The collaboration between UAB and various elements within the DoD illustrates a comprehensive approach to MCP. Replicating appropriate components of this model may aid in the development of a truly integrated trauma system best prepared for the challenges of the future.
KEY WORDS: Military-civilian partnership, military-civilian collaboration, trauma training, clinical proficiency, military research
BACKGROUND
At the University of Alabama at Birmingham (UAB), a multi-tiered military-civilian partnership (MCP) has evolved since 2006. We aimed to outline this model to facilitate potential replication nationally.
METHODS
We performed a comprehensive review of the partnership between UAB, the United States Air Force Special Operations Command, and the Department of Defense (DoD) reviewing key documents and conducting interviews with providers. As a purely descriptive study, this project did not involve any patient data acquisition or analysis and therefore was exempt from institutional review board approval per institutional policy.
RESULTS
At the time of this review, six core programs existed targeting training, clinical proficiency, and research. Training: (1) The Special Operations Center for Medical Integration and Development trains up to 144 combat medics yearly. (2) UAB trains one integrated military Surgery resident yearly with two additional civilian-sponsored military residents in Emergency Medicine. (3) UAB's Surgical Critical Care Fellowship had one National Guard member with two incoming Active-Duty, one Reservist and one prior service member in August 2022. Clinical Proficiency: (4) UAB hosts four permanently assigned United States Air Force Special Operations Command Special Operations Surgical Teams composed of general surgeons, anesthesiologists, certified registered nurse anesthetists, surgical technologists, emergency physicians, critical care registered nurses, and respiratory therapists totaling 24 permanently assigned active-duty health care professionals. (5) In addition, two fellowship-trained Air Force Trauma Critical Care Surgeons, one Active-Duty and one Reservist, are permanently assigned to UAB. These clinicians participate fully and independently in the routine care of patients alongside their civilian counterparts. Research: (6) UAB's Division of Trauma and Acute Care Surgery is currently conducting nine DoD-funded research projects totaling $6,482,790, and four research projects with military relevance funded by other agencies totaling $15,357,191.
CONCLUSION
The collaboration between UAB and various elements within the DoD illustrates a comprehensive approach to MCP. Replicating appropriate components of this model nationally may aid in the development of a truly integrated trauma system best prepared for the challenges of the future.
LEVEL OF EVIDENCE
Economic and Value-based Evaluations; Level IV.
Advancements gained from battlefield trauma care and their subsequent integration into civilian trauma systems and clinical best practices represent some of the few positive outcomes of war.1 Examples include the ambulance system from the Civil War, blood banks in World War I, aeromedical evacuation in Korea and Vietnam, as well as damage-control resuscitation strategies and use of tourniquets from Iraq and Afghanistan.2 The implementation of these advancements across both military and civilian trauma systems is facilitated by a healthy relationship between military and civilian trauma professionals with a shared objective of improving care outcomes.3 However, as with every conflict in the past, those advancements can peak, stagnate, and later decline in peacetime thus contributing to preventable morbidity and mortality at the start of a new conflict, occurrence of a natural disaster, or in the event of a mass casualty incident.3,4 As we transition to an era of significant reduction in major combat operations with a risk of peer and near-peer conflicts looming on the horizon, it is paramount that we learn from the past and remain proactive in our collaborative efforts to prepare for the future.5
In 2016, the National Academies of Science, Engineering, and Medicine published an extensive report outlining concrete steps to ensure the development of an ever-growing, integrated, national military-civilian trauma system.6 This system aims to sustain the military's medical readiness, bolster civilian trauma care advancements through continuous knowledge exchange, and better prepare the nation for disaster and mass casualty incidents. In that spirit, efforts to strengthen existing military-civilian partnerships (MCPs) have been underway and several additional partnerships have been forged between the various military services and our nation's academic medical institutions.7
Some of the existing partnerships are focused on Graduate Medical Education while others target predeployment training of surgical teams, clinical currency sustainment, and or mission specific readiness training.8 In 2018, the Military Health System Strategic Partnership American College of Surgeons (MHSSPACS) published a report outlining several notable MCP models geared toward trauma training platforms, sustainment collaboratives, and research.9
Nonetheless, concerns regarding trauma proficiency have been amplified as the acuity and volume in military hospitals has decreased with the consolidation of hospitals under the Defense Health Agency (DHA).10 A 2019 study published in JAMA Surgery found that only 10.1% of military surgeons met clinical standards of combat readiness using the military's Knowledge, Skills, and Abilities (KSA) metric.11 In response to this concerning statistic, the military has reemphasized initiatives to address these deficits through additional support and expansion of MCP.12 In 2020, Lee et al.13 conducted a review of all published literature related to MCP from January 1980 to October 2020. Military-civilian partnerships were then classified into one of five focus areas: Skill Sustainment, Just-In Time Training, Strategic, Integrated, and Mentorship.
At the University of Alabama at Birmingham (UAB), an American College of Surgeons (ACS) Level I Trauma Center, a multi-tiered MCP has existed and evolved since 2006. The aim of this project was to examine and outline the components of this model, which include programs addressing all five above mentioned focus areas, in order to facilitate possible replication of appropriate components to the potential benefit of both military and civilian trauma care in the United States.
MATERIALS AND METHODS
Setting
UAB Hospital is a 1200 bed regional tertiary care center and ACS Level I trauma center with over 6,500 trauma activations, 4579 trauma admissions, 411 burn evaluations, and 369 burn admissions per year. Of all trauma activations presenting to UAB, 20% are penetrating, 30% have an Injury Severity Score greater than 15, and 12% have an Injury Severity Score greater than 25. The UAB Division of Trauma and Acute Care Surgery independently manages a 28-bed trauma-burn intensive care unit, 8 to 10 dedicated beds for head trauma in the Neurointensive care unit, 48 stepdown and floor beds, and 10 trauma recover unit beds. In the year 2021, the division alone performed 311 laparotomies. As a purely descriptive study, this project did not involve any patient data acquisition or analysis and therefore was exempt from institutional review board approval per institutional policy. In accordance with the Enhancing the QUAlity and Transparency of Health Research guidelines, the Standards for Reporting Qualitative Research checklist was used to conduct the study (Supplemental Digital Content, http://links.lww.com/TA/D41).
Document Review
We conducted a comprehensive review of all elements within the partnership between UAB, the United States Air Force Special Operations Command (AFSOC), and the Department of Defense (DoD). We reviewed key documents including: the Memorandum of Understanding between UAB and the military; Special Operation Center for Medical Integration and Development (SOCMID) curriculum and training data; AFSOC manning, training, clinical duties, deployment cycles, 2021 clinical case volumes across each specialty over 6 months, and 2021 work relative value units (wRVU) generated by nondeployed Special Operations Surgical Team (SOST) surgeons over 6 months; roster of all current military and military-affiliated faculty and house staff that rotate within the Division of Trauma and Acute Care Surgery; as well as a listing of all current and past grant funding for military-relevant research projects within the division.
Interviews
Furthermore, guided by the data obtained from the abovementioned documents, we conducted interviews with providers in order to further outline key components, themes, and potential opportunities for improvement within each aspect of the partnership guided by the standards set forth by the MHSSPACS as described within the Blue Book: Military-Civilian Partnerships for Trauma Training, Sustainment, and Readiness.14
RESULTS
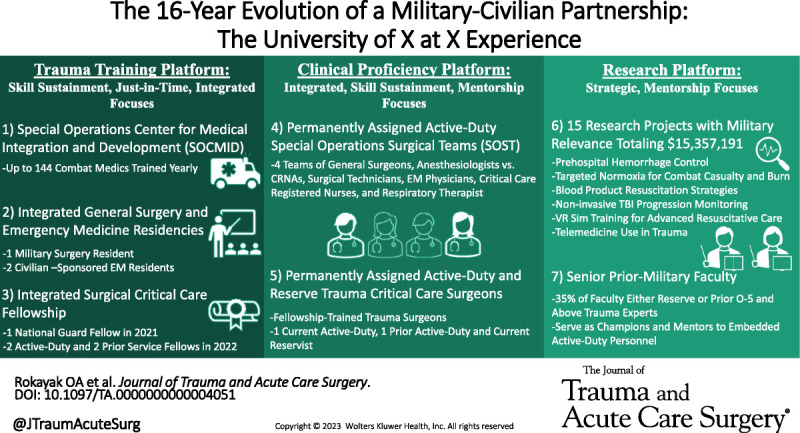
Six core partnership programs are currently in place within trauma training, clinical proficiency, and research platforms (Fig. 1) covering the previously described Just-in-Time training, Skill Sustainment, Integrated, Mentorship, and Strategic focus areas of MCP.
Figure 1.
Components of the MCP at UAB. *Air Force Special Operations Command. †Department of Defense.
Trauma Training Platform: Skill Sustainment, Just-in-Time, and Integrated Focuses
-
(1) Core Partnership Program 1: SOCMID. Special Operations Center for Medical Integration and Development, a collaboration between UAB and AFSOC, is a program for Special Operations Forces (SOF) combat medics that provides intensive trauma training using a formalized curriculum consisting of didactic, tabletop, simulation, and real-world trauma rotations for up to 144 pararescue jumpers (PJs) and SOF medics each year. Students are required to rotate through the program at least once every other year but are able to attend the two-week course as needed on a yearly basis. Week one of the course consists of didactic, tabletop, and virtual reality simulation training. Topics covered include Basic Life Support, Advanced Cardiac Life Support, Pediatric Advanced Life Support, toxicology, blood administration, prolonged casualty care, Tactical Combat Casualty Care (TCCC), and basic ventilator management. The week then culminates with a procedural skills live-tissue and or cadaver laboratory taught by both military and civilian surgeon faculty. The second week of the course focuses on real-world clinical rotations. Students work a series of 12-hour shifts; two in the trauma bay, two in the 28-bed trauma-burn intensive care unit, and one shift in the general emergency department. This on average results in a minimum of 64 patient encounters at UAB per student per course.
Finally, the course concludes with a culmination exercise in a mock deployed environment held at the local Army National Guard base. The exercise allows students to apply their training in a simulated austere setting through a full-mission profile incorporating various elements, including a participating SOST, mass casualty scenarios, and live-tissue models.
(2) Core Partnership Program 2: Integrated Residency Programs. Of the eight general surgery residency positions, UAB Surgery has allocated one as a DHA military-civilian position to train a fully integrated military resident each year starting in 2021. The dedicated military position has had a 50% fill rate since inception of this initiative with one Army resident matching into the program in 2021 and none matched in 2022 due to an insufficient level of competitiveness of military applicants as assessed by UAB that year. To address this in the future, the residency program administration has since implemented more robust and deliberate recruitment efforts with the aid of prior and active military personnel through added marketing via social media, electronic messaging, and biannual webinars to inform military medical students of the opportunities at UAB. Additionally, at the time of this review, UAB was training two deliberately recruited and integrated civilian-sponsored military residents in Emergency Medicine.
(3) Core Partnership Program 3: Integrated Surgical Critical Care Fellowship. At the time of this review, of its four available positions, UAB’s Surgical Critical Care Fellowship Program had one National Guard member in the class of 2021 to 2022 with two integrated Active-Duty, one Reservist, and one prior service member in the incoming class of 2022 to 2023. The program originally accepted two fellows per year but was expanded to four starting with the class of 2019 to 2020 and has maintained a 100% fill rate since inception. Although this expansion was not done specifically at that time for the purposes of enrolling military members, the recruitment and matching of service members into the fellowship program became deliberate starting in 2021. National Guard, Reservist, and Active-Duty fellows go through the same application, interview, and selection process as their civilian counterparts. The fellowship consists of nine months of core surgical critical care rotations and three months of electives all while remaining fully incorporated into the trauma call schedule with each fellow averaging six calls per month and over 200 major cases per year since 2019.
Clinical Proficiency Platform: Integrated, Skill Sustainment, and Mentorship Focuses
(4) Core Partnership Program 4: Permanently assigned AFSOC SOSTs. Since 2019, UAB has hosted four SOSTs, increased over the preceding nine years from one team in 2010, two teams in 2014, and three teams in 2018. Each SOST is composed of a General Surgeon, an Anesthesiologist or Certified Registered Nurse Anesthetist, a Surgical Technologist, an Emergency Medicine Physician, a Critical Care Registered Nurse, and a Respiratory Therapist totaling 24 embedded Active-Duty AFSOC physicians and health care professionals. Members are permanently assigned to UAB for at least three years and undergo a four-phase cycle developed by AFSOC consisting of predeployment, alert, deployment, and post-deployment such that one to two teams are always on clinical duty. When not deployed or away on military duty, SOST personnel integrate with their civilian counterparts as fully credentialed volunteer faculty and staff with SOST physicians serving at the ranks of clinical assistant professors or clinical instructors. As such, and in accordance with UAB requirements, SOST physicians cover 1–1.3 full-time equivalents (FTE) per specialty group, while nonphysicians work on a shift-based model to accomplish their Air Force-mandated Comprehensive Medical Readiness Plan (CMRP) requirements for their given Air Force Specialty Code. In the first six months of 2021, two nondeployed SOST surgeons performed a total of 615 procedures (300 required yearly per surgeon), 109 major surgeries (50 required yearly per surgeon), 36 index trauma operations (25 required yearly per surgeon), and 288 critical care encounters (50 required yearly per surgeon) generating 5766 wRVUs. Major cases included damage control and definitive abdominal surgery for trauma (splenectomy, hepatorrhaphy, diaphragmatic, gastric, small bowel, colonic, and bladder repair or resection), thoracic surgery for trauma (thoracotomy and video assisted thoracoscopic surgery), damage-control vascular surgery for trauma (caval, iliac, and femoral injuries), head and neck surgery (tracheostomy, and neck exploration) burn surgery (escharotomy, fasciotomy, excision, and grafting), emergency general surgery for necrotizing fasciitis, and various abdominal emergencies (gastric, small bowel, colon, biliary). During that same period, nonsurgeon SOST personnel numbers were notable for an average of 186 cases per anesthesiologist (six-month requirement, 72), 51 shifts per emergency physician (six-month requirement, 48), 51 shifts per critical care registered nurses (six-month requirement, 48), 50 shifts per respiratory therapist (six-month requirement, 48), and 80 cases per surgical technologist (six-month requirement, 72). When not on service, requirements of SOST members include attendance of quality improvement, morbidity and mortality, grand rounds, and self-led unit quarterly case conferences. In addition to medical student, resident, and fellow education, teaching responsibilities include Advanced Trauma Life Support (ATLS), Advanced Surgical Skills for Exposure in Trauma (ASSET), Basic Endovascular Skills for Trauma (BEST), SOCMID, TCCC, and STOP THE BLEED instruction. Nonclinical duties include regular unit, joint service, and multinational exercises; annual tactical training including full-mission profile austere battlefield surgical training; predeployment training involving care delivery on air-, sea-, and land-based platforms; as well as alert response and enduring mission deployments. Finally, SOST members provide a minimum of two independent trauma calls per surgeon, while nonsurgeons cover one to two calls each month with their team surgeon. These highly valuable team calls serve as regularly scheduled mock deployment scenarios with all members collocated in the SOST office when not actively delivering care. The office is outfitted with hospital and Air Force computers, call rooms, and a gym. When in the office, the team reviews cases, clinical practice guidelines (CPG), labs, and imaging as a group. Teams respond to all trauma activations as a group and conduct any necessary interventions and patient care under the direct supervision of the SOST surgeon on call. In the first six months of 2021, the primary team on clinical duty independently covered twelve 16-hour team trauma calls and averaged 18 trauma activations, five critical care encounters, four emergent airways, five chest tubes, five fracture reductions with splinting, four wound washouts, four laceration repairs, four burn debridements, two burn resuscitations, two conscious sedations, and two operative traumas per call.
(5) Core Partnership Program 5: Permanently assigned Air Force Trauma Critical Care Surgeons. Two fellowship-trained Air Force Trauma Critical Care Surgeons, one current Active-Duty and one prior Active-Duty and current Reservist, are permanently assigned to UAB since fall of 2021 and spring of 2018, respectively. The Active-Duty surgeon covers 0.8 to 1 of an FTE while not deployed depending on mission requirements while the Reservist covers a full FTE and serves in a full-time leadership role as the Trauma Medical Director for UAB. Both professionals share an equal workload to their civilian partners covering an average of three clinical service weeks and five calls per month per surgeon. In the first six months of 2021, the reservist performed 65 major operations, including 31 laparotomies, 10 extremity debridements, nine tracheostomies, six percutaneous gastrostomies, three amputations, three laparoscopies, two burn excisions with grafting, and one fasciotomy.
Research Platform: Strategic, and Mentorship Focuses
(6) Core Partnership Program 6: Research and Mentorship. In the UAB Division of Trauma and Acute Care Surgery Center for Injury Sciences (CIS), there are currently nine DoD-funded research projects underway totaling $6,482,790, and a further four research projects with military relevance funded by other agencies totaling $15,357,191 (Table 1).Topic areas of current projects at the time of this review include the study of prehospital hemorrhage control devices and adjuncts, such as XSTAT (RevMedX, Wilsonville, OR) and Four-Factor Prothrombin Complex Concentrate, targeted normoxia for combat casualty and burn care, blood product resuscitation strategies, noninvasive traumatic brain injury progression monitoring, and virtual reality simulation training for advanced resuscitative care (Table 1). Previously completed research included three projects with a combined total funding award of $10,685,447 covering the study of prehospital tranexamic acid for traumatic brain injury, portable x-ray device development for austere environments, and the first in-human studies to assess safety and physiologic effects of synthetic Ethinyl Estradiol-3-Sulfate. These projects have grown in number and award amount since the inception of this MCP. Furthermore, 35% (5 of 14) of the current faculty within the Division of Trauma and Acute Care Surgery are prior military or on reserve status, including the Division Director, the Trauma Medical Director, and the Director of the CIS. These clinical and research leaders harness their knowledge and experience to not only deliver high quality trauma care but also actively mentor all permanently assigned military personnel as well as their civilian colleagues.
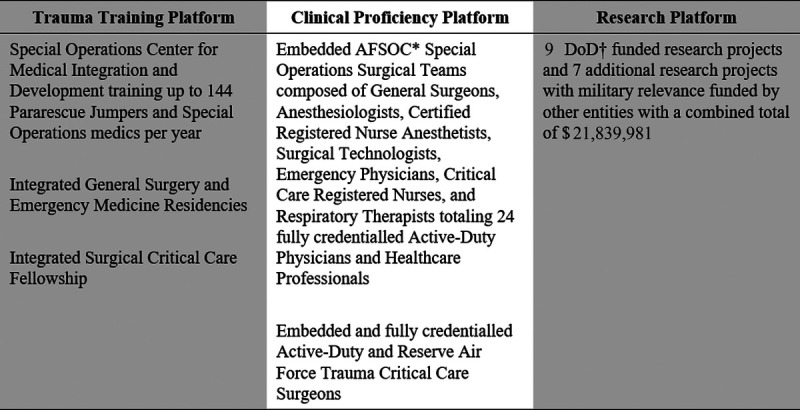
TABLE 1.
Current Military-Relevant Research Projects in UAB's Division of Trauma and Acute Care Surgery
| Project | Funding Agency | Award |
|---|---|---|
| A pilot randomized clinical trial of the XSTAT hemostatic device in the prehospital setting (PhoXSTAT) | DoD* | $750,789 |
| Noninvasive Monitoring of Traumatic Brain Injury Progression Using the Infrascanner (MOBI-0) | Industry | $100,000 |
| Multicenter Implementation Trial of Targeted Normoxia Strategy to Define Oxygen Requirements for Burn Care (Save O2–Burn) | DoD* | $199,397 |
| Multicenter Implementation Trial of Targeted Normoxia Strategy to Define Oxygen Requirements for Combat Casualty Care (Save O2–Trauma) | DoD* | $199,397 |
| Plasma Resuscitation without Lung Injury (PROPOLIS) | DoD* | $203,739 |
| Trauma and 4-Factor Prothrombin Complex Concentrate (TAP) | Industry | $6,652,001 |
| Noninvasive Monitoring of Traumatic Brain Injury Progression Using the Infrascanner (MOBI-1) | DoD* | $2,224,321 |
| Spectral MD | DoD* | $450,000 |
| Type O Whole blood and the assessment of Age early Resuscitation Trial | DoD* | $1,439,700 |
| Prehospital Analgesia Intervention trial (PAIN) | DoD* | $600,000 |
| Reducing Exsanguination Via In-Vivo Expandable Foam (REVIVE) | DoD* | $415,447 |
| Embolization of the Splenic Artery After Trauma (ELSA-2) | Industry | $347,747 |
| Trauma Resuscitation with Group O While Blood or Products (TROOP) | NIH** | $8,257,443 |
| DoD total | $6,482,790 | |
| NIH/industry total | $15,357,191 | |
| Overall total | $21,839,981 |
*Department of Defense.
**National Institute of Health.
DISCUSSION
Trauma and medical readiness are critical components of the military health care system. UAB Hospital is a high-volume urban tertiary care center and ACS-verified Level I trauma center that cares for more than 6500 trauma patients per year. Since 2006, AFSOC and the DoD have recognized the value of training at such a center and strategically embarked on what continues to evolve as a unique and comprehensive MCP with positive impacts on individual, team, and institutional growth (Table 2).
TABLE 2.
UAB MCP Model Programs and Associated Impact Areas
| UAB MCP Programs | Individual Impact | Team Impact | Institutional Impact |
|---|---|---|---|
| SOCMID* | • | • | • |
| Integrated residencies | • | • | |
| SCC** fellowship | • | • | |
| Embedded SOST† | • | • | • |
| Embedded TCC‡ surgeons | • | • | |
| Military research | • | • | • |
*Special operations center for medical integration and development.
**Surgical critical care.
†Special operations surgical teams.
‡Trauma critical care.
Skill Sustainment, Just-in-Time Training, and Integration Impact
Through SOCMID, and upon completing their initial didactic and simulation training, PJs and SOF medics are allowed to work within their extended military scope of practice under direct supervision thereby improving their clinical readiness in a safe yet realistic setting. Real world procedures performed by these students while at UAB include obtaining intravenous access, intraosseous access, intubation and other emergency airways, needle decompression, chest tube placement, laceration repairs, fracture reduction and splinting, burn debridement, Focused Assessment Sonography for Trauma (FAST), and exposure to a variety of cases in the operating room. The projected throughput at full capacity for SOCMID is now targeting the expansion to 12 to 16 students per class and two classes per month thus allowing for the 350 to 400 slots per year needed to meet Total Force PJ and SOF medic biannual requirements.
Furthermore, the fully integrated military residents and fellows at UAB function in the same capacity and share the same workload as their civilian counterparts thus benefiting from a high volume, high acuity, and high complexity (20% penetrating trauma) of cases on a day-to-day basis.
Toward this end, graduating chief residents from the class of 2021 to 2022 averaged 1,001 major cases over the course of their five years at UAB while graduating surgical critical care fellows averaged more than 200 cases per year since 2019.
Integrated Clinical Proficiency, Skill Sustainment, and Mentorship Impact
Following a two-phase standardized AFSOC Assessment and Selection process, all embedded Active-Duty austere battlefield surgery specialists undergo a 10-month training pipeline targeting SOF-specific skills and austere battlefield surgery training. Upon completion, personnel enter into a systemized onboarding process organized by SOST leadership and approved by the leadership of the appropriate respective civilian departments prior to being appointed as fully credentialled faculty and staff at UAB. As such, they function independently within their professional capacity when not deployed in support of SOF missions, provide one to two monthly independent team trauma call coverages per team for UAB, and actively partake in the critical knowledge and skills exchange with colleagues, fellows, residents, students, and staff that makes this partnership beneficial to the advancement of all parties involved. This is accomplished in real-time on rounds and in the operating room in addition to regular participation in all Quality Improvement, Morbidity and Mortality, Grand Rounds, Journal Club, and resident teaching conferences. In addition, all military surgeons are active ATLS, BEST, ASSET, SOCMID, and TCCC instructors. In the first six months of 2021, SOST clinical number averages surpassed CMRP requirements for all Air Force Specialty Codes.
Finally, DoD physician performance is evaluated and reviewed in the same manner as their civilian counterparts through weekly quality improvement and morbidity and mortality conferences, monthly faculty meetings, and annual performance reviews.
Any necessary clinically related counseling/remediation procedures are implemented as per institutional guidelines. That said, no DoD provider has faced disciplinary actions or suspensions to date since the inception of the MCP.
Research, Mentorship, and Strategic Impact
The sustained support and active involvement of civilian and prior military faculty in all aspects of the partnership has been critical to the success of the UAB model. Currently, 35% of the UAB civilian trauma faculty have prior military service, including the Division Director of Trauma and Acute Care Surgery, the Director of the CIS, and the Trauma Medical Director. As such, the unique mentorship opportunities available to current military personnel from experienced, national, and world-renowned trauma clinical and research experts is an ever-present part of the experience at UAB.
This healthy academic partnership combines the decades-long experience of its military and civilian faculty, facilitates a valuable exchange of ideas, and fosters numerous process improvement initiatives, clinical trials, and medical modernization projects focused on improving trauma care both at home and abroad. Examples of such are demonstrated throughout the many military-relevant research projects at UAB as referenced within the results section and Table 1.
The significant increase in both number of military-relevant projects, as well as associated dollar amounts within UAB's Division of Trauma and Acute Care Surgery and the subsequent positive impact on both civilian and military trauma care through their rapid implementation into CPGs, civilian practice, and SOST medical modernization efforts are clear demonstrations of the continuous growth and optimization taking place within this MCP.
Lessons Learned
It is important to emphasize that the various partnership programs within the MCP described in this report are the result of a 16-year process of development, growth, and evolution. As described above and as displayed in Figure 2, component partnership programs were expanded in a stepwise fashion. Throughout this process, many lessons were learned and many adjustments were made. We describe some of those lessons below.
Figure 2.
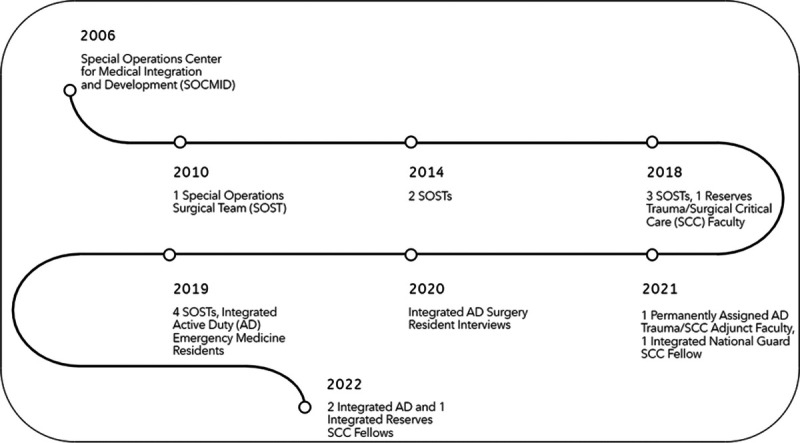
Timeline of Core MCP program development and expansion.
Prior to establishing a single program, it was essential to ensure the long-term commitment of the institution across all levels of leadership within the various departments involved, as well as that of the DoD stakeholders through a series of goal defining leadership meetings. Next came the allocation of funding, resources, space, and personnel to aid in establishing and sustaining each program. Finally, once established, maintaining open channels of communication between leadership of both the host institution and DoD stakeholders through regular meetings, quarterly site visits, and process improvement initiatives remained key in the sustainment efforts of each partnership program.
A key takeaway from these efforts was the importance of ensuring a constant presence of military personnel at the host institution at all times so as not to allow any inadvertent denaturing of the military-civilian relationship. Such denaturing was naturally experienced in the early phases of partnerships when the small number of military personnel assigned to the host institution were absent for prolonged periods due to mission requirements and deployments. This led to the expansion of the quota of medics trained through SOCMID, the number of embedded SOSTs, the deliberate dedication to seek out military-relevant research projects by civilian faculty, and the hiring of additional prior military faculty and staff to help drive and support such expansion efforts further.
Another key to the success of the MCP programs at UAB is the mixed salary-based and production-based billing model that the institution follows. Under this model, Active-Duty personnel are encouraged to take on more clinical duties without an unintended negative impact on their civilian partner’s productivity or income. Furthermore, all services provided by Active-Duty personnel are billed through the standard UAB billing system. Malpractice coverage for military personnel is provided by the UAB Professional Liability and Trust Fund and the hospital does not bill professional fees for TriCare patients managed by Active-Duty personnel. Finally, military personnel are always scheduled as an overage with backup coverage of clinical duties by civilian faculty and staff available as mission and military duty requirements dictate. A more detailed breakdown of financial allocations including cost vs. benefit analysis will be included in a future report.
Blue Book Synergy/Future Studies
Although many of the MCP components at UAB predate the MHSSPACS recommendations as described in the Blue Book: Military-Civilian Partnerships for Trauma Training, Sustainment, and Readiness, the UAB model demonstrates near complete synergy with said guidance.14 Congruency is demonstrated with all elements listed in Part II of the Blue Book outlining the standards of ideal Institutional Commitment, Governance and Administration, Human Resources, Physical Resources, and Educational components. Opportunities for improvement on furthering this synergy can be addressed within the Evaluation Tools component of the standards by implementing a formal and objective mechanism for conducting key stakeholder and quantitative assessments to determine if predefined goals and objectives of the partnership are consistently met at regular intervals outside of yearly case volumes and wRVUs.
We recommend adopting and assessing KSA metrics for all military providers, implementing an annual 360-degree evaluation of all providers and military personnel, and conducting interval assessments of the impact of the MCP on civilian faculty, staff, residents, fellows, and non–Graduate Medical Education programs at UAB. This would inform further growth, optimization, and process improvement.
Limitations/Recommendations
The findings of this review must be interpreted within the context of its limitations. The review was conducted during the months of January 2022 through July of 2022. Data reflecting the number of integrated military residents, embedded military personnel, and dollar amounts for DoD-funded and military-relevant research are consistent with those dates and obviously will change over time. Clinical data was captured from the first six months of 2021 and thus did not include data for the Active-Duty Trauma Critical Care Surgeon. No KSA values were available at the time of this review as the embedded personnel measure productivity under an Air Force-mandated CMRP requirements program. The Special Operations Surgical Teams are currently in the process of transitioning to the KSA system. Given the importance of such data analysis as related to MCP optimization, we recommend a future project focused on comparing calculated KSA values obtained from the UAB group vs. averages from published data across both Military Treatment Facilities and other MCPs.
CONCLUSION
The partnerships between UAB and various elements within the DoD represent a 16-year evolution of a MCP model, documenting the institutional commitment of both UAB and the DoD. The details of this model illustrate a mature, comprehensive, and effective approach to an integrated MCP. It is multipronged and addresses both military and civilian trauma training, clinical proficiency, and research needs. Furthermore, it is a model that incorporates all five focus areas of MCP as defined in the review of 40 years of MCP literature conducted by Lee et al.;13 Skill Sustainment, Just-In Time Training, Integrated, Strategic, and Mentorship.
We believe that potential replication of appropriate components of this MCP model throughout the nation's trauma centers may aid in the development of a truly integrated national trauma system that is best prepared for the challenges of the future, both at home and abroad.
Supplementary Material
AUTHORSHIP
Study conception and design was conducted by J.B.H., O.A.R., and J.D.K. Acquisition of data was conducted by O.A.R., J.B.H., J.O.J., D.B.C., R.D.B., D.T.L., E.W.B., J.P.W., N.R.M., D.M.N., J.K.W., J.D., and J.D.K. Interpretation of data was performed by O.A.R., E.W.B., J.B.H., J.O.J., D.B.C., R.D.B., D.T.L., J.P.W., N.R.M., D.M.N., J.K.W., J.D., and J.D.K. Drafting of the article was led by O.A.R., E.W.B., J.B.H., J.O.J., D.T.L., N.R.M., and J.D.K. Critical revisions and edits were completed by O.A.R., J.B.H., J.O.J., D.B.C., J.P.W., D.T.L., R.D.B., N.R.M., D.M.N., J.K.W., J.D., and J.D.K. All authors read and approved the final article.
ACKNOWLEDGMENTS
We wish to acknowledge the leadership, faculty, and staff of The University of UAB Hospital, the UAB Division of Trauma and Acute Care Surgery, Detachment 1 United States Air Force Special Operations Surgical Teams, D130 Special Operations Surgical Team, the Special Operations Center for Medical Integration and Development, the UAB Surgical Critical Care Fellowship Program, the UAB General Surgery Residency Program, the UAB Emergency Medicine Residency Program, the UAB Center for Injury Science, and the UAB departments of Surgery, Anesthesia, Surgical Technology, Emergency Medicine, Nursing, and Respiratory Therapy without who’s years of dedication, hard work, and service, this project would not have been possible.
DISCLOSURE
The authors declare no funding or conflicts of interest.
The views expressed in this article are those of the authors and do not represent the views of the University of Alabama at Birmingham, the United States Air Force Special Operations Command, the Defense Health Agency, the United States Air Force, the United States Army, the United States Navy, or the Department of Defense.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Daniel T. Lammers, Email: dtlammer@gmail.com.
Emily W. Baird, Email: ewbaird@uabmc.edu.
John B. Holcomb, Email: jbholcomb@uabmc.edu.
Jan O. Jansen, Email: jjansen@uabmc.edu.
Daniel B. Cox, Email: danielcox@uabmc.edu.
Jon P. Winkler, Email: jwinkler@uabmc.edu.
Richard D. Betzold, Email: richard.betzold@gmail.com.
Nathan R. Manley, Email: nathanrmanley@gmail.com.
David Marc Northern, Email: dmarcnorthern@aol.com.
James K. Wright, Email: wright4james@gmail.com.
John Dorsch, Email: john.dorsch@hotmail.com.
Jeffrey D. Kerby, Email: jkerby@uabmc.edu.
REFERENCES
- 1.Feliciano DV. Contributions of military surgeons to the management of vascular trauma. J Trauma Acute Care Surg. 2017;83(5):777–783. [DOI] [PubMed] [Google Scholar]
- 2.Carmichael SP, Mowery NT, Martin RS, Meredith JW. Management of Acute Trauma. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. Elsevier Health Sciences; 2021;387–388. [Google Scholar]
- 3.Schwab WC. Winds of war: enhancing civilian and military partnerships to assure readiness: white paper. J Am Coll Surg. 2015;221(2):235–254. [DOI] [PubMed] [Google Scholar]
- 4.Cannon JW, Gross KR, Rasmussen TE. Combating the peacetime effect in military medicine. 2021;156(1):5–6. [DOI] [PubMed] [Google Scholar]
- 5.Knudson MM. A perfect storm: 2019 scudder oration on trauma. J Am Coll Surg. 2020;230(3):269–282. [DOI] [PubMed] [Google Scholar]
- 6.National Academies of Sciences, Engineering, and Medicine . A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. National Academies Press. 2016. [PubMed] [Google Scholar]
- 7.Eckert MJ Bonifacio AJ Hardin RJ Jr. Brown SR King BT Soliz BA, et al. The University of North Carolina at Chapel Hill and US Army military-civilian medical partnership: a holistic approach to military medical readiness. J Am Coll Surg. 2021;233(5):e126–e127. [Google Scholar]
- 8.Lee J, Hall AB, MacDonald A, Edson TD, Tadlock MD. Military-civilian partnerships for trauma related training and skills sustainment: collective review. J Am Coll Surg. 2021;233(5):S160. [DOI] [PubMed] [Google Scholar]
- 9.Knudson MM, Elster EA, Bailey JA, Woodson J. Military health system strategic partnership with the American College of Surgeons. J Am Coll Surg. 2018;227(2):296–297. [DOI] [PubMed] [Google Scholar]
- 10.Maucione S. DHA set to take over all military hospitals by end of 2021, even after transition halt during pandemic. Federal News Network. 2021. Available at: https://federalnewsnetwork.com/defense-main/2021/02/dha-set-to-takeover-all-military-hospitals-by-end-of-2021-even-after-transition-halt-during-pandemic. Accessed February 12, 2022. [Google Scholar]
- 11.Dalton MK Remick KN Mathias M Trinh QD Cooper Z Elster EA, et al. Analysis of surgical volume in military medical treatment facilities and clinical combat readiness of US military surgeons. JAMA Surg. 2022;157(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tadlock MD Carr M Diaz J Rhee P Cannon JW Eastridge BJ, et al. How to maintain the readiness of forward deployed caregivers. J Trauma Acute Care Sur. 2021;90(5):e87–e94. [DOI] [PubMed] [Google Scholar]
- 13.Lee JJ, Hall AB, Carr MJ, MacDonald AG, Edson TD, Tadlock MD. Integrated military and civilian partnerships are necessary for effective trauma-related training and skills sustainment during the inter-war period. J Trauma Acute Care Surg. 2022;92(4):e57–e76. [DOI] [PubMed] [Google Scholar]
- 14.The MHSSPACS . Blue Book. Available at: https://facs.org/member-services/mhsspacs/blue-book. Accessed March 1, 2022.


