Abstract
Purpose
The present study aimed to treat fractures of the distal end of the radius in children with Robert Jones (RJ) bandage. The objective was to compare this treatment modality with the cast regarding the frequency of the complication occurrence, child comfortability, and family satisfaction.
Methods
The study was a randomized controlled non-inferiority clinical trial including children with recent (less than 5 days) fractures at the distal end of the radius OTA/AO 23-A2, which is usually treated conservatively. Those with open fractures, pathological fracture, severely displaced fracture that needs reduction or multiple injuries were excluded. The participants were divided randomly into 2 groups according to the treatment modalities. Group 1 was treated by plaster of Paris cast (the control group), and Group 2 by modified RJ bandage (the trial group). The difference between the 2 groups was found by the Chi-squared test. The difference was considered statistically significant when the p value was less than 0.05.
Results
There were 150 children (aged 2 – 12 years, any gender) included in the study, 75 in each group. The complications occured in 5 (3.3%) cases only, pressure sores of 3 cases in Group 1 and fracture displacement of 2 cases in Group 2. There was no statistically significant difference in the rate of complication occurrence between both modalities of treatment (p = 0.649). Children treated by RJ bandages were more comfortable than those treated by the cast (97.3% vs. 73.3%, p < 0.001) with a statistically significant difference between them. Contrary to that, the families were more satisfied with the cast than RJ bandage (88.0% vs. 81.3%), but without a statistically significant difference (p = 0.257).
Conclusion
RJ bandage is a non-inferior alternative to the cast for the treatment of fractures at the distal end of the radius that can be treated conservatively in children.
Keywords: Robert Jones bandage, Fracture, Distal end of radius, Children
Introduction
Fractures of the distal forearm (especially the radius fractures) are most commonly reported in children and a frequent reason for visiting the emergency unit and orthopedic clinic in hospitals.1 Because of patient's age and fracture site proximity to the joint, these fractures especially types of OTA/AO 23-A2 heal well and have a good ability to remodel the bone even with mild displacement.2,3 Therefore, most of these fractures are treated conservatively by a short arm cast and needed a frequent visit to the orthopedic clinic within 4 – 6 weeks with no significant complications.3, 4, 5, 6 Several studies report successful treatment of these fractures by removable splints as a substitute for the cast. They have proved to be more comfortable for the patients, efficient in maintaining fracture stability with an acceptable alignment, safe, and relatively cost-effective in managing these common minor injuries in children.7, 8, 9, 10, 11, 12, 13, 14, 15, 16
Robert Jones (RJ) bandage modified by Brodell et al.17 is a thick well-padded dressing often used after trauma and elective orthopedic operations, especially around the knee. It provides a firm compression with evenly distributed pressure and is commonly used for knee disorders.17 It is easy to be applied, provides firm compression, and is light and cheap. The objective of this study was to compare RJ bandage with the cast, regarding the frequency of the complication occurrence, child comfortability, and family satisfaction.
Methods
Study type and approvals
The study was a randomized controlled non-inferiority clinical trial of patients based on a parallel-group type with an allocation ratio of 1:1. The approval for this study was obtained from the Medical Research Ethics Committee, General Directorate of Health, Government of Duhok, Kurdistan Region, Iraq (Reference number: 10112021-11-10R1). The trial was registered at the Clinical Trial.gov PRS website (registration number NCT05521464).
Study design
The study was done in the emergency reception unit and the orthopedic unit of Duhok Emergency Teaching Hospital (single-center study), Duhok city, Iraq during the period extending from October 2021 to August 2022.
A team from the hospital composed of a consultant orthopedic surgeon (person 1), a permanent resident orthopedic doctor (person 2), and a radiologist (person 3) conducted this study. Person 1 generated the random allocation sequence, assessed the outcomes clinically, analyzed the results, and drafted the article. Person 2 enrolled the participants in the study, assigned the interventions, applied the treatment modalities to the participants, and drafted the article. Person 3 assessed the radiological outcome. The medical staffs in both the emergency reception unit and orthopedic outpatient room were requested to inform the study team daily about all the children who attained the hospital with a recent wrist trauma.
Inclusion and exclusion criteria
The study included children who attained the hospital with a history of recent wrist trauma. The inclusion criteria were: (1) patients aged 2 – 12 years; (2) containing both male and female; (3) fracture less than 5 days; (4) fracture at the distal end of radius type OTA/AO 23-A2 proofed by a radiograph film in 2 views (posteroanterior and lateral). OTA/AO 23-A2 fractures are usually treated conservatively without intervention, such as torus (buckle) metaphyseal fracture, greenstick fracture, undisplaced distal radial physis fracture (Salter-Harris classification type 1 and 2 only), or undisplaced or minimal displaced metaphyseal fracture with no need of reduction. The minimally displaced fracture was considered when the fracture fragments have a tilt of fewer than 15° and shift to fewer than 5 mm at the fracture site in both views. Patients with open fractures, pathological fractures, displaced fractures that need reduction, associated fractures of the ulnar bone, polytrauma or having delayed presentation beyond 5 days were excluded. An informed consent signed by one of the parents or the guardian of the child was obtained from the cases eligible for this study.
Hypothesis
The null hypothesis: there is no difference between both treatment modalities (the use of the RJ bandage is as safe as the use of the cast). The alternative hypothesis: there is a difference between both treatment modalities (the use of RJ bandage is associated with a more complication rate than the use of the cast).
Interventions
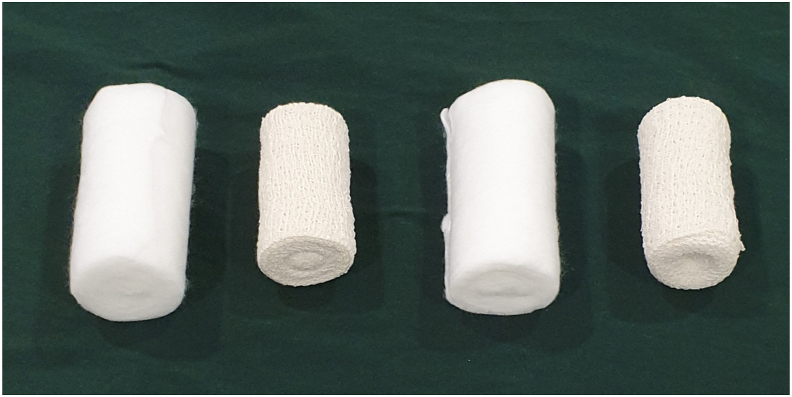
The participants included received one of the treatments planned for this study. The first treatment was to apply a short arm cast from below the elbow to the finger knuckles. The cast was made from a 2-inch plaster of Paris bandage immersed in water and wrapped over a cotton pad until it sets (Fig. 1). The participants who received this treatment with the cast were considered Group 1 (the control group). The second treatment was to use RJ bandage (firmly use with 2 layers of bulky cotton cloth and 2 layers of elastic bandage alternately in the following order: cotton – bandage – cotton – bandage) (Fig. 2).17 It was applied from below the elbow to the finger knuckles (Fig. 3). The participants who received RJ bandage treatment were considered Group 2 (the trial group). Both interventions were applied by the same person, who was a permanent resident orthopedic doctor (person 2 from the team of this study).
Fig. 1.
A patient was treated by a cast.
Fig. 2.
Items used for Robert Jones bandage.
Fig. 3.
A patient was treated by Robert Jones bandage.
The participants and their companions were instructed to keep the dressing clean and dry. Follow-ups (at the end of the 2nd, 4th, 6th, and 12th week) of both groups were conducted. At each visit of follow-up, the participant was checked for possible complications. The final assessment was done at the end of the 26th week by the consultant orthopedic doctor in collaboration with the radiologist.
Outcomes
The primary outcome of the study was the occurrence of complications reported during the follow-up period or at the last assessment. The clinical outcome was assessed by persons 1 and 2, and radiological outcome by person 3. The complications were considered to be present if one of the following was noticed: (1) skin problems like pressure soreness, skin irritation, itching, and dermatitis; (2) bone deformity due to a displacement of the bone fragments at the fracture site to an unacceptable degree (tilt more than 15° and/or shift more than 50% of the bone width at the fracture site) confirmed by the report of the radiologist, or due to growth disturbance from growth plate damage; (3) joint stiffness by limitation of wrist movements (limitation of more than 10° in any direction); and (4) re-fracture within 12 weeks.
The secondary outcomes were the patients’ comfort and family (parents/guardians) satisfaction of the treatment. These outcomes were assessed by taking the opinion of the patient and their family in a special form by persons 1 and 2 from the team of the study. The opinions were recorded in form of yes or no. If the answer was yes, then the cause of discomfort or dissatisfaction was requested. No standardized questionnaires were used to assess these secondary outcomes.
Sample size calculation
The assumed sample size was calculated by using the G∗Power 3.1.9.7 computer software program. A minimum of 148 participants (74 for each group) was required to have an 80% chance of detecting the difference between the groups, and a two-sided 95% confidence level (0.05 level of significance) to avoid the type 1-alpha error, with a probable hypothetical effect size of about 0.3 and a degree of freedom of 1 in the contiguity table.
Randomization
The allocation of the participants into the modalities of the treatment was done by a simple randomization method with an allocation ratio of 1:1. It was generated by using the website program www.randomization.com. The first generator of the program was used to randomize 148 subjects into both modalities of treatment blocks (74 by casts and 74 by RJ bandages). The random allocation sequence was generated by person 1 from the team in the study. It was concealed from the rest of the study team. Person 2 enrolled the participants in the study (assessed the eligibility of the cases, obtained informed consent) and assigned the interventions.
Blinding
The team of the study (apart from person 3 – the radiologist) was not blinded to the modality of treatment that they provided to the patients. The radiologist who assessed the radiological outcome of the cases was blinded to the modalities of treatment. The participants were blinded to the result of the treatment of the other patients included in this study.
Data collection
The data was collected in a special paper for each patient separately. The data included 2 parts: one is the basic demographic data of the patient and injury like name, age, gender, place of living, date of a wrist injury, type of wrist injury (proved by the radiographic film), type of treatment (group), the time interval between the injury and beginning of treatment, duration of treatment, and dates of each follow-up; another is the outcomes during each follow-up visit and at the final assessment like complications of treatment, patient comfortability, and family satisfaction.
Statistical analysis
The data analysis was performed by SPSS 23.0. The statistical analysis included the standard descriptive statistics used to describe the basic descriptive data of the patients and injuries. The means and standard deviations (SD) or medians and interquartile ranges were used for the continuous variables, while frequencies and percentages were used for the categorical variables. The comparison between the outcomes of the treatment modalities in both groups was done by finding the difference between the summary statistics in the Chi-squared test. The difference was considered statistically significant when the p value was less than 0.05.
Results
The total number of 162 patients with fractures at the distal end of the radius treated conservatively in the Duhok Emergency Teaching hospital from October 2021 to August 2022 was enrolled in this study. However, 12 of them were lost to the follow-up and their data were not completed. Finally, 150 patients were included in the statistical analysis (75 in each group, more than the assumed sample size). They were 93 (62.0%) males and 57 (38.0%) females. The mean of age was (7.5 ± 2.4) years (range 2 – 12 years). There were 85 (56.7%) buckle fractures (Fig. 4), 38 (25.3%) metaphyseal fractures (Fig. 5), and 27 (18.0%) physeal fractures (Fig. 6, Table 1). No case of greenstick fracture was found in the current study. All included fractures were of OTA/AO 23-A2 type. The average duration of the treatment was 4.35 (SD 0.7) weeks.
Fig. 4.
Radiographic film of a patient with a buckle fracture at the distal metaphysis of the radial bone.
Fig. 5.
Radiographic film of a patient with a metaphyseal fracture at the distal end of the radius.
Fig. 6.

Radiographic film of a patient with a fracture at the distal physis (Salter-Harris type 1) of the radial bone.
Table 1.
Type of wrist injury and the treatment modality, n (%).
| Type of wrist injury | Treatment modality |
|
|---|---|---|
| Cast | RJ bandage | |
| Buckle fracture | 46 (54.1) | 39 (45.9) |
| Metaphyseal fracture | 14 (36.8) | 24 (63.2) |
| Physeal fracture | 15 (55.6) | 12 (44.4) |
| Total | 75 (50.0) | 75 (50.0) |
RJ: Robert Jones.
The complications occur only in 5 cases (3.3%) (Table 2). Three patients developed pressure sores of the skin in those treated by the cast. Two of the patients in Group 2 developed fracture displacement to unacceptable degrees. They had complete metaphyseal fracture with a mild and acceptable degree of displacement (angulation less than 10°), but worsening (more than 15°) after 2 weeks. The displacement was corrected by manipulation under anesthesia. There was no statistically significant difference in the rate of complication occurrence between both modalities of treatment (p = 0.649). No re-fracture was reported among the participants included in this study during the follow-up period.
Table 2.
The outcomes of complication, child comfortability, and family satisfaction between the 2 groups, n (%).
| Treatment modality | Group 1 | Group 2 | p value |
|---|---|---|---|
| Complications | 0.649 | ||
| Pressure sore | 3 (4.0) | 2 (2.7) | |
| Re-displacement | 72 (96.0) | 73 (97.3) | |
| Child comfortability | < 0.001 | ||
| Comfortable | 55 (73.3) | 73 (97.3) | |
| Not comfortable | 20 (26.7) | 2 (2.7) | |
| Family satisfaction | 0.257 | ||
| Satisfied | 66 (88.0) | 61 (81.3) | |
| Not satisfied | 9 (12.0) | 14 (18.7) |
Most of the children were comfortable with the received treatment for their wrist problems (Table 2). However, those patients treated with the modified RJ bandage were more comfortable than those treated with the cast (97.3% vs. 73.3%) with a statistically significant difference between them (p < 0.001). In Group 1, 17 cases reported non-comfortability due to its relatively heavy weight and 3 due to pressure sore. In Group 2, 2 children were not comfortable because of tight bandages with slight hand and finger swelling, but without neurovascular abnormality. After a few days of hand elevation and use of anti-inflammatory drug, their complaints were improved.
On the contrary, family satisfaction with the treatment modality showed controversy with the preference of the cast over RJ bandage (88.0% vs. 81.3%), but the difference was not statistically significant (p = 0.257) (Table 2). In Group 1, 6 families were not satisfied with the results due to the heavy weight of the cast, and 3 dues to the development of a pressure sore. In Group 2, the causes of families' non-satisfaction were loosening of the bandage (5 cases), the child trying to open the bandage (5 cases), tight bandage (2 cases), and fracture displacement (2 cases).
Discussion
Interpretation of the results
Treatment of the undisplaced or minimally displaced fractures in the distal end of the radius of type OTA/AO 23-A2 with the cast is relatively safe and has a low rate of complications. Therefore, it can be considered the gold modality of treatment of such injuries. However, some patients may complain of its relatively heavy weight (like some of the patients in the present study). Therefore, different previous studies tried to use different types of splints to overcome this issue and minimize the cost of the treatment.4,13, 14, 15,18,19
RJ bandage (and its modification) offers the advantages of being light in weight and cheap with its relative safety (low rate of complications as reported in the results of this study). The types of complication were different between the 2 groups of the study. The complication of patients treated with RJ bandage was displacement of the fracture after a few days, which required correction by manipulation under anesthesia. It did not occur neither in those with torus (buckle) fractures nor in those with physeal fractures. Loss of reduction may occur even in those treated by a cast. Although this issue was not reported in the current study, other studies did with different percentages.3,9,10,18,20,21
Other weak point in RJ bandage modality of treatment was the loosening of the bandage and the child's trial to remove it (5 cases in each group). These were the main causes of family non-satisfaction with this treatment modality. However, they cannot be considered complications of the treatment and they can be overcome by more observation of the case, applying a layer of Tubigrip bandage, or switching the modality of treatment to cast (authors' suggestion). Other studies encouraged the use of soft cotton bandages with or without Tubigrip mainly for torus (buckle fractures) in the distal end of the radius in children and even for the non-displaced extra-articular fractures in the distal radius in adults.22, 23, 24, 25
In general, the rate of complications in this study was low (3.3%) and there was statistically no significant difference between both modalities of treatment. This made RJ bandages a non-inferior modality to the golden treatment (cast) for fractures in children. The null hypothesis was accepted. So, RJ bandage can be considered relatively a safe method that can be used as a substitute for the cast to treat these fractures in this age group.
Although there are lots of studies reporting successful results from the use of different types of removable splints as a substitute for the cast, they still were not been considered as the golden standard method in managing these types of injuries in children.7, 8, 9, 10, 11, 12, 13, 14, 15, 16 Therefore, the current study did not make a comparison of its results with any of these removable splints. However, the authors have the desire to conduct such a study. Theoretically, the RJ bandage method is supposed to be a simpler and cheaper one.
Generalizability
This treatment requires limited materials (cotton and elastic bandages only) and limited experience. The application technology is much simple and easy and can be applied even by non-professional medical personnel. The impact of the current study on clinical practice will facilitate the treatment of minor injuries commonly in these children. Therefore, it will be a helpful method to treat these injuries in different communities especially those with limited resources or living in unusual life conditions like refugee camps.26
Limitations of the study
The random sequence allocation of the participants was not concealed from person 2 of the study team who enrolled the participants in the study and assigned their interventions. Neither the team of the study (apart from person 3) nor the participants were blinded by the modality of the treatment.
In conclusion, RJ bandage is a non-inferior alternative to the cast for the treatment of fractures at the distal end of the radius type OTA/AO 23-A2 that can be treated conservatively in children.
Funding
Nil.
Ethical statement
The approval for this study was obtained from the Medical Research Ethics Committee, General Directorate of Health, Government of Duhok, Kurdistan Region, Iraq (Reference number: 10112021-11-10R1).
Declaration of competing interest
The authors declare no competing interest.
Author contributions
Both authors participated in the conceptualization, drafting, and editing of the manuscript.
Acknowledgments
The authors would like to thank the radiologist (Rahima Salih Nabi, phone: 00964750 480 7202) in the imaging department at Duhok Emergency Hospital for kind her help in evaluating the outcome of the cases radiologically.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Hedström E.M., Svensson O., Bergström U., et al. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81:148–153. doi: 10.3109/17453671003628780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilkins K.E. Principles of fracture remodeling in children. Injury. 2005;36:3–11. doi: 10.1016/j.injury.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Al-Ansari K., Howard A., Seeto B., et al. Minimally angulated pediatric wrist fractures: is immobilization without manipulation enough? CJEM. 2007;9:9–15. doi: 10.1017/s1481803500014676. [DOI] [PubMed] [Google Scholar]
- 4.Do T.T., Strub W.M., Foad S.L., et al. Reduction versus remodeling in pediatric distal forearm fractures: a preliminary cost analysis. J Pediatr Orthop B. 2003;12:109–115. doi: 10.1097/01.bpb.0000043725.21564.7b. [DOI] [PubMed] [Google Scholar]
- 5.Edmonds E.W. No difference in improvement in physical function between splint and cast at 6 weeks in children with minimally angulated fractures of the distal radius. Evid Base Med. 2011;16:49–50. doi: 10.1136/ebm1161. [DOI] [PubMed] [Google Scholar]
- 6.Abraham A., Handoll H.H.G., Khan T. Interventions for treating wrist fractures in children. Cochrane Database Syst Rev. 2008;16:CD004576. doi: 10.1002/14651858.CD004576.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Boutis K., Willan A., Babyn P., et al. Cast versus splint in children with minimally angulated fractures of the distal radius: a randomized controlled trial. CMAJ (Can Med Assoc J) 2010;182:1507–1512. doi: 10.1503/cmaj.100119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al Khudairy A., Hirpara K.M., Kelly I.P., et al. Conservative treatment of the distal radius fracture using thermoplastic splint: pilot study results. Eur J Orthop Surg Traumatol. 2013;23:647–650. doi: 10.1007/s00590-012-1042-8. [DOI] [PubMed] [Google Scholar]
- 9.Denes A.E., Jr., Goding R., Tamborlane J., et al. Maintenance of reduction of pediatric distal radius fractures with a sugar-tong splint. Am J Orthoped. 2007;36:68–70. https://pubmed.ncbi.nlm.nih.gov/17405634/ [PubMed] [Google Scholar]
- 10.Boutis K., Howard A., Constantine E., et al. Evidence into practice: pediatric orthopaedic surgeon use of removable splints for common pediatric fractures. J Pediatr Orthop. 2015;35:18–23. doi: 10.1097/BPO.0000000000000223. [DOI] [PubMed] [Google Scholar]
- 11.Hill C.E., Masters J.P.M., Perry D.C. A systematic review of alternative splinting versus complete plaster casts for the management of childhood buckle fractures of the wrist. J Pediatr Orthop B. 2016;25:183–190. doi: 10.1097/BPB.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 12.von Keyserlingk C., Boutis K., Willan A.R., et al. Cost-effectiveness analysis of cast versus splint in children with acceptably angulated wrist fractures. Int J Technol Assess Health Care. 2011;27:101–107. doi: 10.1017/s0266462311000067. [DOI] [PubMed] [Google Scholar]
- 13.Davidson J.S., Brown D.J., Barnes S.N., et al. Simple treatment for torus fractures of the distal radius. J Bone Joint Surg Br. 2001;83:1173–1175. doi: 10.1302/0301-620x.83b8.11451. [DOI] [PubMed] [Google Scholar]
- 14.Firmin F., Crouch R. Splinting versus casting of "torus" fractures to the distal radius in the paediatric patient presenting at the emergency department (ED): a literature review. Int Emerg Nurs. 2009;17:173–178. doi: 10.1016/j.ienj.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Colaco K., Willan A., Stimec J., et al. Home management versus primary care physician follow-up of patients with distal radius buckle fractures: a randomized controlled trial. Ann Emerg Med. 2021;77:163–173. doi: 10.1016/j.annemergmed.2020.07.039. [DOI] [PubMed] [Google Scholar]
- 16.Wright E. Treating buckle fractures in children with removable splints. Nurs Child Young People. 2011;23:14–17. doi: 10.7748/ncyp2011.12.23.10.14.c8832. [DOI] [PubMed] [Google Scholar]
- 17.Brodell J.D., Axon D.L., Evarts C.M. The Robert Jones bandage. J Bone Joint Surg Br. 1986;68:776–779. doi: 10.1302/0301-620X.68B5.3782244. [DOI] [PubMed] [Google Scholar]
- 18.Acree J.S., Schlechter J., Buzin S. Cost analysis and performance in distal pediatric forearm fractures: is a short-arm cast superior to a sugar-tong splint? J Pediatr Orthop B. 2017;26:424–428. doi: 10.1097/BPB.0000000000000382. [DOI] [PubMed] [Google Scholar]
- 19.Fitzgerald E., Mannion J., Boran S. Management of “torus” or “buckle” fractures of the distal radius: a systematic review. Ir J Med Sci. 2021;191:2311–2318. doi: 10.1007/s11845-021-02801-1. [DOI] [PubMed] [Google Scholar]
- 20.McLauchlan G.J., Cowan B., Annan I.H., et al. Management of completely displaced metaphyseal fractures of the distal radius in children. A prospective, randomised controlled trial. J Bone Joint Surg Br. 2002;84:413–417. doi: 10.1302/0301-620X.84B3.0840413. [DOI] [PubMed] [Google Scholar]
- 21.Goldstein R.Y., Otsuka N.Y., Egol K.A. Re-displacement of extraphyseal distal radius fractures following initial reduction in skeletally immature patients--can it be prevented? Bull Hosp Jt Dis. 2013;71:132–137. https://hjdbulletin.org/archives/view/7 [PubMed] [Google Scholar]
- 22.Pountos I., Clegg J., Siddiqui A. Diagnosis and treatment of greenstick and torus fractures of the distal radius in children: a prospective randomised single blind study. J Child Orthop. 2010;4:321–326. doi: 10.1007/s11832-010-0269-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.West S., Andrews J., Bebbington A., et al. Buckle fractures of the distal radius are safely treated in a soft bandage: a randomized prospective trial of bandage versus plaster cast. J Pediatr Orthop. 2005;25:322–325. doi: 10.1097/01.bpo.0000152909.16045.38. [DOI] [PubMed] [Google Scholar]
- 24.Arti H.R., Farahnak R. A comparative study on treatment outcomes of bandage and casting in non-displaced extra-articular fracture of distal radius: a clinical trial study. Pol Przegl Chir. 2020;92:12–15. doi: 10.5604/01.3001.0014.3760. [DOI] [PubMed] [Google Scholar]
- 25.Perry D.C., Achten J., Knight R., et al. Offer of a bandage versus rigid immobilisation in 4- to 15-year-olds with distal radius torus fractures: the FORCE equivalence RCT. Health Technol Assess. 2022;26:1–78. doi: 10.3310/BDNS6122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.No author Healthcare in refugee camps and settlements. http://www.uniteforsight.org/refugee-health/module1 [Unite for Sight]