Abstract
Background
Hypertension (HTN) is a chronic elevation of arterial blood pressure (BP) due to environmental and lifestyle factors. The lifelong treatment protocol causes poor adherence to anti-hypertensive drugs. Nadi Shodhana and Bhramari pranayama are the most effective yogic treatment for the management of HTN.
Objectives
This study was done to assess and compare the immediate effect of Nadi Shodhana and Bhramari Pranayama on HRV and ART in hypertensive individuals. Thus, to understand the effectiveness of specific pranayama on hypertension.
Methodology
This study is a randomized, comparative study design. The hundred participants were recruited into two groups 1 (n = 50) and 2 (n = 50). The study was conducted on pre-diagnosed patients with HTN, from the inpatient department of SDM Nature Cure Hospital, Shanthivana. Group 1 was asked to practice Nadi Shodhana Pranayama and Group-2 was asked to practice Bhramari Pranayama for 20 min. The patients were assessed for Heart Rate Variability & Auditory Reaction Time before and immediately after the intervention.
Results
Nadi Shodhana Pranayama showed a significant decrease in ART (p = 0.01) and Bhramari Pranayama showed a highly significant decrease in ART (p < 0.00001). Whereas there was no statistically significant difference in both the groups in HRV parameters.
Conclusion
The study showed that both Nadi Shodhana and Bhramari Pranayama can be effective in balancing the sympathovagal tone. Thus, Nadi Shodhana and Bhramari Pranayama can be practised for the management of essential hypertension.
Keywords: Essential hypertension, Nadi shodhana pranayama, Bhramari pranayama, HRV, Auditory reaction time, Blood pressure
1. Introduction
Hypertension is the most prevalent non-communicable disorder affecting the major population of India and it is a huge health challenge in the 21st century [1,2]. HTN is linked with structural changes in the cardiovascular system which may lead to cardiovascular mortality and morbidity [3]. The global load of hypertension prevalence is due to the aging population, exposure to lifestyle risk factors and, sedentary life. In 2015 approximate number of deaths that were correlated with SBP ≥110-115 mmHg was 10.7 million (19.2% of all deaths) and with SBP ≥140 mm Hg was 7.8 million (14% of all deaths). The substantial number of deaths that were linked to SBP ≥110-115 mmHg were attributed to ischemic heart disease (IHD), ischaemic stroke, and haemorrhagic stroke [4]. An alarming Indian study of 2019 revealed that the country-level prevalence of hypertension among the young in India was 13.6% in men, 8.8% in women, and 11.3% overall. Hypertension due to specific causes i.e., secondary hypertension is observed in a small number of cases, but for the majority of individuals (≈90%), its etiology cannot be determined i.e., Primary/Essential hypertension [5]. The exact pathogenesis of essential hypertension is not clear, but the anomaly in the sympathetic nervous system and pressure natriuresis system dysfunction is briefly formulated and the most widely accepted pathophysiology. Genetic (family history), behavioural (such as salty food inclination), psychosocial (mental stress), and lifestyle influences (such as physical inactivity) cause an increased sympathetic activity in the early stage of essential hypertension [6].
Numerous studies have shown that elevated blood pressure (BP) is a major risk factor for cardiovascular morbidity and mortality. There is an increased risk of stroke andIHD on a 20 mmHg difference in usual SBP [7].
In developed countries, despite multiple drug therapy and genetic advancements, the burden of hypertension has not decreased due to nonadherence to the prescribed treatment and strict lifestyle modification. Additionally, poor access to medications, healthcare services, and illiteracy situation is worsening the situation in developing countries [8,9]. The ultimate goal of hypertension management is to reduce the excess of cardiovascular morbidity and mortality due to chronically elevated blood pressure and this can be achieved initially by lifestyle modification like stress management, physical activities, weight reduction, and dietary modification [10].
Yoga is an ancient practice that was first mentioned in Rigveda (yogic meditation), whereas Yajurveda explains yoga practice to boost mental health, physical strength, and prosperity [11]. Yoga is a holistic mind-body intervention aimed at physical, mental, emotional, and spiritual wellbeing. The core components of yoga include stretching exercises, physical postures (Asanas), breath control (Pranayama), and concentration techniques (Meditation) [12].
Pranayamas are gaining significance and becoming more acceptable to the scientific community [13]. Chhandogya Upanishad says that Prana is an internal matrix (subtle energy) and Vayu is an external matrix (gross energy). According to Yoga, the gross body (Annamaya kosha) is nourished by the subtle body (Pranamaya kosha) which consists of Chakras and Nadis. These Nadis carry the prana which stimulates the chakras and thereby nourishes various organs and systems and affects all the physiological activities in the human body [14].
Previous study on pranayama and hypertension showed a reduction in the heart rate, blood pressure, and rate pressure product [15]. Improvement in cardiorespiratory parameters were seen in a recent study on Nadi Shodhana Pranayama, which is suggestive of an increase in cardiorespiratory efficiency [16]. Bhramari Pranayama has been shown in a recent study to boost pulmonary functions, improve autonomic function, sleep quality, and lower infection risk [17]. Bhramari Pranayama practice in home isolated COVID-19 patients showed improvement in the psychological health disorders such as anxiety, depression, and sleep deprivation [18]. The six-month practice of Bhramari Pranayama showed reduction in reaction time in healthy adolescent group which implies improvement in reflexes and information processing [19]. Regular practice of Bhramari Pranayama can be effective in improving stress response [20].
There is a connection between hypertension and HRV, that lies in the autonomic nervous system regulating blood pressure, the sympathetic nervous system, which accelerates the heart rate and constricts blood vessels, and the parasympathetic nervous system, which slows the heart rate and helps in the relaxation. In patients with hypertension, there is often an imbalance of sympathetic activity and parasympathetic activity. This imbalance led to reduced HRV in the time intervals between heartbeats. Low HRV is associated with increased cardiovascular risk [21]. Hypertensive patients are associated with an increased risk of cognitive impairment. By evaluating reaction time, researchers found that yoga and pranayama are more significant in patients with hypertension. Reaction time is index arousal and a reduction in it showed an enhanced sensory-motor performance and improved processing capability of the central nervous system [22]. A study done by McIntyre D et al. found that hypertensives have slower reaction times than normotensives [23].
Although Nadi Shodhana Pranayama and Bhramari Pranayama are used extensively in the management of essential hypertension, there has been no study conducted to compare the immediate effects of Nadi Shodhana and Bhramari Pranayama in hypertensive patients.
The aim of this study is to compare the immediate effects of Nadi Shodhana and Bhramari Pranayama on blood pressure, heart rate variability (HRV), and Auditory reaction time in hypertensive individuals. To demonstrate the scope of efficiency of short-term and specific effect of Pranayama in the management of essential hypertension.
This study hypothesized that there is a different effect following the intervention of Nadi Shodhana and Bhramari Pranayama on hypertensive individuals.
2. Materials and methods
2.1. Trial design
This study is a randomized, comparative study. The patients were randomly divided into group 1 and group 2 with 1:1 allocation ratio.
2.2. Participants
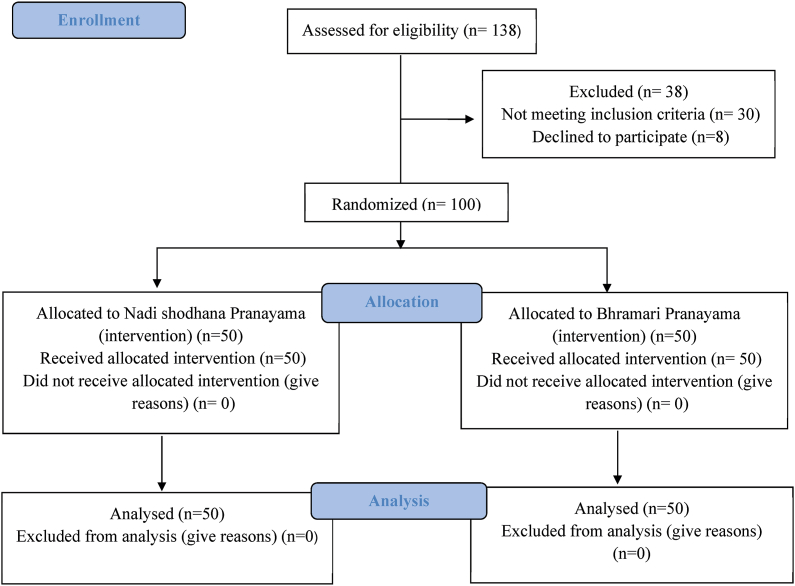
Participants were recruited from the in-patient department of SDM Nature Cure Hospital, Karnataka, India. 138 hypertensive individuals were screened for the study. Out of which 100 participants were able to fulfill the inclusion criteria and were eligible for the study. Recruited patients were randomized in two groups using a simple randomization method (lottery method). The inclusion criteria for the study were male & female within the age group of 30–60 years, pre-diagnosed with essential hypertension , with or without antihypertensive drugs. The participants were excluded from the study if they were diagnosed with secondary hypertension, valvular heart disease, pericarditis/myocarditis, heart failure with EF 35%, CABG, PTCA with or without stenting. Patients who refused to fill the consent form were not included in the study. There were no deviations from the protocol of the study. Any participants who did not fulfill the inclusion criteria and were not willing to participate in the study were excluded in the initial phase of the study. Fig. 1 (trial profile).
Fig. 1.
Participants flow of this study.
2.3. Sample size calculation
The sample size was calculated based on the effect size of systolic blood pressure, post-mean and standard deviation of the study group (113.05 ± 8.01) and control group (119.90 ± 7.05) appropriately. The total sample size of 62 patients were calculated (ɑ = 0.05) and power (1-β = 0.90) by G∗ power software, version 3.1.9.2 based on a previous study [24]. Due to the higher probability of dropout, researchers expected a 25% dropout because of the common trend in Yoga interventions, but after the intervention, there was no dropout. Therefore, analysis was done for 100 participants. For the protocol and basis of analysis, 100 people were recruited. Considering the 25% attrition and dropout rates, all the participants completed the intervention, so the analysis was reported for 100 people.
2.4. Randomization
The randomization of the patients was done using lottery method, where the numbers 1 to 100 were written on the paper and put in the bowl. The patients were asked to pick a chit from the bowl under the supervision of researchers. If patient gets an odd number, he/she was put in group 1 (Nadi Shodhana Pranayama), if patient gets an even number, he/she was put in group 2 (Bhramari Pranayama).
As the patients were taught the pranayama, they were aware of the treatment given to them. Also, the researcher was aware of the practice given to them. The blinding/masking was not done in this study.
2.5. Ethical considerations & trial registration
The study was approved by the institutional ethical committee prior to the study. The study was registered with the clinical trial registry of India (https://ctri.nic.in) under CTRI registration number CTRI/2019/12/022,263. A signed informed consent was obtained from the patients by explaining the study objectives, methods, intervention, and all the rights of the patients pertaining to the study orally in the language best known to them and in writing form in English (Sample of consent form is enclosed).
2.6. Intervention
2.6.1. Group 1
Group 1 performed Nadishodhana Pranayama for 20 min. During the practice participants were asked to sit in “Sukhasana”. The participants were then instructed to perform the following steps: Assume Nasikagra Mudra in the right hand and Chin/Gyan Mudra in left hand. Inhale & exhale slowly & deeply with both nostrils. Inhale slowly and quietly through the left nostril while closing the right. At the end of the inhalation, Keep the left nostril closed and exhale through the right as slowly as possible. After exhaling completely, inhale slowly and quietly through the right nostril. Close the right nostril and then open the left nostril and exhale slowly and silently. Inhale through the same nostril and continue.
2.6.2. Group 2
Group 2 performed Bhramari Pranayama for 20 min. Participants were asked to sit in “Sukhasana”. The eyes must be closed during this process to cut off external inputs of sounds and sight, to internalize the consciousness. Sanmukhi mudra will be adopted so that the sensation of vibration on the facial region is experienced by placing the fingers on the different regions of the face. Inhalation and exhalation should be through nostrils, slowly and deeply. While exhaling, the participants will have to produce sound (humming sound) like a bumble bee strictly through nasal airways, keeping oral cavity closed by the lips, ears closed by fingers. The procedures of both Nadi Shodhana and Bhramari Pranayama were demonstrated by a qualified Yoga expert.
2.7. Assessments
The primary outcome variables were Arterial blood pressure and Heart rate variability. The secondary outcome variable was Auditory reaction time.
2.7.1. Arterial blood pressure (BP)
Blood pressure was recorded before and after the interventions by using a digital sphygmomanometer (OMRON – 7113), auscultating over the right brachial artery, it had a pressure accuracy of ±3 mmHg. The systolic pressure was noted as the first clear tapping sound (Korotkoff sounds) and diastolic pressure was noted as the reading at which the Korotkoff sounds appeared muffled. Blood pressure sample was not continuously monitored.
2.7.2. Heart rate variability (HRV)
The standard electrocardiogram (ECG) was recorded using standard bipolar limb lead II configuration for 5 min as a baseline with patients lying in a supine posture comfortably on a bed. Signals were digitized and recorded with a PowerLab 17T device (ADInstruments Inc., Bella Vista, NSW, Australia). The R waves were detected to obtain a point event series of successive R–R intervals, from which the beat-to-beat heart rate series was computed.
2.7.3. Auditory reaction time (ART)
The reaction time was recorded with patients in sitting posture on bed. The signals were digitized and recorded with a PowerLab 17T device (ADInstruments Inc., Bella Vista, NSW, Australia).
2.8. Data extraction
2.8.1. Heart rate variability
The energy in the HRV series of the following specific bands was studied, viz., the very low- frequency component (0.0–0.05 Hz), low -frequency component (0.05–0.15 Hz), and high -frequency component (0.15–0.50 Hz). The low -frequency and high- frequency values were expressed as normalized units. The low- frequency and high- frequency values are expressed as normalized units. Both time domain and frequency domain values were analyzed. In time domain RMSSD, pRR50 and in frequency domain VLF, LF, HF, LF/HF values were extracted by using the Lab chart software (ADInstruments Inc.) [25]. Limb lead two II is selected for the HRV recording because of the placement of positive electrode in lead II which view the wavefront of the impulse from the inferior aspect of the heart. All the waves are prominent in lead –II, including P wave.
2.8.2. Blood pressure
BP was recorded using the digital sphygmomanometer (OMRON – 7113).
2.8.3. Auditory reaction time
The simple reaction time (ART) waveform is extracted by using the lab chart software (AD Instruments Inc.).
2.8.4. Data analysis
Statistical analysis was done using the SCIKIT-LEARN package in Python. Data was checked for normal distribution using Saphiro Wilk test and analyzed by using Wilcoxon rank sum test and Mann Whitney U test. A P value less than 0.05 was accepted with the confidence interval (CI) 95% as an indicator of significance.
3. Results
The data obtained was analysed for normality by Shapiro Wilk test which shows that the data was skewed distribution. So, the pre-post data of Nadi Shodhana and Bhramari Pranayama groups were analysed separately using Wilcoxon rank sum test and comparative analysis between the Nadi Shodhana and Bhramari Pranayama groups were done by using the Mann Whitney U test. In Group-1 there were 58.6% of males and 41.4% of females with a mean age of 32.38 years and in Group-2 there were 63.4% of males and 36.6% of females with a mean age of 31.5 years.
3.1. Between the group changes
The two groups did not show significant differences in the variables at baseline. The comparison between both groups showed no significant difference in HRV parameters. There was a statistically significant difference in Auditory reaction time in Bhramari group (p < 0.00001). The post scores of the pranayama (Nadi Shodhana and Bhramari) group of the mean SD ± are in Table 1.
Table 1.
Comparison of pre and post- test values Nadi Shodhana and Bhramari Pranayama group.
| Nadi Shodhana Pranayama Group | Bhramari Pranayama Group | |||
|---|---|---|---|---|
| Variables | Mean ± SD Pre | Mean ± SD Post | Mean ± SD Pre | Mean ± SD Post |
| SBP | 124.98 ± 10.58 | 122.18 ± 9.25∗∗ | 126.74 ± 10.66 | 122.56 ± 8.06 ∗∗ |
| DBP | 79.04 ± 8.15 | 76.00 ± 7.24∗ | 81.34 ± 8.68 | 79.08 ± 7.94∗ |
| Median RR | 741.04 ± 115.21 | 755.07 ± 139.63∗ | 764.16 ± 110.11 | 784.90 ± 114.48 ∗∗ |
| Mean HR | 84.93 ± 16.37 | 82.16 ± 18.01∗∗ | 86.50 ± 13.81 | 80.11 ± 12.22 ∗∗ |
| RMSSD | 52.14 ± 45.57 | 59.50 ± 56.36 ∗ | 45.95 ± 31.21 | 57.10 ± 53.59 ∗ |
| pRR50 | 19.66 ± 22.51 | 23.04 ± 23.60 | 19.37 ± 22.89 | 22.27 ± 25.51∗ |
| VLF | 42.00 ± 22.15 | 37.50 ± 20.06 | 44.32 ± 26.54 | 38.86 ± 20.58 |
| LF | 55.08 ± 20.83 | 45.24 ± 19.43 | 54.63 ± 20.91 | 48.61 ± 20.16 |
| HF | 46.07 ± 20.46 | 52.21 ± 20.74 | 45.54 ± 20.73 | 53.52 ± 18.61∗ |
| LF_HF | 1.80 ± 1.70 | 1.21 ± 0.96 ∗ | 1.82 ± 1.78 | 1.17 ± 0.89∗ |
| ART | 0.42 ± 0.22 | 0.38 ± 0.14∗∗ | 1.11 ± 0.76 | 0.45 ± 0.29∗∗ |
There is significant change seen in the pre and post of Nadi Shodhana and Bhramari Pranayama ∗ p < 0.05, ∗∗-p<0.01, ∗∗∗- p < 0.001.
3.2. Within group changes
3.2.1. Nadi Shodhana pranayama
There was a significant decrease in SBP (p = 0.01) and DBP (p = 0.02). In the time domain of heart rate variability, there was a significant increase in RMSSD (p = 0.029), median RR (p = 0.02), and pRR50 (p = 0.031). In the frequency domain of HRV, there was a insignificant increase in HF (p = 0.08857), a decrease in VLF (p = 0.09315), and LF (p = 0.19087). There was a significant decrease in LF/HF ratio (p = 0.02745) and ART (p = 0.011). The Nadi Shodhana group mean ± SD scores are in Table 1.
3.2.2. Bhramari Pranayama
There was a significant decrease in SBP (p = 0.011) and DBP (p = 0.04). In the time domain of HRV, there was a significant increase in RMSSD (p = 0.0295), median RR (0.003), and pRR50 (p = 0.031). In the frequency domain of HRV, there was a significant increase in HF (p = 0.042) and there was a significant decrease in LF/HF ratio (p = 0.023). Whereas there was an insignificant decrease in LF (p = 0.167) and VLF (p = 0.08764). There was a significant decrease in the ART (p < 0.00001). The Bhramari group Mean ± SD scores are in Table 1.
3.3. Repeated measures analysis of variance (RM-ANOVA)
The HRV and ART components show significant change in Table 2.
Table 2.
Repeated Measure Analysis of Variance (RM-ANOA) showing the value of results.
| Variables | Effect | F Value | df | Level of significance/P | pEta2 |
|---|---|---|---|---|---|
| SBP | TIME | 11.32 | 1,98 | 0.001 | 0.10 |
| GROUP | 0.43 | 1,98 | 0.51 | 0.004 | |
| TIME∗ GRUOP | 0.44 | 1,98 | 0.51 | 0.004 | |
| DSP | TIME | 8.31 | 1,98 | 0.005 | 0.078 |
| GROUP | 4.17 | 1,98 | 0.043 | 0.041 | |
| TIME∗ GRUOP | 0.180 | 1,98 | 0.672 | 0.002 | |
| Median R | TIME | 4.02 | 1,98 | 0.047 | 0.040 |
| GROUP | 1.37 | 1,98 | 0.242 | 0.014 | |
| TIME∗ GRUOP | 0.150 | 1,98 | 0.699 | 0.002 | |
| Mean HR | TIME | 16.14 | 1,98 | 0.001 | 0.141 |
| GROUP | 0.007 | 1,98 | 0.933 | 7.322 | |
| TIME∗ GRUOP | 2.50 | 1,98 | 0.116 | 0.025 | |
| RMSSD | TIME | 7.85 | 1,98 | 0.006 | 0.074 |
| GROUP | 0.230 | 1,98 | 0.632 | 0.002 | |
| TIME∗ GRUOP | 0.31 | 1,98 | 0.568 | 0.003 | |
| pRR50 | TIME | 8.80 | 1,98 | 0.004 | 0.083 |
| GROUP | 0.013 | 1,98 | 0.907 | 1.385 | |
| TIME∗ GRUOP | 0.050 | 1,98 | 0.821 | 5.243 | |
| VLF | TIME | 6.76 | 1,98 | 0.011 | 0.065 |
| GROUP | 0.204 | 1,98 | 0.652 | 0.002 | |
| TIME∗ GRUOP | 0.061 | 1,98 | 0.803 | 6.356 | |
| LF | TIME | 11.23 | 1,98 | 0.001 | 0.103 |
| GROUP | 0.18 | 1,98 | 0.660 | 0.002 | |
| TIME∗ GRUOP | 0.64 | 1,98 | 0.421 | 0.007 | |
| HF | TIME | 9.08 | 1,98 | 0.003 | 0.085 |
| GROUP | 0.014 | 1,98 | 0.906 | 1.426 | |
| TIME∗ GRUOP | 0.14 | 1,98 | 0.696 | 0.002 | |
| LF/HR | TIME | 15.17 | 1,98 | 0.001 | 0.134 |
| GROUP | 0.002 | 1,98 | 0.968 | 1.617 | |
| TIME∗ GRUOP | 0.02 | 1,98 | 0.859 | 3.225 | |
| ART | TIME | 59.45 | 1,98 | 0.001 | 0.378 |
| GROUP | 27.83 | 1,98 | 0.001 | 0.221 | |
| TIME∗ GRUOP | 45.39 | 1,98 | 0.001 | 0.317 |
4. Discussion
In the present study, the effect of 20 min practice of Nadi Shodhana and Bhramari Pranayama was found to reduce the heart rate variability along with a significant change in auditory reaction time. This finding indicates that the practice of Nadi Shodhana or Bhramari Pranayama both reduces blood pressure and improves the reaction time in patients with essential hypertension. This is the first study to compare the immediate effect of Nadi Shodhana and Bhramari Pranayama on HRV and ART.
A previous study done on pranayama showed a decrease in the SBP, DBP , and HR due to de-stressing effect of pranayama. This leads to a reduction in sympathetic arousal resulting in decrease in adrenaline secretion, stimulation of stretch receptors in the lungs leading to stimulation of the Hering-Breuer inflation reflex which causes the sympathetic tone withdrawal and vasodilatation and activation of parasympathetic nervous system [26]. In this study, following Nadi Shodhana Pranayama was observed to have a significant reduction in the SBP and DBP. A previous study done by Tripathy et al. on the immediate effect of Nadi Shodhana Pranayama showed a reduction in SBP and DBP which may be due to the activation of parasympathetic dominance [27].
Mechanism behind the effect of Nadi Shodhana Pranayama in reduction of BP may be due to the breathing, that stimulates the olfactory nerves situated in the roof of the nasal cavity. This is transferred to olfactory bulbs which are situated in the region of cribriform plate. This olfactory bundle is connected to the front of the brain, which is in turn connected to the hypothalamus. Hypothalamus is the part of the brain that regulates hormones. In any perceived stress condition, the serotonin receptors in the hypothalamus with the help of splanchnic pathway regulate the stress. When there is a dysregulation of respiration, the face lock of the olfactory signals occurs, and hypothalamus does not receive proper signal. This causes disorganized information to hypothalamus and due to this phenomena hypothalamus pituitary adrenal dysfunction occurs. The regulated breathing pattern in Nadi Shodhana Pranayama causes regulation of the HPA axis. Hence, reduction in BP is observed [28]. In this study, the results showed decrease in LF, VLF, and LF/HF ratio after the intervention. Also, there was an increase in HF after an intervention. Similar changes in HRV can be seen in the study done by Supriya et al. following the Nadi Shodhana Pranayama [29]. A significant decrease in the ART following Nadi Shodhana Pranayama may be due to the voluntary change in the breathing pattern and the state of the parasympathetic dominance followed by the distressing effect and relaxation effect of Nadi Shodhana Pranayama [30].
In the current study following 20 min of Bhramari Pranayama, there was a significant decrease in SBP, DBP and HR. The results of the current study are supported by the study conducted by Vungarala Satyanand et al. which shows a significant reduction in BP and HR following Bhramari Pranayama practice for 10 min due to the humming of the “O–U-Mmmma” sound causes vibration of the nasal/laryngeal mucous membrane during exhalation which causes switching off the inspiratory centres leads to reflex apnoea which causes bradycardia through chemoreceptor sinu-aortic mechanism [31]. The humming helps to boost the production of nitric oxide from sinuses and nasal mucosa which acts as vasodilator, improves blood circulation, and maintain the oxygen supply to heart muscles. Nitric oxide is known to modulate norepinephrine, serotonin, dopamine, glutamate, and the other major neurotransmitters [32,33].
In our study, there was highly significant reduction in ART after the practice of Bhramari Pranayama. Similar observation was done in the study conducted by S. Jore et al. which showed significant reduction in reaction time following pranayama practice in medical students. The stress can cause altered behavioral changes i.e., depression and anxiety, whereas reduction in reaction time could be due to greater cortical arousal & faster rate of information processing, improved concentration power, ability to ignore external stimuli. This act of breathing removes attention from worries & distress and practitioner can better handle day to day emotional, physical & mental stress [34].
In the present study, the effect of 20 min practice of Nadi Shodhana and Bhramari Pranayama was found to reduce the heart rate variability along with the significant change in auditory reaction time.
There no control group in this study and the intervention given to both groups was a different pranayama. Hence, we cannot claim changes in the outcome of this study. Therefore, this limitation has been added to this study.
The strength of this study is that it is the first study done to compare the effect of Nadi Shodhana and Bhramari Pranayama and participated a greater number of hypertensive patients using HRV and ART as assessment criteria. It was a Parallel Randomized controlled trial with clinical application. Standard assessment equipment is used to assess HRV and ART hence precise, reliable data was obtained.
The major limitation of this study was that it was an immediate and comparative study with no control group, and demographical data and Antihypertensive drug levels were not recorded in this study due to a lack of information. For further study, a long-term comparison with the inclusion of educational and occupational background and levels of antihypertensive drugs can be done with various parameters.
5. Conclusions
Our findings suggest that Nadi Shodhana and Bhramari Pranayama are simple, non-invasive, and cost-effective methods that can be helpful in the management of hypertension for immediate blood pressure reduction. As the study was conducted at Nature Cure Hospital, participants were also receiving other yoga and naturopathy interventions during the study period, which can be a confounding factor for the study.
Author contributions
Junu Upadhyay: Conceptualization, Writing Original draft, Writing-review, editing, Funding acquisition, Supervision, Project administration & Resources. Nandish NS: Conceptualization, Writing-Original draft, Writing-review and editing, Formal analysis. Shiva Prasad Shetty: Conceptualization, Investigation. Apar Avinash Saoji: Software, formal analysis, Methodology & Visualization. Sunil Singh Yadav: Editing, Software, Data curation and Validation.
Source of funding
None.
Declaration of interest statement
The authors have no conflicts of declaration. The contents of the manuscript are seen and agreed upon by the authors. There is no financial interest to report. The author certifies that the submission is original work and not under revival at any publication.
Data availability
Data can be obtained from the author on request.
Acknowledgements
We are thankful to Dr. Prashanth Shetty, Principal of SDM College of Naturopathy and Yogic Sciences, Ujire, who gave us the golden opportunity to conduct this research study and for their constant encouragement and support throughout this study.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Murugesan R., Govindarajulu N., Bera T.K. Effect of selected yogic practices on the management of hypertension. Indian J Physiol Pharmacol. 2000;44:207–210. [PubMed] [Google Scholar]
- 2.Rao C.R., Kamath V.G., Shetty A., Kamath A. High blood pressure prevalence and significant correlates: a quantitative analysis from coastal Karnataka, India. ISRN Prev Med. 2013;2013:1–6. doi: 10.5402/2013/574973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kandler M.R., Tejani A.M., Mah G. Hydralazine for essential hypertension. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD004934.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Kearney P.M., Whelton M., Reynolds K., Muntner P., Whelton P.K., He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/s0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 5.Gupta R., Ram C.V.S. Hypertension epidemiology in India: emerging aspects. Curr Opin Cardiol. 2019;34:331–341. doi: 10.1097/HCO.0000000000000632. [DOI] [PubMed] [Google Scholar]
- 6.Bolívar J.J. Essential hypertension: an approach to its etiology and neurogenic pathophysiology. Int J Hypertens. 2013;2013:1–11. doi: 10.1155/2013/547809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anchala R., Kannuri N.K., Pant H., Khan H., Franco O.H., Di Angelantonio E., et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohsen Ibrahim M. Hypertension in developing countries: a major challenge for the future. Curr Hypertens Rep. 2018;20 doi: 10.1007/s11906-018-0839-1. [DOI] [PubMed] [Google Scholar]
- 9.Singh T., Bhatnagar N., Moond G. Lacunae in noncommunicable disease control program: need to focus on adherence issues. J Fam Med Prim Care. 2017;6:610. doi: 10.4103/2249-4863.214434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cuspidi C., Tadic M., Grassi G., Mancia G. Treatment of hypertension: the ESH/ESC guidelines recommendations. Pharmacol Res. 2018;128:315–321. doi: 10.1016/j.phrs.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Sengupta P. Health impacts of yoga and pranayama: a state-of-the-art review. Int J Prev Med. 2012;3:444–458. [PMC free article] [PubMed] [Google Scholar]
- 12.Manchanda S.C., Madan K. Yoga and meditation in cardiovascular disease. Clin Res Cardiol. 2014;103:675–680. doi: 10.1007/s00392-014-0663-9. [DOI] [PubMed] [Google Scholar]
- 13.Gaur G., Sharma V., Madanmohan T., Harichandra Kumar K., Dinesh T., Bhavanani A. Comparative effect of 12 weeks of slow and fast pranayama training on pulmonary function in young, healthy volunteers: a randomized controlled trial. Int J Yoga. 2015;8:22. doi: 10.4103/0973-6131.146051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shyam Karthik P., Chandrasekhar M., Ambareesha K., Nikhil C. Effect of pranayama and suryanamaskar on pulmonary functions in medical students. J Clin Diagn Res. 2014;8 doi: 10.7860/JCDR/2014/10281.5344. BC04–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma V.K., Trakroo M., Subramaniam V., Rajajeyakumar M., Bhavanani A.B., Sahai A. Effect of fast and slow pranayama on perceived stress and cardiovascular parameters in young health-care students. Int J Yoga. 2013;6:104–110. doi: 10.4103/0973-6131.113400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jahan I., Begum M., Akhter S., Islam M.Z., Jahan N., Samad N., et al. Effects of alternate nostril breathing exercise on cardiorespiratory functions in healthy young adults. Ann Afr Med. 2021;20:69–77. doi: 10.4103/aam.aam_114_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trivedi G.Y., Saboo B. Bhramari Pranayama - a simple lifestyle intervention to reduce heart rate, enhance the lung function and immunity. J Ayurveda Integr Med. 2021;12:562–564. doi: 10.1016/j.jaim.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jagadeesan T., Archana R., Kannan R., Jain T., Allu A.R., Maveeran M., et al. Effect of Bhramari Pranayama intervention on stress, anxiety, depression and sleep quality among COVID 19 patients in home isolation. J Ayurveda Integr Med. 2022 Jul-Sep;13(3):100596. doi: 10.1016/j.jaim.2022.100596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuppusamy M., Kamaldeen D., Pitani R., Amaldas J., Ramasamy P., Shanmugam P., et al. Effect of Bhramari pranayama practice on simple reaction time in healthy adolescents - a randomized control trial. Int J Adolesc Med Health. 2020;33:547–550. doi: 10.1515/ijamh-2019-0244. [DOI] [PubMed] [Google Scholar]
- 20.Maheshkumar K., Dilara K., Ravishankar P., Julius A., Padmavathi R., Poonguzhali S., et al. Effect of six months pranayama training on stress-induced salivary cortisol response among adolescents-Randomized controlled study. Explore. 2022;18:463–466. doi: 10.1016/j.explore.2021.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Garafova A., Penesova A., Cizmarova E., Marko A., Vlcek M., Jezova D. Cardiovascular and sympathetic responses to a mental stress task in young patients with hypertension and/or obesity. Physiol Res. 2014;63:S459–S467. doi: 10.33549/physiolres.932931. [DOI] [PubMed] [Google Scholar]
- 22.Sonwane T.D., Mishra N.V. Study of effects of yoga and pranayam on human reaction time and certain physiological parameters in normal and hypertensive subjects. Natl J Physiol Pharm Pharmacol. 2016;6:323–328. doi: 10.5455/njppp.2016.6.04022016136. [DOI] [Google Scholar]
- 23.McIntyre D., Ring C., Edwards L., Carroll D. Simple reaction time as a function of the phase of the cardiac cycle in young adults at risk for hypertension. Psychophysiology. 2008;45:333–336. doi: 10.1111/j.1469-8986.2007.00619.x. [DOI] [PubMed] [Google Scholar]
- 24.Sharma V.K., Elangovan, Subramanian S.K., Rajendran R. Effect of yoga therapy on heart rate variability and blood pressure in sedentary males. Int J Phys. 2018;6:15. doi: 10.5958/2320-608x.2018.00077.x. [DOI] [Google Scholar]
- 25.Mourot L., Bouhaddi M., Gandelin E., Cappelle S., Dumoulin G., Wolf J.P., et al. Cardiovascular autonomic control during short-term thermoneutral and cool head-out immersion. Aviat Space Environ Med. 2008;79:14–20. doi: 10.3357/ASEM.2147.2008. [DOI] [PubMed] [Google Scholar]
- 26.Vasanthan S., Madanmohan T., Bhavanani A.B., Hanifah M., Jaiganesh K. Comparative study on the effect of yogic relaxing asanas and pranayamas on cardiovascular response in healthy young volunteers. Natl J Physiol Pharm Pharmacol. 2017;7:127–130. doi: 10.5455/njppp.2017.7.0824018082016. [DOI] [Google Scholar]
- 27.Tripathy M., Sahu B. Immediate effect of Nadi Shodhana pranayama on blood glucose, heart rate and blood pressure. J Am Sci. 2019;15:65–70. doi: 10.7537/marsjas150519.09. [DOI] [Google Scholar]
- 28.Casikar V. Pranayama a neuro-physiological explanation of the mechanism. J Yoga Physiother. 2017;2:3–4. doi: 10.19080/JYP.2017.02.555577. [DOI] [Google Scholar]
- 29.Saisupriya K., Chandrappa S.H., Shetty S.K., Shetty P., Honnegowda T.M., Hiremath L. Analysis of immediate effect of nadishodhana pranayama in the ratio of 1:3:2 on autonomic and respiratory variables in healthy individuals. Yoga Mimamsa. 2020;52:20. doi: 10.4103/ym.ym. [DOI] [Google Scholar]
- 30.Bhavanani A.B., Ramanathan M., Balaji R., Pushpa D. Differential effects of uninostril and alternate nostril pranayamas on cardiovascular parameters and reaction time. Int J Yoga. 2014;7:60–65. doi: 10.4103/0973-6131.123489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vungarala Satyanan, Bhakthavatsala R., Lilly N., Shaik M., Shaik Basha A., Aditya M. Studying the role of yogic Pranayama in the management of Blood pressure. Int J Biomed Adv Res IJBAR Int J Biomed Adv Res J. 2014;5 doi: 10.7439/ijbar. [DOI] [Google Scholar]
- 32.Upadhye J.A. Health benefits of Bhramari pranayama. ∼ 449. Int J Phys. 2019;4:449–450. [Google Scholar]
- 33.Taneja M.K. Nitric oxide Bhramari pranayam and deafness. Indian J Otol. 2016;22:1–3. doi: 10.4103/0971-7749.176507. [DOI] [Google Scholar]
- 34.Jore S., Kamble P., Bhutada T., Patwardhan M. 2013. Effect of Pranayama training on Audio-Visual Reaction Time. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be obtained from the author on request.