Objective:
To systematically evaluate interventions designed to improve the sustainability of surgical practice with respect to their environmental and financial impact.
Background:
Surgery contributes significantly to emissions attributed to healthcare due to its high resource and energy use. Several interventions across the operative pathway have, therefore, been trialed to minimize this impact. Few comparisons of the environmental and financial effects of these interventions exist.
Materials and methods:
A search of studies published up to 2nd February 2022 describing interventions to increase surgical sustainability was undertaken. Articles regarding the environmental impact of only anesthetic agents were excluded. Data regarding environmental and financial outcomes were extracted with a quality assessment completed dependent upon the study design.
Results:
In all, 1162 articles were retrieved, of which 21 studies met inclusion criteria. Twenty-five interventions were described, which were categorized into five domains: ‘reduce and rationalize’, ‘reusable equipment and textiles’, ‘recycling and waste segregation’, ‘anesthetic alternatives’, and ‘other’. Eleven of the 21 studies examined reusable devices; those demonstrating a benefit reported 40–66% lower emissions than with single-use alternatives. In studies not showing a lower carbon footprint, the reduction in manufacturing emissions was offset by the high environmental impact of local fossil fuel-based energy required for sterilization. The per use monetary cost of reusable equipment was 47–83% of the single-use equivalent.
Conclusions:
A narrow repertoire of interventions to improve the environmental sustainability of surgery has been trialed. The majority focuses on reusable equipment. Emissions and cost data are limited, with longitudinal impacts rarely investigated. Real-world appraisals will facilitate implementation, as will an understanding of how sustainability impacts surgical decision-making.
Keywords: carbon footprint, planetary health, surgery, sustainability
Introduction
Highlights
Surgery contributes a substantial proportion of healthcare carbon emissions.
A systematic evaluation of sustainable interventions in surgery is conducted.
Few sustainable interventions have been trialed, with little emissions or cost data.
A real-world appraisal will facilitate the future implementation of interventions.
Climate change has been declared the biggest global health threat of the 21st century1. Through rising temperatures, environmental pollution, and increasing frequency of extreme weather events, planetary health has been associated with increasing prevalence of infectious diseases, mental health illnesses, and higher mortality rates2,3. Healthcare is responsible for a substantial proportion of the global carbon footprint. In the U.S., healthcare is the second largest contributor to waste nationally and is responsible for 9–10% of the national carbon output4,5. Within healthcare, surgery significantly contributes to overall carbon emissions due to its consumption of consumables, use of anesthetic gases, and high energy requirements6. Operating theaters have been estimated to be three to six times more energy intensive compared to other parts of the hospital as a whole7. Moreover, ∼90% of operating room (OR) waste is improperly sorted and sent for unnecessary biohazard waste processing4. This often includes recoverable medical supplies that can otherwise be reused through sterilization4. Instead, biohazardous regulated medical waste (RMW) requires significant processing, usually in the form of incineration. Finally, the environmental impact of surgery is likely to grow with the increasing demand for surgery in the wake of the COVID-19 (coronavirus disease 2019) pandemic8,9.
Healthcare systems globally have reacted to this emerging need for sustainable healthcare, defined by the Academy of Medical Royal Colleges as ‘ensuring the ability to provide good quality care for future generations by balancing the economic, environmental, and social constraints and demands within healthcare settings’. In October 2020, the U.K.’s National Health Service (NHS) committed to becoming carbon net zero by 204510. In 2020, Kaiser Permanente, the largest U.S. nonprofit healthcare system, became the first to achieve its aim of carbon neutrality11. In an attempt to meet these targets, hospitals have rapidly adopted interventions to achieve more sustainable surgery. However, sustainability initiatives are evolving rapidly. Furthermore, there is significant heterogeneity in the surgical contexts in which they have been employed. There is, therefore, a paucity of robust evidence to support the implementation of these sustainability initiatives, and more work is needed to understand their impact. In addition, sustainability cannot be considered in isolation. Surgery involves complex multifactorial decision-making and trade-offs between various inputs such as clinical outcomes, available expertise, and cost12. Sustainability will, therefore, only form one aspect of this process and, until now, is unlikely to be a high priority. This resistance to sustainable interventions in surgery surrounds the financial implications of implementing these changes13. Environmental effectiveness alone has so far been insufficient to motivate healthcare organizations to implement sustainable interventions without a demonstration of cost-effectiveness. This, however, is expected to change with the imposition of net zero targets, the introduction of carbon budgets, and, more importantly, the measurement of environmental impacts on population health10.
This study, therefore, aims to critically analyze the literature concerning sustainable initiatives in surgical practice and add to the existing evidence base for these interventions. Furthermore, this review will evaluate the environmental effectiveness, be the first to evaluate the cost-effectiveness of these interventions to facilitate the decision-making underpinning their implementation and help identify opportunities within the literature for future research.
Materials and methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA)14, Supplemental Digital Content 1, http://links.lww.com/JS9/A325. The systematic review was also prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO ID: CRD 42022308035).
Search strategy and databases
A comprehensive literature search was performed on the Medline (via Ovid), Embase, and Cochrane databases. Search terms included ‘sustainability’, ‘carbon footprint’, ‘environment’, ‘planetary health’, ‘climate change’, ‘surgery’, ‘interventions’, ‘minimise’, and their synonyms. Free-text words were combined using Boolean operators in addition to medical subject heading (MeSH) terms. The full search strategy can be found in the supplementary appendix (Appendix 1), Supplemental Digital Content 2, http://links.lww.com/JS9/A326. Only English language papers and those published in the last 10 years from the search date were screened. This temporal restriction was placed as calculations regarding emissions and financial costs are based upon assumptions regarding energy production at that time; as these assumptions change longitudinally, comparisons between historical interventions are less valid and relevant. The search was performed in consultation with a librarian at the British Medical Association library on the 2nd of February, 2022.
All identified studies were uploaded to Covidence (Veritas Health Innovation, Melbourne, Australia), a Cochrane-supported systematic review package tool. Initial screening was independently conducted by two investigators (N.G. and K.L.) to determine if the eligibility criteria were met. Discrepancies were discussed and resolved either by consensus or by a third reviewer (A.A.). Studies that met the inclusion criteria underwent full-text screening. In addition, supplemental references were examined for additional relevant articles.
Study selection criteria
Studies published, including the primary and secondary outcomes as detailed below, were included. Inclusion criteria consisted of any primary articles investigating interventions or strategies that aimed to increase sustainability in surgical practice through the evaluation of carbon footprint or other environmental impacts. Exclusion criteria included any study which failed to reference surgery or procedural medical care, sustainability, or any intervention affecting the sustainability of surgery. Articles summarizing secondary data, such as systematic reviews and meta-analyses, non-English language articles, and articles published prior to 2012 were also excluded. Studies investigating the environmental sustainability of anesthetic agents alone were excluded as they do not pertain to the practice of surgical care, and there is an abundance of existing secondary literature within this area15. However, anesthetic interventions altering the modality of the anesthetic were included. Studies with inadequately published data with regard to the primary and secondary outcome measures were also excluded.
Data extraction and outcomes
The primary outcome of this systematic review was to detail the interventions which have been employed in the literature to increase sustainability in surgery. The secondary objectives were to understand the environmental and financial outcomes of these interventions. All study characteristics and outcome measures were independently extracted by two investigators (N.G. and A.A.) into a prespecified table on Covidence with the following columns: first author, year published, country, study details, surgical specialty, process investigated, sustainable intervention, control standard, measure of environmental impact, environmental and cost outcomes. Discrepancies were discussed and resolved either by consensus or by a third reviewer (K.L.).
Interventions and outcome measures
Interventions described within the included studies were subsequently grouped through discussion between authors (A.A. and N.G.) into five key domains based on the Royal College of Surgeons of England’s ‘Sustainability in the operating theatre’ guidelines16: ‘reduce and rationalize’; ‘reusable equipment and textiles’; ‘recycling and correct waste’ segregation’; ‘anaesthetic alternatives’; and ‘other’ interventions.
Outcome measures were those which quantified environmental and cost outcomes. Environmental outcome measures varied depending on the study methodology; however, examples include carbon dioxide/greenhouse gas emissions, waste reduction, and percentage of energy reduction.
Quality assessment
Two assessors (N.G. and K.L.) independently assessed the quality of each paper. Discrepancies were discussed and resolved either by consensus or by a third reviewer (A.A.). Due to the heterogeneity of study design within the included studies, it was necessary to employ multiple different quality assessment tools. The Cochrane Risk of Bias In Non-randomized Studies-of Interventions (ROBINS-I) tool was used to assess the quality of non-randomized trials17. Quality of life cycle assessments (LCAs) were assessed using criteria designed for critical review of LCAs18. Studies that were not appropriate to be assessed by the previous two assessment tools were assessed by a custom tool that considers three key sources of uncertainty concerning sustainability studies: parameter, scenario, and model uncertainty19.
Results
The literature search retrieved a total of 1162 results. Following title and abstract screening, the full texts of 56 studies were analyzed and 25 interventions described in 21 studies were found to be eligible for inclusion (Fig. 1). There was a preponderance of studies from the U.S.A. (11/21). The majority of studies were observational (Table 1). Interventions were mapped to one of five domains.
Figure 1.
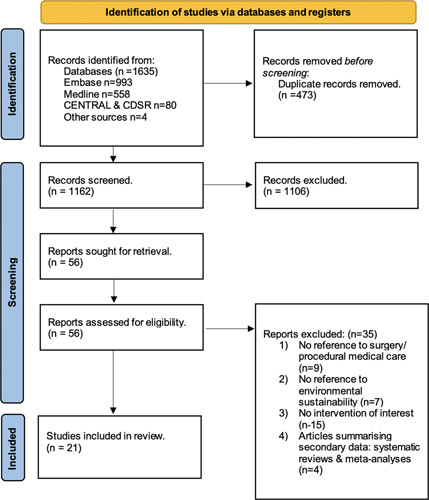
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement) flow diagram of search and study selection process.
Table 1.
Characteristics of included studies, and classification of interventions into five domains.
| Study | Study type | Country | Specialty | Study design and details | |
|---|---|---|---|---|---|
| 1. Reduce and rationalize | |||||
| Thiel et al., 201840 | Quantitative, prospective | U.S.A. | Obstetrics and Gynecology | 17 laparoscopic hysterectomy procedures. Quantitative prospective, single-centered study | |
| Thiel et al., 201921 | Quantitative, retrospective | U.S.A. | Orthoplastic Surgery | 178 small hand surgeries. 2 surgeons performing the surgery. Quantitative, retrospective, single-centered study | |
| Rizan et al., 202222 | Quantitative, prospective, audit data | U.K. | All | Evaluation of carbon footprint and financial cost of decontamination and packaging of reusable surgical instruments | |
| Wormer et al., 201320 | Longitudinal, observational, noncontrolled | U.S.A. | All | 17 000 inpatient surgeries. Measured over a year. One hundred consecutive physicians’, nurses’, residents’, and technicians’ scrub cycles. Quantitative, prospective, single-centered study | |
| 2. Reusable equipment and textiles | |||||
| McGain et al., 201229 | Quantitative, retrospective LCA | Australia | Anesthetic | LCA of one single-use and one reusable central venous catheter (CVC) kit. Quantitative, retrospective, single-centered study | |
| Eckelman et al., 201223 | Quantitative, retrospective LCA | U.S.A. | Anesthetic | LCA of 40 disposable laryngeal masked airways (LMAs) and 40 uses of 1 reusable LMA. Quantitative retrospective, single-centered study | |
| McGain et al., 201732 | Quantitative, retrospective LCA | Australia | Anesthetic | LCA of five scenarios of replacing reusable anesthetic equipment with single-use variants. Quantitative, retrospective, multicentered (two hospitals with six operating rooms) study | |
| Sherman et al., 201824 | Quantitative, retrospective LCA | U.S.A. | Anesthetic | LCA of one stainless steel reusable and two (one metal and one plastic) single-use device rigid laryngoscope handles and blade alternatives. Quantitative, retrospective, single-centered study | |
| Davis et al., 201831 | Quantitative, retrospective LCA | Australia | Urology | LCA of single-use digital flexible ureteroscope and Olympus Flexible Video Ureteroscope per case. Quantitative, retrospective, single-centered study | |
| Astroza et al., 202026 | Pre–post, noncontrolled, prospective study | Chile | Urology | Conference abstract of an evaluation of plastic waste reduction from intervention. Mixed methods: questionnaire (results not included) and quantitative, prospective, pre–post noncontrolled study | |
| Leiden et al., 202030 | Quantitative, retrospective LCA | Germany | Orthopedic Surgery | LCA of reusable or disposable instruments needed for one single-level lumbar fusion surgery. Quantitative, retrospective, single-centered study | |
| Jabouri and Abbott, 202227 | Quantitative, prospective | U.K. | Dermatology | Evaluation of the environmental impact of 62 packs (14 single-use and 48 reusable), reflecting an average weekly use. Quantitative, prospective, single-centered study | |
| Vozzola et al., 202025 | Quantitative, retrospective LCA | U.S.A. | All | LCA of 1000 uses of a gown in an OR setting. Examined 11 reusable and 7 disposable gowns. Quantitative, retrospective, single-centered study | |
| Rizan and Bhutta, 202228 | Quantitative, retrospective LCA | U.K. | General Surgery | LCA of equipment required for one laparoscopic cholecystectomy. Quantitative, retrospective, single-centered study | |
| Rizan et al., 202222 | Quantitative, prospective audit data | U.K. | All | Evaluation of carbon footprint and financial cost of decontamination and packaging of reusable surgical instruments | |
| 3. Recycle and waste segregation | |||||
| Debois et al., 201333 | Pre–post, noncontrolled, prospective study | U.S.A. | Cardiovascular | 400 consecutive cases. Quantitative, prospective, pre–post noncontrolled, single-centered study | |
| Wormer et al., 201320 | Quantitative, prospective | U.S.A. | All | 17 000 inpatient surgeries. Measured over a year. One hundred consecutive physicians’, nurses’, residents’, and technicians’ scrub cycles. Quantitative, prospective, single-centered study | |
| Thiel et al., 201840 | Quantitative, prospective | U.S.A. | Obstetrics and Gynecology | 17 laparoscopic hysterectomy procedures. Quantitative prospective, single-centered study | |
| 4. Anesthetic alternatives | |||||
| McGain et al., 202035 | Pre–post, noncontrolled, prospective study | Australia | Anesthetic | Ex-vivo modeling, simulation study. A simple lung model with fixed CO2 inflow. LCA. | |
| Thiel et al., 201840 | Quantitative, prospective | U.S.A. | Obstetrics and Gynecology | 17 laparoscopic hysterectomy procedures. Quantitative prospective, single-centered study | |
| McGain et al., 202135 | Quantitative, prospective | Australia | Anesthetic | LCA of all anesthesia needed for a total knee replacement, using general, spinal, or combined anesthesia. Twenty-nine patients. Quantitative prospective, single-centered study | |
| Griffin et al., 202234 | Conference abstract of a retrospective study | U.K. | Anesthetic | Conference abstract of a retrospective study | |
| 5. Other | |||||
| Moussa et al., 202236 | Quantitative, retrospective, continuous, comparative, multicenter trial | U.K. | Ophthalmology | 3239 rhegmatogenous retinal detachment procedures in three centers, over 4 years. Quantitative, retrospective, continuous, comparative multicenter trial | |
| Unger et al., 201737 | Quantitative, retrospective | U.S.A. | Obstetrics and Gynecology | LCA of all medical devices that contained petroleum-based plastics suitable for biopolymer substitution for a single hysterectomy, separated into laparoscopic, abdominal, vaginal, and robotic. Quantitative, retrospective, single-centered study | |
| Rizan et al., 202222 | Quantitative, prospective audit data | U.K. | All | Evaluation of carbon footprint and financial cost of decontamination and packaging of reusable surgical instruments | |
LCA, life cycle analysis; OR, operating room; U.K., United Kingdom; U.S.A., United State of America.
Reduce and rationalize
This domain constituted interventions that aimed at minimizing material use or OR energy expenditure, which was included in four studies20–23. Two studies investigated the reduction of OR energy use: installing occupancy sensors to reduce air turnover caused energy usage to reduce by one-third per OR40, and routinely turning off anesthetic and OR equipment when not in use decreased CO2 emissions by 234.3 metric tons over the course of a year20. Additionally, converting from soap to alcohol-based waterless scrub demonstrated a potential saving of 2.7 million liters of water annually23.
Another reduction intervention was minimizing material use by determining a list of only the essential surgical materials required for the procedure: this minimal pack produced 13% (0.3 kg CO2 eq per case) lower CO2 emissions than the standard21. However, in a different study, individually wrapping items produced more (38 g CO2 eq per item) compared to equipment sets22.
Reusable equipment and textiles
Out of the 21 studies, 11 investigated reusable equipment and textiles22,24–33. Studies investigating the environmental impact of reusable equipment found that this was associated with 40–66% lower emissions than the single-use equivalents23–27. Hybrid general surgical equipment, which is predominantly reusable with some single-use components, also remained preferable to single-use approaches28.
Overall, most studies concluded reusable equipment was more environmentally sustainable, with manufacture and disposal processes being the largest contributors to single-use products23,27–31. However, this was not the case in all studies29–32 and was dependent on the electricity source of the hospital29,32, as well as the sterilization process of reusable equipment, which accounted for most of the greenhouse emissions of reusable devices23,24,27–32. Two studies29,32 found that reusable equipment produced higher CO2 emissions than single-use alternatives because of Australian hospitals’ use of brown coal for electricity generation, which is particularly CO2 emissions-intensive. Repeating their analyses with equivalent energy data from the U.K. and U.S., where more renewable sources are used, they demonstrated that reusable approaches remained more sustainable in those areas.
Recycling and correct waste segregation
Three studies investigated recycling and waste segregation interventions20,23,34. This domain incorporated waste management initiatives, including recycling interventions and those that improved appropriate waste segregation. In one study, a primarily educational campaign achieved a 75% reduction in biohazardous RMW20. Another study avoided 7500 kg of RMW by diverting waste from the heart–lung machine bypass circuit to municipal solid waste following a complete rinsing33. Maximizing recycling led to a 2% decrease in greenhouse emissions per case compared to the baseline40.
Anesthetic alternatives
Anesthetic interventions that altered the modality of the anesthetic (and surgical practice) or those in which such innovations were reported with others, were included in four studies20,35–37. Two studies compared CO2 eq produced per year by spinal anesthesia (SA) versus general anesthesia (GA)34,35. Debois et al.33 found that there was an estimated saving of 12 921.51 kg CO2 eq per year by converting all suitable procedures from GA to SA. Conversely, Wormer et al.20 did not find a significant difference between GA, SA, and combined approaches (14.9 vs. 16.9 vs. 18.5 kg CO2 eq) when energy was primarily coal-based. However, when this was modeled using energy data from Europe and the U.S.A., which have more renewable sources, SA use again produced lower carbon dioxide equivalent emissions than the GA and combined approaches.
Due to the abundance of literature already summarizing the environmental sustainability of anesthetic agents, this study did not include papers that only investigated anesthetic agents as interventions. However40, included due to its investigation of other interventions, found that switching from volatile anesthetic agents to propofol yielded the greatest reduction in emission (28%) per case, whereas volatile anesthetic gases avoiding desflurane decreased emissions by 25%.
Other interventions
These included interventions that could not readily be classified into one of the domains. These included a multicentered trial comparing the environmental impact of using air tamponade versus fluorinated gases in repairing selected rhegmatogenous retinal detachment (RRD). When using air tamponade in 70% of RRD repairs, one hospital achieved 47.0% and 41.1% lower CO2 emissions compared to another two hospitals using fluorinated gas36.
Moreover37, investigated the potential environmental benefits of substituting petroleum-based plastics in single-use medical devices, measuring nine endpoints from the Tool for Reduction and Assessment of Chemical and Other Environmental Impacts (TRACI), as well as calculating cumulative energy demand. Though the use of biopolymers correlated with reductions in carcinogenic impacts, noncarcinogenic impacts, and respiratory effects, the significant agricultural inputs associated with manufacturing biopolymers exacerbated environmental impacts.
Finally, Rizan et al.22 concluded that carbon emission due to sterilization could be decreased by integrating individually wrapped instruments into sets, efficient machine loading, using low-carbon energy sources, and recycling sterile barrier systems.
Cost outcomes
Where available, the financial cost is listed in Table 2. In general, the sustainable interventions that reduced environmental impact also offered a long-term financial benefit when implemented20,22–24,27,28,33,34,40. This economic advantage was maintained for reusable equipment even when the Australian coal-based energy sources led to higher environmental impact5,26.
Table 2.
Summary of the sustainability interventions and their environmental and financial effects.
| Study | Intervention | Control | Environmental outcomes | Cost outcomes | Authors’ conclusions |
|---|---|---|---|---|---|
| 1. Reduce and rationalize | |||||
| Thiel et al., 201840 | Occupancy sensors in low-use times, using low-carbon electricity source, and combination | Standard practice | Occupancy sensors led to a 2% reduction in baseline emissions per case and reduced the electricity use by one-third over the course of a year per OR, whilst a switch to renewable energy sources led to a 9% reduction. A combination of these measures | N/A | ‘To reduce the environmental emissions of surgeries, healthcare providers need to implement a combination of approaches, including reducing off-hour energy use in the operating room’ |
| Thiel et al., 201921 | Equipment use: ‘Minimal’ custom pack of disposable surgical supplies for small hand surgery and local anesthetic only | Standard pack (determined by physician choice) with local anesthesia and sedation | Local-only hand surgery with the minimal pack produced 0.3 kg per case (13%) less waste than the use of standard pack during local anesthesia and sedation surgeries | The minimal pack costs $17.60, while the standard pack costs $47.33. If the minimal pack is used the total cost pf equipment (pack plus additional items for respective surgery) per case was $104.69 compared to $230.13 using standard pack with local and sedation | ‘Surgical waste and spending can be reduced by minimizing the materials brought into the operating room in disposable packs. Local-only techniques may provide an opportunity to drive sustainability by paring back what is considered… with concomitant emphases on patient satisfaction and the efficient use of time and resources’. |
| Rizan et al., 202122 | Packaging: instrument sets | Individually wrapped instruments | Decontamination and packaging instruments led to 66–77 g CO2 eq per instrument in the set. Individually wrapped instruments led to a footprint 189 g CO2 eq per item. Removing items from a set proportionally increased the footprint, with an increase on average of 38 g CO2 eq per item removed across all operations requiring the streamlined set. | The cost of decontamination and packaging was €1.05–€1.07 per instrument in containers and €7.35 per individually wrapped instrument | ‘Carbon and financial savings can be made by preparing instruments as part of sets, integrating individually wrapped instruments into sets rather than streamlining them, efficient machine loading, and using low-carbon energy sources alongside recycling’ |
| Wormer et al., 201320 | The Green OR Committee: energy (power down) and water reduction (waterless scrub) | ‘Power down’ initiative to turn off all anesthesia and OR lights and equipment not in use caused CO2 emissions to decrease by 234.3 tons, and the alcohol-based waterless scrub could potentially save 2.7 million liters water | Cost savings (dollars per year) Power down : 33 000 Waterless scrub: 2000 |
‘Green OR Committees can significantly impact the environmental footprint of hospitals. Simple changes by designated leaders in the OR can lead to a sustainable, environmentally conscious workplace with …downstream cost reduction’ | |
| 2. Reusable equipment and textiles | |||||
| McGain et al., 201229 | 300-use reusable CVC insertion kits | Single-use CVC kit | Sterilization was the highest environmental cost for reusable CVC, leading to higher CO2 emissions (1211 g vs. 407 g) and water use (27.7 l vs. 2.5 l). Manufacturing/production was the highest environmental cost for single-use CVC, leading to higher mineral and solid waste |
The cost of the reusable CVC was lower (AUS $6.35 vs. AUS $8.65) per use with LCA calculations. Initial purchase of reusable is more expensive (AUS $35.20 vs. AUS $8) However, loss of equipment from reusable packs could increase the costs of reusable packs to similar costs of those of single-use devices |
‘Reusable central venous catheter insertion kits were less expensive than were the single-use kits. …the environmental costs of the reusable kit were considerably greater than those of the single-use kit. Efforts should be directed toward decreasing the water and energy consumed in cleaning and sterilization. The source of hospital electricity significantly alters the relative environmental effects of reusable items’ |
| Eckelman et al., 201223 | 40-use reusable LMA | Single-use LMA | Reusable LMAs contributed 7.4 kg CO2 over the life cycle, while 40 disposable devices contribute 11.3 kg CO2. The largest source of greenhouse gas emissions for disposable devices is PVC production (23%). Polycarbonate productions (14%), transportation (14%), thermoforming (13%) and waste disposal (11%) also contribute. The main source for reusable LMAs is from sterilization (77%) |
A reusable device costs $8/use, ($5 device cost+$3 cleaning) compared to $9.60/use for single-use device using LCA results. However initial cost of reusable devise is $200, compared to the $9.60 single-use device |
‘The differences in environmental impacts between these devices strongly favor reusable devices. These benefits must be weighed against concerns regarding transmission of infection. Healthcare facilities can decrease their environmental impacts by using reusable LMAs, to a lesser extent by selecting disposable LMA models that are not made of certain plastics, and by ordering in bulk from local distributors’ |
| McGain et al., 201732 | Reusable usable LMAs and direct laryngoscopy blades, facemasks, and circuits | Single-use equipment | Reusable devices had 9% higher emission than using mainly single-use approach (5575 kg CO2 eq vs. 5095 kg CO2 eq). Contributions to reusable emissions were washer electric use (4807 kg CO2 eq) and peroxide electricity (387 kg CO2 eq). For single-use emissions were from facemask purchases (2695 kg CO2 eq) and laryngoscopy blades (1396 kg CO2). Using a European power mix would result in 84% reduction in emissions if using reusable equipment (5575 kg CO2 eq to 802 kg CO2 eq) |
Annual cost to use mainly single- use equipment was AUS $69 018 (46% higher) versus with reusable equipment (AUS $36 985) |
‘Converting from single-use to reusable anesthetic equipment saved more than AUD$30 000 (£18 000) per annum, but increased the CO2 emissions by almost 10%. The CO2 offset is highly dependent on the power source mix, while water consumption is greater for reusable equipment’ |
| Sherman et al., 201824 | 400-use reusable laryngoscopy blade and handles | Single-use laryngoscope blade and handles | Reusable steel handles with high-level disinfection produce 25 times fewer greenhouse emissions (0.06 kg CO2 eq) than single-use plastic (1.41 kg CO2 eq) or metal (1.60 kg CO2 eq) handles. Sterilization of reusable devices increases emissions by 400%, but 40–50% less than single-use alternatives |
When extrapolating over a year of use, using single-use handles increased cost by $495–604 000 and $180–265 000 for blades, depending on the cleaning regimen of reusable devices | ‘The reusable options presented a considerable cost advantage, in addition to offering a better option environmentally. Avoiding overcleaning reusable laryngoscope handles and blades is desirable from an environmental perspective. Costs may vary between facilities, and LCC methodology demonstrates the importance of time–motion labor analysis when comparing device options’ |
| Davis et al., 201831 | Single-use digital flexible ureteroscope | 180-use flexible video ureteroscope | The environmental costs of single-use and reusable flexible ureteroscopes are comparable, with single-use lower (4.43 kg vs. 4.47 kg CO2 per case). Manufacturing contributed most to the footprint of single-use devices (86.5%) (3.83 vs. 0.06 kg CO2 per case) compared to sterilization of reusable scopes (88.4%) (3.95 kg CO2 per case). Replacement would result in 1.6 tons of plastic reduced per year |
N/A | ‘The environmental impacts of the reusable flexible ureteroscope and the single-use flexible ureteroscope are comparable. Urologists should be aware that the typical life cycle of urologic instruments is a concerning source of emissions’ |
| Astroza et al., 202026 | Reuse sterile paper for the C-arm and to reduce to one aspiration hose | Standard practice during flexible ureterolithotomy | Reuse of C-arm paper and reduction in aspiration hose led to a reduced amount of average plastic waste per case compared to usual care (583.8 g vs. 1186 g of plastic) | N/A | ‘Intervention was associated with a significant decrease in plastic waste produced… If all the procedures were developed… with this simple intervention we would reduce 1.7 tons of plastic per year’ |
| Leiden et al., 202030 | 500-use and 300-use reusable instrument sets for single-level lumbar fusion surgeries | Single-use sets | Disposable sets led to an environmental advantage of 45–85% compared to reusable sets in all impact categories. The main impact is with production. Sterilization (predominantly washing/steam) was the major contributor for the reusable devices. Selected sterilization processes account for 90% of emissions of reusable devices |
N/A | ‘The selected cleaning and sterilization process for reusable instruments decides which system is advantageous from an environmental perspective. Reducing the number of instruments to be cleaned and sterilized for a surgery should be the focus for future surgery instruments development from an environmental perspective’ |
| Jabouri and Abbott, 202227 | Reusable instrument sets for skin surgery | Single-use sets | Emissions were greater for single-use compared reusable sets (1.436 vs. 1.121 kg CO2 eq). Sterilization (40.6%), production (37.2%) and disposal (22.2%) contributed to emissions for reusable packs. Production (62.6%) and disposal (37.4%) contributed to single-use set emissions |
The cost of single-use sets was £20.57 compared to £13.35 for reusable devices, per use based on a weekly usage. Based on average weekly use of 14 single-use and 48 reusable sets, this equates to £50 659.54 per year) | ‘As reusable dermatology theatre packs were found to be more sustainable, greater benefits can be expected with a global shift to reusable packs for skin surgery. Studies should explore the benefits and harms to patients and staff for both single-use and reusable packs for skin surgery’ |
| Vozzola et al., 202025 | 60 use reusable surgical gowns | Single-use gowns | Manufacturing processes of reusable gowns (1000 uses) reduced: resource energy (64%), emissions (66%), water use (83%), and solid waste (83%) compared to single-use gowns The mass of reusable gowns (60 use life) was 96% lower than single-use gowns produced. Laundry accounted for 51% of energy consumption and 50% of the emissions for the reusable gowns. Benefit of reusable producing fewer gowns and lower mass offsets the laundry burden |
N/A | ‘The reusable surgical gown system consumed less energy, had a reduced global warming potential, reduced blue water consumption, and solid waste generation. Perioperative and facility leaders can use these results to address environmental sustainability concerns related to surgical gown waste’ |
| Rizan and Bhutta, 202228 | Hybrid laparoscopic clip appliers, scissors, and ports. Hybrid contains both single-use and reusable components | Single-use equipment | The carbon footprint using hybrid devices in laparoscopic cholecystectomy was 24% the level of single-use devices (1756 vs. 7194 g CO2 eq), saving 5.4 kg CO2 eq per operation. This is mainly due to single-use components (62%), and decontamination (37%). Manufacture (57%), onward transportation (29%), and waste (14%) contributed to single-use devices |
Life cycle cost analysis of products, taking into account unit cost, decontamination, and disposal costs: per operation the cost per cholecystectomy of using a combination of hybrid devices was 46% that of using single-use equivalents (£131 vs. £282) | ‘Adoption of hybrid laparoscopic instruments could play an important role in meeting carbon reduction targets for surgery and also save money’ |
| Rizan et al., 202222 | Single-use tray wraps or flexible pouches | Rigid reusable aluminum containers | Carbon footprint per instrument for single-use tray wrap containers was lower than reusable aluminum or flexible pouches (13 vs. 25 vs. 44 g CO2) | The cost of two layers of single-use tray wrap was e1.36. The flexible pouch cost e1.75 per instrument. The cost of the aluminum container was e0.79 per use | ‘Carbon and financial savings can be made by preparing instruments as part of sets, integrating individually wrapped instruments into sets rather than streamlining them, efficient machine loading, and using low-carbon energy sources alongside recycling’ |
| 3. Recycle and waste segregation | |||||
| Debois et al., 201333 | Waste disposal: diverting waste from the heart–lung machine bypass circuit to municipal solid waste (MSW) | Disposal via regulated medical waste (RMW) | Based upon circuit weight of 15 lbs, 7.5 tons of trash will be diverted from RMW. 1800 ml of solution was required per case to rinse the circuit | The additional cost of rinsing was $2/rinse. At a cost of five times higher, traditional RMW significantly adds to operating expenses | ‘This process not only releases a significantly less amount CO2 but helps generate renewable energy. The bypass circuit diversion pilot project effectively demonstrates decreases in the carbon footprint’ |
| Wormer et al., 201320 | The Green OR Committee: campaigns established include solid waste reduction, OR recyclables, and reusables | Standard practice | Recycling devices diverted 12 860 lbs solid waste, 75% of red biohazard bag waste has been reduced, recycling and reusing batteries diverted 500 lbs alkaline waste, reusable gel OR padding caused complete reduction of foam waste | Cost savings (dollars per year) Recycling single-use: 4000 Reducing red biohazard bag waste : 60 000 Recycling batteries: 9000 Reusable gel OR padding : 50 000 |
As previous |
| Thiel et al., 201840 | Maximizing recycling, maximizing RMW, reusing linen, reusable gowns, and drapes, single-use reprocessing, minimizing instrument use, and combination | Standard practice | Recycling led to a 2% decrease in emission per case compared baseline. Reusing towels (2%), using reusable linens (2%), reprocessing single-use devices (13%), and using minimal instruments (64%) all led to decrease in emissions per case. Maximizing regulated medical waste increased emissions by 3% | N/A | As previous |
| 4. Anesthetic alternatives | |||||
| McGain et al., 202035 | Use of high fresh gas flow (FGF) with an efficient heat and moisture exchange filter | Circle breathing system with low FGF | Increasing FGF from 1 to 6 l/min was associated with 93% reduction in the combined running cost with minimal net change to 100 years global warming potential. Most reductions occurred between 4 and 6 l/min. Removing CO2 absorbent, and increasing FGF to control CO2 rebreathing, afforded minimal further cost benefit, but doubled the global warming potential | N/A | ‘In the absence of inhalational anesthetic agents, increasing FGF to 6 l/min reduces running cost compared with lower FGFs, with minimal impact to the environment’ |
| Thiel et al., 201840 | Use of alternative anesthetic agents in clinically appropriate cases | Standard practice | Switching to propofol yielded the greatest reduction in emission (28%) per case, then sevoflurane only (27%) and sevoflurane+N2O (26%). Use of desflurane increased emission compared baseline emissions by 36%. | N/A | As previous |
| McGain et al., 202135 | Use of spinal anesthesia with sedation (SA) or combined general anesthetic and spinal | Use of general anesthetic (GA) (either volatile or total intravenous, i.v.) | The emissions were similar for GA, SA, and combined approaches (14.9 vs. 16.9 vs. 18.5 kg CO2 eq). Electricity for the air warmer contributed 20% for GA, 21% SA, and 19% combination. Sevoflurane contributed to GA (35%) and combined (19%) emissions. Washing and sterilizing reusable items contributed to SA (29%), combined (24%), and GA (4%). Oxygen was key to the SA carbon footprint (18%) | N/A | ‘All anesthetic approaches had similar carbon footprints. Rather than spinal being a default low-carbon approach, several choices determine the final carbon footprint: using low-flow anesthesia/total intravenous anesthesia, reducing single-use plastics, reducing oxygen flows, and collaborating with engineers to augment energy’ |
| Griffin et al., 202234 | Spinal anesthesia | General anesthesia | There was an estimated saving of 12 921.51 kg CO2 eq per year if all suitable procedures were converted from GA to SA | There was an estimated saving £13 054.55 per year if all suitable procedures are undertaken using SA then GA | ‘The greatest reduction in both CO2 and financial cost could be achieved if all suitable day-case operations were performed under SA in preference to GA. This be reduced if the requirement for sterile surgical gowns for SA were not necessary, or reusable gowns were used’ |
| 5. Other | |||||
| Moussa et al., 202236 | Alternative operative technique: air tamponade (AT) | Fluorinated gases in repairing selected rhegmatogenous retinal detachment (RRD) | Employment of fluorinated gas systems led to 63 times higher CO2 emissions per repair than with air tamponade. The hospital which used air tamponade in 70% of RRD repairs, had 47.0% and 41.1% lower emissions compared to hospitals using fluorinated gas. Assuming 30% of repairs are suitable with AT in the U.K., its use could reduce 716.5 tons of CO2 annually, corresponding to a 44.3–56.6% reduction in emissions from RRD repairs, depending on the gas used |
N/A | ‘AT versus the fluorinated gases can reduce in carbon footprint in the management of RRD. Further studies are required to determine the most ‘environment-friendly’ intraocular tamponade without compromising patient outcomes center that also routinely employs AT in selected RRD cases’ |
| Unger et al., 201737 | Single-use medical devices with biopolymers substituted for plastics | Single-use devices containing plastics | Biopolymers are favorable with respect acidification (19–29%), ecotoxicity (1–2%), carcinogenic (3–4%), noncarcinogenic (25–61%), respiratory effects (16–25%), and energy demand (53–84%). But petroleum-based plastics have better impact with respect global warming, eutrophication, ozone depletion, and smog (700% less in laparoscopy), due to agricultural activities associated with manufacturing. | N/A | ‘The integration of biopolymers into medical products is correlated with reductions in carcinogenic impacts, noncarcinogenic impacts and respiratory effects; however, the significant agricultural inputs associated with manufacturing biopolymers exacerbate environmental impacts’ |
| Rizan et al., 202222 | Optimized loading for decontamination | Suboptimal loading for decontamination | Part-loading of machines increased the carbon footprint by a factor of 2.6 compared with typical loading (137 vs. 52 g CO2 eq per instrument). As the number of instruments per set or slot increased, the carbon footprint decreased, and decreased further by improving the loading efficiency |
N/A | ‘Carbon and financial savings can be made by preparing instruments as part of sets, integrating individually wrapped instruments into sets rather than streamlining them, efficient machine loading, and using low-carbon energy sources alongside recycling’ |
AT, air tamponade; AUS, Australian; CO2 eq, carbon dioxide equivalent; CVC, central venous catheter; emissions, greenhouse gas emissions; FGF, fresh gas flow; GA, general anesthetic; LCA, life cycle analysis; LCC, life cycle cost; LMA, laryngeal mask airway; N/A, not applicable; N2O, nitrous oxide; OR, operating room; RMW, regulated medical waste; RRD, rhegmatogenous retinal detachment; SA, spinal anesthetic.
Whilst most studies provided costings from the entire life cycle, a few studies provided short-term information on financial costs, such as the initial cost of manufacture and purchase21–23,29. Reducing and rationalizing initiatives were more financially beneficial in the short term as well as the long term21,22. Conversely, reusable equipment was considerably more costly at initial purchase, despite always providing a significant long-term financial benefit23,29.
Astroza et al.26 concluded that reusable equipment only remained financially beneficial over a period of time if there was a minimization of loss of equipment from reusable packs. The overall cost is increased if reusable equipment is discarded prior to reusing for the recommended number of lifetime uses23,29
Quality assessment
The nonstandardized tool created by Drew et al.18 was used to assess six studies and had a mean percentage score of 65.3% (14/22), ranging from 45.5 to 90.9% (10–20/22). Four studies were evaluated with the ROBINS-1 tool: two studies were found to be at moderate risk of bias, and two were at low risk of bias. Finally, there were 10 LCA papers that were assessed using the LCA criteria by Drew et al.18: the mean quality assessment percentage score was 90.9% (32/35), with scores ranging from 65.7 to 100% (23–35/35). The full table of results can be found in Appendix 2, Supplemental Digital Content 2, http://links.lww.com/JS9/A326.
Discussion
This systematic review has demonstrated that a variety of interventions implemented to improve sustainability have already been evaluated. These interventions can be divided across all stages of the operative pathway (Fig. 2): reducing and rationalizing materials; the use of reusable equipment and textiles; recycling and correcting waste segregation; anesthetic alternatives; and other interventions. However, the volume and quality of evidence for these interventions are variable. More than half of the literature included in this review centered around the use of reusable equipment with limited evidence for other interventions.
Figure 2.
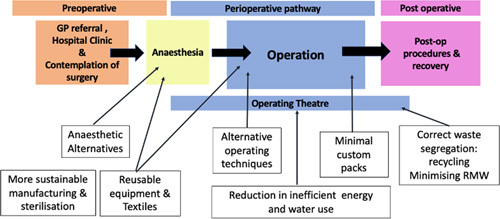
A schematic diagram illustrating how interventions can be implemented in the operative pathway.
Importantly, this study not only gives support to hospitals that may choose to implement reusable equipment strategies, but it does so alongside a careful presentation of the associated financial benefits, which are a core driver of healthcare management and procurement strategies. In addition, this review also highlights the need for more evidence to be generated in lesser studied areas such as energy reduction strategies or waste segregation.
While the majority of included studies found reusable equipment to be environmentally superior to single-use alternatives, it is important to highlight that not all studies found reusable devices to be more sustainable in their particular institutions. For example, a hospital’s electricity source, which is dependent on a hospital’s geographic location and national governance, has a significant impact on the CO2 emissions produced in sterilization processes and ultimately determines whether reusable equipment is more environmentally sustainable than their single-use equivalents29,32. Firstly, this demonstrates the complexity of implementing sustainable changes to surgical practice, as contextual factors will impact their effectiveness. Secondly, this also highlights the need to critically assess the evidence in a constantly evolving environment where interventions are being implemented at pace and may be presumed to be environmentally beneficial.
Moreover, sustainability is only one of the multiple factors when a surgical team elects to use a particular surgical technique or regional anesthesia. This must be balanced with other factors, including the underlying pathology, patient factors and outcomes, surgeon experience with the technique, cost-effectiveness, availability of resources, and hospital and institutional factors38. Our review found limited evidence concerning cost outcomes surrounding sustainable interventions. While those studies that did investigate cost outcomes found that sustainable interventions offered long-term financial benefits when implemented20,22–24,27,28,33,34,40, real-world implementation of these interventions will require higher quality evidence surrounding the initial and longer term financial costs of sustainable alternatives. Only when sustainability can be balanced with cost-effectiveness and other key factors within the surgical decision-making framework can sustainable interventions be effectively scaled.
Despite evidence for successful sustainable interventions existing for over a decade, there has not been widespread implementation within surgical departments13,20,23. Research must move away from looking at the effectiveness of sustainable interventions in isolation and how they can be implemented in real-world clinical practice. Interventions must be not only theoretically effective but also acceptable to all stakeholders, including surgical teams and patients. It is important to understand the perspectives and priorities of these stakeholders with regard to sustainable surgery. Not only will interventions be more appropriate as a result of this, but the results will likely be more effective and long-lasting if stakeholders recognize and are supportive of the value of the change39. Finally, future research must evaluate the long-term impact of sustainable interventions. Most of the studies included in our systematic review were cross-sectional rather than longitudinal. While this data may provide initial evidence, only future longitudinal studies will provide an accurate representation of the effectiveness of an intervention.
Although this study systematically reviewed the available evidence, it was limited by the quality of the included studies. Risk of bias tools were used to ensure that the included studies were of adequate quality. However, most studies were observational cross-sectional studies utilizing retrospective data. This highlights the need for future longitudinal studies to be conducted, particularly as the sources of energy rapidly change among nations. Finally, despite the use of a robust search strategy, it is likely that not all available evidence was included in this review due to the dynamic nature of this field.
Conclusions
The evidence base for sustainable interventions in surgery is variable. The majority of included studies were cross-sectional in nature, with limited longitudinal data available. Significant emphasis is given to reusable equipment and textiles with a lesser focus on other areas. Future research should focus on understanding how sustainability may fit into the surgical decision-making process and the perspectives of real-world users for these interventions to be successfully scaled.
Ethical approval
Not required.
Sources of funding
This systematic review was unfunded; however, infrastructure support was provided by the NIHR Imperial Biomedical Research Centre. K.L. is supported by an NIHR Academic Clinical Fellowship.
Author contribution
K.L., A.A., and S.P.: conceived and designed the study; K.L., N.G., and A.A.: independently screened and reviewed all included articles; K.L., N.G., and A.A.: drafted the manuscript; J.W.B., A.D., and S.P.: contributed to significant amendments to the final manuscript.
Conflicts of interest disclosure
The authors have no conflicts of interest to declare.
Research registration unique identifying number (UIN)
Name of the registry: PROSPERO database.
Unique identifying number or registration ID: CRD 42022308035.
Hyperlink to your specific registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=308035
Data availability statement
All datasets arising from this study are available upon reasonable request to the corresponding author. The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Requests for reprints
Requests should be made to the corresponding author.
Guarantor
Kyle Lam, Clinical Research Fellow, Department of Surgery and Cancer, Imperial College London. E-mail: k.lam@imperial.ac.uk
Study design
Systematic review.
Supplementary Material
Acknowledgments
The authors would like to thank Chloe Turner, Library and Evidence Support Information Specialist, BMA Library, for conducting the literature searches.
Footnotes
K.L., N.G., and S.P. contributed equally and should be considered equal authorship.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.journal-surgery.net.
Published online 13 April 2023
Contributor Information
Kyle Lam, Email: k.lam@imperial.ac.uk.
Nishita Gadi, Email: nishita.gadi1@gmail.com.
Amish Acharya, Email: amish.acharya07@imperial.ac.uk.
Jasmine Winter Beatty, Email: j.winter-beatty@imperial.ac.uk.
Ara Darzi, Email: a.darzi@imperial.ac.uk.
Sanjay Purkayastha, Email: s.purkayastha@imperial.ac.uk.
References
- 1. Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change. Lancet 2009;373:1693–1733. [DOI] [PubMed] [Google Scholar]
- 2. Rocque RJ, Beaudoin C, Ndjaboue R, et al. Health effects of climate change: an overview of systematic reviews. BMJ Open 2021;11:e046333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Watts N, Adger WN, Ayeb-Karlsson S, et al. The Lancet Countdown: tracking progress on health and climate change. Lancet 2017;389:1151–1164. [DOI] [PubMed] [Google Scholar]
- 4. Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg 2011;146:131–136. [DOI] [PubMed] [Google Scholar]
- 5. Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care system and effects on public health. PLoS One 2016;11:e0157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol 2015;49:1779–1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health 2017;1:e381–e388. [DOI] [PubMed] [Google Scholar]
- 8. Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Surgery 2015;158:3–6. [DOI] [PubMed] [Google Scholar]
- 9. Carr A, Smith JA, Camaradou J, et al. Growing backlog of planned surgery due to covid-19. BMJ 2021:n339. [DOI] [PubMed] [Google Scholar]
- 10. National Health Service. NHS becomes the world’s first national health system to commit to become ‘carbon net zero’, backed by clear deliverables and milestones. NHS England, 2020.
- 11. Kaiser Permanente. The first carbon neutral healthcare system in the US. Accessed 12 July 2022. https://about.kaiserpermanente.org/community-health/news/first-carbon-neutral-health-system-in-us
- 12. Szawlowski S, Choong PFM, Li J, et al. How do surgeons’ trade-off between patient outcomes and risk of complications in total knee arthroplasty? a discrete choice experiment in Australia. BMJ Open 2019;9:e029406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris H, Bhutta MF, Rizan C. A survey of UK and Irish surgeons’ attitudes, behaviours and barriers to change for environmental sustainability. Ann R Coll Surg Engl 2021;103:725–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McGain F, Muret J, Lawson C, et al. Environmental sustainability in anaesthesia and critical care. Br J Anaesth 2020;125:680–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Royal College of Surgeons of England. Sustainability in the operating theatre. Accessed 12 July 2022. https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/sustainability-in-operating-theatre/
- 17. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Drew J, Christie SD, Tyedmers P, et al. Operating in a climate crisis: a state-of-the-science review of life cycle assessment within surgical and anesthetic care. Environ Health Perspect 2021;129:76001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rizan C, Steinbach I, Nicholson R, et al. The carbon footprint of surgical operations. Ann Surg 2020;272:986–995. [DOI] [PubMed] [Google Scholar]
- 20. Wormer BA, Augenstein VA, Carpenter CL, et al. The green operating room: simple changes to reduce cost and our carbon footprint. Am Surg 2013;79:666–671. [PubMed] [Google Scholar]
- 21. Thiel CL, Fiorin Carvalho R, Hess L, et al. Minimal custom pack design and wide-awake hand surgery: reducing waste and spending in the orthopedic operating room. Hand (NY) 2019;14:271–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rizan C, Lillywhite R, Reed M, et al. Minimising carbon and financial costs of steam sterilisation and packaging of reusable surgical instruments. Br J Surg 2022;109:200–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Eckelman M, Mosher M, Gonzalez A, et al. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth Analg 2012;114:1067–1072. [DOI] [PubMed] [Google Scholar]
- 24. Sherman JD, Raibley LA, Eckelman MJ. Life cycle assessment and costing methods for device procurement. Anesth Analg 2018;127:434–443. [DOI] [PubMed] [Google Scholar]
- 25. Vozzola E, Overcash M, Griffing E. An environmental analysis of reusable and disposable surgical gowns. AORN J 2020;111:315–325. [DOI] [PubMed] [Google Scholar]
- 26. Astroza G, Morales C, Saez G. As little as possible. A new paradigm in endourology. Eur Urol Open Sci 2020;19:e1846. [Google Scholar]
- 27. Jabouri H, Abbott RA. Sustainability in skin cancer surgery. Br J Dermatol 2022;186:735–736. [DOI] [PubMed] [Google Scholar]
- 28. Rizan C, Bhutta MF. Environmental impact and life cycle financial cost of hybrid (reusable/single-use) instruments versus single-use equivalents in laparoscopic cholecystectomy. Surg Endosc 2022;36:4067–4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. McGain F, McAlister S, McGavin A, et al. A life cycle assessment of reusable and single-use central venous catheter insertion kits. Anesth Analg 2012;114:1073–1080. [DOI] [PubMed] [Google Scholar]
- 30. Leiden A, Cerdas F, Noriega D, et al. Life cycle assessment of a disposable and a reusable surgery instrument set for spinal fusion surgeries. Resour Conserv Recycl 2020;156:104704. [Google Scholar]
- 31. Davis NF, McGrath S, Quinlan M, et al. Carbon footprint in flexible ureteroscopy: a comparative study on the environmental impact of reusable and single-use ureteroscopes. J Endourol 2018;32:214–217. [DOI] [PubMed] [Google Scholar]
- 32. McGain F, Story D, Lim T, et al. Financial and environmental costs of reusable and single-use anaesthetic equipment. Br J Anaesth 2017;118:862–869. [DOI] [PubMed] [Google Scholar]
- 33. Debois W, Prata J, Elmer B, et al. Improved environmental impact with diversion of perfusion bypass circuit to municipal solid waste. J Extra Corpor Technol 2013;45:143–145. [PMC free article] [PubMed] [Google Scholar]
- 34. Griffin L, Brennan F, Fennell-Wells A. Life cycle assessment of a disposable and a reusable surgery instrument set for spinal fusion surgeries. Anaesthesia 2022;77:8–63.35001379 [Google Scholar]
- 35. McGain F, Sheridan N, Wickramarachchi K, et al. Carbon footprint of general, regional, and combined anesthesia for total knee replacements. Anesthesiology 2021;135:976–991. [DOI] [PubMed] [Google Scholar]
- 36. Moussa G, Andreatta W, Ch’ng SW, et al. Environmental effect of air versus gas tamponade in the management of rhegmatogenous retinal detachment VR surgery: a multicentre study of 3,239 patients. PLoS One 2022;17:e0263009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Unger SR, Hottle TA, Hobbs SR, et al. Do single-use medical devices containing biopolymers reduce the environmental impacts of surgical procedures compared with their plastic equivalents. J Health Serv Res Policy 2017;22:218–225. [DOI] [PubMed] [Google Scholar]
- 38. Gunaratnam C, Bernstein M. Factors affecting surgical decision-making – a qualitative study. Rambam Maimonides Med J 2018;9:e0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nilsen P, Seing I, Ericsson C, et al. Characteristics of successful changes in health care organizations: an interview study with physicians, registered nurses and assistant nurses. BMC Health Serv Res 2020;20:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Thiel CL, Woods NC, Bilec MM. Strategies to reduce greenhouse gas emissions from laparoscopic surgery. Am J Public Health 2018;108:S158–S164. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All datasets arising from this study are available upon reasonable request to the corresponding author. The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.


