Summary
Background
Literature is scarce on malocclusion prevalence and orthodontic treatment need (OTN) in subjects with stage III–IV periodontitis. Study aims were to assess prevalence of primary and secondary malocclusions in subjects with stage III–IV periodontitis and OTN based on pathologic tooth migration (PTM) and occlusal trauma of anterior teeth (AT).
Subjects and methods
One hundred and twenty-one subjects with stage III–IV periodontitis were examined. A comprehensive periodontal–orthodontic examination was performed. Exclusion criteria: age <30 years, removable prosthetics, uncontrolled diabetes, pregnancy/lactation, and oncologic disease.
Results
Class II malocclusion was found in 49.6% (Class II div 1—20.7%, Class II div 2—9.9%, subdivision Class II—19.0%), Class I—31.4%, Class III—10.7%, no malocclusion—8.3% of subjects. PTM was observed in 74.4% of maxillary and 60.3% of mandibular AT. Spacing and extrusion were the main types of PTM of AT. Odds ratio for PTM of maxillary AT was 9.3 in cases with >30% of sites with clinical attachment loss ≥5 mm (P = 0.001). Spacing of maxillary AT was influenced by periodontitis, Class III malocclusion, and lost teeth. Tongue habit had impact on spacing of mandibular AT. Dental Health Component of Index of Orthodontic Treatment Need yielded that OTN was found in >50% and OTN due PTM, occlusal trauma and impaired function in 66.1% of subjects.
Conclusions
The most prevalent malocclusion was Class II. Spacing and extrusion were prevalent types of PTM of AT. OTN was found in more than half of the subjects. The study highlights the need for preventive measures for PTM in subjects with stage III–IV periodontitis.
Introduction
Periodontitis is a chronic, plaque-induced, inflammatory disease leading to the deterioration of tooth-supporting tissues (1). The disease results from the imbalance between plaque bacteria and the host immune response (2). Familial anamnesis, systemic health disturbances (e.g. diabetes), behavioural and environmental risk factors such as smoking and diet and decreased immune regulation due to ageing have been described as predispositions to increased susceptibility to the disease (3–8). Local factors, such as ‘hanging’ dental restorations and occlusal trauma, have been found to be associated with deeper probing depths and poorer periodontal prognosis (9, 10). There is an on-going debate in the literature that malocclusion may have a co-destructive influence on the disease progression; however, due to the lack of evidence in human clinical studies, the role of occlusion in periodontal disease is still under question (5, 11, 12).
Periodontal disease has a prevalence up to 50%, but advanced stages of periodontitis have been found to affect from 7.8 to 9.8% of the adult population (13, 14).
A new case definition of periodontitis (staging and grading) was introduced in 2017 based on interdental clinical attachment loss (CAL), alveolar bone loss, number of lost teeth due to periodontitis, and the rate of progression of the disease (15, 16). Periodontitis stages I and II are initial, not exceeding CAL of 5 mm, probing pocket depth (PPD) up to 6 mm and no tooth loss. Periodontitis stages III and IV include the more severe cases of the disease with greater CAL (≥5 mm), greater probing depths (≥6 mm), horizontal and vertical alveolar bone defects and furcation involvement, together with numbers of teeth lost due to periodontitis. Periodontitis grade describes the rate (slow, moderate, and rapid) of progression modified by factors such as cigarette smoking, metabolic control of diabetes, and age (in relation to bone loss) (15, 16). Loss of posterior teeth and decreased height of posterior occlusion, increased numbers of teeth with CAL loss, pathologic migration of anterior teeth, impaired function, and worsened smile aesthetics are the main consequences of the disease (17, 18). Furthermore, impaired chewing function and poor smile aesthetics lead to poor quality of life and impaired physical and psychosocial well-being and are the common reasons for most patients to seek treatment (18–21).
Treatment of subjects with stage III–IV periodontitis and secondary malocclusions is complex, including a team approach (17, 22, 23). Orthodontic treatment (OT) is more often included in the multidisciplinary treatment for adult patients with stage III–IV periodontitis due to impaired smile aesthetics, functional problems, or as an adjunctive treatment prior to prosthetic rehabilitation. Sometimes, orthodontic therapy is the only choice for the conservative rehabilitation of occlusion, function, and aesthetics in subjects with stage III–IV periodontitis (5, 24, 25). A questionnaire study showed that patients do not have enough information about OT possibilities for full occlusal rehabilitation, which can probably be explained by the lack of knowledge in the dental community (26). Interestingly, a large percentage of subjects who had undergone orthodontic consultation was willing to undergo combined periodontal–orthodontic treatment to preserve natural dentition (26).
The effect of orthodontic tooth movement on changes in periodontal tissues in subjects with advanced stages of periodontitis has been studied in numerous clinical studies, where improvement of periodontal parameters, alveolar bone changes, and some risk for external root resorption have been reported (27–30). Alternative treatment options, such as splinting of teeth and occlusal adjustment, have also been described. However, those alternatives are often not suitable for the advanced stages of periodontitis with severe migration of teeth (31). Full mouth prosthetic rehabilitation, usually with multiple extractions of hopeless teeth, tooth or implant-supported prosthesis, has also been described as an alternative to OT. Interestingly, implants, which were often used for substitution of teeth with poor periodontal prognosis, have now discovered to have a high risk of peri-implantitis, especially in subjects with periodontitis (32, 33). Therefore, with its benefits of preservation of natural dentition and its positive effect on tooth surrounding tissues and management of pathologic tooth migration (PTM), OT, even in advanced stages of periodontitis, is becoming increasingly popular both among patients and dentists.
Although the phenomenon of PTM is well described, the literature is scarce on the prevalence of primary and secondary malocclusions in stage III–IV periodontitis and the nature of tooth migration in different sagittal malocclusions. The role of occlusal interferences and oral habits in the aetiology of PTM is also scarcely studied, even though these factors are often observed in subjects with advanced stages of periodontitis (22, 34, 35). The need for OT in stage III–IV periodontitis is unknown.
The aim of the present cross-sectional study was to assess the prevalence of primary and secondary malocclusions in subjects with stage III–IV periodontitis. The secondary aim was to assess OT need based on malocclusions, PTM, and occlusal trauma of anterior teeth.
Materials and methods
Approval by the Regional Ethical Review Board, Kaunas, Lithuania, was obtained (No. BE-2-111; 2019-12-20). The study followed the ethical principles of declaration of Helsinki and STROBE guidelines for cross-sectional studies (36). Detailed oral and written information about the study’s aim and design was provided before the study. All patients signed informed consent to undergo periodontal–orthodontic examination.
Subjects
Selection of subjects was limited to the period of August 2020 to January 2022. Individuals with periodontal disease consecutively attending the Department of Dental and Oral Pathology at the Lithuanian University of Health Sciences (LUHS), Kaunas, Lithuania, were invited to participate in a research study and undergo comprehensive periodontal–orthodontic examination. After signing informed consent forms, subjects were selected according to inclusion and exclusion criteria. Inclusion criteria were: 1. age ≥30 years; 2. diagnosis of periodontitis stage III or IV (15). Exclusion criteria were the following: 1. non-inflammatory periodontal disease; 2. removable prosthetic dental appliances; 3. pregnant or lactating women; 4. uncontrolled diabetes; 5. oncologic disease. Subjects with other systemic diseases were not excluded but carefully recorded.
Periodontal examination
All subjects were clinically examined by an experienced investigator (EZ). The evaluation was performed on the six surfaces around each tooth with a periodontal probe (Hu-Friedy PCP-UNC 15, Chicago, Illinois, USA). The data were recorded in periodontal charts for the study. The following measurements were recorded:
Visible plaque index: evaluated by the presence of dental plaque on the six sites of each tooth [mesiobuccal (MB), buccal (B), distobuccal (DB), mesiolingual (ML), lingual (L), and distolingual (DL)].
Bleeding on probing: recorded bleeding sites immediately after probing.
PPD: measured distance from the gingival margin to the apical portion of the gingival sulcus in millimetres. Data were recorded on all six sites of a tooth (MB, B, DB, ML, L, and DL).
Gingival recession (REC): measured distance from the cementoenamel junction (CEJ) to the gingival margin in millimetres. Data were recorded on all six sites of the tooth (MB, B, DB, ML, L, and DL).
CAL: measured as a distance from the apical portion of the gingival sulcus to the CEJ in millimetres. Data were recorded on all six sites of the tooth (MB, B, DB, ML, L, and DL).
Tooth mobility was assessed by touching the tooth with the index finger on one side and applying a compressive force with an instrument on the other side. Mobility was scored: 1—tooth moves less than 1 mm in the buccolingual or mesiodistal directions, 2—tooth moves 1 mm or more in the buccolingual or mesiodistal directions but does not move in the vertical direction, and 3—tooth moves 1 mm or more in buccolingual or mesiodistal and vertical directions (37).
The number of lost teeth in both dental arches was recorded (the absence of third molars was not considered a loss of teeth) (38). Subjects were grouped according to the number of teeth lost: ≤4 and ≥5 (16).
Assessment of periodontitis stage and grade
Stage and grade of periodontitis were assessed by an experienced periodontist (NB) based on the guidelines of the 2017 World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions (15, 16). Stage III was recorded when: 1. interdental CAL ≥5 mm, 2. tooth loss due to periodontitis ≤4, 3. maximum PPD ≥6 mm, and 4. furcation involvement. Stage IV was recorded when additionally, to stage III, ≥5 teeth were lost due to periodontitis, masticatory dysfunction, secondary occlusal trauma, bite collapse, drifting, and flaring were observed, or less than 20 teeth remained. Periodontitis grade, describing the rate of progression, was adjusted for smoking, diabetes, and age. Grade A (slow rate) was recorded for non-smokers and non-diabetics. Grade B (moderate rate) when smoking <10 cigarettes/day and/or controlled diabetes (blood sugar levels as low as normal using medication); Grade C (rapid rate) when ≥10 cigarettes/day. Subjects with uncontrolled diabetes were not included in the study. Grade C was also recorded for early onset of the periodontitis assessed by bone loss/age ratio (15, 16).
Orthodontic examination
Primary malocclusion—evaluation in maximum intercuspation
Primary malocclusion was assessed on all three planes: sagittal, vertical, and transversal.
Sagittal plane
Sagittal malocclusion was diagnosed according to the canine relationship, because 50.8% of first molars on the right and 45.8% on the left were lost in the subjects of the study sample. The threshold of 2 mm of canine displacement from Class I was used to define Classes II and III (39, 40).
The sagittal incisor relationship was evaluated based on the relation of the mandibular incisor tip and cingulum plateau of the maxillary central incisors. Class I, Class II div 1, Class II div 2, and Class III were defined (39).
-
Overjet (OJ) was measured assessing the horizontal incisors’ relationship (41).
a) Normal OJ—1 to 4 mm;
b) Increased OJ—≥5 mm;
c) Decreased OJ—<1 mm.
Vertical plane
-
Overbite (OB)—vertical OB of incisors (41).
a) Open bite—<0 mm;
b) Normal OB—0–4 mm;
c) Deep bite—≥5 mm.
-
Transversal plane
If present, crossbite (anterior and posterior) was recorded (41).
Primary malocclusion was recorded as follows:
a) No malocclusion—canines in Class I relationship and no vertical, transversal or intra-arch anomalies were observed.
b) Class I malocclusion—canines in a Class I relationship, but vertical and/or transversal or intra-arch anomalies were observed.
c) Class II div 1 malocclusion—canines ≥2 mm Class II, and no retroclination of maxillary incisors was found.
d) Class II div 2 malocclusion—canines ≥2 mm Class II and Class II div 2 relationship of incisors was observed.
e) Class III was recorded—canines were ≥2 mm Class III and/or OJ ≤0 mm.
f) Subdivision Class II—an asymmetric canine relationship (Class II on one side and Class I on the other) was found (42).
Functional occlusal examination
Functional occlusion was assessed by evaluating lower jaw movements during protrusion and laterotrusion. For visualization of occlusal contacts, 8 µm foil was used (43).
a) Protrusion: incorrect guidance was registered if only a single incisor or other teeth than incisors guided. The acceptable/correct anterior guidance path was recorded if two, three, or all four incisors were in contact during lower jaw movement and all posterior teeth were disoccluded (44).
b) Laterotrusion: lateral movement was considered correct if only canines (canine guidance) or lateral teeth (posterior teeth group function) of the working side were in contact during the function. Incorrect lateral guidance was registered when incisors guided or contacts were present on the non-working side (44).
Assessment of occlusal trauma
Anterior teeth with secondary occlusal trauma were recorded when contacts between maxillary and mandibular incisors in maximum intercuspation were detected using 8 µm occlusal foil (43). During maximum intercuspation, anterior teeth either have light contact or are slightly out of contact according to the principles of mutually protected occlusion (44). One more test: fremitus (vibration of the tooth root) was assessed by manual palpation of the labial side of the anterior tooth during clenching to maximum intercuspation (45).
Evaluation of secondary malocclusion
PTM:
The diagnosis of PTM was based on the main complaints of the subject, the presence of occlusal trauma and/or spacing/flaring/extrusion between teeth (35).
1) Isolated spacing was recorded when spaces (≥1 mm) were observed in isolated interdental spaces, mesial or distal to a tooth or teeth that were exposed to occlusal trauma (34).
2) Diastema was recorded as a presence of developing spacing between two central incisors, which was not present in the past or existed but increased (38).
3) Flaring was recorded as multiple spaces between anterior teeth with protrusion caused by labial migration of the teeth (34).
4) Extrusion/overeruption was recorded as migration of a tooth in the incisal direction (34).
Assessment of oral habits
a) Tongue habit was assessed (by an orthodontist EZ) by tongue position at rest and swallow pattern and was registered when both infantile swallowing and inferior tongue position at rest was detected (38, 46).
b) Clenching was registered based on anamnesis and palpation of painful and tensed chewing muscles (47).
c) Bruxism was registered based on self-report, palpation of chewing muscles and the presence of severe tooth attrition and enamel cracks (48).
OT need
The need for OT and occlusal rehabilitation was determined by two experienced orthodontists (authors AS and EZ) and judged in two ways.
Firstly, Dental Health Component (DHC) of Index of Orthodontic Treatment Need (IOTN) was applied for all subjects (49). Very great/great (Grade 5 or 4), borderline (Grade 3), and little/no (Grade 2 or 1) need for OT were registered.
Secondarily, OT need was assessed by clinical assessment of the severity of secondary malocclusion based on occlusal trauma (which could not be treated by alternative methods such as selective grinding), severe PTM (flaring and/or extrusion of anterior teeth) and/or impaired function (15, 50).
Data preparation
Analyses were based on the patient as the unit of measure. Measurement analysis included mean CAL and the percentage of the affected sites by CAL ≥5 mm (≤30, >30%) (51). Patients were grouped by gender (male/female) and age. Age was assessed as a continuous variable. As the prevalence of severe forms of periodontitis has been described to reach its peak at the age 40 years, for this study, we transformed subjects’ age into two categories of age groups (≤40 and >40 years) (52).
Variables were grouped as dependent to be used in a multivariate binary logistic regression analysis model for PTM: sites with CAL ≥5 mm were grouped ≤30/>30%; periodontitis of anterior teeth yes/no based on CAL ≥5 mm; OJ as increased (≥5 mm) and other (<5 mm); and similarly, OB as deep (≥5 mm) and other (<5 mm); and posterior loss of occlusion yes/no. The number of lost teeth was grouped ≤4 and ≥5 (15).
Statistical analysis
Sample size
Sample size was based on the 7.8% prevalence of severe periodontitis (13). To be able to describe this group of adult patients with stage III–IV periodontitis, we aimed to collect 120 patients. The alpha level was set at 5%.
Statistical methods
Statistical analysis was carried out using SPSS software version 27.0 (SPSS Inc, Chicago, Illinois, USA). A P value less than 0.05 was considered significant.
Descriptive statistics were used to describe the characteristics of the study sample. Normality of every data set was checked using a Kolmogorov–Smirnov (BOM) test. When the distribution of variables was normal, a Student’s t-test was used to compare the quantitative sizes of the two independent samples. The Mann–Whitney U and Kruskal–Wallis tests were used to compare non-normally distributed variables. The chi-square test was performed to specify whether the relationship between two categorical variables was statistically significant. The interdependence of qualitative evidence was evaluated by chi-square criteria. Depending on the sample size, exact (for small size) and asymptomatic criteria were used.
Binary associations between variables were evaluated with a non-parametric Spearman or Kendall correlation coefficient. The odds ratio was determined by performing logistic regression.
The Cohen’s kappa coefficient and intraclass correlation coefficient (ICC) were used as a measure of reliability (53).
Reliability of measurements
The clinical attachment level (CAL) was selected for reliability measurements as recommended in the literature on the severity and prevalence of periodontitis (54). The calibration of the principal investigator (EZ) involved a total of 120 repeated measurements performed on 30 teeth, which were performed twice by an orthodontist (EZ) and periodontist (NB) and then compared with each other. The ICC yielded a value of 0.93 [95% confidence interval (CI): 0.87, 0.95: P = 0.0001], and interclass agreement between authors EZ and NB was 0.95 (95% CI: 0.92, 0.96; P = 0.0001).
Periodontist (author NB) calibrated with two other experienced periodontists for assessment of stage and grade. Inter-examiner reliability yielded Cohen’s kappa coefficient of value 0.92 and intra-examiner reliability of 0.97.
Calibration for assessment of PTM was performed by two experienced orthodontists (authors EZ and RL), which resulted in the values of Cohen’s kappa coefficient of 0.81 (for evaluation in maxillary anterior teeth) and 0.87 (for evaluation in mandibular anterior teeth).
Calibration for assessment of OTN according to DHC-IOTN was performed by two experienced orthodontists (authors EZ and AS). Inter-examiner reliability yielded Cohen’s kappa coefficient of value 0.88 and intra-examiner reliability of 0.95.
Any disagreement between the examiners was solved by thorough discussion.
Results
Participant flow
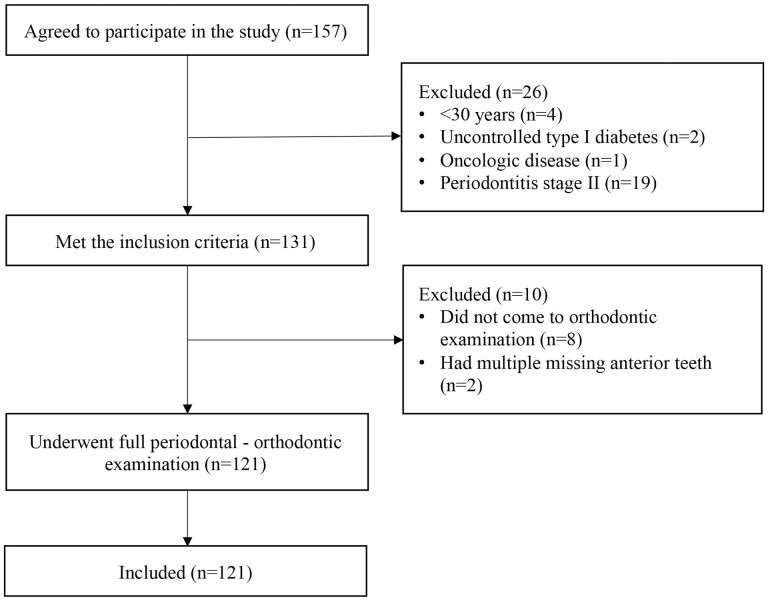
The selection period lasted between August 2020 and January 2022. One hundred and fifty-seven subjects agreed to participate in the study, 131 met the inclusion criteria, but 10 of these needed to be excluded. The flowchart of included patients is presented in Figure 1.
Figure 1.
Flowchart of included subjects.
Baseline data
A total of 121 subjects met the inclusion criteria and participated in the study, 70.2% females and 29.8% males, with a mean age of 46.2 years (95% CI: 44.4; 48.0, range 30–78), and 65.3% of subjects were older than 40 years. Only 62.8% of the subjects were systemically healthy. Cardiovascular diseases were the most prevalent conditions among those with systemic diseases. Systemic diseases mainly (82.2%) were reported in subjects >40 years (P = 0.002), and 20.6% of the subjects were smokers. Full baseline data can be seen in Table 1.
Table 1.
Baseline data of the subjects enrolled in the study.
| Variable | n (%) |
|---|---|
| Total | 121 (100) |
| Gender | |
| Male | 36 (29.8) |
| Female | 85 (70.2) |
| Age (years) | |
| Mean (95% CI) | 46.2 (44.4; 48.0) |
| Range | 30–78 |
| Systemic disease | |
| Endocrine/autoimmune disease | 8 (6.6) |
| Cardiovascular disease | 26 (21.5) |
| Other systemic disease | 11 (9.1) |
| Systemically healthy | 76 (62.8) |
| Smoking status | |
| Smoker ≥10 cigarettes/day | 12 (9.9) |
| Smoker <10 cigarettes/day | 13 (10.7) |
| Non-smoker | 96 (79.4) |
| Previous orthodontic treatment | |
| Yes | 18 (14.9) |
| No | 103 (85.1) |
| Family anamnesis of periodontitis | |
| Yes | 78 (64.5) |
| No | 43 (35.5) |
| Clinical attachment loss (CAL) ≥5 mm | |
| ≤30% sites | 84 (69.4) |
| >30% sites | 37 (30.6) |
| Anterior tooth mobility | |
| Yes | 87 (71.9) |
| No | 34 (28.1) |
| Periodontitis stage | |
| III | 75 (62.0) |
| IV | 46 (38.0) |
| Periodontitis grade | |
| A (slow rate) | 48 (39.7) |
| B (moderate rate) | 21 (17.3) |
| C (rapid rate) | 52 (43.0) |
Results of the periodontal examination
Based on the case definition, the majority of subjects (62.0%), who participated in the study, were diagnosed with stage III periodontitis. An objective clinical examination yielded a mean CAL of 3.5 mm (95% CI: 3.31; 3.70) of included subjects, and 30.6 % of subjects had >30% of sites with CAL ≥5 mm (Table 1). Males were significantly more often found to have >30% of sites with CAL ≥5 mm than females, with an odds ratio of 2.9 [CI: 1.28; 6.63; P = 0.01].
Seventy-six per cent of subjects had at least one maxillary and 66.9% had at least one mandibular anterior teeth with PPD ≥6 mm and/or interdental CAL ≥5 mm. Age had no impact on the severity of periodontitis defined by stage (III or IV) (P = 0.11). However, subjects with age ≤40 years were significantly more (88.1%) likely to have Grade C (rapid progression) periodontitis (P = 0.02). On average, subjects had 2.7 teeth (CI: 2.21; 3.11) lost due to periodontitis. Unilateral posterior tooth loss was observed in 19.8% and bilateral tooth loss in 50.4% of subjects. Subjects >40 years had more than twice as frequent posterior tooth loss (72.0%) compared with subjects ≤40 (28.0%) (P = 0.02).
Evaluation of complaints and malocclusions
The chief complaint of included subjects, who agreed to orthodontic examination, was the deterioration of smile aesthetics (Table 2).
Table 2.
Results of the orthodontic examination.
| Variable | n (%) |
|---|---|
| Complaints | |
| Aesthetics | 44 (36.4) |
| Function (and aesthetics) | 18 (14.9) |
| Referred by the dentist | 31 (25.6) |
| Other/many complaints | 28 (23.1) |
| Canine classification | |
| Class I | 48 (39.7) |
| Class II | 33 (27.3) |
| Class II subdivision | 27 (22.3) |
| Class III | 13 (10.7) |
| Incisor classification | |
| Class I | 68 (56.2) |
| Class II-1 | 27 (22.3) |
| Class II-2 | 12 (9.9) |
| Class III | 14 (11.6) |
| Overjet | |
| <1 mm | 12 (9.9) |
| 1–4 mm | 80 (66.1) |
| ≥5 mm | 29 (24.0) |
| Overbite | |
| <0 mm | 3 (2.5) |
| 0–4 mm | 85 (70.2) |
| ≥5 mm | 33 (27.3) |
| Crossbite | |
| Anterior | 11 (9.1) |
| Posterior | 36 (29.8) |
| Anterior and posterior | 5 (4.1) |
| Scissorsbite | 1 (0.8) |
| Crowding (maxillary) | |
| Yes | 39 (32.2) |
| No | 82 (67.8) |
| Crowding (mandibular) | |
| Yes | 66 (54.5) |
| No | 55 (45.5) |
| Primary malocclusion | |
| Class I | 38 (31.4) |
| Class II-1 | 25 (20.7) |
| Class II-2 | 12 (9.9) |
| Class II subdivision | 23 (19.0) |
| Class III | 13 (10.7) |
| No primary malocclusion | 10 (8.3) |
| Anterior guidance | |
| Incorrect | 99 (81.8) |
| Lateral guidance (right) | |
| Incorrect | 103 (85.1) |
| Lateral guidance (left) | |
| Incorrect | 97 (80.2) |
Analysis of sagittal canine relationship yielded that nearly half (49.6%) of the subjects had Class II malocclusion. However, a large part of them (45.0%) had subdivision II (Class II on one side and Class I on the other). 10.7% of subjects had a canine Class III relationship. Evaluation of sagittal incisor relationship resulted in a Class II div 1 incisor relationship in 22.3% of cases. Interestingly, 63.0% of cases with subdivision II of the canines had a Class I incisor relationship. Examples of malocclusions can be seen in Figure 2.
Figure 2.
Examples of malocclusions in stage III–IV periodontitis. Class I: 1a–c; Class II div 1 with normal overbite (OB): 2a–c; Class II div 1 with severe occlusal trauma: 2d–f; subdivision Class II (asymmetric canine relationship): 2g–i; Class III with no tongue habit: 3a–c; Class III with lost tooth 21, tongue habit and severe pathologic tooth migration (PTM): 3d–f.
After adjusting all parameters for primary malocclusion evaluation, Class II div 1 malocclusion was found in 20.7% of subjects. Data on malocclusions can be seen in Table 2.
Increased OJ (≥5 mm) was found in 24.0% of subjects; deep bite (≥5 mm) was found in 27.3% (n = 33) of subjects. When adjusted for a sagittal canine relationship, increased OJ was found only in 8.3% of Class II div 2 subjects and in 80% of Class II div 1 subjects; deep bite was found in 83.3% of Class II div 2 and 40.0% of Class II div 1 subjects (P = 0.001); open bite was found in only 3 subjects.
Posterior crossbite was found in 29.8% of subjects and was most prevalent in Class II malocclusion (61.1%), followed by Class I (30.6%) and Class III (8.3%).
Proclination of maxillary anterior teeth was observed in 48.8% (n = 59) of cases. Of them, 49.1% were found in Class II malocclusion (27.1% in Class II div 1 and 22.0% in subdivision II). Of all who had proclination (n = 59), 33.9% (n = 20) had lingual gingival recession (GR) on their maxillary central incisors, which was mostly observed together with Class II div 1 malocclusion (77.8%) (P = 0.001).
The percentage of subjects with no primary malocclusion was only 8.3%. Data on malocclusions can be seen in Table 2.
Sagittal canine malocclusion had no impact on the mean CAL either on all teeth (P = 0.63) or maxillary (P = 0.09) or mandibular anterior teeth (P = 0.69). No correlation between >30% or ≤30% of sites affected by CAL ≥5 mm and primary malocclusion was found (P > 0.05). Increased OB (P = 0.04) and OJ (P = 0.04) impacted higher mean CAL loss of maxillary anterior teeth.
Results of functional occlusal examination
More than 80% of subjects had incorrect anterior or lateral guidance (Table 2).
Occlusal trauma
At least one pair of anterior teeth with occlusal trauma was found in 82.6% of study subjects. There was no difference between occlusal trauma prevalence in stage III and IV periodontitis patients—81.3 and 84.8%, respectively (P = 0.63). 81.5 and 84.0% of subjects with periodontitis-affected maxillary and mandibular anterior teeth, respectively, had at least one pair of anterior teeth exposed to occlusal trauma. Occlusal trauma of anterior teeth was not influenced by sagittal malocclusion (P = 0.10), OJ (P = 0.62), OB (P = 0.46), or loss of posterior support of occlusion (P = 0.44).
Secondary malocclusions—PTM
PTM was observed in 74.4% of maxillary and 60.3% of mandibular anterior dentitions and was not affected by age (≤40/>40 years) (P = 0.33 and P = 0.36, respectively), presence/absence of systemic disease (P = 0.51 and P = 0.74, respectively), or smoking/non-smoking (P = 0.22 and P = 0.67). However, PTM of mandibular teeth was found more in men (75.0%) compared with women (54.1%) (P = 0.03).
Two major types of PTM of anterior teeth were recorded—first, more prevalent was spacing, which was found in 56.2% (n = 68) of maxillary and 31.4% (n = 38) of mandibular anterior teeth within included subjects. Second, extrusion (40.5% in maxillary and 38.0% in mandibular) was found either with spacing, which was more prevalent in the maxillary anterior region (20.7% in maxillary versus 9.1% in mandibular) or with crowding, which was more prevalent in the mandibular anterior teeth (28.9% mandibular versus 19.8% maxillary). Interestingly, significantly more subjects with Class III malocclusion had spacing (84.6%), followed by Class I (63.2%) and Class II (46.7%), P = 0.03.
Overeruption of posterior teeth was found in 51.2% of subjects and mostly in cases of lost antagonist teeth.
PTM in maxillary anterior teeth
The mean CAL of maxillary anterior teeth subjects with PTM was significantly greater (3.7 mm) compared with the mean CAL (3.1 mm) of anterior teeth in subjects without PTM (P = 0.04). PTM of maxillary anterior teeth was significantly more often observed in subjects with periodontally affected anterior teeth with CAL ≥5 mm (P = 0.001). Odds ratio for PTM of maxillary anterior teeth was 9.3 [CI: 2.07; 41.12; P = 0.001] in cases of >30% sites with CAL ≥5 mm.
In total, pathological maxillary diastema was observed in 29.7% of the subjects (developing maxillary diastema in 14.0% and diastema had always been present but has been increasing in 15.7%). Of those with periodontitis-affected maxillary anterior teeth (n = 92), 64.1% had spacing (31.5% had isolated interdental spacing and 32.6% flaring). A comparison of secondary malocclusions in periodontitis affected and periodontally healthy anterior teeth is available in Table 3.
Table 3.
Comparison of secondary malocclusions in periodontitis affected and periodontally healthy maxillary and mandibular anterior teeth.
| Secondary malocclusion | Maxillary anterior teeth | Mandibular anterior teeth | ||||
|---|---|---|---|---|---|---|
| Periodontitis affected | Periodontally healthy | P | Periodontitis affected | Periodontally healthy | P | |
| n (%) | n (%) | n (%) | n (%) | |||
| Spacing total | 59 (86.8) | 9 (13.2) | 0.001 | 30 (78.9) | 8 (21.1) | 0.01 |
| Minor | 29 (76.3) | 9 (23.7) | 15 (65.2) | 8 (34.8) | ||
| Flaring | 30 (100) | 0 (0) | 15 (100) | 0 (0) | ||
| No spacing | 33 (62.3) | 20 (37.7) | 51 (61.4) | 32 (38.6) | ||
| Extrusion total | 47 (95.9) | 2 (4.1) | 0.001 | 45 (97.8) | 1 (2.2) | 0.001 |
| Extrusion with spacing | 23 (92.0) | 2 (8.0) | 10 (90.9) | 1 (9.1) | ||
| Extrusion with crowding | 24 (100) | 0 (0) | 35 (100) | 0 (0) | ||
| No extrusion | 45 (62.5) | 27 (37.5) | 36 (48.0) | 39 (52.0) | ||
| Total subjects, n= 121 | n = 92 | n = 29 | n = 81 | n = 40 | ||
Tooth extrusion was mostly registered in cases with periodontitis-affected teeth and occurred both in subjects with spacing and crowding (Table 3).
Crowding of maxillary anterior teeth was observed similarly in subjects with (31.5%) and without (34.5%) signs of periodontitis in the anterior region and was not related to periodontitis (P = 0.47).
PTM in mandibular anterior teeth
The most prevalent type of PTM of anterior teeth in the mandibular dental arch was extrusion, observed in 38.0% of subjects. Notably, extrusion of mandibular anterior teeth more often appeared in periodontitis-affected crowded dental arches than in spaced ones (Table 3). However, there was no extrusion in crowded cases when teeth were periodontally healthy.
Spacing was not observed in 80.0% of subjects with periodontally healthy mandibular anterior teeth. On the contrary, if periodontally affected, 37.1% of subjects had spacing or flaring (P = 0.01).
Diastema in the mandibular anterior region was observed in 7.4% (n = 9) subjects.
Crowding of mandibular anterior teeth was observed similarly in subjects with (56.8%) and without (50.0%) signs of periodontitis in the anterior region and was not related to periodontitis (P = 0.31).
Oral habits
Only 10.4% of subjects had bruxism, and 21.2% had clenching. However, tongue habit was mostly observed (43.2% of subjects). Tongue habit was significantly associated with spacing in the lower anterior region and was observed in 56.8% of subjects with periodontitis-affected mandibular anterior teeth compared with 19.5% with no tongue habit (P = 0.001).
PTM in relation to factors
Factors influencing spacing of anterior teeth:
A bivariate logistic regression analysis yielded the following risk determinants significantly associated with spacing in maxillary anterior teeth: >30% of sites with CAL ≥5 mm (OR = 2.8), periodontitis-affected maxillary anterior teeth (OR = 4.0), number of lost teeth ≤4 (OR = 4.1) or ≥5 (OR = 6.9), posterior loss of occlusion (OR = 2.7), and Class III malocclusion (OR = 4.9). Risk determinants associated with spacing in mandibular anterior teeth included: number of lost teeth (OR = 3.5 if ≤4, and OR = 6.2 if ≥5 teeth lost), posterior loss of occlusion (OR = 3.9), Class III malocclusion (OR = 6.6), and tongue habit (OR = 5.7) (Table 4).
Table 4.
Results of the bivariate logistic regression analysis for risk association of spacing in maxillary and mandibular anterior teeth.
| Risk determinants | Spacing in maxillary anterior teeth | Spacing in mandibular anterior teeth | ||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Clinical attachment loss (CAL) ≥5 mm | ||||
| ≤30% sites | 1.0 | 1.0 | ||
| >30% sites | 2.8 (1.2; 6.6) | 0.01 | 1.1 (0.5; 2.5) | 0.87 |
| Periodontitis in anterior teeth | ||||
| Periodontally healthy | 1.0 | 1.0 | ||
| Periodontitis affected (CAL ≥5 mm) | 4.0 (1.6; 9.7) | 0.002 | 2.4 (1.0; 5.8) | 0.58 |
| Number of lost teeth | ||||
| No loss | 1.0 | 1.0 | ||
| ≤4 teeth | 4.1 (1.6; 10.3) | 0.003 | 3.5 (1.1; 11.3) | 0.03 |
| ≥5 teeth | 6.9 (2.1; 23.3) | 0.002 | 6.2 (1.6; 23.4) | 0.007 |
| Posterior loss of occlusion | ||||
| No loss | 1.0 | 1.0 | ||
| Unilateral/bilateral | 2.7 (1.2; 6.1) | 0.01 | 3.9 (1.4; 11.1) | 0.007 |
| Class III canine malocclusion | ||||
| Class I/Class II | 1.0 | 1.0 | ||
| Class III | 4.9 (1.0; 23.1) | 0.04 | 6.6 (1.9; 23.2) | 0.003 |
| Tongue habit | ||||
| No | 1.0 | 1.0 | ||
| Yes | 1.5 (0.7; 3.1) | 0.30 | 5.7 (2.5; 13.2) | 0.001 |
Spacing in maxillary anterior teeth was not associated with tongue habit (Table 4), increased OJ (P = 0.90) and deep OB (P = 0.82), incorrect anterior guidance (P = 0.86), incorrect lateral (right and left) guidance (P = 0.65 and P = 0.82, respectively), and occlusal trauma (P = 0.92). In mandibular anterior teeth, no association was found between spacing and increased OJ (P = 0.34), deep OB (P = 0.55), incorrect anterior guidance (P = 0.64), incorrect lateral (right and left) guidance (P = 0.85 and P = 0.82, respectively), and occlusal trauma (P = 0.83).
Analysis showed multicollinearity between the loss of posterior support of the occlusion and number of lost teeth (r = 0.9, P = 0.001); therefore, we decided to test the number of lost teeth (≤4/≥5). Finally, sagittal malocclusion, periodontitis of anterior teeth and the number of lost teeth were tested.
Multivariate logistic regression yielded (overall percentage of the model, 68.6%) a higher odds ratio for spacing of maxillary anterior teeth, if they were periodontitis affected [OR 3.3; 95% CI: 1.29; 8.37, P = 0.01], had missing teeth [if ≤4 teeth missing—OR 3.6; 95% CI: 1.41; 9.39, P = 0.008 and OR 5.7; 95% CI: 1.64; 19.68, P = 0.006 if missing ≥5 teeth] and Class III malocclusion [OR 5.7; CI: 1.1; 28.8, P = 0.03].
For spacing of mandibular anterior teeth, a logistic regression model included sagittal malocclusion of canines and tongue habit. Multivariate logistic regression yielded (overall percentage of the model, 73.9%) a higher odds ratio for spacing of mandibular anterior teeth in subjects with Class III malocclusion [OR 6.9; 95% CI: 1.77; 26.91, P = 0.005] and tongue habit [OR 5.05; 95% CI: 2.02; 12.63, P = 0.001].
Factors influencing extrusion of anterior teeth:
The same factors as for spacing were tested for extrusion of anterior teeth; however, the odds ratio for extrusion was found only if the anterior teeth were affected by periodontitis [OR 14.1; 95% CI: 3.2; 62.8; P = 0.03] and if >30% of sites were affected by CAL ≥5 mm [OR 2.6; 95% CI: 1.19; 5.81, P = 0.016].
A bivariate logistic regression analysis did not show previous OT as a risk determinant for PTM of maxillary (P = 0.35) or mandibular (P = 0.33) anterior teeth.
OT need
According to DHC of IOTN, very great OT need (Grade 5) was judged for 9.1%, great (Grade 4) for 49.6% and moderate (Grade 3) for 21.5% of subjects. 76.9% of subjects with Class III, 68.3% with Class II, and 44.7% with Class I malocclusion were judged to have great or very great OT need (Grade 4 or 5) (P = 0.55).
When assessed for secondary malocclusions (PTM, severe occlusal trauma, and/or impaired function), as many as 66.1% (n = 80) of subjects were judged in need of OT (91.3% of stage IV and 50.7% of stage III). Sixty per cent (n = 48) of them agreed to undergo OT. When OT need due to secondary malocclusions was analysed in sagittal malocclusions, subjects with Class III malocclusion needed treatment the most (92.3%) compared with Class II (73.3%) and Class I (55.3%) (P = 0.03).
Comparing both methods (DHC-IOTN and clinical assessment of secondary malocclusions), all subjects of DHC-IOTN Grade 5, 80.0% of subjects of Grade 4 and 53.8% of Grade 3 also needed OT due to secondary malocclusion. Subjects with Class II or III malocclusions needed orthodontic correction significantly more often, based on both assessment methods, DHC-IOTN [OR 3.3; CI: 1.20; 9.14, P = 0.02] and secondary malocclusions [OR 2.7; CI: 1.15; 6.17, P = 0.02] compared with subjects with Class I malocclusion.
Limitations
Despite the relatively high number of subjects who agreed to participate in the study during the study period, 23% (n = 36) of them needed to be excluded (Figure 1). We aimed to collect special data on subjects ≥30 years and advanced stages of periodontitis, which has been reported to be between 7.8 and 9.8% of the adult population (13, 14). Most of the other studies usually include younger subjects (cut-off age of 17–18 years), and all stages (I–IV) of periodontitis severity in order to increase the sample size (35, 55). The low prevalence of the disease and the Covid-19 pandemic could have influenced the number of included participants in the present study. We observed that subjects, who declined to participate during an initial consultation, were afraid to be infected with Covid-19 during the additional appointment, which was needed to perform a full periodontal–orthodontic evaluation. So, during the course of the study, it was decided to perform a full periodontal and orthodontic examination at the same time as the consultation. This decision increased the rate of positive response.
One of the limitations was that X-rays, due to ethical reasons, were not performed for all included subjects. Therefore, for some subjects, grading of periodontitis was performed based on other valid clinical parameters listed in the guidelines (16).
One more limitation was that Angle classification of malocclusion was not applicable due to the large percentage of lost first molars (due to periodontitis), and therefore, primary malocclusion was based on the sagittal relationship of canines and incisors.
Discussion
The present study is the first cross-sectional study analysing orthodontic anomalies in all three planes of space in subjects with stage III–IV periodontitis. The research is in high demand due to vastly increasing interest in OT by both dentists and patients, as shown in the literature (26). However, there is a lack of data on malocclusion prevalence and also influencing factors. The present study included not only periodontal but also orthodontic evaluation, including assessment of primary and secondary malocclusions. Stage IV periodontitis, which was found in 38% of the included subjects, is a particularly severe advanced form of the disease that, if not treated, leads to several or multiple tooth losses, secondary occlusal trauma and drifting and flaring of teeth. More importantly, implants, which are often used to replace lost teeth, have been shown to have a high risk for the development of peri-implantitis in subjects with periodontitis (56). Therefore, timely periodontal treatment is essential for saving natural teeth. Malocclusions have been described as co-destructive factors on the faster progression of CAL (11, 12, 57).
In the present study, canine and incisor relationship was used for the final judgement of primary malocclusion as the majority of first molars on both sides had already been lost. The results yielded that Class II malocclusion was observed in 49.6% of subjects.
Class II div 1 was found in only 21% of included subjects, which is similar to the adolescent population; however, increased OJ was 80% and deep bite (OB) was only 40% of them (41). A number of subjects had subdivision Class II (asymmetric class of canines), where OJ was normal (63% had a Class I incisor relationship). Class II div 2 was found in 9.9% of subjects and mostly together with increased OB (≥5 mm). More importantly, Class III also had quite high prevalence (10.7%), which was higher than the prevalence found among younger population in Europe (6.2%) (58). This may be partly explained by the loss of posterior height of occlusion. Class III has also been associated in the literature with thin gingiva and increased risk for GR, especially in the lower anterior region (59). Furthermore, OT in periodontally healthy Class III subjects with GR did not influence their improvement (60). Knowing that subjects with stage III–IV periodontitis may already have attachment loss in the lower anterior region, one should keep in mind the risk for further deterioration of soft tissues as tooth movement increases the risk for labial alveolar bone loss and consequently GR (30). In contrast, the literature emphasizes Class II as a major risk for PTM, which could not be confirmed by the results of the present study (22, 61). However, it can be seen in the present study that Class III malocclusion had a high odds ratio for PTM, such as spacing and/or flaring, especially in subjects with tongue habit. As previously discussed, risk for PTM in Class III subjects has never been discussed in earlier literature.
At least one pair of anterior teeth with occlusal trauma, which was assessed in maximum intercuspation of anterior teeth in the present study, was found in more than 80% of subjects (44). Occlusal trauma was registered as a heavy contact of anterior teeth when the fremitus of the root was present during palpation (11, 62). It is well described in the literature that heavy occlusal contacts induce risk for further periodontal breakdown and migration of teeth, especially in cases of untreated periodontitis (12). The literature has also described that teeth, exposed to traumatic occlusal interferences, have worse healing after periodontal therapy (10).
Spacing was the most prevalent secondary malocclusion found in the present study, followed by extrusion. The results of the present study yielded that anterior teeth with periodontitis had more PTM than periodontally healthy anterior teeth. Furthermore, reduced clinical attachment levels were associated also with deep OB and increased OJ. This is in line with the earlier literature, which has also suggested that spacing, deep OB, and increased OJ in adult subjects might be related to deeper pockets and increased CAL (11, 63). Other studies also state that general spacing, flaring, and extrusion of single teeth is typically seen, especially with local periodontal disease (64). In the present study, the odds ratio for spacing in maxillary anterior teeth was associated with Class III malocclusion, loss of teeth, and periodontitis of anterior teeth.
It is described in the literature that the nature of tooth migration may vary in different malocclusions and may depend on soft tissue parafunctions (38). The present study found that the most prevalent oral habit was tongue habit (43%), which influenced spacing of the mandibular anterior teeth. In subjects with tongue habit, teeth may not only procline but may also end up in the open bite malocclusion. However, open bite in the present study was found in only three subjects.
Literature on the prevalence of various types of PTM is scarce. Martinez-Canut et al. only studied PTM cases with diastema, which either appeared or was increasing; however, in the present study, it can be seen that diastema was not so prevalent (38).
The literature states that periodontally healthy anterior teeth bear the entire load on excursive movements of the mandible. If posterior teeth are lost, the load on the anterior teeth increases even more. Due to the loss of attached tissues, the movements of the mandible become too heavy and traumatizing for anterior teeth with reduced periodontium (34, 44). In the present study, incorrect anterior and lateral guidance was very prevalent; however, its association with PTM was not found.
Pathological migration of teeth and impaired smile aesthetics were found to be the main reasons for subjects to seek OT (26). In the present study, OT need was firstly determined according to the DHC of IOTN, where more than half of the subjects were determined to be in a great or very great OT need. Additionally, in 21.5% of cases, OT need was moderate. However, in the process of applying DHC-IOTN on the present sample, we encountered some difficulties that did not reflect real need of orthodontic tooth movement due to secondary malocclusions. One of them was the assessment of the extrusion of a maxillary and/or mandibular anterior tooth with periodontitis resulting in severe secondary occlusal trauma (fremitus in maximum intercuspation), functional problems, permanent tooth mobility, and further periodontal breakdown. So, the amount of displacement did not reflect the severity of secondary malocclusion, which, if not treated, would pose a risk for tooth loss in the long term. Furthermore, many of the subjects in the present study did not have an increased or OB with gingival contact (which would be of great OT need) but still had severe secondary occlusal trauma. One more problem was found that the loss of posterior support of occlusion was not included in the tool. Also, the IOTN does not take into consideration CAL and root disclosure. Finally, the original DHC-IOTN describes that subjects needing collaborative care, including restorative, periodontal, and orthodontic treatment, fall directly into Grade 4 (great OT need). So, application of other features would become unimportant (49)
Due to the previously listed reasons, final OT need in the present study was assessed not only by DHC-IOTN, but supplemented by clinical assessment of pathological changes due to the periodontal disease. It was assessed that 66.1% of subjects, due to secondary malocclusions, would benefit from OT. Interestingly, among them, 60% of subjects agreed to start OT, showing that consent to undergo OT in older ages is not a problem. However, one recent study found that possibilities of such treatment are not always presented to the patients (26). Extraction of multiple teeth may be considered as an alternative; however, the prevalence of peri-implantitis, especially in subjects with periodontitis, is bringing back the idea of saving natural teeth (31–33). OT in subjects with severe PTM is sometimes the only option (24).
Studies with larger sample sizes are needed to increase validity and generalizability of the findings of the present study.
Conclusions
The most prevalent malocclusion was Class II. Spacing and extrusion were prevalent types of PTM, which were mainly influenced by CAL and tooth loss due to periodontitis. Preventive measures for PTM should be applied in cases with periodontally affected anterior teeth, before tooth extractions, in subjects with Class III malocclusion and tongue habit.
Orthodontists should be prepared for increased treatment demand as OT need, based on the results of the present study, was determined for more than half of the subjects. However, there is a lack of validated tools for assessment of OT need in adult subjects with advanced stages of periodontitis and secondary malocclusions.
Acknowledgements
The authors would like to kindly thank Professor Dr Andreas Stavropoulos and Dr Kristina Bertl (Dept. of Periodontology, Centre of Oral Health Sciences, Faculty of Odontology, Malmö University, Sweden) for their valuable advice for this study; Professor Ola Norderyd and Dr Shariel Sayardoust (Dept. of Periodontology, Institute for Postgraduate Dental Education, Jonkoping, Sweden) for sincere help with staging of periodontitis; Associate Professor Dr Ewa Czochrowska (Dept.Orthodontics, Medical University, Warsaw, Poland) for consultations and advice; Associate Professor Dr Krister Bjerklin for comments on the article, advice and support; Statistician Irena Nedzelskienė for her contribution to statistical analysis of the data.
Contributor Information
Eglė Zasčiurinskienė, Department of Orthodontics, Faculty of Odontology, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania.
Liveta Rastokaitė, Faculty of Odontology, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania.
Rune Lindsten, Department of Orthodontics, Institute for Postgraduate Dental Education, Jönköping, Sweden; Centre for Oral Health, School of Health and Welfare, Jönköping University, Sweden.
Nomeda Basevičienė, Department of Dental and Oral Pathology, Faculty of Odontology, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania.
Antanas Šidlauskas, Department of Orthodontics, Faculty of Odontology, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania.
Funding
European Social Fund (project no. 09.3.3-LMT-K-712-19-0024) under a grant agreement with the Research Council of Lithuania.
Authors’ contribution
Eglė Zasčiurinskienė: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, visualization, writing—original draft, and writing—review and editing. Liveta Rastokaitė: formal analysis, writing—original draft, and writing—review and editing. Rune Lindsten: formal analysis and writing—review and editing. Nomeda Basevičienė: formal analysis and investigation. Antanas Šidlauskas: formal analysis, funding acquisition, supervision, and writing—review and editing.
Conflicts of interest
None to declare.
Data availability
The data are available from the corresponding author, upon reasonable request.
References
- 1. Darveau, R. (2010) Periodontitis: a polymicrobial disruption of host homeostasis. Nature Reviews Microbiology, 8, 481–490. [DOI] [PubMed] [Google Scholar]
- 2. Hajishengallis, G. (2014) The inflammophilic character of the periodontitis-associated microbiota. Molecular Oral Microbiology, 29, 248–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Broadbent, E., Donkin, L. and Stroh, J.C. (2011) Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care, 34, 338–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Genco, R.J. and Borgnakke, W.S. (2013) Risk factors for periodontal disease. Periodontology 2000, 62, 59–94. [DOI] [PubMed] [Google Scholar]
- 5. Jepsen, S., et al. (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. Journal of Clinical Periodontology, 45, S219–S229. [DOI] [PubMed] [Google Scholar]
- 6. Kanasi, E., Ayilavarapu, S. and Jones, J. (2016) The aging population: demographics and the biology of aging. Periodontology 2000, 72, 13–18. [DOI] [PubMed] [Google Scholar]
- 7. Leite, F.R.M., Nascimento, G.G., Scheutz, F. and López, R. (2018) Effect of smoking on periodontitis: a systematic review and meta-regression. American Journal of Preventive Medicine, 54, 831–841. [DOI] [PubMed] [Google Scholar]
- 8. Nociti, F.H., Jr, Casati, M.Z. and Duarte, P.M. (2015) Current perspective of the impact of smoking on the progression and treatment of periodontitis. Periodontology 2000, 67, 187–210. [DOI] [PubMed] [Google Scholar]
- 9. Broadbent, J.M., Williams, K.B., Thomson, W.M. and Williams, S.M. (2006) Dental restorations: a risk factor for periodontal attachment loss? Journal of Clinical Periodontology, 33, 803–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Harrel, S.K. and Nunn, M.E. (2009) The association of occlusal contacts with the presence of increased periodontal probing depth. Journal of Clinical Periodontology, 36, 1035–1042. [DOI] [PubMed] [Google Scholar]
- 11. Fan, J. and Caton, J.G. (2018) Occlusal trauma and excessive occlusal forces: narrative review, case definitions, and diagnostic considerations. Journal of Periodontology, 89, S214–S222. [DOI] [PubMed] [Google Scholar]
- 12. Passanezi, E. and Sant’Ana, A.C.P. (2019) Role of occlusion in periodontal disease. Periodontology 2000, 79, 129–150. [DOI] [PubMed] [Google Scholar]
- 13. Eke, P.I., Thornton-Evans, G.O., Wei, L., Borgnakke, W.S., Dye, B.A. and Genco, R.J. (2018) Periodontitis in US adults: National Health and Nutrition Examination Survey 2009–2014. The Journal of the American Dental Association, 149, 576–588.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bernabe, E.M., et al. (2020) Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the Global Burden of Disease 2017 study. Journal of Dental Research, 99, 362–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Papapanou, P.N., et al. (2018) Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions. Journal of Clinical Periodontology, 45, S162–S170. [DOI] [PubMed] [Google Scholar]
- 16. Tonetti, M.S., Greenwell, H. and Kornman, K.S. (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. Journal of Clinical Periodontology, 45, S149–S161. [DOI] [PubMed] [Google Scholar]
- 17. Gkantidis, N., Christou, P. and Topouzelis, N. (2010) The orthodontic–periodontic interrelationship in integrated treatment challenges: a systematic review. Journal of Oral Rehabilitation, 37, 377–390. [DOI] [PubMed] [Google Scholar]
- 18. Spanemberg, J.C., Cardoso, J.A., Slob, E.M.G.B. and López-López, J. (2019) Quality of life related to oral health and its impact in adults. Journal of Stomatology, Oral and Maxillofacial Surgery, 120, 234–239. [DOI] [PubMed] [Google Scholar]
- 19. Araújo, A.C., Gusmão, E.S., Batista, J.E. and Cimões, R. (2010) Impact of periodontal disease on quality of life. Quintessence International, 41, e111–e118. [PubMed] [Google Scholar]
- 20. Gerritsen, A.E., Allen, P.F., Witter, D.J., Bronkhorst, E.M. and Creugers, N.H.J. (2010) Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health and Quality of Life Outcomes, 8, 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jansson, H., Wahlin, Å., Johansson, V., Åkerman, S., Lundegren, N., Isberg, P.-E. and Norderyd, O. (2014) Impact of periodontal disease experience on oral health-related quality of life. Journal of Periodontology, 85, 438–445. [DOI] [PubMed] [Google Scholar]
- 22. Brunsvold, M.A. (2005) Pathologic tooth migration. Journal of Periodontology, 76, 859–866. [DOI] [PubMed] [Google Scholar]
- 23. Tondelli, P.M. (2019) Orthodontic treatment as an adjunct to periodontal therapy. Dental Press Journal of Orthodontics, 24, 80–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Melsen, B. (2016) The role of orthodontics in the regeneration of the degenerated dentition. Journal of Oral Rehabilitation, 43, 226–237. [DOI] [PubMed] [Google Scholar]
- 25. Sanz, M. and Martin, C. (2015) Tooth movement in the periodontally compromised patient. In Lang, N.P. and Lindhe, J. (eds.), Clinical Periodontology and Implant Dentistry. Wiley Blackwell, Chichester, West Sussex, UK, 6th edn, pp. 1326–1371. [Google Scholar]
- 26. Hirschfeld, J., Reichardt, E., Sharma, P., Hilber, A., Meyer-Marcotty, P., Stellzig-Eisenhauer, A., Schlagenhauf, U. and Sickel, F.E. (2019) Interest in orthodontic tooth alignment in adult patients affected by periodontitis: a questionnaire-based cross-sectional pilot study. Journal of Periodontology, 90, 957–965. [DOI] [PubMed] [Google Scholar]
- 27. Papageorgiou, S.N., Antonoglou, G.N., Michelogiannakis, D., Kakali, L., Eliades, T. and Madianos, P. (2022) Effect of periodontal–orthodontic treatment of teeth with pathological tooth flaring, drifting, and elongation in patients with severe periodontitis: a systematic review with meta-analysis. Journal of Clinical Periodontology, 49, 102–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zasčiurinskienė, E., Basevičienė, N., Lindsten, R., Slotte, C., Jansson, H. and Bjerklin, K. (2018) Orthodontic treatment simultaneous to or after periodontal cause-related treatment in periodontitis susceptible patients. Part I: Clinical outcome. A randomized clinical trial. Journal of Clinical Periodontology, 45, 213–224. [DOI] [PubMed] [Google Scholar]
- 29. Zasčiurinskienė, E., Lund, H., Lindsten, R., Jansson, H. and Bjerklin, K. (2019) Outcome of orthodontic treatment in subjects with periodontal disease. Part III: A CBCT study of external apical root resorption. European Journal of Orthodontics, 41, 575–582. [DOI] [PubMed] [Google Scholar]
- 30. Zasčiurinskienė, E., Lund, H., Lindsten, R., Jansson, H. and Bjerklin, K. (2019) Outcome of periodontal–orthodontic treatment in subjects with periodontal disease. Part II: A CBCT study of alveolar bone level changes. European Journal of Orthodontics, 41, 565–574. [DOI] [PubMed] [Google Scholar]
- 31. Dommisch, H., Walter, C., Difloe-Geisert, J.C., Gintaute, A., Jepsen, S. and Zitzmann, N.U. (2022) Efficacy of tooth splinting and occlusal adjustment in patients with periodontitis exhibiting masticatory dysfunction: a systematic review. Journal of Clinical Periodontology, 49, 149–166. [DOI] [PubMed] [Google Scholar]
- 32. Carra, M.C., Rangé, H., Swerts, P.-J., Tuand, K., Vandamme, K. and Bouchard, P. (2022) Effectiveness of implant-supported fixed partial denture in patients with history of periodontitis: a systematic review and meta-analysis. Journal of Clinical Periodontology, 49, 208–223. [DOI] [PubMed] [Google Scholar]
- 33. Montero, E., Molina, A., Palombo, D., Morón, B., Pradíes, G. and Sanz-Sánchez, I. (2022) Efficacy and risks of tooth-supported prostheses in the treatment of partially edentulous patients with stage IV periodontitis. A systematic review and meta-analysis. Journal of Clinical Periodontology, 49, 182–207. [DOI] [PubMed] [Google Scholar]
- 34. Pirih, F.Q., Camargo, P.M., Takei, H.H. and Carranza, F.A. (2019) Periodontal response to external forces. In Newman, M.G., Takei, H.H., Klokkevold, P.R. and Carranza, F.A. (eds.), Newman and Carranza’s Clinical Periodontology. Elsevier, Philadelphia, PA, pp. 328–336. [Google Scholar]
- 35. Towfighi, P.P., Brunsvold, M.A., Storey, A.T., Arnold, R.M., Willman, D.E. and McMahan, C.A. (1997) Pathologic migration of anterior teeth in patients with moderate to severe periodontitis. Journal of Periodontology, 68, 967–972. [DOI] [PubMed] [Google Scholar]
- 36. von Elm, E., Altman, D.G., Egger, M., Pocock, S.J., Gøtzsche, P.C. and Vandenbroucke, J.P. (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet, 370, 1453–1457. [DOI] [PubMed] [Google Scholar]
- 37. Salvi, G.E., Lindhe, J. and Lang, N.P. (2008) Examination of patients with periodontal diseases. In Lindhe, J., Lang, N.P. and Karring, T. (eds.), Clinical Periodontology and Implant Dentistry. Blackwell Munksgaard, Oxford, UK, 5th edn, p. 583. [Google Scholar]
- 38. Martinez-Canut, P., Carrasquer, A., Magán, R. and Lorca, A. (1997) A study on factors associated with pathologic tooth migration. Journal of Clinical Periodontology, 24, 492–497. [DOI] [PubMed] [Google Scholar]
- 39. Cobourne, M. and DiBiase, A. (2015)Handbook of Orthodontics. Elsevier, Oxford, UK, 2nd edn, pp. 1–6. [Google Scholar]
- 40. Pancherz, H. and Bondemark, L. (2021) The bite-type malocclusion classification—an extended Angle-method. Is the new classification reliable? APOS Trends in Orthodontics, 11, 100–105. [Google Scholar]
- 41. Proffit, W. (2019) Malocclusion and dentofacial deformity in contemporary society. In Proffit, W., Fields, H., Larson, B. and Sarver, D. (eds.), Contemporary Orthodontics. Elsevier, Philadelphia, PA, 6th edn, pp. 5–7. [Google Scholar]
- 42. Daskalogiannakis, J. (2000) Glossary of Orthodontic Terms. Quintessence Publishing Co., Inc, Berlin, Germany, p. 8. [Google Scholar]
- 43. Fraile, C., Ferreiroa, A., Romeo Rubio, M., Alonso, R. and Pradíes Ramiro, G. (2022) Clinical study comparing the accuracy of interocclusal records, digitally obtained by three different devices. Clinical Oral Investigations, 26, 4663–4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shillingburg, H.T., Sather, D.A., Wilson, E.L., Cain, J.R., Mitchell, D.L., Blanco, L.J. and Kessler, J.C. (2012) Fundamentals of Fixed Prosthodontics. Quintessence Publishing Co, Inc, Chicago, IL, 4th edn, pp. 13–24. [Google Scholar]
- 45. Branschofsky, M., Beikler, T., Schafer, R., Flemming, T.F. and Lang, H. (2011) Secondary trauma from occlusion and periodontitis. Quintessence International, 42, 515–522. [PubMed] [Google Scholar]
- 46. Proffit, W.R. (1978) Equilibrium theory revisited: factors influencing position of the teeth. The Angle Orthodontist, 48, 175–186. [DOI] [PubMed] [Google Scholar]
- 47. Glaros, A. and Burton, E. (2004) Parafunctional clenching, pain, and effort in temporomandibular disorders. Journal of Behavioral Medicine, 27, 91–100. [DOI] [PubMed] [Google Scholar]
- 48. Lobbezoo, F., et al. (2018) International consensus on the assessment of bruxism: report of a work in progress. Journal of Oral Rehabilitation, 45, 837–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Brook, P.H. and Shaw, W.C. (1989) The development of an index of orthodontic treatment priority. European Journal of Orthodontics, 3, 309–320. [DOI] [PubMed] [Google Scholar]
- 50. Burgett, F.G., Ramfjord, S.P., Nissle, R.R., Morrison, E.C., Charbeneau, T.D. and Caffesse, R.G. (1992) A randomized trial of occlusal adjustment in the treatment of periodontitis patients. Journal of Clinical Periodontology, 19, 381–387. [DOI] [PubMed] [Google Scholar]
- 51. Kinane, D.F., Lindhe, J. and Trombelli, L. (2008) Chronic periodontitis. In Lindhe, J., Lang, N.P. and Karring, T. (eds.), Clinical Periodontology and Implant Dentistry. Blackwell Munksgaard, Oxford, UK, 5th edn, p. 420. [Google Scholar]
- 52. Nocini, R., Lippi, G. and Mattiuzzi, C. (2020) Periodontal disease: the portrait of an epidemic. Journal of Public Health and Emergency, 4, 10. [Google Scholar]
- 53. Koo, T. and Li, M. (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15, 155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Holtfreter, B., Albandar, J.M., Dietrich, T., Dye, B.A., Eaton, K.A., Eke, P.I., Papapanou, P.N. and Kocher, T. (2015) Standards for reporting chronic periodontitis prevalence and severity in epidemiologic studies. Journal of Clinical Periodontology, 42, 407–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Khorshidi, H., Moaddeli, M., Golkari, A., Heidari, H. and Raoufi, S. (2016) The prevalence of pathologic tooth migration with respect to the severity of periodontitis. Journal of International Society of Preventive and Community Dentistry, 6, S122–S125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sgolastra, F., Petrucci, A., Severino, M., Gatto, R. and Monaco, A. (2015) Periodontitis, implant loss and peri-implantitis. A meta-analysis. Clinical Oral Implants Research, 26, e8–e16. [DOI] [PubMed] [Google Scholar]
- 57. Shaw, W.C., Addy, M. and Ray, C. (1980) Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a review. Community Dentistry and Oral Epidemiology, 8, 36–45. [DOI] [PubMed] [Google Scholar]
- 58. Alhammadi, M.S., Halboub, E., Fayed, M.S., Labib, A. and El-Saaidi, C. (2018) Global distribution of malocclusion traits: a systematic review. Dental Press Journal of Orthodontics, 23, 40.e1–40.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Gorbunkova, A., Pagni, G., Brizhak, A., Farronato, G. and Rasperini, G. (2016) Impact of orthodontic treatment on periodontal tissues: a narrative review of multidisciplinary literature. International Journal of Dentistry, 2016, 4723589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Antanavičienė, G., Zasčiurinskienė, E., Smailienė, D. and Basevičienė, N. (2021) The impact of orthodontic treatment on pre-existing gingival recessions: a retrospective study. Applied Sciences, 11, 9036. [Google Scholar]
- 61. Selwyn, S.L. (1973) An assessment of patients with periodontally involved migrated incisors. Journal of Dentistry, 1, 153–157. [DOI] [PubMed] [Google Scholar]
- 62. Lindhe, J., Nyman, S. and Ericsson, I. (2008) Trauma from occlusion: periodontal tissues. In Lindhe, J., Lang, N.P. and Karring, T. (eds.), Clinical Periodontology and Implant Dentistry. Blackwell Munksgaard, Oxford, UK, 5th edn, pp. 349–361. [Google Scholar]
- 63. Bernhardt, O., Krey, K.-F., Daboul, A., Völzke, H., Kindler, S., Kocher, T. and Schwahn, C. (2019) New insights in the link between malocclusion and periodontal disease. Journal of Clinical Periodontology, 46, 144–159. [DOI] [PubMed] [Google Scholar]
- 64. Janer, J. and Melsen, B. (2012) A systematic approach to the orthodontic treatment of periodontally involved anterior teeth. In Melsen, B. (ed.), Adult Orthodontics. John Wiley & Sons, West Sussex, UK, 1st edn, pp. 250–260. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available from the corresponding author, upon reasonable request.