Combat readiness for surgeons without trauma fellowships training requires integration of civilian and military entities. We demonstrate the impact a regional partnership can have on readiness, litigation claims and impacts from graduate medical education.
KEY WORDS: Military surgery, trauma surgery, combat readiness, Feres doctrine
BACKGROUND
Appropriate operative volume remains a critical component in mitigating surgical atrophy and maintaining clinical competency. The initiation of military-civilian surgical partnerships (MCPs) has been proposed for addressing knowledge, skills, and abilities (KSA) metrics to address concerns over operational readiness and the low acuity experienced by military surgeons. This study investigates the first partnership for Navy surgical staff at a nonacademic Military Treatment Facility (MTF) with a regional academic Army Military Treatment Facility (AMTF) and a civilian, nonacademic level II trauma center devised to improve operational readiness for attending surgeons. We hypothesize that a skill sustainment MCP will allow military surgeons to meet combat readiness standards as measured by the KSA metric.
METHODS
A memorandum of understanding was initiated between the Navy Military Treatment Facility (NMTF), the AMTF, and the level II civilian trauma center (CTC). The single military surgeon in this study was classified as “voluntary faculty” at the CTC. Total case volume and acuity were recorded over an 11-month period. Knowledge, skills, and abilities metrics were calculated using the standard national provider identifier number and the novel case-log based method.
RESULTS
A total of 156 cases were completed by a single surgeon over the study period, averaging 52 cases per institution. Significantly more KSAs were obtained at the CTC compared with NMTF (5,954 vs. 2,707; p < 0.001). Significantly more emergent cases were observed at the CTC compared with the MTFs (χ2 = 7.1, n = 96, p < 0.05). At a single site, AMTF, a significant difference in the calculated KSA score, was observed between the national provider identifier and case-log methods (5,278 vs. 3,297; p = 0.04).
CONCLUSION
The skill sustainment MCP between NMTF and CTC increased surgical readiness and exposed surgeons to increased operative acuity. The voluntary faculty model reduces direct litigation exposure and encourages clinical competency for military surgeons while remaining a deployable asset to the global military effort.
LEVEL OF EVIDENCE
Therapeutic/Care Management; Level IV.
Low surgical volume may lead to decreased combat surgical readiness for military surgeons.1 Low volume combined with low operative complexity exacerbates this readiness issue. The dynamics underlying low volume and complexity within the military health care system (MHS) have previously been well described.2–6
As presented by British Royal Navy Surgeon VADM Alasdair Walker, the “Walker Dip” phenomenon describes the poor or degraded transfer of knowledge, skills, and abilities (KSA) between experienced combat surgeons and junior military surgeons who enter military service during times of peace.2–5 This peacetime paradox reduces surgical combat readiness by charging the surgeon's home Military Treatment Facility (MTF) with the responsibility of combat skill sustainment, for which the criterion standard is operative trauma.4 Reliance on a domestic or overseas MTF for maintenance of complex combat surgical skills does not supply sufficient operative trauma to maintain combat readiness for the majority of military surgeons.3,4,7 Therefore, a metric was designed to translate peacetime surgical volume into an objective metric for combat readiness. The result was the development of the KSA metric. The KSA metric for general surgery reflects the specific 484 KSAs that a consortium of trauma surgeons with extensive deployment experience, the American College of Surgeons, and relevant literature deemed most useful to the deployed general surgeon.8 A total of 2,000 current procedural terminology (CPT) codes were then tied to those 484 KSAs, with each CPT code carrying a variable value based on the relevance to combat readiness; for example, an inguinal hernia might carry a KSA value of 67 “points,” while a traumatic splenectomy might carry a KSA value of 171 points (Fig. 1). To be deemed deployable, general surgeons currently target an annual minimum goal of 14,000 KSAs points.8 Currently, KSAs can only be tracked for cases completed at MTFs; thus, KSAs obtained at civilian centers are not tracked and only calculated for research purposes. The KSA metric is one part on a continuum of readiness designed to maintain a combat ready force of military surgeons.9,10 Recent studies have demonstrated that only 10.8% of military surgeons are combat ready based on KSA thresholds.1 Currently, the KSA metric is the most widely accepted value used to “translate” peacetime operative volume into potential combat readiness.10
Figure 1.
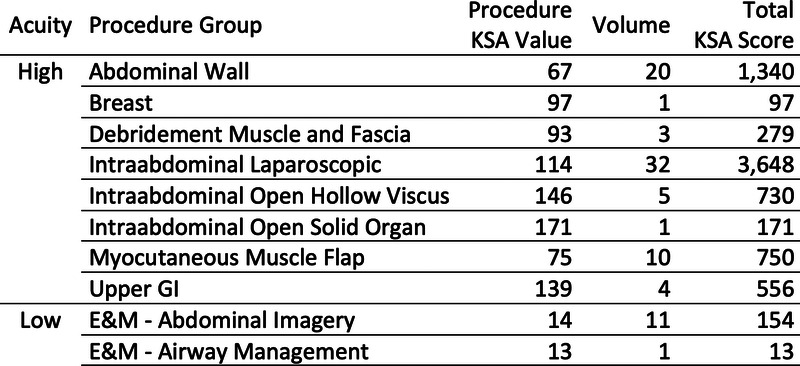
Sample of KSA value per procedural group.
Outside of the MHS, there are five types of military-civilian partnerships (MCPs) that allow military surgeons to augment their KSAs and maintain operative skill sets; three variations are relevant to this research and will be subsequently described.2 Integrated MCPs consist of a 3-year contractual agreement whereby a trauma fellowship–trained military surgeon is embedded within a level 1 civilian trauma team.2 The military surgeon functions as a fully credentialed staff surgeon, which typically includes billing for all services rendered and independently covering intensive care unit (ICU) call. These partnerships support one to two military trauma surgeons per program and are funded by the military (salary support, housing allowance, and full active duty benefits). In addition, given the financial incentive to having a military surgeon on staff, civilian institutions commonly provide malpractice insurance for the embedded military surgeon.
Skill sustainment MCPs consist of military surgeons rotating at a local civilian trauma center while remaining on staff at a regional MTF.2 There are four important distinctions between the integrated and skill sustainment partnerships. Principally, military surgeons participating in a skill sustainment partnership do not need to be trauma fellowship trained, greatly expanding the potential pool of participants. Second, skill sustainment participants are not fully embedded within the civilian institution and remain “immediately deployable assets” with retention of significant collateral duties at their home MTF. Third, skill sustainment participants can be recognized by the civilian institution as “volunteer clinical faculty” since the individual is not fully embedded. This designation requires military surgeons to be supervised by civilian faculty but importantly removes the potential need for additional malpractice coverage for the military surgeon when acting in this capacity. Finally, the number of supported military surgeons in a skill sustainment partnership is limited only by the capacity of the civilian institution.
Just-in-time MCPs embed a military medical team within a level 1 trauma center 2 to 12 weeks before a scheduled deployment.2 These partnerships function to build team cohesion and expose the medical team, partly through the effects of “active shadowing,” to as many trauma scenarios, resuscitations, and cases as possible to reflect the combat environment.
Using the principals detailed in the MHS Strategic Partnership with the American College of Surgeons (MHSSPACS) Blue Book: Military-Civilian Partnerships for Trauma Training, Sustainment and Readiness, we sought to build an MCP in Navy Region Northwest. We hypothesize that a regional skill sustainment MCP will allow military surgeons to meet combat readiness standards as measured by the KSA metric.9
PATIENTS AND METHODS
The military health care marketplace in the Pacific Northwest is centered around a Navy Military Treatment Facility (NMTF) and an Army Military Treatment Facility (AMTF). Navy Military Treatment Facility is an outpatient surgical center supporting the Navy's mission in the Pacific Northwest and is the home facility for the single surgeon assigned to it. There is no Graduate Medical Education (GME) component within the department of surgery at NMTF. South of NMTF is the AMTF where Navy surgeons cover the Trauma and Acute Care Surgery service call with full independent practice authority. Army Military Treatment Facility is a level 2 trauma center and boasts a full complement of surgical residents and four trauma fellowship–trained staff surgeons.
The civilian trauma landscape includes a centrally located academic level 1 trauma center buttressed by two level II trauma centers to the North and South. The northern level II civilian trauma center (CTC) is staffed with 8.5 trauma fellowship–trained surgeons. There are more than 4,000 trauma registry patients and 2,600 trauma activations at CTC per year with just under a 10% penetrating injury rate. In addition to trauma and critical care (surgical ICU coverage), the Trauma and Acute Care Surgery group also covers emergency general surgery (EGS), completing just more than 1,500 EGS cases per year. There is no surgical GME complement.
After evaluating these institutions, a memorandum of understanding between NMTF and CTC was developed.9 The legal representatives from each institution contributed to the unique characteristics shaping the MCP. Navy MTF is currently staffed with one surgeon who is board certified and licensed in the state of Washington. The NMTF staff surgeon is not trauma fellowship trained; therefore, they were not permitted to independently cover surgical ICU call at CTC (internal policy). This requirement is common among most major trauma centers and an American College of Surgeons requirement for all surgical ICU directors.11 Furthermore, although not an explicit requirement, it is highly encouraged for all CTC providers covering trauma call to be fellowship trained in surgical critical care (Jacob Glaser, MD, Personal verbal communication, July 2021). To address the aforementioned concerns, as well as any legal concerns regarding the need for additional malpractice insurance, partnered surgeons were designated as “volunteer faculty,” working directly under the supervision of a CTC staff surgeon.
Institutional review board exemption for human subjects research was obtained. From September 2021 to August 2022, personal case logs from each of the three participating institutions (NMTF, AMTF, CTC) were collected. At the end of the study period, operative case logs were submitted to a third-party government contractor charged with calculating KSA scores for the entire MHS. The KSA scores were calculated using two different standard methods. First, the KSA was calculated using the surgeon's national provider identifier number (NPI) and tracking all CPT codes within the MTF database linked to that unique NPI number. These CPT codes are then “translated” to KSA points, and a final KSA score is generated. This is the standard method of KSA calculation for the MHS and is referred to as the “CAPER/M2” score. Second, the KSA score was calculated based only on the procedures submitted from the case log record. Since CTC is not within the MHS, KSA scores can only be calculated using personal case log data and not with the CAPER/M2 method. Additional metrics were prospectively collected including hours spent at each institution, acuity of operative cases (emergent, urgent, and elective), and number of cases involving surgical residents. Emergent operation is defined as having the patient on the operating room table within 1 hour of arrival, and urgent is defined as having the patient on the operating room table within 5 hours of arrival. Continuous variables were compared using the Student's t test, while categorical variables were compared using the χ2 statistic. Significance was defined as p < 0.05. The STrengthening the Reporting of OBservational studies in Epidemiology guideline was used to ensure proper reporting of methods, results, and discussion (Supplemental Digital Content, Supplementary Data 1, http://links.lww.com/TA/D26).
RESULTS
Table 1 shows the KSAs completed at each institution using the case log and CAPER/M2 data sets. There was a significant difference in CAPER/M2 and case log data set with respect to the KSA volume completed at AMTF (5,827 vs. 3,297, p = 0.04). This concerning finding prompted interpretation of the results to be based on both data sets separately.
TABLE 1.
Operative Volume and KSA Data
| Case Log | CAPER/M2 | |||
|---|---|---|---|---|
| Volume | KSA | Volume | KSA | |
| NMTF | 54 | 2,707 | 39 | 2,098 |
| AMTF | 52 | 5,827 | 35 | 3,297 |
| CTC | 50 | 5,954 | — | — |
Case Log Data Set Results
Table 2 demonstrates the number of hours spent at each institution and the subsequent rate of KSA per hour attainment per institution. Table 3 demonstrates a significant difference between the amount of KSAs obtained at NMTF and CTC (2,707 vs. 5,954; p < 0.0001). The KSA analysis was not significantly different between CTC and AMTF (5,954 vs. 5,287; p = 0.6) or CTC and all KSAs obtained at a military installation (AMTF-NMTF) (5,954 vs. 8,534, p = 0.5). Table 4 highlights the operative volume of emergent versus urgent cases for AMTF and CTC. The data demonstrate a significantly higher observed volume of emergent cases at CTC compared with AMTF (χ2 = 7.1, n = 96, p < 0.05). Since emergent cases resulted from EGS consults and trauma activations, we sought to identify only those cases resultant from traumatic indications. Six operative trauma cases were identified; 100% of these cases were completed at the CTC accounting for a KSA volume of 645.
TABLE 2.
Metrics of Effort
| NMTF | AMTF | CTC | |
|---|---|---|---|
| Time analysis | |||
| Case volume | 54 | 52 | 50 |
| Time at facility, h | 912 | 816 | 504 |
| KSA analysis | |||
| KSA per h | 3 | 7 | 12 |
| KSA per case | 17 | 112 | 119 |
TABLE 3.
KSA Analysis
| Case Log Analysis | ||
|---|---|---|
| KSA | p* | |
| CTC | 5,954 | <0.001 |
| NMTF | 2,707 | |
| CTC | 5,954 | 0.6 |
| AMTF | 5,287 | |
| AMTF-NMTF | 8,534 | 0.4 |
| CTC | 5,954 | |
| CAPER Analysis | ||
|---|---|---|
| KSA | p* | |
| CTC | 5,954 | 0.004 |
| NMTF | 2,098 | |
| CTC | 5,954 | 0.008 |
| AMTF | 3,297 | |
| AMTF-NMTF | 5,395 | 0.19 |
| CTC | 5,954 | |
*p calculated using Student's t test.
TABLE 4.
Case Categorization
| Emergent Cases | Urgent Cases | p* | |
|---|---|---|---|
| n (%) | n (%) | ||
| AMTF | 4 (8) | 42 (92) | <0.007 |
| CTC | 34 (68) | 16 (32) |
*p calculated using χ2 analysis.
CAPER/M2 Data Set Results
When using the CAPER/M2 data set, the significant difference between NMTF versus CTC KSA scores persisted (2,098 vs. 5,954, p < 0.004); however, a new significant difference was identified between KSAs obtained at AMTF versus CTC (3,297 vs. 5,954 p = 0.008) (Table 3). There was no difference observed when combining all KSAs obtained at a military installation (AMTF-NMTF) to CTC (5,395 vs. 5,954, p = 0.19).
DISCUSSION
The only operative cases completed in the combat setting are traumatic and emergent in nature; therefore, trauma readiness is critical to the success of all military surgeons and the wartime surgery effort. Trauma trained military surgeons can leverage their fellowship training to maintain readiness through numerous programs ranging from embedded partnerships to “moonlighting” engagements. Military surgeons who are not trauma fellowship trained are held to the same standards as trauma trained surgeons when operating in the deployed setting; however, the readiness opportunities available to these two groups are not equal. Therefore, identifying a supporting institution with the highest volume of emergent operative cases from trauma and EGS is critical for the success of the non–trauma-trained surgeon in the combat setting. As highlighted in Table 4, CTC exposes the non–trauma-trained surgeon to the highest volume of emergent operative cases in the region. Furthermore, the CTC accounted for 100% of the operative volume secondary to trauma, despite the relatively low case volume and subsequent KSA value, reflecting the critical nature of this MCP. The volunteer faculty designation was adopted out of recognition for the CTC staff as subject matter experts (SMEs) in the field of trauma surgery; abstaining from the opportunity to learn from SMEs is discouraged within the military.
Voluntary Faculty Model
The potential reduction in autonomy created by the volunteer faculty designation invites criticism; however, practicing within this model promotes and achieves numerous readiness goals. Principally, this model allows non–trauma-fellowship-trained surgeons to participate in patient care within the structure of a highly specialized civilian trauma facility. Second, the model allows for technical skill acquisition through direct mentorship with SMEs in the field. Third, since the surgeons in this MCP are not protected from combat deployments, it is important that the absence of military surgeons from the MCP does not destabilize the civilian trauma call pool. Remaining an immediately deployable asset, while still participating in the MCP, is a strength of the skill sustainment MCP. This latter principal is in line with the MHSSPACS: Blue Book guidance9 and in contrast to the ‘”partially deployable” status imbued on integrated MCP participants. Finally, maintaining a direct presence within the surgeon's military command is critical for the development of a military officer12 and distinct from the benefits offered at civilian institutions or within the integrated MCP model. Ruggero et al.13 recently published their experience with three non–fellowship-trained surgeons using the “voluntary faculty” model at a level 1 trauma center. They report over a 12-month period, covering 12 calls lasting 24 hours per call the accumulation of 11,683 KSAs with an average of 3,894 KSA per surgeon.13 The current study further supports the generation of a substantial volume of KSAs to be completed at civilian institutions. Importantly, in the study by Ruggero et al.,13 it is unclear what impact GME held on the experiential learning of the military surgeon, and in the current study, there was no GME component. In addition, the current data include EGS cases in the overall KSA score. Finally, 20% of the total hours worked were completed at the CTC; this percentage is not standardized for MCP participation, but in the current study, there was no degradation in associated military responsibilities experienced by the military surgeon.
There is no widely accepted KSA target for MCPs; however, an objective framework for evaluating potential civilian partnerships,12 in conjunction with these two studies, present a baseline for building an MCP that supports combat readiness while encouraging military career development for non–fellowship-trained military surgeons.
Split Services
Interestingly, if a civilian institution splits its trauma and EGS service lines, the non–trauma-fellowship-trained military surgeon can theoretically cover the EGS service, working alongside the trauma surgeon when available. In this scenario, the military surgeon could practice independently, bill for services rendered, and still participate in trauma activations and operations. However, if the volume within an institution supports the separation of EGS and trauma, the military surgeon will likely be occupied with EGS cases and patient care throughout the shift, negatively impacting the development of trauma/critical care combat readiness.
Malpractice Insurance
The federal government is a sovereign entity and thus immune to litigation. Military surgeons are Department of Defense (DOD) health care providers and, therefore, as agents of a sovereign government, protected from individual litigation.14 The Federal Tort Claims Act of 1940 breaks the immunity of the government and allows certain lawsuits, including civilians charging malpractice by a federal employee, to be brought against the government.15 Critically, when a malpractice claim is brought against a military physician liability shifts from the physician to the federal government.14 The Federal Tort Claims Act grants the government the authority to adjudicate any claims brought against it through a structured settlement process.16 This unique situation regarding liability is a common vein of confusion for developing MCPs, manifesting as legal resistance to finalizing a memorandum of understanding between the two institutions.
Importantly, the subsequent decision of Feres v United States17 by the Supreme Court in 1950 upheld the immunity of the federal government from malpractice claims filed by active duty service members. The Feres doctrine only referenced claims brought by active duty service members and holds no precedent for adjudicating claims brought by civilians. It is not the Feres doctrine that shields DOD physicians from civilian malpractice litigation; it is their status as agents of the federal government. The Feres doctrine should not be extrapolated to represent any type of malpractice insurance or immunity for DOD health care providers functioning as attending physicians within the civilian sector. Therefore, when framework publications including the MHSSPACS: Blue Book state that “The Feres doctrine prevents military health care professionals from being sued for malpractice. There are several ongoing legal arguments about the validity of Feres when applied to civilian patients… Regardless, the Feres doctrine… may not be acceptable to many civilian institutions that will still require malpractice coverage for participating military personnel,”9 it is clear to see why there is stark legal resistance from civilian institutions toward granting military physicians unrestricted privileges.
For this specific study, the CTC did not accept the Feres doctrine as sufficient legal protection and required use of either the voluntary faculty model or additional malpractice insurance to be obtained for the participating military physicians. The military participants chose to engage the voluntary faculty model because of the added benefit of working with SMEs in the field of trauma. Certain MCPs may not benefit from voluntary faculty model, and if the civilian institution requires additional malpractice coverage, the authors find the framework where the civilian institution adds the military surgeon to the group insurance policy to be the most palatable outcome.
Graduate Medical Education
To date, the model described in the present study is the only MCP where military surgeons do not interact with surgical residents. Developing an MCP outside of a teaching institution is challenging and risks missing the benefit of surgical mentorship and the culture of learning inherent to major academic centers; however, if the cornerstone upon which the nonacademic MCP is built is mentorship, success will follow. At the CTC, there is a Navy reservist on staff who mentored both the CTC faculty and the military surgeon throughout the study period. This mentorship included defining roles and responsibilities for all parties and translating to the CTC leadership how impactful the MCP could be for military readiness. The impact of a liaison between the military surgeon and the CTC cannot be understated.18 In the current study, the only major academic center in the region has a well-established MCP; however, it requires participants to be trauma fellowship trained and thus excluded the current military surgeon. While academic centers are strong options for new MCPs, when regional limitations exist, novel partnerships must be evaluated.
Finally, this study highlights several other known limitations of reliance on KSA data. We demonstrate the challenges to using provider NPI numbers to generate accurate KSA values. Discordant KSA values between CAPER/M2 and case log data are dangerous and hold the potential to deem surgeons “combat ready” who are otherwise unprepared. This specific issue has been raised to the national level for further investigation. In addition, we raise the question of KSA assignment specifically at teaching institutions: if a chief resident competently completes a case without input from the attending, should the entire KSAs value be assigned to the attending? This question has yet to be evaluated; however, at the CTC, all KSAs recorded by the military surgeon were completed as the primary operator. In conclusion, the skill sustainment MCP between NMTF and CTC increases surgical readiness for military surgeons assigned to MTFs in the Pacific Northwest while limiting their direct exposure to litigious claims. This study has a few limitations. Principally, it reflects the case volume and experience of one surgeon over 11 months, which negatively influences the ability of our data to be generalized to the entire MHS but highlights the regional structure of military medical installations. Second, although a locally developed MCP, this study is limited by the unique nature of the Pacific Northwest military and civilian hospital systems. We acknowledge that, in trauma “deserts” around other MTFs, our model is not reproducible.
Supplementary Material
AUTHORSHIP
J.Y. and J.G. contributed in the literature search, study design, data collection, data analysis, data interpretation, writing, and critical revision. S.S., J.P., and M.S. contributed in the data collection, data analysis, data interpretation, writing, and critical revision. G.J., J.W., B.O., and G.P. contributed in the literature search, study design, writing, and critical revision.
DISCLOSURE
The authors declare no conflicts of interest.
The views expressed in this article reflect the results of research conducted by the author and do not necessarily reflect the official policy or position of the Department of the Navy, DOD, or the United States Government. This work was not funded by the government of the United States.
Footnotes
This study was presented at the 2022 annual meeting of the Military Health System Research Symposium, September 13, 2022, in Orlando, Florida.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Shaina Schaetzel, Email: Shaina.Schaetzel@providence.org.
Jessie Paull, Email: jessie.paull.87@gmail.com.
Guy Jensen, Email: gwj208@gmail.com.
James Wallace, Email: jw05umass@gmail.com.
Brendan O'Brien, Email: brendanobrien9@gmail.com.
Grace Pak, Email: gpak20@gmail.com.
Martin Schreiber, Email: schreibm@ohsu.edu.
Jacob Glaser, Email: jacob.glaser1@gmail.com.
REFERENCES
- 1.Dalton MK Remick KN Mathias M Trinh QD Cooper Z Elster EA, et al. Analysis of surgical volume in military medical treatment facilities and clinical combat readiness of US military surgeons. JAMA Surg. 2022 Jan 1;157(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee JJ, Hall AB, Carr MJ, MacDonald AG, Edson TD, Tadlock MD. Integrated military and civilian partnerships are necessary for effective trauma-related training and skills sustainment during the inter-war period. J Trauma Acute Care Surg. 2022;92(4):e57–e76. [DOI] [PubMed] [Google Scholar]
- 3.Jenkins DH Winchell RJ Coimbra R Rotondo MF Weireter LJ Bulger EM, et al. Position statement of the American College of Surgeons Committee on Trauma on the National Academies of Sciences, Engineering and Medicine Report, a National Trauma Care System: integrating military and civilian trauma systems to achieve zero preventable deaths after injury. J Trauma Acute Care Surg. 2016;81(5):819–823. [DOI] [PubMed] [Google Scholar]
- 4.Brandt M-M. Civilian-military partnerships. J Trauma Acute Care Surg. 2017;82(5):977–978. [DOI] [PubMed] [Google Scholar]
- 5.Jensen G, van Egmond T, Örtenwall P, Peralta R, Aboutanos MB, Galante J. Military civilian partnerships: international proposals for bridging the Walker Dip. J Trauma Acute Care Surg. 2020;89(2S Suppl 2):S4–S7. [DOI] [PubMed] [Google Scholar]
- 6.Carius BM, April MD, Schauer SG. Procedural volume within military treatment facilities-implications for a ready medical force. Mil Med. 2020;185(7–8):e977–e981. [DOI] [PubMed] [Google Scholar]
- 7.Haag A Cone EB Wun J Herzog P Lyon S Nabi J, et al. Trends in surgical volume in the military health system—a potential threat to mission readiness. Mil Med. 2021;186(7–8):646–650. [DOI] [PubMed] [Google Scholar]
- 8.Elster E. Clinical Readiness Program: Combat Casualty Care KSAs. Department of Surgery, Walter Reed National Military Medical Center. Available at: https://www.amsus.org/wp-content/uploads/2019/12/Elster-KSA-Overview-AMSUS-2019-RC.pdf. Accessed October 20, 2022. [Google Scholar]
- 9.American College of Surgeons . Military-civilian partnerships for trauma training, sustainment and readiness. Available at: http://www.facs.org/military. Accessed July 2, 2022.
- 10.Tadlock MD Carr M Diaz J Rhee P Cannon JW Eastridge BJ, et al. How to maintain the readiness of forward deployed caregivers. J Trauma Acute Care Surg. 2021;90(5):e87–e94. [DOI] [PubMed] [Google Scholar]
- 11.Savel RH, Cohen W, Borgia D, Simon RJ. The intensive care unit perspective of becoming a level I trauma center: challenges of strategy, leadership, and operations management. J Emerg Trauma Shock. 2018. Jan-Mar;11(1):65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall A Qureshi I Shackelford S Glaser J Bulger EM Scalea T Shackelford S, et al. Objective model to facilitate designation of military-civilian partnership hospitals for sustainment of military trauma readiness. Trauma Surg Acute Care Open. 2019;4:e000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruggero JM, Farnand AW, Roach PB, Starr F, Tadlock MD, Bokhari F. Initial assessment of a regional military-civilian partnership on trauma surgery skills sustainment. Mil Med. 2022:usac229. [DOI] [PubMed] [Google Scholar]
- 14.Dewar CD, Boulter JH, Curry BP, Bowers DM, Bell RS. The changing landscape of military medical malpractice: from the Feres Doctrine to present. Neurosurg Focus. 2020;49(5):E7. Retrieved July 13, 2022. Available at: https://thejns.org/focus/view/journals/neurosurg-focus/49/5/article-pE7.xml. Accessed July 12, 2022. [DOI] [PubMed] [Google Scholar]
- 15.28 U.S.C . §§ 1346(b)(1), 2401(b), 2671-80—Federal Tort Claims Act. Available at: https://tile.loc.gov/storageservices/service/ll/uscode/uscode1958-00602/uscode1958-006028171/uscode1958-006028171.pdf. Accessed July 15, 2021.
- 16.Mendez BH, Lewis KM. Military medical malpractice and the Feres doctrine. Congressional Research Service — In Focus. June 16, 2021. Retrieved December 20, 2022.
- 17. Feres v United States, 340 US 135 (1950)
- 18.Knowlton LM Butler WJ Dumas RP Bankhead BK Meizoso JP Bruns B, et al. Power of mentorship for civilian and military acute care surgeons: identifying and leveraging opportunities for longitudinal professional development. Trauma Surg Acute Care Open. 2023;8(1):e001049. [DOI] [PMC free article] [PubMed] [Google Scholar]


