Objective:
Efficacy and safety of five common surgical treatments for lower calyceal (LC) stones were assessed for LC stones 20 mm or less.
Methods:
A systematic literature search was conducted up to June 2020 using PubMed, EMBASE, and Cochrane Library. The study has been registered in PROSPERO, CRD42021228404. Randomized controlled trials evaluating the efficacy and safety of five common surgical treatments for LC stones were collected, including percutaneous nephrolithotomy (PCNL), mini-PCNL (MPCNL), ultramini-PCNL (UMPCNL), extracorporeal shock wave lithotripsy (ESWL), and retrograde intrarenal surgery (RIRS). Heterogeneity among studies was assessed by using global inconsistency and local inconsistency. Both pooled odds ratio, along with 95% credible interval (CI) and the surface under the cumulative ranking curve values were calculated to assess the outcomes, paired comparisons of efficacy and safety of five treatments.
Results:
Nine peer-reviewed randomized controlled trials, comprising 1674 patients in recent 10 years, were included. Heterogeneity tests showed no statistical significance, and a consistency model was chosen, respectively. The order of surface under the cumulative ranking curve values for efficacy was as follows: PCNL (79.4), MPCNL (75.2), UMPCNL (66.3), RIRS (29), and eSWL (0). For safety: eSWL (84.2), UMPCNL (82.2), RIRS (52.9), MPCNL (16.6), and PCNL (14.1).
Conclusion:
In the current study, all five treatments are both effective and safe. Many factors must be considered to choose surgical treatments for LC stones 20 mm or less; the results that we separate conventional PCNL into PCNL, MPCNL, and UMPCNL make the questions even more controversial. However, relative judgments are still needed to be used as reference data in clinical management. For efficacy, PCNL>MPCNL>UMPCNL>RIRS>ESWL, ESWL is statistically inferior to the other four treatments, respectively. RIRS is statistically inferior to PCNL and MPCNL, respectively. For safety, ESWL>UMPCNL>RIRS>MPCNL>PCNL, ESWL is statistically superior to RIRS, MPCNL, and PCNL, respectively. RIRS is statistically superior to PCNL. We cannot reach conclusions about which surgical treatment is the best choice for all patients with LC stones 20 mm or less; therefore, tailored treatments based on individual patients still demand more attention than ever before for both patients and urologists.
Keywords: efficacy, lower calyceal stones, meta-analysis, safety
Introduction
Lower calyceal (LC) stones account for ∼35% of entire renal stones1. Percutaneous nephrolithotomy (PCNL), extracorporeal shock wave lithotripsy (ESWL), and retrograde intrarenal surgery (RIRS) are the active surgical management for LC stones. However, LC stones have been a problem for both patients and urologists. Due to the anatomical variations of LC, especially considering stone clearance, ESWL has usually failed here. But again, because of some anatomical reasons and the durability of the instrument, it may not always be easy to perform RIRS for all LC stones2. Conventional PCNL has been an effective, successful, and easy approach for LC stones. Nevertheless, risks of complications and nephron loss are unavoidable3. In addition, along with the development of technology, the miniaturization of PCNL also developed in order to diminish access-related varied complications4. Conventionally the miniaturization of PCNL has been defined by a diameter of less than 20 Fr5. The mini-PCNL (MPCNL) (16–18 Fr) and ultramini-PCNL (UMPCNL) (11–14 Fr) are currently feasible and modern alternatives with minimal invasiveness3. The MPCNL is accepted as suitable for renal stones less than 20 mm in size, while UMPCNL is for renal stones less than 15 mm5,6. Although the application of different methods needs to meet various conditions, the rough superior and interior of the treatments are necessary to study.
In the current study, a systemic review and network meta-analysis was designed to evaluate the safety and efficacy of the common surgical options for LC stones 20 mm or less.
Materials and methods
Search strategy
Cochrane Library, PubMed, and EMBASE were searched for randomized controlled trials (RCTs) (search performed on 3 June 2020 with no date restriction). The search terms that we used were ‘kidney stone,’ ‘lower,’ ‘randomized controlled trials’ (Supplementary Tables 1–3, Supplemental Digital Content 4, http://links.lww.com/JS9/A62, Supplemental Digital Content 5, http://links.lww.com/JS9/A63, Supplemental Digital Content 6, http://links.lww.com/JS9/A64). We also reviewed the references of relevant articles, and no additional papers were obtained. The study protocol was not prepared. The study has been registered in PROSPERO, CRD42021228404; it can be accessed here:https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=228404.
Each article identified through the electronic searches was screened by two reviewers for relevance, initially using the title and the abstract and subsequently reading the full text to select articles that met inclusion criteria. The work was reported in line with the search strategy promoted by the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA, Supplemental Digital Content 1, http://links.lww.com/JS9/A59) guidelines7. Only peer-reviewed studies were searched; we did not search for gray literature, non-English papers, and studies in registries. Beyond that, our self-evaluate of the quality of work met the high level of compliance with Assessing the Methodological Quality of Systematic Reviews (AMSTAR) guidelines8, Supplemental Digital Content 3, http://links.lww.com/JS9/A61. Records of the selection process were retained, and a PRISMA flowchart was generated (Fig. 1), Supplemental Digital Content 2, http://links.lww.com/JS9/A60. Finally, nine articles containing nine RCTs were included; the baseline characteristics of these nine studies were summarized in Table 1. All disputes arising during the systematic literature review process were resolved by a third reviewer.
Figure 1.
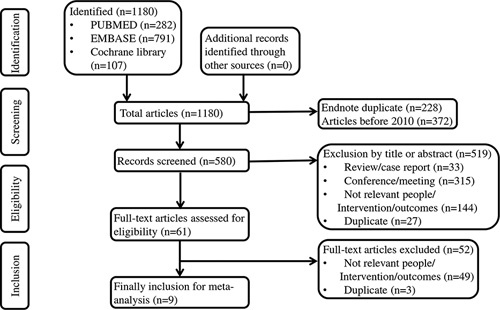
PRISMA flow diagram showing study selection process and rationale for exclusions. EMBASE, Excerpta Medica database; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Assessment of basic characteristics.
| References | Trial design | Groups | Diagnosis | Stone size (mm) | Number | SFR (months) | Population |
|---|---|---|---|---|---|---|---|
| Bozzini et al.9 | RCT | PCNL, RIRS, ESWL | CT | 10–20 | 582 | 3 | LC, 18–75 years |
| Bozzini et al.10 | RCT | PCNL, MPCNL, UMPCNL | CT | 10–20 | 132 | 3 | LC, 18–75 years |
| Fayad et al.11 | RCT | MPCNL, RIRS | CT | ≤20 | 120 | 3 | LC, 18–75 years |
| Jiang et al.12 | RCT | MPCNL, RIRS | CT | ≤20 | 116 | 3 | LC, ≥18 years |
| Jin et al.13 | RCT | MPCNL, RIRS | CT | 10–20 | 220 | 3 | LC, average 52.3 years |
| Kumar et al.14 | RCT | MPCNL, RIRS, ESWL | CT | 10–20 | 158 | 3 | LC, ≥15 years |
| Sener et al.15 | RCT | RIRS, ESWL | CT | ≤10 | 100 | 3 | LC, average 35.67 years |
| Yuruk et al.16 | RCT | PCNL, ESWL | CT | ≤20 | 66 | 3 | LC, 18–75 years |
| Zhang et al.17 | RCT | UMPCNL, RIRS, ESWL | CT | 10–20 | 180 | 3 | LC, ≥18 years |
| Total | – | – | 1674 | – | – |
CT, computed tomography; ESWL, extracorporeal shock wave lithotripsy; LC, stones located in lower calyceal; MPCNL, mini-PCNL; PCNL, percutaneous nephrolithotomy; RCT, randomized controlled trial; RIRS, retrograde intrarenal surgery; SFR, stone-free rate; UMPCNL, ultramini-PCNL.
Inclusion and exclusion criteria
RCTs in recent 10 years were included if patients with LC stones were treated by PCNL or RIRS or ESWL or MPCNL, or UMPCNL with a follow-up of 3-month stone-free rate (3SFR) after the procedure. Patients with urinary stones in other locations, non-English articles, conference papers, case reports, or case series were excluded.
Assessment of quality and baseline characteristics
All nine RCTs9–17 are randomized studies. None mentioned allocation concealment, selective report, etc. (Table 2). The quality of evidence for retrieved references was determined using the Cochrane risk of bias tool18. Was randomization carried out appropriately? Was the baseline between groups comparable? Was the concealment of treatment allocation adequate? Were the care providers, participants, and outcome assessors blind to the treatment allocation? Were the lost visit reported, and what is the specific number of missing data? Was there any evidence to suggest that the authors measured more outcomes than they reported? Did the analysis include an ITT (intention to treat) analysis?
Table 2.
Assessment of quality.
| References | Randomization | Allocated | Blinding | Baseline | Loss of follow-up | Selective report results | ITT |
|---|---|---|---|---|---|---|---|
| Bozzini et al.9 | Unclear | No | Unblinded | Comparable | Yes (n=18) | Unclear | Unclear |
| Bozzini et al.10 | Randomized number table | No | Unclear | Comparable | Unclear | Unclear | Unclear |
| Fayad et al.11 | Unclear | No | Unclear | Comparable | Yes (n=14) | Unclear | Unclear |
| Jiang et al.12 | Unclear | No | Unclear | Comparable | Yes (n=3) | Unclear | Unclear |
| Jin et al.13 | Simple random sampling | No | Unblinded | Comparable | Yes (n=0) | Unclear | Yes |
| Kumar et al.14 | Computer generated | No | Unclear | Comparable | Yes (n=23) | Unclear | Unclear |
| Sener et al.15 | Online randomization tool | No | Unclear | Unclear | Yes (n=3) | Unclear | Unclear |
| Yuruk et al.16 | Unclear | No | Unclear | Comparable | Yes (n=9) | Unclear | Unclear |
| Zhang et al.17 | Unclear | No | Unclear | Comparable | Unclear | Unclear | Unclear |
ITT, intention to treat.
Data analysis
Data were analyzed by using ‘Stata’ (version 16; StataCorp, College Station, Texas, USA) using ‘mvmeta’ command19 and ‘network’ and ‘network graph’ packages. The odds ratio (OR) was employed to assess dichotomous data. We analyzed comparable data using 95% credible intervals (CIs), and the surface under the cumulative ranking curve (SUCRA) values also were calculated. Heterogeneity among studies was assessed by using global inconsistency, local inconsistency, and loop inconsistency; an individual study could be characterized as a consistency model if heterogeneity was low; otherwise, an inconsistency model was chosen.
Results
Heterogeneity
All the results of global inconsistency (P=0.3237), local inconsistency (all P>0.05), and loop inconsistency (Supplementary Fig. 4, Supplemental Digital Content 16, http://links.lww.com/JS9/A74) suggested no significant difference was found; therefore, consistency model was chosen for efficacy outcome.
All the results of global inconsistency (P=0.4446), local inconsistency (all P values>0.05), and loop inconsistency (Supplementary Fig. 6, Supplemental Digital Content 20, http://links.lww.com/JS9/A78) suggested no significant difference was found; therefore, consistency model was chosen for safety outcome.
Publication bias
Funnel plots were performed to assess publication bias (Supplementary Fig. 3, Supplemental Digital Content 15, http://links.lww.com/JS9/A73 and Fig. 5, Supplemental Digital Content 19, http://links.lww.com/JS9/A77). The results showed no apparent asymmetry, which indicated no obvious publication bias.
Efficacy
The distribution of probabilities for each treatment being ranked for their 3SFR and complication in the treatment of LC stones according to SUCRA values is presented in Table 3. Network comparisons were shown in 17 two-arm studies (Supplementary Fig. 1, Supplemental Digital Content 13, http://links.lww.com/JS9/A71). The order of SUCRA values for 3SFR was as follows: PCNL (79.4), MPCNL (75.2), UMPCNL (66.3), RIRS (29), and ESWL (0) (Table 3). Therefore, PCNL had the highest probability of being the best intervention option in terms of 3SFR. The pooled OR for the network estimates, along with 95% CI, is presented in Figure 2A. A significant difference was shown in the following groups, ESWL versus PCNL: OR, 0.20 [95% CI, 0.12–0.32]; ESWL versus MPCNL: OR, 0.19 [95% CI, 0.10–0.36]; ESWL versus UMPCNL: OR, 0.22 [95% CI, 0.09–0.56]; ESWL versus RIRS: OR, 0.36 [95% CI, 0.25–0.52]; RIRS versus PCNL: OR, 0.55 [95% CI, 0.34–0.90]; and RIRS versus MPCNL: OR, 0.52 [95% CI, 0.29–0.93]. No significant difference was found among PCNL, MPCNL, and UMPCNL, respectively. ESWL was significantly inferior to the other four treatments. RIRS was significantly inferior to PCNL and MPCNL, respectively. No significant difference was found in the rest of the groups. A simple figure was designed creatively to show the complicated results concisely and explicitly (Fig. 3A).
Table 3.
SUCRA of lower calyceal treatments.
| Outcome | Treatment | SUCRA | PrBest | Mean rank |
|---|---|---|---|---|
| 3SFR | PCNL | 75.2 | 31.4 | 2 |
| MPCNL | 79.4 | 40.7 | 1.8 | |
| UMPCNL | 66.3 | 27.9 | 2.3 | |
| RIRS | 29 | 0.0 | 3.8 | |
| ESWL | 0.0 | 0.0 | 5.0 | |
| Complication | PCNL | 14.1 | 0.0 | 4.4 |
| MPCNL | 16.6 | 0.0 | 4.3 | |
| UMPCNL | 82.2 | 62.3 | 1.7 | |
| RIRS | 52.9 | 0.1 | 2.9 | |
| ESWL | 84.2 | 37.5 | 1.6 |
3SFR, 3-month stone-free rate; ESWL, extracorporeal shock wave lithotripsy; MPCNL, mini-PCNL; PCNL, percutaneous nephrolithotomy; PrBest, probability of being the best; RIRS, retrograde intrarenal surgery; SUCRA, surface values under the cumulative ranking; UMPCNL, ultramini-PCNL.
Figure 2.
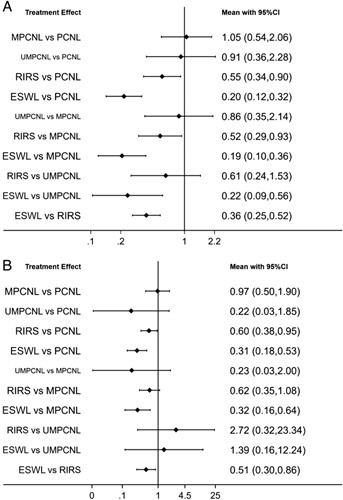
Forest plot showing changes in efficacy (A) and safety (B), comparison of five treatments. ESWL, extracorporeal shock wave lithotripsy; MPCNL, mini-PCNL; PCNL, percutaneous nephrolithotomy; RIRS, retrograde intrarenal surgery; UMPCNL, ultramini-PCNL.
Figure 3.
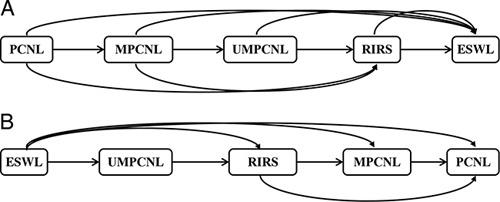
Efficacy (A) and safety (B) results of the network meta-analysis. The former → the latter=the former is superior to the latter; the former ~> the latter=the former is statistically superior to the latter. ESWL, extracorporeal shock wave lithotripsy; MPCNL, mini-PCNL; PCNL, percutaneous nephrolithotomy; RIRS, retrograde intrarenal surgery; UMPCNL, ultramini-PCNL.
Safety
Network comparisons were shown in 16 two-arm studies (Supplementary Fig. 2, Supplemental Digital Content 14, http://links.lww.com/JS9/A72). The order of SUCRA values for complication was as follows: ESWL (84.2), UMPCNL (82.2), RIRS (52.9), MPCNL (16.6), and PCNL (14.1) (Table 3). Therefore, ESWL had the highest probability of being the best intervention option in terms of complication. The pooled OR for the network estimates, along with 95% CI, is presented in Figure 2B. A significant difference was shown in the following groups, ESWL versus PCNL: OR, 0.31 [95% CI, 0.18–0.53]; ESWL versus MPCNL: OR, 0.32 [95% CI, 0.16–0.64]; ESWL versus RIRS: OR, 0.51 [95% CI, 0.30–0.86]; and RIRS versus PCNL: OR, 0.60 [95% CI, 0.38–0.95]. No significant difference was found among PCNL, MPCNL, and UMPCNL, respectively. ESWL was significantly superior to the other four treatments, respectively. RIRS was significantly superior to PCNL. No significant difference was found in the rest of the groups. A simple figure was designed creatively to show the complicated results concisely and explicitly (Fig. 3B).
Discussion
Based on the European Association of Urology guidelines as considered for LC stones, in case of unfavorable conditions for ESWL, endourological interventions such as PCNL or RIRS are advised to be the first choice20. However, on account of the anatomical variations of LC, such as the narrow ureter or calyceal infundibulum3, both patients and urologists have been troubled by LC stones frequently, especially considering stone clearance21. Accompanied by auxiliary procedures and re-treatments9, ESWL has usually failed here. Although RIRS has gained popularity over time for especially endoscopic treatment of less than 2 cm sized LC stones21, it may not always be easy to perform RIRS for all LC stones of anatomical difficulties again and the durability of the instrument2. Previously, a systematic review and meta-analysis of high quality showed PCNL and RIRS were superior to ESWL in stone clearance, and even PCNL is more effective than RIRS22. Set aside handicaps as we introduced before, RIRS looked like a feasible and better option against PCNL when complication rates were also taken into consideration3. With the intention of decreasing complications, the instrument calibers of PCNL have been progressively reduced, and the minimally invasive PCNL technique, UMP, has been developed with 11–13 Fr materials (3.5 Fr nephroscope)23. Advances in technology made the arguments more controversial.
For lacking direct evidence, a network meta-analysis was designed to assess the efficacy and safety of five interventions, including three PCNL techniques.
According to the current study, for efficacy, based on 3SFR, there was no significant difference among PCNL, MPCNL, and UMPCNL, respectively. The result was inconsistent with the findings of the original document10, the results of which showed the efficacy of UMPCNL was statistically lower than PCNL and MPCNL, respectively. The following might be the key reasons: first, lack of RCTs designed for directly comparing results of the three methods; second, highly skilled urologists might enhance the efficacy of the MPCNL; third, the size of stones might be another important factor.
For safety, based on complication, There was no doubt that the efficacy of ESWL was worst and the safety was best; the result was consistent with the findings of previous meta-analyses or agreed with the outcomes shown in original documents. UMPCNL was statistically the most safety intervention compared with PCNL and MPCNL, respectively. Similarly, MP seems to be the preferential alternative for 1–2 cm LC stone intervention among the others10.
There are some main merits of our study. First, a recent 10-year RCTs-based network meta-analysis. Second, conventional PCNL was separated into PCNL, MPCNL, and UMPCNL. Third, based on efficacy or safety, five techniques were ranked by SUCRA values respectively. Forth, whether the results had statistical differences also were calculated between each of them. Fifth, aimed at the complicated results of the network meta-analysis, we creatively designed a simple figure to show concisely and explicitly. Five treatments are listed, straight lines with arrows mean the former is superior to the latter; curve lines with arrows mean the former is statistically superior to the latter (Fig. 3).
A major limitation of our study was that no subgroup analysis was performed on the size of the LC stones. If subgroup analyses were performed, there was a possibility it might lead to different outcomes because the recommended treatments heavily depend on the size of the LC stones. However, the conventional PCNL had been separated into PCNL, MPCNL, and UMPCNL, further limited by the lack of available randomized trials. There is only 1 trial comprising RIRS versus ESWL for stone less than 10 mm in Table 1, therefore, no subgroup analysis was applied. After all, too few studies to design a subgrouping analysis, and even if the subgrouping analysis were designed, the results would not be convincing. With the increasing of relevant randomized trials, our team might design another meta-analysis focusing on the stone diameter, at that time; the subdivided surgical treatments (PCNL, MPCNL, and UMPCNL, for example) for subdivided stone diameter (<10 mm and >10 mm for example) will be assessed comprehensively.
Another major limitation was that the results of the current study did not take into account other outcomes shown in original RCTs, such as the need for auxiliary procedures and re-treatments, operating time, and hospitalization. Moreover, the cost of different operation styles also plays a key role in influencing patients’ choices.
Conclusion
In the current study, all five treatments are both effective and safe. Many factors must be considered to choose surgical treatments for LC stones 20 mm or less; the results that we separate conventional PCNL into PCNL, MPCNL, and UMPCNL make the questions even more controversial. However, relative judgments are still needed to be used as reference data in clinical management. For efficacy, PCNL>MPCNL>UMPCNL>RIRS>ESWL, ESWL is statistically inferior to the other four treatments, respectively. RIRS is statistically inferior to PCNL and MPCNL, respectively. For safety, ESWL>UMPCNL>RIRS>MPCNL>PCNL, ESWL is statistically superior to RIRS, MPCNL, and PCNL, respectively. RIRS is statistically superior to PCNL. We cannot reach conclusions about which surgical treatment is the best choice for all patients with LC stones to 20 mm or less; therefore, tailored treatments based on individual patients still demand more attention than ever before for both patients and urologists.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Patient consent
Not applicable.
Sources of funding
The research was supported by the educational department of Liaoning Province No.: QN2019018 grant to Ning Li.
Author contribution
J.H., H.X., F.D., and N.L.: conceived and designed the studies; J.H., H.X., and F.D.: performed the studies; J.H., H.X., and F.D.: reviewed the literature and analyzed the data; N.L.: contributed technical and material support; J.H. and N.L.: wrote the paper.
Conflicts of interest disclosure
The authors all declare that they have no conflicts of interest.
Research registration unique identifying number (UIN)
Name of the registry: PROSPERO.
Unique identifying number or registration ID: CRD42021228404.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=228404.
Guarantor
Ning Li, Associate Professor of Urology, Department of Urology, Fourth Affiliated Hospital of China Medical University, 4 Chongshan East Rd, Shenyang 110032, Liaoning, China. Tel: +86 189 0091 3059. E-mail: air-nick@hotmail.com.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Data availability
Not applicable.
Color printing
Not applicable.
Supplementary Material
Acknowledgments
The research was supported by the educational department of Liaoning Province No.: QN2019018 grant.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 24 March 2023
Contributor Information
Jun Hou, Email: 727990713@qq.com.
Feihong Xu, Email: 1287335417@qq.com.
Huifang Du, Email: 1148898786@qq.com.
Jingxuan Liu, Email: 422311904@qq.com.
Ning Li, Email: air-nick@hotmail.com.
References
- 1. Cass AS, Grine WB, Jenkins JM, et al. The incidence of lower-pole nephrolithiasis – increasing or not? Br J Urol 1998;82:12–5. [DOI] [PubMed] [Google Scholar]
- 2. Monga M, Best S, Venkatesh R, et al. Durability of flexible ureteroscopes: a randomized, prospective study. J Urol 2006;176:137–41. [DOI] [PubMed] [Google Scholar]
- 3. Moore SL, Bres-Niewada E, Cook P, et al. Optimal management of lower pole stones: the direction of future travel. Cent Eur J Urol 2016;69:274–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ghani KR, Andonian S, Bultitude M, et al. Percutaneous nephrolithotomy: update, trends, and future directions. Eur Urol 2016;70:382–96. [DOI] [PubMed] [Google Scholar]
- 5. Ganpule AP, Bhattu AS, Desai M. PCNL in the twenty-first century: role of Microperc, Miniperc, and Ultraminiperc. World J Urol 2015;33:235–40. [DOI] [PubMed] [Google Scholar]
- 6. Mishra S, Sharma R, Garg C, et al. Prospective comparative study of miniperc and standard PNL for treatment of 1 to 2 cm size renal stone. BJU Int 2011;108:896–9; discussion 9-900. [DOI] [PubMed] [Google Scholar]
- 7. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 8. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bozzini G, Verze P, Arcaniolo D, et al. A prospective randomized comparison among ESWL, PCNL and RIRS for lower calyceal stones less than 2 cm: a multicenter experience: a better understanding on the treatment options for lower pole stones. World J Urol 2017;35:1967–75. [DOI] [PubMed] [Google Scholar]
- 10. Bozzini G, Aydogan TB, Muller A, et al. A comparison among PCNL, Miniperc and Ultraminiperc for lower calyceal stones between 1 and 2 cm: a prospective, comparative, multicenter and randomised study. BMC Urol 2020;20:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fayad AS, Elsheikh MG, Ghoneima W. Tubeless mini-percutaneous nephrolithotomy versus retrograde intrarenal surgery for lower calyceal stones of ⩽2 cm: a prospective randomised controlled study. Arab J Urol 2017;15:36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jiang K, Chen H, Yu X, et al. The “all-seeing needle” micro-PCNL versus flexible ureterorenoscopy for lower calyceal stones of ≤2 cm. Urolithiasis 2019;47:201–6. [DOI] [PubMed] [Google Scholar]
- 13. Jin L, Yang B, Zhou Z, et al. Comparative efficacy on flexible ureteroscopy lithotripsy and miniaturized percutaneous nephrolithotomy for the treatment of medium-sized lower-pole renal calculi. J Endourol 2019;33:914–99. [DOI] [PubMed] [Google Scholar]
- 14. Kumar A, Kumar N, Vasudeva P, et al. A prospective, randomized comparison of shock wave lithotripsy, retrograde intrarenal surgery and miniperc for treatment of 1 to 2 cm radiolucent lower calyceal renal calculi: a single center experience. J Urol 2015;193:160–4. [DOI] [PubMed] [Google Scholar]
- 15. Sener NC, Bas O, Sener E, et al. Asymptomatic lower pole small renal stones: shock wave lithotripsy, flexible ureteroscopy, or observation? A prospective randomized trial. Urology 2015;85:33–7. [DOI] [PubMed] [Google Scholar]
- 16. Yuruk E, Binbay M, Sari E, et al. A prospective, randomized trial of management for asymptomatic lower pole calculi. J Urol 2010;183:1424–8. [DOI] [PubMed] [Google Scholar]
- 17. Zhang H, Hong TY, Li G, et al. Comparison of the efficacy of ultra-mini PCNL, flexible ureteroscopy, and shock wave lithotripsy on the treatment of 1-2 cm lower pole renal calculi. Urol Int 2019;102:153–9. [DOI] [PubMed] [Google Scholar]
- 18. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. White IR, Barrett JK, Jackson D, et al. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods 2012;3:111–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Türk C, Petřík A, Sarica K, et al. EAU guidelines on diagnosis and conservative management of urolithiasis. Eur Urol 2016;69:468–74. [DOI] [PubMed] [Google Scholar]
- 21. Mi Y, Ren K, Pan H, et al. Flexible ureterorenoscopy (F-URS) with holmium laser versus extracorporeal shock wave lithotripsy (ESWL) for treatment of renal stone <2 cm: a meta-analysis. Urolithiasis 2016;44:353–65. [DOI] [PubMed] [Google Scholar]
- 22. Donaldson JF, Lardas M, Scrimgeour D, et al. Systematic review and meta-analysis of the clinical effectiveness of shock wave lithotripsy, retrograde intrarenal surgery, and percutaneous nephrolithotomy for lower-pole renal stones. Eur Urol 2015;67:612–66. [DOI] [PubMed] [Google Scholar]
- 23. Desai J, Solanki R. Ultra-mini percutaneous nephrolithotomy (UMP): one more armamentarium. BJU Int 2013;112:1046–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


