Abstract
Background
Effective teams are essential to high-quality healthcare. However, teams, team-level constructs, and team effectiveness strategies are poorly delineated in implementation science theories, models, and frameworks (TMFs), hindering our understanding of how teams may influence implementation. The Exploration, Preparation, Implementation, Sustainment (EPIS) framework is a flexible and accommodating framework that can facilitate the application of team effectiveness approaches in implementation science.
Main Text
We define teams and provide an overview of key constructs in team effectiveness research. We describe ways to conceptualize different types of teams and team constructs relevant to implementation within the EPIS framework. Three case examples illustrate the application of EPIS to implementation studies involving teams. Within each study, we describe the structure of the team and how team constructs influenced implementation processes and outcomes.
Conclusions
Integrating teams and team constructs into the EPIS framework demonstrates how TMFs can be applied to advance our understanding of teams and implementation. Implementation strategies that target team effectiveness may improve implementation outcomes in team-based settings. Incorporation of teams into implementation TMFs is necessary to facilitate application of team effectiveness research in implementation science.
Keywords: team, teamwork, implementation outcomes, EPIS
Plain Language Summary
Teams and team-level constructs are neglected in implementation theories, models, and frameworks (TMFs). This paper calls attention to the importance of teams in implementation research and practice and provides an overview of team effectiveness research for implementation science. We illustrate how the EPIS framework can be applied to advance our understanding of how teams influence implementation processes and outcomes. We identify future directions for research on teams and implementation, including developing and testing implementation strategies that focus on team effectiveness.
Background
Team effectiveness research examines how people work together to accomplish shared goals. Over a century of research on teams and numerous meta-analyses have identified team constructs critical to team effectiveness (Mathieu et al., 2017, 2019), and findings are widely applied in business, industry, healthcare, aviation, and military settings with proven results (Mathieu et al., 2019; Salas, Goodwin et al., 2008; Salas et al., 2013, 2017). Effective teams are productive, efficient, and innovative, while problems in teamwork can cause serious errors and failures (Burke et al., 2018; Gregory et al., 2013; Salas et al., 2017). In healthcare settings, interventions that improve teamwork improve clinical outcomes (Buljac-Samardzic et al., 2020; Hughes et al., 2016; Weaver et al., 2014). However, despite the increasing use of teams in healthcare, team effectiveness research is underutilized, and teams are poorly delineated in the implementation TMFs.
In this paper, we define teams, provide an overview of key constructs in team effectiveness research, and highlight examples of studies that test associations of team constructs with implementation outcomes. Next, we demonstrate how the Exploration, Preparation, Implementation, Sustainment (EPIS) framework (Aarons et al., 2011; Moullin et al., 2019) can be used to integrate and apply team research in implementation science. We describe how to conceptualize different types of teams within the EPIS framework and illustrate them with examples. Finally, we discuss future directions to advance research on teams in implementation science and practice.
Defining Teams
Across healthcare and related service sectors, work is increasingly completed by teams of professionals (Institute of Medicine, 2001; Kerrissey et al., 2023; Mitchell et al., 2012; Rosen et al., 2018; Rosland et al., 2013; Sandoval et al., 2018). A team is “a distinguishable set of two or more people who interact dynamically, interdependently, and adaptively toward a common and valued goal/objective/mission” (Salas et al., 1992, p. 4). Teams engage in both taskwork and teamwork. Taskwork refers to the work-related activities that teams are doing; teamwork describes how teams are doing their work (Dinh & Salas, 2017; Marks et al., 2001). Hackman (2002) described “real teams” as those with a shared task, clear boundaries, authority to manage their work, and reasonable membership stability. Other traditional definitions of teams also emphasize the importance of stability and clear team member role definitions (Kozlowski & Bell, 2003; Rousseau et al., 2006). Many modern teams, however, exhibit dynamic fluctuations in membership and boundaries, making defining teams an ongoing challenge (Benishek & Lazzara, 2019; Kerrissey et al., 2020, 2023; Mathieu et al., 2019).
A key feature distinguishing teams from small groups is interdependence—the extent to which team members are interconnected (Courtright et al., 2015; Kozlowski & Bell, 2003). Task interdependence is “the degree to which taskwork is designed so that team members depend upon one another for access to critical resources and create workflows that require coordinated action” (Courtright et al., 2015, p. 4). Outcome interdependence is “the degree to which the outcomes of taskwork are measured, rewarded, and communicated at the group level” (Courtright et al., 2015, p. 4). Although interdependence varies across teams, task interdependence is an essential feature of teams (Courtright et al., 2015; Kozlowski & Bell, 2003).
Teams can be differentiated from groups of individuals who may work together but who do not constitute a team. For example, in the patient-centered medical home model for primary care practices, providers work as part of a care team that may include medical assistants, nurses, and care coordinators. Instead of primary care providers holding sole responsibility, team members provide different but coordinated types of care and share responsibility for patient outcomes at the team level (Fiscella & McDaniel, 2018). In contrast, consider outpatient mental health clinicians delivering psychotherapy in the same organization. This group is clearly bounded and may have a shared supervisor, but the clinicians can complete their clinical work independently and are evaluated separately. Thus, they would not be classified as a team.
Teams may be constructed from groups. For example, if clinicians formed a workgroup to revise their clinic's intake process, they would become a team. The team members have a shared purpose, depend on one another to complete tasks, and are evaluated on shared output. Similarly, organizations may choose to create multidisciplinary teams of clinicians who work together to provide patient care and share responsibility for outcomes (Miller et al., 2022). In some team-based models, the patient and their family are explicitly included as part of the team (Drake et al., 2009; Katkin et al., 2017).
Attention to teams in implementation science has focused primarily on implementation support teams (Higgins et al., 2012; Metz & Bartley, 2020). An implementation team is “a group of stakeholders that oversees, attends to, and is accountable for facilitating key activities in the selection, implementation, and continuous improvement of an intervention” (Metz & Bartley, 2020, p. 200). In an early synthesis of the implementation science literature, D. L. Fixsen et al. (2005) identified the creation of implementation teams as a critical strategy during the exploration phase. The Active Implementation Frameworks highlight the importance of implementation teams at multiple levels with competencies in implementation, innovation, and change management (A. A. M. Fixsen et al., 2021; Metz & Bartley, 2020; Metz et al., 2014). Similarly, the updated Consolidated Framework for Implementation Research now includes “implementation team members” in the individuals domain and “teaming” (“intentionally coordinating and collaborating on interdependent tasks to implement the innovation”) in the implementation process domain (Damschroder et al., 2022).
Other types of teams are also relevant for implementation science. Common team archetypes in the implementation science literature (in addition to implementation teams) include existing care teams selected to implement an innovation, care teams formed as part of the innovation (i.e., team-based service models such as assertive community treatment; Bond et al., 2001), and quality improvement teams (Mosel & Shamp, 1993; Tyler & Glasgow, 2021). Some implementation efforts may involve multiteam systems, in which several types of teams interact with one another in pursuit of shared goals (Luciano et al., 2018; Marks et al., 2005; Shuffler et al., 2015). Multiteam systems are “two or more teams that interface directly and interdependently in response to environmental contingencies toward the accomplishment of collective goals” (Mathieu et al., 2001, p. 290). For instance, an implementation effort could include existing teams expected to provide a new service, a team to train and coach service providers on the new practice, and support teams (e.g., technical assistance team and evaluation/research team). Each team has its own goals, but the teams depend on one another and must work together to achieve the broader shared goal of implementing the new practice. Table 1 describes the characteristics of these common team archetypes with examples from implementation studies. 1
Table 1.
Common team archetypes in implementation science
| Team type | Description | Examples |
|---|---|---|
| Implementation support team | The team is created to facilitate the implementation of an innovation. Members share responsibility for implementation. Teams may be within or across organizations/systems. Membership may be voluntary. Teams are typically time-limited. | Teams of external change agents and staff implementing diverse innovations in the Veterans Health Administration (Nevedal et al., 2020). Community-based teams tasked with selecting, implementing, and sustaining preventive interventions (Perkins et al., 2011). |
| Existing care team | Members share responsibility and work together to provide care. Implementation of an innovation requires participation and change from all members. | Surgical teams implementing the surgical safety checklist (Gillespie et al., 2016). Multidisciplinary child abuse teams implementing mental health screening (McGuier, Aarons, Byrne et al., 2023). |
| New care team | Implementation of the innovation requires providers to shift from individual responsibilities and tasks to sharing responsibility and working together. | Primary care teams in practices that begin implementing the patient-centered medical home model (Cromp et al., 2015). Creation of assertive community treatment teams (Phillips et al., 2001). |
| Quality improvement (QI) team | Members share responsibility for improving care. QI teams may be existing teams or new teams created for specific projects; teams typically exist within organizations. Membership may be voluntary. | QI teams working to improve chronic illness care at a hospital (Shortell et al., 2004). QI teams improve access to and quality of care for hepatitis C virus in a health system (Yakovchenko et al., 2021). |
| Multiteam system | Networks of interdependent teams working toward shared goals as well as individual team goals. | The leadership team (implementation support team), “seed team” responsible for training and coaching (implementation support team), and interagency collaborative teams delivering services (new care teams; Hurlburt et al., 2014) |
Team constructs for implementation science
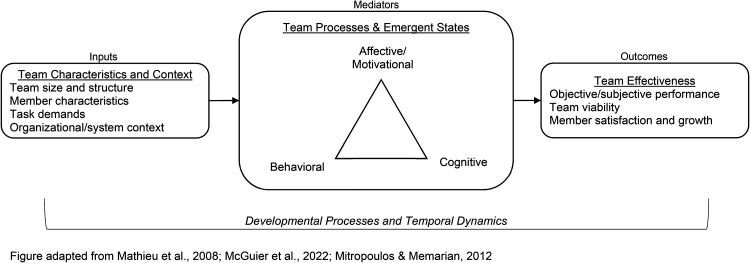
In this section, we briefly describe key team constructs for implementation scientists, guided by the input-mediator-outcome-input (IMOI) framework of team effectiveness (Ilgen et al., 2005; Mathieu et al., 2008). The IMOI model is widely used in team effectiveness research and has been applied to healthcare teams specifically (Rosen et al., 2018). It provides a broad framework to organize the diverse array of team constructs that may be relevant to implementation science. As shown in Figure 1, inputs are features of team members, teams, and their tasks and context that shape mediators and outcomes. Mediators are team processes and emergent states that are influenced by inputs to subsequently partly or fully affect outcomes (Ilgen et al., 2005; Mathieu et al., 2008). Outcomes are valued results of team activities, including diverse metrics of team effectiveness (Kozlowski & Bell, 2003; Mathieu et al., 2008; Rosen & Dietz, 2017).
Figure 1.
Conceptual model of team effectiveness
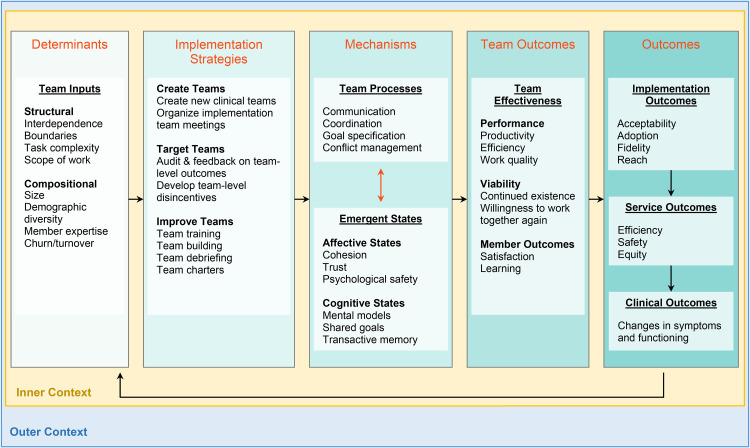
The IMOI framework is nonlinear, as teams are affected by complex temporal dynamics (see Mathieu et al., 2019 for a nonlinear visualization of the model). Teams develop over time, respond to changing tasks and contextual demands, and receive cyclical feedback (Georganta et al., 2021; Ilgen et al., 2005; Marks et al., 2001; Mathieu et al., 2008, 2014). Teams are also situated within organizational and system contexts and subject to external influences (Salas et al., 2003). We describe below some well-studied team constructs relevant to implementation science. Figure 2 illustrates examples of team constructs, organized by the IMOI model, integrated into an Implementation Research Logic Model (Smith et al., 2020).
Figure 2.
Implementation Research Logic Model with examples of team constructs and team-focused implementation strategies
Note. This figure was adapted from the Implementation Science and Team Effectiveness in Practice (IN STEP) Children's Mental Health Research Center (P50MH126231). Although this figure is organized linearly, there are recursive and nonlinear associations between these constructs.
Inputs: Team Structure and Composition
Team inputs include structural and compositional factors. Structural features of teams include task and outcome interdependence, task characteristics (e.g., complexity and scope of work), location in time and space (e.g., synchronous vs. asynchronous and virtual vs. in-person), and differentiation of skills and authority within the team (Hollenbeck et al., 2012; Kozlowski & Bell, 2003; Mathieu et al., 2017, 2019). Compositional features refer to the combination of team members’ characteristics. Examples include team size, demographic and professional diversity, team member attributes (e.g., skills and personality), and changes in team members (i.e., “churn” or turnover; Jackson et al., 2003; Kozlowski & Bell, 2003; Mathieu et al., 2017, 2019).
Mediators: Team Processes and States
Mediators are team processes and states that may be affective, behavioral, or cognitive (Grossman et al., 2017; Ilgen et al., 2005; Mathieu et al., 2008; Mitropoulos & Memarian, 2012). Affective/motivational and cognitive mediators are conceptualized as emergent states arising from behavioral team processes; they can also serve as inputs that impact behavioral team processes (Marks et al., 2001). Team functioning is a broad term referring to multiple, intertwined processes and states. Many specific processes and states, as well as overall team functioning, are associated with team effectiveness.
Behavioral team processes describe what team members do—how they interact with one another, their task(s), and their resources to produce outcomes. Marks et al. (2001, p. 357) define team processes as “members’ interdependent acts that convert inputs to outcomes through cognitive, verbal, and behavioral activities directed toward organizing taskwork to achieve collective goals.” Their conceptual framework of team processes identifies three broad categories of processes: transition processes occurring between performance episodes, action processes occurring as members engage in active work, and ongoing interpersonal processes (Marks et al., 2001; Mathieu et al., 2020). Processes can be narrowly or broadly defined; research supports a hierarchical structure of processes consistent with Marks et al.’s (2001) framework (LePine et al., 2008; Mathieu et al., 2020). Examples of behavioral processes are mission analysis, goal specification, communication, coordination, backup/supporting behavior, learning behavior, and conflict management (Bisbey & Salas, 2019; Grossman et al., 2017; Kozlowski & Ilgen, 2006). These processes can be further delineated into types of behaviors or specific dimensions, such as communication quality and frequency (Marlow, Lacerenza et al., 2018) or types of learning behaviors (Wiese et al., 2022).
Affective/motivational states reflect shared feelings and attitudes that emerge from team members’ interactions with each other (Bisbey & Salas, 2019; Grossman et al., 2017). Examples include team cohesion, collective efficacy, trust, and psychological safety (Grossman et al., 2017; Kozlowski & Bell, 2003). Well-studied cognitive states include team mental models and transactive memory (DeChurch & Mesmer-Magnus, 2010; Mohammed et al., 2017; Ren & Argote, 2011). Mental models are “organized mental representations of the key elements within a team's relevant environment that are shared across team members” (Mohammed et al., 2010, p. 877). When team members are “on the same page” about what to do and how to do it, teams perform better (Mohammed et al., 2010). Transactive memory refers to how teams encode, store, and retrieve information by building a shared awareness of who knows what, allowing increasing specialization and greater cognitive efficiency (Ren & Argote, 2011).
Processes and states are closely intertwined. For example, the affective state of psychological safety (i.e., the extent to which interpersonal risk-taking is safe) is associated with learning behaviors (e.g., seeking feedback and discussing errors; Edmondson, 1999). Shared mental models increase coordination, therefore improving team performance (Marks et al., 2002). Because of reciprocal associations between processes and states, they may be conceptualized as inputs, mediators, or outcomes, depending on the research question.
Outcomes: Team Effectiveness
We use the term “team effectiveness” as an overarching term for team outcomes, acknowledging that an outcome can vary across studies given the complexity of temporal dynamics within teams. Hackman and colleagues’ model of team effectiveness (Hackman, 1983, 2012; Hackman & Wageman, 2005) specifies three dimensions of team effectiveness: (a) perceptions of the team's output by those who receive, review, or use it (i.e., performance); (b) the extent to which the team improves their capacity to work together and the sustainment of the team over time (i.e., team viability), and (c) the impact of the team on members’ learning and development. Teams can be effective in different ways and at multiple levels.
Although effectiveness and performance are sometimes used interchangeably, we use team performance to indicate the first dimension of effectiveness. Team performance refers to the quality, efficiency, and productivity of teams (Rosen & Dietz, 2017; Slyngstad et al., 2017). For example, a team may increase organizational profits, produce innovative products, or attain effective implementation or service outcomes (e.g., reach, fidelity, and safety; Proctor et al., 2011). Performance is context-specific and depends on the goals of the team; it is typically assessed at the team or organizational level. The latter two dimensions of effectiveness (i.e., team viability and impact on members) are often assessed at the team and individual levels. Effectiveness may be demonstrated through member satisfaction and team viability (e.g., members want to continue on the team) as well as gains in team members’ skills, knowledge, and self-efficacy (Bisbey & Salas, 2019; Slyngstad et al., 2017). Importantly, given the dynamic nature of teams, these team outcomes serve as inputs into recurring and dynamic cycles of team interactions.
Research on Teams and Implementation
Relatively few studies have examined how team constructs impact implementation of evidence-based practices (EBPs; McGuier et al., 2022). In existing care teams, more adaptive team functioning has been associated with greater improvements in chronic care delivery (Cramm et al., 2014), implementation of more elements of a mental health EBP (Ditty et al., 2015), and greater EBP sustainment in outpatient mental health clinics (Mohr et al., 2018). A study of implementation support teams found that “early adopter” teams had better team functioning than later adopters (Yakovchenko et al., 2021). Some studies have examined how team effectiveness affects implementation outcomes. One study of teams responding to child abuse found that team members’ subjective perceptions of overall team performance were positively associated with innovation acceptability, appropriateness, and feasibility, but not reach (McGuier, Aarons, Byrne et al., 2023).
Overall, prior studies support the relevance of team constructs and approaches for implementation. However, team constructs are often poorly specified, and findings are rarely situated in the well-developed literature on teams. The small number of studies and heterogeneity in team types and constructs limits our capacity to identify team-level targets and mechanisms of change. Building our understanding of how teams affect implementation requires a better conceptualization of team-level constructs in implementation science TMFs.
Application of the EPIS Framework to Implementation Research With Teams
Conceptualizing Teams Within the EPIS Framework
Teams and team constructs are not explicitly included in most implementation TMFs, hindering our capacity to understand the diverse ways that teams influence implementation processes and outcomes. The EPIS framework (Aarons et al., 2011; Moullin et al., 2019) is a widely used process and determinant implementation framework (Moullin et al., 2019). Although EPIS, like other TMFs, does not highlight teams, EPIS is a flexible framework that can facilitate the application of team effectiveness approaches.
EPIS invokes the outer system context, inner organizational context, bridging factors that span and link outer and inner contexts, innovation characteristics and developers, and interconnections and linkages within and across contexts (Lengnick-Hall et al., 2021; Moullin et al., 2019). EPIS identifies four implementation phases within which teams may function (Moullin et al., 2019). Teams can be conceptualized in multiple ways within EPIS depending on their composition, level, functions, and existence across implementation phases. EPIS can accommodate existing teams within and across outer and inner contexts, the creation and efforts of implementation support teams, and multiteam systems. In the following sections, we illustrate how team constructs fit within the EPIS framework.
Inner Context
The EPIS inner context refers to factors within an organization (e.g., leadership, staffing, and individual characteristics) that may be associated with implementation processes and outcomes. Many teams operate within the inner context, as teams within organizations. Within the inner organizational context, different types of teams may be identified. For example, within a hospital, there may be surgical teams, care teams on specific units, and administrative teams. For teams within organizations, team characteristics can be considered part of the inner context, alongside individual and organizational characteristics.
Outer Context
The outer context refers to factors in the environment outside the organization, such as policy/regulatory context and patient/client population characteristics that may be associated with implementation processes and outcomes. Some teams exist within the outer context and shape service environments, funding, and inter-organizational networks. For example, in the United States, state service systems may be characterized by functions or focus areas such as public health, behavioral health services, adult services, child services, funding, and contracting. Individuals from different divisions may work together as a team on initiatives such as creating dedicated EBP funding streams (Crable et al., 2022). Similarly, state leadership teams may be created to improve public health through cross-system collaboration (Brown et al., 2023).
Bridging Factors
While teams can operate within outer or inner contexts, some teams span system and organization levels and can be conceptualized as engaging in bridging or being bridging factors (Lengnick-Hall et al., 2021). Bridging factors include “relational ties, formal arrangements, and processes” that link the inner and outer context (Lengnick-Hall et al., 2021, p. 2), such as research-community partnerships (Brookman-Frazee et al., 2016, 2020). For example, in one study, community and academic partners interacted to develop system-level contracting arrangements to support implementation of EBPs for substance use disorders (Crable et al., 2022). These contracting arrangements are a bridging factor formally connecting the outer context of the system to the inner context of community-based organizations.
Interconnections and Linkages
EPIS also explicitly includes “interconnections, interactions, linkages, and relationships” within and across domains. In contrast to bridging factors which formally link outer and inner contexts, interconnections and linkages are more informal and can exist within and across domains, between individuals, or between formal entities such as groups or organizations. Interconnections and linkages can shape implementation processes and outcomes through individuals’ influence on one another, personal relationships, and interaction histories.
Implementation Phases
The EPIS phases provide a way to stage team activities through the implementation process. This may include the creation of implementation support teams and the act of “teaming” during implementation (i.e., a dynamic “way of working that brings people together to generate new ideas, find answers, and solve problems”; Edmondson, 2012, p. 24). The phases also provide a framework for considering planned and ad hoc changes to team configuration and/or relevant teams over time and across phases (Becan et al., 2018). Lastly, EPIS phases are recursive and can be used to identify potential team challenges during each phase and consider additions or revisions to team-based implementation strategies as teams evolve.
Case Examples Illustrating Application of the EPIS Framework
In the following section, we describe three case examples of implementation studies involving teams, situate the teams within the EPIS framework, and describe how team constructs influenced implementation processes and/or outcomes. Table 2 lists the type of teams studied, their position within EPIS domains, and the team constructs examined in each study.
Table 2.
Examples of implementation studies examining team constructs
| Example 1 Teams Improving Chronic Illness Care |
Example 2 Community-Based Prevention Teams |
Example 3 Interagency Collaborative Teams |
|
|---|---|---|---|
| Team type | Quality improvement teams | Implementation support teams | Multiteam system
|
| EPIS domain | Inner context: Teams within healthcare organizations | Outer context: Cross-sector teams within communities | Bridging factors: Cross-sector leadership team and interagency provider teams. |
| Team constructs | |||
| Inputs | Composition Size |
Member expertise Membership (in)stability |
|
| Mediators (processes and states) | Team functioning Integration of new members Participation Collaboration with prevention coordinators (linkage quality) |
Shared vision, role clarity, conflict and conflict management, communication, trust Interagency communication |
|
| Outcomes | Effectiveness |
Example 1: Teams Improving Chronic Illness Care (Quality Improvement Teams)
Shortell et al. (2004) assessed healthcare system teams participating in a learning collaborative to improve chronic care management using quality improvement methods (Cretin et al., 2004). The collaborative was sponsored by an external organization with the goal of creating a network and empowering teams to make effective changes. Participating healthcare organizations were expected to create interdisciplinary teams supported by organizational leadership (Cretin et al., 2004). The teams in this example were situated within the inner context of healthcare organizations with strong interconnections with the collaborative, a bridging factor.
The study tested associations between team composition (i.e., presence of champion and proportion of physicians), size, effectiveness, and the number of changes made and the depth of changes (i.e., expert ratings of expected impact on patient outcomes; Shortell et al., 2004). The reported presence of a team champion and a greater proportion of physicians were positively associated with team members’ ratings of effectiveness. Team composition was not directly associated with the number or depth of changes. Team size was negatively associated with effectiveness and curvilinearly associated with the depth of changes, with a positive association initially and then a negative association as teams became larger (>10 members). Team effectiveness was positively associated with both the number and depth of changes, indicating that teams who consider themselves more effective take more actions (and more impactful actions) to improve care (Shortell et al., 2004). Importantly, team-level constructs in this study were examined alongside organization-level measures (e.g., organizational culture). These findings suggest that team- and organization-level constructs have unique influences on implementation, even when teams are situated within the inner context of an organization.
Example 2: Community-Based Prevention Teams (Implementation Support Teams)
The PROSPER study created teams in participating communities to select, implement, and sustain evidence-based prevention programming for youth and families. Prevention teams included Cooperative Extension Service educators, representatives from schools and community agencies, parents, and youth. They worked closely with academic researchers and prevention coordinators who provided consultation and technical assistance. The PROSPER model resulted in high implementation quality that was sustained over time (Spoth et al., 2007, 2011).
Prevention teams are conceptualized as part of the outer context, with strong interconnections/linkages to academics and prevention coordinators who act as intermediaries (bridging factors). Although individual members of the prevention teams were part of organizations, the teams themselves were not situated within any one organization or inner context. Prevention teams were formed early in Exploration and remained active through Preparation, Implementation, and Sustainment (Spoth et al., 2007).
Perkins et al. (2011) examined whether prevention team functioning during early phases predicted sustainability planning two years later. Using a global measure of team functioning, they found strong positive correlations between team functioning and the team's expertise for sustainment and funding plans, as rated by both team members and external consultants (Perkins et al., 2011). Integration of new team members, team participation, and perceptions of leadership and community support was also associated with later expertise and funding plans (Perkins et al., 2011). Another study from this project found that the quality of collaboration between the prevention team and prevention coordinator predicted later team functioning (Chilenski et al., 2016). These findings indicate that the quality of linkages between the outer context and bridging factors influences the functioning of teams, which in turn influences EBP sustainment.
Example 3: Interagency Collaborative Teams (Multiteam System)
The Interagency Collaborative Team (ICT) model is an example of how implementation support teams, new care teams, and their interactions in a multiteam system can be leveraged to support EBP implementation (Aarons et al., 2014; Hurlburt et al., 2014). The ICT model was used to implement an EBP for child neglect in a large urban county. Teams were created within and across levels to support implementation, funded by a large investment from a philanthropic organization.
Core components of the ICT model included creating a cross-level, interagency leadership team focused on practice change, a “seed team” trained and certified to be a local training and coaching resource, and service-level interagency collaborative teams that were trained by the seed team and delivered the EBP across the service area. Although each team had its own specific goals, the teams needed to interact directly and interdependently with one another to achieve the superordinate goal of EBP implementation (Hurlburt et al., 2014).
The leadership team was a bridging factor linking the outer and inner context. It was composed of representatives from the philanthropic funder, child welfare system, and advocacy organizations (outer context), as well as representatives from community-based service agencies (inner context). It had strong linkages to other bridging factors, including academic partners and intervention developers. The seed team had members from two organizations and the interagency collaborative teams were comprised of providers from two or more organizations working under a common supervisor to provide services across different regions. Both the seed team and the interagency collaborative teams were composed of staff from multiple agencies to distribute local expertise and enhance interagency communication (Hurlburt et al., 2014). The ICT model was successful in implementing the EBP, which has been sustained for over six years.
Each team played a critical role in the multiteam system created by the ICT model, with their importance and influence varying across implementation phases (Aarons et al., 2014). During the Exploration phase, the funder collaborated with the child welfare system, community-based provider organizations, and advocacy organizations to identify population service needs, select an EBP, and create a vision for sustained evidence-based services for child neglect. During the Preparation phase, the cross-level leadership team developed strategies and processes to support implementation and sustainment. The seed team was developed during the Implementation phase and was closely linked to EBP developers and key stakeholders, especially early in implementation. Throughout the Implementation phase, the seed team provided ongoing supervision and coaching for newly trained interagency collaborative teams. Contracts, funding, and detailed statements of work were bridging factors that formalized and strengthened the multiteam system (Aarons et al., 2014; Hurlburt et al., 2014). Informal connections between individuals varied in nature and degree and influenced team interactions.
Key themes identified during implementation included the quality of collaboration between key stakeholders, communication within and between teams, and leadership (Hurlburt et al., 2014). At times, differences in expectations and ambiguity in roles, responsibilities, and authority created power dynamics, conflicts, and strained relationships (Aarons et al., 2014; Hurlburt et al., 2014). Without a clear communication structure, breakdowns occurred, and some stakeholders reported feeling “out of the loop” or unsure who to contact with questions. Critical to overcoming these challenges were a clear goal for EBP sustainment, a shared vision, realistic expectations for implementation, and a willingness to persevere (Aarons et al., 2014). Although complex, the process of contract negotiation was effective in clarifying roles and responsibilities and resolving fiscal and operational concerns. Early successes in implementation helped reduce power struggles, increase trust, and facilitate communication and joint problem-solving (Aarons et al., 2014; Hurlburt et al., 2014). Results suggest that explicit processes for communication and conflict management, a shared problem-solving orientation, and commitment to a shared vision are critical to teams’ capacity to provide the structural and process supports needed for implementation success (Aarons et al., 2014; Hurlburt et al., 2014).
Future Directions
Conducting Rigorous Implementation Research with Teams
Teams have received little attention in implementation science. Incorporating teams into TMFs may increase attention to their importance and provide new team-level targets for implementation strategies. Increasing attention to teams in implementation research must be accompanied by efforts to improve the description of teams and reporting of team-level findings. An ongoing systematic review of teams in implementation research found that the term “team” was often used without any description and sometimes used to refer to groups that did not actually constitute a team (e.g., staff in an organization who work independently; McGuier et al., 2021, 2022). Better description and reporting of team structures, processes, and outcomes will allow us to identify and replicate associations between team constructs and implementation outcomes to isolate robust predictors that can be targeted in implementation efforts.
Measurement of team constructs should be informed by existing theory and research. While the IMOI framework is a helpful starting point, other models of team effectiveness provide more specific theories about drivers of team effectiveness (e.g., Hackman, 2012; Tannenbaum & Salas, 2020), developmental processes in teams (e.g., Tuckman, 1965), and team interventions (Hackman & Wageman, 2005; Tannenbaum & Cerasoli, 2013); these models may be useful in developing and testing specific research questions. An array of well-validated measures of team constructs are available, including measures that are aligned with theories of team effectiveness (e.g., Mathieu et al., 2020; see Marlow, Bisbey et al., 2018; Valentine et al., 2014). Team constructs can also be assessed through observational measures and unobtrusive methods using existing data. For example, natural language processing methods can be applied to routinely produced materials (e.g., agendas, notes, and recordings/transcripts) to evaluate team functioning during meetings. Improving the measurement of team constructs is critical to enhancing the rigor of research on teams and implementation.
Implementation Strategies Targeting Teams
In team-based settings, implementation strategies that target team effectiveness may improve implementation outcomes (see Figure 2). Teams are promising targets because they can remain relatively stable even when individual members leave or change positions. Teams may also change more quickly than organizations. In addition, strategies that improve care team effectiveness may improve clinical outcomes above and beyond the effects of the EBP. However, implementation strategy compilations do not provide sufficient guidance for how to target the team level or include strategies to improve team effectiveness (Powell et al., 2015).
Implementation strategies targeting team effectiveness are intended to change how teams work together (i.e., teamwork) and can be applied to teams engaged in diverse taskwork. These strategies may take three forms: (a) existing implementation strategies that create teams, (b) existing implementation strategies that can be modified to target teams, and (c) novel implementation strategies that draw from team development interventions (TDIs) and aim to improve teams. Some strategies included in the Expert Recommendations for Implementing Change (ERIC) compilation involve the creation of teams (e.g., create new clinical teams, organize clinician implementation team meetings; Powell et al., 2015). However, little guidance is provided about how to apply these team-based strategies or evaluate their effectiveness in the context of implementation. Future research could examine team structure and processes as potential moderators or mediators of the effectiveness of these strategies, as well as ways to support new teams over time and across different phases of the implementation process. Other frequently used ERIC strategies could be easily adapted to target the team level. For example, audit and feedback could be leveraged to increase outcome interdependence in teams (i.e., attention to team vs. individual outcomes). Alongside support for collaboration, this strategy may improve work performance (Markon et al., 2017).
Another approach is to add or incorporate effective TDIs. TDIs can improve team functioning and patient outcomes in real-world settings (Hughes et al., 2016; Klein et al., 2009; McCulloch et al., 2011; McEwan et al., 2017; Miller et al., 2018; Salas, DiazGranados et al., 2008; Shuffler et al., 2018). Two well-established types of TDIs are team training (Salas, DiazGranados et al., 2008) and team building (Klein et al., 2009; Miller et al., 2018). Team training targets team members’ knowledge, skills, and attitudes through strategies such as team self-correction, coordination training, and cross-training and is effective in improving team functioning (Hughes et al., 2016; Salas, DiazGranados et al., 2008; Sheppard et al., 2013; Weaver et al., 2014). Team building targets goal-setting, relationship management, role clarification, and/or problem-solving and is effective in improving behavioral processes and affective states (Klein et al., 2009; Miller et al., 2018). Other effective TDIs include team debriefs (Tannenbaum & Cerasoli, 2013), team coaching (Hackman & Wageman, 2005), team charters (Sverdrup & Schei, 2015), and team leadership (Burke et al., 2011). For more information on effective TDIs, see Buljac-Samardzic et al. (2020), Lacerenza et al. (2018), and Shuffler et al. (2011, 2018).
Despite strong evidence for TDIs, they have not been considered in the implementation TMFs. TDIs can be delivered alongside implementation strategies or integrated into specific implementation strategies. For example, an implementation effort could include training providers in the EBP (implementation strategy) as well as training in communication skills (TDI). As another example, the organization of clinical implementation team meetings (implementation strategy) could incorporate the creation of team charters (TDI). In this case, the TDI adds additional structure to enhance the effectiveness of the implementation strategy. Team processes and states should be considered as possible mechanisms of effectiveness when testing team-based implementation strategies.
To date, there has been limited attention to teamwork processes and their relevance to implementation strategies. Ongoing research on teams and team-based models in healthcare highlights the importance of teams in healthcare settings. Incorporating evidence-based team interventions may improve the effectiveness of implementation strategies. A new research center (P50MH126231) and ongoing research studies (Kolko et al., 2022; McGuier, Aarons, Wright et al., 2023) focused on developing and testing novel team-based strategies will advance understanding of these implementation strategies.
Conclusions
Effective teams are critical to high-quality healthcare. Despite the increasing use of teams to provide services and reliance on teams to implement new practices, teams, and team-level constructs are neglected in implementation TMFs. We integrated teams and team constructs into the EPIS framework, demonstrating how EPIS can be applied to advance our understanding of teams and implementation. We encourage implementation scientists to consider how the complexity of teams and team dynamics impact implementation research and practice. Integration of team effectiveness research, including testing implementation strategies targeting teams, can optimize the efficiency and effectiveness of implementation efforts in team-based service settings.
Acknowledgments
The conceptualization of team-based implementation strategies was informed by the development of the Implementation Science and Team Effectiveness in Practice (IN STEP) Children's Mental Health Research Center (P50MH126231; PIs: Brookman-Frazee [contact], Aarons).
“Team science” is also relevant to implementation research, but outside the scope of this paper. Team science is research conducted by collaborative, cross-disciplinary, and interdependent groups of researchers. The “science of team science” refers to research on the processes and outcomes of team science initiatives. Interested readers are referred to (Hall et al., 2018; Liu et al., 2020).
Footnotes
Authors’ contributions: EAM and GAA conceptualized the manuscript. EAM led manuscript development and writing. DJK, NAS, LBF, CBW, CSB, and GAA reviewed multiple drafts of the manuscript and provided critical input and editing. CTY contributed to manuscript revisions. All authors approved the final manuscript.
Availability of Data and Materials: Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: GAA is a member of the Implementation Research and Practice Editorial Board; all decisions on this paper were made by other editors. The authors declare that they have no other conflicting interests.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Drug Abuse, National Institute of Mental Health, and Agency for Healthcare Research and Quality (grant numbers DA049891, MH123729, MH124914, MH126231, and HS026862).
ORCID iD: Elizabeth A. McGuier https://orcid.org/0000-0002-6219-6358
References
- Aarons G. A., Fettes D. L., Hurlburt M. S., Palinkas L. A., Gunderson L., Willging C. E., Chaffin M. J. (2014). Collaboration, negotiation, and coalescence for interagency-collaborative teams to scale-up evidence-based practice. Journal of Clinical Child & Adolescent Psychology, 43(6), 915–928. 10.1080/15374416.2013.876642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons G. A., Hurlburt M., Horwitz S. M. (2011). Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health, 38(1), 4–23. 10.1007/s10488-010-0327-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becan J. E., Bartkowski J. P., Knight D. K., Wiley T. R. A., DiClemente R., Ducharme L., Welsh W. N., Bowser D., McCollister K., Hiller M., Spaulding A. C., Flynn P. M., Swartzendruber A., Dickson M. F., Fisher J. H., Aarons G. A. (2018). A model for rigorously applying the exploration, preparation, implementation, sustainment (EPIS) framework in the design and measurement of a large scale collaborative multi-site study. Health & Justice, 6(1), 9. 10.1186/s40352-018-0068-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benishek L. E., Lazzara E. H. (2019). Teams in a new era: Some considerations and implications. Frontiers in Psychology, 10, 1006. 10.3389/fpsyg.2019.01006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisbey T., Salas E. (2019). Team dynamics and processes in the workplace. In Oxford research encyclopedia of psychology. Oxford University Press. 10.1093/acrefore/9780190236557.013.13 [DOI] [Google Scholar]
- Bond G. R., Drake R. E., Mueser K. T., Latimer E. (2001). Assertive community treatment for people with severe mental illness. Disease Management and Health Outcomes, 9(3), 141–159. 10.2165/00115677-200109030-00003 [DOI] [Google Scholar]
- Brookman-Frazee L., Chlebowski C., Suhrheinrich J., Finn N., Dickson K. S., Aarons G. A., Stahmer A. (2020). Characterizing shared and unique implementation influences in two community services systems for autism: Applying the EPIS framework to two large-scale autism intervention community effectiveness trials. Administration and Policy in Mental Health and Mental Health Services Research, 47(2), 176–187. 10.1007/s10488-019-00931-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L., Stahmer A., Stadnick N., Chlebowski C., Herschell A., Garland A. F. (2016). Characterizing the use of research-community partnerships in studies of evidence-based interventions in children’s community services. Administration and Policy in Mental Health and Mental Health Services Research, 43(1), 93–104. 10.1007/s10488-014-0622-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. B., Miller-Walfish S., Scott S., Ali A., Marjavi A., Miller E., McGuier E. A. (2023). Cross-sector collaboration in project catalyst: Creating state partnerships to address the health impact of intimate partner violence. Preventive Medicine Reports, 33, 102204. 10.1016/j.pmedr.2023.102204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buljac-Samardzic M., Doekhie K. D., van Wijngaarden J. D. H. (2020). Interventions to improve team effectiveness within health care: A systematic review of the past decade. Human Resources for Health, 18(1), 2. 10.1186/s12960-019-0411-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke C. S., DiazGranados D., Salas E. (2011). Team leadership: A review and look ahead. In A. Bryman, D. L. Collinson, K. Grint, B. Jackson, & M. Uhl-Bien (Eds.), The Sage handbook of leadership. pp. 338–351. SAGE Publications. [Google Scholar]
- Burke C. S., Priest H. A., Salas E., Sims D., Mayer K. (2018). Stress and teams: How stress affects decision making at the team level. In: Performance under stress. CRC Press [Google Scholar]
- Chilenski S. M., Perkins D. F., Olson J., Hoffman L., Feinberg M. E., Greenberg M., Welsh J., Crowley D. M., Spoth R. (2016). The power of a collaborative relationship between technical assistance providers and community prevention teams: A correlational and longitudinal study. Evaluation and Program Planning, 54, 19–29. 10.1016/j.evalprogplan.2015.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtright S. H., Thurgood G. R., Stewart G. L., Pierotti A. J. (2015). Structural interdependence in teams: An integrative framework and meta-analysis. Journal of Applied Psychology, 100(6), 1825–1846. 10.1037/apl0000027 [DOI] [PubMed] [Google Scholar]
- Crable E. L., Benintendi A., Jones D. K., Walley A. Y., Hicks J. M., Drainoni M.-L. (2022). Translating Medicaid policy into practice: Policy implementation strategies from three US states’ experiences enhancing substance use disorder treatment. Implementation Science, 17(1), 3. 10.1186/s13012-021-01182-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramm J. M., Strating M. M. H., Nieboer A. P. (2014). The role of team climate in improving the quality of chronic care delivery: A longitudinal study among professionals working with chronically ill adolescents in transitional care programmes. BMJ Open, 4(5), e005369. 10.1136/bmjopen-2014-005369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cretin S., Shortell S. M., Keeler E. B. (2004). An evaluation of collaborative interventions to improve chronic illness care: Framework and study design. Evaluation Review, 28(1), 28–51. 10.1177/0193841X03256298 [DOI] [PubMed] [Google Scholar]
- Cromp D., Hsu C., Coleman K., Fishman P. A., Liss D. T., Ehrlich K., Johnson E., Ross T. R., Trescott C., Trehearne B., Reid R. J. (2015). Barriers and facilitators to team-based care in the context of primary care transformation. The Journal of Ambulatory Care Management, 38(2), 125–133. 10.1097/JAC.0000000000000056 [DOI] [PubMed] [Google Scholar]
- Damschroder L. J., Reardon C. M., Widerquist M. A. O., Lowery J. (2022). The updated consolidated framework for implementation research based on user feedback. Implementation Science, 17(1), 75. 10.1186/s13012-022-01245-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeChurch L. A., Mesmer-Magnus J. R. (2010). The cognitive underpinnings of effective teamwork: A meta-analysis. Journal of Applied Psychology, 95(1), 32–53. 10.1037/a0017328 [DOI] [PubMed] [Google Scholar]
- Dinh J. V., Salas E. (2017). Factors that influence teamwork. In E. Salas, R. Rico, & J. Passmore (Eds.), The Wiley Blackwell handbook of the psychology of team working and collaborative processes (pp. 13–41). John Wiley & Sons, Ltd. [Google Scholar]
- Ditty M. S., Landes S. J., Doyle A., Beidas R. S. (2015). It takes a village: A mixed method analysis of inner setting variables and dialectical behavior therapy implementation. Administration and Policy in Mental Health and Mental Health Services Research, 42(6), 672–681. 10.1007/s10488-014-0602-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake R. E., Cimpean D., Torrey W. C. (2009). Shared decision making in mental health: Prospects for personalized medicine. Dialogues in Clinical Neuroscience, 11(4), 455–463. 10.31887/DCNS.2009.11.4/redrake [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmondson A. C. (1999). Psychological safety and learning behavior in work teams. Administrative Science Quarterly, 44(2), 350–383. 10.2307/2666999 [DOI] [Google Scholar]
- Edmondson A. C. (2012). Teaming: How organizations learn, innovate, and compete in the knowledge economy (1st ed.). Jossey-Bass. [Google Scholar]
- Fiscella K., McDaniel S. H. (2018). The complexity, diversity, and science of primary care teams. American Psychologist, 73(4), 451–467. 10.1037/amp0000244 [DOI] [PubMed] [Google Scholar]
- Fixsen A. A. M., Aijaz M., Fixsen D. L., Burks E., Schultes M.-T. (2021). Implementation frameworks: An analysis. Active Implementation Research Network. https://www.activeimplementation.org/wp-content/uploads/2021/04/AIRN-AFixsen-FrameworksAnalysis-2021.pdf
- Fixsen D. L., Naoom S. F., Blase K. A., Friedman R. M., Wallace F. (2005). Implementation research: A synthesis of the literature . http://centerforchildwelfare2.fmhi.usf.edu/kb/Implementation/Implementation%20Research%20-%20A%20Synthesis%20of%20Literature%20%20-%202005.pdf
- Georganta E., Burke C. S., Merk S., Mann F. (2021). Understanding how team process-sequences emerge over time and their relationship to team performance. Team Performance Management: An International Journal, 27(1/2), 159–174. 10.1108/TPM-03-2020-0018 [DOI] [Google Scholar]
- Gillespie B. M., Withers T. K., Lavin J., Gardiner T., Marshall A. P. (2016). Factors that drive team participation in surgical safety checks: A prospective study. Patient Safety in Surgery, 10(3), 1–9. 10.1186/s13037-015-0090-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory M. E., Feitosa J., Driskell T., Salas E. (2013). Designing, delivering, and evaluating team training in organizations: Principles that work. In Salas E., Tannenbaum S. I., Cohen D., Latham G. (Eds.), Developing and enhancing teamwork in organizations: Evidence-based best practices and guidelines (pp. 441–487). Jossey-Bass. [Google Scholar]
- Grossman R., Friedman S. B., Kalra S. (2017). Teamwork processes and emergent states. In E. Salas, R. Rico, & J. Passmore (Eds.), The Wiley Blackwell handbook of the psychology of team working and collaborative processes (pp. 243–269). John Wiley & Sons, Ltd. [Google Scholar]
- Hackman J. R. (1983). A normative model of work team effectiveness. Office of Naval Research. https://apps.dtic.mil/sti/citations/ADA136398
- Hackman J. R. (2012). From causes to conditions in group research. Journal of Organizational Behavior, 33(3), 428–444. 10.1002/job.1774 [DOI] [Google Scholar]
- Hackman, J. R. (2002). Leading teams: Setting the stage for great performances. Harvard Business Press. [Google Scholar]
- Hackman J. R., Wageman R. (2005). A theory of team coaching. The Academy of Management Review, 30(2), 269–287. 10.2307/20159119 [DOI] [Google Scholar]
- Hall K. L., Vogel A. L., Huang G. C., Serrano K. J., Rice E. L., Tsakraklides S. P., Fiore S. M. (2018). The science of team science: A review of the empirical evidence and research gaps on collaboration in science. American Psychologist, 73(4), 532–548. 10.1037/amp0000319 [DOI] [PubMed] [Google Scholar]
- Higgins M. C., Weiner J., Young L. (2012). Implementation teams: A new lever for organizational change. Journal of Organizational Behavior, 33(3), 366–388. 10.1002/job.1773 [DOI] [Google Scholar]
- Hollenbeck J. R., Beersma B., Schouten M. E. (2012). Beyond team types and taxonomies: A dimensional scaling conceptualization for team description. Academy of Management Review, 37(1), 82–106. 10.5465/amr.2010.0181 [DOI] [Google Scholar]
- Hughes A. M., Gregory M. E., Joseph D. L., Sonesh S. C., Marlow S. L., Lacerenza C. N., Benishek L. E., King H. B., Salas E. (2016). Saving lives: A meta-analysis of team training in healthcare. Journal of Applied Psychology, 101(9), 1266–1304. 10.1037/apl0000120 [DOI] [PubMed] [Google Scholar]
- Hurlburt M., Aarons G. A., Fettes D., Willging C., Gunderson L., Chaffin M. J. (2014). Interagency collaborative team model for capacity building to scale-up evidence-based practice. Children and Youth Services Review, 39, 160–168. 10.1016/j.childyouth.2013.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen D. R., Hollenbeck J. R., Johnson M., Jundt D. (2005). Teams in organizations: From input-process-output models to IMOI models. Annual Review of Psychology, 56, 517–543. 10.1146/annurev.psych.56.091103.070250 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press. [PubMed] [Google Scholar]
- Jackson S. E., Joshi A., Erhardt N. L. (2003). Recent research on team and organizational diversity: SWOT analysis and implications. Journal of Management, 29(6), 801–830. 10.1016/S0149-2063(03)00080-1 [DOI] [Google Scholar]
- Katkin J. P., Kressly S. J., Edwards A. R., Perrin J. M., Kraft C. A., Richerson J. E., Tieder J. S., Wall L., & Task Force of Pediatric Practice Change (2017). Guiding principles for team-based pediatric care. Pediatrics, 140(2), e20171489. 10.1542/peds.2017-1489 [DOI] [PubMed] [Google Scholar]
- Kerrissey M. J., Novikov Z., Tietschert M., Phillips R., Singer S. J. (2023). The ambiguity of “we”: Perceptions of teaming in dynamic environments and their implications. Social Science & Medicine, 320, 115678. 10.1016/j.socscimed.2023.115678 [DOI] [PubMed] [Google Scholar]
- Kerrissey M. J., Satterstrom P., Edmondson A. C. (2020). Into the fray: Adaptive approaches to studying novel teamwork forms. Organizational Psychology Review, 10(2), 62–86. 10.1177/2041386620912833 [DOI] [Google Scholar]
- Klein C., DiazGranados D., Salas E., Le H., Burke C. S., Lyons R., Goodwin G. F. (2009). Does team building work? Small Group Research, 40(2), 181–222. 10.1177/1046496408328821 [DOI] [Google Scholar]
- Kolko D. J., McGuier E. A., Turchi R., Thompson E., Iyengar S., Smith S. N., Hoagwood K., Liebrecht C., Bennett I. M., Powell B. J., Kelleher K., Silva M., Kilbourne A. M. (2022). Care team and practice-level implementation strategies to optimize pediatric collaborative care: Study protocol for a cluster-randomized hybrid type III trial. Implementation Science, 17(1), 20. 10.1186/s13012-022-01195-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlowski S. W. J., Bell B. S. (2003). Work groups and teams in organization. In Borman W. C., Ilgen D. R., Klimoski R. J. (Eds.), Handbook of psychology (Vol. 12): Industrial and organizational psychology (pp. 333–375). Wiley-Blackwell. [Google Scholar]
- Kozlowski S. W. J., Ilgen D. R. (2006). Enhancing the effectiveness of work groups and teams. Psychological Science in the Public Interest, 7(3), 77–124. 10.1111/j.1529-1006.2006.00030.x [DOI] [PubMed] [Google Scholar]
- Lacerenza C. N., Marlow S. L., Tannenbaum S. I., Salas E. (2018). Team development interventions: Evidence-based approaches for improving teamwork. American Psychologist, 73(4), 517–531. 10.1037/amp0000295 [DOI] [PubMed] [Google Scholar]
- Lengnick-Hall R., Stadnick N. A., Dickson K. S., Moullin J. C., Aarons G. A. (2021). Forms and functions of bridging factors: Specifying the dynamic links between outer and inner contexts during implementation and sustainment. Implementation Science, 16(1), 34. 10.1186/s13012-021-01099-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- LePine J. A., Piccolo R. F., Jackson C. L., Mathieu J. E., Saul J. R. (2008). A meta-analysis of teamwork processes: Tests of a multidimensional model and relationships with team effectiveness criteria. Personnel Psychology, 61(2), 273–307. 10.1111/j.1744-6570.2008.00114.x [DOI] [Google Scholar]
- Liu Y., Wu Y., Rousseau S., Rousseau R. (2020). Reflections on and a short review of the science of team science. Scientometrics, 125(2), 937–950. 10.1007/s11192-020-03513-6 [DOI] [Google Scholar]
- Luciano M. M., DeChurch L. A., Mathieu J. E. (2018). Multiteam systems: A structural framework and meso-theory of system functioning. Journal of Management, 44(3), 1065–1096. 10.1177/0149206315601184 [DOI] [Google Scholar]
- Markon M.-P., Chiocchio F., Fleury M.-J. (2017). Modelling the effect of perceived interdependence among mental healthcare professionals on their work role performance. Journal of Interprofessional Care, 31(4), 520–528. 10.1080/13561820.2017.1305951 [DOI] [PubMed] [Google Scholar]
- Marks M. A., Burke C. S., Sabella M. J., Pharmaceuticals B., Zaccaro S. J. (2002). The impact of cross-training on team effectiveness. Journal of Applied Psychology, 87(1), 3–13. 10.1037/0021-9010.87.1.3 [DOI] [PubMed] [Google Scholar]
- Marks M. A., DeChurch L. A., Mathieu J. E., Panzer F. J., Alonso A. (2005). Teamwork in multiteam systems. Journal of Applied Psychology, 90(5), 964–971. 10.1037/0021-9010.90.5.964 [DOI] [PubMed] [Google Scholar]
- Marks M. A., Mathieu J. E., Zaccaro S. J. (2001). A temporally based framework and taxonomy of team processes. Academy of Management Review, 26(3), 356–376. 10.5465/amr.2001.4845785 [DOI] [Google Scholar]
- Marlow S. L., Bisbey T., Lacerenza C., Salas E. (2018). Performance measures for health care teams: A review. Small Group Research, 49(3), 306–356. 10.1177/1046496417748196 [DOI] [Google Scholar]
- Marlow S. L., Lacerenza C. N., Paoletti J., Burke C. S., Salas E. (2018). Does team communication represent a one-size-fits-all approach?: A meta-analysis of team communication and performance. Organizational Behavior and Human Decision Processes, 144, 145–170. 10.1016/j.obhdp.2017.08.001 [DOI] [Google Scholar]
- Mathieu J. E., Gallagher P. T., Domingo M. A., Klock E. A. (2019). Embracing complexity: Reviewing the past decade of team effectiveness research. Annual Review of Organizational Psychology and Organizational Behavior, 6(1), 17–46. 10.1146/annurev-orgpsych-012218-015106 [DOI] [Google Scholar]
- Mathieu J. E., Hollenbeck J. R., van Knippenberg D., Ilgen D. R. (2017). A century of work teams in the Journal of Applied Psychology. Journal of Applied Psychology, 102(3), 452–467. 10.1037/apl0000128 [DOI] [PubMed] [Google Scholar]
- Mathieu J. E., Luciano M. M., D’Innocenzo L., Klock E. A., LePine J. A. (2020). The development and construct validity of a team processes survey measure. Organizational Research Methods, 23(3), 399–431. 10.1177/1094428119840801 [DOI] [Google Scholar]
- Mathieu J. E., Marks M. A., Zaccaro S. J. (2001). Multiteam systems. In Anderson N., Ones D. S., Sinangil H. K., Viswesvaran C. (Eds.), Handbook of Industrial, Work & Organizational Psychology: Volume 2: Organizational psychology (pp. 289–313). Sage Publications. [Google Scholar]
- Mathieu J. E., Maynard M. T., Rapp T., Gilson L. (2008). Team effectiveness 1997-2007: A review of recent advancements and a glimpse into the future. Journal of Management, 34(3), 410–476. 10.1177/0149206308316061 [DOI] [Google Scholar]
- Mathieu J. E., Tannenbaum S. I., Donsbach J. S., Alliger G. M. (2014). A review and integration of team composition models: Moving toward a dynamic and temporal framework. Journal of Management, 40(1), 130–160. 10.1177/0149206313503014 [DOI] [Google Scholar]
- McCulloch P., Rathbone J., Catchpole K. (2011). Interventions to improve teamwork and communications among healthcare staff. British Journal of Surgery, 98(4), 469–479. 10.1002/bjs.7434 [DOI] [PubMed] [Google Scholar]
- McEwan D., Ruissen G. R., Eys M. A., Zumbo B. D., Beauchamp M. R. (2017). The effectiveness of teamwork training on teamwork behaviors and team performance: A systematic review and meta-analysis of controlled interventions. PLOS ONE, 12(1), e0169604. 10.1371/journal.pone.0169604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuier E. A., Aarons G. A., Byrne K. A., Campbell K. A., Keeshin B., Rothenberger S. D., Weingart L. R., Salas E., Kolko D. J. (2023). Associations between teamwork and implementation outcomes in multidisciplinary cross-sector teams implementing a mental health screening and referral protocol. Implementation Science Communications, 4(1), 13. 10.1186/s43058-023-00393-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuier E. A., Aarons G. A., Wright J., Fortney J. C., Powell B. J., Rothenberger S. D., Weingart L. R., Kolko D. J. (2023). Team-focused implementation strategies to improve implementation of mental health screening and referral in rural child advocacy centers: study protocol for a pilot cluster randomized hybrid type 2 trial. Implementation Science Communications, 4, Article 58. 10.1186/s43058-023-00437-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuier E. A., Kolko D. J., Aarons G. A., Schachter A., Klem M. L., Diabes M. A., Weingart L. R., Salas E., Wolk C. B. (2022, December 11). Teamwork and implementation of innovations in healthcare and human service settings: A systematic review [Poster presentation]. 15th Annual Conference on the Science of Dissemination and Implementation in Health, Washington, DC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuier, E. A., Rothenberger, S. D., Campbell, K. A., Keeshin, B., Weingart, L. R., & Kolko, D. J. (2022). Team functioning and performance in Child Advocacy Center multidisciplinary teams. Child Maltreatment, 10775595221118932. 10.1177/10775595221118933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuier E. A., Kolko D. J., Klem M. L., Feldman J., Kinkler G., Diabes M. A., Weingart L. R., Wolk C. B. (2021). Team functioning and implementation of innovations in healthcare and human service settings: A systematic review protocol. Systematic Reviews, 10, Article 189. 10.1186/s13643-021-01747-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metz A., Bartley L. (2020). Implementation teams: A stakeholder view of leading and sustaining change. In Albers B., Shlonsky A., Mildon R. (Eds.), Implementation science 3.0 (pp. 199–225). Springer International Publishing. [Google Scholar]
- Metz A., Bartley L., Ball H., Wilson D., Naoom S., Redmond P. (2014). Active implementation frameworks for successful service delivery: Catawba county child wellbeing project. Research on Social Work Practice, 25(4), 11–18. 10.1177/1049731514543667 [DOI] [Google Scholar]
- Miller C. J., Kim B., Silverman A., Bauer M. S. (2018). A systematic review of team-building interventions in non-acute healthcare settings. BMC Health Services Research, 18(1), 146. 10.1186/s12913-018-2961-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller C. J., Sullivan J. L., Harvey K. L. L., Williamson A. K., Stadnick N. A. (2022). Promoting high-functioning mental health treatment teams in the context of low staffing ratios. Health Care Management Review, 47(1), 12–20. 10.1097/HMR.0000000000000312 [DOI] [PubMed] [Google Scholar]
- Mitchell P., Wynia M., Golden R., McNellis B., Okun S., Webb C. E., Rohrbach V., Kohorn I. V. (2012). Core principles and values of effective team-based health care. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine. 10.31478/201210c [DOI] [Google Scholar]
- Mitropoulos P., Memarian B. (2012). Team processes and safety of workers: Cognitive, affective, and behavioral processes of construction crews. Journal of Construction Engineering and Management, 138(10), 1181–1191. 10.1061/(ASCE)CO.1943-7862.0000527 [DOI] [Google Scholar]
- Mohammed S., Ferzandi L., Hamilton K. (2010). Metaphor no more: A 15-year review of the team mental model construct. Journal of Management, 36(4), 876–910. 10.1177/0149206309356804 [DOI] [Google Scholar]
- Mohammed S., Hamilton K., Sánchez-Manzanares M., Rico R. (2017). Team cognition. In E. Salas, R. Rico, & J. Passmore (Eds.), The Wiley Blackwell handbook of the psychology of team working and collaborative processes (pp. 369–392). John Wiley & Sons, Ltd. 10.1002/9781118909997.ch16 [DOI] [Google Scholar]
- Mohr D. C., Rosen C. S., Schnurr P. P., Orazem R. J., Noorbaloochi S., Clothier B. A., Eftekhari A., Bernardy N. C., Chard K. M., Crowley J. J., Cook J. M., Kehle-Forbes S. M., Ruzek J. I., Sayer N. A. (2018). The influence of team functioning and workload on sustainability of trauma-focused evidence-based psychotherapies. Psychiatric Services, 69(8), 879–886. 10.1176/appi.ps.201700432 [DOI] [PubMed] [Google Scholar]
- Mosel D., Shamp M. J. (1993). Enhancing quality improvement team effectiveness. Quality Management in Healthcare, 1(2), 47–58. 10.1097/00019514-199301020-00006 [DOI] [PubMed] [Google Scholar]
- Moullin J. C., Dickson K. S., Stadnick N. A., Rabin B., Aarons G. A. (2019). Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework. Implementation Science, 14(1), Article 1. 10.1186/s13012-018-0842-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nevedal A. L., Reardon C. M., Jackson G. L., Cutrona S. L., White B., Gifford A. L., Orvek E., DeLaughter K., White L., King H. A., Henderson B., Vega R., Damschroder L. (2020). Implementation and sustainment of diverse practices in a large integrated health system: A mixed methods study. Implementation Science Communications, 1(1), 61. 10.1186/s43058-020-00053-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins D. F., Feinberg M. E., Greenberg M. T., Johnson L. E., Chilenski S. M., Mincemoyer C. C., Spoth R. L. (2011). Team factors that predict to sustainability indicators for community-based prevention teams. Evaluation and Program Planning, 34(3), 283–291. 10.1016/j.evalprogplan.2010.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips S. D., Burns B. J., Edgar E. R., Mueser K. T., Linkins K. W., Rosenheck R. A., Drake R. E., McDonel Herr E. C. (2001). Moving assertive community treatment into standard practice. Psychiatric Services, 52(6), 771–779. 10.1176/appi.ps.52.6.771 [DOI] [PubMed] [Google Scholar]
- Powell B. J., Waltz T. J., Chinman M. J., Damschroder L. J., Smith J. L., Matthieu M. M., Proctor E. K., Kirchner J. E. (2015). A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing change (ERIC) project. Implementation Science, 10(1), 21. 10.1186/s13012-015-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor E., Silmere H., Raghavan R., Hovmand P., Aarons G., Bunger A., Griffey R., Hensley M. (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research, 38(2), 65–76. 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Y., Argote L. (2011). Transactive memory systems 1985–2010: An integrative framework of key dimensions, antecedents, and consequences. Academy of Management Annals, 5(1), 189–229. 10.5465/19416520.2011.590300 [DOI] [Google Scholar]
- Rosen M. A., DiazGranados D., Dietz A. S., Benishek L. E., Thompson D., Pronovost P. J., Weaver S. J. (2018). Teamwork in healthcare: Key discoveries enabling safer, high-quality care. The American Psychologist, 73(4), 433–450. 10.1037/amp0000298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen M. A., Dietz A. S. (2017). Team performance measurement. In E. Salas, R. Rico, & J. Passmore (Eds.), The Wiley Blackwell handbook of the psychology of team working and collaborative processes (pp. 479–502). John Wiley & Sons, Ltd. [Google Scholar]
- Rosland A.-M., Nelson K., Sun H., Dolan E. D., Maynard P., Bryson C., Stark R., Shear J. M., Kerr E. (2013). The patient-centered medical home in the Veterans Health Administration. The American Journal of Managed Care, 19(7), 263–272. PMID: 23919446. [PubMed] [Google Scholar]
- Rousseau V., Aubé C., Savoie A. (2006). Teamwork behaviors: A review and an integration of frameworks. Small Group Research, 37(5), 540–570. 10.1177/1046496406293125 [DOI] [Google Scholar]
- Salas E., DiazGranados D., Klein C., Burke C. S., Stagl K. C., Goodwin G. F., Halpin S. M. (2008). Does team training improve team performance? A meta-analysis. Human Factors, 50(6), 903–933. 10.1518/001872008X375009 [DOI] [PubMed] [Google Scholar]
- Salas E., Dickinson T. L., Converse S. A., Tannenbaum S. I. (1992). Toward an understanding of team performance and training. In Swezey R. W., Salas E. (Eds.), Teams: Their training and performance (pp. 3–29). Ablex. [Google Scholar]
- Salas E., Goodwin G. F., Burke C. S. (2008). Team effectiveness in complex organizations: Cross-disciplinary perspectives and approaches. Routledge. [Google Scholar]
- Salas E., Rico R., Passmore J. (2017). The Wiley Blackwell handbook of the psychology of team working and collaborative processes. John Wiley & Sons, Ltd. [Google Scholar]
- Salas E., Stagl K. C., Burke C. S. (2003). 25 Years of team effectiveness in organizations: Research themes and emerging needs. In C. Cooper & I. T. Robertson (Eds.), International review of industrial and organizational psychology 2004 (pp. 47–91). John Wiley & Sons, Ltd. 10.1002/0470013311.ch2 [DOI] [Google Scholar]
- Salas E., Tannenbaum S., Cohen D., Latham G. (2013). Developing and enhancing teamwork in organizations: Evidence-based best practices and guidelines. John Wiley & Sons. [Google Scholar]
- Sandoval B. E., Bell J., Khatri P., Robinson P. J. (2018). Toward a unified integration approach: Uniting diverse primary care strategies under the primary care behavioral health (PCBH) model. Journal of Clinical Psychology in Medical Settings, 25(2), 187–196. 10.1007/s10880-017-9516-9 [DOI] [PubMed] [Google Scholar]
- Sheppard F., Williams M., Klein V. R. (2013). TeamSTEPPS and patient safety in healthcare. Journal of Healthcare Risk Management, 32(3), 5–10. 10.1002/jhrm.21099 [DOI] [PubMed] [Google Scholar]
- Shortell S. M., Marsteller J. A., Lin M., Pearson M. L., Wu S.-Y., Mendel P., Cretin S., Rosen M. (2004). The role of perceived team effectiveness in improving chronic illness care. Medical Care, 42(11), 1040–1048. 10.1097/00005650-200411000-00002 [DOI] [PubMed] [Google Scholar]
- Shuffler M. L., Diazgranados D., Maynard M. T., Salas E. (2018). Developing, sustaining, and maximizing team effectiveness: An integrative, dynamic perspective of team development interventions. Academy of Management Annals, 12(2), 688–724. 10.5465/annals.2016.0045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuffler M. L., DiazGranados D., Salas E. (2011). There’s a science for that: Team development interventions in organizations. Current Directions in Psychological Science, 20(6), 365–372. 10.1177/0963721411422054 [DOI] [Google Scholar]
- Shuffler M. L., Jiménez-Rodríguez M., Kramer W. S. (2015). The science of multiteam systems: A review and future research agenda. Small Group Research, 46(6), 659–699. 10.1177/1046496415603455 [DOI] [Google Scholar]
- Slyngstad D. J., DeMichele G., Salazar M. R. (2017). Team performance in knowledge work. In E. Salas, R. Rico, & J. Passmore (Eds.), The Wiley Blackwell handbook of the psychology of team working and collaborative processes (pp. 43–71). John Wiley & Sons, Ltd. 10.1002/9781118909997.ch3 [DOI] [Google Scholar]
- Smith J. D., Li D. H., Rafferty M. R. (2020). The implementation research logic model: A method for planning, executing, reporting, and synthesizing implementation projects. Implementation Science, 15(1), Article 1. 10.1186/s13012-020-01041-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R., Guyll M., Lillehoj C. J., Redmond C., Greenberg M. (2007). Prosper study of evidence-based intervention implementation quality by community–university partnerships. Journal of Community Psychology, 35(8), 981–999. 10.1002/jcop.20207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R., Guyll M., Redmond C., Greenberg M., Feinberg M. (2011). Six-year sustainability of evidence-based intervention implementation quality by community-university partnerships: The PROSPER study. American Journal of Community Psychology, 48(3–4), 412–425. 10.1007/s10464-011-9430-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sverdrup T. E., Schei V. (2015). Cut me some slack”: The psychological contracts as a foundation for understanding team charters. The Journal of Applied Behavioral Science, 51(4), 451–478. 10.1177/0021886314566075 [DOI] [Google Scholar]
- Tannenbaum S. I., Cerasoli C. P. (2013). Do team and individual debriefs enhance performance? A meta-analysis. Human Factors, 55(1), 231–245. 10.1177/0018720812448394 [DOI] [PubMed] [Google Scholar]
- Tannenbaum S. I., Salas E. (2020). Teams that work: The seven drivers of team effectiveness (Illustrated ed.). Oxford University Press. [Google Scholar]
- Tuckman B. W. (1965). Developmental sequence in small groups. Psychological Bulletin, 63(6), 384–399. 10.1037/h0022100 [DOI] [PubMed] [Google Scholar]
- Tyler A., Glasgow R. E. (2021). Implementing improvements: Opportunities to integrate quality improvement and implementation science. Hospital Pediatrics, 11(5), 536–545. 10.1542/hpeds.2020-002246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine M. A., Nembhard I. M., Edmondson A. C. (2014). Measuring teamwork in health care settings: A review of survey instruments. Medical Care, 53(4), e16–e30. 10.1097/MLR.0b013e31827feef6 [DOI] [PubMed] [Google Scholar]
- Weaver S. J., Dy S. M., Rosen M. A. (2014). Team-training in healthcare: A narrative synthesis of the literature. BMJ Quality & Safety, 23(5), 359–372. 10.1136/bmjqs-2013-001848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiese C. W., Burke C. S., Tang Y., Hernandez C., Howell R. (2022). Team learning behaviors and performance: A meta-analysis of direct effects and moderators. Group & Organization Management, 47(3), 571–611. 10.1177/10596011211016928 [DOI] [Google Scholar]
- Yakovchenko V., Morgan T. R., Chinman M. J., Powell B. J., Gonzalez R., Park A., Malone P. S., Chartier M., Ross D., Rogal S. S. (2021). Mapping the road to elimination: A 5-year evaluation of implementation strategies associated with hepatitis C treatment in the Veterans Health Administration. BMC Health Services Research, 21(1), 1348. 10.1186/s12913-021-07312-4 [DOI] [PMC free article] [PubMed] [Google Scholar]