Abstract
Medication therapy management (MTM) services include comprehensive medication reviews (CMRs), which have been completed with millions of patients since their inception in the United States. The current MTM quality measure focuses on whether CMRs were completed (ie, the CMR completion rate). However, this process measure does not assess quality of care, or patient-reported or other outcomes of CMRs, and, therefore, does not reward MTM providers for improving health outcomes. In this viewpoint article, we present 3 reasons that shape our argument for new MTM quality measures and offer recommendations on next steps to achieve this.
Plain language summary
Comprehensive medication reviews (CMRs) are a type of medication therapy management (MTM) service to find and solve patients’ medication-related problems. However, the current MTM quality measure assesses only whether a CMR was completed and not the quality of care or outcomes of CMRs. In this viewpoint article, we explain why new quality measures are needed to ensure patients are getting the most out of CMRs.
Implications for managed care pharmacy
This viewpoint presents 3 reasons that shape our argument for advancing MTM quality measurement and offers recommendations on the next steps to achieve this objective. Focusing on outcome and patient-reported measures provides opportunities for MTM measures to support reimbursement based on quality of care rather than CMR completion rate. This viewpoint may inform the development of new measures to evaluate the quality of CMRs and other MTM services.
The Centers for Medicare & Medicaid Services (CMS) require Medicare Part D plan sponsors to implement a medication therapy management (MTM) program in their benefits plan.1 Among its several requirements, an MTM program must ensure optimal therapeutic outcomes for targeted beneficiaries through improved medication use and reduce the likelihood of adverse drug events.1 One of the required services MTM programs offer to beneficiaries is an annual comprehensive medication review (CMR).2
A CMR has been defined as “a systematic process of collecting patient-specific information, assessing medication therapies to identify medication-related problems, developing a prioritized list of medication-related problems, and creating a plan to resolve them with the patient, caregiver, and/or prescriber.”2 CMRs can be conducted via telehealth or in-person.2 They involve the patient (or an authorized representative) and a qualified provider (eg, pharmacist) with the goal of improving patients’ medication knowledge and allowing providers the opportunity to resolve any questions or issues.2,3 Given the importance of an annual CMR for MTM program beneficiaries, the Pharmacy Quality Alliance has developed and stewards a quality measure that has been used in the Medicare Part D Star Ratings program since 2016.4 The MTM Program Completion Rate for CMR measure is calculated as the percentage of MTM program beneficiaries who have received a CMR within a specified reporting time frame.5 However, the CMR completion rate measure, as its name suggests, assesses only whether a CMR was completed, not the quality of the CMR or the impact that it had on the patient. Thus, it is time to push the needle to encourage quality of services rather than receipt of services by including more robust MTM measures in the Medicare Part D Star Ratings program.
In our following arguments, we describe why new measure concepts are important and are supported by evidence. Figure 1 describes the logic model to facilitate discussion of potential concepts for future measure development. Table 1 includes the current CMR measure but also provides examples of measure concepts that go beyond the documentation of CMR completion. It should be noted that other than the current CMR measure, these concepts are for illustrative purposes only; prioritization and thorough vetting and testing are needed to determine the appropriateness of these example measure concepts.
FIGURE 1.
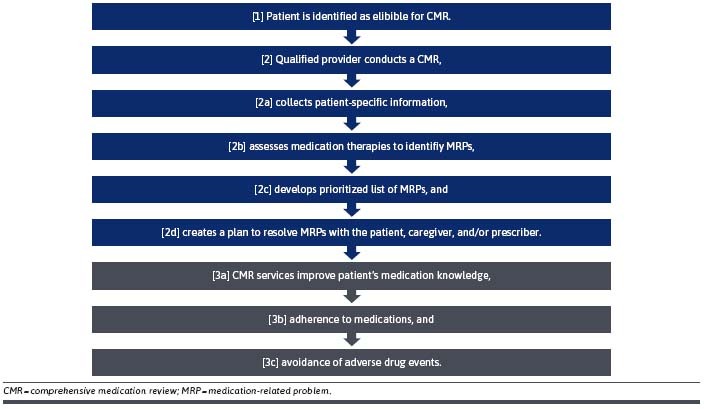
Logic Model Associated With CMR Measure Concepts
TABLE 1.
Measure Concepts Related to CMR by Measure Type and the Associated Measurement Point in the Logic Model
| Measure type | Measure concept | Description | Logic model measured |
|---|---|---|---|
| Process measure (current measure) | CMR completion rate | The percentage of beneficiaries who have received a CMR. | [2] |
| Process measure | CMR quality | The completion rate of multiple components of CMR quality (ie, 4 clinical activities: [1] collecting patient-specific information, [2] assessing medication therapies to identify medication-related problems, [3] developing a prioritized list of medication-related problems, and [4] creating a plan to resolve them with the patient, caregiver, and/or prescriber.) | [2a-d] |
| Intermediate outcome | CMR adherence rate | The rate of adherence to medications among beneficiaries who have received a CMR. | [3b] |
| Outcome | CMR adverse event rate | The rate of adverse drug events among beneficiaries who have received a CMR. | [3c] |
| PROM | Patient medication knowledge | The level of medication knowledge assessed by a validated tool among MTM program beneficiaries who have received a CMR. | [3a] |
| PRO-PM | Patient medication knowledge | The use of the patient medication knowledge PROM to assess the quality of CMR services between providers. | [3a] |
CMR could be replaced with another MTM service as an example of another measure concept.
CMR = comprehensive medication review; MTM = medication therapy management; PROM = patient-reported outcome measure; PRO-PM = patient-reported outcome performance measure.
Argument
REASON 1
Given the expansion of Medicare Part D MTM program requirements over time and the investment required by Part D plan sponsors to meet such requirements,6 assessing the quality of CMRs and other MTM services is warranted. Our research suggests that variation in the execution of CMRs exists in both the consistency and the depth of topics covered and that this variation exists within and among providers.
Through a scoping literature review and key informant interviews we identified 10 components that should be covered in a CMR.7,8 Then, we analyzed real-world CMRs from 3 large provider organizations and identified 21 themes that represented 4 stages of the CMR process.8,9 When applying these themes to explore consistency in CMRs, we found that while many of the key components were covered by all 3 provider organizations, inconsistencies were apparent. This was further amplified by the depth of coverage of topics within the transcripts, wherein one organization might routinely offer greater depth of advice on monitoring blood pressure or insulin levels than the others. Furthermore, variations in CMR execution also existed within the same CMR provider organization. For example, some pharmacists briefly mentioned a medication adherence practice but did not imbue it with the same depth of meaning as their peers.
This observed variation in CMRs may have downstream effects in terms of patient self-efficacy for medication adherence and disease management. Although MTM services are associated with improved outcomes, CMR completion rate has limited and inconsistent association with other measures of medication-use quality,10,11 further suggesting that documentation of CMR completion does not adequately address quality. Consistent application of patient-centered care processes is essential for MTM services to reliably contribute to improved medication-related outcomes.
REASON 2
Aligned with putting patients at the center of their care, there is a strong call for measures that are meaningful to patients.12,13 A taxonomy created to describe what patients value in various health care contexts suggests that patient values and preferences are related to the individual patient, the expected behavior of professionals, and the interaction between patients and professionals.14 One might wonder if existing satisfaction or patient experience measures could be used to assess quality of CMRs or other MTM services. However, research suggests that while existing instruments to assess patient experience have been fit-for-purpose in intraorganizational quality improvement, they are not appropriate as performance measures in accountability programs based on the results of psychometric analyses.15,16
Patients want to influence their care by providing clinicians with actionable information from their own perspectives. Patient-reported outcomes (PROs) are directly reported by patients without interpretation of the patient’s response by clinicians and are inclusive of the following 5 categories: health-related quality of life, functional status, symptom and symptom burden, health behaviors, and experience with care.12,17 The latter 2 categories may be most applicable to MTM services. The measurement of PROs are PRO measures (PROMs). PROMs can be 1-dimensional instruments like the Medicare Part C quality measure, Improving or Maintaining Physical Health, which asks patients through surveys if their physical health was the same or better than expected after 2 years,5 or PROs can be multidimensional focusing on multiple domains of interest, such as the various components of CMRs. Understanding what patients’ value from the CMR experience should be incorporated into the development of a PROM focused on CMRs in conjunction with clinical expertise. A valid and reliable PROM that can be interpreted by both clinicians and patients is needed before a quality measure5 to compare provider performance, or a PRO performance measure (PRO-PM), can be developed.12
The types of measure concepts described here extend beyond the current CMR completion rate measure, which is assessed in a binary fashion (ie, did it happen or not) and focuses on a process of care defined as the delivery of a service from a provider to a patient.11 For example, a new MTM quality measure focused on CMRs could assess patient-reported improvement in medication knowledge and patient empowerment for disease self-management, and/or identify and address patients’ medication- and health-related concerns. Using a multidimensional PROM could move us closer to an outcome measure that assesses multiple components of the CMR goals put forward by CMS, which include improving patient medication knowledge, identifying and addressing patients’ medication- and health-related concerns, and empowering patient self-management.2
REASON 3
At the present time, there is a lack of financial incentive to spend time focusing on the quality of a CMR, as performance measurement is based simply on whether the CMR was completed or not. In fact, many of the key informants in our research indicated that they would prefer to have their CMRs evaluated using a comprehensive PROM. This would allow pharmacists to better use their clinical knowledge and have a more meaningful impact on patient health. It is important to align value-based care with patient-centered care explicitly to ensure alignment of incentives with patients and their caregivers at the core of care delivery.18 A PRO-PM for CMRs or other MTM services therefore offers the opportunity to advance toward a more robust measurement of quality while also helping to improve the value for money spent on these services given ever-increasing demand for health care services.
Recommendations
The variability of the CMR process and lack of consistent correlation between CMR completion and improved quality of care support the need for new MTM quality measures. More meaningful, patient-centered MTM measures in the Part D Star Ratings would incentivize higher quality of these valuable services.
There have been some initiatives to advance MTM quality measurement that can be leveraged. For example, industry stakeholders have created frameworks for standardized documentation of MTM services, which is critical for more outcome-focused measures.19,20 For example, the Pharmacy Quality Alliance Medication Therapy Problem Resolution monitoring measure assesses the percentage of interventions that resolve medication therapy problems among individuals participating in an MTM program, though the measure is not currently used by CMS in Medicare Part D Star Ratings.3 The Part D Enhanced MTM Model can likely provide insights for advancing quality measurement of MTM services.21 We, therefore, recommend prioritizing research efforts that will support new MTM measure concepts, such as the development and validation of a PROM for ultimate use in a PRO-PM.
Conclusions
The CMR completion rate process measure currently used by CMS is a useful measure that has brought attention to the importance of CMR as a core MTM service. CMS’ emphasis on outcome and patient-reported measures13 provides opportunity for new MTM measures to support reimbursement based on quality rather than completion rate of CMRs. Given the current evidence base, measure development, and policy implementation efforts required to support this recommendation, the current CMR measure should be retained at least until new MTM quality measures are developed to continue the focus on this critical service.
REFERENCES
- 1.Centers for Medicare & Medicaid Services. Medication therapy management. US Department of Health and Human Services. 2021. Accessed August 4, 2021. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/MTM [Google Scholar]
- 2.Centers for Medicare & Medicaid Services. CY 2022 MTM Program Guidance and Submission Instructions. US Department of Health and Human Services. 2021. Accessed August 4, 2021. https://www.cms.gov/files/document/memo-contract-year-2022-medication-therapy-management-mtm-program-submission-v-043021.pdf [Google Scholar]
- 3.Medication management services. Pharmacy Quality Alliance. 2022. Accessed February 16, 2022. https://www.pqaalliance.org/medication-management-services
- 4.Centers for Medicare & Medicaid Services. Part C and D performance data. Centers for Medicare & Medicaid Services. Accessed April 1, 2022. https://www.cms.gov/medicare/prescription-drug-coverage/prescriptiondrugcovgenin/performancedata
- 5.Centers for Medicare & Medicaid Services. Medicare 2021 Part C & D star rating technical notes. US Department of Health and Human Services. 2020. Accessed August 4, 2021. https://www.cms.gov/files/document/2021technotes20201001.pdf-0 [Google Scholar]
- 6.Gray C, Cooke CE, Brandt N. Evolution of the Medicare Part D medication therapy management program from inception in 2006 to the present. Am Health Drug Benefits. 2019;12(5) 243-51. [PMC free article] [PubMed] [Google Scholar]
- 7.Vaffis S, Dhatt H, Anderson EJ, et al. Trends in telephonic comprehensive medication review in the United States from 2000 to present: A scoping literature review. J Am Pharm Assoc (2003). 2022; 62(2):406-12.e1. doi:10.1016/j.japh.2021.12.010 [DOI] [PubMed] [Google Scholar]
- 8.Anderson EJ, Dhatt H, Vaffis S, et al. Key informant perspectives about telephonic comprehensive medication review services in the United States. J Am Pharm Assoc (2003). 2022; 62(3);817-25.e1. doi:10.1016/j.japh.2022.01.006 [DOI] [PubMed] [Google Scholar]
- 9.Dhatt H, Vaffis S, Le D, et al. Qualitative analysis of telephonic comprehensive medication review content and delivery. J Am Pharm Assoc (2003). 2023;63(2):555-65. doi:10.1016/j.japh.2022.11.006 [DOI] [PubMed] [Google Scholar]
- 10.Wang Y, Farley J, Ferreri SP, Chelsea P. Do comprehensive medication review completion rates predict medication use and management quality? Res Social Adm Pharm. 2019;15(4):417-24. doi:10.1016/j.sapharm.2018.06.010 [DOI] [PubMed] [Google Scholar]
- 11.Harris IM, Phillips B, Boyce E, et al. Clinical pharmacy should adopt a consistent process of direct patient care. Pharmacotherapy. 2014; 34(8):e133-48. doi:10.1002/phar.1459 [DOI] [PubMed] [Google Scholar]
- 12.Patient-reported outcomes: Best practices on selection and data collection - Final technical report. National Quality Forum. September 2020. Accessed December 20, 2021. https://www.qualityforum.org/Publications/2020/09/Patient-Reported_Outcomes__Best_Practices_on_Selection_and_Data_Collection_-_Final_Technical_Report.aspx
- 13.Centers for Medicare & Medicaid Services. Meaningful Measures 2.0: Moving from measure reduction to modernization. US Department of Health and Human Services. 2021. Accessed November 5, 2021, 2021. https://www.cms.gov/meaningful-measures-20-moving-measure-reduction-modernization [Google Scholar]
- 14.Bastemeijer C, Voogt L, van Ewijk J, Hazelzet J. What do patient values and preferences mean? A taxonomy based on a systematic review of qualitative papers. Patient Educ Couns. 2017;100(5):871-881. doi:10.1016/j.pec.2016.12.019 [DOI] [PubMed] [Google Scholar]
- 15.Campbell PJ, Axon DR, Anderson EJ, Ekstrand MJ, Brummel A, Warholak T. Psychometric evaluation of a comprehensive medication management service experience instrument. J Am Pharm Assoc (2003). 2022;62(1):218-23. doi:10.1016/j.japh.2021.08.024 [DOI] [PubMed] [Google Scholar]
- 16.Vaffis S, Patel M, Potisarach P, Warholak T, Law A. Comparison of the properties of the English and Spanish versions of the Patient Satisfaction with Pharmacist Services Questionnaire 2.0. J Am Pharm Assoc (2003). 2022;62(6):1799-806. doi:10.1016/j.japh.2022.06.006 [DOI] [PubMed] [Google Scholar]
- 17.Weldring T, Smith SM. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights. 2013; 6:61-8. doi:10.4137/HSI.S11093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tseng E, Hicks L. Value based care and patient-centered care: Divergent or complementary? Curr Hematol Malig Rep. 2016; 11(4):303-10. doi:10.1007/s11899-016-0333-2 [DOI] [PubMed] [Google Scholar]
- 19.AMCP. Standardized framework for cross-walking medication therapy management (MTM) services to SNOMED CT codes. 2016. Accessed February 16, 2022. https://www.amcp.org/sites/default/files/2019-03/SNOMED%20Framework%20FINAL%20Oct%202016.pdf
- 20.PQA Medication Therapy Problem Categories Framework. Pharmacy Quality Alliance. 2017. Accessed February 16, 2022. https://www.pqaalliance.org/pqa-measures
- 21.Centers for Medicare & Medicaid Services. Part D Enhanced Medication Therapy Management Model. US Department of Health and Human Services. 2022. Accessed February 16, 2023. https://innovation.cms.gov/innovation-models/enhancedmtm [Google Scholar]


