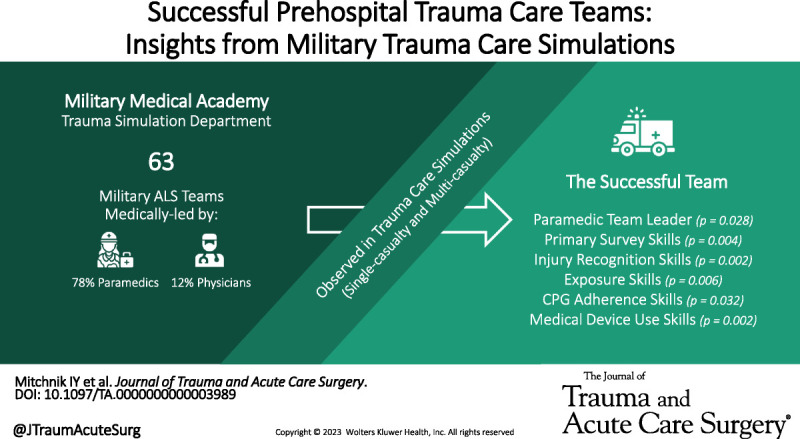
Findings from a study of military trauma care simulation teams reveal that paramedics are more likely to lead successful teams. #TraumaCare #MilitaryMedicine #Paramedics
KEY WORDS: Prehospital trauma care, trauma simulation, military paramedics, military physicians, Military Trauma Life Support (MTLS), Advanced Life Support (ALS) teams, trauma team performance
BACKGROUND
Trauma care teams play a crucial role in determining the outcomes of trauma victims. The composition and training of these teams can vary. Our study seeks to examine the characteristics of successful military Advanced Life Support (ALS) teams and the factors that affect them.
METHODS
A retrospective study was conducted at the Israel Defense Force (IDF) Military Medical Academy throughout 2021, where prehospital medical teams were observed in trauma care simulations. Teams were led by ALS providers (military physicians or paramedics) trained in IDF Military Trauma Life Support. Demographic and training data were collected. Teams were categorized into high or subpar performance groups based on simulation scores. Specific skills were assessed by trauma instructors using a points system. Scores were compared between the groups and analyzed for correlations with demographic and training data.
RESULTS
Overall, 63 team simulations were analyzed, with teams led by a military paramedic in 78% of simulations. The mean overall simulation performance was 81% ±6.2, and there were no differences in scores of single or multicasualty simulations. A total 3% of the teams achieved successful results and were more likely to have a paramedic as the ALS provider (p = 0.028). A sensitivity analysis excluding physicians was conducted and showed that high-performance teams had significantly higher skill assessments for primary survey (p = 0.004), injury recognition (p = 0.002), exposure (p = 0.006), adherence to clinical practice guidelines (p = 0.032), and medical device use (p = 0.002).
CONCLUSION
Our study found that ALS provider is associated with overall simulation performance in prehospital ALS teams, with military paramedics more likely to be successful. These findings have implications for the training and staffing of prehospital ALS teams, suggesting that teams should be composed accordingly and that training should focus on skills affected by the ALS provider type.
LEVEL OF EVIDENCE
Prognostic and Epidemiological; Level IV.
Trauma care teams play a crucial role in determining the outcomes for trauma victims.1 The composition of hospital trauma bay teams is generally consistent across different facilities.2 However, depending on the trauma system in place, the composition of prehospital Advanced Life Support (ALS) teams may differ.3 In addition, the training of these teams can vary depending on the country or region. Various organizations adopted different prehospital trauma care guidelines, such as Prehospital Trauma Life Support (PHTLS), Advanced Trauma Life Support (ATLS), and Trauma and Combat Casualty Care (TCCC).2,4,5 The Israel Defense Force (IDF) uses Military Trauma Life Support (MTLS) which was developed based on the Trauma and Combat Medicine branch clinical practice guidelines (CPGs).6
The efficiency of trauma care teams can be affected by several factors, including the composition of the team and the training or experience of its members.7,8 Teamwork is the essential component for optimal team function.7 Teamwork includes leadership and clear communication skills.9 While these skills may be dependent on the team leader's medical education,10 the performance of teams may also be improved using simulation training.11,12
The nature of prehospital treatment makes it difficult to study trauma performance in real-world scenarios.13,14 Simulation is a promising and effective method of learning as it allows for controlled environments.14,15 Accordingly, we aimed to determine the characteristics of high-performing prehospital ALS teams via the assessment of simulation scenarios. Our study seeks to fill this gap by examining the characteristics of successful military ALS teams and identifying factors that affect these characteristics. We hypothesized that leadership and team experience are the key factors contributing to the success of these teams.
METHODS
Study Design
This was a retrospective observational study of prehospital IDF medical teams participating in prehospital trauma care simulations at the IDF Military Medical Academy between January 2021 and December 2021. The study aimed to determine the characteristics of successful prehospital military ALS teams and the factors affecting their success. This study was approved by the institutional review board of the IDF and was exempt from informed consent, as no medical data were collected and the study was performed as part of quality improvement initiatives in the IDF Military Medical Academy (Approval 19.300). All personal data were kept confidential and used only for IDF Military Medical Academy studies. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline16 was used to ensure proper reporting of our findings (see Supplemental Digital Content for STROBE checklist; SDC1, http://links.lww.com/TA/C1000).
SETTING AND PARTICIPANTS
The IDF medical teams are tasked with providing Role 1 care in the field. These teams are generally composed of four individuals: two military medics, an incident commander, and an ALS provider who is either a physician or a paramedic, trained in IDF MTLS.6 These teams are offered annual allocations for supervised refresher training at the IDF Military Medical Academy's Trauma Instruction Department (see Supplemental Video File; SDC2, http://links.lww.com/TA/D2). Before arriving for their simulation training allocation, participating teams provide a detailed report outlining the composition and experience of each team member. Training sessions are a single-day event that includes a basic skills workshop, followed by one single casualty simulation and then one multicasualty simulation. Throughout the day, the teams are assessed using a trauma simulation assessment form developed by the Military Medical Academy (see Supplemental Digital Content for Skill Assessment form; SDC3, http://links.lww.com/TA/D3). At the end of the training session, teams receive feedback and are provided their assessment forms. We included all reports of teams who completed the entire training session and excluded those with missing information.
ALS PROVIDERS IN THE IDF
The IDF MTLS training is required by all military ALS providers (both active duty and reserves) to be certified to care for trauma victims in the IDF. The MTLS course is a 5-day course that includes didactic lectures and simulation training. The course is uniform for all types of ALS providers. To achieve MTLS certification, ALS providers must pass both a written and a practical examination. The written examination is a multiple-choice question test for IDF Trauma and Combat Medicine CPGs. The practical examination is a single casualty simulation assessed by military medics who are trained in MTLS instruction. The training of military physicians includes a reserve academic program at a civilian medical school followed by a medical officer's course which includes MTLS training. Military paramedics are enrolled in a civilian paramedic training program that includes PHTLS followed by a military paramedic course, which includes MTLS training. Annually, our organization trains up to 60 military physicians and 90 paramedics who are on active duty and fit for Role 1 field care. Due to military physician shortages and increased demand as primary care providers and officers, military paramedics are more commonly expected to be on call for medical emergencies within our organization.
Variables and Measures
Simulation scores were calculated for each team based on the sum of points received for each of the assessed criteria (SDC3). This assessment form was used since January 2021 and its format remained consistent during the study period. Each team was composed of different medical personnel who participated in a single training day. The simulations were conducted in a controlled environment and were evaluated by a pool of 10 trauma instructors with at least 6 months of simulation instruction experience. During the study period, these instructors performed a median of 10 simulations each (interquartile range [IQR], 7–13). Demographic and training data were collected for the ALS providers, including medical education (profession and MTLS examination scores) and their team seniority (the number of days they served in their ALS team since completing the MTLS course). All data were collected from the assessment forms used for this study (SDC3) and entered into a dedicated spreadsheet for statistical analysis.
Statistical Analyses
We characterized the performance of the medical teams using the overall simulation and specific skill scores, calculated based on the sum of points relative to the maximum possible score. Each skill (SDC3) was scored according to expected performance: 1 point if performance was inappropriate, 3 points if it was partially appropriate or expected, and 5 points if it was as expected. The correlations between these scores and demographic and training data were calculated.
After calculating the mean and standard deviation of the simulation scores, medical teams were categorized into “high performance” and “subpar performance” teams according to a z score of 0.5. Differences in the characteristics of these two groups were compared using Mann-Whitney U and Student t tests. Effect sizes were assessed using correlation coefficients. Calculations of interrater and intrarater reliabilities were not possible due to the retrospective nature of this study. Statistical analysis was performed using SPSS version 19.0 and Excel 2019. A p value of less than 0.05 was considered statistically significant.
RESULTS
During the study period, 76 team simulations were recorded. We excluded two records with missing ALS provider information, three records of teams that did not participate in a single casualty simulation, and eight records of teams that did not participate in a multicasualty simulation. Overall, 63 team simulations were analyzed (Fig. 1).
Figure 1.
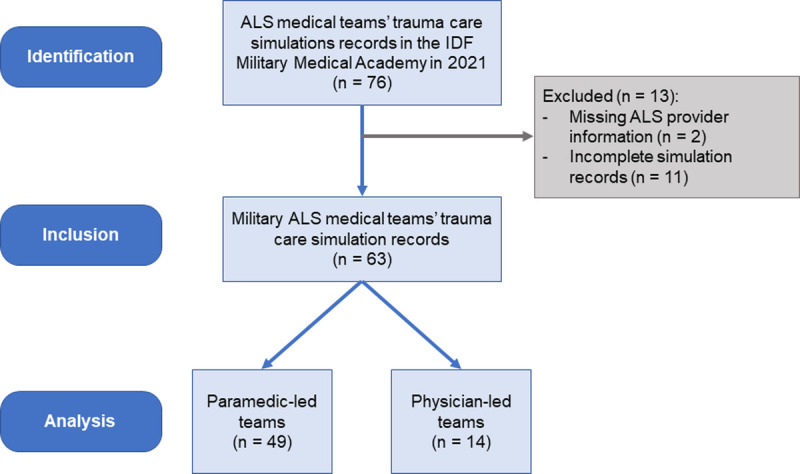
Study cohort flowchart.
Study Population
Teams included in the simulation analysis consisted of 38 of 63 (61%) battalion medical teams, 15 of 63 (24%) military intensive care ambulance teams, 6 of 63 (10%) military medical clinic teams, and 4 of 63 (6%) special forces medical teams. Teams were led by a paramedic in 49 of 63 (78%) simulations and a physician in 14 of 63 (22%) simulations. The ALS providers' median overall MTLS certification scores were 87 of 100 (IQR, 81–94) and their median team seniority was 234 days (IQR, 111–450 days).
Team Simulation Performance
The mean overall simulation performance was 81 ± 6.2% (95% confidence interval, 79–83). The single casualty simulation had a mean score of 80 ± 7.6% [78 to 82] and the multicasualty simulation had a mean score of 82 ± 7.6% [80–84]. Teams achieved a higher ranking on the team communication skill assessment in multicasualty simulations than in single casualty simulations (median, 5.0 compared with 3.0; p = 0.040). In casualty-single simulations, teams ranked higher than in multicasualty simulations on the information relaying skill assessment (5.0 compared with 3.0; p = 0.002). There were no differences in other skill assessments between single and multicasualty simulations.
The ALS provider profession significantly correlated with the rankings of injury recognition (Spearman's coefficient = 0.378, p = 0.002), exposure (0.306, p = 0.015), drug management (0.303, p = 0.016), and CPG adherence (0.255, p = 0.044). Team seniority significantly correlated with evacuation planning rankings (0.409, p = 0.001) as presented in Figure 2. There were no significant correlations between MTLS scores and assessment rankings. Overall, baseline characteristics did not correlate well with overall simulation performance on regression analysis (R2 = 0.174, p = 0.053). Advanced Life Support providers who were paramedics were the only significant factor associated with better overall simulation performance (regression coefficient, 4.869 [1.262–8.477]).
Figure 2.
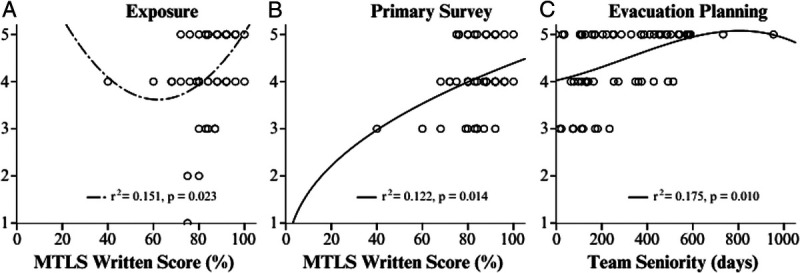
Significant correlations with skill assessments.
Successful Performances
The characteristics of high and subpar-performance teams are described in Table 1. Overall, 46 of 63 (73%) teams achieved successful results. The simulation score was significantly higher in high-performance teams, both in single casualty simulation (72% ±5.8 in subpar performance teams and 84% ±5.7 in high-performance teams, p < 0.001) and multicasualty simulation (74% ±5.5 in subpar performance teams and 85% ±5.9 in high-performance teams, p < 0.001). High-performance teams were more likely to have an ALS provider who is a paramedic (59% in subpar-performance teams vs. 85% in high-performance teams; p = 0.028). The odds ratio for medical teams to achieve high-performance scores given a paramedic in the team was 3.69 [1.01–13.45]. The type of ALS team, team seniority, and MTLS scores did not have significant effects on the simulation scores (Table 1).
TABLE 1.
Study Demographics
| Subpar Performance (n = 17) | High Performance (n = 46) | p | |
|---|---|---|---|
| ALS provider, n (%) | 0.028 | ||
| Paramedic | 10 (59%) | 39 (85%) | |
| Physician | 7 (41%) | 7 (15%) | |
| ALS team, n (%) | 0.343 | ||
| Special Forces Medical Team | 1 (6%) | 3 (7%) | |
| Military medical clinic | 3 (18%) | 3 (7%) | |
| Military intensive care ambulance | 2 (12%) | 13 (28%) | |
| Battalion Medical Team | 11 (65%) | 27 (59%) | |
| Team seniority, d (min–max) | 128 (75–386) | 253 (134–482) | 0.099 |
| MTLS score, n (%) | |||
| Written examination | 86 ± 6.6% | 84 ± 11.7% | 0.434 |
| Practical examination | 86 ± 7.4% | 87 ± 10.4% | 0.666 |
| Simulation score, n (%) | |||
| Single-casualty simulation | 72 ± 5.8% | 84 ± 5.7% | <0.001 |
| Multicasualty simulation | 74 ± 5.5% | 85 ± 5.9% | <0.001 |
IDF, Israel Defense Force; min, minimum; max, maximum.
PARAMEDIC-LED MEDICAL TEAMS SENSITIVITY ANALYSIS
Due to the significant effects of ALS Provider types on team success, we performed a sensitivity analysis excluding physician-led teams, to characterize successful paramedic-led teams. Overall, 39 of 49 (80%) paramedic-led medical teams achieved successful simulation performances. Paramedic-led medical teams that were high performance were characterized by significant differences in various skill assessments, including primary survey, injury recognition, exposure, adherence to CPGs, and medical device use (Table 2).
TABLE 2.
Comparison of Skill Scores Between Subpar and High-Performance Teams
| Assessment, M (IQR) | Subpar Performance (n = 10) | High Performance (n = 39) | p | Correlation effect Size | p |
|---|---|---|---|---|---|
| Primary survey | 3.5 (3.0–4.0) | 4.0 (3.5–4.5) | 0.004 | 0.436 | 0.002 |
| Injury recognition | 4.0 (3.5–4.5) | 5.0 (5.0–5.0) | 0.035 | 0.386 | 0.006 |
| Exposure | 3.0 (2.0–4.0) | 5.0 (4.0–5.0) | 0.006 | 0.419 | 0.002 |
| Adherence to CPG | 3.0 (3.0–3.0) | 4.0 (3.5–4.5) | 0.016 | 0.369 | 0.009 |
| Medical device use | 4.0 (4.0–4.0) | 5.0 (4.0–5.0) | 0.016 | 0.377 | 0.008 |
The table shows the comparison of skill scores between subpar and high-performance teams, where the scores are significantly higher in high-performance teams for all the skills assessed in the table. Each skill was assessed on a scale of 1–5, where 1 is inappropriate performance, 3 is partial performance, and 5 is expected performance. The correlation coefficients indicate moderate to strong statistically significant correlations.
High-performance paramedic-led teams had significantly higher scores in the primary survey (p = 0.004), exposure (p = 0.006), adherence to CPG (p = 0.016), and medical device use (p = 0.016) compared with subpar-performance teams. Similarly, the high-performance teams also had significantly higher scores in injury recognition (p = 0.035) compared with subpar-performance teams. The correlation and effect size (measured by Cohen's d) for each skill was also calculated, with values ranging from 0.369 to 0.436 for correlation and 0.006 to 0.009 for effect size. This suggests a moderate correlation and small to moderate effect size for these skills.
Military Trauma Life Supports written examination scores were significantly correlated with primary SURVEY rankings (Spearman's coefficient = 0.323, p = 0.023) and exposure rankings (0.321, p = 0.029). Primary survey assessments were especially ranked higher at single casualty simulations in high-performance teams (median, 5.0 compared with 3.0; p = 0.016). In multicasualty simulations, exposure skill assessments were especially ranked higher in high-performance teams (median, 5.0 compared with 3.0; p = 0.007). The correlation between team seniority and evacuation planning skills was found to be 0.409, with a p value of 0.001. An R2 value of 0.175 and a p value of 0.010 was found. Calculating the optimal team seniority time for high-performance simulation scores resulted in a range of 648 to 945 days (or 21–31 months). There were no other significant correlations between paramedic characteristics and successful teams' assessment rankings (Table 3).
TABLE 3.
Correlations Between ALS Provider's Factors and Simulation Scores
| ALS Provider Factors | Correlation | Effect Size | p |
|---|---|---|---|
| Military paramedic | |||
| Exposure | 0.306 | Medium | 0.015 |
| Injury recognition | 0.378 | Medium | 0.002 |
| Drug management | 0.303 | Medium | 0.016 |
| CPG adherence | 0.255 | Small | 0.044 |
| MTLS written examination score | |||
| Primary survey | 0.323 | Medium | 0.023 |
| R2 = 0.122, p = 0.014 | |||
| Exposure | 0.321 | Medium | 0.029 |
| R2 = 0.151, p = 0.023 | |||
| Team seniority | |||
| Evacuation planning | 0.409 | Medium | 0.001 |
| R2 = 0.175, p = 0.010 | |||
The table shows the correlations for the ALS provider factors with simulation scores. The R2 and p value are only given when the correlation is between an ALS provider factor and a simulation score.
The ALS Provider
Simulation performances were successful in 80% of paramedic and 50% of physician-led military medical teams (p = 0.028). Paramedics achieved a higher mean score of 82 ± 5.7% than the 77 ± 6.5% of physicians (p = 0.010). There were no significant differences in team seniority (p = 0.653) or MTLS examination scores (both written and practical) between paramedics and physicians (p = 0.521 and p = 0.766, respectively).
The overall rankings of ALS providers in different assessment criteria are presented in Figure 3. Paramedic-led teams achieved higher multicasualty simulation scores than physician-led teams (83 ± 7.4% compared with 78 ± 6.5%, p = 0.019), but there were no differences for single-casualty simulations (p = 0.067). On multicasualty simulations, paramedic-led teams ranked higher than physician-led teams in the primary survey (median rank, 3.4 compared with 2.5; p = 0.047). On single-casualty simulations, paramedic-led teams ranked higher in CPG adherence (3.4 compared with 2.5; p = 0.041) and drug management (3.3 compared with 2.3; p = 0.030). Overall, paramedic-led teams achieved higher rankings in injury recognition, exposure, and drug management skills (Fig. 3).
Figure 3.
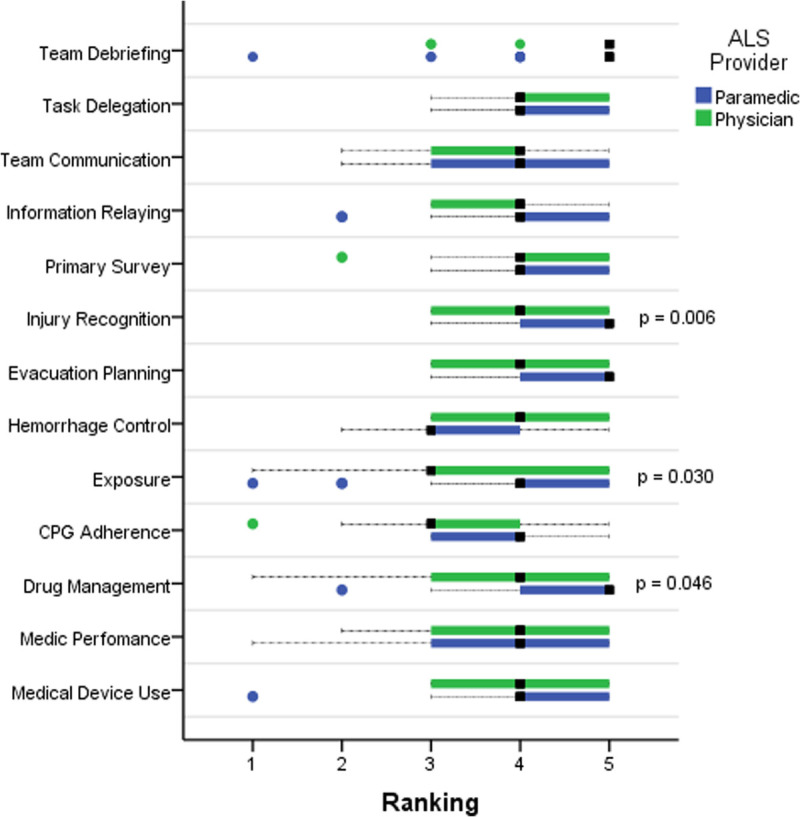
Performances of ALS providers on trauma care simulations Boxplot charts demonstrating the differences in median (black squares) ranking scores of ALS providers and their significance level (p).
DISCUSSION
This study aimed to learn about the characteristics of successful prehospital ALS teams. Using a prehospital trauma care simulated environment, it was found that the ALS provider's profession (physician vs. paramedic) was the only significant predictive factor for overall simulation performance. In a sensitivity analysis, successful paramedic-led ALS teams had significantly higher scores in primary survey, exposure, injury recognition, adherence to CPG, and medical device use skills. Successful prehospital medical teams were more likely to be led by a paramedic, and paramedics were found to excel in exposure, injury recognition, and drug management skills. In addition, we found that primary survey and exposure skills were positively affected by the ALS provider's MTLS training examination scores, whereas evacuation planning skills were affected by the ALS provider's team seniority.
The skills of primary survey and injury recognition are considered nontechnical, as they rely on cognitive, social, and personal resources.17 A commonly used tool for assessing nontechnical skills in trauma care teams is the Non-Technical Skills Scale for Trauma (T-NOTECHS), which is a five-item scale that has been validated in both real-life and simulation scenarios and is associated with improved performance of trauma teams.18,19 The T-NOTECHS includes the Assessment and Decision Making domain, which evaluates the team's ability to perform orderly and complete primary and secondary surveys and effectively communicate their findings and plan. Research suggests that nontechnical skills play an important role in the performance of prehospital ALS teams,20,21 as they may impact the time for diagnosis and treatment and ultimately benefit patient outcomes by reducing prehospital stabilization time and expediting prompt evacuation to definitive care.
The skills for exposure, CPG adherence, drug management, and medical device use are technical in nature, relying on technique and theoretical knowledge. Technical skills are affected by nontechnical skills, especially those of the team leader.22 An orderly primary survey includes a thorough exposure procedure to seek potentially missed injuries. Accurate injury recognition by the ALS provider affects their choice of the appropriate CPG to follow, as well as any use of drugs or medical devices.
A significant body of research has investigated factors affecting in-hospital trauma team performance.23 However, few studies have evaluated the performance of prehospital medical teams. Nagaraj et al.24 reported how higher nontechnical team skill assessments correlated with improved patient hand-off. Herzberg et al.25 demonstrated that improved prehospital teamwork skills are related to reduced rates of medical errors. Our study shows that successful prehospital medical teams are characterized by good nontechnical decision-making skills and good technical skills for thorough primary surveys and knowledge of CPGs, drugs, and medical devices.
Prehospital military ALS teams led by paramedics were more likely to perform successfully in prehospital trauma care simulations compared with teams led by physicians. Our study shows that paramedics outperformed physicians in the technical skills of exposure and drug management and the nontechnical decision-making skill of injury recognition. In addition, paramedics had a positive impact on CPG adherence skill assessments in single-casualty simulations and primary survey skill assessments in multicasualty simulations. The greatest disparities in overall performance between paramedics and physicians were observed in scenarios involving multiple casualties.
A systematic review by Garner et al.26 showed better endotracheal intubation outcomes in pediatric patients treated by prehospital physician teams rather than paramedic teams. In contrast, Fullerton et al. and McQueen et al.27,28 found no significant differences between prehospital physicians and paramedics tending to adult patients, attributing this to high levels of experience. It is possible that in our cohort, paramedics have more prehospital clinical experience than physicians due to their civilian training in ambulance services. Levy et al.29 demonstrated these technical skill differences when they examined whether military physicians and paramedics are interchangeable in military operations. While these disparities may explain the differences we have observed in technical skill assessments, a systematic review by Dyson et al.30 did not find clear evidence for an association between ALS provider experience and technical ALS skill outcomes.
Roberts et al.31 demonstrated that the addition of physicians to paramedic teams improved nontechnical decision-making skills. Similarly, Benov et al.32 described how military physicians performed more accurate triage than paramedics and suggested this was due to differences in medical education. This strengthens our observation that MTLS knowledge affected the nontechnical primary survey skill (Fig. 2B and Table 2). However, our study also showed that paramedics demonstrated better injury recognition skills (Fig. 3) and multicasualty simulation performance despite comparable MTLS training scores. The strength of our study is that it observed ALS provider performance in situ, rather than relying on recall and documentation, which may be subject to bias. These results require further studies to ascertain the causes for differences in technical and nontechnical skill assessments between paramedics and physicians.
Our findings have implications for the training of prehospital ALS teams. The study suggests that paramedics may be better suited for prehospital trauma care. In cases where a dilemma concerning whether a physician or a paramedic should be emergently deployed for trauma care, the latter appears to be a safe option. It also suggests that training should focus on the skills that are affected by the ALS provider type such as exposure, injury recognition, CPG adherence, and drug management. For example, scrutinizing exposure skill assessments (such as complete removal of clothes during training and rigorous screening for hidden injuries hidden by simulation instructors), case discussions concerning injury recognitions and suitable CPG algorithms, and memorizing drug indications, dosages, and side effects throughout training. Perhaps, military physician training should incorporate some additional aspects of paramedic training, such as joining ambulance teams during their medical education. In addition, the study suggests that the seniority of the team should be considered when deploying teams to missions that require careful planning of evacuation strategies. For example, if a mission is expected to require complicated evacuations in case of a trauma emergency, the most senior ALS provider should be deployed for the mission.
The major limitation of this study is its retrospective design, convenience sampling with heterogenic simulations, and various assessors which limits the ability to adjust our results to a single standardized scenario. The score sheet utilized in this study has not been validated in other organizations, and we were not able to measure its reliability due to trauma instructor heterogeneities and since it was not possible to test the same team twice. Our study is further limited by its power, due to the relatively small sample size. Some differences between paramedics and physicians may not have been discovered. In addition, our study only used a 1-day training session, which may not fully capture the teams' abilities in real-life situations. Lastly, the composition and training of the IDF medical teams may be different from the composition of other prehospital medical teams around the globe.
In conclusion, our study provides evidence that paramedics outperformed physicians in prehospital trauma care simulations, suggesting that they may be a viable alternative to physician deployment in this context. The type of ALS provider profession is a significant predictor of overall simulation performance in prehospital ALS teams, and both technical and nontechnical skills may be influenced by the ALS provider's medical education. The differences in technical and nontechnical skills between paramedics and physicians, such as exposure, injury recognition, CPG adherence, and drug management, suggest that a more tailored approach to skills training may be beneficial for different types of ALS providers. Further research to explore which unique aspects of paramedic training may contribute to these skills is warranted, as these findings may have implications for the training and staffing of prehospital ALS teams.
Supplementary Material
AUTHORSHIP
I.Y.M. participated in the study design, data collection, data analysis, and article writing. T.T., B.F., O.A., and I.F. participated in the critical revision.
DISCLOSURE
The authors declare no funding or conflicts of interest.
This study does not represent the official views of the Israel Defense Force (IDF) Medical Corps.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Tomer Talmy, Email: ttalmy@gmail.com.
Barak Feldman, Email: feld.barak@gmail.com.
Ofer Almog, Email: ofer18181@gmail.com.
Itay Fogel, Email: fogelitay@gmail.com.
REFERENCES
- 1.van Maarseveen OEC, Huijsmans RLN, Leenen LPH, Ham WHW. Variation of in-hospital trauma team staffing: new resuscitation, new team. BMC Emerg Med. 2022;22(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American College of Surgeons, Committee on Trauma . Advanced Trauma Life Support: Student Course Manual. 10th ed. Chicago, IL: American College of Surgeons; 2018. [Google Scholar]
- 3.Wilson MH, Habig K, Wright C, Hughes A, Davies G, Imray CHE. Pre-hospital emergency medicine. Lancet. 2015;386(10012):2526–2534. [DOI] [PubMed] [Google Scholar]
- 4.National Association of Emergency Medical Technicians (NA) . PHTLS: Prehospital Trauma Life Support. 9th ed. Jones & Bartlett Learning; 2020. [Google Scholar]
- 5.Scott TE, Stuke L. Prehospital damage control resuscitation. Damage Control in Trauma Care: An Evolving Comprehensive Team Approach. 2018;71–83. [Google Scholar]
- 6.Scope A, Lynn M, Farkash U, Zeev F, Goldberg A, Eldad A. Military trauma life support: a comprehensive training program for military physicians. Mil Med. 2001;166(5):385–388. [PubMed] [Google Scholar]
- 7.Murphy M, Curtis K, McCloughen A. What is the impact of multidisciplinary team simulation training on team performance and efficiency of patient care? An integrative review. Australas Emerg Nurs J. 2016;19(1):44–53. [DOI] [PubMed] [Google Scholar]
- 8.Speck RM, Jones G, Barg FK, McCunn M. Team composition and perceived roles of team members in the trauma bay. J Trauma Nurs. 2012;19(3):133–138. [DOI] [PubMed] [Google Scholar]
- 9.Schmutz JB, Meier LL, Manser T. How effective is teamwork really? The relationship between teamwork and performance in healthcare teams: a systematic review and meta-analysis. BMJ Open. 2019;9(9):e028280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steinemann S Bhatt A Suares G Wei A Ho N Kurosawa G, et al. Trauma team discord and the role of briefing. J Trauma Acute Care Surg. 2016;81(1):184–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller D, Crandall C, Washington C, 3rd, McLaughlin S. Improving teamwork and communication in trauma care through in situ simulations. Acad Emerg Med. 2012;19(5):608–612. [DOI] [PubMed] [Google Scholar]
- 12.Roberts NK Williams RG Schwind CJ Sutyak JA McDowell C Griffen D, et al. The impact of brief team communication, leadership and team behavior training on ad hoc team performance in trauma care settings. Am J Surg. 2014;207(2):170–178. [DOI] [PubMed] [Google Scholar]
- 13.McManamny T, Sheen J, Boyd L, Jennings PA. Mixed methods and its application in prehospital research. J Mixed Methods Res. 2015;9(3):214–231. [Google Scholar]
- 14.Maurin Söderholm H, Andersson H, Backlund P, Bergman J, Lundberg L, Sjöqvist BA. Research challenges in prehospital care: the need for a simulation-based prehospital research laboratory. Adv Simul (Lond). 2019;4(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abelsson A, Rystedt I, Suserud B-O, Lindwall L. Learning by simulation in prehospital emergency care—an integrative literature review. Scand J Caring Sci. 2016;30(2):234–240. [DOI] [PubMed] [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. [DOI] [PubMed] [Google Scholar]
- 17.Flin R, O’Connor P, Crichton M. Safety at the Sharp End. CRC Press; 2017. [Google Scholar]
- 18.Steinemann S Berg B DiTullio A Skinner A Terada K Anzelon K, et al. Assessing teamwork in the trauma bay: introduction of a modified “NOTECHS” scale for trauma. Am J Surg. 2012;203(1):69–75. [DOI] [PubMed] [Google Scholar]
- 19.Stevenson C, Bhangu A, Jung JJ, MacDonald A, Nolan B. The development and measurement properties of the trauma NOn-TECHnical skills (T-NOTECHS) scale: a scoping review. Am J Surg. 2022;224:1115–1125. [DOI] [PubMed] [Google Scholar]
- 20.El-Shafy IA, Delgado J, Akerman M, Bullaro F, Christopherson NAM, Prince JM. Closed-loop communication improves task completion in pediatric trauma resuscitation. J Surg Educ. 2018;75(1):58–64. [DOI] [PubMed] [Google Scholar]
- 21.Dumas RP Vella MA Chreiman KC Smith BP Subramanian M Maher Z, et al. Team assessment and decision making is associated with outcomes: a trauma video review analysis. J Surg Res. 2020;246:544–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krage R Zwaan L Tjon Soei Len L Kolenbrander MW van Groeningen D Loer SA, et al. Relationship between non-technical skills and technical performance during cardiopulmonary resuscitation: does stress have an influence? Emerg Med J. 2017;34(11):728–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barach P, Weinger M. Trauma Team Performance. In: Trauma. CRC Press; 2007. [Google Scholar]
- 24.Nagaraj MB Lowe JE Marinica AL Morshedi BB Isaacs SM Miller BL, et al. Using trauma video review to assess EMS handoff and trauma team non-technical skills. Prehosp Emerg Care. 2023;27(1):10–17. [DOI] [PubMed] [Google Scholar]
- 25.Herzberg S Hansen M Schoonover A Skarica B McNulty J Harrod T, et al. Association between measured teamwork and medical errors: an observational study of prehospital care in the USA. BMJ Open. 2019;9(10):e025314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garner AA, Bennett N, Weatherall A, Lee A. Success and complications by team composition for prehospital paediatric intubation: a systematic review and meta-analysis. Crit Care. 2020;24(1):149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fullerton JN, Roberts KJ, Wyse M. Can experienced paramedics perform tracheal intubation at cardiac arrests? Five years experience of a regional air ambulance service in the UK. Resuscitation. 2009;80(12):1342–1345. [DOI] [PubMed] [Google Scholar]
- 28.McQueen C Crombie N Hulme J Cormack S Hussain N Ludwig F, et al. Prehospital anaesthesia performed by physician/critical care paramedic teams in a major trauma network in the UK: a 12 month review of practice. Emerg Med J. 2015;32(1):65–69. [DOI] [PubMed] [Google Scholar]
- 29.Levy G Goldstein L Erez Y Levite R Bar U Marmor M, et al. Physician versus paramedic in the setting of ground forces operations: are they interchangeable? Mil Med. 2007;172(3):301–305. [DOI] [PubMed] [Google Scholar]
- 30.Weiss N Ross E Cooley C Polk J Velasquez C Harper S, et al. Does experience matter? Paramedic cardiac resuscitation experience effect on out-of-hospital cardiac arrest outcomes. Prehosp Emerg Care. 2018;22(3):332–337. [DOI] [PubMed] [Google Scholar]
- 31.Roberts K, Blethyn K, Foreman M, Bleetman A. Influence of air ambulance doctors on on-scene times, clinical interventions, decision-making and independent paramedic practice. Emerg Med J. 2009;26(2):128–134. [DOI] [PubMed] [Google Scholar]
- 32.Benov A Glassberg E Nadler R Gendler S Erlich T Bader T, et al. Role I trauma experience of the Israeli Defense Forces on the Syrian border. J Trauma Acute Care Surg. 2014;77(3):S71–S76. [DOI] [PubMed] [Google Scholar]


