Background:
Thyroid disease is a common endocrine disorder, and thyroid surgeries and postoperative complications have increased recently. This study aimed to explore the effectiveness of intraoperative nerve monitoring (IONM) in endoscopic thyroid surgery using subgroup analysis and determine confounding factors.
Materials and Methods:
Two researchers individually searched for relevant studies published till November 2022 in the PubMed, Embase, Web of Science and Cochrane Library databases. Eventually, eight studies met the inclusion criteria. Heterogeneity was assessed using the Cochran’s Q test, and a funnel plot was implemented to evaluate publication bias. The odds ratio or risk difference were calculated using fixed-effects models. The weighted mean difference of continuous variables was calculated. Subgroup analysis was performed according to the disease type.
Results:
Eight eligible papers included 915 patients and 1242 exposed nerves. The frequencies of transient, permanent and total recurrent laryngeal nerve (RLN) palsy were 2.64, 0.19 and 2.83%, respectively, in the IONM group and 6.15, 0.75 and 6.90%, respectively, in the conventional exposure group. In addition, analysis of the secondary outcome indicators for the average total length of surgery, localisation time of the RLN, recognition rate of the superior laryngeal nerve and length of incision revealed that IONM reduced the localisation time of the RLN and increased the identification rate of the superior laryngeal nerve. Subgroup analysis showed that IONM significantly reduced the incidence of RLN palsy in patients with malignancies.
Conclusions:
The use of IONM significantly reduced the incidence of transient RLN palsy during endoscopic thyroid surgery, but it did not significantly reduce the incidence of permanent RLN palsy. However, the reduction in the total RLN palsy was statistically significant. In addition, IONM can effectively reduce the location time of the RLN and increase the recognition rate of the superior laryngeal nerve. Therefore, the application of IONM for malignant tumours is recommended.
Keywords: endoscopic thyroid surgery, intraoperative nerve monitoring, meta-analysis, permanent recurrent laryngeal nerve palsy, total recurrent laryngeal nerve palsy, transient recurrent laryngeal nerve palsy
Introduction
Highlights
The number of thyroid surgeries has risen sharply, with an increasing incidence each year.
Injury to the recurrent laryngeal nerve (RLN) is a serious complication of thyroid surgery.
Intraoperative nerve monitoring (IONM) reduced the location time of the RLN.
Intraoperative nerve monitoring reduced the recognition rate of the superior laryngeal nerve and the incidence of transient RLN palsy.
However, the incidence of persistent RLN palsy did not decrease.
Thyroid disease is a common endocrine disorder. In the past decades, the number of thyroid surgeries has risen sharply, with an increasing incidence each year1. Meanwhile, postoperative complications, such as recurrent laryngeal nerve (RLN) palsy, postoperative infections and hypoparathyroidism, have become increasingly prominent2,3. Meanwhile, the degree of RLN injury is currently one of the most significant indicators for evaluating the quality of thyroid surgery4,5.
With the development of endoscopy and minimally invasive surgeries and the patients’ demand for postoperative aesthetics, endoscopic thyroid surgery is performed with only a small, concealed incision and can simultaneously ensure the therapeutic effect of the surgery and reduce postoperative pain6. At the same time, endoscopic thyroid surgery has already developed a variety of surgical approaches7, which can be flexibly adjusted and changed according to the patient’s condition and are widely used in current thyroid surgery. Therefore, reducing the incidence of RLN injury as much as possible is a question that clinicians need to consider nowadays.
In 1996, Eisele et al. reported intraoperative tracheal intubation combined with an electromyogram. This method has led to the rapid development of intraoperative neuromonitoring (IONM), which is widely used as an important auxiliary method in thyroid surgery8. The basic principle of IONM is that the stimulation electrode directly stimulates the RLN or vagus nerve, which enters the larynx via the RLN and innervates the vocal fold muscle to generate electromyographic signals. Simultaneously, the recording electrode receives the electrical signal and generates the electromyogram. During thyroid surgery, IONM not only enables quick localisation and identification of the RLN, but also makes it easier to locate and heal the injury site9. In the past, IONM has been reported to reduce the incidence of RLN palsy and is particularly important for the prevention of bilateral vocal cord palsy10. However, the effectiveness of IONM in endoscopic thyroid surgery remains unclear. This article incorporates relevant articles from a literature review and meta-analysis to evaluate the effectiveness of IONM for monitoring in endoscopic thyroid surgery to provide theoretical support for the clinical application of IONM in thyroid disease.
Materials and methods
This work was reported in line with the PRISMA, Supplemental Digital Content 1, http://links.lww.com/JS9/A699, Supplemental Digital Content 2, http://links.lww.com/JS9/A700 (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 202011 and AMSTAR, Supplemental Digital Content 3, http://links.lww.com/JS9/A701 (Assessing the methodological quality of systematic reviews) 2 Guidelines12. IRB approval was not needed as this is a meta-analysis of published data. This systematic review was registered on PROSPERO with the registration number: CRD42022362727.
Search strategy
Two researchers independently searched PubMed, Embase, the Cochrane Library and the Web of Science for articles published before November 2022 on the application of IONM in endoscopic thyroidectomy. The search strategy is shown in Supplementary Table 1, Supplemental Digital Content 4, http://links.lww.com/JS9/A702.
Inclusion and exclusion criteria
Inclusion criteria
The analysis included studies in which patients had undergone endoscopic thyroid surgery, patients in the experimental group underwent intraoperative neural monitoring, and complete data of patients with postoperative RLN palsy were explicitly included.
Exclusion criteria
The meta-analysis excluded case reports, review articles, descriptive articles, animal trials, uncontrolled studies, incomplete data on RLN palsy, conventional open thyroid surgery, failure of endoscopic thyroid surgery and conversion to conventional open surgery, endoscopic simple thyroid isthmus surgery and percutaneous thyroid ablative techniques.
Data extraction and quality assessment
Data extraction
Two investigators performed data extraction independently. All the following data were retrieved for each study: Subsequently, the following details were collected: first author (year), study type, nerve monitoring format, electrode, pre/postoperative cord/ laryngeal nerve assessment, sex, approach, pathology type, surgery type, nerves at risk, RLN palsy, location time of the RLN, tracking and exposure time, surgery time, identification rate of the external branch of the superior laryngeal nerve (EBSLN), length of incision, etc. According to Anuwong et al. 13, we defined ‘RLN palsy’ as impaired movement of one or both vocal cords on laryngoscopy. ‘Transient RLN palsy’ is the complete recovery of vocal cord functional impairment detected using fiberoptic laryngoscopy within 6 months after surgery. ‘Permanent RLN palsy’ was defined as the persistence of incomplete recovery of vocal cord function detected by fiberoptic laryngoscopy within 6 months after surgery. ‘Total RLN palsy’ is a statistical concept, that is, the sum of the transient and permanent RLN palsy in the literature.
Quality assessment
The quality of the included studies was assessed using the Newcastle–Ottawa scale for observational studies and the Cochrane Collaboration’s tool for assessing the risk of bias in randomized trials14.
Study object and outcome
Our primary object is to explore whether IONM could reduce the complications and the secondary object is to evaluate whether IONM could provide assistance for intraoperative operation. The primary outcomes were temporary RLN palsy, permanent RLN palsy and total RLN palsy. Secondary outcomes were length of surgery, location time of the RLN, length of incision and recognition rate of the EBSLN. The location of the RLN was defined as the time between exposure of the thyroid lobe and clear identification of the RLN. The recognition rate of the EBSLN was defined as the ratio of the number of clearly identified supraglottic nerves to the total number of RLNs.
Statistical analysis
STATA software (version 14.0) was used to perform data effects analysis. The Mantel–Haenszel test was used to calculate the dichotomous variable odds ratio (OR), weighted mean difference (WMD) of continuous variables and the combined effect value was expressed as 95% CI. A forest plot was drawn, and differences were considered statistically significant when P<0.05. Heterogeneity analysis (Cochran’s Q test) was performed to compare the results of the included studies. If heterogeneity analysis suggested no significant heterogeneity (P>0.1, I 2 <50%), a fixed-effects model was adopted; if the heterogeneity test suggested the presence of heterogeneity (P>0.1, I 2 <50%), the causes were further analysed. A random-effects model can be used in the absence of clinical heterogeneity. The publication bias in eligible literature was analysed using funnel plots. Subgroup analysis was performed according to the disease type.
Results
Article-selection process and data extraction
The initial search using this formula yielded 635 papers. A flow diagram of the screening process is shown in Supplement Figure 1, Supplemental Digital Content 5, http://links.lww.com/JS9/A703. The titles and abstracts were read to remove any material that did not meet the requirements for inclusion. Sixteen papers were initially included, and eight papers15,22 were finally included after reading the full text, retaining two randomised controlled trials, three retrospective studies and three prospective studies involving a total of 915 patients and 1242 exposed nerves (620 in the IONM group and 622 in the non-IONM group). The characteristics of eligible studies, outcomes of the included studies, and results of the quality assessment are presented in Tables 1–3. It has been suggested that inconsistency in the definition of the timing of RLN palsy may affect the analysis of results23. Six of the eight papers included in this study defined permanent RLN palsy as the persistence of incomplete recovery of vocal cord function for 6 months after surgery. Fei et al.16 defined permanent RLN palsy as impairment of vocal cord function for at least 3 months, whereas Lee et al.21 defined permanent RLN palsy as impairment of vocal cord function for at least 12 months. Furthermore, when calculating the OR value, the number of events for total, transient and permanent RLN palsy was zero, which did not follow the statistical calculation. We excluded the literature by Fei and Lee and included the remaining six studies with primary outcome indicators to ensure consistency in the definition of laryngeal return nerve palsy and the soundness of the statistical analysis.
Figure 1.
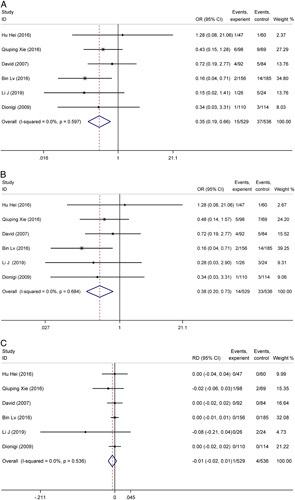
A. Forest plot of the incidence of total recurrent laryngeal nerve palsy in the intraoperative nerve monitoring (IONM) and non-IONM groups during endoscopic thyroid surgery. B. Forest plot of the incidence of transient recurrent laryngeal nerve palsy in the IONM and non-IONM groups during endoscopic thyroid surgery. C. Forest plot of the incidence of permanent recurrent laryngeal nerve palsy in the IONM and non-IONM groups during endoscopic thyroid surgery.
Table 1.
Basic characteristics of the included studies.
| S | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| References | Study type | Nerve monitoring format | Electrode | Pre/Postoperative cord/ laryngeal nerve assessment | Patients (F/M) | Permanent injury definition | Approach | Pathology Type | IONM | non-IONM |
| Hu Hei 15 | RCT | Medtronic NIM-Response | Endotracheal tube-based surface electrode | Fiberoptic laryngoscopy /fiberoptic laryngoscopy | 78/19 | 6 months | VAT | Benign | Lobectomy, subtotal lobectomy | Lobectomy, subtotal lobectomy |
| Yang Fei 16 | RCS | Medtronic NIM-Neuro, Jacksonville, FL, USA | Endotracheal tube-based surface electrode | Fiberoptic laryngoscopy/ laryngoscopy | 106 | 3 months | Breast-approach | Malignant | Radical thyroid lobectomy, radical thyroidectomy | Radical thyroid lobectomy, radical thyroidectomy |
| Qiuping Xie 17 | RCS | Medtronic, NIM-Response Jacksonville, FL | Endotracheal tube-based surface electrode | Flexible laryngoscopy/ direct laryngoscopy | 118/5 | 6 months | Breast-approach | Malignant | Thyroid lobectomy with same-side CCD, thyroidectomy and CCD for both side | Thyroid lobectomy with same-side CCD, thyroidectomy and CCD for both side |
| David 2007 18 | PCS | NIM 2, Medtronic Xomed, Jacksonville, Florida | Endotracheal tube-based surface electrode | Indirect mirror laryngeal examination, flexible fiberoptic laryngoscopy/ flexible fiberoptic laryngoscopy | 137 | 6 months | VAT | Benign/ malignant | Total thyroidectomy, hemithyroidectomy | Total thyroidectomy, hemithyroidectomy |
| Bin Lv 19 | RCS | Medtronic NIM, Minnesota, USA | Endotracheal tube-based surface electrode | Laryngoscopy/ laryngoscopy | 269/11 | 6 months | Breast-approach | Benign | Total thyroidectomy, hemithyroidectomy | Total thyroidectomy, hemithyroidectomy |
| Dionigi 20 | PCS | NIM-Response 2.0 System, Medtronic Xomed, Jacksonville, FL | Endotracheal tube-based surface electrode | Direct laryngoscopy/ direct laryngoscopy | 62/10 | 6 months | VAT | Benign | Lobectomy, total thyroidectomy | Lobectomy, total thyroidectomy |
| Hye Yoon Lee 21 | PCS | Medtronic Xomed Surgical Products, Jacksonville, FL | Endotracheal tube-based surface electrode | VHI, VRP, laryngoscopy/ VHI, VRP, laryngoscopy | 42/8 | 12 months | Breast-approach | Malignant | Total lobectomy | Total lobectomy |
| Li J 22 | RCT | NS | NS | Hoarseness of the voice | 50 | 6 months | Breast-approach | Malignant | Thyroidectomy | Thyroidectomy |
CCD, central compartment dissection; F, female; M, male; NS, not stated; PCS, postoperative comparative study; RCS, retrospective comparative study; RCT, randomized controlled trial; VAT, video-assisted thyroidectomy; VHI, voice handicap index; VRP, voice range profile.
Table 3.
NOS quality assessment of the included studies.
Table 2.
Outcomes of the included studies.
| NAR | Total RLN palsy | Transient RLN palsy | Permanent RLN palsy | Location time of RLN | Tracking and exposure time | Surgery time (min) | Identification rate of EBSLN | Length of incision | Seroma | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| References | IONM | non-IONM | IONM | non-IONM | IONM | non-IONM | IONM | non-IONM | IONM | non-IONM | IONM | non-IONM | IONM | non-IONM | IONM | non-IONM | IONM | non-IONM | IONM | non-IONM |
| Hu Hei 15 | 47 | 60 | 1 | 1 | 1 | 1 | 0 | 0 | 6.06±1.48 | 6.92±1.34 | 28.96±4.75 | 32.17±5.56 | NS | NS | NS | NS | 2.13±0.22 | 2.09±0.20 | NS | NS |
| Yang Fei16 | 66 | 61 | 1 | 9 | 1 | 8 | 0 | 1 | 3.05±1.58 | 9.36±4.82 | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Qiuping Xie 17 | 98 | 69 | 6 | 9 | 5 | 7 | 1 | 2 | 9.91±1.68 | 12.49±1.63 | NS | NS | 130±11.83 | 135±12.83 | NS | NS | NS | NS | NS | NS |
| David 18 | 92 | 84 | 4 | 5 | 4 | 5 | 0 | 0 | NS | NS | NS | NS | NS | NS | NS | NS | 3.0±1.0 | 3.7±0.9 | NS | NS |
| Bin Lv 19 | 156 | 185 | 2 | 14 | 2 | 14 | 0 | 0 | NS | NS | NS | NS | 39.87±5.39 | 40.77±4.42 | 118/156 (75.6%) | 73/185 (39.5%) | NS | NS | NS | NS |
| Dionigi 20 | 110 | 114 | 1 | 3 | 1 | 3 | 0 | 0 | NS | NS | NS | NS | 120±13.5 | 110±13 | 46/55 (83.6%) | 24/57 (42.1%) | 1.8 | 1.7 | NS | 1 |
| Hye Yoon Lee 21 | 25 | 25 | 0 | 0 | 0 | 0 | 0 | 0 | NS | NS | NS | NS | 266.40±67.26 | 274.20±44.45 | NS | NS | NS | NS | NS | NS |
| Li J 2019 22 | 26 | 24 | 1 | 5 | 1 | 3 | 0 | 2 | NS | NS | NS | NS | 118 | 149 | NS | NS | NS | NS | NS | NS |
EBSLN, external branch of superior laryngeal nerve; IONM, intraoperative nerve monitoring; NAR, nerves at risk; RLN, recurrent laryngeal nerve.
Results of data analysis
Primary outcome measure
The incidence of total RLN palsy: Six studies provided data on the incidence of total RLN palsy, without heterogeneity among study results (I 2=0%, P=0.597); thus, the fixed-effects model was adopted for meta-analysis. The prevalence of total RLN palsy in the IONM group was 2.83% (15/529) and that of total RLN palsy in the non-IONM group was 6.90% (37/536). The results of this study indicated that the difference between the two groups was statistically significant (OR=0.35, 95% CI=0.19–0.66, P=0.001). In addition, IONM significantly reduced the frequency of total RLN palsy during endoscopic thyroid surgery (Fig. 1A). The funnel plot revealed that each study’s distribution of effect points was essentially symmetrical, and that there was little publication bias. (Fig. 2A).
Figure 2.
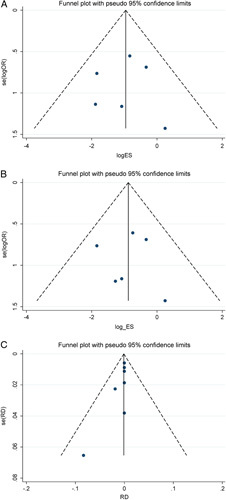
A. Funnel plot of the incidence of total recurrent laryngeal nerve palsy in the intraoperative nerve monitoring (IONM) and non-IONM groups during endoscopic thyroid surgery. B. Funnel plot of the incidence of transient recurrent laryngeal nerve palsy in the IONM and non-IONM groups during endoscopic thyroid surgery. C. Funnel plot of the incidence of permanent recurrent laryngeal nerve palsy in the IONM and non-IONM groups during endoscopic thyroid surgery.
Transient RLN palsy: Six studies provided data on the frequency of transient RLN palsy. The heterogeneity test suggested that there was no heterogeneity among the study results (I 2=0%, P=0.684); thus, the fixed-effects model was adopted for meta-analysis. The prevalence of transient RLN palsy in the IONM group was 2.64% (14/529), and the incidence of transient RLN palsy in the non-IONM group was 6.15% (33/536). In addition, the statistically significant difference between the two groups (OR=0.38, P=0.003) revealed that intraoperative neural monitoring reduced the incidence of transient RLN paralysis during endoscopic thyroid surgery (Fig. 1B). The funnel plot revealed that the degree of publication bias was minimal, and that the distribution of the effect points in each study was essentially symmetrical. (Fig. 2B).
Permanent RLN palsy: Six studies had available permanent RLN palsy data. The results showed no heterogeneity among studies (I 2=0%, P=0.536); therefore, the fixed-effects model was adopted for the meta-analysis. The rates of permanent RLN paralysis in the IONM and non-IONM groups were 0.19% (1/529) and 0.75% (4/536), respectively. The application of IONM during endoscopic thyroid surgery may lower the risk of permanent RLN damage; however, there was no statistically significant difference between the two groups (risk difference=–0.01, P= 0.260) (Fig. 1C). According to the funnel plot, the distribution of effect points among the studies was not symmetrical, and some publication bias was present (Fig. 2C).
Secondary outcome measure
Length of surgery: Five of the studies provided data on the length of surgery, with large heterogeneity between the results of the individual studies (I 2=96.7%, P<0.001); therefore, a random-effects model was used. The results of the meta-analysis showed WMD=–6.78, 95% CI=–18.54–4.99, and P=0.259 (Fig. 3), indicating that IONM might reduce operative time, but the difference between the two was not statistically significant.
Figure 3.
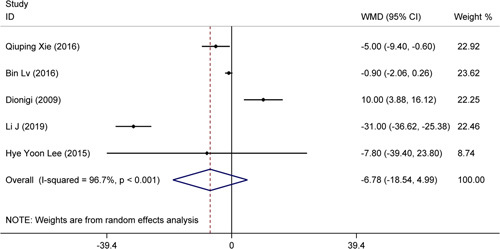
Forest plot of the surgery time in the intraoperative nerve monitoring (IONM) and non-IONM groups during endoscopic thyroid surgery.
Location time of the RLN: Three studies provided data on the location time of the RLN, with large heterogeneity between the results of each study (I 2=96.5%, P<0.001). Therefore, a random-effects model was used. Meta-analysis revealed that WMD=–3.15, P=0.007, which suggested that neuromonitoring reduced the intraoperative location time of the RLN. The results showed no significant differences between them (Fig. 4).
Figure 4.
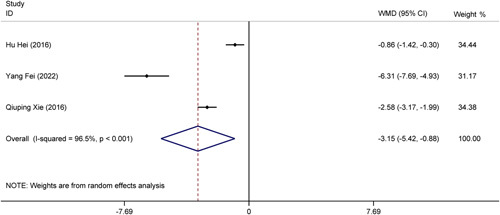
Forest plot of the location time of RLN in the intraoperative nerve monitoring (IONM) and non-IONM groups during endoscopic thyroid surgery.
Length of incision: Two studies were available with data on the length of the incision. We used a random-effects model because of the large heterogeneity between the results of the individual studies (I 2=94.9%, P<0.001). From the meta-analysis results (WMD=–0.31, P=0.396), it was clear that neuromonitoring may reduce incision length. However, none of the differences were statistically significant (Fig. 5).
Figure 5.
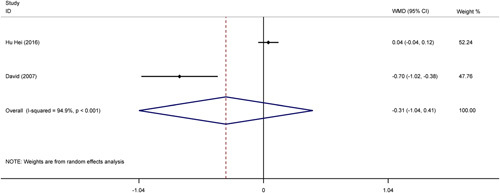
Forest plot of the length of incision in the intraoperative nerve monitoring (IONM) and non-IONM groups during endoscopic thyroid surgery.
Recognition rate of the superior laryngeal nerve: Two of the studies provided data on supraglottic nerve recognition rates, and the heterogeneity between the results was low (I 2=0.0%, P=0.448); therefore, a fixed-effects model was used. The results of the meta-analysis (OR=5.20, P<0.001) showed that the neuromonitoring technique significantly improved the recognition rate of the superior laryngeal nerve (Fig. 6).
Figure 6.
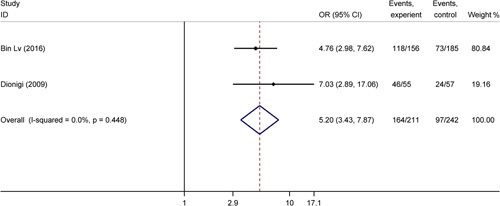
Forest plot of the recognition rate of external branch of superior laryngeal nerve in the intraoperative nerve monitoring (IONM) and non-IONM groups during endoscopic thyroid surgery.
Subgroup analysis
For the subgroup analysis of malignant tumours and benign disease, we analysed five papers, excluding two with inconsistent definitions of permanent RLN palsy and one in which the type of pathology did not distinguish between benign and malignant tumours.
The results showed that compared with benign tumours, IONM significantly reduced the incidence of transient RLN palsy in patients with malignant tumours; however, the incidence of permanent RLN palsy was not statistically significant between the two groups (total RLN palsy: OR=0.29, P=0.001; transient RLN palsy: OR=0.32, P=0.003; permanent RLN palsy: risk difference=–0.01, P=0.236) (Supplement Figs. 2–4), Supplemental Digital Contents 6-8, http://links.lww.com/JS9/A704, http://links.lww.com/JS9/A705, http://links.lww.com/JS9/A706.
Discussion
One of the most frequent complications of thyroid surgery is vocal cord paralysis caused by an RLN injury24. However, in most cases, intraoperative functional impairment of the RLN cannot be detected in time, and permanent vocal cord paralysis due to severe injury can cause serious problems in the patients’ lives, which is an important cause of medical disputes25. IONM has been widely applied as an adjunctive technique in open thyroid surgery19,26–28. Since the first successful endoscopic partial thyroidectomy in 1977, endoscopic thyroid surgery has commonly been performed in clinical practice29. Endoscopic thyroidectomy is now widely welcomed by young patients owing to its cosmetic effect, especially for total endoscopic thyroidectomy, which not only hides the scars perfectly, but also has extended indications from benign thyroid disease to thyroid cancer with or without specific lymphatic metastasis30–32. However, it is difficult to identify the RLN in patients undergoing thyroid cancer surgery; in particular, endoscopic thyroid surgery is more complicated and time-consuming than open thyroid surgery for identifying important anatomical structures, such as the RLN, and prolonged surgical time might cause more harm to the patients33. Whether IONM has the same monitoring effectiveness in endoscopic thyroid surgery remains to be explored. A systematic evaluation by Dionigi et al. 34 demonstrated the feasibility of IONM in endoscopic thyroid surgery, but did not prove its effectiveness. To investigate the influence of IONM on the occurrence of RLN palsy, this meta-analysis included eight relevant papers.
According to these findings, the incidence of transient RLN palsy during endoscopic thyroid surgery was dramatically reduced as a result of the administration of IONM. The incidence of persistent RLN palsy; however, did not decrease in a statistically significant way, which was consistent with the finding that IONM did not lower the rate of persistent RLN palsy in many thyroid surgeries23,35–37. However, the reduction of total RLN palsy rate is statistically significant. Additionally, one study with a negative link to the use of nerve monitors was visible in a forest plot (Hei, 2016). The reasons were as follows: there is a very low risk of RLN palsy after thyroid surgery. Research data show that the incidence of permanent RLN paralysis during thyroid surgery is ~0.8–1%, while that of temporary RLN paralysis is ~2.2–8%38–41. However, the sample size included in Hei’s study was small, which may be the reason for the opposite statistical results; Since all patients included in the literature were treated in a high-capacity tertiary surgical centre, endoscopic-assisted thyroidectomy was mostly performed by surgeons of middle-to-high age, with skilled surgical operation and a deep anatomical knowledge reserve. Moreover, the additional cost of INOM itself was high and was only applicable to a small number of patients. Therefore, many deviations in choice led to heterogeneity.
The results showed that IONM reduced the location time of the RLN and improved the recognition rate of the superior laryngeal nerve. The prevention of laryngeal nerve injury is critical for thyroid surgery. However, owing to the complex anatomical variations of the laryngeal nerve, even a skilled surgeon may take a lot of time to locate the RLN with the naked eye, and consequently, the operation time increases. Injuries to the RLN are often noticed by physicians, but injuries to the superior laryngeal nerve are often overlooked, and data have shown that the frequency of injury to the EBSLN during thyroid surgery reached 58%42. Injuries to this nerve seriously affect the quality of life of patients; therefore, reducing the rate of injury to the superior laryngeal nerve also became crucial in thyroid surgery. The interior and exterior branches of the superior laryngeal nerve form this nerve. While the exterior branch primarily innervates the cricothyroid muscle and stretches the vocal folds during vocalisation43, the interior branch innervates the sensory fibres of the larynx. The possibility of unintentional medically caused damage is increased by the superior laryngeal nerve’s varied path, proximity to the superior thyroid arteries, and the small area and challenging exposure of the superior pole of the thyroid gland. The application of IONM reduces the extent of dissection, improves the recognition rate of the superior laryngeal nerve, and shortens the location time of the RLN. The supraglottic nerve is variable and close to the superior thyroid vessels; however, the space at the superior pole of the thyroid is narrow and difficult to expose, which increases the risk of accidental iatrogenic injuries. The application of IONM reduces the extent of dissection, improves identification of the supraglottic nerve, and shortens the localisation time. Intraoperatively, by capturing changes in the strength of myoelectric signals, the surgeon can assist in detecting nerve function impairment that are difficult to detect with the naked eye because of many previously unappreciated operations, such as ligation, clamping, compression, pulling, electrical burns, ischaemia and suction44. Furthermore, we cannot know the results of the analysis of the operative time and length of the incision, which may be related to the ease of the operation, surgical approach, etc. Due to the paucity of data, further studies with larger sample sizes are still needed.
Regarding conventional thyroid surgery, many studies have explored the value of IONM for clinical application in thyroid reoperation, especially for patients with a thyroid malignancy pathologically confirmed postoperatively19,26,37. Consequently, patients who underwent endoscopic thyroidectomy were divided into the malignant and benign tumour groups, according to the type of postoperative pathology. In the subgroup analysis, the use of IONM during endoscopic surgery significantly reduced the incidence of temporary and permanent RLN injury in patients with thyroid malignancies, like the finding that IONM is more appropriate for advanced malignancies in conventional thyroid surgery26. Previous studies have shown that IONM reduces the incidence of transient RLN palsy, especially in high-risk thyroid cancer patients who require central compartment neck dissection. Generally, a central compartment dissection (CCD) may be performed at the same time as thyroidectomy for a malignant as opposed to a benign tumour, which requires longer exposure and tracking of the RLN than thyroidectomy alone38,45. In addition, central lymph nodes often serve as the first station of lymph node metastasis. Metastatic lymph nodes next to the RLN may adhere to the RLN, or the tumour may directly compress and invade the RLN. Therefore, the use of IONM in CCD surgery allows for better identification of the RLN and testing of the function of the RLN, as well as identification of anatomical variants of the RLN, including the Berry’s ligament, non-RLNs, extra-laryngeal bifurcation, and the varied course of the RLN at the level of the inferior thyroid artery. They also include the link between the RLN and the posterior tubercle (Zuckerkandl’s tubercle). This leads to better preservation of the RLN branches, thus improving patient outcomes and quality of life. This may be the reason why malignant tumours are more likely to benefit from IONM46,47. However, in most of the included original studies, it was difficult to determine whether CCD was performed simultaneously with thyroidectomy. Therefore, we need to carefully examine the relationship between CCD performance and the benefits of IONM application in future studies.
We attempted to performed a subgroup analysis for confounding factors (thyroiditis, surgical approaches and electrodes). When performing thyroid surgery, especially endoscopic surgery, the risk factors for thyroiditis complicate the operation method and may affect the operation time, postoperative complications and prognosis. Research has shown that in endoscopic thyroid surgery for high-risk patients (Graves’ disease), IONM can reduce the incidence of temporary RLN palsy after surgery38. In the literature we included, Xie et al. divided the study cohort into two subgroups with or without autoimmune thyroiditis and analysed the time required for surgery at different periods and the incidence of RLN injury. The results suggested that separating the RLN near the cricothyroid joint of patients with autoimmune thyroiditis is more likely to cause nerve traction injury due to stretching of the surrounding tissue, which makes the tracking and exposure of the RLN more difficult and time-consuming. However, none of the other seven studies that were included had a detailed analysis or discussion about whether the patients were complicated with thyroiditis, which limited further exploration of this factor. Currently reported lumpectomy thyroid access approaches include transthoracic breast, areolar, axillary, axillary-breast and oral. Reducing the incision during surgery and achieving the best disease treatment using advanced endoscopic instruments is a hot topic of research in endoscopic thyroid surgery48. The various approaches to endoscopic thyroidectomy have several advantages and disadvantages. Clinicians should choose the most appropriate thyroid surgery based on the location of the thyroid mass and the aesthetic needs of the patient. In this study, we planned to analyse the data in subgroups according to the surgical approach. Unfortunately, owing to the lack of data, we were unable to perform this subgroup analysis. The endotracheal surface tube electrodes, also known as recording electrodes, must contact the medial surface of the bilateral cords when appropriately positioned to monitor the surface summated depolarisation of the bilateral thyroarytenoid/vocalis muscle. Endotracheal surface tube electrodes might reduce the frequency of damage, including vocal cord or laryngeal bleeding, vocal cord laceration, infection, cuff deflation and the need for reintubation, compared with recording electrodes. For a variety of reasons, including safety, usefulness and simplicity, endotracheal tube-based surface electrode systems have become widespread and are now the most common monitoring equipment configurations41. Because all seven studies used the same manufacturer and model of neural monitors and all used endotracheal tube surface electrodes, we could not conduct further subtype analysis according to the type of neural monitors. Besides, in seven (Hei, Lee, Fei, Xie, Terris, Lv and Dionigi) of the eight articles, each patient underwent a fibreoptic laryngoscope examination before surgery to evaluate the vocal cord motor function. Patients with normal vocal cord motor function (normal RLN function) were included in these studies. Only Li et al. defined RLN paralysis as hoarseness and did not specify whether to use fibreoptic laryngoscopy, which is also the source of confounding factors and heterogeneity in the article.
During unilateral thyroidectomy, damage or rupture of the unilateral RLN may result in limited or fixed postoperative unilateral vocal fold abduction. This condition would result in hoarseness or mild dyspnoea that could be alleviated by functional compensation of the contralateral vocal fold49. The left RLN has a deep and long course, which makes it more likely to be injured during operation50. However, in total thyroidectomy, bilateral damage to the RLN caused hoarseness and a small vocal fissure, which could lead to laryngeal obstruction and even life-threatening symptoms51. In the later stage, tracheotomy should be performed to improve respiratory symptoms, and then RLN transplantation or lateral or total arytenoid cartilage excision should be performed to relieve obstructive symptoms. However, these patients generally have poor prognoses. Intraoperative nerve monitoring is clinically important in open thyroid surgery to reduce the incidence of those complications52,53. Compared with open thyroid surgery, endoscopic thyroid surgery has a longer operative time, a narrower operative field, poorer exposure, and increased operative difficulty, which could lead to a relatively higher rate of RLN injury. Therefore, intraoperative nerve monitoring is necessary and important during endoscopic thyroid surgery. This combined analysis of previous studies showed that the use of IONM can significantly improve the safety and effectiveness of endoscopic thyroid surgery to the benefit of patients.
Our meta-analysis had some limitations. For the included articles, the meta-analysis only synthesised their findings, as we could only obtain information from the published literature and could not ensure the accuracy of their methods, data, and conclusions. In addition, limited availability in relevant control trials and insufficient sample size might lead to insufficient dependability of the results.
Conclusion
The application of IONM significantly reduced the incidence of transient RLN palsy and the location time of the RLN in endoscopic thyroid surgery and improved the recognition rate of the superior laryngeal nerve. We recommend the use of IONM in endoscopic thyroid surgery, particularly in complex surgical situations. More high-quality, large-sample-sized and prospective studies are needed to further validate and explore the clinical significance of IONM.
Ethical approval
IRB approval was not needed as this is a meta-analysis of published data, however, PROSPERO registration was done.
Sources of funding
This research was supported by National Natural Science Fundation (grant number 82171127). The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Author contribution
Y.-C.L., C.-L.S.: conceptualization, formal analysis, software; Z.-Y.F., Y.-C.Z.: data curation, software, writing-original draft; writing - review and editing; Y.-X.H., B.-J.C., Y.J., S.-Y.Y., Z.T.: methodology, writing - review and editing; S.-Y.S., J.-P.W., B.-Y.L., L.Z., D.W., K.-L.W., H.-F.P., Y.-H.L.: software; supervision; validation; visualisation, writing - review and editing.
Conflict of interest disclosure
The authors have indicated they have no potential conflicts of interest to disclose.
Research registration unique identifying number (UIN)
Name of the registry: Prospero
Unique Identifying number or registration ID: CRD42022362727
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022362727
Guarantor
Prof. Ye-Hai Liu: Department of Otolaryngology, Head and Neck Surgery, the First Affiliated Hospital of Anhui Medical University, Hefei, Anhui 230031, People’s Republic of China. Tel.: +86 138 569 069 86, Fax: +0551 629 233 03. E-mail: liuyehai@ahmu.edu.cn.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Supplementary Material
Acknowledgements
The authors thank the experts who kindly responded to specific questions during the conduct of this research.
Footnotes
Y.-C.L., C.-L.S., Z.-Y.F., and Y.-C.Z. have contributed equally to this work and share the first authorship.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.lww.com/international-journal-of-surgery.
Published online 14 June 2023
Contributor Information
Yu-Chen Liu, Email: 136856076@qq.com.
Chuan-Lu Shen, Email: 2463299270@qq.com.
Zi-Yue Fu, Email: 1914010098@stu.ahmu.edu.cn.
Yu-Chen Zhang, Email: 1579141283@qq.com.
Yan-Xun Han, Email: 1423857841@qq.com.
Bang-Jie Chen, Email: chenbangjieahmu@163.com.
Yuan Jiang, Email: 2971819298@qq.com.
Si-Yue Yin, Email: 845599650@qq.com.
Zhi Tao, Email: 1274508074@qq.com.
Shu-Yan Sheng, Email: ahmussy@163.com.
Jian-Peng Wang, Email: 1455481507@qq.com.
Bing-Yu Liang, Email: 1543049251@qq.com.
Liang Zhang, Email: 568325180@qq.com.
Dong Wang, Email: yueyu1114@163.com.
Kai-Le Wu, Email: wukaile@ahmu.edu.cn.
Hai-Feng Pan, Email: panhaifeng@ahmu.edu.cn.
Ye-Hai Liu, Email: liuyehai@ahmu.edu.cn.
References
- 1. Dralle H. Surgical assessment of complications after thyroid gland operations. Chirurg 2015;86:70–77. [DOI] [PubMed] [Google Scholar]
- 2. Serpell JW, Lee JC, Yeung MJ, et al. Differential recurrent laryngeal nerve palsy rates after thyroidectomy. Surgery 2014;156:1157–1166. [DOI] [PubMed] [Google Scholar]
- 3. Bures C, Bobak-Wieser R, Koppitsch C, et al. Late-onset palsy of the recurrent laryngeal nerve after thyroid surgery. Br J Surg 2014;101:1556–1559. [DOI] [PubMed] [Google Scholar]
- 4. Chiang FY, Lee KW, Chen HC, et al. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J Surg 2010;34:223–229. [DOI] [PubMed] [Google Scholar]
- 5. Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 2004;136:1310–1322. [DOI] [PubMed] [Google Scholar]
- 6. Papaspyrou G, Ferlito A, Silver CE, et al. Extracervical approaches to endoscopic thyroid surgery. Surg Endosc 2011;25:995–1003. [DOI] [PubMed] [Google Scholar]
- 7. Zhang Z, Sun B, Ouyang H, et al. Endoscopic lateral neck dissection: a new frontier in endoscopic thyroid surgery. Front Endocrinol (Lausanne) 2021;12:796984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eisele DW. Intraoperative electrophysiologic monitoring of the recurrent laryngeal nerve. Laryngoscope 1996;106:443–449. [DOI] [PubMed] [Google Scholar]
- 9. Thomusch O, Sekulla C, Machens A, et al. Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg 2004;389:499–503. [DOI] [PubMed] [Google Scholar]
- 10. Duclos A, Lifante JC, Ducarroz S, et al. Influence of intraoperative neuromonitoring on surgeons’ technique during thyroidectomy. World J Surg 2011;35:773–778. [DOI] [PubMed] [Google Scholar]
- 11. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 12. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Anuwong A, Ketwong K, Jitpratoom P, et al. Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg 2018;153:21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hei H, Zhai Y, Qin J, et al. Intermittent Intraoperative Neural Monitoring Technology in Minimally Invasive Video-Assisted Thyroidectomy: A Preliminary Study. J Invest Surg 2016;29:93–97. [DOI] [PubMed] [Google Scholar]
- 16. Fei Y, Li Y, Chen F, et al. Intraoperative neuromonitoring of the recurrent laryngeal nerve is indispensable during complete endoscopic radical resection of thyroid cancer: A retrospective study. Laryngoscope Investigative Otolaryngology 2022;7:1217–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Xie Q, Wang P, Yan H, et al. Feasibility and Effectiveness of Intraoperative Nerve Monitoring in Total Endoscopic Thyroidectomy for Thyroid Cancer. J Laparoendosc Adv Surg Tech A 2016;26:109–115. [DOI] [PubMed] [Google Scholar]
- 18. Terris DJ, Anderson SK, Watts TL, et al. Laryngeal nerve monitoring and minimally invasive thyroid surgery. Arch Otolaryngol Head Neck Surg 2007;133:1254–1257. [DOI] [PubMed] [Google Scholar]
- 19. Lv B, Zhang B, Zeng QD. Total endoscopic thyroidectomy with intraoperative laryngeal nerve monitoring. Int J Endocrinol 2016;2016:7381792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dionigi G, Boni L, Rovera F, et al. Neuromonitoring and video-assisted thyroidectomy: A prospective, randomized case-control evaluation. Surg Endosc. 2009;233:996–1003. [DOI] [PubMed] [Google Scholar]
- 21. Lee HY, Lee JY, Dionigi G, et al. The Efficacy of Intraoperative Neuromonitoring During Robotic Thyroidectomy: A Prospective, Randomized Case-Control Evaluation. J Laparoendosc Adv Surg Tech A 2015;25:908–914. [DOI] [PubMed] [Google Scholar]
- 22. Li J, Liu C, Xi H, et al. Endoscopic thyroidectomy via bilateral axillo-breast approach with or without intraoperative nerve monitoring in patients with papillary thyroid. Surg Endosc. 2019;33:S381. [Google Scholar]
- 23. Lombardi CP, Carnassale G, Damiani G, et al. The final countdown”: is intraoperative, intermittent neuromonitoring really useful in preventing permanent nerve palsy? Evidence from a meta-analysis. Surgery 2016;160:1693–1706. [DOI] [PubMed] [Google Scholar]
- 24. Caldarelli DD, Holinger LD. Complications and sequelae of thyroid surgery. Otolaryngol Clin North Am 1980;13:85–97. [PubMed] [Google Scholar]
- 25. Bai B, Chen W. Protective effects of intraoperative nerve monitoring (IONM) for recurrent laryngeal nerve injury in thyroidectomy: meta-analysis. Sci Rep 2018;8:7761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wong KP, Mak KL, Wong CK, et al. Systematic review and meta-analysis on intra-operative neuro-monitoring in high-risk thyroidectomy. Int J Surg 2017;38:21–30. [DOI] [PubMed] [Google Scholar]
- 27. Vasileiadis I, Karatzas T, Charitoudis G, et al. Association of intraoperative neuromonitoring with reduced recurrent laryngeal nerve injury in patients undergoing total thyroidectomy. JAMA Otolaryngol Head Neck Surg 2016;142:994–1001. [DOI] [PubMed] [Google Scholar]
- 28. Kai H, Xixia L, Miaoyun L, et al. Intraoperative nerve monitoring reduces recurrent laryngeal nerve injury in geriatric patients undergoing thyroid surgery. Acta Otolaryngol 2017;137:1275–1280. [DOI] [PubMed] [Google Scholar]
- 29. Hüscher CS, Chiodini S, Napolitano C, et al. Endoscopic right thyroid lobectomy. Surg Endosc 1997;11:877. [DOI] [PubMed] [Google Scholar]
- 30. Li-Tsang CW, Lau JC, Chan CC. Prevalence of hypertrophic scar formation and its characteristics among the Chinese population. Burns 2005;31:610–616. [DOI] [PubMed] [Google Scholar]
- 31. Jeong JJ, Kang SW, Yun JS, et al. Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol 2009;100:477–480. [DOI] [PubMed] [Google Scholar]
- 32. Chung YS, Choe JH, Kang KH, et al. Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg 2007;31:2302–2306; discussion 7-8. [DOI] [PubMed] [Google Scholar]
- 33. Chan WF, Lo CY. Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg 2006;30:806–812. [DOI] [PubMed] [Google Scholar]
- 34. Dionigi G, Kim HY, Wu CW, et al. Neuromonitoring in endoscopic and robotic thyroidectomy. Updates Surg 2017;69:171–179. [DOI] [PubMed] [Google Scholar]
- 35. Pisanu A, Porceddu G, Podda M, et al. Systematic review with meta-analysis of studies comparing intraoperative neuromonitoring of recurrent laryngeal nerves versus visualization alone during thyroidectomy. J Surg Res 2014;188:152–161. [DOI] [PubMed] [Google Scholar]
- 36. Higgins TS, Gupta R, Ketcham AS, et al. Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope 2011;121:1009–1017. [DOI] [PubMed] [Google Scholar]
- 37. Zheng S, Xu Z, Wei Y, et al. Effect of intraoperative neuromonitoring on recurrent laryngeal nerve palsy rates after thyroid surgery–a meta-analysis. J Formos Med Assoc 2013;112:463–472. [DOI] [PubMed] [Google Scholar]
- 38. Barczyński M, Konturek A, Cichoń S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 2009;96:240–246. [DOI] [PubMed] [Google Scholar]
- 39. Calò PG, Pisano G, Medas F, et al. Intraoperative recurrent laryngeal nerve monitoring in thyroid surgery: is it really useful? Clin Ter 2013;164:e193–e198. [DOI] [PubMed] [Google Scholar]
- 40. Bergenfelz A, Salem AF, Jacobsson H, et al. Risk of recurrent laryngeal nerve palsy in patients undergoing thyroidectomy with and without intraoperative nerve monitoring. Br J Surg 2016;103:1828–1838. [DOI] [PubMed] [Google Scholar]
- 41. Randolph GW, Dralle H, Abdullah H, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 2011;121(Suppl 1):S1–S16. [DOI] [PubMed] [Google Scholar]
- 42. Jansson S, Tisell LE, Hagne I, et al. Partial superior laryngeal nerve (SLN) lesions before and after thyroid surgery. World J Surg 1988;12:522–527. [DOI] [PubMed] [Google Scholar]
- 43. Cernea CR, Nishio S, Hojaij FC. Identification of the external branch of the superior laryngeal nerve (EBSLN) in large goiters. Am J Otolaryngol 1995;16:307–311. [DOI] [PubMed] [Google Scholar]
- 44. Cirocchi R, Arezzo A, D’Andrea V, et al. Intraoperative neuromonitoring versus visual nerve identification for prevention of recurrent laryngeal nerve injury in adults undergoing thyroid surgery. Cochrane Database Syst Rev 2019;1:Cd012483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Seybt MW, Terris DJ. Minimally invasive thyroid and parathyroid surgery: where are we now and where are we going? Otolaryngol Clin North Am 2010;43:375–380; ix. [DOI] [PubMed] [Google Scholar]
- 46. Wojtczak B, Kaliszewski K, Sutkowski K, et al. A functional assessment of anatomical variants of the recurrent laryngeal nerve during thyroidectomies using neuromonitoring. Endocrine 2018;59:82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Toniato A, Mazzarotto R, Piotto A, et al. Identification of the nonrecurrent laryngeal nerve during thyroid surgery: 20-year experience. World J Surg 2004;28:659–661. [DOI] [PubMed] [Google Scholar]
- 48. Tae K, Ji YB, Song CM, et al. Robotic and endoscopic thyroid surgery: evolution and advances. Clin Exp Otorhinolaryngol 2019;12:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Laccourreye O, Malinvaud D, Ménard M, et al. [Unilateral laryngeal nerve paralysis in the adult: epidemiology, symptoms, physiopathology and treatment]. Presse Med 2014;43(4 Pt 1):348–352. [DOI] [PubMed] [Google Scholar]
- 50. Mountain JC, Stewart GR, Colcock BP. The recurrent laryngeal nerve in thyroid operations. Surg Gynecol Obstet 1971;133:978–980. [PubMed] [Google Scholar]
- 51. Jeon YJ, Cho JH, Lee HK, et al. Management of patients with bilateral recurrent laryngeal nerve paralysis following esophagectomy. Thorac Cancer 2021;12:1851–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gür EO, Haciyanli M, Karaisli S, et al. Intraoperative nerve monitoring during thyroidectomy: evaluation of signal loss, prognostic value and surgical strategy. Ann R Coll Surg Engl 2019;101:589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Pardal-Refoyo JL, Ochoa-Sangrador C. Bilateral recurrent laryngeal nerve injury in total thyroidectomy with or without intraoperative neuromonitoring. Systematic review and meta-analysis. Acta Otorrinolaringol Esp 2016;67:66–74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.


