Abstract
Purpose
The aim of this study was to analyze if any difference exists on the type of immobilisation (above elbow vs. below elbow) in the conservative treatment of distal end radius fractures in adults.
Methods
The study was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-analyses. An electronic literature search was performed up to 1st October 2021 in Medline, Embase, Ovid and Cochrane database using the search terms, “distal end radius fractures OR fracture of distal radius”, “conservative treatment OR non-surgical treatment”, “above elbow immobilisation” and “below elbow immobilisation”. Randomized clinical trials written in English, describing outcome of distal end radius fractures in adults by conservative or non-surgical means using above elbow immobilisation or below elbow immobilisation were included and assessed according to the risk of bias assessment (RoB2) tool by Cochrane collaboration. Non-randomized clinical trials, observational studies, retrospective studies, review articles, commentaries, editorials, conference presentations, operative techniques and articles without availability of full text were excluded from this review. The meta-analysis was performed using Review Manager version 5.4.1 (The Cochrane Collaboration, Copenhagen, Denmark).
Results
Six randomized clinical trials were included for quantitative review. High heterogeneity (I2 > 75%) was noted among all the studies. The standard mean difference (MD) between the disability of the arm, shoulder and hand scores in both the groups was 0.52 (95% CI: −0.28 to 1.32) which was statistically non-significant. There was no statistical difference in the radial height (MD = 0.10, 95% CI: −0.91 to 1.12), radial inclination (MD = 0.5, 95% CI: −1.88 to 2.87, palmar tilt (MD =1.06, 95% CI: −0.31 to 2.43) and ulnar variance (MD = 0.05, 95% CI: −0.74 to 0.64). It was observed that shoulder pain occurred more commonly as a complication in above elbow immobilisation and the values were statistically significant (above elbow: 38/92, 41.3%; below elbow: 19/94, 20.2%).
Conclusion
This two-armed systematic review on the above elbow or below elbow immobilisation to be used for conservative treatment of the distal end radius fracture in adults resulted in non-significant differences in terms of functional and radiological scores among the 2 groups but significant increase in the complication rates in the above elbow group.
Keywords: Distal radius fractures, Conservative treatment, Above elbow immobilisation, Below elbow immobilisation, DASH scores
Introduction
Distal end radius fractures are one of the most common fractures seen in daily practice. It is estimated to affect about 18% of the adult population worldwide.1 There is a bimodal distribution in the incidence with the first peak in young adults (18–50 years, males) occurring due to high energy injuries while the second peak is in older age groups (> 50 years, females) occurring due to low energy trauma/trivial falls.2 The treatment of distal end radius aims mainly to maintain alignment and function of the wrist joint. Whenever, conservative treatment is indicated, they are shown to have satisfactory results.2, 3, 4, 5, 6, 7 The methods used for conservative treatment of distal end radius fractures and immobilisation of wrist are varied and a consensus is still lacking among the orthopedic fraternity regarding the superiority of any particular method over others.4, 5, 6, 7, 8
After a satisfactory reduction of fracture is obtained, the wrist is immobilised using plaster of Paris. There exists a controversy regarding the benefits and necessity of including the elbow in the plaster of Paris cast.4,9,10 The aim of this study was to analyze if any difference exists on the type of immobilisation (above elbow vs. below elbow) in the conservative treatment of these fractures.
Methods
Study identification
The study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses format (Fig. 1). An electronic literature search was performed up to 1st October 2021 in Medline, Embase, Ovid and Cochrane database using the search terms, “distal end radius fractures OR fracture of distal radius”, “conservative treatment OR non-surgical treatment”, “above elbow immobilisation” and “below elbow immobilisation”. The population intervention comparison outcome model of search was carried out in the data bases using the keywords mentioned earlier. Various combinations along with the use of Boolean operators were used to maximize the search results. The search was also replicated using the appropriate MeSH terms. Additional articles were identified through related articles feature. All bibliographies were checked for further probable studies for inclusion. Full text articles were obtained for articles after screening of title and abstract.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-analyses flow chart describing the study methodology of the systematic review.
Eligibility criteria
The following articles were included in the study: (1) randomized clinical trials, (2) describing outcome of distal end radius fractures in adults by conservative or non-surgical means using above elbow immobilisation or below elbow immobilisation, and (3) written in English. Non-randomized clinical trials, observational studies, retrospective studies, review articles, commentaries, editorials, conference presentations, operative techniques and articles without availability of full text were excluded from this review. In presence of a disagreement about inclusion or exclusion of a particular article, the senior author's opinion was sought.
Risk of bias assessment
The included articles were assessed according to the risk of bias assessment (RoB2) tool by Cochrane collaboration (Copenhagen, Denmark).11 The bias was reported according to random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other sources of bias.
Data extraction
The data was extracted by 2 authors and included the following: study details, demographic data (number of patients, gender, age, side involved, interval between fracture and cast application, classification of fracture pattern), type of immobilisation, duration of immobilisation and the following outcome measures: radiological outcomes (radial height, radial inclination, palmar tilt and ulnar variance) and functional outcomes (disability of the arm, shoulder and hand (DASH) scores and visual analogue score (VAS) scores). The data was extracted mainly from the tables provided in the articles and in cases of missing data, full texts were read by the authors to locate the same, if present. Oxford centre for evidence based medicine guidelines were used to ascertain the level of evidence. The data was collected in a excel spread sheet (Microsoft, USA) and appropriate coding was done.
Evaluation of heterogeneity
A hypothesis for data heterogeneity was postulated before the data analysis. It was hypothesised that the demographic data and the type of immobilisation used would account for the observer heterogeneity. I2 statistic tool was used to describe the proportion of total variation in the study estimates and quantify the interstudy variability. Cut off values of 25%, 50% and 75% in I2 values were used to denote low, moderate and high level of heterogeneity, respectively. Sensitivity analyses were performed for our primary outcome based on the inclusion criteria and the meta-analytic model.
Statistical analysis
The pooled data was described in terms of mean, standard deviation and ranges across the included studies. The meta-analysis was performed using Review Manager version 5.4.1 (The Cochrane Collaboration, Copenhagen, Denmark). It was performed using a random effects model and DerSemonian Laird method. Forest and funnel plots were derived from the software for pictographic description of results.
Results
Literature search
The initial data search yielded 5735 articles for consideration among which 5650 articles were excluded for being non-randomized studies. Among the remaining 55 articles, the full text of each were assessed and 49 of them were excluded (pediatric study population (n = 20), surgical intervention evaluated (n = 10), other associated fractures (n = 3) and studies not comparing above elbow and below elbow immobilisation (n = 16). Finally, 6 articles were included for the quantitative review.
Study characteristics
All the 6 studies included were randomized clinical trials.12, 13, 14, 15, 16, 17 Random sequence generation (n = 6)12, 13, 14, 15, 16, 17, and allocation concealment (n = 4)12,13,15,17 were the strength of the included studies. Attrition bias (high risk) across all the studies and detection bias (unclear risk)14, 15, 16, 17 across 4 studies were commonest biases noted. High heterogeneity (I2 > 75%) was noted among all the studies. Sensitivity analysis showed all the articles contributed to heterogeneity of I2 > 75%. All the included studies compared different methods of above elbow and below elbow immobilisation in distal end radius fractures in adult population. Functional outcome in terms of DASH scores was noted in 4 studies12,14,15,17, and VAS score in 2 studies12,17, Radiological outcomes were assessed in all the studies. AO classification of fractures was used to characterise the fracture pattern in 3 studies.13,15,17
Demographic data
A total of 515 patients were included in the review across all the articles (Table 1). The majority of the patients were females (371/430, 86.2%) and had a fracture of the left wrist (138/261, 53.9%). The mean age of the patients across the included studies varied from 60.5 years to 78.5 years. The majority of the fractures were of AO type A (209/289, 72.3%). The interval between the occurrence of fracture and cast application varied from 3.5 days to 7 days.12,17
Table 1.
Demographic data of the studies included in the review.
| Study (year) | Study design | Bias (high/unclear) | Number of patients | Mean age (year) | Gender (n) | Laterality (n) | Classification (n) | Mean follow-up |
|---|---|---|---|---|---|---|---|---|
| Okamura et al.17 (2021) | RCT | Blinding of the outcome assessment; selective reporting; attrition; other biases. | AE: 64; BE: 64 | AE: 62.97 ± 13.03; BE: 60.52 ± 14.74 | AE: M = 17, F = 47; BE: M = 23, F = 41 | AE: Rt = 31, Lt = 33; BE: Rt = 36, Lt = 28 | AE: AO Type A2 = 11, AO Type A3 = 26, AO Type C1 = 9, AO Type C2 = 16, AO Type C3 = 2; BE: AO Type A2 = 16; AO Type A3 = 29, AO Type C1 = 5, AO Type C2 = 13, AO Type C3 = 1 | 24 weeks |
| Caruso et al.15 (2019) | RCT | Attrition; blinding of the participants; blinding of the outcome assessment; selective reporting; other biases | AE: 36; BE: 36 | AE: 69.5 ± 15.2; BE: 72.3 ± 14.4 | AE: M = 4, F = 32; BE: M = 3, F = 33 | AE: Rt = 12, Lt = 24; BE: Rt = 13, Lt = 23 | AE: AO type A2.2 = 36; BE: AO type A2.2 = 36 | 12 weeks |
| Maluta et al.13 (2019) | RCT | Attrition; selective reporting; other biases | AE: 50; BE: 50 | AE: 68 (63.9–72.6); BE: 70 (66.1–74.1) | AE: M = 8, F = 42; BE: M = 6, F = 44 | – | AO classification in AE group: AO Type A = 25, AO Type B = 2, AO Type C = 23; La Fontaine in AE group: stable = 24, unstable = 26; AO classification in BE group: AO Type A = 30, AO Type B = 0, AO Type C = 20 La Fontaine in BE group: stable = 26, unstable = 24 | 32 days |
| Gamba et al.16 (2017) | RCT | Attrition; allocation concealment; blinding of the participants; blinding of the outcome assessment; selective reporting; other biases | AE: 32; BE: 40 | AE: 78.5 ± 8.3; BE: 75.9 ± 10.8 | AE: M = 1, F = 31; BE: M = 2, F = 38 | AE: Rt = 16, Lt = 16; BE: Rt = 15, Lt = 25 | La Fontaine: stable = 6, unstable = 66 | 6 weeks |
| Park et al.12 (2017) | RCT | Attrition; selective reporting; other biases | AE: 33; BE: 36 | AE: 67.5 ± 10.2; BE: 66.1 ± 8.5 | AE: M = 4, F = 29; BE: M = 2, F = 34 | – | – | AE: 6.6 months; BE: 7.0 months |
| Bong et al.14 (2006) | RCT | Attrition; allocation concealment; blinding of the participants; blinding of the outcome assessment; selective reporting; other biases | AE: 47; BE: 38 | 64 (27–91) | M = 26, F = 59 | Rt = 39, Lt = 46 | La Fontaine in AE group: stable = 22, unstable = 25; La Fontaine in BE group: stable = 18, unstable = 20 | 8 days |
RCT: randomized controlled trial; AE: above elbow; BE: below elbow; M: male; F: female; Rt: right; Lt: left.
Functional outcomes
There was no significant difference between the DASH scores in both the subgroups.12,14,15,17 (Table 2, Fig. 2) The standard mean difference (MD) between the DASH scores in both the groups was 0.52, 95% CI: −0.28 to 1.32. Two of the studies analysed VAS scores for the wrist (7.03 vs. 4.89, 6.0 vs. 5.3), elbow (0.88 vs. 0.01) and shoulder (3.52 vs. 2.69) and found that although the pain levels in the above elbow group were higher, there was no statistical difference between the 2 subgroups.12,17
Table 2.
Functional and radiological outcomes of the studies included
| Study (year) | DASH score |
Maintenance of reduction |
Loss of reduction at 8 days | PRWE at 24 weeks | VAS at 24 weeks | Adverse effects | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 8 days | 12 weeks | 24 weeks | 32 days | 6 weeks | 12 weeks | 24 weeks | |||||
| Okamura et al.17 (2021) | AE: 9.44, BE: 9.88 | AE: RH=7.49, RI=16.31, P =-1.27, UV=1.93, SO =0.13 BE: RH=7.89, RI=18.00, P=-1.04, UV=1.41, SO=0.16 |
AE: 7.36, BE: 9.18 | AE: wrist =7.03, elbow=0.88, shoulder=3.52 BE: wrist=4.89, elbow=0.00, shoulder=2.69 |
AE: shoulder pain=17/64, CRPS=1, DRUJ instability=1 BE: shoulder pain=9/64 |
||||||
| Caruso et al.15 (2019)∗ | AE: 1.7, BE: 0.8 | AE: RH=8, RI=21, P =0, UV=0 BE: RH=9, RI=22, P=0, UV=0 |
|||||||||
| Maluta et al.13 (2019) | AE: RH=10.2, RI=20.2, P=-2.1 BE: RH=9.3, RI=17.8, P=-3.7 |
||||||||||
| Gamba et al.16 (2017) | AE: UV=-0.3, RI=18.5, P =-1.2 BE: UV=-1.2, RI=19.9, P =-1.2 |
||||||||||
| Park et al.12 (2017) | AE: 78.4, BE: 81.2 | AE: RH=9.2, RI=19.5, P=8.6 BE: RH=8.7, RI=19.3, P=8.1 |
AE: 5.3, BE: 6.0 | AE: shoulder pain=21/33 BE: shoulder pain=10/36 |
|||||||
| Gamba et al.16 (2006) | AE: 70, BE: 62 | AE: 17/47, BE: 16/38 | |||||||||
DASH: disabilities of arm, shoulder and hand; PRWE: patient related wrist evaluation; VAS: visual analogue scale; AE: above elbow; BE: below elbow; RH: radial height (mm); RI: radial inclination (degrees); P: palmar tilt (degrees); UV: ulnar variance (mm); SO: articular step off (mm); CRPS: complex regional pain syndrome; DRUJ: distal radioulnar joint.
In study of Caruso et al.15, functional outcome was evaluated at 12 weeks, 4 AE and 3 BE cases with Mayo wrist scores, 4 AE and 4 BE cases with Mayo elbow scores.
Fig. 2.
Forest plot comparing the disability of the arm, shoulder and hand scores of above elbow and below elbow immobilisation groups.
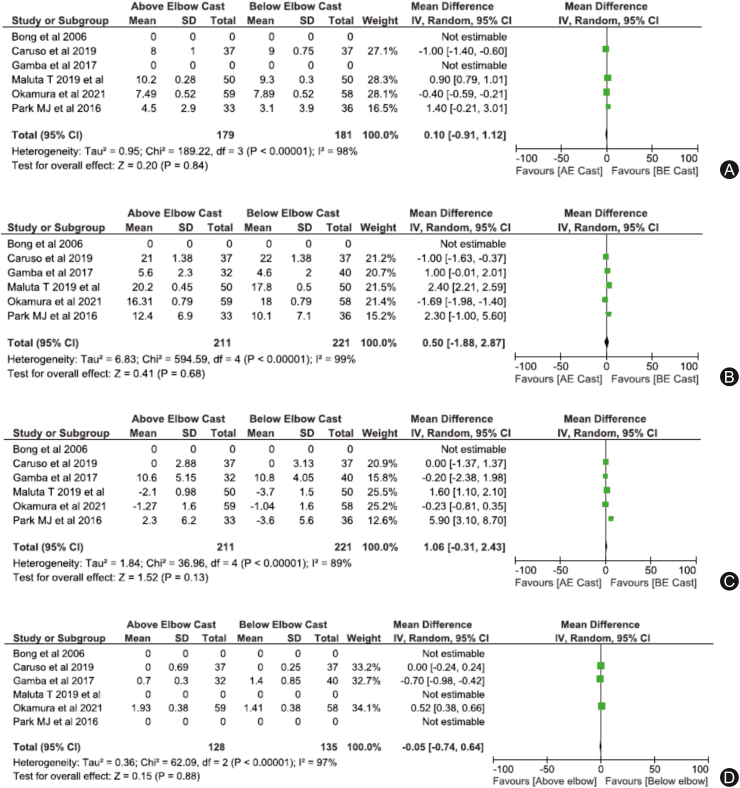
Radiological outcomes
The included studies used the difference between radial height, radial inclination, palmar/volar tilt and ulnar variance in the radiographs of the patients on presentation and final follow-up to quantify the radiological outcomes of the 2 subgroups.12,13,15, 16, 17 There was no statistical difference in the radial height (MD = 0.10, 95% CI: −0.9 to 1.12), radial inclination (MD = 0.5, 95% CI: (−1.88 to 2.87), palmar tilt (MD = 1.06, 95% CI: −0.31 to 2.43) and ulnar variance (MD = 0.05, 95% CI: −0.74 to 0.64) (Table 2, Fig. 3).
Fig. 3.
Forest plot comparing the (A) radial height; (B) radial inclination; (C) palmer tilt; and (D) ulnar variance of above elbow and below elbow immobilisation groups.
Complications
Loss of reduction till the 3rd week was the most common complication observed across all the studies. Two of the studies quantified the loss of reduction in numbers (above elbow: 42/81, 51.8%, below elbow: 39/76, 51.3%) while the others commented but did not provide any exact data for the same.14,17 It was observed that shoulder pain occurred as a complication more commonly in above elbow immobilisation and the values were statistically significant (above elbow: 38/92, 41.3%, below elbow: 19/94, 20.2%).12,17 One of the studies also noted that the shoulder pain in the above elbow group was persistent and needed interventions in the form of corticosteroid injections.14 The rates of malunion were high in both the groups (above elbow: 45.3% vs. below elbow: 45.3%).17
Discussion
The treatment of distal end radius fracture has traditionally been conservative and non-surgical by immobilisation using some sort of splinting of the wrist. The immobilisation can be with or without the elbow to achieve satisfactory healing of the fracture followed by gradual mobilisation of the wrist and hand after 4 – 6 weeks to gain function. There has been a shift towards surgical treatment of distal end radius fracture especially in case of young patients and patients with intra articular extension of fracture with the advent of better designed anatomically contoured locking plates which allows for much better reduction, early mobilisation and reduced complications in the form of malunion, articular step off, implant failure and joint stiffness. However in spite these perceived benefits, various studies conducted in this regard have failed to establish the same beyond doubt.18,19 The concerns over the complications arising due to co-morbid conditions, advancing age and anaesthesia. It has also been seen that though conservative treatment may be radiologically inferior to the operative group but the long-term functional outcomes and patient satisfaction in both the groups remains same. Keeping in mind the above facts, conservative treatment is still the preferred treatment for distal radius fractures unless the fracture pattern is irreducible, highly unstable, associated with other fractures, involves both the wrists, or an open fracture for which surgical treatment is needed.
The aim of this review was to analyze if any difference exists on the type of immobilisation (above elbow vs. below elbow) in the conservative treatment of distal end radius fractures. No significant difference in functional or radiological outcome was noted. In terms of complications in the form of shoulder pain and stiffness, a significant difference was noted with above elbow immobilisation. In terms of loss of reduction and malunion, no difference was noted in both the groups.
The literature is still in debate regarding the type of immobilisation best suited for the conservative treatment of distal radius fractures and whether the elbow immobilisation is of any real advantage or not. This study has tried to gather the highest level of evidence on this point of contention and concluded that there is no significant difference in the final outcome in terms of failure of reduction, functional scores or radiological scores whether we immobilise the elbow or not in the splints. Rather the complication rates are higher if the elbows are immobilised due to inadvertent involvement of the shoulder joint. Involvement of shoulder in the form of frozen shoulder further increases the morbidity and recovery of the patient is delayed.
It has been noted in various studies that as age increases functional level decreases, the patients are more acceptable to functional outcome not similar to the opposite well-limb.20,21 Since most of the patients analysed in this study were above 60 years, owing to their low functional demands, a below elbow immobilisation would be optimal. Studies also have shown that with the elbow immobilised, the activities of daily living are comparatively difficult to perform, which leads to a vicious cycle of stiffness and pain at the shoulder joint.12
As extensive database search across various data sources hence the selection bias for the studies included is low. This study has certain limitations in the form of high level of heterogeneity in the type of splint used, duration of splint being used, period of follow-ups, frequency of follow-up and data collected in the follow-ups. All the studies included in this analysis had I2 > 75% due to which the results of the meta-analysis should be interpreted with caution. The data analysed were not uniform across all studies included leading to further heterogeneity. Subgroup analysis of the outcomes based on classification of the distal radius fractures was not done in these studies precluding. Furthermore, the mean age of patients were above 60 years, so these results may not apply to the younger population who have higher muscle power and increased functional demands. Also, the number of studies available for evaluation was very less hence the results need to be interpreted with caution. Publication bias could not be assessed due to the number of studies reviewed.
Conclusion
This two-armed systematic review on the above elbow or below elbow splint to be used for immobilisation in case of conservative treatment of the fracture of distal radius in adults resulted in non-significant differences in terms of functional and radiological scores among the 2 groups but significant increase in the complication rates in the above elbow group. Loss of reduction and stiffness of the joints were the most common complications seen. There remains the need for standardising the method of conservative treatment of distal radius fractures in adults which can be done by a well-planned large scale prospective study design.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical statement
Not applicable.
Declarations of competing interest
The authors have no relevant financial or non-financial interests to disclose.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Vikash Raj, Sitanshu Barik and Richa. The first draft of the manuscript was written by Vikash Raj and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Nellans K.W., Kowalski E., Chung K.C. The epidemiology of distal radius fractures. Hand Clin. 2012;28:113–125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rundgren J., Bojan A., Navarro C.M., et al. Epidemiology, classification, treatment and mortality of distal radius fractures in adults: an observational study of 23,394 fractures from the national Swedish fracture register. BMC Muscoskel Disord. 2020;21:88. doi: 10.1186/s12891-020-3097-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meena S., Sharma P., Sambharia A.K., et al. Fractures of distal radius: an overview. J Fam Med Prim Care. 2014;3:325–332. doi: 10.4103/2249-4863.148101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lichtman D.M., Bindra R.R., Boyer M.I., et al. American Academy of Orthopaedic Surgeons clinical practice guideline on: the treatment of distal radius fractures. J Bone Joint Surg Am. 2011;93:775–778. doi: 10.2106/JBJS.938ebo. [DOI] [PubMed] [Google Scholar]
- 5.Bales J.G., Stern P.J. Treatment strategies of distal radius fractures. Hand Clin. 2012;28:177–184. doi: 10.1016/j.hcl.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Arora R., Lutz M., Deml C., et al. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93:2146–2153. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 7.Egol K.A., Walsh M., Romo-Cardoso S., et al. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92:1851–1857. doi: 10.2106/JBJS.I.00968. [DOI] [PubMed] [Google Scholar]
- 8.Mittal S., Agrawal A.C., Sakale H., et al. Distal radial fractures: conservative treatment. J Orthop Dis Traumatol. 2020;3:41. doi: 10.4103/JODP.JODP_28_20. [DOI] [Google Scholar]
- 9.Handoll H.H., Madhok R. Conservative interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2003;(2):CD000314. doi: 10.1002/14651858.CD000314. [DOI] [PubMed] [Google Scholar]
- 10.Raittio L., Launonen A., Hevonkorpi T., et al. Comparison of volar-flexion, ulnar-deviation and functional position cast immobilization in the non-operative treatment of distal radius fracture in elderly patients: a pragmatic randomized controlled trial study protocol. BMC Muscoskel Disord. 2017;18:401. doi: 10.1186/s12891-017-1759-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.RoB 2: a revised Cochrane risk-of-bias tool for randomized trials. https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials [DOI] [PubMed]
- 12.Park M.J., Kim J.P., Lee H.I., et al. Is a short arm cast appropriate for stable distal radius fractures in patients older than 55 years? A randomized prospective multicentre study. J Hand Surg Eur. 2017;42:487–492. doi: 10.1177/1753193417690464. [DOI] [PubMed] [Google Scholar]
- 13.Maluta T., Cengarle M., Dib G., et al. SLA-VER: study protocol description and preliminar results of the first Italian RCT on conservative treatment of distal radial fractures. Acta Biomed. 2019;90:54–60. doi: 10.23750/abm.v90i1-S.8083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bong M.R., Egol K.A., Leibman M., et al. A comparison of immediate postreduction splinting constructs for controlling initial displacement of fractures of the distal radius: a prospective randomized study of long-arm versus short-arm splinting. J Hand Surg Am. 2006;31:766–770. doi: 10.1016/j.jhsa.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 15.Caruso G., Tonon F., Gildone A., et al. Below-elbow or above-elbow cast for conservative treatment of extra-articular distal radius fractures with dorsal displacement: a prospective randomized trial. J Orthop Surg Res. 2019;14:477. doi: 10.1186/s13018-019-1530-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gamba C., Fernandez F.A.M., Llavall M.C., et al. Which immobilization is better for distal radius fracture? A prospective randomized trial. Int Orthop. 2017;41:1723–1727. doi: 10.1007/s00264-017-3518-y. [DOI] [PubMed] [Google Scholar]
- 17.Okamura A., de Moraes V.Y., Neto J.R., et al. No benefit for elbow blocking on conservative treatment of distal radius fractures: a 6-month randomized controlled trial. PLoS One. 2021;16 doi: 10.1371/journal.pone.0252667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Q., Ke C., Han S., et al. Nonoperative treatment versus volar locking plate fixation for elderly patients with distal radial fracture: a systematic review and meta-analysis. J Orthop Surg Res. 2020;15:263. doi: 10.1186/s13018-020-01734-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alharbi A.A. Operative vs. Conservative management of adult patients with distal radius fractures: a systematic review and meta-analysis. Ann Med Health Sci Res. 2020;10:5. [Google Scholar]
- 20.Beharrie A.W., Beredjiklian P.K., Bozentka D.J. Functional outcomes after open reduction and internal fixation for treatment of displaced distal radius fractures in patients over 60 years of age. J Orthop Trauma. 2004;18:680–686. doi: 10.1097/00005131-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Koenig K.M., Davis G.C., Grove M.R., et al. Is early internal fixation preferred to cast treatment for well-reduced unstable distal radial fractures? J Bone Joint Surg Am. 2009;91:2086–2093. doi: 10.2106/JBJS.H.01111. [DOI] [PubMed] [Google Scholar]