Abstract
People suffering from fatigue syndromes spend less time exercising each day, thus aggravating their motor difficulties. Indeed, muscles and mobility deteriorate with age, while exercising muscles is the only sure countermeasure. It is useful to offer a safe and toll-free rehabilitation training: Full-Body In-Bed Gym, easy to learn and performe at home. We suggest a 10–20 min daily routine of easy and safe physical exercises that may improve the main 200 skeletal muscles used for every-day activities. Many of the exercises can be performed in bed (Full-Body In-Bed Gym), so hospital patients can learn this light workout before leaving the hospital. The routine consists of series of repetitions of 15 bodyweight exercises to be performed one after the other without time breaks in between. Alternating sequences of arm and leg exercises are followed by moving body parts in lying and sitting positions in bed. These are followed by series of tiptoeing off the bed. Progressive improvements can be tested by a series of push-ups on the floor. Starting from 3-5, number of repetitions are increased by adding 3 more every week. To maintain or even shorten total daily time of workout each movement is weekly speeded up. The devoted time every morning (or at least five days a week) to train all the major muscles of the body can remain under 10 minutes. Because there are no breaks during and between sets, the final push-ups become very challenging: at the end of the daily workout heart rate, depth and number of ventilations and frontal perspiration increase for a few minutes. We here provide an example of how to implement the progression of the Full-Body In-Bed Gym presenting an educational Case Report of a trained 80-year old person in stable pharmacological managements. In addition to strengthening the main muscles, including the ventilatory muscles, Although performed in bed, Full-Body In-Bed Gym is a resistance training equivalent to a short jog.. Started in early winter and continued regularly throughout spring and summer, Full-Body In-Bed Gym can help maintain independence of frail people, including those younger persons suffering with the fatigue syndrome related to the viral infection of the recent COVID-19 pandemic.
Key Words: skeletal muscle weakness, borderline mobility disorders, full-body in-bed gym
Ethical Publication Statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
There are about 700 skeletal muscles in the human body, including roughly 200 that are serious bone-movers and another 100 little muscles of hands, feet, head and face. The aim of this report is to convince persons-in-need, and their practitioners, to counteract age- or rest-muscle decay, maintaining at their best function, strength, fatigue resistance and shape of the main body muscles.1 Geriatric subjects, due to advanced age and/or associated diseases, spend only short time for daily physical activity. The consequent disuse muscle atrophy contributes to limit their independence, ultimately enforcing them to bed and to hospitalization for longer periods. Low mobility-related muscle atrophy is associated with neuromuscular weakness, functional limitations, thromboembolism, and high costs.2-4 All progressive muscle contractile impairments need permanent management. Besides eventual pharmacological treatment, a home-based physical exercise approach is helpful in counteracting muscle atrophy. Awaiting development of implantable devices for muscle stimulation, as effective as pacemakers for cardiac arrhythmias,5 implantable stimulators for ventilatory supports,6,7 or cochlear implants for hearing loss,8,9 education of sedentary patients to perform home physical exercises could be an effective low-cost alternative during and after hospitalization.10-13
Fig. 1.

From left to right the Panels 1, 2 and 3 show the 14 exercises that are a routine that could be a seasonal warm up also for active persons, i. e, those able to make at least 10 consecutive push-ups (Panel 3, Exercise 15). The cardiovascular responses to a challenging series of trainings are exemplified in Panel 4: Arterial pressure and cardiac frequency before and after 10 minutes of Full-Body in-Bed Gym (20 repetitions of each exercise, including push-up) during seven consecutive days (November 8 to 14, 2016). Mean +/- SD. After a self-challenging routine, cardiac and ventilatory frequency increased together with the maximal, but not the minimal arterial pressure. Indeed, the latter is more related to peripheral blood resistance. If the series of exercise reach the level of fatigue threshold, the workout induces an increase of blood perfusion of all the body skeletal muscles.13
Cardiovascular and respiratory physical rehabilitation protocols of surgical patients are well established approaches, whose main goal is to reverse muscle weakness/atrophy.14,15 We extended those routines to a daily short (10–20 min) sequence of easy-to-learn, safe and tool-free volitional physical exercises to be performed in bed (Full-Body in-Bed Gym) to improve muscles and, hence, mobility of impaired persons.
Materials and Methods
In untrained persons the series could start from 3-5 repetitions of each of 15 free-body physical exercises: 1. closing of hands; 2. extend and flex ankles; 3. extend arms and close hands; 4. Cyclic movements of the legs in a lying position in bed; 5. Deep inspirations aided by arm movements; 6. Lying in bed flex the chest; 7. Sitting in bed, left and right torsion of the neck and head; 8. Sitting on the bed, raise the body on the hands; 9. In a sitting position on the bed extend and flex the spinal cord; 10. In a sitting position stretch your legs; 11. In sitting position rotate the head; 12. Stretch and rotate your arms above your head; 13. Get out of bed, even on tiptoe to load the body weight on the soleus muscle; 14. (only after a few weeks of bed training) push-ups on the floor; 15. one final stand-up from the floor. The suggested workout can be seen in panels 1, 2 and 3 of Figure 1 (redrawn from figures of an earlier EJTM typescript).13
The following educational case report will detail the yearly progression of the Full-Body In-Bed Gym program. This workout could be a seasonal warm up, specifically after a long winter to recover fitness for demanding physical activities also for active persons, i. e., those able to make at least 10 consecutive push-ups. After advice of his/her family physician to avoid the very low risks of exercise pain and eventual muscle and joint damage, any sedentary people may start with five repetitions of each exercise. After one-two weeks of training, they may add groups of five additional repetitions, up to 30, every additional week. If compliant, even older olds will progressively increase their muscle strength if they reach and continue to perform 15 or 20 daily repetitions of the 14 exercises.
It is prudent to start performing the exercises at slow speed, but when the maximum number of each exercise is reached (15 or 20 repetitions), improving effects will be obtained by speeding up each exercise and thus increasing volume and intensity of the workout and maintime decreasing its time. The daily routine may last from 10 min (in the beginning) to 30 min (for complete sessions in accustomed persons). Alongside the panels in Figure 1, a video dynamically depicts the Full-Body in-Bed Gym sessions, both at low and higher speeds (Link to: https://youtu.be/pcHKmxCLYFs).16
If sedentary persons with rest-related muscle weakness, but without major comorbidities, challenge themselves avoiding much stress in a few weeks of Full-Body in-Bed Gym they may increase their muscle strength, fatigue resistance and independence in daily life activities.
In particular, cautious Full-Body in-Bed Gym may help patients to recover earlier after hospitalization, decreasing the risk of thromboembolism after surgical interventions, and concurring to reduce eventually present arterial hypertension. 17-19 In fact, after a series of exercises that challenge personal fitness, i. e., which induce sweating of the forehead and an increase in the cardio-respiratory frequency, the maximum blood pressure, but not the minimum, increases to then return in a few minutes to the pre-exercise values. An example of those behaviors of the cardiovascular system to demanding exercises is presented in panel 4 of Figure 1. This is strong evidence that peripheral arterial resistance is decreased during the demanding exercises because blood perfusion is increased by relaxation of the perforating arteries of the main skeletal muscles of the body, i. e., for functional hyperemia of the main muscles of the body.13
Fig. 2.
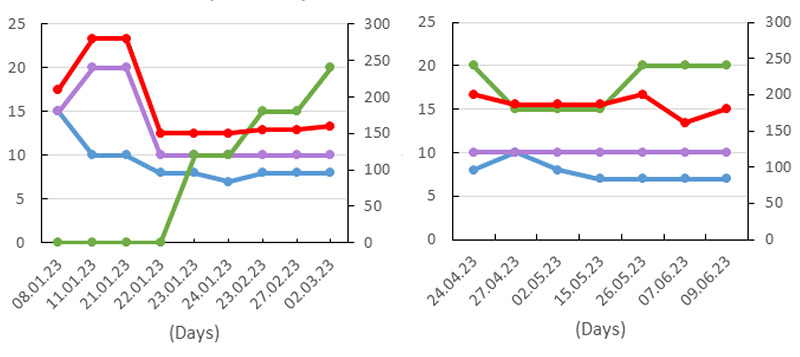
Left abscissa: Minutes or Number of repetitions of each of the 14 exercises or Number of repetitions of push-ups; right abscissa: Total muscle events per day.
Results and Discussion
An educational Case Report
We here provide an example of how to implement the progression of the Full-Body In-Bed Gym describing an educational Case Report of a well trained 80-year old person in stable pharmacological treatment for high arterial pressure, and anti-colesterol, vitamins and dietetic measures.
UC, born February 23, 1943, started in 2013 to do some voluntary exercise right after waking up. Year after year he has come to realize that many of the traditional bodyweight exercises can be done in bed. Then during his hospitalizations for cardiovascular complications and an acute intestinal blockage resolved by surgery, he realized that his workout could be continued in the hospital: Full-Body In-Bed Gym was born!
For the past 10 years he has been making notes about his in-bed-gym and its effects on his high blood pressure, concluding that it was worth circulating results among friends and eventually into the scientific arena. Although most of the colleagues were skeptical about the value of the naïve protocol and its eventual results, some publications came out and a first protocol was established.10-13 The state of the art of UC training is published below, along with the report on full-body-in-bed-gym progression performed in early 2023. The main finding from this year's experience is that less than 10 minutes of morning exercise is enough to look and feel five to ten years younger — a big improvement if you are in your 80s. It is fully accepted that age decline occurs between the ages of 40 and 80 at 1% per year:1,20-22 improving muscle strength by 10%, a goal achievable by Full-Body-in-Bed-Gym, is a 10-year rejuvenation, at least of major bone-mover muscles, if not of skin and joints.
Figure 2 shows the progression of the Full-Body In-Bed Gym from January to June 2023, the seventh year of a discontinuous Full-Body In-Bed Gym life style. Indeed UC was able to maintain his country house garden and the vegetable garden using heavy tools such as electric saws for pruning hedges or pickaxes for uprooting bamboo roots, which invariably invade the garden surrounding the areas dedicated to them. Figure 3 shows the pea production, Figure 4 a hedge bordering a garden path, while Figure 5 the pressing of the wine grapes harvested from the 50 wine trees that UC, often alone or with the help of his wife Annalisa, prunes, takes care of and harvests from February to the end of August in his country house in Trebaseleghe (Padua, Italy). The results of these farming activities are those that a very imprecise amateur can obtain, but who has a physical work capacity not too much inferior to that of a mature adult. Certainly not that of an octogenarian pensioner who limits himself to short walks every day to buy food. Naturally, this opens up the question of whether work capacity is linked to the in-bed-gym or to agricultural activities. A rational answer is that both are essential factors, but that the morning exercise period at the end of winter establishes the preconditions for exploiting and maintaining better fitness during spring and summer activities.
Fig 3.

Planting and weeding of flowering peas during spring 2021.
Fig 4.

Hedge maintenance during spring 2023.
After few months of discontinued In-Bed-Gym during the Autumn of 2022, the left panel of Figure 2 show that the new year work-out started January 8, 2023 with 15 repetition of the 14 In-Bed exercises for a total of 210 repetitions performed at slow speed in a total time of 15 minutes, but push-ups were not performed. Because during the following two weeks, despite increasing the number of repetitions to 20, the speed of movements were not increased, but their total number decreased to 140 (10 repetitions of the 14 In-Bed exercises) the total time of the workout decreased from 15 to 10 minutes. The day after the improved fitness allowed to perform ten push-ups at the end of the work-out that lasted less than 10 minutes. Having slightly further increased the speed of the 10 repetitions of the 14 physical exercises of the In-Bed-Gym the total time during the following months (February, March and April, see left panel of Figure 2) stayed regularly around 7 to 9 minutes, but included an increasing number of push-ups that steadily increased from 10 in late January up to 20 for a total number of around 200 repetitions, a non-trivial performance for a 80-year old man.
Discussion
That behavior is in line with the general expectation, but it must be stressed that it was achieved with less than 10 minutes per day of the in-bed special training. Increasing the speed of each movement, the time to devote every morning (or at least five days a week) to training of all the major muscles of the body can remain under 10 minutes.
To exercise attention and memory, it is recommended to sequentially count the number of daily repetitions, starting from 3 x 13 + 1 = 40 to reach 20 x 14 +1 = 281 exercises. Adding the post-workout 30-40 contractions of the diaphragm sustaining deep ventilation, a total of more than 200 strong sustained contractions of major muscle’s groups with agonists-antagonists co-contractions were performed. The last contraction modality is well known to substantially increase the anti-atrophy effects of even passive muscle contractions induced by electrical stimulation in experimental animals in the vivo and in vitro studies of Jarvis J. et al.23,24 and in functional electrical stimulation of permanent denervated muscles in human SCI cases.25-31
Since there are no breaks between sets of exercises, the final set of push-ups can become very challenging if continued until fatigue of the arms' muscles: at the end of the daily workout heart rate, depth and number of inhalations-exhalations and frontal perspiration increase, but only for a few minutes.
Furthermore, Full-Body in-Bed Gym routine mitigates the bad mood that is usually associated to mobility limitations,32,33 strengthening confidence of patient in recovering partial or total independence, and in reducing risks of accidental falls. Eventually, during hospitalizations the monitoring of the responses to challenging trainings could include oxygen saturation and many more fitness variables. Furthermore to speed-up positive changes, the trainings could be performed twice a day to improve fatigue resistance and cardio-respiratory reserve.34,35 Wearable devices are an emerging and cost-effective technology that allows to monitor several biometric data,36 and have been tested in many diseases.37 It might be interesting to add one of these devices (e.g. smartwatches, fitbands, smartphones, etc.) which could represent a guide for the patient during workout (heart rate monitoring and oxyhemoglobin saturation, reminder to perform exercises every day, stopwatch for timing workout.38
Fig 5.

Grape harvest and pressing (upper panel) and happy friends at work (lower panel).
In any case, during the initial learning period of Full-Body In-bed Gym, all seniors, if not hospitalized, must be supervised by at least one trainer, if not a health professional to avoid harmful exercise. These, in fact, are linked to their fitness and, nothing to say to comorbidities often present in elderly population. In young people these complications include the recent Chronic COVID-19 pandemic syndrome that is characterized by the psychological response to the global problem of COVID-19 pandemic, and often by muscle weakness that negatively influences the quality of life of persons for weeks or months before or after resolution of the infection.39-41 Certainly it changes in people the ordinary lifestyle for the forced lockdown measures imposed to control the epidemics.42,43 However, the most severe responses are expected later on after recovering COVID-19. In this case the pandemic syndrome is similar to post-traumatic stress disorders. The problem is that pandemic syndrome will affect the working capacity of population even when economic recovery will be possible and essential. Adequate prophylaxis and management of the syndrome in high-risk groups are important for maintaining global mental health and economy. Beside pharmacological support and psychotherapy in the acute phases, it will be mandatory to prevent and control the mild cases by general prophylactic measures and healthy lifestyle, i.e., by normalization of sleep-wake schedule, by controlling dietary intake of vitamins and microelements and by inducing moderate physical activity. All these measures are important to maintain a good physical condition that improves body adaptive potentials and the immune system. Altogether, our results demonstrate that volitional physical exercise improves the functional performance of skeletal muscles, including those essential for ventilation, a main problem in COVID-19 patients.
On the other hand, we have an ethical obligation to add that, if people, usually patients, are unwilling or unable to engage in voluntary physical activities, a very useful option is to offer them Functional Electrical Stimulation (FES), even in the worst cases of long-term peripheral denervation of skeletal muscles.10,11,25-29,31,44-48
In conclusion, it is never too early, and it is never too late to increase tool-free daily levels of volitional muscle contractions in aging and early-aging syndromes. Full-Body in-Bed Gym could help patients suffering with mild cases to prevent chronic COVID-19 syndrome and to counteract the decay of skeletal muscles, an inevitable consequence of normal aging as well. Here our contribution is to convince practitioners,49-55 and the population at large that Full-Body in-Bed Gym is an option to be taken seriously, despite being toll-free and requiring seemingly minimal efforts.10-13
Acknowledgments
A&C M-C Foundation for Translational Myology, Padova, Italy and PAGEpress, Scientific Publications, Pavia, Italy sponsored publication of this typescript.
List of acronyms
- COVID-19
Coronavirus disease 2019
- FES
functional electrical stimulation
- SCI
spinal cord injury
Funding Statement
Funding: The authors received no specific funding for this work.
Contributor Information
Barbara Ravara, Email: barbara.ravara@unipd.it.
Walter Giuriati, Email: walter.giuriati@unipd.it.
Maria Chiara Maccarone, Email: mariachiara.maccarone@phd.unipd.it.
Helmut Kern, Email: helmut@kern-reha.at.
Stefano Masiero, Email: stef.masiero@unipd.it.
References
- 1.Gava P, Kern H, Carraro U. Age-associated power decline from running, jumping, and throwing male masters world records. Exp Aging Res. 2015;41(2):115-35. doi: 10.1080/0361073X.2015.1001648. PMID: 25724012. [DOI] [PubMed] [Google Scholar]
- 2.Hopkins RO, Mitchell L, Thomsen GE, Schafer M, Link M, Brown SM. Implementing a Mobility Program to Minimize Post-Intensive Care Syndrome. AACN Adv Crit Care. 2016. Apr-Jun;27(2):187-203. doi: 10.4037/aacnacc2016244. PMID: 27153308. [DOI] [PubMed] [Google Scholar]
- 3.Camillo CA, Osadnik CR, van Remoortel H, Burtin C, Janssens W, Troosters T. Effect of "add-on" interventions on exercise training in individuals with COPD: a systematic review. ERJ Open Res. 2016. Mar 29;2(1):00078-2015. doi: 10.1183/23120541.00078-2015. PMID: 27730178; PMCID: PMC5005161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czyrny JJ, Kaplan RE, Wilding GE, Purdy CH, Hirsh J. Electrical foot stimulation: a potential new method of deep venous thrombosis prophylaxis. Vascular. 2010. Jan-Feb;18(1):20-7. doi: 10.2310/6670.2010.00001. Erratum in: Vascular. 2010. Mar-Apr;18(2): 121. PMID: 20122356. [DOI] [PubMed] [Google Scholar]
- 5.Saleem-Talib S, van Driel VJ, Chaldoupi SM, Nikolic T, van Wessel H, Borleffs CJW, Ramanna H. Leadless pacing: Going for the jugular. Pacing Clin Electrophysiol. 2019. Apr;42(4):395-399. doi: 10.1111/pace.13607. Epub 2019 Feb 25. PMID: 30653690; PMCID: PMC6850455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glenn WW, Hogan JF, Loke JS, Ciesielski TE, Phelps ML, Rowedder R. Ventilatory support by pacing of the conditioned diaphragm in quadriplegia. N Engl J Med. 1984. May 3;310(18):1150-5. doi: 10.1056/NEJM198405033101804. PMID: 6608692. [DOI] [PubMed] [Google Scholar]
- 7.Skalsky AJ, Lesser DJ, McDonald CM. Evaluation of phrenic nerve and diaphragm function with peripheral nerve stimulation and M-mode ultrasonography in potential pediatric phrenic nerve or diaphragm pacing candidates. Phys Med Rehabil Clin N Am. 2015. Feb;26(1):133-43. doi: 10.1016/j.pmr.2014.09.010. PMID: 25479785. [DOI] [PubMed] [Google Scholar]
- 8.Eskridge HR, Park LR, Brown KD. The impact of unilateral, simultaneous, or sequential cochlear implantation on pediatric language outcomes. Cochlear Implants Int. 2021. Jul;22(4):187-194. doi: 10.1080/14670100.2020.1871267. Epub 2021 Jan 12. PMID: 33430719 [DOI] [PubMed] [Google Scholar]
- 9.Gallo S, Trevisi P, Rigon C, Caserta E, Seif Ali D, Bovo R, Martini A, Cassina M. Auditory Outcome after Cochlear Implantation in Children with DFNB7/11 Caused by Pathogenic Variants in TMC1 Gene. Audiol Neurootol. 2021;26(3):157-163. doi: 10.1159/000510156. Epub 2020 Dec 22. PMID: 33352559. [DOI] [PubMed] [Google Scholar]
- 10.Carraro U, Gava K, Musumeci A, Baba A, Piccione F, Marcante A. Safe Antiaging Full-Body In-Bed Gym and FES for Lazy Persons: Home In-Bed Exercises for Fighting Muscle Weakness in Advanced Age. In: Rehabilitation Medicine for Elderly Patients, Masiero S, Carraro U, Eds., 2018; pag. 43-52. ISBN 978-3-319-57405-9 ISBN 978-3-319-57406-6 (eBook). doi 10.1007/978-3-319-57406-6. [Google Scholar]
- 11.Carraro U, Gava K, Baba A, Marcante A, Piccione F. To Contrast and Reverse Skeletal Muscle Atrophy by Full-Body In-Bed Gym, a Mandatory Lifestyle for Older Olds and Borderline Mobility-Impaired Persons. Adv Exp Med Biol. 2018;1088:549-560. doi: 10.1007/978-981-13-1435-3_25. PMID: 30390269. [DOI] [PubMed] [Google Scholar]
- 12.Carraro U, Marcante A, Ravara B, Albertin G, Maccarone MC, Piccione F, Kern H, Masiero S. Skeletal muscle weakness in older adults home-restricted due to COVID-19 pandemic: a role for full-body in-bed gym and functional electrical stimulation. Aging Clin Exp Res. 2021. Jul;33(7):2053-2059. doi: 10.1007/s40520-021-01885-0. Epub 2021 May 28. PMID: 34047931; PMCID: PMC8160559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carraro U, Albertin G, Martini A, Giuriati W, Guidolin D, Masiero S, Kern H, Hofer C, Marcante A, Ravara B. To contrast and reverse skeletal muscle weakness by Full-Body In-Bed Gym in chronic COVID-19 pandemic syndrome. Eur J Transl Myol. 2021. Mar 26;31(1):9641. doi: 10.4081/ejtm.2021.9641. PMID: 33709653; PMCID: PMC8056156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ades PA, Keteyian SJ, Wright JS, Hamm LF, Lui K, Newlin K, Shepard DS, Thomas RJ. Increasing Cardiac Rehabilitation Participation From 20% to 70%: A Road Map From the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017. Feb;92(2):234-242. doi: 10.1016/j.mayocp.2016.10.014. Epub 2016 Nov 15. PMID: 27855953; PMCID: PMC5292280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vorona S, Sabatini U, Al-Maqbali S, Bertoni M, Dres M, Bissett B, Van Haren F, Martin AD, Urrea C, Brace D, Parotto M, Herridge MS, Adhikari NKJ, Fan E, Melo LT, Reid WD, Brochard LJ, Ferguson ND, Goligher EC. Inspiratory Muscle Rehabilitation in Critically Ill Adults. A Systematic Review and Meta-Analysis. Ann Am Thorac Soc. 2018. Jun;15(6):735-744. doi: 10.1513/AnnalsATS.201712-961OC. PMID: 29584447; PMCID: PMC6137679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.EASY AGING in ITALY - the Myology way. Available at: https://youtu.be/pcHKmxCLYFs. [Google Scholar]
- 17.Börjesson M, Onerup A, Lundqvist S, Dahlöf B. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med. 2016. Mar;50(6):356-61. doi: 10.1136/bjsports-2015-095786. Epub 2016 Jan 19. PMID: 26787705. [DOI] [PubMed] [Google Scholar]
- 18.Seguro CS, Rebelo ACS, Silva AG, Santos MMAD, Cardoso JS, Apolinário V, Jardim PCV, Gentil P. Use of low volume, high effort resistance training to manage blood pressure in hypertensive patients inside a public hospital: a proof of concept study. Eur J Transl Myol. 2021. Mar 26;31(1):9547. doi: 10.4081/ejtm.2021.9547. PMID: 33709656; PMCID: PMC8056164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang W, Xu R, Cai Z, Zheng X, Zheng M, Ni C. Association between physical activity and resistant hypertension in treated hypertension patients: analysis of the national health and nutrition examination survey. BMC Cardiovasc Disord. 2023. Jun 7;23(1):289. doi: 10.1186/s12872-023-03303-x. PMID: 37286953; PMCID: PMC10249321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mosole S, Rossini K, Kern H, Löfler S, Fruhmann H, Vogelauer M, Burggraf S, Grim-Stieger M, Cvečka J, Hamar D, Sedliak M, Šarabon N, Pond A, Biral D, Carraro U, Zampieri S. Reinnervation of Vastus lateralis is increased significantly in seniors (70-years old) with a lifelong history of high-level exercise (2013, revisited here in 2022). Eur J Transl Myol. 2022. Feb 28;32(1):10420. doi: 10.4081/ejtm.2022.10420. PMID: 35234026; PMCID: PMC8992670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Narici M, McPhee J, Conte M, Franchi MV, Mitchell K, Tagliaferri S, Monti E, Marcolin G, Atherton PJ, Smith K, Phillips B, Lund J, Franceschi C, Maggio M, Butler-Browne GS. Age-related alterations in muscle architecture are a signature of sarcopenia: the ultrasound sarcopenia index. J Cachexia Sarcopenia Muscle. 2021. Aug;12(4):973-982. doi: 10.1002/jcsm.12720. Epub 2021 Jun 1. PMID: 34060717; PMCID: PMC8350200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perkisas S, Bastijns S, Baudry S, Bauer J, Beaudart C, Beckwée D, Cruz-Jentoft A, Gasowski J, Hobbelen H, Jager-Wittenaar H, Kasiukiewicz A, Landi F, Małek M, Marco E, Martone AM, de Miguel AM, Piotrowicz K, Sanchez E, Sanchez-Rodriguez D, Scafoglieri A, Vandewoude M, Verhoeven V, Wojszel ZB, De Cock AM. Application of ultrasound for muscle assessment in sarcopenia: 2020 SARCUS update. Eur Geriatr Med. 2021. Feb;12(1):45-59. doi: 10.1007/s41999-020-00433-9. Epub 2021 Jan 2. PMID: 33387359. [DOI] [PubMed] [Google Scholar]
- 23.Schmoll M, Unger E, Sutherland H, Haller M, Bijak M, Lanmüller H, Jarvis JC. SpillOver stimulation: A novel hypertrophy model using co-contraction of the plantar-flexors to load the tibial anterior muscle in rats. PLoS One. 2018. Nov 20;13(11):e0207886. doi: 10.1371/journal.pone.0207886. eCollection 2018. PMID: 30458051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turner DC, Gorski PP, Seaborne RA, Viggars M, Murphy M, Jarvis JC, Martin NRW, Stewart CE, Sharples AP. Mechanical loading of bioengineered skeletal muscle in vitro recapitulates gene expression signatures of resistance exercise in vivo. J Cell Physiol. 2021. Sep;236(9):6534-6547. doi: 10.1002/jcp.30328. Epub 2021 Feb 15. PMID: 33586196] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kern H, Carraro U, Adami N, Biral D, Hofer C, Forstner C, Mödlin M, Vogelauer M, Pond A, Boncompagni S, Paolini C, Mayr W, Protasi F, Zampieri S. Home-based functional electrical stimulation rescues permanently denervated muscles in paraplegic patients with complete lower motor neuron lesion. Neurorehabil Neural Repair. 2010. Oct;24(8):709-21. doi: 10.1177/1545968310366129. Epub 2010 May 11. PMID: 20460493. [DOI] [PubMed] [Google Scholar]
- 26.Carraro U, Kern H, Gava P, Hofer C, Loefler S, Gargiulo P, Mosole S, Zampieri S, Gobbo V, Ravara B, Piccione F, Marcante A, Baba A, Schils S, Pond A, Gava F. Biology of Muscle Atrophy and of its Recovery by FES in Aging and Mobility Impairments: Roots and By-Products. Eur J Transl Myol. 2015. Aug 25;25(4):221-30. doi: 10.4081/ejtm.2015.5272. PMID: 26913160; PMCID: PMC4748978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carraro U, Kern H, Gava P, Hofer C, Loefler S, Gargiulo P, Edmunds K, Árnadóttir ÍD, Zampieri S, Ravara B, Gava F, Nori A, Gobbo V, Masiero S, Marcante A, Baba A, Piccione F, Schils S, Pond A, Mosole S. Recovery from muscle weakness by exercise and FES: lessons from Masters, active or sedentary seniors and SCI patients. Aging Clin Exp Res. 2017. Aug;29(4):579-590. doi: 10.1007/s40520-016-0619-1. Epub 2016 Sep 3. PMID: 27592133. [DOI] [PubMed] [Google Scholar]
- 28.Kern H, Carraro U. Home-Based Functional Electrical Stimulation of Human Permanent Denervated Muscles: A Narrative Review on Diagnostics, Managements, Results and Byproducts Revisited 2020. Diagnostics (Basel). 2020. Jul 29;10(8):529. doi: 10.3390/diagnostics10080529. PMID: 32751308; PMCID: PMC7460102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carraro U, Edmunds KJ, Gargiulo P. 3D False Color Computed Tomography for Diagnosis and Follow-Up of Permanent Denervated Human Muscles Submitted to Home-Based Functional Electrical Stimulation. Eur J Transl Myol. 2015. Mar 17;25(2):5133. doi: 10.4081/ejtm.2015.5133. eCollection 2015 Mar 11. PMID: 26913154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edmunds K, Gíslason M, Sigurðsson S, Guðnason V, Harris T, Carraro U, Gargiulo P. Advanced quantitative methods in correlating sarcopenic muscle degeneration with lower extremity function biometrics and comorbidities. PLoS One. 2018. Mar 7;13(3):e0193241. doi: 10.1371/journal.pone .0193241. eCollection 2018. PMID: 29513690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gargiulo P, Kern H, Carraro U, Ingvarsson P, Knútsdóttir S, Gudmundsdóttir V, Yngvason S, Vatnsdal B, Helgason T. Quantitative color three-dimensional computer tomography imaging of human long-term denervated muscle. Neurol Res. 2010. Feb;32(1):13-9. doi: 10.1179/016164109X 12536042424171. PMID: 20092691. [DOI] [PubMed] [Google Scholar]
- 32.Carneiro LS, Fonseca AM, Vieira-Coelho MA, Mota MP, Vasconcelos-Raposo J. Effects of structured exercise and pharmacotherapy vs. pharmacotherapy for adults with depressive symptoms: A randomized clinical trial. J Psychiatr Res. 2015. Dec;71:48-55. doi: 10.1016/j.jpsychires.2015.09.007. Epub 2015 Sep 16. PMID: 26522871. [DOI] [PubMed] [Google Scholar]
- 33.Carneiro LS, Fonseca AM, Serrão P, Mota MP, Vasconcelos-Raposo J, Vieira-Coelho MA. Impact of physical exercise on catechol-O-methyltransferase activity in depressive patients: A preliminary communication. J Affect Disord. 2016. Mar 15;193:117-22. doi: 10.1016/j.jad.2015.12.035. Epub 2016 Jan 1. PMID: 26773917. [DOI] [PubMed] [Google Scholar]
- 34.Masiero S, Maccarone MC, Agostini F. Health resort medicine can be a suitable setting to recover disabilities in patients tested negative for COVID-19 discharged from hospital? A challenge for the future. Int J Biometeorol. 2020. Oct;64(10):1807-1809. doi: 10.1007/s00484-020-01947-4. Epub 2020 Jun 5. PMID: 32504142; PMCID: PMC7272594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35 Masiero S, Zampieri D, Del Felice A. The Place of Early Rehabilitation in Intensive Care Unit for COVID-19. Am J Phys Med Rehabil. 2020. Aug;99(8):677-678. doi: 10.1097/PHM.0000000000001478. PMID: 32467490; PMCID: PMC7299104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khoshmanesh F, Thurgood P, Pirogova E, Nahavandi S, Baratchi S. Wearable sensors: At the frontier of personalised health monitoring, smart prosthetics and assistive technologies. Biosens Bioelectron. 2021. Mar 15;176:112946. doi: 10.1016/j.bios.2020.112946. Epub 2020 Dec 30. PMID: 33412429. [DOI] [PubMed] [Google Scholar]
- 37.Gatsios D, Antonini A, Gentile G, Marcante A, Pellicano C, Macchiusi L, Assogna F, Spalletta G, Gage H, Touray M, Timotijevic L, Hodgkins C, Chondrogiorgi M, Rigas G, Fotiadis DI, Konitsiotis S. Feasibility and Utility of mHealth for the Remote Monitoring of Parkinson Disease: Ancillary Study of the PD_manager Randomized Controlled Trial. JMIR Mhealth Uhealth. 2020. Jun 29;8(6):e16414. doi: 10.2196/16414. PMID: 32442154; PMCID: PMC7367523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graña Possamai C, Ravaud P, Ghosn L, Tran VT. Use of wearable biometric monitoring devices to measure outcomes in randomized clinical trials: a methodological systematic review. BMC Med. 2020. Nov 6;18(1):310. doi: 10.1186/s12916-020-01773-w. PMID: 33153462; PMCID: PMC7646072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soloveva NV, Makarova EV, Kichuk IV. Coronavirus syndrome: COVID-19 psychotrauma. Eur J Transl Myol. 2021. Jan 14;30(4):9302. doi: 10.4081/ejtm.2020.9302. PMID: 33520144; PMCID: PMC7844407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khosravi M. COVID-19 quarantine: Two-way interaction between physical activity and mental health. Eur J Transl Myol. 2021. Jan 14;30(4):9509. doi: 10.4081/ejtm.2020.9509. PMID: 33520149; PMCID: PMC7844403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Angelini C, Siciliano G. Neuromuscular diseases and Covid-19: Advices from scientific societies and early observations in Italy. Eur J Transl Myol. 2020. Jun 22;30(2):9032. doi: 10.4081/ejtm.2019.9032. PMID: 32782765; PMCID: PMC7385692.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moro T, Paoli A. When COVID-19 affects muscle: effects of quarantine in older adults. Eur J Transl Myol. 2020. Jun 17;30(2):9069. doi: 10.4081/ejtm.2019.9069. PMID: 32782767; PMCID: PMC7385699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Hara Jennifer. Rehabilitation after COVID-19. Mayo Clinic News Network. 2020. October 3. Available: https://newsnetwork.mayoclinic.org/discussion/rehabilitation-after-covid-19/ [Google Scholar]
- 44.Bersch I, Fridén J. Electrical stimulation alters muscle morphological properties in denervated upper limb muscles. EBioMedicine. 2021. Dec;74:103737. doi: 10.1016/j.ebiom.2021.103737. Epub 2021 Dec 9. PMID: 34896792; PMCID: PMC8671101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dolbow DR, Gorgey AS, Johnston TE, Bersch I. Electrical Stimulation Exercise for People with Spinal Cord Injury: A Healthcare Provider Perspective. J Clin Med. 2023. Apr 27;12(9):3150. doi: 10.3390/jcm12093150. PMID: 37176591; PMCID: PMC10179213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arnold D, Thielker J, Klingner CM, Puls WC, Misikire W, Guntinas-Lichius O, Volk GF. Selective Surface Electrostimulation of the Denervated Zygomaticus Muscle. Diagnostics (Basel). 2021. Jan 28;11(2):188. doi: 10.3390/diagnostics11020188. PMID: 33525522; PMCID: PMC7912406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kurz A, Volk GF, Arnold D, Schneider-Stickler B, Mayr W, Guntinas-Lichius O. Selective Electrical Surface Stimulation to Support Functional Recovery in the Early Phase After Unilateral Acute Facial Nerve or Vocal Fold Paralysis. Front Neurol. 2022. Apr 4;13:869900. doi: 10.3389/fneur.2022.869900. PMID: 35444611; PMCID: PMC9013944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gorgey AS, Khalil RE, Alrubaye M, Gill R, Rivers J, Goetz LL, Cifu DX, Castillo T, Caruso D, Lavis TD, Lesnefsky EJ, Cardozo CC, Adler RA. Testosterone and long pulse width stimulation (TLPS) for denervated muscles after spinal cord injury: a study protocol of randomised clinical trial. BMJ Open. 2022. Oct 5;12(10):e064748. doi: 10.1136/bmjopen-2022-064748. PMID: 36198461; PMCID: PMC9535184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fiorenzato E, Zabberoni S, Costa A, Cona G. Cognitive and mental health changes and their vulnerability factors related to COVID-19 lockdown in Italy. PLoS One. 2021. Jan 27;16(1):e0246204. doi: 10.1371/journal.pone.0246204. PMID: 33503055; PMCID: PMC7840042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Demeco A, Marotta N, Barletta M, Pino I, Marinaro C, Petraroli A, Moggio L, Ammendolia A. Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res. 2020. Aug;48(8):300060520948382. doi: 10.1177/0300060520948382. PMID: 32840156; PMCID: PMC7450453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang TJ, Chau B, Lui M, Lam GT, Lin N, Humbert S. Physical Medicine and Rehabilitation and Pulmonary Rehabilitation for COVID-19. Am J Phys Med Rehabil. 2020. Sep;99(9):769-774. doi: 10.1097/PHM.0000000000001505. PMID: 32541352; PMCID: PMC7315835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Smith JM, Lee AC, Zeleznik H, Coffey Scott JP, Fatima A, Needham DM, Ohtake PJ. Home and Community-Based Physical Therapist Management of Adults With Post-Intensive Care Syndrome. Phys Ther. 2020. Jul 19;100(7):1062-1073. doi: 10.1093/ptj/pzaa059. PMID: 32280993; PMCID: PMC7188154.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lan CC, Hsieh PC, Yang MC, Su WL, Wu CW, Huang HY, Wu YK. Early pulmonary rehabilitation of COVID-19 patients in an isolation ward and intensive care unit. Tzu Chi Med J. 2022. Nov 2;35(2):137-142. doi: 10.4103/tcmj.tcmj_136_22. PMID: 37261306; PMCID: PMC10227681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Miner D, Smith K, Foroozesh M, Price JH. Implementation of Early Rehabilitation in Severe COVID-19 Respiratory Failure: A Scoping Review. J Acute Care Phys Ther. 2023. Apr;14(2):63-77. doi: 10.1097/JAT.0000000000000204. Epub 2022 Sep 27. PMID: 36968180; PMCID: PMC10032217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marrero HDJG, Stålberg EV, Cooray G, Corpeno Kalamgi R, Hedström Y, Bellander BM, Nennesmo I, Larsson L. Neurogenic vs. Myogenic Origin of Acquired Muscle Paralysis in Intensive Care Unit (ICU) Patients: Evaluation of Different Diagnostic Methods. Diagnostics (Basel). 2020. Nov 18;10(11):966. doi: 10.3390/diagnostics10110966. [DOI] [PMC free article] [PubMed] [Google Scholar]


