Abstract
Development of extramural health care for chronic wounds is still in its infancy in China, and thus it is urgent and vital to establish a correct concept and practicable principles. The authors reviewed recent domestic and international literature and summarized the following treatment procedures and principles for extramural health care of chronic wounds. (1) The patient needs to do self-assessment of the wound by using available simple methods; (2) The patient consults with professional physicians or nurses on wound care to define the severity and etiology of the non-healing wound; (3) Professionals evaluate the existing treatment strategies; (4) Etiological treatments are given by professionals; (5) Patients buy needed dressings via the more convenient ways from pharmacies, e-commerce platform or others; (6) Professionals provide a standardized and reasonable therapeutic plan based on the patient's wound conditions; (7) Both professionals and the patient pay attention to complications to prevent adverse outcomes; (8) Professionals strengthen the public education on wound care and integrated rehabilitation. This review expected to provide new perspectives on the therapeutic strategies for chronic wounds in an extramural setting.
Keywords: Chronic wound, Extramural health care, Home-based therapy, Wound healing, Wound management
Introduction
Chronic refractory wound, also called chronic wound, is a complex and time-consuming disease and a big challenge for physicians. With the improved daily life in China, the incidence of chronic wounds is increasing and gradually presented as a threat to life and health, resulting in a great social and economic burden.1 Clinically a chronic wound is defined as that unable to achieve or show the tendency of healing within 30 days.2,3 It is reported that the proportion of patients requiring hospitalization due to chronic wounds is 1.7% in China, mostly in the population of 40 – 60 years old (31%) and 60 – 80 years old (38%). The main causes of chronic wounds are diabetes, traumatic and pressure injuries, etc. However, only few patients (22.36%) are treated with modern dressings or new techniques.4 Moreover, there is a high rate of bacterial resistance after chronic wound infection, mainly caused by gram-negative bacteria, of which Pseudomonas aeruginosa is the predominant pathogen.5 Patients with a chronic wound often require hospitalization to define the pathogen and make the best treatment plan. After discharge, patients normally need dressing change and rehabilitation in an extramural setting.6,7
The general principles of chronic wound management have been raised by experts after repeated clinical practice and discussion, i.e., (1) keep the wound clean following debridement; (2) do appropriate debridement (to avoid excessive or insufficient debridement); (3) conduct needed differential examinations to ensure a correct diagnosis and find the etiology; (4) carry on etiological treatment; (5) monitor complications timely and prevent adverse outcomes; (6) timely change and choose the correct treatment options. If conservative therapies were adopted to promote healing, the concept of etiological treatment should be also followed, combined with the consideration of safety, phased & suitable treatment plans, and therapeutic effect. Following the preparation for wound bed, continuous conservative treatment or surgical treatment should be determined timely. For the latter, a reasonable surgery and donor site should be well selected, and the healing of the surgical wound as well as the outcome of the donor sites should be noted, so as to provide sufficient protection for the postoperative wounds; (7) education on rehabilitation and health care following the healing of wounds are also important.8
The above-mentioned principles should be applied during both intramural and extramural health care for chronic wounds. Here we reviewed related literature worldwide, hoping to standardized the rapid development of extramural health care for chronic wound management in China.
Extramural health care status of chronic wounds
Diagnosis and treatment of chronic wounds in China
Review on the characteristic domestic treatment system of chronic wounds in China
Every year in China, there are over 30 million patients requiring the treatment for chronic refractory wounds.9 On December 3, 2019, the General Office of the National Health Commission of the People's Republic of China issued a notice on further strengthening management on the treatment of chronic refractory wounds (ulcer), which both clearly puts forward the policy requirements to speed up the development of wound repair departments and establishes standards for their construction. By 2020, the number of wound repair departments officially licensed by the Chinese Medical Doctor Association had reached 357.10,11 The establishment of specialized wound repair departments and the provision of specialized treatments for refractory wounds has become the industry consensus and standard practice. The technical communication and guidance between wound care centers and the community hospital have been strengthened through the use of 4G network, and additional home-based guidance for wound care has been made available via WeChat public platforms during the outbreak of COVID-19.12,13 The current disciplinary system for wound repair provides important social benefits by offering high-quality specified care and reducing the economic consumption and burden.14 Furthermore, it is necessary to develop an appropriate out-of-hospital system for chronic wound management with domestic characteristics based on this framework.
Domestic management of chronic wounds in an extramural hospital setting
Public health plays a crucial role in the measure of a nation’s well-being. In line with the principle of “people first, life first” during China's construction and development, the country is also actively promoting the extramural medical services. The current home-based medical model in China; however, is still in its early stage and cannot fully meet the needs of chronic wound patients after their discharge from hospital.15 General condition and local wound changes are required for the management of chronic wounds, and professionalism is a prerequisite for out-of-hospital management. However, the participation of professional medical staff in home-based wound management is limited.16 The majority of patients with chronic wounds are elderly or frail individuals, including manual workers, retirees and the unemployed4 who lack basic understanding and awareness of health-related knowledge. Poor compliance from these patients often results in ineffective dressing change and rehabilitation, leading to a higher rate of recurrence.
These problems yet to be addressed properly. The standardization of domestic home-based medical services is still unformed, and the system for monitoring service quality has not been improved. The mechanism to ensure the security of medical staff has not been fully established and the nursing service is still restricted. The coverage of medical insurance for out-of-hospital treatment costs has not been universalized.17
The Chinese government has recognized the importance of the aforementioned problems and has taken steps to address them. Since 2019, both the national and provincial health commissions have issued some documents concerning “Internet Plus Medical Care” to encourage qualified medical institutions to provide professional nursing services, particularly for home-based wound care. Only nurses with a minimum of 3 years of clinical experience and a wound care qualification are permitted to provide home-based nursing services.
Out-of-hospital management of chronic wounds in other countries
The Europe and some countries like the United States, Canada, Australia, etc. begin providing the out-of-hospital chronic wound care early with rich practical experience and research findings.
Out-of-hospital management of chronic wounds in the United States
Home-based healthcare in the United States is subject to strict regulations, requiring home healthcare providers to possess an extensive array of wound dressings and treatments, as well as a thorough understanding of medical practices in the home setting. In order to promote cost-effectiveness and interdisciplinary collaboration, the providers are expected to maintain accurate and comprehensive wound records, evaluations, and treatments.18 The integration of telemedicine technology has enabled providers to treat wounds effectively, even in the absence of medical staff, by providing proper training and education to patients.19 The outcome and assessment information set (OASIS) is used to evaluate the treatments and effects of home-based care comprehensively. The application of various management technologies has resulted in successful wound treatment outcomes, as demonstrated by third-party platforms. For instance, the treatment of pressure ulcers with moist and breathable dressings, facilitated by home-based care, costs $514, and has a higher healing rate compared to traditional gauze treatment over an 8-week period.20 Meanwhile, the use of negative pressure treatment has also greatly reduced medical costs and the frequency of visits.21 As for diabetic foot ulcers, home-based treatment using negative pressure wound therapy and wet wound therapy is equally safe and effective,22 which doubles the healing rate compared to traditional community care without a platform for out-of-hospital treatment. The number of nursing visits per case has dropped from 37 to 25, and the supply cost per case has been reduced from $1923 to $406,23 highlighting the advantages of out-of-hospital care via telemedicine technology platforms.
Out-of-hospital treatment of chronic wounds in Europe
The European Telemedicine Organization has identified 3 essential requirements for effective chronic wound care in an extramural hospital setting: the competency of healthcare professionals, the continuity of care, and accessibility. The first 2 are key factors that determine patients’ trust in home-based care, while accessibility becomes critical when the first 2 are met and the 3 are inseparably linked.24 Relevant experimental research in Europe has shown that telemedicine platforms offer higher cost-effectiveness than traditional hospital-based treatment, improving the effectiveness of home care services. This approach reduces the need for hospital consultation and transportation, and mitigates safety concerns, supporting the use of telemedicine platforms.25, 26, 27 The European Telemedicine Organization is committed to prioritizing patients’ needs and refining treatment protocols and clinical practice guidelines in response to advancements in the field.28, 29, 30
Out-of-hospital treatment of chronic wounds in other countries
A study in Canada suggests that it is the healthcare organizations, rather than the care setting, has a significant impact on the wound healing rate. To this end, it is crucial to establish a platform system that presents evidence-based recommendations and provids out-of-hospital care by a skilled nursing team.31 In addition, based on an Iranian investigation, the home care strategy is more effective and cost-efficient, compared with the hospital care.32
A comparison on the out-of-hospital management of chronic wounds across different nations
The distinctive developmental background and characteristics of out-of-hospital chronic wound care have been well evidenced. The United States, for instance, has established a professional medical platform to deliver and enhance home-based healthcare services in conjunction with third-party platforms. In Europe, on the other hand, great focus has been emphasized on training professional medical personnel and integrating in-hospital and out-of-hospital resources to provide door-to-door medical services. On the basis of the existing in-hospital treatment, some diversified medical services have been proposed in China, including traditional medical platforms, family doctor consultations, and internet-based medical platforms, all of which can meet the requirements of patients with varying services. These various out-of-hospital management models from different countries have provided some valuable experience and reference for the development of home healthcare services in China.
The reflection on the out-of-hospital management of chronic wounds
In the out-of-hospital management of chronic wounds, it is essential to prioritize accurate diagnosis before treatment. An accurate diagnosis serves as the foundation for effective medical services, and continuous assessment of wounds by medical professionals is required to ensure that the correct diagnosis is maintained throughout treatment. However, even after the basic medical education, the diagnosis is more challenging than the assessment for both patients and primary healthcare providers. To address this issue, some recommendations have been proposed by us, including: (1) continuing education for primary healthcare providers regarding the diagnosis of chronic wounds, (2) regular examination of confirmed cases to improve the diagnostic quality, (3) more information exchange and cooperation between primary healthcare providers and specialists in chronic wounds, (4) use of “Internet Plus” by primary healthcare providers to assist in chronic wound diagnosis, and (5) development of guidelines for the out-of-hospital management of chronic wounds.
Insights into out-of-hospital treatment of chronic wounds
In view of the current situation in China and the progress made in this field in developed countries, the following aspects of principles should be taken into consideration in out-of-hospital practice for the management of chronic wounds.
(a) General principles of management for chronic wounds should be adhered to, as they form the foundation of clinical activities.
(b) It is prudent to assimilate and integrate the characteristics of different disciplines into out-of-hospital management, and the cross-disciplinary collaboration can result in a more comprehensive pattern of medical practice.
(c) Medical staff involved in out-of-hospital service should complete home-based care training to improve the standardization of the management process, thereby improving the overall medical standard.
(d) Primary care physicians can communicate with specialists via the internet to improve their medical expertise in dealing with patients with complex conditions.33
(e) The education related to health and self-assessment methods should be promoted to the patients and their family members so as to improve their understanding and recovery of chronic wounds.
(f) Patients should be transferred to community hospitals or other healthcare centers smoothly and the availability of medical supplies should be improved; thus the convenience for medical staffs and patients is facilitated.
(g) Some necessary measures for special situations should be prepared, and the management should be taken in a proper manner according to corresponding specialized principles for patients based on the particular condition.
(h) The diagnostic ability of medical professionals and their assessment on the status of chronic wounds should be improved.
Recommendations for the out-of-hospital treatment of chronic wounds with the common types
Diabetic foot ulcers
It is important for diabetic patients to adhere to the comprehensive treatment principles to control the following indicators, including the blood glucose, blood pressure, lipids and body weight, etc. Targeted prevention and intervention may be required for diabetics who experience complications with psychological and nutritional issues. When dressing chronic wounds, patients should follow general guidelines and receive regular assessments and specific education if needed, whether they are receiving care in community or at home. The healthcare practitioners are supposed to provide the patients with medication guidelines for specific drugs, exercises to improve circulation, such as Beecher's exercise, and decompressive means or instruments to protect the wound.34
Pressure injuries
Decompression therapy is an effective treatment and the key to prevent pressure injuries. Healthcare providers should instruct the patients to select an appropriate base of support according to the injured area, and shift their position every 2 h in order to reduce local pressure and friction.
Nutritional support is helpful for patients with hypoproteinemia and nutritional risks. These patients may require a comprehensive nutritional assessment by a qualified professional. Different diet programs should be developed under the guidance of physicians and nutritionists.
Aggressive treatment of the underlying and primary diseases is crucial.
It is recommended for the patients to receive surgical treatment within a hospital setting. Afterwards, they may continue their out-of-hospital treatment plan.35
Chronic venous ulcers of lower extremities
The fundamental therapy focuses on the postoperative wound care and elastic compression therapy, except in cases of severe lower-limb arterial obstruction and heart failure. This approach is the preferred and most effective treatment, along with regular debridement of exudate and necrotic tissues, dressing change with appropriate material and aggressive treatment against underlying and primary diseases. Supplementary treatments include the application of medicines to promote blood circulation and reduce swelling, as well as exercises that strengthen the muscles of the lower extremities.36
A reflection on process of out-of-hospital treatment of chronic wounds
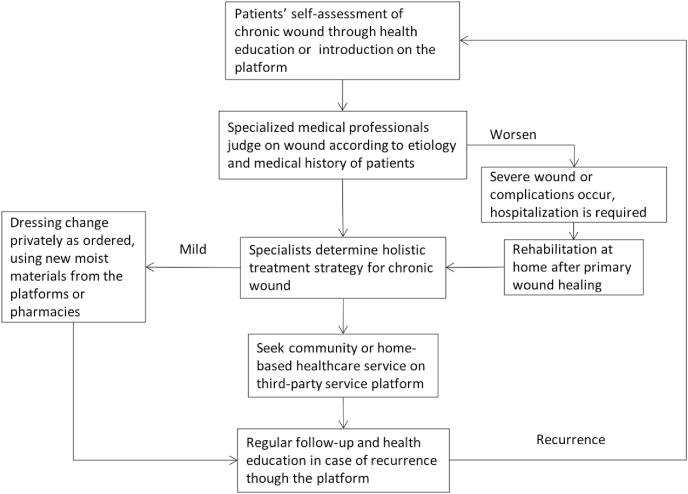
Given the fact that the out-of-hospital treatment for chronic wounds in China is still in its initial stage, it is recommended that the processes be designed on the basis of general principle in line with local conditions (Fig. 1).
Fig. 1.
Out-of-hospital treatment flow for chronic wounds.
In the case of out-of-hospital treatment carried out by professional platforms, we propose a new model of “APPENDS”, which stands for, “A (available)": dressings are available outside the hospital; “P (principle)": selection of dressings should follow the principles of chronic wound treatment; “P (professional)", the expertise of medical staff should be enhanced through continuing education and professional training on various platforms; “E (education)", the knowledge related to wound care should be popularized through various platforms; “N (normative)", the standardization of diagnoses and treatments should be improved; “D (different)", multidisciplinary management should be taken into account; “S (special)", the efficient treatment is supposed to be performed in the specific situations.
Expectations of out-of-hospital treatment for chronic wounds
Bidirectional referral mechanism
The implementation of a bidirectional referral mechanism can bolster the management of key issues and weaknesses in quality, thereby facilitating the consistent and incremental enhancement of extramural medical care. Additionally, it alleviates the burden on general hospitals and promotes the development of primary hospitals, resulting in a more rational distribution of medical resources.
Platform mode
The novel internet technology has the potential to elevate the standard of wound management for chronic wounds in out-of-hospital institutions, by outlining the appropriate techniques and criteria in home-based management procedures and fostering a harmonious doctor-patient relationship. The extensive utilization of medical resources in community health service centers, guided by diverse levels of hospitals, allows patients to have the access to high-quality medical services conveniently at home, resolving the issue of “last-mile” problem of patients in seeking medical care. Furthermore, there is a pressing need to provide sufficient guidance to the elderly population on the proper use of electronic devices.
Medical insurance
In light of the growing demand for medical attention in an aging society, significant funding may be necessary to ensure the progress of out-of-hospital managing chronic wounds. Medical and commercial insurances, as common medical payment methods, medical insurances and commercial insurances, with the support of medical evidence and relevant clinical data, are projected to offer tailored policies and services, supported by medical evidence and relevant clinical data, to meet people's needs on the out-of-hospital treatments in the future.
Diagnosis-related groups (DRGs)
The bidirectional referral mechanism represents a breakthrough in addressing the problem of “Difficult and Expensive Medical Treatments” in China. By optimizing the allocation of healthcare resources, reducing medical costs, and promoting the rational distribution of medical resources, this approach can improve the efficiency of the entire medical system. The out-of-hospital treatments should be strictly priced by group and implemented according to DRGs payment policy, in order to fully leverage the promotion effect of DRGs payment on the bidirectional referral mechanism.
Traditional Chinese medicine (TCM)
TCM, known for its efficacy in treating chronic wounds, has a long history of application in this field. The external preparation can treat wounds directly through some evidence-based procedures, offering the unique advantages of affordability and ease of application. In addition, physicians nationwide have accumulated extensive clinical experience, leading to a shorter healing period and an increased healing rate. Therefore, the role of TCM in the treatment of chronic wounds should be highly appreciated, and its potential in promoting this field should be thoroughly utilized.37
Conclusion
The out-of-hospital treatments offer several advantages. Firstly, for patients, it can relieve their psychological pressure in hospital, along with the decreased economic burden, reduced nursing frequency, and improved wound healing rate particularly when combined with the platform model. Secondly, for the hospital, it can alleviate the shortage of hospital beds and enhance the professional knowledge and skill of the medical staff. It also extends the scope of medical services, promotes the emergence of new treatment methods, and provides new job opportunities in the healthcare industry. Lastly, for medical care service, out-of-hospital treatments allow the innovation of a new mode for managing chronic wounds, solves the “last-mile” problem for medical services and opens a new chapter of telemedicine.
In summary, despite its late start, modern out-of-hospital treatments of chronic wounds in China has recently seen significant progress. China's relevant policies and the sufficient experiences of foreign out-of-hospital treatments experiences have encouraged the medical industry to actively explore and conduct research on such treatments. This endeavor has led to the specialization, professionalization, systematization and modernization of extramural medical care for patients with chronic wounds in various ways, such as the use of third-party internet service platforms, bidirectional referral mechanism, etc.
Funding
This work was funded by Medical and Health Science and Technology Program of Zhejiang Province, China (grant number: 2018247152), and Key Laboratory of The Diagnosis and Treatment of Severe Trauma and Burn of Zhejiang Province, The Second Affiliated Hospital of Zhejiang University School of Medicine, China (grant number: 2022K05).
Ethical statement
Not applicable.
Declaration of competing interest
The authors declare that there is no conflict of interests about this research.
Author contributions
Chun-Mao Han: study design, supervising the findings, editing draft; Bin Xu: Data collection and analysis, draft writing; Xin-Gang Wang, Zi-Lun Meng, Ling-Ya Zhu, Yu-Xiang Zhang, Pan Wu: draft editing, communication with team members. All authors provided critical feedback and discussed the results and contributed to the final manuscript.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Fu X.B. Establishment of a wound care discipline system in China: the review of the construction of wound care center with Chinese characteristics in 20 years and prospect. Chin J Burns. 2018;34:859–863. doi: 10.3760/cma.j.issn.1009-2587.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Wei Z.R., Huang G.T. Progress in the treatment of chronic wound and discussion on the integrated surgical wound treatment mode. Chin J Burns. 2019;35:824–827. doi: 10.3760/cma.j.issn.1009-2587.2019.11.012. [DOI] [PubMed] [Google Scholar]
- 3.Yao Z.X., Fu X.B., Cheng B. New concept of chronic wound healing: advances in the research of wound management in palliative care. Chin J Burns. 2020;36:4. doi: 10.3760/cma.j.cn501120-20190929-00388. [DOI] [PubMed] [Google Scholar]
- 4.Jiang Y., Huang S., Fu X., et al. Epidemiology of chronic cutaneous wounds in China. Wound Repair Regen. 2011;19:181–188. doi: 10.1111/j.1524-475X.2010.00666.x. [DOI] [PubMed] [Google Scholar]
- 5.Yang H., Wang W.S., Tan Y., et al. Investigation and analysis of the characteristics and drug sensitivity of bacteria in skin ulcer infections. Chin J Trauma. 2017;20:194–197. doi: 10.1016/j.cjtee.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fu X.B. Achievements and prospects of wound repair discipline system with Chinese characteristics during "13th five-year plan" period. Chin J Trauma. 2021;37:2–5. doi: 10.3760/cma.j.cn501098-20201230-00751. [DOI] [Google Scholar]
- 7.Fu X.B. Application of constructing standardized and well-developed wound repair department in China. Chin J Trauma. 2020;36:3–5. doi: 10.3760/cma.j.issn.1001-8050.2020.01.002. [DOI] [Google Scholar]
- 8.Dong W., Xiao Y.R., Wu M.J., et al. Thoughts and principles of diagnosis and treatment of chronic refractory wounds in China. Chin J Burns. 2018;34:868–873. doi: 10.3760/cma.j.issn.1009-2587.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Fu X.B. Guiding the disciplinary construction of wound treatment and related personnel development based on the general guideline of research-oriented hospital. J Chin Res Hospitals. 2016;3:2–5. doi: 10.19450/j.cnki.jcrh.2016.01.002. [DOI] [Google Scholar]
- 10.General Office of National Health Commission Notice from the General Office of the National Health Commission on strengthening the management of diagnosis and treatment of superficial chronic refractory wounds (ulcers): medical letter of the National Health Office (No. 865). (2019-12-02) 2019-12-05. http://www.nhc.gov.cn/yzygj/s7659/201912/602716f0471944b8b63b0adabe4546df.shtml
- 11.Fu X. State policy for managing chronic skin wounds in China. Wound Repair Regen. 2020;28:576–577. doi: 10.1111/wrr.12808. [DOI] [PubMed] [Google Scholar]
- 12.Fu X.B. Connotation of the construction of the discipline system of wound repair with Chinese characteristics. Chin J Injury Repair Wound Healing (Electronic Edition) 2020;15:1–4. doi: 10.3877/cma.j.issn.1673-9450.2020.01.001. [DOI] [Google Scholar]
- 13.Ting X., Minjie W., Hu L., et al. Application of telemedicine system with 4G and high-resolution video in diagnosis and treatment of wounds between wound healing department and community health care center in China. Int J Low Extrem Wounds. 2011;10:167–168. doi: 10.1177/1534734611420493. [DOI] [PubMed] [Google Scholar]
- 14.Fu X.B. To build a well-developed wound repair department in China with the original mind and mission. Chin J Burns. 2020;36:1–4. doi: 10.3760/cma.j.issn.1009-2587.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Chen T., Bai M., Zhou R., et al. Strategies to develop home-based medical care in China: a SWOT-CLPV analysis. Chin General Pract. 2020;23:4285–4290. doi: 10.12114/j.issn.1007-9572.2020.00.579. [DOI] [Google Scholar]
- 16.Chen T., Yao N.L., Su M.Z., et al. Challenges of home-based medical care in China: a telephone interview from the perspectives of home care providers. Chin General Practice. 2020;23:1459–1465. [Google Scholar]
- 17.Lu M., Yu Y.J., Li Z.D., et al. Construction and application of continuity nursing model based on family medical platform. Chin J Nurs. 2019;54:1851–1855. doi: 10.3761/j.issn.0254-1769.2019.12.017. [DOI] [Google Scholar]
- 18.Meah Y.S., Gliatto P.M., Ko F.C., et al. In: Hayashi J.L., Leff B., et al., editors. 2016. Wound Care in Home-Based Settings; pp. 195–236. (Geriatric Home-Based Medical Care. Principles and Practice Springer International Publishing New York). [DOI] [Google Scholar]
- 19.Litzinger G., Rossman T., Demuth B., et al. In-home wound care management utilizing information technology. Home Healthc Nurse. 2007;25:119–130. doi: 10.1097/00004045-200702000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Sebern M.D. Pressure ulcer management in home health care: efficacy and cost effectiveness of moisture vapor permeable dressing. Arch Phys Med Rehabil. 1986;67:726–729. doi: 10.1016/0003-9993(86)90004-3. [DOI] [PubMed] [Google Scholar]
- 21.Schwien T., Gilbert J., Lang C. Pressure ulcer prevalence and the role of negative pressure wound therapy in home health quality outcomes. Ostomy/Wound Manag. 2005;51:47–60. [PubMed] [Google Scholar]
- 22.Blume P.A., Walters J., Payne W., et al. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial. Diabetes Care. 2008;31:631–636. doi: 10.2337/dc07-2196. [DOI] [PubMed] [Google Scholar]
- 23.Harrison M.B., Graham I.D., Lorimer K., et al. Leg-ulcer care in the community, before and after implementation of an evidence-based service. CMAJ. 2005;172:1447–1452. doi: 10.1503/cmaj.1041441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith-Strøm H., Iversen M.M., Graue M., et al. An integrated wound-care pathway, supported by telemedicine, and competent wound management-Essential in follow-up care of adults with diabetic foot ulcers. Int J Med Inf. 2016;94:59–66. doi: 10.1016/j.ijmedinf.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 25.Bergersen T.K., Storheim E., Gundersen S., et al. Improved clinical efficacy with wound support network between hospital and home care service. Adv Skin Wound Care. 2016;29:511–517. doi: 10.1097/01.ASW.0000499714.97688.4b. [DOI] [PubMed] [Google Scholar]
- 26.Téot L., Geri C., Lano J., et al. Complex wound healing outcomes for outpatients receiving care via telemedicine, home health, or wound clinic: a randomized controlled trial. Int J Low Extrem Wounds. 2020;19:197–204. doi: 10.1177/1534734619894485. [DOI] [PubMed] [Google Scholar]
- 27.Zarchi K., Haugaard V.B., Dufour D.N., et al. Expert advice provided through telemedicine improves healing of chronic wounds: prospective cluster controlled study. J Invest Dermatol. 2015;135:895–900. doi: 10.1038/jid.2014.441. [DOI] [PubMed] [Google Scholar]
- 28.Morrell C.J., Walters S.J., Dixon S., et al. Cost effectiveness of community leg ulcer clinics: randomised controlled trial. BMJ. 1998;316:1487–1491. doi: 10.1136/bmj.316.7143.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Souliotis K., Kalemikerakis I., Saridi M., et al. A cost and clinical effectiveness analysis among moist wound healing dressings versus traditional methods in home care patients with pressure ulcers. Wound Repair Regen. 2016;24:596–601. doi: 10.1111/wrr.12433. [DOI] [PubMed] [Google Scholar]
- 30.García-Sánchez F.J., Martínez-Vizcaíno V., Rodríguez-Martín B. Conceptualisations on home care for pressure ulcers in Spain: perspectives of patients and their caregivers. Scand J Caring Sci. 2019;33:592–599. doi: 10.1111/scs.12652. [DOI] [PubMed] [Google Scholar]
- 31.Harrison M.B., Graham I.D., Lorimer K., et al. Nurse clinic versus home delivery of evidence-based community leg ulcer care: a randomized health services trial. BMC Health Serv Res. 2008;8:243. doi: 10.1186/1472-6963-8-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jafary M.R., Amini M.R., Sanjari M., et al. Comparison home care service versus hospital-based care in patients with diabetic foot ulcer: an economic evaluation study. J Diabetes Metab Disord. 2020;19:445–452. doi: 10.1007/s40200-020-00527-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dong W., Nie L.J., Wu M.J., et al. WoundCareLog APP—A new application to record wound diagnosis and healing. Chin J Traumatol. 2019;22:296–299. doi: 10.1016/j.cjtee.2019.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chinese Diabetes Society Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition) Chin J Diabetes. 2021;13:315–409. doi: 10.3760/cma.j.cn115791-20210221-00095. [DOI] [Google Scholar]
- 35.Wang W., Zhang X., Li Y., et al. The hospital-community-family linkage nursing practice of elderly patients with stress injury at home. Chin J Nurs. 2021;56:1225–1229. doi: 10.3761/j.issn.0254-1769.2021.08.017. [DOI] [Google Scholar]
- 36.Chinese Society of Microcirculation & Professional Committee of Vascular Disease Blood pressure group. Chinese expert consensus on vascular pressure therapy (2021 version) Natl Med J China (Peking) 2021;101:1214–1225. doi: 10.3760/cma.j.cn112137-20201111-03062. [DOI] [Google Scholar]
- 37.Yin S.P., Xu Z.Y., Min W., et al. Research progress on external preparations of traditional Chinese medicine for chronic wound treatment. J Nanjing Univ Traditional Chin Med. 2020;36:690–695. doi: 10.14148/j.issn.1672-0482.2020.0690. [DOI] [Google Scholar]