Dear Editor,
LS is a zoonotic infection known by the name Weil’s disease. It is caused by the bacteriumLeptospira interrogans. This genus involves 66 species with 300+ serovars, including saprophytic and pathogenic species1. Infected animals can transmit it via their urine, both directly as well as through contaminated water or soil2. Its symptoms can range from mild influenza-like illness that is self-limiting to serious progression to multiorgan failure, ultimately resulting in death. Progression to acute renal failure and pulmonary hemorrhage is called Weil’s disease, which is life-threatening. Case fatality rates range from 5 to 50%3. In Tanzania, the incubation period of L. interrogans ranges from 2 days to 4 weeks after exposure4. Famous sources of contraction of LS in humans involve contaminated water and handling of waste products from infected animals. Confirmed cases are managed supportively. Antibiotics have also shown promising results in milder cases.
The world is currently affected by monkeypox and coronavirus disease 2019 (COVID-19)5. Gupta et al. 6 has published the evidences of coinfection between LS and COVID-19. LS and COVID-19, both can show pulmonary involvements and both can show cytokine storms and acute febrile-like illness7,8. Thus, LS can be misdiagnosed as COVID-19 in the current scenario9.
Tanzania, being a tropical country, is considered one of the favorable areas for the growth of L. interrogans 10. First incidence of LS in Tanzania dates back to 199011. Concentration of LS cases in Tanzania was found to be highest among farm and agricultural workers and also among areas with poor sanitation11, which can provide important clues about the distribution and spread of this bacterium. The Tanzanian Ministry of Health confirmed an outbreak of LS on 18 July 2022, in Lindi, a region in the southern part of the country12. Tanzania confirmed 20 cases (Fig. 1) of LS, out of which three cases from Lindi were reported dead4. These 20 cases presented in hospitals with complaints of fever, headache, epistaxis, and fatigue4. As per WHO factsheet, out of 20 cases, 15 were confirmed LS (one died), three cases were negative for LS (one died), in two cases samples were not taken (one died)13. The cases range from 18 to 77 years with a median of 45 years. Males are more affected than females.
Figure 1.
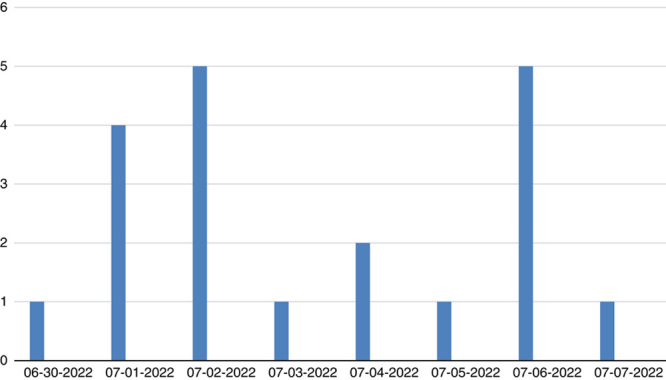
The date wise incidence rate. Source: WHO and United Republic of Tanzania Ministry of Health13.
Factors including lack of sanitation and consumption of contaminated water by the general population are the main culprit behind LS disease in Tanzania11. The tropical location of Tanzania, recurrent heavy rainfalls, irrational urbanization, wildlife intervention, floodwaters, and poor management of these issues are the leading causes of the rapid spread of the spirochetes in Tanzania14. Due to the destruction of wildlife habitats in Tanzania, animals are forced to live closer to human settlements, increasing the chances of L. interrogans infection in public14. Improper methods of agriculture and the carelessness of the masses about the proper use of safe water purification methods are causing havoc11. Misdiagnosis of LS by clinicians due to overlapping symptoms with other febrile infections is also a major concern. Lack of advanced facilities for detection of L. interrogans in developing countries like Tanzania has led many cases of LS go undiagnosed15. Another important concern is casual behavior of the population as well as travelers about improper use of preventive measures like the use of gloves while touching animals, especially their fluids, and proper covering of their body surfaces during animal activities16.
Prevention must be the earliest step to eradicate LS from Tanzania. It should be carried out by proper water sanitation, immunization of livestock, strict control of rodent population, personal hygiene, effective water purification, and wearing protective clothing. Other important guidelines include mass education, a traveler’s guide about prophylactic medicines like doxycycline, special clothing for outside trips, and taking care of any exposed surface of the body. Any febrile illness should be reported quickly, as early treatment can help medical authorities to treat and localize the source of disease in its early stages. Rapid diagnostic testing facilities must be made available to the healthcare settings as a prompt diagnosis is necessary for such deadly zoonotic disease. People who are associated with farming and livestock activities must use protective eyewear, rubber boots, and gloves, as they are at more risk of being infected with L. interrogans 17. According to Centers for Disease Control and Prevention (CDC), the government of Tanzania need to take early and effective steps to minimize the spread of the disease by implementing guidelines released by WHO16. Public service awareness campaigns are a necessary solution, considering the situation of the country and current challenges. Awareness campaigns through television, social media platforms, and advertisements by public figures can play a key role. The population should be encouraged to exercise preventive measures issued by the WHO. The community must be engaged actively, and integrated collaboration should be ensured between all the relevant departments of the country. The government of Tanzania should work on improving healthcare infrastructure, providing quick, reliable, and effective treatments, imposing safety regulations, providing personal protective equipment to medical authorities, and strict actions on the improvement of water sanitation. We believe these measures if taken effectively, can make LS-free Tanzania.
HIGHLIGHTS
Leptospirosis (LS) outbreak in Tanzania.
The Tanzanian Ministry of Health confirmed an outbreak of LS on 18 July 2022.
Tanzania confirmed 20 cases of LS, out of which 3 cases from Lindi were reported dead.
Factors including lack of sanitation and consumption of contaminated water by the general population are the main culprit behind LS disease in Tanzania.
Prevention should be carried out by proper water sanitation, immunization of livestock, strict control of rodent population, personal hygiene, effective water purification, and wearing protective clothing.
Ethical approval
Not applicable.
Sources of funding
None.
Author’s contribution
S.T. and D.M.: conceptualization and editing. S.T., A.N., R.U.A., F.N., and D.M.: writing. S.T., A.N., M.O.O., and D.M.: review with critical comments.
Conflicts of interest disclosure
The authors declare that they have no financial conflict of interest with regard to the content of this report.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
All authors.
Footnotes
This manuscript has been peer reviewed.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 27 January 2023
Contributor Information
Shehroze Tabassum, Email: shehrozetabassum8074@gmail.com.
Aroma Naeem, Email: aroma123naeem@gmail.com.
Rana U. Ahmad, Email: ranauzair503@gmail.com.
Farhan Naeem, Email: farhannaeem1231@gmail.com.
Malik O. Oduoye, Email: malikolatunde36@gmail.com.
Dattatreya Mukherjee, Email: dattatreyamukherjee4u@outlook.com.
References
- 1. Caimi K, Ruybal P. Leptospira spp., a genus in the stage of diversity and genomic data expansion. Infect Genet Evol 2020;81:104241. [DOI] [PubMed] [Google Scholar]
- 2. Russell CD, Jones ME, O’Shea DT, et al. Challenges in the diagnosis of leptospirosis outwith endemic settings: a Scottish single centre experience. J R Coll Physicians Edinb 2018;48:9–15. [DOI] [PubMed] [Google Scholar]
- 3. BMJ Best Practice US. Leptospirosis – symptoms, diagnosis and treatment. 2022 Accessed August 21, 2022. https://bestpractice.bmj.com/topics/en-us/913
- 4. The East African. Tanzania confirms outbreak of leptospirosis. 2022. Accessed August 21, 2022. https://www.theeastafrican.co.ke/tea/science-health/tanzania-confirms-outbreak-of-leptospirosis-3883916
- 5. Mukherjee D, Roy S, Singh V, et al. Monkeypox as an emerging global health threat during the COVID-19 time. Ann Med Surg (Lond) 2022;79:104075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gupta N, Wilson W, Ravindra P, et al. Coinfection of leptospirosis and coronavirus disease 2019: a retrospective case series from a coastal region in South India. J Med Virol 2022;94:4508–4511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ittyachen AM. Covid-19 and leptospirosis: cytokine storm and the use of steroids. Trop Doct 2021;51:128–130. [DOI] [PubMed] [Google Scholar]
- 8. Xavier V, Baby B, George JM, et al. Covid-19 and leptospirosis, pulmonary involvement and response to steroids: a comparative observational study from a rural tertiary care center in Kerala. J Family Med Prim Care 2022;11:294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Turmel JM, Olive C, Bigeard B, et al. Case report: pulmonary leptospirosis misdiagnosed as COVID-19. Am J Trop Med Hyg 2022;107:97–99. [DOI] [PubMed] [Google Scholar]
- 10. De Laroche M, Jauréguiberry S. Leptospirosis. Rev Prat 2016;66:886–892. [PubMed] [Google Scholar]
- 11. Motto SK, Shirima GM, de Clare Bronsvoort BM, et al. Epidemiology of leptospirosis in Tanzania: a review of the current status, serogroup diversity and reservoirs. PLoS Negl Trop Dis 2021;15:e0009918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Team HTH. NewsDetail – Fit for Travel. 2022 Accessed 21 August 2022. https://www.fitfortravel.nhs.uk/news/newsdetail.aspx?id=24263 .
- 13. World Health Organization. Leptospirosis – United Republic of Tanzania. 2022 Accessed 11 September 2022. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON403#:~:text=Leptospirosis%20%2D%20United%20Republic%20of%20Tanzania&text=As%20of%208%20August%2C%20the,cases%20have%20been%20laboratory%2Dconfirmed
- 14. Kizito Makoye. After COVID-19 Tanzania grappling with another zoonotic disease. Accessed 21 August 2022. https://www.aa.com.tr/en/africa/after-covid-19-tanzania-grappling-with-another-zoonotic-disease/2641095 .
- 15. Goarant C. Leptospirosis: risk factors and management challenges in developing countries. Res Rep Trop Med 2016;7:49–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention (CDC). Leptospirosis. 2019. Accessed August 21, 2022. https://www.cdc.gov/leptospirosis/index.html
- 17. Hookey JV. Leptospira and leptospirosis. J Biol Educ 2016;25:169–172. [Google Scholar]


