Abstract
High-grade neuroendocrine neoplasms are a rare disease entity and account for approximately 10% of all neuroendocrine neoplasms. Because of their rarity, there is an overall lack of prospectively collected data available to advise practitioners as to how best to manage these patients. As a result, best practices are largely based on expert opinion. Recently, a distinction was made between well-differentiated high-grade (G3) neuroendocrine tumors and poorly differentiated neuroendocrine carcinomas, and with this, pathologic details, appropriate imaging practices and treatment have become more complex. In an effort to provide practitioners with the best guidance for the management of patients with high-grade neuroendocrine neoplasms of the gastrointestinal tract, pancreas, and gynecologic system, the North American Neuroendocrine Tumor Society convened a panel of experts to develop a set of recommendations and a treatment algorithm that may be used by practitioners for the care of these patients. Here, we provide consensus recommendations from the panel on pathology, imaging practices, management of localized disease, management of metastatic disease and surveillance and draw key distinctions as to the approach that should be utilized in patients with well-differentiated G3 neuroendocrine tumors vs poorly differentiated neuroendocrine carcinomas.
Keywords: neuroendocrine tumors, neuroendocrine carcinoma, recommendations, high-grade
Introduction
High-grade neuroendocrine neoplasms (NENs) constitute a rare disease entity and account for approximately 10% of all NENs. Given their rarity, there is a paucity of prospective data to guide the optimal diagnosis and management of these patients. In recent years, updates to the pathologic classification of high-grade NENs have made this additionally complex with high-grade NENs now being subcategorized based on tumor differentiation. These subcategories include well-differentiated high-grade neuroendocrine tumors (G3 NET) and poorly differentiated high-grade neuroendocrine carcinomas (NECs). Most available literature does not account for this subcategorization and as a result, much of the management of high-grade NENs is based on expert opinion. Extra-pulmonary G3 NETs most commonly arise within the pancreas, followed by the small bowel. NECs most commonly arise within the lower gastrointestinal tract (colon and rectum), upper gastrointestinal tract (stomach and esophagus), and pancreas (Liu et al. 2021). Other commonly reported NEC sites of origin are in the genitourinary tract and the female pelvic organs but up to one-third of NECs are of the unknown primary site (Dasari et al. 2018). The prognosis of patients with metastatic G3 NET is fair, averaging around 42 months (Liu et al. 2021). Unfortunately, NEC has a much poorer prognosis with the median overall survival (OS) being less than a year, particularly for primaries arising from sites other than the small bowel and appendix (Dasari et al. 2017, 2018, 2022). In an effort to provide guidance on best treatment practices, we now put forth these consensus practice recommendations from the North American Neuroendocrine Tumor Society (NANETS) for the management of high-grade NENs of gastroenteropancreatic and gynecologic origin.
Methods for developing consensus practice recommendations
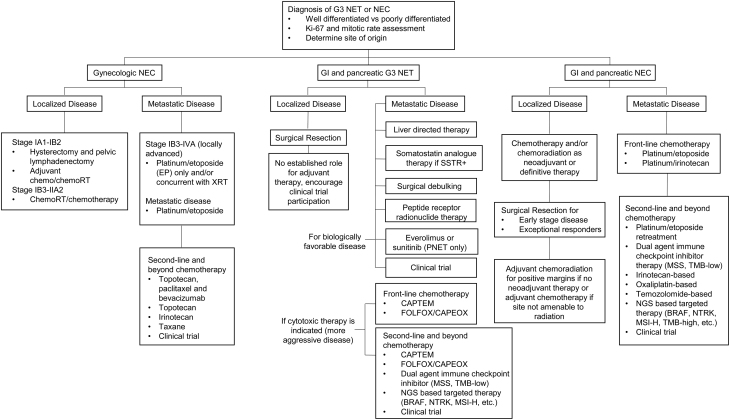
A panel consisting of 17 neuroendocrine experts from 13 institutions was convened by the NANETS Publications and Guidelines Committee. This panel consisted of nine medical oncologists, two radiation oncologists, two nuclear medicine physicians, one of whom is also an interventional radiologist, two surgeons, one gynecologic oncologist, and one pathologist. A subgroup of the panelists identified key topics for inclusion in these recommendations, all of which were vetted by the whole panel. Topics were assigned to appropriate panel members to conduct an extensive literature search and a face-to-face consensus meeting was held from October 2nd to 3rd, 2019, to discuss those findings. Surveys were conducted to ascertain consensus vs majority vs lack of consensus on multiple topics, generally where data was less clear. Panelists were permitted to abstain from voting on a particular topic if they did not feel they held the appropriate expertise. Consensus was defined as no more than one individual disagreeing with the rest of the voting group, majority as at least 75% of voting participants agreeing on a topic and lack of consensus as less than 75% of voting participants agreeing on a topic. Additional data to supplement the initial literature search were identified during the course of manuscript writing into 2022. Detailed recommendations are outlined later and are summarized in Fig. 1. All panelists contributed to the writing of these recommendations.
Figure 1.
Management of high-grade neuroendocrine neoplasms.
Initial assessment
Pathology
Definition and WHO criteria
High-grade NENs include G3 NET and NEC. The World Health Organization Classification of Tumours series of organ-system-based ‘Blue Books’ represents the gold standard for tumor classification. The diagnostic entity of G3 NET was first recognized in the pancreas and codified in the 2017 Endocrine Tumours Blue Book and then extended to encompass all gastroenteropancreatic sites in the 2019 Digestive Tumours Blue Book (World Health Organization 2019). G3 NETs are well-differentiated while NECs are poorly differentiated and include small-cell and large-cell variants. The former diagnosis is made predominantly based on morphology, while the latter formally requires the demonstration of general neuroendocrine marker expression to distinguish it from morphologic mimics. Diagnostic criteria for G3 NENs require a Ki-67 proliferation index > 20% and/or mitotic count > 20 per 2 mm2 though the vast majority of NECs well exceed these thresholds (Travis et al. 2015, Rinde et al. 2022).
Histology
Small-cell NEC is usually readily recognizable on hematoxylin-and-eosin stained slides, characterized by a high nucleus:cytoplasmic ratio, typically fusiform nuclei, finely granular chromatin, and frequent necrosis. Large-cell NEC often demonstrates organoid architecture (e.g. nested, trabecular); nuclei tend to be round with prominent nucleoli, and cytoplasm is fairly abundant; necrosis is, again, often prominent. NECs, particularly those of extra-pulmonary viscera, may arise in association with a non-NEC (in the digestive system, such tumors are referred to as mixed neuroendocrine-nonneuroendocrine neoplasm). G3 NET may demonstrate either typical well-differentiated histomorphology (including organoid architecture, low nucleus:cytoplasm ratio, finely granular chromatin) or show ambiguous histomorphology that is indeterminate for G3 NET vs large-cell NEC. Immunohistochemistry (IHC) is useful in these latter cases.
Immunohistochemistry
IHC is used to confirm a high-grade NEN’s neuroendocrine epithelial nature, for grading purposes (i.e. Ki-67), and to determine the site of origin in metastases of unknown primary. NENs are nearly always positive for broad-spectrum low molecular weight or pankeratins (e.g. CAM5.2, AE1/AE3); antibodies to EMA and/or EpCAM can be used in rare negative cases. NETs are nearly always positive for synaptophysin, though several diagnostic mimics may also be positive. As such, chromogranin A is typically performed concurrently. In contrast, up to one-quarter of NECs are negative for all traditional general neuroendocrine markers. INSM1 has emerged as the most sensitive general neuroendocrine marker in this setting, expressed by up to 95% of NECs (Rooper et al. 2017).
Ki-67 IHC is mandatory for the grading of extra-pulmonary NET, and in the vast majority of cases, the diagnosis is made based on a proliferation index > 20%, rather than a mitotic count > 20 per 2 mm2. Ki-67 IHC may be useful in NEC, as it is predictive and prognostic. Studies have identified various Ki-67 cutpoints in regard to prognosis (Sorbye et al. 2013, Walter et al. 2017) but there is a lack of consensus as to if any specific Ki-67 cut point should be used as it generally does not affect the treatment approach. Though the Digestive Tumours Blue Book recommends evaluating the Ki-67 proliferation index in ‘hot-spots’ encompassing at least 500 cells, proliferation indices in NEC are typically uniformly very high. In contrast, in many G3 NETs, foci of high proliferation are more limited in extent. Although the median proliferation index in NEC (80% in one recent series) exceeds that in G3 NET (50% in the same series), the ranges are overlapping such that Ki-67 should not be used alone in the distinction of these two tumor types (Tang et al. 2016a ). Additional useful markers in this diagnostic setting include p53 (missense-mutation and null-pattern staining support a diagnosis of NEC), Rb (loss of staining supports a diagnosis of NEC), SSTR2A (diffuse, strong staining favors a diagnosis of NET, though up to one-third of NECs demonstrate strong staining), and CXCR4 (diffuse, strong staining favors a diagnosis of NEC, though this marker is not widely available).
Site of origin assignment in metastatic NEC of the unknown primary has historically been only of academic interest, as platinum and etoposide are standard therapy for distant disease independent of the primary site. With first-line immunotherapy having emerged as the standard of care in advanced Merkel cell carcinoma and with extra-pulmonary visceral NECs being increasingly treated with organ-specific regimens typically used in non-NECs, site of origin assignment is increasingly important. Despite this, extensive IHC testing to identify the primary site of origin is not performed by most pathologists. Transcription factor IHC can facilitate NET site of origin assignment, with most occult primaries arising in the midgut (CDX2) or pancreas (islet 1, PAX6 or polyclonal PAX8, PR), and fewer cases arising in the lung (OTP, TTF-1) or rectum (SATB2).
G3 NET vs NEC – molecular considerations
While G3 NET and NEC are often readily distinguished by morphology, the diagnosis may be challenging, especially in small biopsies. The presence of a lower grade (i.e. G1/2) NET component confirms the diagnosis of G3 NET, while a concurrent non-NEC component strongly supports a diagnosis of NEC. NEC outnumbers G3 NET on the order of 90:1 (Bellizzi 2020a ). The molecular genetic hallmark of small-cell lung cancer is biallelic inactivation of the TP53 and RB1 tumor suppressors (George et al. 2015). This is also the case in many large-cell NECs and extra-pulmonary visceral NECs, but mutations are less frequent than in small-cell lung cancer (Sorbye et al. 2014, Bergsland et al. 2016, George et al. 2018) and vary considerably depending on the site of origin (Uccella et al. 2021, Venizelos et al. 2021, Metovic et al. 2022, Yachida et al. 2022). The IHC distinction of NEC from G3 NET largely relies on protein correlates of these molecular genetic events, with mutant-pattern p53 staining (either missense mutation- or null-pattern) and/or Rb loss being supportive of but not diagnostic for the diagnosis of NEC (Basturk et al. 2015, Konukiewitz et al. 2017, Bellizzi 2020b ). Molecular pathology is also used to identify clinically actionable events (e.g. mismatch repair (MMR) deficiency/microsatellite instability, pan-TRK overexpression/NTRK fusion).
Biopsy of primary vs metastatic site
The purpose of the biopsy in high-grade NENs is to secure the diagnosis, assess the proliferation index (especially in G3 NET), assign site of origin if possible (in metastases of unknown primary), and identify clinically actionable molecular genetic events. Biopsy of either primary or metastatic tumor should achieve these goals and there was consensus that a biopsy of both the primary and a metastasis is not necessary. As systemic and biologic therapies are directed at metastatic disease, this is theoretically the optimal tissue to target, though most oncogenic drivers are stable in matched primary-metastatic pairs (Brannon et al. 2014). In general, there is no reason to re-biopsy NEC on disease progression as this does not generally change management (majority). It is reasonable to re-biopsy G3 NET patients, particularly if there is an escalation in the pace of the disease or if one lesion seems to be growing faster than others and the majority of the group agreed with this approach as it may impact treatment selection. It is very unusual for G3 NET to transform to NEC although there is consensus that this would certainly change how a patient would be managed.
Summary of recommendations
High-grade NENs include both G3 NET and NEC and Ki-67 IHC is indispensable to NET grading and is prognostic and predictive in NEC. Mutant-pattern p53 staining and/or Rb loss generally support a diagnosis of NEC over G3 NET. Biopsy of either primary or metastatic tumor is sufficient for diagnosis and biomarker testing.
Imaging
Anatomical imaging
Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) all have well-established roles for imaging NENs with CT, particularly multiphase CT, being the cornerstone of neuroendocrine imaging. This modality is well suited for the identification of the primary tumor, staging, and for response assessments (van Essen et al. 2014), but multiple studies have also shown that key characteristics can be used to differentiate high-grade lesions from their low or intermediate counterparts. Among characteristics associated with G3 lesions are larger size, ill-defined features, portal and arterial enhancement and textural analysis to name a few (Feng et al. 2014, Utsumi et al. 2015, Zamboni et al. 2017, Canellas et al. 2018, Guo et al. 2019). For pancreatic primaries, larger tumor size and main pancreatic duct obstruction are associated with G2/G3 tumors (Fujimori et al. 2016). Multiphase MRI is an acceptable alternative with advantages including the lack of ionizing radiation and better soft-tissue contrast than CT. As with CT, a variety of MRI features have been shown to differentiate grade, including the apparent diffusion coefficient and diffusion-weighted imaging (Lotfalizadeh et al. 2017, Kulai et al. 2018, Mebis et al. 2020).
Functional imaging
Functional (nuclear) imaging is essential for NENs as an adjunct to anatomical imaging. The options include 111In-pentetreotide, 68Ga-DOTATATE, 68Ga-DOTATOC, 64Cu-DOTATATE, and 18F-fluorodeoxyglucose (FDG). The first four are somatostatin analogs (SSAs) showing the somatostatin-receptor (SSTR) expression levels in tumors, while 18F-FDG is a glucose analog showing the glucose transporter levels in tumors (Hicks 2010, Hofman & Hicks 2012, Toumpanakis et al. 2014). Throughout the remainder of this article, these will generically be referred to as SSTR imaging and FDG imaging. Importantly, DOTATATE/DOTATOC positron emission tomography (PET) is superior to pentetreotide gamma imaging in several significant respects including resolution, radiation dose and imaging time. As such, wherever available, DOTATATE PET is the current agent of choice for SSTR imaging.
The added value of SSTR imaging over anatomical imaging includes identification of the primary when not already known, identification of additional lesions without clear anatomical correlates, and evaluation of SSTR expression which is important for therapeutic decision-making, especially for SSTR-directed therapy. SSTR expression is inversely correlated with tumor grade with SSTR expression being seen mainly in G3 NETs and sometimes with NEC (Kaemmerer et al. 2011, Majala et al. 2019). In 40.9% of patients, the treatment plan is changed after the scans, owing mainly to new, unexpected findings (Skoura et al. 2016). There was consensus among panelists that SSTR imaging should be obtained at baseline for all patients with a G3 NET as this will be required if 177Lu-DOTATATE is being considered as a treatment option (Sorbye et al. 2020). Conversely, the role of SSTR imaging for NEC is not clearly supported and there was consensus that baseline SSTR imaging should not be obtained for patients with a newly diagnosed NEC.
In contrast, the level of glucose transporters (FDG uptake) is directly correlated with tumor grade. Several studies have shown that the degree of FDG uptake can be used to differentiate G1/G2 from G3 tumors and that the degree of uptake is strongly correlated with prognosis (Panagiotidis & Bomanji 2014, Tomimaru et al. 2015, Majala et al. 2019). It should be the functional imaging of choice for NECs, and for NETs of all grades when SSTR expression is low or not present but there was lack of consensus that an 18F-FDG PET should be obtained at baseline for either patient with an NEC or a G3 NET.
The inverse correlation between SSTR imaging and FDG imaging across tumor grade suggests they provide complementary information with regard to sensitivity, tumor grade and aggressiveness (especially important for those with potentially heterogeneous disease), and for prognosis (Kayani et al. 2008, Partelli et al. 2014, Kubota & Okasaki 2014, Zhang et al. 2018). This is especially applicable to the G3 NETs given their inherent heterogeneity (Panagiotidis et al. 2017). There was a lack of consensus on whether discrepant findings between SSTR- and FDG-PET imaging would warrant additional biopsies as the more aggressive element of disease should be prioritized in determining treatment strategy.
CNS imaging
The incidence of brain metastases in extra-pulmonary high-grade NENs is less than 2% (Alese et al. 2019, Fottner et al. 2019). As such, routine brain imaging is not indicated for asymptomatic patients with NEC or in those with a low volume of systemic disease (consensus) (Alese et al. 2019, Fottner et al. 2019). Patients with a high burden of systemic disease may be at higher risk for developing brain metastases (Hlatky et al. 2004, Akimoto et al. 2016). For patients with a G3 NET, the majority of the panel felt that baseline CNS imaging was not indicated but there was a lack of consensus as to the role of baseline CNS imaging in all patients with a NEC.
Summary of recommendations
Anatomical imaging with CT/MRI (often multi-phase) is the mainstay of imaging across all grades of NEN and all patients with a G3 NET or NEC should have some form of anatomical imaging at the time of diagnosis. Functional imaging with SSTR- and/or FDG-PET are important adjuncts. SSTR-PET should be obtained for all patients with G3 NET, particularly for patients with metastatic disease, as there are associated treatment implications. FDG-PET is indicated if there is a lack of clarity between G3 NET and NEC and in cases where the tumor appears disproportionately aggressive. CNS imaging is indicated in symptomatic patients and may be considered in patients with high disease burden.
Biomarkers and molecular characteristics
Biomarker levels, both hormonal and non-hormonal (chromogranin A) can be elevated in the presence of some G3 NENs although hormone-secreting G3 NENs are rare (Jensen et al. 2008, Metz & Jensen 2008, Reidy-Lagunes 2012, Castellano et al. 2015) No studies have demonstrated a clear correlation between levels of any biomarker and clinical and/or radiographic response to therapy. There was a lack of consensus that evaluation of biomarkers should be conducted during the initial assessment of patients with a G3 NET aside from patients with a clinical syndrome. For patients with a clinical hormonal syndrome, there was consensus that hormone levels tailored to the patient’s symptoms should be checked at diagnosis and throughout their treatment course. There was also consensusthat monitoring of biomarkers during treatment of patients with non-functional tumors would not change management, should not be used in isolation for treatment decision-making and that there is no role for biomarker evaluation at the time of diagnosis for NEC.
G3 NET and NECs are characterized by distinct molecular profiles, reflective of differing mechanisms of pathogenesis; however, our understanding of the treatment implications of these distinct mutational spectrums remains limited. Multiple sequencing efforts (whole-exome, whole-genome, next-generation) have identified an increased number of somatic mutations in the cell cycle regulator CDKN1B, chromatin remodeling genes (MEN1, DAXX, ATRX, ARID1A), DNA repair genes, and mammalian target of rapamycin (mTOR) pathway genes in well-differentiated NETs (Jiao et al. 2011, Scarpa et al. 2017, Raj et al. 2018). In regard to DAXX and ATRX specifically, although there are some conflicting data (Jiao et al. 2011, Raj et al. 2018), one of these genes appears to be more commonly mutated in G2 or G3 NET (70%) as compared to G1 NET (30%) (Singhi et al. 2017), and presence of a DAXX or ATRX mutation is associated with a significantly decreased disease-free survival (HR 4.69, P < 0.001). Another study similarly showed a poorer prognosis with an ATRX mutation (HR 16.982, P = 0.012) (Chou et al. 2018). G3 NET specimens are represented in very low numbers and are included in only a few of these studies, making this an area in need of further exploration.
Sequencing efforts in NEC have identified somatic alterations most commonly in TP53 and in retinoblastoma (Rb) pathway genes, (McNamara et al. 2020). Up to 50% of extra-pancreatic NECs have mutations in TP53 but RB1 mutations are somewhat less common (Bergsland et al. 2016, McNamara et al. 2020). Mutations in KRAS, TP53, BRAF (especially V600E), and APC are commonly seen in colorectal NECs (Puccini et al. 2020, Chen et al. 2021, Lee & Sung 2021). Some studies of NEC have also identified tumor microsatellite instability (Yachida et al. 2012, Tang et al. 2016b , Girardi et al. 2017).
Molecular characterization in NEC of gynecologic origin suggests yet still different features, particularly in cervical primaries. Positivity for human papillomavirus (HPV) is known to be present in 85.6% of these cancers. Akin to NEC of the gastroenteropancreatic system, Rb1 mutations are seen but in lower percentages and differ between HPV-positive and HPV-negative patients (4 and 32%, respectively). Mutations in PIK3CA (19.6%), MYC (15.5%), TP53 (15.5%), and PTEN (14.4%) are also seen, as are tumors with intermediate or high tumor mutational burden (18.6%), at times also showing DNA MMR deficiency (Eskander et al. 2020).
Despite an improved understanding of NET and NEC genetics, current data are not strong enough to use genomic profiles for standard of care treatment selection. Studies evaluating the use of the targeted therapy everolimus in the setting of mTOR pathway alterations have not identified a neuroendocrine subgroup more likely to respond (Zatelli et al. 2016). Further study is clearly needed but the availability of therapeutics that are disease agnostic make next-generation sequencing (NGS) and an evaluation for DNA MMR deficiency reasonable; approximately 10% of NEC demonstrate MMR deficiency (Girardi et al. 2017), 0.31% of NENs have NTRK fusions (Solomon et al. 2020), and it has been reported that at least 20% of NECs have some form of druggable molecular alternation (Garcia-Carbonero et al. 2023). Rare cases of RET fusions have also been reported (Subbiah et al. 2022).
Of note, the earlier NEN sequencing efforts have been conducted in tumor tissue specimens and work on circulating tumor specimens is limited and investigational. In the CIRCAN-NEC pilot study, circulating tumor DNA (ctDNA) was evaluated during the course of a patient’s therapy and in the context of their mutational status (BRAF, KRAS, RB, etc). This study included 24 patients but demonstrated early findings that ctDNA may potentially be helpful in predicting prognosis and could aid in selecting the best therapy (Gerard et al. 2021). Circulating tumor cells (CTCs) have been identified in NENs and CTC presence has been associated with increased tumor burden and higher tumor grade (Khan et al. 2013, Zatelli et al. 2017, Rizzo & Meyer 2018). While still investigational, given the CTC presence in some NENs, at some point, molecular testing of CTCs may provide an opportunity to non-invasively identify clinically actionable events in G3 NETs and NECs.
Summary of recommendations
Initial and subsequent biomarker assessments should only be conducted for patients with a hormone-mediated clinical syndrome and should not be used in isolation for diagnosis or monitoring of either G3 NET or NEC. There was consensus from the group that NGS and MMR testing should be routinely conducted for patients with an NEC as this may identify targets for disease-agnostic treatments, but there was lack of consensus in regard to its use for G3 NETs. Blood collection for ctDNA and CTCs remains investigational and should be encouraged in the context of clinical trials.
Studies to be done as part of initial assessment
Studies to be performed as part of the initial NEN evaluation have been provided by three other societies that have generated neuroendocrine guidelines. These include the National Comprehensive Cancer Network (NCCN) (Shah et al. 2021), the European Society of Medical Oncology (ESMO) (Pavel et al. 2020), and the European Neuroendocrine Tumor Society (ENETS) (Garcia-Carbonero et al. 2016, Sorbye et al. 2023). Based on these societal recommendations as well as the data presented earlier, we recommend the following be performed as part of the initial grade 3 NEN assessment (Table 1).
Table 1.
Recommended assessments for a newly diagnosed grade 3 neuroendocrine neoplasm.
| G3 NET | NEC | |
|---|---|---|
| Imaging | Multiphase, high-resolution CT or MRI with contrast | Multiphase, high-resolution CT or MRI with contrast |
| SSTR-PET imaging | MRI brain for high systemic burden and/or if symptomatic | |
| FDG-PET if indicated | FDG-PET if indicated | |
| SSTR-PET imaging if indicated | ||
| Laboratory (if metastatic disease present) | MSI/MMR testing may be considered | MSI/MMR testing (should not delay initiation of treatment) |
| Next-generation sequencing may be considered | Next-generation sequencing (should not delay initiation of treatment) | |
| Endoscopy | Endoscopic evaluation (EGD, colonoscopy) for known or suspected GI primaries |
Endoscopic evaluation (EGD, colonoscopy) if possible for known or suspected GI primaries – identification of primary should not delay treatment |
Management of localized disease
Gastrointestinal G3 neuroendocrine tumors (NET)
Surgical resection
Outcomes for patients undergoing surgery for the locoregional disease are confounded by a limited number of studies that combine G3 NET and NEC, combine disparate primary tumor sites, and include patients with locoregional and advanced disease (Haugvik et al. 2016, Tang et al. 2016b , Dasari et al. 2018, Yoshida et al. 2019, Pommergaard et al. 2021). Nevertheless, median survival exceeding 43–55 months has been reported for G3 NET patients, suggesting favorable biology (Crippa et al. 2016, Tang et al. 2016b , Yoshida et al. 2019) and there was consensus from the group that surgery may be appropriate for locoregional control and possibly cure. The goals of surgery for patients with localized G3 NET are an oncologic resection of the primary tumor and regional lymph nodes. Since most patients with G3 NENs have lymph node metastases, a thorough lymphadenectomy is necessary. For pancreatic primaries involving the pancreatic body and tail, a distal pancreatectomy with en-bloc splenectomy is the recommended surgical approach (Nakakura 2018).
Radiation therapy, chemotherapy, and chemoradiotherapy
There are limited data regarding definitive, neoadjuvant, or adjuvant radiation therapy in the management of G3 NEN. Optimal concurrent chemotherapy is unknown; commonly used regimens include fluoropyrimidine-based treatment or platinum and etoposide. This treatment may be delivered as a neoadjuvant treatment for patients planned to undergo surgery, which is favored over delivery in the adjuvant setting based on extrapolation from data describing improved toxicity and efficacy with gastrointestinal adenocarcinoma treatment (Spitz et al. 1997, Sauer et al. 2012, Wong et al. 2015). The majority of the group felt that there is no role for neoadjuvant radiation or chemoradiation for patients with G3 NETs but there was a lack of consensus as to its use in the adjuvant setting, regardless of margin status following surgery. For patients with pancreatic NETs with adverse postoperative features, there may be a local control benefit (Contessa et al. 2009, Arvold et al. 2012, Zagar et al. 2012). This is an area where further investigation is sorely needed.
There are no data regarding the use of adjuvant chemotherapy for patients with a resected G3 NET despite their high risk of recurrence. The SWOG 2104 trial is addressing the role of postoperative adjuvant temozolomide and capecitabine in patients with a resected well-differentiated G3 NET of the pancreas, specifically those with a Ki-67 of <55% (NCT05040360).
Gastrointestinal neuroendocrine carcinomas (NEC)
Role of surgery
Patients with NEC have an extremely poor prognosis with median survival in most cases of 13 months or less, even for patients with locoregional disease undergoing resection with curative intent (Smith & Reidy-Lagunes 2013, Basturk et al. 2014, Smith et al. 2014, Crippa et al. 2016, Fields et al. 2019, Yoshida et al. 2019, Ueberroth et al. 2021). Therefore, the role of surgery for G3 NEC is highly questionable. Although a preoperative diagnosis of a localized G3 NEC is rarely made, if indeed the diagnosis is known, the panel strongly recommends multidisciplinary evaluation and consideration of systemic therapy and possible definitive chemoradiation, particularly for surgeries with higher morbidity (esophageal, gastric, pancreatic, and rectal primaries) (Crippa et al. 2016, Deng et al. 2016). Both the ENETS and ESMO guidelines recommend surgery for patients with a localized NEC although both also indicate a role for chemotherapy and possibly radiation for some of these patients, particularly those with esophageal, anal, and some rectal primaries (Garcia-Carbonero et al. 2016, Pavel et al. 2020, Sorbye et al. 2023). An evaluation of the role of surgery in localized NEC in the United States carried out on data from the National Cancer Database (NCDB) suggests that for patients with stage I–II disease, surgery does confer a survival benefit and should be considered. This study, however, was conducted on data that did not adhere to current WHO criteria and Ki-67 data was not available to determine if these patients had G3 NET or NEC (Dasari et al. 2022). Another retrospective study of patients with localized poorly differentiated NEC showed a survival advantage for patients undergoing surgery but again, Ki-67 data were not available and it is unclear if patients were appropriately classified (Thornblade et al. 2021). Additional limited studies suggest definitive chemoradiation may yield favorable outcomes compared with surgery for esophageal and rectal primaries (Meng et al. 2013, Bertani et al. 2018, Dasari et al. 2022).
Radiation therapy, chemotherapy, and chemoradiotherapy
Distant progression is the most common site of failure for NEC, demonstrating the importance of systemic therapy. However, (chemo)radiation may provide durable local control for primary and metastatic disease (Chakravarthy & Abrams 1995). NECs have most commonly been treated with concurrent doublet platinum-based therapy (Meng et al. 2013) with four cycles (based on small-cell lung cancer data) (Faivre-Finn et al. 2017) or five to six cycles (based on gynecologic data) (Viswanathan et al. 2004) being the norm. When given alongside radiation, platinum and etoposide are the recommended radiosensitizing regimen (Yamashita et al. 2009, Meng et al. 2013, Katada et al. 2020). If the ability to deliver etoposide is hampered, carboplatin and paclitaxel is an acceptable alternative, based on small-cell lung cancer data (Groen et al. 1999). Several retrospective studies evaluating the benefits of adjuvant chemotherapy have yielded discordant results (Pellat et al. 2020, Mao et al. 2021, Schmitz et al. 2021). In the aforementioned NCDB study (Dasari et al. 2022) where surgery was recommended for very early disease, chemoradiation was found to likely be preferred over surgery for patients with primary tumors where a morbid surgery would be undertaken. Currently ongoing is the French NEONEC trial (NCT04268121) which is evaluating both neoadjuvant treatment with platinum and etoposide followed by surgery or chemoradiation as well as the role of adjuvant platinum and etoposide chemotherapy in patients with localized GI NEC. This prospectively collected data will be critical in guiding physicians as to how best to manage this unique patient population. It is the view of ENETS that adjuvant therapy following surgical resection of a localized NEC may be considered (Sorbye et al. 2023).
Summary of recommendations
There was an overall lack of consensus from the panel in regard to the role of surgery for NEC although it was more favorably viewed to pursue surgery following a course of systemic therapy and/or chemoradiation, particularly in exceptional responders or patients with very early disease. Following surgery or as definitive therapy, there was consensus that four to six cycles of platinum and etoposide with the inclusion of radiation at some point during the course of chemotherapy be considered and that capecitabine is an acceptable radiation sensitizer if consolidation chemoradiation is given following completion of four to six cycles of platinum and etoposide chemotherapy. There was a lack of consensusas to if chemoradiation should be used in the adjuvant setting for patients with a negative surgical margin although there was consensus that adjuvant chemoradiation is indicated following resection of a NEC with positive margins. There was consensus that patients with a resected NEC in a location not amenable to subsequent radiation should receive adjuvant chemotherapy.
Surveillance assessments for localized disease
Surveillance studies to be performed for patients who have been treated for a localized NEN have also been provided in the guidelines of the aforementioned societies (NCCN, ESMO, and ENETS) (Garcia-Carbonero et al. 2016, Pavel et al. 2020, Shah et al. 2021). Based on these societal recommendations and in line with the data presented earlier, the majority of the panel agreed that the following surveillance studies be performed for patients who have been treated for a localized grade 3 NEN (Table 2).
Table 2.
Surveillance assessments for patients treated for a localized grade 3 neuroendocrine neoplasm.
| G3 NET | NEC | |
|---|---|---|
| Imaging | Multiphase, high-resolution CT or MRI with contrast every 3 months for 2–3 years, then every 6–12 months for at least 10 years | Multiphase, high-resolution CT or MRI with contrast every 3 months for 3 years, then every 6 months for years 4–5 |
| SSTR-PET imaging as indicated | MRI brain as indicated based on symptoms | |
| FDG-PET imaging as indicated | FDG-PET as indicated | |
| SSTR-PET imaging as indicated | ||
| Biopsy | Biopsy as indicated to confirm recurrence and/or to re-establish grade | Biopsy as indicated to confirm recurrence |
Localized gynecologic G3 neuroendocrine carcinoma
When it comes to the gynecologic tract, the vast majority will be NEC as opposed to NETs. If a NET is found in the gynecologic tract, metastatic disease from a gastrointestinal primary should be ruled out. Small-cell carcinoma is more frequently seen than large-cell NEC. NECs of the cervix predominate, found in descending order of frequency by those arising in the uterus, vulvo/vagina, and ovary. Due to the extreme rarity of these cancers (<300/year in the United States), multi-modal treatment recommendations have evolved by combining strategies for small-cell carcinoma of the lung and squamous cell/adenocarcinoma of the cervix. Prospective clinical trials, however, have not been performed in patients with these cancers.
For patients with disease confined to the cervix and <4 cm in size (FIGO stage IA1–IB2), surgery remains the first line of treatment. Standard surgery includes a radical hysterectomy and either sentinel lymph node biopsies or complete pelvic lymphadenectomy. In one large study, patients with early stage disease who did not undergo surgery had a hazard ratio for death of 4.74 compared to those who underwent surgery (Ishikawa et al. 2018). In a SEER database review, patients with early stage disease who underwent surgery had an odds ratio for recurrence of 0.62 compared to those who do not undergo surgery (Cohen et al. 2010). Although patients with NEC of the cervix were not included in the LACC study, which showed that minimally invasive radical hysterectomy had significantly higher recurrences and cancer-related deaths than open surgery, we recommend an open surgery as opposed to a minimally invasive approach (Ramirez et al. 2018). Fertility-sparing surgeries such as cone biopsy or radical trachlectomy should not be performed (Plante et al. 2011).
Postoperative chemotherapy is an integral part of adjuvant therapy for patients with early stage NEC of the cervix. Patients with stage IA2–IB2 disease who recur will have a distant component (i.e. outside the pelvis) 86% of the time (Zivanovic et al. 2009). The most common site of first recurrence is the lung followed by the liver and then the peritoneum, which further argues for systemic therapy (Stecklein et al. 2016). The addition of chemotherapy to surgery significantly reduces the risk of extrapelvic recurrence (OR for recurrence 0.37) (Ishikawa et al. 2018). Cisplatin and etoposide are the most commonly used therapeutic agents for adjuvant chemotherapy in patients with NEC of the cervix. In one study, patients who received chemotherapy other than cisplatin and etoposide had a hazard ratio for recurrence of 3.42 (Pei et al. 2017). Those patients who did not get any adjuvant chemotherapy had a hazard ratio for recurrence of 5.4. Furthermore, patients who received ≥5 cycles of cisplatin and etoposide had an improved 5-year recurrence-free survival. By consensus, we, therefore, recommend six cycles of adjuvant cisplatin and etoposide for patients with early stage disease who undergo surgery as primary therapy.
The benefit of radiation in addition to chemotherapy and surgery is less clear. Pelvic radiation after surgery does reduce pelvic recurrence. Patients receiving postoperative pelvic radiation have a 13–16% chance of pelvic recurrence vs a 25–31% chance if no radiation is received (Chen et al. 2015, Ishikawa et al. 2018). However, although postoperative pelvic radiation reduces pelvic recurrences, no studies have shown that it improves survival. This may be because studies are inadequately powered to show such a difference due to small sample sizes or due to the high risk of distant recurrence (liver, lung), local control of the pelvis does not improve survival. As there are no definitive data showing a survival benefit for postoperative pelvic radiation, we recommend postoperative radiation in addition to chemotherapy as adjuvant therapy in patients with high-risk factors such as tumors >2 cm, deep stromal invasion and/or lymphovascular space invasion (consensus).
Guidelines from the Society of Gynecologic Oncology and the Gynecologic Cancer Intergroup allow for neoadjuvant chemotherapy and surgery for cervix confined lesions >4 cm in size (FIGO stage IB3) or tumors with extension onto the upper vagina (stage IIA2) (Gardner et al. 2011, Satoh et al. 2014); however, there does not appear to be sound rationale for this approach. First, this strategy is not utilized for small-cell carcinoma of the lung or for squamous or adenocarcinoma of the cervix. Second, the likelihood of metastatic disease with tumors >4 cm is high. Finally, radiation therapy provides good pelvic control with pelvic recurrences only 10–20% with chemoradiation therapy (Hoskins et al. 2003, Stecklein et al. 2016). Recurrence rates for patients undergoing this approach are quite high at 79% (Bermudez et al. 2001, Lee et al. 2008, Nasu et al. 2011, Dongol et al. 2014). For those reasons, by consensus, we recommend chemoradiation followed by chemotherapy and not surgery for patients with stage IB3–IIA2 disease.
Summary of recommendations
For patients with early stage NEC of the cervix (FIGO stage IA1–IB2), we recommend radical hysterectomy and sentinel lymph node biopsy or complete pelvic lymphadenectomy with postoperative adjuvant therapy inclusive of pelvic chemoradiation with cisplatin and etoposide (rwo cycles) followed by an additional four cycles of cisplatin and etoposide for a total of six cycles. Patients with stage IB3–IIA2 disease should be treated with platinum/etoposide chemoradiation (two to three cycles) followed by an additional three to four cycles of chemotherapy (to complete a total of six cycles of chemotherapy) but not surgery given the high risk of distant recurrence.
Treatment of metastatic G3 NET
To date, there is a paucity of prospective trials evaluating systemic therapy for G3 NETs and the majority of available studies are entirely retrospective in nature, small, and of low quality. Considerable controversies exist regarding the choice of systemic therapy in first-line therapy and beyond (Sonbol & Haldanarson 2019, Sorbye et al. 2019). There is substantial heterogeneity among the published studies in terms of the populations studied, the regimens used, and the methodology used for response assessment. Given the relatively recent recognition of G3 NETs as a subset of G3 NENs, many older studies do not adequately distinguish G3 NETs from NECs (for development of these recommendations, studies that did not analyze outcomes of the subset of patients with G3 NETs were excluded). Interpretation of these results is further limited due to G3 NETs constituting only a small proportion of the total study populations often without confirmatory expert pathological review prior to inclusion to firmly establish grade and differentiation. Common response criteria such as RECIST were uncommonly applied.
In the absence of higher-quality data, there was consensusamong the panel members that it would be appropriate to apply knowledge from G1 and G2 NETs to G3 NETs, particularly for those tumors exhibiting favorable tumor biology. The majority of the group felt that surgical debulking of patients with G3 NETs may also be appropriate.
Liver-directed therapy
The presence of liver metastases has been shown to negatively affect the quality of life and prognosis of patients with NETs (Janson et al. 1997, Yao et al. 2007, Frilling et al. 2010). Liver-directed therapies using thermal ablation and/or intra-arterial embolization are commonly used for non-surgical NET patients with the liver-dominant disease to improve survival and quality of life, especially in patients with hormonal syndromes (Touzios et al. 2005, Kennedy 2016, Al-Toubah et al. 2019). Current guidelines endorse hepatic arterial embolization for symptomatic or progressive hepatic metastases, without recommendations among the different embolotherapies (chemoembolization, radioembolization, or bland embolization) (Pavel et al. 2016, 2020, Strosberg et al. 2017). Despite the lack of completed randomized trials comparing these embolization modalities, they have shown good clinical, biochemical, and morphological responses when liver tumor burden is beyond ablative therapies (Zappa et al. 2012). The ongoing RETNET trial (Randomized Embolization Trial for Neuroendocrine Tumor Metastases to the Liver, NCT02724540) is comparing bland embolization to conventional chemoembolization in patients with well-differentiated tumors, including G3 NET, and will provide much needed prospective data in this space.
There is a paucity of data in regard to the role of liver-directed therapy in G3 NET (Del Prete et al. 2014, Coriat et al. 2016, Chen et al. 2017). In one larger multi-institutional series, the number of G3 NET patients reached only 20 (13% of evaluated patients) – chemoembolization (n = 12), radioembolization (n = 7), and bland embolization (n = 1) (Chen et al. 2017). Patients with G3 NET were found to have a worse prognosis with shorter survival after embolization than patients with G1/G2 tumors (Chen et al. 2017).
From an expert opinion point of view, liver-directed therapy for metastatic G3 NET is considered a valid therapy similar to G2 NET if Ki-67 is <55%. Clinical considerations should be taken into account including rate of progression, tumor proliferative activity, and the overall disease course of the patient. The technique used is left to the discretion of the treating physician. In G3 NET with Ki-67 >55%, and in patients with extrahepatic metastases, especially bone, a systemic treatment is preferred. There was consensus that the use of liver-directed therapy in G3 NET is warranted; however, the ideal type of embolotherapy remains unclear.
Somatostatin analog therapy
SSAs are routinely used for the control of hormone-mediated symptoms in low-grade NETs (Rubin et al. 1999, Fisher et al. 2018). Functional G3 NETs are relatively uncommon, but up to a quarter of patients demonstrate hormone-mediated symptoms (Sorbye et al. 2018). Very little data exist to guide our approach to the use of SSAs in SSTR-positive G3 NETs from either symptom control or cancer growth standpoint, but data suggest that up to 88% of tumors express SSTR by imaging (Sorbye et al. 2018). A few small series lend support for activity in G3 disease. In a study of 14 G3 NET patients (median Ki-67 25%) treated with SSA monotherapy, half of the patients experienced stable disease or better (McGarrah et al. 2020a ). The median PFS was 4.4 months. Three retrospective studies assessing the efficacy of SSA therapy in G3 NETs showed a median PFS of 4–8 months (Faggiano et al. 2016, de Mestier et al. 2021, Lithgow et al. 2021). None of the current NET guidelines addresses the use of SSAs for G3 NETs (Boudreaux et al. 2010, Pavel & de Herder 2017, Pavel et al. 2017).
Summary of recommendations
Extrapolating from well-differentiated G1/G2 NET, there was consensusfrom the panel that a trial of SSA therapy as the initial front-line therapy for tumor control in patients with a G3 NET with favorable biology is reasonable. The majority of the panel felt that this approach is only appropriate if the patient has positive SSTR imaging. Restricting the use of SSAs to SSTR-positive G3 NET with a relatively low Ki-67 makes the most sense, recognizing that the anticipated benefit is likely to be less durable than in G1/G2 NETs.
Front-line chemotherapy
All the studies reporting on first-line therapies for G3 NET were hampered by one or more of the limitations discussed earlier. The majority of front-line studies have evaluated cytotoxic chemotherapy, patients with a median Ki-67 ranging from 21 to 47% and the majority have assessed pancreatic NENs (Brixi-Benmansour et al. 2011, Ferrarotto et al. 2013, Hijioka et al. 2017, Jia et al. 2017, Girardi et al. 2017, Roquin et al. 2018, Apostolidis et al. 2018, Rogowski et al. 2019, Apostolidis et al. 2021, de Mestier et al. 2021, Lithgow et al. 2021, Liu et al. 2021). Platinum (cisplatin/carboplatin)-based regimens had response rates ranging from 0 to 38% with PFS ranging from 2.6 to 8.9 months (Velayoudom-Cephise et al. 2013, Heetfeld et al. 2015, Girardi et al. 2017, Hijioka et al. 2017, Jia et al. 2017, Li et al. 2017, Roquin et al. 2018, Apostolidis et al. 2021, Liu et al. 2021). The NORDIC NEC study retrospectively evaluated outcomes in 196 patients with gastroenteropancreatic NENs treated with platinum-based therapies of which 24 were G3 NETs. These patients had an overall response rate of 24% with a PFS of 5 months (as compared to an overall response rate of 44% for NEC with a Ki-67 of >55% and PFS of 5 months in NECs) (Sorbye et al. 2013). Together, these data suggest that platinum-based regimens have modest activity in G3 NETs. However, these data need to be interpreted with caution given the lack of information as to whether these regimens were selected due to concern about more aggressive NENs in these patients consistent with NECs. Temozolomide, especially in combination with capecitabine (CAPTEM), was the next most commonly reported regimen after platinum-based regimens with response rates ranging from 12 to 38% and PFS ranging from 6.7 to 15 months (Sorbye et al. 2013, Girardi, Silva et al. 2017, Jia et al. 2017, Sahu et al. 2018, Rogowski et al. 2019, Sahu et al. 2019, Chan et al. 2021, de Mestier et al. 2021, Lithgow et al. 2021). CAPTEM as an alternative front-line option was prospectively evaluated in the EA2142 clinical trial in which 63 patients with a non-small-cell gastroenteropancreatic G3 NEN (21 G3 NET, 36 NEC, 5 unknown) received either platinum and etoposide or CAPTEM. PFS with CAPTEM was not superior to platinum and etoposide at 3.45 vs 5.36 months. OS with CAPTEM was slightly better than platinum and etoposide at 12.6 vs 10.6 months (Eads et al. 2022). Studies evaluating FOLFOX reported a response rate of 64% in one study (Apostolidis et al. 2021) and two studies reported PFS of 8.6 and 10.8 months (Apostolidis et al. 2021). A single-center study reported similar findings but substantially shorter PFS with platinum/etoposide regimens than FOLFOX, 2.9 vs 13 months, respectively (Liu et al. 2021).
Summary of recommendations
G3 NET with Ki-67 <55–60% may have modest responses to platinum-based first-line therapies and the majority of the panel felt that this was not an appropriate front-line chemotherapy regimen in this setting. The majority of the group felt that CAPTEM was an appropriate front-line option particularly for patients with pancreatic primaries although patients with a G3 NET of the bowel may also benefit (despite data for this regimen in bowel primaries being less strong). The majority of the group felt that for pancreatic and bowel primaries, a fluoropyrimidine plus oxaliplatin regimen (either FOLFOX or CapeOx) is also appropriate.
Chemotherapies for second-line and beyond
Several small studies have evaluated the role of temozolomide-based therapy in the second line, most commonly as CAPTEM (Rogowski et al. 2019, Sahu et al. 2019, Chan et al. 2021). Most patients reported in these studies had a pancreatic primary and were previously treated, usually with a platinum-based regimen. Objective response rates ranged from 47 to 52% by RECIST and median PFS and median OS ranged from 6 to 15 months and 24 to 30 months, respectively. Multiple other chemotherapy regimens have been evaluated in small studies, including FOLFOX/CAPOX, FOLFIRI, and streptozocin-based and gemcitabine-based regimens, but the small sample sizes and the heterogeneity of the studies preclude recommendations for use (Cassier et al. 2009, Hentic et al. 2012, Ferrarotto et al. 2013, Dussol et al. 2015). One study found that among various cytotoxic regimens used in the second-line setting, FOLFOX yielded the longest PFS (13.9 months), while the PFS with CAPTEM and FOLFIRI was 7.7 and 2.4 months, respectively (Apostolidis et al. 2021). As such, CAPTEM is a reasonable choice for second-line therapy and beyond if not used in first line, with FOLFOX and FOLFIRI being alternative options.
Targeted therapies
Targeted therapy in both G3 NET and NEC is not well established with only a few retrospective studies describing the use of everolimus and sunitinib in patients with pancreatic G3 NETs (Panzuto et al. 2017, Mizuno et al. 2018, Pellat et al. 2018). Based on consensus, it is acceptable to consider everolimus for patients with progressive and refractory high-grade NETs of both pancreatic and bowel origin as well as sunitinib for G3 pancreatic NET, particularly in patients with favorable biology. Given the absence of good quality evidence and in light of the availability of agnostic targeted therapies (Drilon et al. 2018), the panel encourages the use of NGS for patients with G3 NETs as another tool to guide therapy in the refractory setting, especially if a clinical trial is not available.
Peptide receptor radionuclide therapy
Peptide receptor radionuclide therapy (PRRT) is approved in the United States for the treatment of somatostatin receptor-positive gastroenteropancreatic NETs, including foregut, midgut, and hindgut tumors. Although no randomized trial has established the role of PRRT in patients with G3 NENs, a few studies show encouraging results in patients with G3 NETs, reporting objective and durable responses ranging from 35 to 42% and a PFS ranging from 9 to 14 months (Thang et al. 2018, Zhang et al. 2019, Carlsen et al. 2019, Raj et al. 2022). The randomized clinical trial NETTER-2 evaluated the role of PRRT in G2/3 gastroenteropancreatic NETs with a Ki-67 index of ≥10 to ≤55% and completed accrual in late 2022 (NCT03972488). The COMPOSE trial is investigating 177Lu-Edotreotide vs best standard of care in aggressive G2/G3 gastroenteropancreatic NET (NCT04919226). Based on consensus, it is reasonable to consider PRRT in patients with progressive G3 NET showing homogeneously high (avidity greater than liver) SSTR expression by imaging.
Immunotherapy
Immunotherapy has not been shown to be active in NETs as suggested by the KEYNOTE-158 trial. In this trial, an overall response rate of 3.7% was observed with zero complete responses and four partial responses (Strosberg et al. 2020). A few single-arm phase II trials in G3 NENs suggest similar outcomes. A joint analysis of two phase II studies that enrolled 29 patients with previously treated metastatic G3 NENs to receive pembrolizumab showed limited activity with single-agent therapy with a response rate of only 3.5% (Vijayvergia et al. 2020). Avelumab was studied in G3 NENs through the AVENEC trial and included 10 patients with a G3 NET. The response rate was 6.9% in the entire cohort and PFS was similar for G3 NET as well as NEC (Fottner et al. 2019). The only trial to demonstrate the benefit of immunotherapy is a phase II trial of JS001 in 21 patients with NENs, 3 of which were G3 NET. Two of the G3 NET patients achieved a partial response and a response rate of 19% was observed amongst the whole cohort. Unfortunately, these responses did not translate into improvement in PFS (median PFS 2.8 months) (Zhang et al. 2018a ).
Combination therapy with nivolumab and ipilimumab has shown promising activity in G3 NENs but the proportion of G3 NET vs NEC included is unknown (Patel et al. 2020). The recently reported DUNE study of durvalumab plus tremelimumab in different neuroendocrine cohorts included 33 patients with G3 NEN, including 15 patients with G3 NET. Overall, the G3 NEN cohort had a modest immune-related overall response rate of 9.4% and a 9-month OS of 36.1% (Capdevila et al. 2021). One-third of patients with G3 NEN had OS greater than 1 year, including patients with both G3 NET and NEC. The role of immunotherapy in G3 NET is not supported by data at this time and further prospective trials are needed.
Surgical debulking
Studies evaluating the outcomes of patients with metastatic G3 NEN who have undergone surgical resection/debulking have been limited by small numbers and the inclusion of patients with both G3 NET and NEC. There is evidence suggesting acceptable outcomes following liver debulking in select patients with G3 NET, particularly those with more favorable biology. A retrospective study of 32 patients with G3 NEN who underwent surgical and/or radiofrequency ablation of liver metastases with curative intent showed a median PFS of 8.4 months (95% CI: 20.6–51.3 months), OS of 35.9 months (95% CI: 20.6–51.3 months) and a 5-year OS of 43% (Galleberg et al. 2017). Factors associated with improved OS were Ki-67 <55% and receiving adjuvant chemotherapy. A retrospective analysis from Japan included 63 patients with G3 NEN and found that surgery and low Ki-67 value (<52%) were independent factors associated with improved survival (Asano et al. 2020). There was no difference in survival between those undergoing surgery vs chemotherapy in patients with a higher Ki-67 (≥52%). Morphologic differentiation as defined by WHO 2017 criteria showed no association with OS. Although selection bias may influence results, additional small retrospective studies have also indicated a potential survival benefit in patients with G3 NEN undergoing aggressive locoregional therapy (Du et al. 2015, Crippa et al. 2016). Overall, the majority of the panel felt that surgical debulking for patients with a metastatic G3 NET was appropriate, particularly for those with favorable biology, but that this should be determined within the context of a multidisciplinary discussion.
Treatment of metastatic GI NEC
Liver-directed therapy
Please see the liver-directed therapy section earlier for details regarding this therapy. No data exist that would justify the use of liver-directed therapy in NEC. However, there was a lack of consensus from the group in regard to its role in this patient population.
Front-line chemotherapy
For the past 30 years, NEC has been treated akin to small-cell lung cancer. Early studies by Moertel and Mitry were the first to report on the favorable response rates of NECs with combined etoposide and cisplatin chemotherapy (Moertel et al. 1991, Mitry et al. 1999), although the response was not measured using conventional techniques. The largest cohort of advanced GI NEC patients reported is from the Nordic group (Sorbye et al. 2013). This retrospective study reported detailed data on treatment, outcomes, and survival. A total of 252 patients received palliative chemotherapy with platinum and etoposide chemotherapy. Responses were seen in 31% of patients and stable disease in 33% of patients. Patients with a Ki-67 < 55% had a lower response rate than patients with a Ki-67 ≥ 55% (15 vs 42%, P < 0.001) but better survival than patients with a Ki-67 ≥ 55% (14 vs 10 months, P < 0.001). It was also found that cisplatin could probably be replaced by the less toxic carboplatin, as the two compounds were comparable in efficacy. The addition of immunotherapy to platinum/etoposide has been shown to be superior to chemotherapy alone in small-cell lung cancer (Horn et al. 2018, Paz-Ares et al. 2019) and an ongoing SWOG trial is evaluating platinum/etoposide with or without atezolizumab in NEC (NCT05058651).
Summary of recommendations
These published reports, as well as the consensus opinion of the panel, recommend that patients with metastatic GI NEC be given palliative platinum and etoposide chemotherapy. The majority of the group felt that this regimen may be used for six cycles or longer provided there is no disease progression and the patient is tolerating treatment well. Immunotherapy should not be added to this regimen at this time and we await the results of the ongoing platinum/etoposide with or without atezolizmab trial (NCT05058651).
Alternative front-line therapies
The combination of cisplatin and irinotecan (IP) has demonstrated at least equivalent efficacy as cisplatin and etoposide (EP) in advanced NEC of the intestinal system (Morizane et al. 2022). In the JCOG1213 randomized phase III trial, 170 patients with NEC received either EP or IP and no significant difference was seen in median OS (12.5 months with EP, 10.9 months with IP, HR 1.042, P = 0.797) or PFS (5.6 months with EP, 5.1 months with IP). Response rates were also similar (54.5% with EP, 52.5% with IP). IP was associated with less hematologic toxicity, making this a reasonable alternative front-line therapy. Similar results were observed in a smaller randomized phase II trial (Zhang et al. 2020) as well as several retrospective NEC trials (Okita et al. 2011, Nakano et al. 2012, Lu et al. 2013, Ramella Munhoz et al. 2013, Okuma et al. 2014, Yamaguchi et al. 2014). The triplet chemotherapy regimen of carboplatin, etoposide and paclitaxel did not show superiority to dual-agent therapy and was associated with higher rates of grade 3/4 toxicity (Hainsworth et al. 2006). Temozolomide and capecitabine have been evaluated as detailed in the G3 NET section (Eads et al. 2022).
In the front-line setting, capecitabine plus oxaliplatin (CAPOX) yielded a response rate of approximately 20% and 5-fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFIRINOX) showed a near complete response in a patient with pancreatic NEC (Bajetta et al. 2007, Ferrarotto et al. 2013, Zhu et al. 2015). Although these results are encouraging, the studies are limited by small patient numbers and a lack of information regarding tumor differentiation. FOLFIRINOX is being compared prospectively to platinum/etoposide in the FOLFIRINEC trial, a randomized phase II trial (NCT04325425) (Hadoux et al. 2021).
Summary of recommendations
Cisplatin plus irinotecan is associated with response rates and PFS durations comparable to cisplatin plus etoposide, particularly for NEC arising in the GI tract or pancreas. There was consensus that platinum plus irinotecan is a reasonable alternative front-line chemotherapy option for NEC.
Second- and third-line treatment options
Options for salvage therapy in patients with NEC have not been rigorously evaluated. There was consensus from the group that retreatment with platinum-based therapy can be considered in patients who experience a durable response to therapy and progression during a break from treatment. Several studies have also evaluated alternative regimens in patients whose disease has progressed on platinum-based therapy. A retrospective study of 64 patients with progressive NEC receiving second-line therapy of any sort after first-line platinum/etoposide showed limited efficacy of any second-line therapy and short survival (McGarrah et al. 2020b ). The median PFS and OS were 2.3 and 6.2 months, respectively, and no particular regimen appeared superior to another. The recent phase II PRODIGE 41-BEVANEC trial randomized 133 patients to receive FOLFIRI with or without bevacizumab. The trial did not show any benefit for the addition of bevacizumab to chemotherapy but did report a 6-month OS rate of 53% (Walter et al. 2023). While this study did not compare FOLFIRI to an alternative cytotoxic backbone, the survival rate was favorable, making FOLFIRI an acceptable second-line treatment option with some groups suggesting this as a favored approach (Garcia-Carbonaro et al. 2023). In addition to irinotecan-based regimens, oxaliplatin-based therapy is also an option with retrospective data showing response rates of 20–30% with FOLFOX and CAPOX (Hentic et al. 2012, Hadoux et al. 2015, Heetfeld et al. 2015, Walter et al. 2017). Although CAPTEM has been evaluated in patients with G3 NENs, response and survival have been correlated with a Ki-67 index of <60%; there is limited data regarding the efficacy of CAPTEM specifically in patients with NEC (Welin et al. 2011, Owen et al. 2017, Chan et al. 2021). A second-line study of dacarbazine or temozolomide-based therapy reported a median PFS of 3 months and median OS of 7.2 months (Couronne et al. 2020). Other regimens such as topotecan and anthracyclines have been studied yielding similar disappointing results, sometimes with substantial toxicity, and are generally not recommended (Olsen et al. 2014, Apostolidis et al. 2016, Munker et al. 2020). The NET-02 trial was a randomized phase II study evaluating liposomal irinotecan (Nal-IRI) and 5-fluorouracil vs docetaxel with a primary endpoint of 6-month PFS rate. Although Nal-IRI/5-FU met the primary endpoint with a 32% 6-month PFS rate, both regimens had short median PFS of 3 and 2 months, respectively (Craig et al. 2020, McNamara et al. 2022). Clearly prospective trials in the second-line NEC space are needed. The SENECA trial is a randomized phase II trial evaluating CAPTEM vs FOLFIRI with a primary endpoint of disease control rate and safety (NCT03387592) (Bongiovanni et al. 2018).
Summary of recommendations
Depending on the timeline, re-treatment with platinum and etoposide is an option. FOLFIRI is a second-line option with the most evidence; however, additional options include oxaliplatin- or temozolomide-based regimens.
Immunotherapy
Single-agent PD-1/PD-L1 inhibitor therapy has shown disappointing results in NEC as noted earlier. The only outlier was a phase II trial of JS001 in 21 patients with NENs, 15 of which were NECs (Zhang et al. 2018b ). The response rate among NEC patients was 13% and unfortunately, no improvement in PFS was observed (median PFS 2.8 months).
In terms of combination therapy, a phase II basket study of ipilimumab (CTLA-4 inhibitor) and nivolumab (PD-1 inhibitor) in rare cancers (DART trial) suggested that dual checkpoint inhibition may yield a higher response rate than anti-PD-1 monotherapy in patients with G3 NENs. In a cohort of 18 patients with non-pancreatic NENs, a response rate of 44% and a median PFS of 4 months were observed. In a cohort of DART patients with high-grade NENs, including unknown, pancreas, GI, and cervical primaries, the response rate was 26%, including durable responses in some patients (Patel et al. 2021). Detailed information regarding the differentiation/grade of the bowel primaries was not reported, but all tumors were microsatellite stable (Patel et al. 2021). In yet another basket trial evaluating ipilimumab and nivolumab in rare cancers, combination immunotherapy was shown to have activity in subgroups of patients with advanced NENs. Objective responses were seen in 31% of the 13 patients with G3 disease (Klein et al. 2020). In the DUNE study, the combination of durvalumab (PD-L1 inhibitor) and tremelimumab (CTLA-4 inhibitor) in four NEN cohorts, including G3 NET/NEC, demonstrated a very modest response rate with the immune-related response rate of 9.4% in the G3 NEN cohort and a 9-month OS of 36.1% (Capdevila et al. 2021). PD-L1 expression was not found to enrich for response to immunotherapy. One of the largest trials specifically evaluating NEC was the phase II NIPINEC trial where 93 patients with gastroenteropancreatic NEC and 90 patients with large-cell NEC of the lung were randomized to nivolumab vs nivolumab plus ipilimumab in the second or third line setting. The overall response rate at 8 weeks and the median OS in the nivo vs combination therapy group were 7.5% and 7.2 months vs 14.9% and 5.8 months, respectively (Girard et al. 2021). Lastly, two recent and partially overlapping retrospective studies evaluated the role of immunotherapy in patients with refractory NEC (Al-Toubah et al. 2021, Gile et al. 2021). Immune checkpoint inhibitor monotherapy was ineffective but dual therapy yielded modest response rates of 13–15% and PFS was short at 1 to 3.5 months. Recent guidance from ENETS indicates that most patients with NEC do not benefit from immune checkpoint inhibitor therapy and that it should not be used in routine practice but may be considered in instances where patients have DNA MMR deficiency or high tumor mutational burden (Sorbye et al. 2023).
Summary of recommendations
Current data do not support the use of single-agent immune checkpoint inhibitors in G3 NECs. Preliminary data point to the role of dual immunotherapy and the majority of the group felt that this is a reasonable second line (and beyond) treatment option; however, data are sparse and clinical trial enrollment is encouraged. There was consensus that single- or dual-agent immunotherapy is appropriate in patients with DNA MMR deficiency or high tumor mutational burden, given the agnostic drug approvals of pembrolizumab (DNA MMR deficiency or high tumor mutational burden) and dostarlimab-gxly (DNA MMR deficiency).
Somatostatin analogs
Traditionally reserved for well-differentiated NETs, SSAs are not thought to have a role in controlling tumor growth in NECs. In a study of 28 patients with G3 NENs receiving an SSA, G3 NETs were significantly more likely to be associated with positive SSTR imaging compared to NEC (88 vs 50% respectively) and demonstrated a better median OS (41 vs 17 months, respectively) (Velayoudom-Cephise et al. 2013). The ENETS guideline panel specifically notes that there are no data to support the use of SSAs in patients with SSTR-positive GI and pancreatic NECs, and neither the NANETS nor NCCN guidelines advocate for the use of SSAs in this setting (Strosberg et al. 2010, Garcia-Carbonero et al. 2016, Shah et al. 2021). As such, we do not recommend SSAs for tumor control in NEC.
PRRT and targeted therapies
There is no data to support the use of PRRT in NEC. Given the expected low SSTR expression in this group, it is unlikely to have an effect. Similarly, data supporting the use of targeted therapies in NEC is lacking. Reports about BRAF inhibitors (+/− MEK inhibitors) in BRAF-mutated colorectal NECs are available (Klempner et al. 2016, Burkart et al. 2018); however, the use of BRAF inhibitors, MEK inhibitors, everolimus, and sunitinib are not approved for treatment of NEC. Targeted therapies with disease agnostic indications (immune checkpoint inhibitors for microsatellite unstable/deficient DNA MMR or high tumor mutational burden; larotrectinib or entrectinib for tumors with NTRK fusions; selpercatinib or pralsetinib for tumors with RET fusions) are a reasonable consideration for NEC patients harboring the appropriate molecular abnormalities but are rare.
Role of surgery
Given the generally aggressive nature of NEC, surgical debulking is not performed. The importance of distinguishing G3 NET from NEC was highlighted in a retrospective multicenter analysis from Japan that evaluated the outcomes of 67 patients with G3 NEN of pancreatic origin (Yoshida et al. 2019). Patients with a pancreatic G3 NET who had undergone surgery had improved survival compared to those who had not; however, this was not the case for patients with pancreatic NEC. There was consensus from the group that there is no role for surgical debulking of patients with metastatic NEC.
Monitoring assessments for metastatic disease
Given the relatively aggressive nature of high-grade NENs, regular assessment of disease status during treatment is important. Monitoring assessments have been recommended within the NCCN, ESMO, and ENETS NEN guidelines as previously mentioned (Garcia-Carbonero et al. 2016, Pavel et al. 2020, Shah et al. 2021). In line with these guidelines and based upon our review of the data, the majority of the panel recommends the following monitoring assessments be performed for patients receiving treatment for a metastatic grade 3 NEN (Table 3).
Table 3.
Monitoring assessments for patients being treated for a metastatic G3 neuroendocrine neoplasm
| G3 NET | NEC | |
|---|---|---|
| Imaging | Multiphase, high-resolution CT or MRI with contrast every 3 months (every 6 months if more indolent disease) | Multiphase, high-resolution CT or MRI with contrast every 2–3 months |
| SSTR-PET imaging as indicated | MRI brain if high systemic disease burden or if symptomatic | |
| FDG-PET as indicated | FDG-PET as indicated | |
| SSTR-PET imaging as indicated | ||
| Biopsy | As indicated if pace of progression suggests a change in biology | Not indicated |
Treatment of metastatic gynecologic G3 NEC
Locally advanced disease, defined as a disease limited to the pelvis +/− aortocaval nodal disease (FIGO stages IB3–IVA) may be treated with intent to cure. Although some may be concerned with the use of radiation therapy concurrently with cisplatin and etoposide, studies have shown this is safe and tolerable and this approach has become the standard of care (Hoskins et al. 2003). Radiation can be started with cycle 1 of cisplatin and etoposide, utilized as ‘sandwich’ therapy (i.e. in the middle of chemotherapy), or added to the final two cycles of chemotherapy. As is the case with early stage disease, it is important to complete six cycles of chemotherapy if tolerated. Studies have shown improved disease-free survival and OS when ≥5 cycles are given (Wang et al. 2012). For metastatic disease to liver, lungs, or peritoneum (stage IVB), palliative chemotherapy with cisplatin and etoposide is recommended.
For patients with small-cell carcinoma of the cervix, commonly used second-line and beyond cytotoxic chemotherapy agents include topotecan, irinotecan and taxanes. A single institution retrospective analysis demonstrated superior PFS in patients with advanced cervical small-cell carcinoma receiving the combination of topotecan, paclitaxel, and bevacizumab (median PFS 8 vs 4 months for other regimens) (Frumovitz et al. 2017).
Management of brain metastases
Given the low rate of intracranial metastases in patients with extra-pulmonary NENs, prophylactic cranial irradiation is not a recommended treatment strategy. General principles surrounding the management of brain metastases are recommended; patients with ≤4 metastases should be treated with stereotactic radiosurgery (SRS) while patients with more advanced CNS disease may be considered for SRS or whole brain radiation.
Cardiac considerations
G3 NENs rarely result in functional syndromes, and therefore, there is little need for cardiac monitoring for carcinoid heart disease in this patient population (Sorbye et al. 2018). G3 NECs rarely if ever produce serotonin and among the G3 NETs, many are of pancreatic origin and therefore unlikely to produce serotonin (Phan et al. 2017, Tsoukalas et al. 2017, Zavras et al. 2017). While G3 NETs of small bowel primary are rare, they can be associated with carcinoid syndrome and therefore, carcinoid heart disease among all patients with G3 NENs is expected to be rare. Routine cardiac evaluation and/or monitoring is therefore not recommended. In cases of suspected carcinoid syndrome, tumor production of serotonin should be investigated, either with plasma or urinary 5-HIAA and if elevated, an echocardiogram should be performed. Cardiotoxicity of anti-cancer therapy is increasingly recognized and should be considered in cases of symptoms thought to be of cardiac origin (Finet & Tang 2018).
Hereditary risk
Genetic risk factors for the development of high-grade NENs have not been well elucidated and a detailed search of the literature failed to reveal any studies addressing this question. Established genetic syndromes associated with NETs such as neurofibromatosis 1 and multiple endocrine neoplasia 1 have rarely reported G3 NENs as part of their syndromes (Bordi et al. 1997, Chakrabarti et al. 2019). Similarly, an association of germline mutations in homologous recombination repair pathways, for example, BRCA2 and PALB2 mutations, with G3 NENs is limited to case reports (Bhatla et al. 2016, Herold et al. 2018). MMR deficiency, however, is being increasingly reported in G3 NENs. In one study, microsatellite instability (MSI) analysis and IHC for DNA MMR proteins were performed in 89 GI or pancreatic NECs or mixed adeno-NECs. MSI was observed in 11 cases (12.4%). All but two of the MSI cases showed MLH1 methylation and loss of MLH1 protein suggesting that these were not Lynch syndrome-related tumors (Sahnane et al. 2015). Another study identified MSI or MMR deficiency in colorectal G3 NEC in approximately 7% of cases, but no clear association with Lynch syndrome has been established (Olevian et al. 2016). Current evidence does not suggest inherited syndromes as a possible etiology for the development of G3 NENs and the panel does not recommend routine genetic evaluation based solely on the diagnosis of a G3 NEN.
Discussion
High-grade NENs are a rare disease entity for which little prospective data are available. In more recent years, the distinction between well-differentiated G3 NET and poorly differentiated NEC has further complicated the management of this disease. The first step to a successful treatment strategy is a strong pathologic evaluation, allowing for the confident interpretation of tumor grade and differentiation. Advances over the past several years have broadened our diagnostic and treatment capabilities for this disease and include a multidisciplinary approach involving pathology, medical oncology, surgical oncology, nuclear medicine, radiation oncology, and interventional radiology. Given the nuanced management that is often needed for the care of patients with high-grade NENs, it is recommended that patients seek care or at least an opinion at a comprehensive neuroendocrine treatment center. With the lack of prospective data available in this disease, the panel also encourages clinical trial participation whenever possible.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author contribution statement
JRE: consulting—Advanced Accelerator Applications, Ipsen, Lexicon; employment (spouse)—Bristol Myers Squibb, Janssen; research support—Hutchmed, Seagen, Oncolys, Medimmune, Xencor, AstraZeneca, Genentech; stock (spouse)—Bristol Myers Squibb. TRH: consulting—Advanced Accelerator Applications, TerSera, Ipsen, Crinetics, Terumo, Viewpoint Molecular Imaging, ITM Isotopen Technologien Muenchen; research support—Advanced Accelerator Applications, Turnstone Biologics, Basilea, Thermo Fisher Scientific, Agios. TA: consulting—Ipsen, Eisai, Bristol Myers Squibb, Taiho, Amgen, Novartis, Bayer; speaker—Ipsen, Amgen, Novartis. AMB: no disclosures. EB: research support—Merck. AD: consulting—Novartis, Ipsen, Voluntis, Abbvie, Crinetics, Hutchmed, Personalis; research support—Novartis, Eisai, Ipsen, Hutchmed, Guardant Health, Natera. GEH: consulting—Novartis, Canon Medical Systems, Terumo, Boston Scientific, Bayer, Curium Pharma. MF: consulting—Stryker, Seagen; research support—AkesoBio, GlaxoSmithKline, AstraZeneca. JEM: honoraria—Varian; research support—Varian Medical Systems. EM: consulting—Curium, Ipsen, ITM, Telix, TerSera, Lantheus; research support—Curium, ITM, Novartis, Nordic Nanovector. SM: honoraria—Advanced Accelerator Applications/Novartis, Tersera; research support—Advanced Accelerator Applications/Novartis, Ipsen. EN: no disclosures. NR: Ipsen, HRA Pharma, Advanced Accelerator Applications/Novartis; research support—Novartis, Xencor, Corcept Therapeutics, ITM Isotope Technologies Munich. HS: consulting—Helsinn, Excelixis, AstraZeneca, Pfizer, TerSera, Ipsen, Novartis. BU: no disclosures. NV: consulting—ITM, Novartis, AstraZeneca/Daiichi Sankyo, Taiho Oncology, Tersera Therapeutics; honoraria—Guidepoint Global; research support—Zymeworks, Puma Biotechnology. JAC: consulting—Advanced Accelerator Applications/Novartis, TerSera; honoraria—Advanced Accelerator Applications/Novartis, Ipsen, Bayer (spouse), Pfizer (spouse); stock—Merck; research support—Lilly, Sanofi.
References
- Akimoto J Fukuhara H Suda T Nagai K Ichikawa M Fukami S Kohno M Matsubayashi J & Nagao T. 2016Clinicopathological analysis in patients with neuroendocrine tumors that metastasized to the brain. BMC Cancer 16 36. ( 10.1186/s12885-015-1999-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alese OB Jiang R Shaib W Wu C Akce M Behera M & El-Rayes BF. 2019High-grade gastrointestinal neuroendocrine carcinoma management and outcomes: a national cancer database study. Oncologist 24911–920. ( 10.1634/theoncologist.2018-0382) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Toubah T Halfdanarson T Gile J Morse B Sommerer K & Strosberg JR. 2021Efficacy of ipilimumab and nivolumab in patients with high grade neuroendocrine neoplasms. ESMO Open 7 100364. doi:10.1016/j.esmoop.2021.100364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Toubah T Partelli S Cives M Andreasi V Silvestris F Falconi M Anaya DA & Strosberg J. 2019Local treatment for focal progression in metastatic neuroendocrine tumors. Endocrine-Related Cancer 26405–409. ( 10.1530/ERC-18-0462) [DOI] [PubMed] [Google Scholar]
- Apostolidis L Bergmann F Jager D & Winkler EC. 2016Efficacy of topotecan in pretreated metastatic poorly differentiated extrapulmonary neuroendocrine carcinoma. Cancer Medicine 52261–2267. ( 10.1002/cam4.807) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apostolidis L Dal Buono A Merola E Jann H Jager D Wiedenmann B Winkler EC & Pavel M. 2021Multicenter analysis of treatment outcomes for systemic therapy in well differentiated grade 3 neuroendocrine tumors (NET G3). Cancers (Basel) 13 1936. ( 10.3390/cancers13081936) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arvold ND, Willett CG, Fernandez-del Castillo C, Ryan DP, Ferrone CR, Clark JW, Blaszkowsky LS, Deshpande V, Niemierko A, Allen JN, et al. 2012Pancreatic neuroendocrine tumors with involved surgical margins: prognostic factors and the role of adjuvant radiotherapy. International Journal of Radiation Oncology, Biology, Physics 83e337–e343. ( 10.1016/j.ijrobp.2011.12.068) [DOI] [PubMed] [Google Scholar]
- Asano D Kudo A Akahoshi K Maekawa A & Murase Y. 2020Curative surgery and Ki-67 Value rather than tumor differentiation predict the survival of patients with high-grade neuroendocrine neoplasms. Annals of Surgery 276e, 108–e. ( 10.1097/SLA.0000000000004495) [DOI] [PubMed] [Google Scholar]
- Bajetta E, Catena L, Procopio G, De Dosso S, Bichisao E, Ferrari L, Martinetti A, Platania M, Verzoni E, Formisano B, et al. 2007Are capecitabine and oxaliplatin (XELOX) suitable treatments for progressing low-grade and high-grade neuroendocrine tumours? Cancer Chemotherapy and Pharmacology 59637–642. ( 10.1007/s00280-006-0306-6) [DOI] [PubMed] [Google Scholar]
- Basturk O, Tang L, Hruban RH, Adsay V, Yang Z, Krasinskas AM, Vakiani E, La Rosa S, Jang KT, Frankel WL, et al. 2014Poorly differentiated neuroendocrine carcinomas of the pancreas: a clinicopathologic analysis of 44 cases. American Journal of Surgical Pathology 38437–447. ( 10.1097/PAS.0000000000000169) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basturk O, Yang Z, Tang LH, Hruban RH, Adsay V, McCall CM, Krasinskas AM, Jang KT, Frankel WL, Balci S, et al. 2015The high-grade (WHO G3) pancreatic neuroendocrine tumor category is morphologically and biologically heterogeneous and includes both well differentiated and poorly differentiated neuroendocrine neoplasms. American Journal of Surgical Pathology 39683–690. ( 10.1097/PAS.0000000000000408) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellizzi AM.2020aAn algorithmic immunohistochemical approach to define tumor type and assign site of origin. Advances in Anatomic Pathology 27114–163. ( 10.1097/PAP.0000000000000256) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellizzi AM.2020bImmunohistochemistry in the diagnosis and classification of neuroendocrine neoplasm: what can brown do for you? Human Pathology 968–33. ( 10.1016/j.humpath.2019.12.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergsland EK Roy R Stephens P Ross JS Bailey M & Olshen A. 2016Genomic profiling to distinguish poorly differentiated neuroendocrine carcinomas arising in different sites. Journal of Clinical Oncology 34(Supplement) 4020. ( 10.1200/JCO.2016.34.15_suppl.4020) [DOI] [Google Scholar]
- Bermudez A Vighi S Carcia A & Sardi J. 2001Neuroendocrine cervical carcinoma: a diagnostic and therapeutic challenge. Gynecologic Oncology 8232–39. ( 10.1006/gyno.2001.6201) [DOI] [PubMed] [Google Scholar]
- Bertani E Ravizza D Milione M Massironi S Grana CM Zerini D Piccioli AN Spinoglio G & Fazio N. 2018Neuroendocrine neoplasms of rectum: a management update. Cancer Treatment Reviews 6645–55. ( 10.1016/j.ctrv.2018.04.003) [DOI] [PubMed] [Google Scholar]
- Bhatla T, Dandekar S, Lu BY, Wang J, Han E, Bitterman D, Jones CL, Evensen NA, Magid M, Meyer JA, et al. 2016Genomic characterization of poorly differentiated neuroendocrine carcinoma in a pediatric patient. Journal of Pediatric Hematology/Oncology 38e21–e25. ( 10.1097/MPH.0000000000000463) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bongiovanni A, Pusceddu S, Leo S, Di meglio G, Gelsomino F, Pucci F, Berardi R, Ricci S, Lolli I, Bergamo F, et al. 2018CAPTEM or FOLFIRI as second-line therapy in neuroendocrine carcinomas and exploratory analysis of predictive role of PET imaging and biological markers (Seneca study). Annals of Oncology 29(Supplement 8) viii477–viii478. ( 10.1093/annonc/mdy293.026) [DOI] [Google Scholar]
- Bordi C Falchetti A Azzoni C D’Adda T Canavese G Guariglia A Santini D Tomassetti P & Brandi ML. 1997Aggressive forms of gastric neuroendocrine tumors in multiple endocrine neoplasia type I. American Journal of Surgical Pathology 211075–1082. ( 10.1097/00000478-199709000-00012) [DOI] [PubMed] [Google Scholar]
- Boudreaux JP, Klimstra DS, Hassan MM, Woltering EA, Jensen RT, Goldsmith SJ, Nutting C, Bushnell DL, Caplin ME, Yao JC, et al. 2010The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well-differentiated neuroendocrine tumors of the jejunum, ileum, appendix, and cecum. Pancreas 39753–766. ( 10.1097/MPA.0b013e3181ebb2a5) [DOI] [PubMed] [Google Scholar]
- Brannon AR, Vakiani E, Sylvester BE, Scott SN, McDermott G, Shah RH, Kania K, Viale A, Oschwald DM, Vacic V, et al. 2014Comparative sequencing analysis reveals high genomic concordance between matched primary and metastatic colorectal cancer lesions. Genome Biology 15 454. ( 10.1186/s13059-014-0454-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brixi-Benmansour H Jouve JL Mitry E Bonnetain F Landi B Hentic O Bedenne L & Cadiot G. 2011Phase II study of first-line FOLFIRI for progressive metastatic well-differentiated pancreatic endocrine carcinoma. Digestive and Liver Disease 43912–916. ( 10.1016/j.dld.2011.07.001) [DOI] [PubMed] [Google Scholar]
- Burkart J, Owen D, Shah MH, Abdel-Misih SRZ, Roychowdhury S, Wesolowski R, Haraldsdottir S, Reeser JW, Samorodnitsky E, Smith A, et al. 2018Targeting BRAF mutations in high-grade neuroendocrine carcinoma of the colon. Journal of the National Comprehensive Cancer Network 161035–1040. ( 10.6004/jnccn.2018.7043) [DOI] [PubMed] [Google Scholar]
- Canellas R Burk KS Parakh A & Sahani DV. 2018Prediction of pancreatic neuroendocrine tumor grade based on CT features and texture analysis. AJR. American Journal of Roentgenology 210341–346. ( 10.2214/AJR.17.18417) [DOI] [PubMed] [Google Scholar]
- Capdevila J, Hernando J, Teule A, Lopez C, Garcia-Carbonero R, Benavent M, Custodio A, Garcia-Alvarez A, Cubillo A. et al. 2023Durvalumab plus tremelimumab for the treatment of advanced neuroendocrine neoplasms of gastroenteropancreatic and lung origin. Nature Communications 142973. ( 10.1038/s41467-023-38611-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsen EA, Fazio N, Granberg D, Grozinsky-Glasberg S, Ahmadzadehfar H, Grana CM, Zandee WT, Cwikla J, Walter MA, Oturai PS, et al. 2019Peptide receptor radionuclide therapy in gastroenteropancreatic NEN G3: a multicenter cohort study. Endocrine-Related Cancer 26227–239. ( 10.1530/ERC-18-0424) [DOI] [PubMed] [Google Scholar]
- Cassier PA Walter T Eymard B Ardisson P Perol M Paillet C Chayvialle JA Scoazec JY Hervieu V & Lombard-Bohas CL. 2009Gemcitabine and oxaliplatin combination chemotherapy for metastatic well-differentiated neuroendocrine carcinomas: a single-center experience. Cancer 1153392–3399. ( 10.1002/cncr.24384) [DOI] [PubMed] [Google Scholar]
- Castellano D Grande E Valle J Capdevila J Reidy-Lagunes D O’Connor JM & Raymond E. 2015Expert consensus for the management of advanced or metastatic pancreatic neuroendocrine and carcinoid tumors. Cancer Chemotherapy and Pharmacology 751099–1114. ( 10.1007/s00280-014-2642-2) [DOI] [PubMed] [Google Scholar]
- Chakrabarti D Qayoom S Ghosh A & Gupta R. 2019Neuroendocrine carcinoma of the gall bladder in a young lady presenting with upper abdominal heaviness: a common complaint and a rare diagnosis. BMJ Case Reports 12 e229684. ( 10.1136/bcr-2019-229684) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakravarthy A & Abrams RA. 1995Radiation therapy in the management of patients with malignant carcinoid tumors. Cancer 751386–1390. () [DOI] [PubMed] [Google Scholar]
- Chan DL, Bergsland EK, Chan JA, Gadgil R, Halfdanarson TR, Hornbacker K, Kelly V, Kunz PL, McGarrah PW, Raj NP, et al. 2021Temozolomide in grade 3 gastroenteropancreatic neoplasms: a multicenter retrospective review. Oncologist 26950–955. ( 10.1002/onco.13923) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen JX, Rose S, White SB, El-Haddad G, Fidelman N, Yarmohammadi H, Hwang W, Sze DY, Kothary N, Stashek K, et al. 2017Embolotherapy for neuroendocrine tumor liver metastases: prognostic factors for hepatic progression-free survival and overall survival. Cardiovascular and Interventional Radiology 4069–80. ( 10.1007/s00270-016-1478-z) [DOI] [PubMed] [Google Scholar]
- Chen L Liu M Zhang Y Guo Y Chen MH & Chen J. 2021Genetic characteristics of colorectal neuroendocrine carcinoma: more similar to colorectal adenocarcinoma. Clinical Colorectal Cancer 20177–185.e13. ( 10.1016/j.clcc.2020.09.001) [DOI] [PubMed] [Google Scholar]
- Chen TC, Huang HJ, Wang TY, Yang LY, Chen CH, Cheng YM, Liou WH, Hsu ST, Wen KC, Ou YC, et al. 2015Primary surgery versus primary radiation therapy for FIGO stages I–II small cell carcinoma of the uterine cervix: a retrospective Taiwanese gynecologic oncology group study. Gynecologic Oncology 137468–473. ( 10.1016/j.ygyno.2015.03.015) [DOI] [PubMed] [Google Scholar]
- Chou A, Itchins M, de Reuver PR, Arena J, Clarkson A, Sheen A, Sioson L, Cheung V, Perren A, Nahm C, et al. 2018ATRX loss is an independent predictor of poor survival in pancreatic neuroendocrine tumors. Human Pathology 82249–257. ( 10.1016/j.humpath.2018.07.032) [DOI] [PubMed] [Google Scholar]
- Cohen JG Kapp DS Shin JY Urban R Sherman AE Chen LM Osann K & Chan JK. 2010Small cell carcinoma of the cervix: treatment and survival outcomes of 188 patients. American Journal of Obstetrics and Gynecology 203347.e1–347.e6. ( 10.1016/j.ajog.2010.04.019) [DOI] [PubMed] [Google Scholar]
- Contessa JN Griffith KA Wolff E Ensminger W Zalupski M Lawrence TS & Ben-Josef E. 2009Radiotherapy for pancreatic neuroendocrine tumors. International Journal of Radiation Oncology, Biology, Physics 751196–1200. ( 10.1016/j.ijrobp.2008.12.044) [DOI] [PubMed] [Google Scholar]
- Coriat R Walter T Terris B Couvelard A & Ruszniewski P. 2016Gastroenteropancreatic well-differentiated grade 3 neuroendocrine tumors: review and position statement. Oncologist 211191–1199. ( 10.1634/theoncologist.2015-0476) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couronne T Girot P Hadoux J Lecomte T Durand A Fine C Vandevoorde K Lombard-Bohas C & Walter T. 2020Post first-line dacarbazine or temozolomide in neuroendocrine carcinoma. Endocrine Connections 9498–505. ( 10.1530/EC-20-0192) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig Z, Swain J, Batman E, Wadsley J, Reed N, Faluyi O, Cave J, Sharma R, Chau I, Wall L, et al. 2020NET-02 trial protocol: a multicentre, randomized, parallel group, open-label, phase II, single-stage selection trial of liposomal irinotecan (nal-IRI) and 5-fluorouracil (5-FU)/folinic acid or docetaxel as second-line therapy in patients with progressive poorly differentiated extrapulmonary neuroendocrine carcinoma. BMJ Open 10 e034527. ( 10.1136/bmjopen-2019-034527) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crippa S Partelli S Bassi C Berardi R Capelli P Scarpa A Zamboni G & Falconi M. 2016Long-term outcomes and prognostic factors in neuroendocrine carcinomas of the pancreas: morphology matters. Surgery 159862–871. ( 10.1016/j.surg.2015.09.012) [DOI] [PubMed] [Google Scholar]
- Dasari A Mehta K Byers LA Sorbye H & Yao JC. 2018Comparative study of lung and extrapulmonary poorly differentiated neuroendocrine carcinomas: a SEER database analysis of 162,983 cases. Cancer 124807–815. ( 10.1002/cncr.31124) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasari A Shen C Devabhaktuni A Nighot R & Sorbye H. 2022Survival according to primary tumor location, stage, and treatment patterns in locoregional gastroenteropancreatic high-grade neuroendocrine carcinomas. Oncologist 27299–306. ( 10.1093/oncolo/oyab039) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasari A Shen C Halperin D Zhao B Zhou S Xu Y Shih T & Yao JC. 2017Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncology 31335–1342. ( 10.1001/jamaoncol.2017.0589) [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mestier L, Lamarca A, Hernando J, Zandee W, Alonso-Gordoa T, Perrier M, Walenkamp AM, Chakrabarty B, Landolfi S, Van Velthuysen MF, et al. 2021Treatment outcomes of advanced digestive well-differentiated grade 3 NETs. Endocrine-Related Cancer 28549–561. ( 10.1530/ERC-21-0109) [DOI] [PubMed] [Google Scholar]
- Del Prete M, Fiore F, Modica R, Marotta V, Marciello F, Ramundo V, Di Sarno A, Carratu A, di Roseto Cd, Tafuto S, et al. 2014Hepatic arterial embolization in patients with neuroendocrine tumors. Journal of Experimental and Clinical Cancer Research 33 43. ( 10.1186/1756-9966-33-43) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng HY Ni PZ Wang YC Wang WP & Chen LQ. 2016Neuroendocrine carcinoma of the esophagus: clinical characteristics and prognostic evaluation of 49 cases with surgical resection. Journal of Thoracic Disease 81250–1256. ( 10.21037/jtd.2016.04.21) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dongol S Tai Y Shao Y Jiang J & Kong B. 2014A retrospective clinicopathological analysis of small-cell carcinoma of the uterine cervix. Molecular and Clinical Oncology 271–75. ( 10.3892/mco.2013.193) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drilon A, Laetsch TW, Kummar S, DuBois SG, Lassen UN, Demetri GD, Nathenson M, Doebele RC, Farago AF, Pappo AS, et al. 2018Efficacy of larotrectinib in TRK fusion-positive cancers in adults and children. New England Journal of Medicine 378731–739. ( 10.1056/NEJMoa1714448) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du S, Wang Z, Sang X, Lu X, Zheng Y, Xu H, Xu Y, Chi T, Zhao H, Wang W, et al. 2015Surgical resection improves the outcome of the patients with neuroendocrine tumor liver metastases: large data from Asia. Medicine (Baltimore) 94 e388. ( 10.1097/MD.0000000000000388) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dussol AS Joly MO Vercherat C Forestier J Hervieu V Scoazec JY Lombard-Bohas C & Walter T. 2015Gemcitabine and oxaliplatin or alkylating agents for neuroendocrine tumors: comparison of efficacy and search for predictive factors guiding treatment choice. Cancer 1213428–3434. ( 10.1002/cncr.29517) [DOI] [PubMed] [Google Scholar]
- Eads JR, Catalano PJ, Fisher GA, Rubin D, Iagaru A, Klimstra DS, Konda B, Kwong MS, Chan JA, De Jesus-Acosta A, et al. 2022Randomized phase II study of platinum and etoposide versus temozolomide and capecitabine in patients with advanced G3 non-small cell gastroenteropancreatic neuroendocrine neoplasms (GEPNENs): ECOG-ACRIN EA2142. Journal of Clinical Oncology 40 (Supplement) 4020. ( 10.1200/JCO.2022.40.16_suppl.4020) [DOI] [Google Scholar]
- Eskander RN Elvin J Gay L Ross JS Miller VA & Kurzrock R. 2020Unique genomic landscape of high-grade neuroendocrine cervical carcinoma: implications for rethinking current treatment paradigms. JCO Precision Oncology 4972–987. ( 10.1200/PO.19.00248) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faggiano A, Carratu AC, Guadagno E, Tafuto S, Tatangelo F, Riccardi F, Mocerino C, Palmieri G, Damiano V, Siciliano R, et al. 2016Somatostatin analogues according to Ki67 index in neuroendocrine tumours: an observational retrospective-prospective analysis from real life. Oncotarget 75538–5547. ( 10.18632/oncotarget.6686) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faivre-Finn C, Snee M, Ashcroft L, Appel W, Barlesi F, Bhatnagar A, Bezjak A, Cardenal F, Fournel P, Harden S, et al. 2017Concurrent once-daily versus twice-daily chemoradiotherapy in patients with limited-stage small-cell lung cancer (CONVERT): an open-label, phase 3, randomized, superiority trial. Lancet. Oncology 181116–1125. ( 10.1016/S1470-2045(1730318-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng ST Luo Y Chan T Peng Z Chen J Chen M & Li ZP. 2014CT evaluation of gastroenteric neuroendocrine tumors: relationship between CT features and the pathologic classification. AJR. American Journal of Roentgenology 203W260–W266. ( 10.2214/AJR.13.11310) [DOI] [PubMed] [Google Scholar]
- Ferrarotto R Testa L Riechelmann RP Sahade M Siqueira LT Costa FP & Hoff PM. 2013Combination of capecitabine and oxaliplatin is an effective treatment option for advanced neuroendocrine tumors. Rare Tumors 5 e35. ( 10.4081/rt.2013.e35) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields AC Lu P Vierra BM Hu F Irani J Bleday R Goldberg JE Nash GM & Melnitchouk N. 2019Survival in patients with high-grade colorectal neuroendocrine carcinomas: the role of surgery and chemotherapy. Annals of Surgical Oncology 261127–1133. ( 10.1245/s10434-019-07203-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finet JE & Tang WHW. 2018Protecting the heart in cancer therapy. F1000 Faculty Rev 7. ( 10.12688/f1000research.15190.1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher GA, Wolin EM, Liyanage N, Pitman Lowenthal S, Mirakhur B, Pommier RF, Shaheen M, Vinik A. & ELECT Study Group 2018Patient-reported symptom control of diarrhea and flushing in patients with neuroendocrine tumors treated with lanreotide depot/autogel: results from a randomized, placebo-controlled, double-blind and 32-week open-label study. Oncologist 2316–24. ( 10.1634/theoncologist.2017-0284) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fottner C Apostolidis L Ferrata M Krug S Michi P Schad A Roth W Jaeger D Galle PR & Weber MM. 2019A phase II, open label, multicenter trial of avelumab in patients with advanced, metastatic, high-grade neuroendocrine carcinomas NEC G3 (WHO 2010) progressive after first-line chemotherapy (AVENEC). Journal of Clinical Oncology 37(15_suppl) 4103. ( 10.1200/JCO.2019.37.15_suppl.4103) [DOI] [Google Scholar]
- Frilling A Sotiropoulos GC Li J Kornasiewicz O & Plockinger U. 2010Multimodal management of neuroendocrine liver metastases. HPB (Oxford) 12361–379. ( 10.1111/j.1477-2574.2010.00175.x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frumovitz M Munsell MF Burzawa JK Byers LA Ramalingam P Brown J & Coleman RL. 2017Combination therapy with topotecan, paclitaxel, and bevacizumab improves progression-free survival in recurrent small cell neuroendocrine carcinoma of the cervix. Gynecologic Oncology 14446–50. ( 10.1016/j.ygyno.2016.10.040) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimori N, Osoegawa T, Lee L, Tachibana Y, Aso A, Kubo H, Kawabe K, Igarashi H, Nakamura K, Oda Y, et al. 2016Efficacy of endoscopic ultrasonography and endoscopic ultrasonography-guided fine-needle aspiration for the diagnosis and grading of pancreatic neuroendocrine tumors. Scandinavian Journal of Gastroenterology 51245–252. ( 10.3109/00365521.2015.1083050) [DOI] [PubMed] [Google Scholar]
- Galleberg RB, Knigge U, Tiensuu Janson E, Vestermark LW, Haugvik SP, Ladekarl M, Langer SW, Gronbaek H, Osterlung P, Hjortland GO, et al. 2017Results after surgical treatment of liver metastases in patients with high-grade gastroenteropancreatic neuroendocrine carcinomas. European Journal of Surgical Oncology 431682–1689. ( 10.1016/j.ejso.2017.04.010) [DOI] [PubMed] [Google Scholar]
- Garcia-Carbonero R Anton-Pascual B Modrego A Riesco-Martinez MDC Lens-Paardo A Carretero-Puche C Rubio-Cuesta B & Soldevilla B. 2023Advances in the treatment of gastroenteropancreatic neuroendocrine carcinomas: are we moving forward? Endocrine Reviews 001–13. ( 10.1210/endrev/bnad006) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Carbonero R, Sorbye H, Baudin E, Raymond E, Wiedenmann B, Niederle B, Sedlackova E, Toumpanakis C, Anlauf M, Cwikla JB, et al. 2016Enets consensus guidelines for high-grade gastroenteropancreatic neuroendocrine tumors and neuroendocrine carcinomas. Neuroendocrinology 103186–194. ( 10.1159/000443172) [DOI] [PubMed] [Google Scholar]
- Gardner GJ Reidy-Lagunes D & Gehrig PA. 2011Neuroendocrine tumors of the gynecologic tract: a society of gynecologic oncology (SGO) clinical document. Gynecologic Oncology 122190–198. ( 10.1016/j.ygyno.2011.04.011) [DOI] [PubMed] [Google Scholar]
- George J, Walter V, Peifer M, Alexandrov LB, Seidel D, Leenders F, Maas L, Muller C, Dahmen I, Delhomme TM, et al. 2018Integrative genomic profiling of large-cell neuroendocrine carcinomas reveals distinct subtypes of high-grade neuroendocrine lung tumors. Nature Communications 9 1048. ( 10.1038/s41467-018-03099-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- George J, Lim JS, Jang SJ, Cun Y, Ozretić L, Kong G, Leenders F, Lu X, Fernández-Cuesta L, Bosco G, et al. 2015Comprehensive genomic profiles of small cell lung cancer. Nature 52447–53. ( 10.1038/nature14664) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerard L, Garcia J, Gauthier A, Lopez J, Durand A, Hervieu V, Lemelin A, Chardon L, Landel V, Gibert B, et al. 2021ctDNA in neuroendocrine carcinoma of gastroenteropancreatic origin or of unknown primary: the CIRCAN-NEC pilot study. Neuroendocrinology 111951–964. ( 10.1159/000512502) [DOI] [PubMed] [Google Scholar]
- Gile JJ Liu AJ McGarrah PW Eiring RA Hobday TJ Starr JS Sonbol MB & Halfdanarson TR. 2021Efficacy of checkpoint inhibitors in neuroendocrine neoplasms: mayo clinic experience. Pancreas 50500–505. ( 10.1097/MPA.0000000000001794) [DOI] [PubMed] [Google Scholar]
- Girard N, Mazieres J, Otto J, Lena H, Lepage C, Egenod T, Smith D, Madelaine J, Geriniere L, El Hajbi F, et al. 2021Nivolumab +/- ipilimumab in pre-treated patients with advanced, refractory pulmonary or gastroenteropancreatic poorly differentiated neuroendocrine tumors (NECs) (GCO-001 NIPINEC). Annals of Oncology 32(Supplement 5) S1283–S1346. [Google Scholar]
- Girardi DM Silva ACB Rego JFM Coudry RA & Riechelmann RP. 2017Unraveling molecular pathways of poorly differentiated neuroendocrine carcinoma of the gastroenteropancreatic system: a systematic review. Cancer Treatment Reviews 5628–35. ( 10.1016/j.ctrv.2017.04.002) [DOI] [PubMed] [Google Scholar]
- Groen HJ Fokkema E Biesma B Kwa B van Putten JW Postmus PE & Smit EF. 1999Paclitaxel and carboplatin in the treatment of small-cell lung cancer patients resistant to cyclophosphamide, doxorubicin, and etoposide: a non-cross-resistant schedule. Journal of Clinical Oncology 17927–932. ( 10.1200/JCO.1999.17.3.927) [DOI] [PubMed] [Google Scholar]
- Guo C Zhuge X Wang Z Wang Q Sun K Feng Z & Chen X. 2019Textural analysis on contrast-enhanced CT in pancreatic neuroendocrine neoplasms: association with WHO grade. Abdominal Radiology 44576–585. ( 10.1007/s00261-018-1763-1) [DOI] [PubMed] [Google Scholar]
- Hadoux J, Afchain P, Walter T, Tougeron D, Hautefeuille V, Monterymard C, Lorgis V, Thuillier F, Baudin E, Scoazec JY, et al. 2021FOLFIRINEC: a randomized phase II trial of mFOLFIRINOX vs platinum-etoposide for metastatic neuroendocrine carcinoma of gastroenteropancreatic or unknown origin. Digestive and Liver Disease 53824–829. ( 10.1016/j.dld.2021.04.016) [DOI] [PubMed] [Google Scholar]
- Hadoux J, Malka D, Planchard D, Scoazec JY, Caramella C, Guigay J, Boige V, Leboulleux S, Burtin P, Berdelou A, et al. 2015Post-first-line FOLFOX chemotherapy for grade 3 neuroendocrine carcinoma. Endocrine-Related Cancer 22289–298. ( 10.1530/ERC-15-0075) [DOI] [PubMed] [Google Scholar]
- Hainsworth JD Spigel DR Litchy S & Greco FA. 2006Phase II trial of paclitaxel, carboplatin, and etoposide in advanced poorly differentiated neuroendocrine carcinoma: a Minnie Pearl Cancer Research Network Study. Journal of Clinical Oncology 243548–3554. ( 10.1200/JCO.2005.05.0575) [DOI] [PubMed] [Google Scholar]
- Haugvik SP Janson ET Osterlund P Langer SW Falk RS Labori KJ Vestermark LW Gronbaek H Gladhaug IP & Sorbye H. 2016Surgical treatment as a principle for patients with high-grade pancreatic neuroendocrine carcinoma: a Nordic multicenter comparative study. Annals of Surgical Oncology 231721–1728. ( 10.1245/s10434-015-5013-2) [DOI] [PubMed] [Google Scholar]
- Heetfeld M, Chougnet CN, Olsen IH, Rinke A, Borbath I, Crespo G, Barriuso J, Pavel M, O’Toole D, Walter T, et al. 2015Characteristics and treatment of patients with G3 gastroenteropancreatic neuroendocrine neoplasms. Endocrine-Related Cancer 22657–664. ( 10.1530/ERC-15-0119) [DOI] [PubMed] [Google Scholar]
- Hentic O, Hammel P, Couvelard A, Rebours V, Zappa M, Palazzo M, Maire F, Goujon G, Gillet A, Levy P, et al. 2012FOLFIRI regimen: an effective second-line chemotherapy after failure of etoposide-platinum combination in patients with neuroendocrine carcinomas grade 3. Endocrine-Related Cancer 19751–757. ( 10.1530/ERC-12-0002) [DOI] [PubMed] [Google Scholar]
- Herold N Wappenschmidt B Markiefka B Keupp K Krober S Hahnen E Schmutzler R & Rhiem K. 2018Non-small cell neuroendocrine carcinoma of the ovary in a BRCA2-germline mutation carrier: a case report and brief review of the literature. Oncology Letters 154093–4096. ( 10.3892/ol.2018.7836) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks RJ.2010. a Use of molecular targeted agents for the diagnosis, staging and therapy of neuroendocrine malignancy. Cancer Imaging 10(Spec no A) S83–S91. ( 10.1102/1470-7330.2010.9007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hijioka S, Hosoda W, Matsuo K, Ueno M, Furukawa M, Yoshitomi H, Kobayashi N, Ideda M, Ito T, Nakamori S, et al. 2017Rb loss and KRAS mutation are predictors of the response to platinum-based chemotherapy in pancreatic neuroendocrine neoplasm with grade 3: a Japanese multicenter pancreatic NEN-G3 study. Clinical Cancer Research 234625–4632. ( 10.1158/1078-0432.CCR-16-3135) [DOI] [PubMed] [Google Scholar]
- Hlatky R Suki D & Sawaya R. 2004Carcinoid metastasis to the brain. Cancer 1012605–2613. ( 10.1002/cncr.20659) [DOI] [PubMed] [Google Scholar]
- Hofman MS & Hicks RJ. 2012Changing paradigms with molecular imaging of neuroendocrine tumors. Discovery Medicine 1471–81. [PubMed] [Google Scholar]
- Horn L, Mansfield AS, Szczesna A, Havel L, Krzakowski M, Hochmair MJ, Huemer F, Losonczy G, Johnson ML, Nishio M, et al. 2018First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. New England Journal of Medicine 3792220–2229. ( 10.1056/NEJMoa1809064) [DOI] [PubMed] [Google Scholar]
- Hoskins PJ Swenerton KD Pike JA Lim P Aquino-Parsons C Wong F & Lee N. 2003Small-cell carcinoma of the cervix: fourteen years of experience at a single institution using a combined-modality regimen of involved-field irradiation and platinum-based combination chemotherapy. Journal of Clinical Oncology 213495–3501. ( 10.1200/JCO.2003.01.501) [DOI] [PubMed] [Google Scholar]
- Ishikawa M, Kasamatsu T, Tsuda H, Fukunaga M, Sakamoto A, Kaku T, Nakanishi T, Hasumi Y, Iwata T, Baba T, et al. 2018Prognostic factors and optimal therapy for stages I–II neuroendocrine carcinoma of the uterine cervix: a multi-center retrospective study. Gynecologic Oncology 148139–146. ( 10.1016/j.ygyno.2017.10.027) [DOI] [PubMed] [Google Scholar]
- Janson ET Holmberg L Stridsberg M Eriksson B Theodorsson E Wilander E & Oberg K. 1997Carcinoid tumors: analysis of a prognostic factors and survival in 301 patients from a referral center. Annals of Oncology 8685–690. ( 10.1023/a:1008215730767) [DOI] [PubMed] [Google Scholar]
- Jensen RT Berna MJ Bingham DB & Norton JA. 2008Inherited pancreatic endocrine tumor syndromes: advances in molecular pathogenesis, diagnosis, management, and controversies. Cancer 113(7)(Supplement) 1807–1843. ( 10.1002/cncr.23648) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia R Tan HY & Bai CM. 2017Clinical characteristics and treatment options of patients with G3 gastroenteropancreatic neuroendocrine neoplasms in China. International Journal of Clinical and Experimental Medicine 105300–5306. [Google Scholar]
- Jiao Y, Shi C, Edil BH, de Wilde RF, Klimstra DS, Maitra A, Schulick RD, Tang LH, Wolfgang CL, Choti MA, et al. 2011DAXX/ATRX, MEN1, and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science 3311199–1203. ( 10.1126/science.1200609) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaemmerer D Peter L Lupp A Schulz S Sanger J Prasad V Kulkarni H Haugvik SP Hommann M & Baum RP. 2011Molecular imaging with 68ga-sstr PET/CT and correlation to immunohistochemistry of somatostatin receptors in neuroendocrine tumors. European Journal of Nuclear Medicine and Molecular Imaging 381659–1668. ( 10.1007/s00259-011-1846-5) [DOI] [PubMed] [Google Scholar]
- Katada C, Komori S, Yoshida T, Kawakami S, Watanabe A, Ishido K, Azuma M, Wada T, Hosoda K, Yamashita K, et al. 2020A retrospective study of definitive chemoradiotherapy in patients with resectable small cell neuroendocrine carcinoma of the esophagus. Esophagus 17135–140. ( 10.1007/s10388-019-00686-9) [DOI] [PubMed] [Google Scholar]
- Kayani I Bomanji JB Groves A Conway G Gacinovic S Win T Dickson J Caplin M & Ell PJ. 2008Functional imaging of neuroendocrine tumors with combined PET/CT using 68ga-DOTATATE (DOTA-DPhe1,Tyr3-octreotate) and 18F-FDG. Cancer 1122447–2455. ( 10.1002/cncr.23469) [DOI] [PubMed] [Google Scholar]
- Kennedy AS.2016Hepatic-directed therapies in patients with neuroendocrine tumors. Hematology/Oncology Clinics of North America 30193–207. ( 10.1016/j.hoc.2015.09.010) [DOI] [PubMed] [Google Scholar]
- Khan MS Kirkwood A Tsigani T Garcia-Hernandez J Hartley JA Caplin ME & Meyer T. 2013Circulating tumor cells as prognostic markers in neuroendocrine tumors. Journal of Clinical Oncology 31365–372. ( 10.1200/JCO.2012.44.2905) [DOI] [PubMed] [Google Scholar]
- Klein O, Kee D, Markman B, Michael M, Underhill C, Carlino MS, Jackett L, Lum C, Scott C, Nagrial A, et al. 2020Immunotherapy of ipilimumab and nivolumab in patients with advanced neuroendocrine tumors: a subgroup analysis of the CA209-538 clinical trial for rare cancers. Clinical Cancer Research 264454–4459. ( 10.1158/1078-0432.CCR-20-0621) [DOI] [PubMed] [Google Scholar]
- Klempner SJ, Gershenhorn B, Tran P, Lee TK, Erlander MG, Gowen K, Schrock AB, Morosini D, Ross JS, Miller VA, et al. 2016BRAFV600E mutations in high-grade colorectal neuroendocrine tumors may predict responsiveness to BRAF-MEK combination therapy. Cancer Discovery 6594–600. ( 10.1158/2159-8290.CD-15-1192) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konukiewitz B, Schlitter AM, Jesinghaus M, Pfister D, Steiger K, Segler A, Agaimy A, Sipos B, Zamboni G, Weichert W, et al. 2017Somatostatin receptor expression related to TP53 and RB1 alterations in pancreatic and extrapancreatic neuroendocrine neoplasms with Ki67-index above 20. Modern Pathology 30587–598. ( 10.1038/modpathol.2016.217) [DOI] [PubMed] [Google Scholar]
- Kubota K Okasaki M Minamimoto R Miyata Y Morooka M Nakajima K & Sato T. 2014Lesion-based analysis of (18)F-FDG uptake and (111)In-pentetreotide uptake by neuroendocrine tumors. Annals of Nuclear Medicine 281004–1010. ( 10.1007/s12149-014-0900-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulai F Semiz-Oysu A Demir M Segmen-Yilmaz M & Bukte Y. 2018Role of diffusion-weighted MR imaging in predicting the grade of nonfunctional pancreatic neuroendocrine tumors. Diagnostic and Interventional Imaging 99301–309. ( 10.1016/j.diii.2017.10.012) [DOI] [PubMed] [Google Scholar]
- Lee JM, Lee KB, Nam JH, Ryu SY, Bae DS, Park JT, Kim SC, Cha SD, Kim KR, Song SY, et al. 2008Prognostic factors in FIGO stage IB-IIA small cell neuroendocrine carcinoma of the uterine cervix treated surgically: results of a multi-center retrospective Korean Study. Annals of Oncology 19321–326. ( 10.1093/annonc/mdm465) [DOI] [PubMed] [Google Scholar]
- Lee SM & Sung CO. 2021Comprehensive analysis of mutational and clinicopathologic characteristics of poorly differentiated colorectal neuroendocrine carcinomas. Scientific Reports 11 6203. ( 10.1038/s41598-021-85593-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Lu M, Lu Z, Li Z, Liu Y, Yang L, Li J, Zhang X, Zhou J, Wang X, et al. 2017Irinotecan plus cisplatin followed by octreotide long-acting release maintenance treatment in advanced gastroenteropancreatic neuroendocrine carcinoma: IPO-NEC study. Oncotarget 825669–25678. ( 10.18632/oncotarget.12900) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lithgow K, Venkataraman H, Hughes S, Shah H, Kemp-Blake J, Vickrage S, Smith S, Humphries S, Elshafie M, Taniere P, et al. 2021Well-differentiated gastroenteropancreatic G3 NET: findings from a large single centre cohort. Scientific Reports 11 17947. ( 10.1038/s41598-021-97247-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu AJ Ueberroth BE McGarrah PW Buckner Petty SA Kendi AT Starr J Hobday TJ Halfdanarson TR & Sonbol MB. 2021Treatment outcomes of well-differentiated high-grade neuroendocrine tumors. Oncologist 26383–388. ( 10.1002/onco.13686) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotfalizadeh E Ronot M Wagner M Cros J Couvelard A Vullierme MP Allaham W Hentic O Ruzniewski P & Vilgrain V. 2017Prediction of pancreatic neuroendocrine tumour grade with MR imaging features: added value of diffusion-weighted imaging. European Radiology 271748–1759. ( 10.1007/s00330-016-4539-4) [DOI] [PubMed] [Google Scholar]
- Lu ZH, Li J, Lu M, Zhang XT, Li J, Zhou J, Wang XC, Gong JF, Gao J, Li Y, et al. 2013Feasibility and efficacy of combined cisplatin plus irinotecan chemotherapy for gastroenteropancreatic neuroendocrine carcinomas. Medical Oncology 30 664. ( 10.1007/s12032-013-0664-y) [DOI] [PubMed] [Google Scholar]
- Majala S, Seppanen H, Kemppainen J, Sundstrom J, Schalin-Jantti C, Gullichsen R, Schildt J, Mustonen H, Vesterinen T, Arola J, et al. 2019Prediction of the aggressiveness of non-functional pancreatic neuroendocrine tumors based on the dual-tracer PET/CT. EJNMMI Research 9 116. ( 10.1186/s13550-019-0585-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao R Li K Cai JQ Luo S Turner M Blazer D & Zhao H. 2021Adjuvant chemotherapy versus observation following resection for patients with nonmetastatic poorly differentiated colorectal neuroendocrine carcinomas. Annals of Surgery 274e126–e133. ( 10.1097/SLA.0000000000003562) [DOI] [PubMed] [Google Scholar]
- McGarrah PW Hobday TJ Starr JS Kendi AT Graham RP Sonbol MB & Halfdanarson TR. 2020aEfficacy of somatostatin analog (SSA) monotherapy for well-differentiated grade 3 (G3) gastroenteropancreatic neuroendocrine tumors (NETs). Journal of Clinical Oncology 38617–617. ( 10.1200/JCO.2020.38.4_suppl.617) [DOI] [Google Scholar]
- McGarrah PW Leventakos K Hobday TJ Molina JR Finnes HD Westin GF & Halfdanarson TR. 2020bEfficacy of second-line chemotherapy in extrapulmonary neuroendocrine carcinoma. Pancreas 49529–533. ( 10.1097/MPA.0000000000001529) [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara MG Scoazec JY & Walter T. 2020Extrapulmonary poorly differentiated NECs, including molecular and immune aspects. Endocrine-Related Cancer 27R219–R238. ( 10.1530/ERC-19-0483) [DOI] [PubMed] [Google Scholar]
- McNamara MG, Swain J, Craig Z, Sharma R, Faluyi OO, Wadsley J, Morgan C, Wall LR, Chau I, Reed N, et al. 2022NET-02: a multicenter, randomized, phase II trial of liposomal irinotecan (nal-IRI) and 5-fluorouracil (5-FU)/folic acid or docetaxel as second-line therapy in patients (pts) with progressive poorly differentiated extra-pulmonary neuroendocrine carcinoma (PD-EP-NEC). Journal of Clinical Oncology 164005. [Google Scholar]
- Mebis W Snoeckx A Corthouts B El Addouli H Nicolay S Van Hoyweghen A Spinhoven M & Op de Beeck BO. 2020Correlation between apparent diffusion coefficient value on MRI and histopathologic WHO grades of neuroendocrine tumors. Journal of the Belgian Society of Radiology 104 7. ( 10.5334/jbsr.1925) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng MB, Zaorsky NG, Jiang C, Tian LJ, Wang HH, Liu CL, Wang J, Tao Z, Sun Y, Want J, et al. 2013Radiotherapy and chemotherapy are associated with improved outcomes over surgery and chemotherapy in the management of limited-stage small cell esophageal carcinoma. Radiotherapy and Oncology 106317–322. ( 10.1016/j.radonc.2013.01.008) [DOI] [PubMed] [Google Scholar]
- Metovic J, La Salvia A, Rapa I, Napoli F, Birocco N, Bizzi MP, Garcia-Carbonero R, Ciuffreda L, Scagliotti G, Papotti M, et al. 2022Molecular subtypes of extra-pulmonary neuroendocrine carcinomas identified by the expression of neuroendocrine lineage-specific transcription factors. Endocrine Pathology 33388–399. ( 10.1007/s12022-022-09722-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metz DC & Jensen RT. 2008Gastrointestinal neuroendocrine tumors: pancreatic endocrine tumors. Gastroenterology 1351469–1492. ( 10.1053/j.gastro.2008.05.047) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitry E, Baudin E, Ducreux M, Sabourin JC, Rufie P, Aparicio T, Aparicio T, Lasser P, Elias D, Duvillard P, et al. 1999Treatment of poorly differentiated neuroendocrine tumours with etoposide and cisplatin. British Journal of Cancer 811351–1355. ( 10.1038/sj.bjc.6690325) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuno Y, Kudo A, Akashi T, Akahoshi K, Ogura T, Ogawa K, ono H, Mitsunori Y, Ban D, Tanaka S, et al. 2018Sunitinib shrinks NET-G3 pancreatic neuroendocrine neoplasms. Journal of Cancer Research and Clinical Oncology 1441155–1163. ( 10.1007/s00432-018-2636-2) [DOI] [PubMed] [Google Scholar]
- Moertel CG Kvols LK O’Connell MJ & Rubin J. 1991Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin. Evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer 68227–232. (https://doi.org/10.1002/1097-0142(19910715)68:2<227::aid-cncr2820680202>3.0.co;2-i) [DOI] [PubMed] [Google Scholar]
- Morizane C, Machida N, Honma Y, Okusaka T, Boku N, Kato K, Nomura S, Hiraoka N, Sekine S, Taniguchi H, et al. 2022Effectiveness of etoposide and cisplatin vs irinotecan and cisplatin therapy for patients with advanced neuroendocrine carcinoma of the digestive system: the TOPIC-NEC phase 3 randomized clinical trial. JAMA Oncology 81447–1455. ( 10.1001/jamaoncol.2022.3395) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munker S, Vogelhuber M, Bornschein J, Stroszczynski C, Evert M, Schlitt H, Herr W, Teufel A.2020EpiCO (epirubicin, cyclophosphamide and vincristine) as treatment for extrapulmonary 1483 high-grade neuroendocrine neoplasms. Zeitschrift für Gastroenterologie 58133–136. ( 10.1055/a-1042-6504) [DOI] [PubMed] [Google Scholar]
- Nakakura EK.2018Challenges staging neuroendocrine tumors of the pancreas, jejunum and ileum, and appendix. Annals of Surgical Oncology 25591–593. ( 10.1245/s10434-017-602609) [DOI] [PubMed] [Google Scholar]
- Nakano K Takahashi S Yuasa T Nishimura N Mishima Y Sakajiri S Yokoyama M Tsuyama N Ishikawa Y & Hatake K. 2012Feasibility and efficacy of combined cisplatin and irinotecan chemotherapy for poorly differentiated neuroendocrine carcinomas. Japanese Journal of Clinical Oncology 42697–703. ( 10.1093/jjco/hys085) [DOI] [PubMed] [Google Scholar]
- Nasu K Hirakawa T Okamoto M Nishida M Kiyoshima C Matsumoto H Takai N & Narahara H. 2011Advanced small cell carcinoma of the uterine cervix treated by neoadjuvant chemotherapy with irinotecan and cisplatin followed by radical surgery. Rare Tumors 3 e6. ( 10.4081/rt.2011.e6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okita NT, Kato K, Takahari D, Hirashima Y, Nakajima TE, Matsubara J, Hamaguchi T, Yamada Y, Shimada Y, Taniguchi H, et al. 2011Neuroendocrine tumors of the stomach: chemotherapy with cisplatin plus irinotecan is effective for gastric poorly-differentiated neuroendocrine carcinoma. Gastric Cancer 14161–165. ( 10.1007/s10120-011-0025-5) [DOI] [PubMed] [Google Scholar]
- Okuma HS Iwasa S Shoji H Takashima A Okita N Honma Y Kato K Hamaguchi T Yamada Y & Shimada Y. 2014Irinotecan plus cisplatin in patients with extensive-disease poorly differentiated neuroendocrine carcinoma of the esophagus. Anticancer Research 345037–5041. [PubMed] [Google Scholar]
- Olevian DC Nikiforova MN Chiosea S Sun W Bahary N Kuan SF & Pai RK. 2016Colorectal poorly differentiated neuroendocrine carcinomas frequently exhibit BRAF mutations and are associated with poor overall survival. Human Pathology 49124–134. ( 10.1016/j.humpath.2015.11.004) [DOI] [PubMed] [Google Scholar]
- Olsen IH Knigge U Federspiel B Hansen CP Skov A Kjaer A & Langer SW. 2014Topotecan monotherapy in heavily pretreated patients with progressive advanced stage neuroendocrine carcinomas. Journal of Cancer 5628–632. ( 10.7150/jca.9409) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen DH, Alexander AJ, Konda B, Wei L, Hemminger JA, Schmidt CR, Abdel-Misih SRZ, Dillhoff ME, Sipos JA, Kirschner LS, et al. 2017Combination therapy with capecitabine and temozolomide in patients with low and high grade neuroendocrine tumors, with an exploratory analysis of O(6)-methylguanine DNA methyltransferase as a biomarker of response. Oncotarget 8104046–104056. ( 10.18632/oncotarget.22001) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panagiotidis E, Alshammari A, Michopoulou S, Skoura E, Naik K, Maragkoudakis E, Mohmaduvesh M, Al-Harbi M, Belda M, Caplin ME, et al. 2017Comparison of the impact of 68ga-DOTATATE and 18F-FDG PET/CT on clinical management in patients with neuroendocrine tumors. Journal of Nuclear Medicine 5891–96. ( 10.2967/jnumed.116.178095) [DOI] [PubMed] [Google Scholar]
- Panagiotidis E & Bomanji J. 2014Role of 18F-fluorodeoxyglucose PET in the study of neuroendocrine tumors. PET Clinics 943–55. ( 10.1016/j.cpet.2013.08.008) [DOI] [PubMed] [Google Scholar]
- Panzuto F Finzivillo M Spada F Antonuzzo L Ibrahim T Campana D Fazio N & Delle Fave G. 2017Everolimus in pancreatic neuroendocrine carcinomas G3. Pancreas 46302–305. ( 10.1097/MPA.0000000000000762) [DOI] [PubMed] [Google Scholar]
- Partelli S Rinzivillo M Maurizi A Panzuto F Salgarello M Polenta V Delle Fave G & Falconi M. 2014The role of combined Ga-DOTANOC and (18)FDG PET/CT in the management of patients with pancreatic neuroendocrine tumors. Neuroendocrinology 100293–299. ( 10.1159/000368609) [DOI] [PubMed] [Google Scholar]
- Patel SP, Mayerson E, Chae YK, Strosberg J, Wang J, Konda B, Hayward J, McLeod CM, Chen HX, Sharon E, et al. 2021A phase II basket trial of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors (DART) SWOG S1609: high-grade neuroendocrine neoplasm cohort. Cancer 1273194–3201. ( 10.1002/cncr.33591) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SP, Othus M, Chae YK, Giles FJ, Hansel DE, Singh PP, Fontaine A, Shah MH, Kasi A, Baghdadi TA, et al. 2020A phase II basket trial of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors (DART SWOG 1609) in patients with nonpancreatic neuroendocrine tumors. Clinical Cancer Research 262290–2296. ( 10.1158/1078-0432.CCR-19-3356) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavel M & de Herder WW. 2017Enets consensus guidelines for the standard of care in neuroendocrine tumors. Neuroendocrinology 105193–195. ( 10.1159/000457957) [DOI] [PubMed] [Google Scholar]
- Pavel M, O’Toole D, Costa F, Capdevila J, Gross D, Kianmanesh R, Krenning E, Knigge U, Salazar R, Pape UF, et al. 2016Enets consensus guidelines update for the management of distant metastatic disease of intestinal, pancreatic, bronchial neuroendocrine neoplasms (NEN) and NEN of unknown primary site. Neuroendocrinology 103172–185. ( 10.1159/000443167) [DOI] [PubMed] [Google Scholar]
- Pavel M, Oberg K, Falconi M, Krenning EP, Sundin A, Perren A, Berruti A. & ESMO Guidelines Committee 2020Gastroenteropancreatic neuroendocrine neoplasms: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Annals of Oncology 31844–860. ( 10.1016/j.annonc.2020.03.304) [DOI] [PubMed] [Google Scholar]
- Pavel M, Valle JW, Eriksson B, Rinke A, Caplin M, Chen J, Costa F, Falkerby J, Fazio N, Gorbounova V, et al. 2017Enets consensus guidelines for the standards of care in neuroendocrine neoplasms: systemic therapy-biotherapy and novel targeted agents. Neuroendocrinology 105266–280. ( 10.1159/000471880) [DOI] [PubMed] [Google Scholar]
- Paz-Ares L, Dvorkin M, Chen Y, Reinmuth N, Hotta K, Trukhin D, Statsenko G, Hochmair MJ, Ozguroglu M, Ji JH, et al. 2019Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (Caspian): a randomized, controlled, open-label, phase 3 trial. Lancet 3941929–1939. ( 10.1016/S0140-6736(1932222-6)31590988 [DOI] [Google Scholar]
- Pei X Xiang L Ye S He T Cheng Y Yang W Wu X & Yang H. 2017Cycles of cisplatin and etoposide affect treatment outcomes in patients with FIGO stage I–II small cell neuroendocrine carcinoma of the cervix. Gynecologic Oncology 147589–596. ( 10.1016/j.ygyno.2017.09.022) [DOI] [PubMed] [Google Scholar]
- Pellat A, Dreyer C, Couffignal C, Walter T, Lombard-Bohas C, Niccoli P, Seitz JF, Hentic O, Andre T, Coriat R, et al. 2018Clinical and biomarker evaluations in sunitinib in patients with grade 3 digestive neuroendocrine neoplasms. Neuroendocrinology 10724–31. ( 10.1159/000487237) [DOI] [PubMed] [Google Scholar]
- Pellat A, Walter T, Augustin J, Hautefeuille V, Hentic O, Do Cao C, Lievre A, Coriat R, Hammel P, Dubreuil O, et al. 2020Chemotherapy in resected neuroendocrine carcinomas of the digestive tract: a national study from the French group of endocrine tumors. Neuroendocrinology 110404–412. ( 10.1159/000502825) [DOI] [PubMed] [Google Scholar]
- Phan AT Wolin EM Liyanage N Mirakhur B & Pitman SW. 2017Elevated levels of 5-HIAA and CgA in patients with pancreatic neuroendocrine tumors (PanNETs): analysis from the CLARINET study. NANETS 2017 Symposium Abstracts C16. [Google Scholar]
- Plante M Gregoire J Renaud MC & Roy M. 2011The vaginal radical trachelectomy: an update of a series of 125 cases and 106 pregnancies. Gynecologic Oncology 121290–297. ( 10.1016/j.ygyno.2010.12.345) [DOI] [PubMed] [Google Scholar]
- Pommergaard HC, Nielsen K, Sorbye H, Federspiel B, Tabaksblat EM, Vestermark LW, Janson ET, Hansen CP, Ladekarl M, Garresori H, et al. 2021Surgery of the primary tumor in 201 patients with high-grade gastroenteropancreatic neuroendocrine and mixed neuroendocrine-non-neuroendocrine neoplasms. Journal of Neuroendocrinology 33 e12967. ( 10.1111/jne.12967) [DOI] [PubMed] [Google Scholar]
- Puccini A, Poorman K, Salem ME, Soldato D, Seeber A, Goldberg RM, Shields AF, Xiu J, Battaglin F, Berger MD, et al. 2020Comprehensive genomic profiling of gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs). Clinical Cancer Research 265943–5951. ( 10.1158/1078-0432.CCR-20-1804) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj N, Coffman K, Le T, Do RKG, Rafailov J, Choi Y, Chou JF, Capanu M, Dunphy M, Fox JJ, et al. 2022Treatment response and clinical outcomes of well differentiated high grade neuroendocrine tumors to lutetium-177 DOTATATE. Neuroendocrinology 1121177–1186. ( 10.1159/000525216) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj N, Shah R, Stadler Z, Mukherjee S, Chou J, Untch B, Li J, Kelly V, Saltz LB, Mandelker D, et al. 2018Real-time genomic characterization of metastatic pancreatic neuroendocrine tumors has prognostic implications and identifies potential germline actionability. JCO Precision Oncology 20181–18. ( 10.1200/PO.17.00267) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramella Munhoz R de Mendonca Rego JF de Celis Ferrari AR Ignez Braghiroli M Mendonca Bariani G Marcelo Hoff P Perego Costa F Eduardo Flesch Pfiffer T & Riechelmann R. 2013Combination of irinotecan and a platinum agent for poorly differentiated neuroendocrine carcinomas. Rare Tumors 5 e39. ( 10.4081/rt.2013.e39) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez PT, Frumovitz M, Pareia R, Lopez A, Vieira M, Ribeiro R, Buda A, Yan X, Shuzhong Y, Chetty N, et al. 2018Minimally invasive versus abdominal radical hysterectomy for cervical cancer. New England Journal of Medicine 3791895–1904. ( 10.1056/NEJMoa1806395) [DOI] [PubMed] [Google Scholar]
- Reidy-Lagunes DL.2012Systemic therapy for advanced pancreatic neuroendocrine tumors: an update. Journal of the National Comprehensive Cancer Network 10777–783. ( 10.6004/jnccn.2012.0077) [DOI] [PubMed] [Google Scholar]
- Rinde G, Mete O, Uccella S, Basturk O, La Rosa S, Brosens LAA, Ezzat S, de Herder WW, Klimstra DS, Papotti M, et al. 2022Overview of the 2022 WHO classification of neuroendocrine neoplasms. Endocrine Pathology 33115–154. ( 10.1007/s12022-022-09708-2) [DOI] [PubMed] [Google Scholar]
- Rizzo FM & Meyer T. 2018Liquid biopsies for neuroendocrine tumors: circulating tumor cells, DNA, and microRNAs. Endocrinology and Metabolism Clinics of North America 47471–483. ( 10.1016/j.ecl.2018.04.002) [DOI] [PubMed] [Google Scholar]
- Rogowski W Wachula E Gorzelak A Lebiedzinska A Sulzyc-Bielicka V Izycka-Swieszewska E Zolnierek J & Kos-Kudla B. 2019Capecitabine and temozolomide combination for treatment of high-grade, well-differentiated neuroendocrine tumour and poorly-differentiated neuroendocrine carcinoma-retrospective analysis. Endokrynologia Polska 70313–317. ( 10.5603/EP.a2019.0010) [DOI] [PubMed] [Google Scholar]
- Rooper LM Sharma R Li QK Illei PB & Westra WH. 2017INSM1 demonstrates superior performance to the individual and combined use of synaptophysin, chromogranin and CD56 for diagnosing neuroendocrine tumors of the thoracic cavity. American Journal of Surgical Pathology 411561–1569. ( 10.1097/PAS.0000000000000916) [DOI] [PubMed] [Google Scholar]
- Roquin G, Baudin E, Lombard-Bohas C, Cadiot G, Dominguez S, Guimbaud R, Niccoli P, Legoux JL, Mitry E, Rohmer V, et al. 2018Chemotherapy for well-differentiated pancreatic neuroendocrine tumours with a Ki-67 index ≥ 10%: is there a more effective antitumour regimen? A retrospective multicentre study of the French group of endocrine tumours (GTE). Neuroendocrinology 10638–46. ( 10.1159/000457955) [DOI] [PubMed] [Google Scholar]
- Rubin J Ajani J Schirmer W Venook AP Bukowski R Pommier R Saltz L Dandona P & Anthony L. 1999Octreotide acetate long-acting formulation versus open-label subcutaneous octreotide acetate in malignant carcinoid syndrome. Journal of Clinical Oncology 17600–606. ( 10.1200/JCO.1999.17.2.600) [DOI] [PubMed] [Google Scholar]
- Sahnane N Furlan D Monti M Romualdi C Vanoli A Vicari E Solcia E Capella C Sessa F & La Rosa S. 2015Microsatellite unstable gastrointestinal neuroendocrine carcinomas: a new clinicopathologic entity. Endocrine-Related Cancer 2235–45. ( 10.1530/ERC-14-0410) [DOI] [PubMed] [Google Scholar]
- Sahu A Jefford M & Hicks RJ. 2018Capecitabine and temozolomide (CAPTEM) for intermediate to high grade metastatic neuroendocrine tumours (NET): a single centre experience. Journal of Clinical Oncology 36e16159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu A Jefford M Lai-Kwon J Thai A Hicks RJ & Michael M. 2019CAPTEM in metastatic well-differentiated intermediate to high grade neuroendocrine tumors: a single centre experience. Journal of Oncology 2019 9032753. ( 10.1155/2019/9032753) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satoh T, Takei Y, Treilleux I, Devouassoux-Shisheboran M, Ledermann J, Viswanathan AN, Mahner S, Provencher DM, Mileshkin L, Avall-Lundqvist E, et al. 2014Gynecologic cancer intergroup (GCIG) consensus review for small cell carcinoma of the cervix. International Journal of Gynecological Cancer 24(Supplement 3) S102–S108. ( 10.1097/IGC.0000000000000262) [DOI] [PubMed] [Google Scholar]
- Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, Becker H, Raab HR, Villanueva MT, Witzigmann H, et al. 2012Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. Journal of Clinical Oncology 301926–1933. ( 10.1200/JCO.2011.40.1836) [DOI] [PubMed] [Google Scholar]
- Scarpa A, Chang DK, Nones K, Corbo V, Patch AM, Bailey P, Lawlor RT, Johns AL, Miller DK, Mafficini A, et al. 2017Whole-genome landscape of pancreatic neuroendocrine tumours. Nature 5436, 5–71. ( 10.1038/nature21063) [DOI] [PubMed] [Google Scholar]
- Schmitz R Mao R Moris D Strickler JH & Blazer DG. 2021Impact of postoperative chemotherapy on the survival of patients with high-grade gastroenteropancreatic neuroendocrine carcinoma. Annals of Surgical Oncology 28114–120. ( 10.1245/s10434-020-08730-0) [DOI] [PubMed] [Google Scholar]
- Shah MH, Goldner WS, Benson AB, Bergsland E, Blaszkowsky LS, Brock P, Chan J, Das S, Dickson PV, Fanta P, et al. 2021Neuroendocrine and adrenal tumors, version 2.2021, National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network 19839–868. ( 10.1038/nature21063) [DOI] [PubMed] [Google Scholar]
- Singhi AD, Liu TC, Roncaioli JL, Cao D, Zeh HJ, Zureikat AH, Tsung A, Marsh JW, Lee KK, Hogg ME, et al. 2017Alternative lengthening of telomeres and loss of DAXX/ATRX expression predicts metastatic disease and poor survival in patients with pancreatic neuroendocrine tumors. Clinical Cancer Research 23600–609. ( 10.1158/1078-0432.CCR-16-1113) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoura E, Michopoulou S, Mohmaduvesh M, Panagiotidis E, Al Harbi M, Toumpanakis C, Almukhailed O, Kayani I, Syed R, Navalkissoor S, et al. 2016The impact of 68ga-DOTATATE PET/CT imaging on management of patients with neuroendocrine tumors: experience from a national referral center in the United Kingdom. Journal of Nuclear Medicine 5734–40. ( 10.2967/jnumed.115.166017) [DOI] [PubMed] [Google Scholar]
- Smith J & Reidy-Lagunes D. 2013The management of extrapulmonary poorly differentiated (high-grade) neuroendocrine carcinomas. Seminars in Oncology 40100–108. ( 10.1053/j.seminoncol.2012.11.011) [DOI] [PubMed] [Google Scholar]
- Smith JD Reidy DL Goodman KA Shia J & Nash GM. 2014A retrospective review of 126 high-grade neuroendocrine carcinomas of the colon and rectum. Annals of Surgical Oncology 212956–2962. ( 10.1245/s10434-014-3725-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon JP, Linkov I, Rosado A, Mullaney K, Rosen EY, Frosina D, Jungbluth AA, Zehir A, Benayed R, Drilon A, et al. 2020NTRK fusion detection across multiple assays and 33,997 cases: diagnostic implications and pitfalls. Modern Pathology 3338–46. ( 10.1038/s41379-019-0324-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonbol MB & Halfdanarson TR. 2019Management of well-differentiated high-grade (G3) neuroendocrine tumors. Current Treatment Options in Oncology 20 74. ( 10.1007/s11864-019-0670-1) [DOI] [PubMed] [Google Scholar]
- Sorbye H, Baudin E, Borbath I, Caplin M, Chen J, Cwikla JB, Frilling A, Grossman A, Kaltsas G, Scarpa A, et al. 2019Unmet needs in high-grade gastroenteropancreatic neuroendocrine neoplasms (WHO G3). Neuroendocrinology 10854–62. ( 10.1159/000493318) [DOI] [PubMed] [Google Scholar]
- Sorbye H Baudin E & Perren A. 2018The problem of high-grade gastroenteropancreatic neuroendocrine neoplasms: well-differentiated neuroendocrine tumors, neuroendocrine carcinomas, and beyond. Endocrinology and Metabolism Clinics of North America 47683–698. ( 10.1016/j.ecl.2018.05.001) [DOI] [PubMed] [Google Scholar]
- Sorbye H, Grande E, Pavel M, Tesselaar M, Fazio N, Simon Reed NS, Knigge U, Christ E, Ambrosini V, Couvelard A, et al. 2023European Neuroendocrine Tumor Society (ENETS) 2023 guidance paper for digestive neuroendocrine carcinoma. Journal of Neuroendocrinology 35 e13249. ( 10.1111/jne.13249) [DOI] [PubMed] [Google Scholar]
- Sorbye H Kong G & Grozinsky-Glasberg S. 2020PRRT in high-grade gastroenteropancreatic neuroendocrine neoplasms (WHO G3). Endocrine-Related Cancer 27R67–R77. ( 10.1530/ERC-19-0400) [DOI] [PubMed] [Google Scholar]
- Sorbye H Strosberg J Baudin E Klimstra DS & Yao JC. 2014Gastroenteropancreatic high-grade neuroendocrine carcinoma. Cancer 1202814–2823. ( 10.1002/cncr.28721) [DOI] [PubMed] [Google Scholar]
- Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P, Dueland S, Hofsli E, Guren MG, Ohrling K, et al. 2013Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the Nordic NEC study. Annals of Oncology 24152–160. ( 10.1093/annonc/mds276) [DOI] [PubMed] [Google Scholar]
- Spitz FR, Abbruzzese JL, Lee JE, Pisters PW, Lowy AM, Fenoglio CJ, Cleary KR, Janjan NA, Goswitz MS, Rich TA, et al. 1997Preoperative and postoperative chemoradiation strategies in patients treated with pancreaticoduodenectomy for adenocarcinoma of the pancreas. Journal of Clinical Oncology 15928–937. ( 10.1200/JCO.1997.15.3.928) [DOI] [PubMed] [Google Scholar]
- Stecklein SR Jhingran A Burzawa J Ramalingam P Klopp AH Eifel PJ & Frumovitz M. 2016Patterns of recurrence and survival in neuroendocrine cervical cancer. Gynecologic Oncology 143552–557. ( 10.1016/j.ygyno.2016.09.011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strosberg J, Mizuno N, Doi T, Grande E, Delord JP, Shapira-Frommer R, Bergsland E, Shah M, Fakih M, Takahashi S, et al. 2020Efficacy and safety of pembrolizumab in previously treated advanced neuroendocrine tumors: results from the phase II KEYNOTE-158 study. Clinical Cancer Research 262124–2130. ( 10.1158/1078-0432.CCR-19-3014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strosberg JR, Coppola D, Klimstra DS, Phan AT, Kulke MH, Wiseman GA, Kvols LK. & North American Neuroendocrine Tumor Society (NANETS) 2010The NANETS consensus guidelines for the diagnosis and management of poorly differentiated (high-grade) extrapulmonary neuroendocrine carcinomas. Pancreas 39799–800. ( 10.1097/MPA.0b013e3181ebb56f) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strosberg JR, Halfdanarson TR, Bellizzi AM, Chan JA, Dillon JS, Heaney AP, Kunz PL, O’Dorisio TM, Salem R, Segelov E, et al. 2017The North American Neuroendocrine Tumor Society consensus guidelines for surveillance and medical management of midgut neuroendocrine tumors. Pancreas 46707–714. ( 10.1097/MPA.0000000000000850) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbiah V, Wolf J, Konda B, Kang H, Spira A, Weiss J, Takeda M, Ohe Y, Khan S, Ohashi K, et al. 2022Tumour-agnostic efficacy and safety of selpercatinib in patients with RET fusion-positive solid tumours other than lung or thyroid tumours (LIBRETTO-001): a phase 1/2, open-label, basket trial. Lancet. Oncology 231261–1273. ( 10.1016/S1470-2045(2200541-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang LH Basturk O Sue JJ & Klimstra DS. 2016aA practical approach to the classification of WHO Grade 3 (G3) well-differentiated neuroendocrine tumor (WD-NET) and poorly differentiated neuroendocrine carcinoma (PD-NEC) of the pancreas. American Journal of Surgical Pathology 401192–1202. ( 10.1097/PAS.0000000000000662) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang LH Untch BR Reidy DL O’Reilly E Dhall D Jih L Basturk O Allen PJ & Klimstra DS. 2016bWell-differentiated neuroendocrine tumors with a morphologically apparent high-grade component: a pathway distinct from poorly differentiated neuroendocrine carcinomas. Clinical Cancer Research 221011–1017. ( 10.1158/1078-0432.CCR-15-0548) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thang SP Lung MS Kong G Hofman MS Callahan J Michael M & Hicks RJ. 2018Peptide receptor radionuclide therapy (PRRT) in European Neuroendocrine Tumor Society (ENETS) grade 3 (G3) neuroendocrine neoplasia (NEN)-a single institution retrospective analysis. European Journal of Nuclear Medicine and Molecular Imaging 45262–277. ( 10.1007/s00259-017-3821-2) [DOI] [PubMed] [Google Scholar]
- Thornblade LW Warner SG Melstrom L Ituarte PHG Chang S Li D Fong Y & Singh G. 2021Does surgery provide a survival advantage in non-disseminated poorly differentiated gastroenteropancreatic neuroendocrine neoplasms? Surgery 1691417–1423. ( 10.1016/j.surg.2021.01.026) [DOI] [PubMed] [Google Scholar]
- Tomimaru Y, Eguchi H, Tatsumi M, Kim T, Hama N, Wada H, Kawamoto K, Kobayashi S, Morii E, Mori M, et al. 2015Clinical utility of 2-[(18)F] fluoro-2-deoxy-D-glucose positron emission tomography in predicting World Health Organization grade in pancreatic neuroendocrine tumors. Surgery 157269–276. ( 10.1016/j.surg.2014.09.011) [DOI] [PubMed] [Google Scholar]
- Toumpanakis C Kim MK Rinke A Bergestuen DS Thirlwell C Khan MS Salazar R & Oberg K. 2014Combination of cross-sectional and molecular imaging studies in the localization of gastroenteropancreatic neuroendocrine tumors. Neuroendocrinology 9963–74. ( 10.1159/000358727) [DOI] [PubMed] [Google Scholar]
- Touzios JG Kiely JM Pitt SC Rilling WS Quebbeman EJ Wilson SD & Pitt HA. 2005Neuroendocrine hepatic metastases: dose aggressive management improve survival? Annals of Surgery 241776–83; discussion 783. ( 10.1097/01.sla.0000161981.58631.ab) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis WD Brambilla E Burke AP Marx A & Nicholson AG, Eds. 2015WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart 4th ed.Lyon: IARC. [DOI] [PubMed] [Google Scholar]
- Tsoukalas N Chatzellis E Rontogianni D Alexandraki KI Boutzios G Angelousi A & Kaltas G. 2017Pancreatic carcinoids (serotonin-producing pancreatic neuroendocrine neoplasms): report of 5 cases and review of the literature. Medicine (Baltimore) 96 e6201. ( 10.1097/MD.0000000000006201) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uccella S La Rosa S Metovic J Marchiori D Scoazec JY Volante M Mete O & Papotti M. 2021Genomics of high-grade neuroendocrine neoplasms: well-differentiated neuroendocrine tumor with high-grade features (G3 NET) and neuroendocrine carcinomas (NEC) of various anatomic sites. Endocrine Pathology 32192–210. ( 10.1007/s12022-020-09660-z) [DOI] [PubMed] [Google Scholar]
- Ueberroth BE Liu AJ Starr JS Hobday TJ Ashman JB Mishra N Bekaii-Saab TS Halfdanarson TR & Sonbol MB. 2021Neuroendocrine carcinoma of the anus and rectum: patient characteristics and treatment options. Clinical Colorectal Cancer 20 e139–e149. ( 10.1016/j.clcc.2020.12.001) [DOI] [PubMed] [Google Scholar]
- Utsumi M Umeda Y Takagi K Takashi K Nobuoka D Yoshida R Shinoura S Dadamori H Yagi T & Fujiwara T. 2015Correlation of computed tomography imaging features and pathological features of 41 patients with pancreatic neuroendocrine tumors. Hepatogastroenterology 62441–446. [PubMed] [Google Scholar]
- van Essen M Sundin A Krenning EP & Kwekkeboom DJ. 2014Neuroendocrine tumours: the role of imaging for diagnosis and therapy. Nature Reviews. Endocrinology 10102–114. ( 10.1038/nrendo.2013.246) [DOI] [PubMed] [Google Scholar]
- Velayoudom-Cephise FL, Duvillard P, Foucan L, Hadoux J, Chougnet CN, Leboulleux S, Malka D, Guigay J, Goere D, Debaere T, et al. 2013Are G3 Enets neuroendocrine neoplasms heterogeneous? Endocrine-Related Cancer 20649–657. ( 10.1530/ERC-13-0027) [DOI] [PubMed] [Google Scholar]
- Venizelos A, Elvebakken H, Perren A, Nikolaienko O, Deng W, Lothe IMB, Couvelard A, Hjortland GO, Sundlov A, Svensson J, et al. 2021The molecular characteristics of high-grade gastroenteropancreatic neuroendocrine neoplasms. Endocrine-Related Cancer 291–14. ( 10.1530/ERC-21-0152) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayvergia N, Dasari A, Deng M, Litwin S, Al-Toubah T, Alpaugh RK, Dotan E, Hall MJ, Ross NM, Runyen MM, et al. 2020Pembrolizumab monotherapy in patients with previously treated metastatic high-grade neuroendocrine neoplasms: joint analysis of two prospective, non-randomised trials. British Journal of Cancer 1221309–1314. ( 10.1038/s41416-020-0775-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanathan AN Deavers MT Jhingran A Ramirez PT Levenback C & Eifel PJ. 2004Small cell neuroendocrine carcinoma of the cervix: outcome and patterns of recurrence. Gynecologic Oncology 9327–33. ( 10.1016/j.ygyno.2003.12.027) [DOI] [PubMed] [Google Scholar]
- Walter T, Lievre A, Coriat R, Malka D, Elhajbi F, Di Fiore F, Hentic O, Smith D, Hautefeuille V, Roquin G, et al. 2023Bevacizumab plus FOLFIRI after failure of platinum-etoposide first-line chemotherapy in patients with advanced neuroendocrine carcinoma (PRODIGE 41-BEVANEC): a randomized, multicentre, non-comparative, open-label, phase 2 trial. Lancet. Oncology 24297–306. ( 10.1016/S1470-2045(2300001-3) [DOI] [PubMed] [Google Scholar]
- Walter T, Tougeron D, Baudin E, Le Malicot K, Lecomte T, Malka D, Hentic O, Menfredi S, Bonnet I, Guimbaud R, et al. 2017Poorly differentiated gastro-entero-pancreatic neuroendocrine carcinomas: are they really heterogeneous? Insights from the FFCD-GTE national cohort. European Journal of Cancer 79158–165. ( 10.1016/j.ejca.2017.04.009) [DOI] [PubMed] [Google Scholar]
- Wang KL, Chang TC, Jung SM, Chen CH, Cheng YM, Wu HH, Liou WS, Hsu ST, Ou YC, Yeh LS, et al. 2012Primary treatment and prognostic factors of small cell neuroendocrine carcinoma of the uterine cervix: a Taiwanese Gynecologic Oncology Group study. European Journal of Cancer 481484–1494. ( 10.1016/j.ejca.2011.12.014) [DOI] [PubMed] [Google Scholar]
- Welin S Sorbye H Sebjornsen S Knappskog S Busch C & Oberg K. 2011Clinical effect of temozolomide-based chemotherapy in poorly differentiated endocrine carcinoma after progression on first-line chemotherapy. Cancer 1174617–4622. ( 10.1002/cncr.26124) [DOI] [PubMed] [Google Scholar]
- Wong RK Jang R & Darling G. 2015Postoperative chemoradiotherapy vs. preoperative chemoradiotherapy for locally advanced (operable) gastric cancer: clarifying the role and technique of radiotherapy. Journal of Gastrointestinal Oncology 689–107. ( 10.3978/j.issn.2078-6891.2014.089) [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization 2019Diges tive System Tumours: WHO Classification of Tumours (Medicine), 5th ed. [Google Scholar]
- Yachida S, Totoki Y, Noe M, Nakatani Y, Horie M, Kawasaki K, Nakamura H, Saito-Adachi M, Suzuki M, Takai E, et al. 2022Comprehensive genomic profiling of neuroendocrine carcinomas of the gastrointestinal system. Cancer Discovery 12692–711. ( 10.1158/2159-8290.CD-21-0669) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yachida S, Vakiani E, White CM, Zhong Y, Saunders T, Morgan R, de Wilde RF, Maitra A, Hicks J, Demarzo AM, et al. 2012Small cell and large cell neuroendocrine carcinomas of the pancreas are genetically similar and distinct from well-differentiated pancreatic neuroendocrine tumors. American Journal of Surgical Pathology 36173–184. ( 10.1097/PAS.0b013e3182417d36) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaguchi T, Machida N, Morizane C, Kasuga A, Takahashi H, Sudo K, Nishina T, Tobimatsu K, Ishido K, Furuse J, et al. 2014Multicenter retrospective analysis of systemic chemotherapy for advanced neuroendocrine carcinoma of the digestive system. Cancer Science 1051176–1181. ( 10.1111/cas.12473) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamashita H Nakagawa K Asari T Murakami N Igaki H Okuma K & Ohtomo K. 2009Concurrent chemoradiation alone with curative intent for limited-disease small-cell esophageal cancer in nine Japanese patients. Diseases of the Esophagus 22113–118. ( 10.1111/j.1442-2050.2008.00863.x) [DOI] [PubMed] [Google Scholar]
- Yao JC Eisner MP Leary C Dagohoy C Phan A Rashid A Hassan M & Evans DB. 2007Population-based study of islet cell carcinoma. Annals of Surgical Oncology 143492–3500. ( 10.1245/s10434-007-9566-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshida T, Hijoka S, Hosoda W, Ueno M, Furukawa M, Kobayashi N, Ikeda M, Ito T, Kodama Y, Morizane C, et al. 2019Surgery for pancreatic neuroendocrine tumor G3 and carcinoma G3 should be considered separately. Annals of Surgical Oncology 261385–1393. ( 10.1245/s10434-019-07252-8) [DOI] [PubMed] [Google Scholar]
- Zagar TM White RR Willett CG Tyler DS Papavassiliou P Papalezova KT Guy CD Broadwater G Clough RW & Czito BG. 2012Resected pancreatic neuroendocrine tumors: patterns of failure and disease-related outcomes with or without radiotherapy. International Journal of Radiation Oncology, Biology, Physics 831126–1131. ( 10.1016/j.ijrobp.2011.09.041) [DOI] [PubMed] [Google Scholar]
- Zamboni GA Ambrosetti MC Zivelonghi C Lombardo F Butturini G Cingarlini S Capelli P & Mucelli RP. 2017Solid non-functioning endocrine tumors of the pancreas: correlating computed tomography and pathology. HPB (Oxford) 19986–991. ( 10.1016/j.hpb.2017.06.013) [DOI] [PubMed] [Google Scholar]
- Zappa M Abdel-Rehim M Hentic O Vullierme MP Ruszniewski P & Vilgrain V. 2012Liver-directed therapies in liver metastases from neuroendocrine tumors of the gastrointestinal tract. Targeted Oncology 7107–116. ( 10.1007/s11523-012-0219-8) [DOI] [PubMed] [Google Scholar]
- Zatelli MC, Fanciulli G, Malandrino P, Ramundo V, Faggiano A, Colao A. & NIKE Group 2016Predictive factors of response to mTOR inhibitors in neuroendocrine tumours. Endocrine-Related Cancer 23R173–R183. ( 10.1530/ERC-15-0413) [DOI] [PubMed] [Google Scholar]
- Zatelli MC Grossrubatscher EM Guadagno E Sciammarella C Faggiano A & Colao A. 2017Circulating tumor cells and miRNAs as prognostic markers in neuroendocrine neoplasms. Endocrine-Related Cancer 24R223–R237. ( 10.1530/ERC-17-0091) [DOI] [PubMed] [Google Scholar]
- Zavras N Schizas D Machairas N Damaskou V Economopoulos N & Machairas A. 2017Carcinoid syndrome from a carcinoid tumor of the pancreas without liver metastases: a case report and literature review. Oncology Letters 132373–2376. ( 10.3892/ol.2017.5678) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J Kulkarni HR Singh A Niepsch K Muller D & Baum RP. 2019Peptide receptor radionuclide therapy in grade 3 neuroendocrine neoplasms: safety and survival analysis in 69 patients. Journal of Nuclear Medicine 60377–385. ( 10.2967/jnumed.118.215848) [DOI] [PubMed] [Google Scholar]
- Zhang P Li J Li J Zhang X Zhou J Wang X Peng Z Shen L & Lu M. 2020Etoposide and cisplatin versus irinotecan and cisplatin as the first-line ttherapy for patients with advanced, poorly differentiated gastroenteropancreatic neuroendocrine carcinoma: a randomized phase 2 study. Cancer 126(Supplement 9) 2086–2092. ( 10.1002/cncr.32750) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang P Lu M Li J & Shen L. 2018aEfficacy and safety of PD-1 blockade with JS001 in patients with advanced neuroendocrine neoplasms: a non-randomized, open-label, phase Ib trial. Annals of Oncology 29 viii468. ( 10.1093/annonc/mdy293.002) [DOI] [Google Scholar]
- Zhang P Yu J Li J Shen L Li N Zhu H Zhai S Zhang Y Yang Z & Lu M. 2018bClinical and prognostic value of PET/CT imaging with combination of 68ga-DOTATATE and 18F-FDG in gastroenteropancreatic neuroendocrine neoplasms. Contrast Media and Molecular Imaging 2018 2340389. ( 10.1155/2018/2340389) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J Strosberg JR Dropkin E & Strickler JH. 2015Treatment of high-grade metastatic pancreatic neuroendocrine carcinoma with FOLFIRINOX. Journal of Gastrointestinal Cancer 46166–169. ( 10.1007/s12029-015-9689-0) [DOI] [PubMed] [Google Scholar]
- Zivanovic O Leitao MM Park KJ Zhao H Diaz JP Konner J Alektiar K Chi DS Abu-Rustum NR & Aghajanian C. 2009Small cell neuroendocrine carcinoma of the cervix: analysis of outcome, recurrence pattern and the impact of platinum-based combination chemotherapy. Gynecologic Oncology 112590–593. ( 10.1016/j.ygyno.2008.11.010) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a