–22. [PubMed] [Google Scholar]
- 51.Ramage-Morin PL. Chronic pain in Canadian seniors. Health Rep 2008;19:37–52. [PubMed] [Google Scholar]
- 52.Hogan ME, Taddio A, Katz J, et al. Incremental health care costs for chronic pain in Ontario, Canada: a population-based matched cohort study of adolescents and adults using administrative data. Pain 2016;157:1626–33. 10.1097/j.pain.0000000000000561 [DOI] [PubMed] [Google Scholar]
- 53.Andrew R, Derry S, Taylor RS, et al. The costs and consequences of adequately managed chronic non-cancer pain and chronic neuropathic pain. Pain Pract 2014;14:79–94. 10.1111/papr.12050 [DOI] [PubMed] [Google Scholar]
- 54.Lacasse A, Pagé MG, Choinière M, et al. Conducting gender-based analysis of existing databases when self-reported gender data are unavailable: the GENDER index in a working population. Can J Public Health 2020;111:155–68. 10.17269/s41997-019-00277-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Methods Res 2007;35:542–71. 10.1177/0049124106292364 [DOI] [Google Scholar]
- 56.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 2010;6:109–38. 10.1146/annurev.clinpsy.121208.131413 [DOI] [PubMed] [Google Scholar]
- 57.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res 2001;29:374–93. 10.1177/0049124101029003005 [DOI] [Google Scholar]
- 58.Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods 1999;4:139–57. 10.1037/1082-989X.4.2.139 [DOI] [PubMed] [Google Scholar]
- 59.Nguena Nguefack HL, Pagé MG, Katz J, et al. Trajectory modelling techniques useful to epidemiological research: a comparative narrative review of approaches. Clin Epidemiol 2020;12:1205–22. 10.2147/CLEP.S265287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Johnson JL, Greaves L, Repta R. Better science with sex and gender: facilitating the use of a sex and gender-based analysis in health research. Int J Equity Health 2009;8:14. 10.1186/1475-9276-8-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bekker MHJ. Investigating gender within health research is more than sex disaggregation of data: a multi-facet gender and health model. Psychol Health Med 2003;8:231–43. 10.1080/1354850031000087618 [DOI] [Google Scholar]
- 62.Simard M, Sirois C, Candas B. Validation of the combined comorbidity index of Charlson and Elixhauser to predict 30-day mortality across ICD-9 and ICD-10. Med Care 2018;56:441–7. 10.1097/MLR.0000000000000905 [DOI] [PubMed] [Google Scholar]
- 63.Heidari S, Babor TF, De Castro P, et al. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev 2016;1:2. 10.1186/s41073-016-0007-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Canadian Institutes of Health Research . Online training modules: integrating sex & gender in health research - sex and gender in the analysis of data from human participants. Ottawa, 2017. Available: http://www.cihr-irsc.gc.ca/e/49347.html [Google Scholar]
- 65.Mena E, Bolte G, Bolte G, et al. Intersectionality-based quantitative health research and sex/gender sensitivity: a scoping review. Int J Equity Health 2019;18:199. 10.1186/s12939-019-1098-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nguena Nguefack HL, Pagé MG, Choinière M, et al. Distinct care trajectories among persons living with Arthritic conditions: a two-year state sequence analysis. Front Pain Res (Lausanne) 2022;3:1014793. 10.3389/fpain.2022.1014793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bauer G. Meet the methods series: quantitative intersectional study design and primary data collection, Issue 3 Part 1. Canadian Institutes of Health Research, 2021. [Google Scholar]
- 68.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter J Health Soc Behav 1995;36:1–10. [PubMed] [Google Scholar]
- 69.Babitsch B, Gohl D, von Lengerke T. Re-revisiting andersen’s behavioral model of health services use: a systematic review of studies from 1998-2011. Psychosoc Med 2012;9:Doc11. 10.3205/psm000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vatcheva KP, Lee M, McCormick JB, et al. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology (Sunnyvale) 2016;6:227. 10.4172/2161-1165.1000227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pilote L, Humphries KH. Incorporating sex and gender in cardiovascular research: the time has come. Can J Cardiol 2014;30:699–702. 10.1016/j.cjca.2013.09.021 [DOI] [PubMed] [Google Scholar]
- 72.Tannenbaum C, Ellis RP, Eyssel F, et al. Sex and gender analysis improves science and engineering. Nature 2019;575:137–46. 10.1038/s41586-019-1657-6 [DOI] [PubMed] [Google Scholar]
- 73.Tannenbaum C, Clow B, Haworth-Brockman M, et al. Sex and gender considerations in Canadian clinical practice guidelines: a systematic review. CMAJ Open 2017;5:E66–73. 10.9778/cmajo.20160051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thompson AE, Anisimowicz Y, Miedema B, et al. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract 2016;17:38. 10.1186/s12875-016-0440-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rasu RS, Bawa WA, Suminski R, et al. Health literacy impact on national healthcare utilization and expenditure. Int J Health Policy Manag 2015;4:747–55. 10.15171/ijhpm.2015.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Meghani SH, Gallagher RM. Disparity vs inequity: toward Reconceptualization of pain treatment disparities. Pain Med 2008;9:613–23. 10.1111/j.1526-4637.2007.00344.x [DOI] [PubMed] [Google Scholar]
- 77.Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action 2015;8:27106. 10.3402/gha.v8.27106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lacasse A, Cauvier Charest E, Dault R, et al. Validity of algorithms for identification of individuals suffering from chronic Noncancer pain in administrative databases: a systematic review. Pain Med 2020;21:1825–39. 10.1093/pm/pnaa004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lacasse A, Ware MA, Dorais M, et al. Is the Quebec provincial administrative database a valid source for research on chronic non-cancer pain? Pharmacoepidemiol Drug Saf 2015;24:980–90. 10.1002/pds.3820 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-070509supp001.pdf (115.7KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. TorSaDE Cohort data links Statistics Canada’s Canadian Community Health Survey (CCHS) data and Quebec Health Ministry data that are not publicly available. Access must be granted by the Institut de la statistique du Québec (ISQ) (data holder) and the Commission d’accès à l’information du Québec. Programming codes can be obtained directly from the corresponding author.