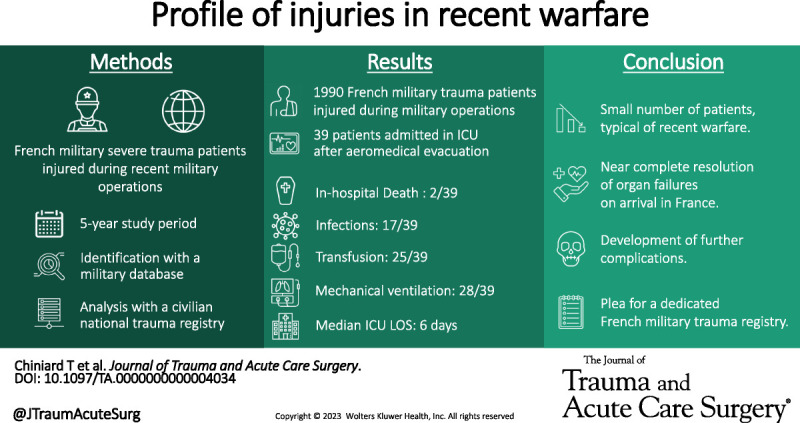
A small number of military severe trauma patients injured during recent military operations presented with near complete resolution of almost all initial organ failures upon arrival at the national territory hospital but developed further complications during their hospital stay.
KEY WORDS: Trauma, military, war, intensive care unit, recent conflicts
BACKGROUND
The epidemiology of French military severe trauma patients injured during recent military operations remains poorly described, even if French operations, casualties sustained, and care rendered in a different trauma system are distinct from others. This study aimed at describing the characteristics of these patients upon arrival at hospital in France and during hospital stay.
METHODS
This 5-year retrospective cohort study included all French military servicemen injured during military operations and admitted to the intensive care unit. Data on the characteristics upon arrival at the Percy hospital in France and during hospital stay were obtained from a national civilian trauma registry.
RESULTS
Of 1,990 military trauma patients injured in military operations, 39 were finally admitted to the intensive care unit of the Percy hospital and included in the analysis. Traumas were related to battle injuries and nonbattle injuries in 27 and 12 patients, respectively. Ninety-eight wounds were described: torso (n = 32), limbs (n = 32), head and neck (n = 25), and spine (n = 9). The mechanism of injury was explosion in 19 patients, gunshot wound in 8 patients, motor vehicular crash in 7 patients, or other mechanisms in 5 patients. The median Injury Severity Score was 25.5 (interquartile range, 14–34).
CONCLUSION
This study highlights the small number of military severe trauma patients injured in recent warfare and their characteristics. The use of dedicated systemic military trauma registries could improve the specific epidemiological knowledge on recent warfare and help better prepare for future conflicts that may include major engagements and large-scale combat operations.
LEVEL OF EVIDENCE
Prognostic and Epidemiological; Level V.
In France, medical support in military operations is based on three principles: forward resuscitation, forward surgery, and early strategic aeromedical evacuation to the national territory1 within 24 to 48 hours.2,3 Gaining a better understanding of the epidemiology is essential in improving the management of military severe trauma patients injured during military operations.4–6 To this regard, epidemiological surveillance data are crucial in clarifying the extent of the problem.7 Trauma registries such as the US Department of Defense Trauma Registry and the UK Joint Theater Trauma Registry have provided better characterization of injuries, including their severity and mechanisms.8–11 Some few and scattered French data were collected for some periods of past (e.g., Afghanistan) and recent conflicts (e.g., Mali).12–21 However, to date, the French armed forces do not have such unique, systematic, and exhaustive military trauma registry.4,21 Recent military operations have specific characteristics different from those of past conflicts (e.g., Iraq and Afghanistan), particularly in terms of terrain configuration, combat techniques, medical support, and combat intensity.22–26 Moreover, recent military operations did not largely involve the US and UK armed forces, particularly those in the Sahel-Saharan strip.27 Thus, the US Department of Defense Trauma Registry and UK Joint Theater Trauma Registry could not be used. This lack of data collection from a comprehensive military trauma registry, combined with a low combat intensity, did not allow for a complete description of the characteristics of military severe trauma patients injured during recent military operations. However, the Percy hospital (a Role 4 military teaching hospital located in metropolitan France near Paris, main destination of military severe trauma patients after strategic aeromedical evacuation) became member of a civilian national trauma registry in January 2015. This systematic and comprehensive civilian national trauma registry collects prehospital and hospital data from trauma patients admitted to a partner trauma center. Inclusion in the civilian national trauma registry is achieved when admission to the trauma center occurs no later than 48 hours after the trauma. As a member of the civilian national trauma registry, the Percy hospital receives civilian severe trauma patients injured in France and military severe trauma patients injured during military operations. The present study aimed to describe the characteristics of military severe trauma patients injured during recent military operations upon their arrival at the Percy hospital, and during hospital stay.
PATIENTS AND METHODS
This single-center retrospective study investigated all military severe trauma patients injured during military operations and admitted to the intensive care unit (ICU) of the Percy hospital, from September 1, 2016, to December 31, 2021. The STrengthening the Reporting of OBservational studies in Epidemiology guideline for reporting cohort studies was used to ensure proper reporting of methods, results, and discussion (Supplemental Digital Content, Supplementary Data 1, http://links.lww.com/TA/D21). The inclusion criteria were French military service membership, severe trauma acquired during military operations, and admission to an ICU. Military operations included prepositioned forces dedicated to the defense of national interests and operational support, and overseas operations dedicated to war operations. To identify military severe trauma patients injured during military operations, we queried the National Patient Evacuation Coordination Center (N-PECC) database, a military administrative database that collects all strategic aeromedical evacuations performed for on-duty military personnel worldwide. Thus, all military personnel who required a strategic aeromedical evacuation to France over the study period, with “trauma” as the cause of evacuation and “ICU of Percy hospital” as the requested destination, were identified.2 The data collected included the demographic characteristics, country of origin, date of strategic aeromedical evacuation, and requested destination in France. We then searched for the corresponding cases in the civilian national trauma registry. The data collected therein included patient characteristics, trauma characteristics, prehospital and hospital care, and outcomes, including death, infections, and respiratory and neurological outcomes. In this study, the prehospital phase included all events occurring before arrival at the Percy hospital, while the hospital phase included all events occurring from arrival at the Percy hospital. A substantial hemorrhage was defined as a blood loss requiring transfusion of 4 U or more of packed red blood cell (pRBC) or whole blood between the point of injury and arrival at the Percy hospital. A severe hemorrhage after arrival was defined as the need for transfusion of more than four pRBC units in the first 6 hours after arrival at the Percy hospital.28 Trauma-associated coagulopathy (TAC) was defined as a prothrombin time of <70% or a platelet count of <100 109/L,29 derived from laboratory tests on arrival at the Percy hospital. Quick time (in seconds) is obtained from prothrombin time (in percentage) by a linear transformation with coefficients specific to the device used. Quick ratio is the ratio between measured Quick time in the patient over a mean normal Quick time. International normalized ratio (INR) is obtained by applying to the Quick ratio a correction factor specific to the device and the batch of reagents used, called the International Sensitivity Index (ISI).30 Hence, taking into account the calibration coefficients of the device used and the mean ISI value recorded, a prothrombin time measured at 70% at Percy hospital is equivalent to an INR of 1.3. The computerized medical records of the Percy hospital were consulted to complete the missing data and to identify the missing cases. The civilian national trauma registry received approval from the Advisory Committee for Information Processing in Health Research and the National Commission for Information Technology and Civil Liberties (CNIL authorization 911.461). This study was approved by the Ethics Committee for Research in Anesthesia and Intensive Care of our institution (institutional review board number, 00010254-2022-018).
The primary outcomes included the anatomic distribution of wounds, type of trauma, mechanism of injury, and Injury Severity Score (ISS). The secondary outcomes included ICU length of stay, ICU-free days on day 28, hospital length of stay for survivors, mortality rate, total number of blood products transfused during ICU stay, and neurological, respiratory, and infectious events during ICU stay.
Descriptive statistics and statistical associations were evaluated using Epi-info version 7.2 (Center for Disease Control and Prevention, Atlanta, GA). Quantitative variables were described as means and SDs in case of normal distribution or as medians and 25% to 75% interquartile ranges (IQRs) in case of nonnormal distribution, and qualitative variables as frequencies and percentages. Wilson 95% confidence intervals (CIs) were used when an interval estimation of a proportion was indicated. Tests of statistical association were performed in a two-sided situation. For quantitative variables, Student's t test or nonparametric tests (in case of nonhomogeneous variances in Bartlett's test, Kruskal-Wallis test, or Mann-Whitney test) were used. For categorical variables, the χ2 test or Fisher's exact test (when the number of participants was insufficient) was used. A result was considered significant when the p value was <0.05.
RESULTS
Between September 1, 2016, and December 31, 2021, the N-PECC database recorded 1,990 military trauma patients injured during military operations who required a strategic aeromedical evacuation to France and hospitalization to a military hospital. Among them, the theoretical requested destination was an ICU in 61 patients, and the ICU admission rate was 3.07% (95% CI, 2.39–3.92%). The theoretical requested destination was the ICU of the Percy hospital in 55 patients. The data of interest were obtained directly from the civilian national trauma registry for 19 of 55 cases and completed from the computerized medical records of the Percy hospital for 36 of 55 cases. After screening for inclusion, 16 cases were excluded, and 39 cases were actually admitted to the ICU and finally included in the analysis. The ICU admission rate at the Percy hospital was 2% (95% CI, 1.4–2.7%) (Fig. 1). Table 1 summarizes the characteristics of the 39 patients included in the analysis. Twenty-seven patients (69%) had battle injuries (BIs), while 12 (31%) had nonbattle injuries (NBIs). The NBIs that occurred in prepositioned forces were motor vehicular crashes in six patients and helicopter crash in one patient. There were no differences between the BIs and NBIs, except for the location of the point of injury and the mechanism of injury. Ninety-eight wounds were described, with a median number of 2 (IQR, 2–3) wounds per casualty. Head injuries were significantly associated with more facial injuries (70% vs. 28%, p = 0.03) and fewer lower limb injuries (10% vs. 62%, p = 0.008). Penetrating trauma occurred in 24 patients (62%) and was more common in wounds involving the lower limbs (89% vs. 35%, p < 0.001). Closed trauma occurred in 13 patients (38%) and was more common in wounds involving the head or spine (80% vs. 24%, p = 0.003 and 78% vs. 27%, p = 0.02, respectively). Between the point of injury and arrival at the Percy hospital, 21 of 37 military severe trauma patients injured during military operations received measures to control bleeding (14 of 27, tourniquet; 8 of 23, pressure bandage; 7 of 39, pelvic belt; and 7 of 23, others or not specified), 24 of 39 received transfusion of blood products (including a substantial hemorrhage in 16 patients), and 32 of 39 underwent surgery.
Figure 1.

Flowchart. *Six cases were hospitalized at Bégin military teaching hospital, Saint-Mandé, France. **When idenfication in the national civilian trauma registry was not possible, data were collected from the Percy hospital computerized medical records. †The sum does not equal the total because of one case arrived beyond 48 hours and was also redirected outside of the ICU.
TABLE 1.
Characteristics of the Study Population (n = 39)
| Patient Characteristics | All Patients (n = 39) | BIs (n = 27) | NBIs (n = 12) | p |
|---|---|---|---|---|
| Personal characteristics | ||||
| Age, median (IQR), y | 30 (25–33) | 30 (25–33) | 29 (26–33) | 0.58 |
| Male sex, n (%) | 39 (100) | 27 (100) | 12 (100) | >0.99 |
| Body mass index, median (IQR), kg/m2 | 26.7 (24.1–29.6) | 26.4 (24.1–29.7) | 27.3 (23.7–28.3) | 0.89 |
| ASA status, n (%) | 0.42 | |||
| ASA 1 | 30 (77) | 22 (81) | 8 (67) | |
| ASA 2 | 9 (23) | 5 (19) | 4 (33) | |
| Military characteristics | ||||
| Rank category, n (%) | 0.33 | |||
| Officers | 4 (10) | 2 (7) | 2 (17) | |
| Noncommissioned officers | 9 (23) | 5 (19) | 4 (33) | |
| Enlisted men | 26 (67) | 20 (74) | 6 (50) | |
| Armed forces branch of affiliation, n (%) | 0.22 | |||
| French Army | 29 (74) | 18 (67) | 11 (92) | |
| French Air Force | 3 (8) | 3 (11) | 0 (−) | |
| French Navy | 2 (5) | 2 (7) | 0 (−) | |
| Other branch* | 5 (13) | 4 (15) | 1 (8) | |
| Special operations forces, n (%) | 8 (21) | 6 (22) | 2 (17) | >0.99 |
| Trauma characteristics | ||||
| Location of the point of injury, n (%) | <0.001 | |||
| Overseas operations** | 32 (82) | 27 (100) | 5 (42) | |
| Prepositioned forces† | 7 (18) | 0 (−) | 7 (58) | |
| ISS, median (IQR) | 26 (14–34) | 24 (13–29) | 29 (21–35) | 0.44 |
| Wound distribution, n (%)‡ | ||||
| Head | 10 (26) | 4 (15) | 6 (50) | 0.04 |
| Face | 15 (38) | 9 (33) | 6 (50) | 0.48 |
| Spine | 9 (23) | 7 (26) | 2 (17) | 0.69 |
| Thorax | 15 (38) | 10 (37) | 5 (42) | >0.99 |
| Abdomen | 11 (28) | 7 (26) | 4 (33) | 0.71 |
| Pelvis | 6 (15) | 3 (11) | 3 (25) | 0.35 |
| Upper limb | 13 (33) | 11 (41) | 2 (17) | 0.27 |
| Lower limb | 19 (58) | 17 (63) | 2 (17) | 0.02 |
| Mechanism of injury, n (%) | <0.001 | |||
| Explosion | 19 (49) | 18 (67) | 1 (8) | |
| Gunshot wound | 8 (20) | 7 (26) | 1 (8) | |
| Motor vehicular crash | 7 (18) | 0 (−) | 7 (59) | |
| Other | 5 (13) | 2 (7) | 3 (25) | |
| Evacuation time to Percy hospital, median (IQR), h | 25 (21–27) | 24 (21–29) | 27 (22–27) | 0.49 |
*Other armed forces branches: French Military Medical Service (n = 2), French Military Fuels Service (n = 2), and not specified (n = 1).
**Overseas operations: Sahel-Saharan strip (n = 30) and Middle East (n = 2).
†Prepositioned forces: Djibouti (n = 4), Ivory Coast (n = 1), Senegal (n = 1), and not specified (n = 1).
‡Total greater than 100% because of wound associations.
ASA, American Society of Anesthesiology.
Table 2 summarizes the clinical and biological characteristics of the patients upon arrival at the Percy hospital. The median dose of vasopressors was 1.4 mg/h (IQR, 0.4–3 mg/h). There was no association found between any injury and the administration of vasopressors. Mechanical ventilation upon arrival was more frequent in the patients with wounds involving the abdomen (100% vs. 61%, p = 0.02). The biological criteria for TAC were present in 27 patients (69%), including 26 of 27 with a prothrombin time of <70% and 9 of 27 with a platelet count of <100 × 109/L (8 of 27 had both criteria). In patients presenting with TAC, platelet count was 129 ×109/L (IQR, 86–149 ×109/L), and prothrombin time was 56% (IQR, 52–66%). In patients presenting without TAC, platelet count was 185 ×109/L (IQR, 117–221 × 109/L), and prothrombin time was 78% (IQR, 73–90%). Trauma-associated coagulopathy was more frequent in the patients with wounds involving the lower limbs (89% vs. 50%, p = 0.01), those who sustained a substantial hemorrhage (100% vs. 48%, p < 0.001), and those who underwent surgery during military operations (81% vs. 14%, p = 0.002). Anemia (hemoglobin level <13 g/dL) was present in 33 patients (85%). The shock index (ratio of the heart rate to the systolic blood pressure) was >0.9 in 8 patients (21%). In comparison with all patients, it was higher in the patients who sustained a substantial hemorrhage (0.87 [IQR, 0.72–1.06] vs. 0.68 [IQR, 0.54–0.77], p = 0.02) and those who underwent surgery in the theater of military operations (0.75 [IQR, 0.66–0.94] vs. 0.56 [IQR, 0.46–0.71], p = 0.03). Patients with a shock index >0.9 sustained BIs in five of eight cases and NBIs in three of eight cases. These patients presented 25 wounds with a median number of 3 (IQR, 2–4) wounds per casualty, involving the head in two of eight cases, the face in five of eight cases, the spine in two of eight cases, the thorax in two of eight cases, the abdomen in four of eight cases, the pelvis in one of eight cases, the upper limb in four of eight cases, and the lower limb in five of eight cases. Injury Severity Score in these patients was 31 (IQR, 25–42). These patients received measures to control bleeding in seven of eight cases (five of seven, tourniquet; three of five, pressure bandage; two of eight, pelvic belt; and two of five, others or not specified), seven of eight received transfusion of blood products (including a massive transfusion substantial hemorrhage in six patients), and eight of eight underwent surgery during military operations. Two military severe trauma patients injured during military operations died from their wounds after their arrival at the Percy hospital. The causes of death were a brain death in a traumatic brain injury (TBI) after 9 days of hospitalization in one patient and sepsis with multiple organ failure after 8 days of hospitalization in the other patient. Both patients had sustained a substantial hemorrhage and had undergone surgery during military operations.
TABLE 2.
Clinical and Biological Characteristics Upon Arrival at Percy Hospital
| Patient Characteristics | Missing Data (Number) | Available Data (Number) | Observed Data |
|---|---|---|---|
| Clinical characteristics | |||
| Systolic blood pressure, median (IQR), mm Hg | 0 | 39 | 121 (110–136) |
| Mean blood pressure, median (IQR), mm Hg | 0 | 39 | 87 (79–95) |
| Diastolic blood pressure, median (IQR), mm Hg | 0 | 39 | 68 (60–80) |
| Heart rate, median (IQR), beats/min | 0 | 39 | 93 (79–106) |
| Oxygen pulsed saturation, median (IQR), % | 4 | 35 | 100 (99–100) |
| Temperature, median (IQR), °C | 1 | 38 | 37.7 (37–38.4) |
| Shock Index, median (IQR) | 0 | 39 | 0.73 (0.63–0.88) |
| Mechanical ventilation, n (%) | 0 | 39 | 27 (69%) |
| Vasopressor treatment, n (%) | 0 | 39 | 16 (41%) |
| Biological characteristics | |||
| Arterial blood gas analysis | |||
| pH, median (IQR) | 5 | 34 | 7.41 (7.38–7.43) |
| pCO2, median (IQR), mm Hg | 5 | 34 | 38 (36–41) |
| Base excess, median (IQR), mEq/L | 5 | 34 | 0.06 (−0.79 to 0.90) |
| pO2, median (IQR), mm Hg | 5 | 34 | 247 (154–441) |
| pO2/FIO2, median (IQR) | 5 | 34 | 432 (348–967) |
| Lactate, median (IQR), mmol/L | 5 | 34 | 1.1 (0.8–1.9) |
| Standard biological tests | |||
| Hemoglobin, median (IQR), g/dL | 0 | 39 | 11.2 (10.0–12.1) |
| Platelet count, median (IQR), 109/L | 0 | 39 | 136 (112–185) |
| Prothrombin time, median (IQR), % | 0 | 39 | 65 (54–74) |
| Fibrinogen, median (IQR), g/L | 0 | 39 | 3.5 (3.0–4.2) |
| Creatinine, median (IQR), mmol/L | 1 | 38 | 93 (78–124) |
| Bicarbonate, median (IQR), mmol/L | 7 | 32 | 25.0 (23.3–25.5) |
| Severity scores | |||
| SAPS II, median (IQR) | 0 | 39 | 29 (18–39) |
| SOFA, median (IQR) | 0 | 39 | 5 (2–8) |
SAPS II, Simplified Acute Physiology Score II; SOFA, Sepsis-related Organ Failure Assessment.
Table 3 summarizes the outcomes of the patients included in the analysis. Table 4 presents the associations between the characteristics of the included patients before and upon arrival at the Percy hospital and outcomes. Severe hemorrhage was retrospectively diagnosed in six patients, with five patients having limb trauma and two patients having torso trauma. All these patients underwent initial critical care (including transfusion therapy and initial surgery in the theater of military operations), resulting in a clinical presentation without organ failure on arrival at Percy hospital, more than 24 hours after the trauma. The median time from admission to surgery was 2 hours 47 minutes (IQR, 2 hours 20 minutes to 3 hours 35 minutes) for these six patients. Of the 10 patients with TBI included in the analysis, only 1 had a Glasgow Coma Scale score of ≤13 at ICU discharge.
TABLE 3.
In-hospital Outcomes
| Missing Data (Number) | Available Data (Number) | Observed Data | |
|---|---|---|---|
| In-hospital death | 0 | 39 | 2 (5%) |
| Lengths of stay | |||
| ICU length of stay, median (IQR), d | 0 | 39 | 6 (4–16) |
| Free days of ICU at day 28, median (IQR), d | 0 | 39 | 22 (9–24) |
| Hospital length of stay in survivors, median (IQR), d | 1 | 36 | 39 (14–91) |
| Transfusion during the stay in ICU | |||
| Transfusion of ≥1 blood product, n (%) | 0 | 39 | 25 (64%) |
| Total no. pRBC per patient, median (IQR) | 0 | 39 | 2 (0–7) |
| Total no. plasma units per patient, median (IQR) | 0 | 39 | 0 (0–6) |
| Total no. platelets units per patient, median (IQR) | 0 | 39 | 0 (0–1) |
| Infectious events during the stay in ICU | |||
| Occurrence of ≥1 infection, n (%) | 0 | 39 | 17 (44%) |
| Respiratory infection, n (%) | 0 | 39 | 11 (28%) |
| Urinary tract infection, n (%) | 0 | 39 | 1 (3%) |
| Abdomen infection, n (%) | 0 | 39 | 0 (−) |
| Cerebral infection, n (%) | 0 | 39 | 0 (−) |
| Surgical site infection, n (%) | 0 | 39 | 8 (21%) |
| Material infection, n (%) | 0 | 39 | 0 (−) |
| Occurrence of ≥1 septic shock, n (%) | 0 | 39 | 4 (10%) |
| Acquisition of MDR bacteria, n (%) | 1 | 38 | 13 (34%) |
| Respiratory events during the stay in ICU | |||
| Mechanical ventilation for ≥1 day, n (%) | 0 | 39 | 28 (72%) |
| Mechanical ventilation length, median (IQR), d | 0 | 39 | 2 (0–8) |
| Free days of mechanical ventilation at day 28, median (IQR), d | 0 | 39 | 26 (20–28) |
| Tracheostomy, n (%) | 0 | 39 | 2 (5%) |
| Acute respiratory distress syndrome, n (%) | 0 | 39 | 2 (5%) |
| Neurological events during the stay in ICU in TBI patients (n = 10) | |||
| Intracranial hypertension, n (%) | 2 | 8 | 3 (38%) |
| Glasgow Coma Scale at discharge, median (IQR) | 3 | 7 | 15 (14–15) |
MDR, multidrug resistant.
TABLE 4.
Associations Between the Characteristics Before and Upon Arrival at Percy Hospital, and In-hospital Outcomes
| ICU Length of Stay, Median (IQR), d | p | Hospital Length of Stay, Median (IQR), d | p | No. pRBC per Patient, Median (IQR) |
p | No. Plasma Units per Patient, Median (IQR) | p | No. Platelets Units per Patient, Median (IQR) | p | Mechanical Ventilation Length, Median (IQR), d | p | Respiratory Infection, n (%) | p | Surgical Site Infection, n (%) | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wound involving the abdomen | 0.03 | 0.12 | 0.003 | <0.001 | 0.15 | 0.20 | 0.69 | 0.003 | ||||||||
| Yes | 16 (6–26) | 81 (40–106) | 6 (4–14) | 6 (4–11) | 0 (0–2) | 5 (2–12) | 4 (36) | 6 (55) | ||||||||
| No | 5 (3–10) | 28 (12–91) | 1 (0–3) | 0 (0–0) | 0 (0–0) | 1 (0–6) | 7 (25) | 2 (7) | ||||||||
| Wound involving the pelvis | 0.10 | 0.02 | 0.97 | 0.24 | 0.07 | 0.01 | 0.04 | 0.58 | ||||||||
| Yes | 16 (11–19) | 97 (84–106) | 7 (1–10) | 5 (0–8) | 1 (0–2) | 10 (7–15) | 4 (67) | 2 (33) | ||||||||
| No | 5 (4–10) | 28 (13–83) | 2 (0–6) | 0 (0–4) | 0 (0–0) | 2 (0–5) | 7 (21) | 6 (18) | ||||||||
| ISS | 0.002 | 0.54 | 0.11 | 0.36 | 0.56 | 0.04 | 0.08 | >0.99 | ||||||||
| >15 | 8 (4–20) | 40 (18–91) | 2 (0–6) | 0 (0–5) | 0 (0–1) | 2 (1–10) | 10 (36) | 6 (21) | ||||||||
| ≤15 | 3 (2–4) | 18 (12–75) | 0 (0–3) | 0 (0–2) | 0 (0–0) | 0 (0–2) | 0 (−) | 1 (13) | ||||||||
| Substantial hemorrhage* | 0.001 | <0.001 | <0.001 | <0.001 | 0.001 | 0.04 | 0.31 | 0.04 | ||||||||
| Yes | 10 (7–25) | 94 (38–122) | 8 (4–20) | 7 (1–12) | 1 (0–2) | 6 (3–10) | 6 (38) | 6 (38) | ||||||||
| No | 4 (3–7) | 18 (11–49) | 0 (0–2) | 0 (0–0) | 0 (0–0) | 1 (0–2) | 5 (22) | 2 (9) | ||||||||
| Surgery during military operations | 0.03 | 0.053 | 0.004 | 0.02 | 0.08 | 0.002 | 0.65 | — | ||||||||
| Yes | 8 (4–18) | 49 (18–97) | 3 (0–9) | 0.5 (0–8) | 0 (0–1) | 4 (1–8) | 10 (31) | 8 (25) | ||||||||
| No | 3 (3–5) | 14 (7–41) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 1 (14) | 0 (−) | ||||||||
| Shock index | <0.001 | 0.07 | 0.01 | 0.02 | 0.04 | 0.004 | 0.66 | 0.04 | ||||||||
| >0.9 | 21 (12–28) | 99 (38–122) | 18 (2–37) | 11 (0–26) | 1 (0–4) | 8 (6–13) | 3 (38) | 4 (50) | ||||||||
| ≤0.9 | 5 (3–10) | 32 (13–84) | 2 (0–4) | 0 (0–3) | 0 (0–0) | 1 (0–4) | 8 (26) | 4 (13) | ||||||||
| Mechanical ventilation on arrival at hospital | 0.001 | 0.06 | 0.001 | 0.002 | <0.001 | <0.001 | — | — | ||||||||
| Yes | 9.5 (4–20) | 55 (18–102) | 4 (1–10) | 2 (0–8) | 0 (0–2) | 4 (2–10) | 11 (39) | 8 (29) | ||||||||
| No | 3 (2–5) | 22 (10–49) | 0 (0–1) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (−) | 0 (−) | ||||||||
| Vasopressors on arrival at hospital | 0.02 | 0.17 | 0.07 | 0.12 | 0.006 | 0.04 | 0.15 | 0.24 | ||||||||
| Yes | 10 (4–23) | 55 (19–122) | 6 (2–13) | 5 (0–9) | 0 (0–2) | 7 (2–10) | 7 (44) | 5 (31) | ||||||||
| No | 5 (3–10) | 36 (13–83) | 1 (0–4) | 0 (0–0) | 0 (0–0) | 1 (0–4) | 4 (17) | 3 (13) | ||||||||
| Anemia on arrival at hospital** | 0.27 | 0.06 | 0.85 | 0.76 | 0.68 | 0.15 | 0.65 | — | ||||||||
| Yes | 6 (4–18) | 40 (16–94) | 3 (0–7) | 0 (0–6) | 0 (0–1) | 2 (1–8) | 10 (30) | 8 (100) | ||||||||
| No | 6 (2–8) | 9 (7–19) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 1 (17) | 0 (−) | ||||||||
| TAC on arrival at hospital† | 0.03 | 0.07 | 0.007 | 0.007 | 0.01 | 0.03 | >0.99 | — | ||||||||
| Yes | 8 (4–21) | 45 (15–102) | 4 (0–10) | 2 (0–8) | 0 (0–2) | 4 (1–9) | 8 (30) | 8 (100) | ||||||||
| No | 4 (2–6) | 18 (10–54) | 0 (0–2) | 0 (0–0) | 0 (0–0) | 0 (0–1) | 3 (25) | 0 (−) |
IQR indicates 25% to 75% interquartile range.
*Transfusion of ≥4 U of whole blood or pRBCs between trauma and arrival at Percy hospital.
**Hemoglobin level <13 g/dL.
†Prothrombin time <70% and/or platelets <100 ×109/L.
DISCUSSION
This study analyzed the characteristics of 39 French military severe trauma patients injured during recent military operations and admitted to the ICU of the Percy hospital, between 2016 and 2021. The study population was a specific subgroup of French military trauma patients injured during military operations. To the best of our knowledge, this is the first study to provide data on the health status and hospital outcomes of severe military trauma patients injured during recent military operations since their arrival at the hospital in France. In this study, nearly 2% of the patients required an ICU admission after strategic aeromedical evacuation. It should be noted that the N-PECC database, used for identification of the military severe trauma patients injured during military operations, collects all strategic aeromedical evacuations back to metropolitan France, regardless of their severity. Hence, this database recorded 1,990 trauma patients, of which 61 had a theoretical destination in ICU after the strategic aeromedical evacuation. In comparison, Poyat et al.31 reported a similar median ISS at 21 (IQR, 10–32) but an ICU admission rate of 51% among French military trauma patients repatriated from Afghanistan between 2001 and 2010. Similarly, Jackson et al.32 investigated a British cohort of patients with BIs and NBIs acquired during military operations in 2009 and reported an ICU admission rate of 32%, but ISS was not reported for this subgroup of patients. Another study of patients with NBIs acquired during military operations in 2012 observed an ICU admission rate of 27%, but ISS was not reported for these patients.33 In our study, two patients died upon their arrival at the hospital, yielding a mortality rate of 0.2 per 1,000 repatriated casualties per year. In the study by Jackson et al.,32 the mortality rate was 7.7 per 1,000 repatriated casualties per year. Three hypotheses may explain such differences. First, hospitalization policies for patients with less severe trauma may vary according to the country. Indeed, a large number of patients with mild trauma may have been hospitalized within the French armed forces, which might not be the case within the British armed forces. Thus, with the denominator being different, the ICU admission and mortality rates may have been mechanically reduced in our cohort. However, this cannot be supported without further knowledge of trauma severity (e.g., ISS). Second, differences in the characteristics of military operations (e.g., battlefield configuration, combat intensity, enemy tactics, period of engagement, nature of military operations, and distance from medical treatment facilities) are associated with differences in the number and type of casualties, as already emphasized in other studies.11,18,34 In the study by Jackson et al.,32 casualties were evacuated from Iraq and Afghanistan, which have theaters of operation differing from those in our study. Third, our study had a retrospective design. However, the N-PECC collects all aeromedical evacuations of French military personnel injured during military operations prospectively and exhaustively. Our study identified all cases based on the requested destination of patients recorded in the N-PECC database—ICU of the Percy hospital. Thus, only few cases may have been missed. Our study reported data consistent with previous reports regarding the type of injuries. For example, the predominance of penetrating trauma, injury mechanisms by explosion and gunshot wounds, and multiple wounds in military trauma patients during recent military operations have been widely reported.10,22,35 However, hospital data of military severe trauma patients injured during military operations and admitted to ICUs are limited. Our study also reported original data. First, the analysis of the anatomic distribution of injuries revealed lower proportions of limb injuries (33%) as well as torso (26%) and head and neck injuries (26%). United States data from Iraq and Afghanistan between 2001 and 2005 demonstrated incidence rates of limb, head and neck, and torso injuries of 54.5%, 30%, and 14.3%, respectively.10 The low proportion of single-limb injuries requiring ICU admission may explain the differences in the anatomic distribution of injuries in our study population. Second, the characteristics of injury showed an unusual trend. Head and neck injuries were most often nonpenetrating, with the presence of intracranial hypertension in 38% of the patients and a median Glasgow Coma Scale score at ICU discharge of 15 (IQR, 14–15). Similarly, in the study by Ponsin et al.3 of French service members requiring an intensive care strategic aeromedical evacuation, only 12% of head injuries were associated with severe TBI, with coma and an indication for the installation of an intracranial pressure sensor. Despite the fact that hemorrhage remains the leading cause of potentially preventable death on the battlefield, catastrophic tissue destruction, including severe TBI, has been described to be the leading cause of death on the battlefield since two decades.35–39 This suggests that, in our study, only patients with the least severe TBI survived and could be admitted to the ICU.
The biological criteria for TAC, defined by a prothrombin time <70% or a platelet count <100 × 109/L, were present upon arrival at the hospital in 69% of our patients. In comparison, Pidcoke et al.40 reported in military trauma patients in Iraq and Afghanistan that only 32.6% of patients who were transfused at least 1 U of blood product presented with TAC, defined by an INR value of >1.5. Despite similar ISS with our study, two hypotheses may explain this discrepancy. First, the timing of TAC screening was different and, consequently, the resuscitation performed in this time interval: less than 1 hour with no transfusion or surgery in the study of Pidcoke et al.40 against more than 24 hours, with possible transfusion and surgery in our study. Second, the definition of TAC in our study relies on low prothrombin time <70% or low platelet count <100 × 109/L, unlike other definitions based on high INR >1.2 or >1.5. The inherent influence of prothrombin time or platelet count in defining TAC may be questionable. However, prothrombin time and INR are strongly correlated when ISI is in the lower part of the recommended range41 (which is the case at Percy hospital), and only 1 of 27 trauma patients in our study was classified as TAC solely because of a platelet count <100 × 109/L. Therefore, misclassification is a concern, but it may not have played a major role in explaining this discrepancy. In our study, patients with TAC had a longer ICU length of stay, longer mechanical ventilation duration, and greater transfusion requirements during ICU stay. Large series of civilian trauma patients also showed that the presence of TAC, defined by a prothrombin time <70% or a platelet count <100 ×109/L, was associated with a longer mechanical ventilation duration, a longer ICU length of stay, and greater transfusion requirements.29,42 Similarly, Peltan et al.43 reported in another cohort of civilian trauma patients that the presence of TAC, defined by an INR value either >1.2 or >1.5, was associated in both cases with a longer mechanical ventilation duration and a longer ICU length of stay. Our data suggest that the trauma characteristics, initial management, and clinical and biological characteristics upon arrival at the hospital may predict longer ICU length of stay, greater ICU transfusion requirements, and/or longer mechanical ventilation duration. However, some characteristics are strongly associated with the presence of TAC and are therefore likely to be only confounding factors. An ISS of >15 or severe abdominal or limb trauma has been reported to be associated with the presence of TAC.29
Herein, 17 patients (44%) developed an infection during ICU stay. Similarly, a previous analysis of 2,513 US service members with BIs and NBIs in Iraq and Afghanistan found a 34% rate of infection during hospital stay. This study showed that massive transfusion of pRBC units in the first 24 hours, an ISS of >15, admission to an ICU, and improvised explosive device-related injury were independent risk factors for infection.44 In addition, accumulating evidence suggests that immune dysregulation may underlie increased susceptibility to infection in severe trauma patients. Some authors have suggested a possible interaction between trauma-induced immunosuppression and blood transfusion-related immunomodulation.45
This study has some limitations. First, the civilian national trauma registry is a powerful tool for the analysis of trauma patients46 but is not tailored for the specific analysis of military severe trauma patients injured during military operations. This study emphasizes the difficulties in identifying and collecting all relevant cases. Using the N-PECC database, 55 patients were identified for inclusion. Among these 55 patients, 19 were included in the civilian national trauma registry, allowing direct data collection, whereas 36 were not included, requiring manual data collection from the computerized medical records of the Percy hospital. Moreover, the civilian national trauma registry is better adapted to the civilian setting, especially regarding the prehospital data. Indeed, in this study, prehospital data referred to all data from the point of injury to the arrival at the Percy hospital, including data from the theater of military operations and during strategic aeromedical evacuation. However, in the military setting, as compared with the civilian setting, the prehospital care on the battlefield is unique, as it involves prolonged delay before reaching the hospital and more frequent transfusion and emergency surgery in the combat zone. Prehospital data are of primary importance, since 87.3% of deaths on the battlefield during recent military operations occur before reaching the first medical treatment facility.36 In this respect, a French military prehospital trauma registry had been temporarily implemented in Afghanistan and might be of interest.4 However, the civilian national trauma registry was the only appropriate database allowing the analysis of hospital data of military trauma patients. There is currently no French military trauma registry collecting data from the point of injury to hospital discharge.4,21 As a trauma organization devoted to the care of military trauma patients injured during military operations, the French Military Medical Service meets most of the requirements recommended by the World Health Organization and American College of Surgeons.47 Focusing on the Percy hospital, its activity as a trauma center is of primary importance for the civilian health territory. During the study period, 1,485 trauma patients were included in the civilian national trauma registry. This homeland experience is of importance to continue to prepare military medical teams for the management of military severe trauma patients after deployment in theaters of military operations. However, the lack of a dedicated and comprehensive trauma registry is a barrier to identifying morbidity and mortality characteristics.48,49 Second, our study included a small number of patients. Thus, the number of events observed was also small. The validity of logistic models becomes problematic when the number of events per variable is <10.50 Thus, our study used univariate analyses only, with no possibility to conclude about causes or prognostic factors. Finally, military severe trauma patients injured during military operations from other nations or civilian trauma patients treated by operational medical units during military operations were not included for reasons of confidentiality. Similarly, the six patients not hospitalized at the Percy hospital were not included, since the receiving hospital was not a partner trauma center of the civilian national trauma registry. However, their analysis would also allow an improvement of the epidemiological knowledge of combat casualties.
In conclusion, this study highlights the characteristics of a small number of military severe trauma patients over the study period. Military severe trauma patients injured during recent military operations presented with near complete resolution of almost all initial organ failures upon arrival at the national territory hospital but developed further complications during their hospital stay. The use of dedicated systemic military trauma registries, including prehospital data during military operations and hospital data in national territories, would improve the specific epidemiological knowledge of injuries during recent military operations and help better prepare for future conflicts that may include major engagements and large-scale combat operations.
Supplementary Material
AUTHORSHIP
T.C. contributed in the literature search, study design, data collection, data analysis, data interpretation, and writing. M.B. contributed in the data collection and critical revision. S.D. contributed in the critical revision. K.B. contributed in the data collection and critical revision. S.T. contributed in the critical revision. P.P. contributed in the literature search, study design, data interpretation, and critical revision.
ACKNOWLEDGMENTS
We thank all French military medical teams involved in the management of military trauma patients injured during military operations, from the point of injury to France. We also thank the Military Medical Service Operational Center for the exploitation of the N-PECC database, and the national registry group for the exploitation of the registry.
DISCLOSURE
The authors declare no conflicts of interest.
The opinions or assertions expressed herein are the private views of the authors and are not to be considered as reflecting the official views of the French Military Medical Service.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Thomas Chiniard, Email: tom.0741@hotmail.fr.
Mathieu Boutonnet, Email: mathieu.boutonnet@intradef.gouv.fr.
Sandrine Duron, Email: sandrine.duron@intradef.gouv.fr.
Kilian Bertho, Email: kilian.bertho@intradef.gouv.fr.
Pierre Pasquier, Email: pierre.pasquier@intradef.gouv.fr.
REFERENCES
- 1.Centre interarmées de concepts, de doctrines et d'expérimentations. Doctrine interarmées DIA-4.0.10_SOUTMED-OPS (2014) relative au soutien médical aux engagements opérationnels. Effective July 31, 2014. Available at: https://www.irsem.fr/data/files/irsem/documents/document/file/68/20140731_np_cicde_dia-4-0-10-soutmed-ops.pdf. Accessed February 22, 2023.
- 2.Luft A Corcostegui SP Millet M Gillard J Boissier J Rondy P, et al. Aeromedical evacuations within the French Armed Forces: analysis of 2,129 patients. Mil Med. 2020;185(3–4):468–476. [DOI] [PubMed] [Google Scholar]
- 3.Ponsin P Swiech A Poyat C Alves F Jacques AE Franchin M, et al. Strategic air medical evacuation of critically ill patients involving an intensive care physician: a retrospective analysis of 16 years of mission data. Injury. 2020;52(5):1176–1182. [DOI] [PubMed] [Google Scholar]
- 4.Précloux P Bérend M Petitjeans F Lamblin A Lohéas D Wey PF, et al. Évolution de la stratégie de prise en charge des blessés de guerre au Role 1. Concepts pédagogiques et intérêts d’un registre des soins d’urgence au combat. Médecine Armées. 2011;39(5):387–393. [Google Scholar]
- 5.Howard JT, Kotwal RS, Santos-Lazada AR, Martin MJ, Stockinger ZT. Reexamination of a battlefield trauma Golden hour policy. J Trauma Acute Care Surg. 2018;84(1):11–18. [DOI] [PubMed] [Google Scholar]
- 6.Pasquier P, de Rudnicki S, Donat N, Auroy Y, Merat S. Epidemiology of war injuries, about two conflicts: Iraq and Afghanistan. Ann Fr Anesth Reanim. 2011;30(11):819–827. [DOI] [PubMed] [Google Scholar]
- 7.Haus-Cheymol R Bouguerra C Mayorg E Nivoix P Prat N Verret C, et al. Blessures par arme à feu et engins explosifs dans les armées. Résultats de la surveillance épidémiologique de 2004 à 2008. Médecine Armées. 2011;39(1):89–96. [Google Scholar]
- 8.Glenn MA Martin KD Monzon D Nettles W Rodriquez VM Lovasz D, et al. Implementation of a combat casualty trauma registry. J Trauma Nurs. 2008;15(4):181–184. [DOI] [PubMed] [Google Scholar]
- 9.Eastridge BJ Costanzo G Jenkins D Spott MA Wade C Greydanus D, et al. Impact of joint theater trauma system initiatives on battlefield injury outcomes. Am J Surg. 2009;198(6):852–857. [DOI] [PubMed] [Google Scholar]
- 10.Owens BD, Kragh JF, Jr., Wenke JC, Macaitis J, Wade CE, Holcomb JB. Combat wounds in operation Iraqi freedom and operation enduring freedom. J Trauma. 2008;64(2):295–299. [DOI] [PubMed] [Google Scholar]
- 11.Kelly JF Ritenour AE McLaughlin DF Bagg KA Apodaca AN Mallak CT, et al. Injury severity and causes of death from operation Iraqi freedom and operation enduring freedom: 2003–2004 versus 2006. J Trauma. 2008;64(2 Suppl):S21–S26. discussion S26-27. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann C Poyat C Alhanati L Haus-Cheymol R de Rudnicki S Bouix-Picasso J, et al. French military deaths in Afghanistan: a retrospective analysis of 450 combat casualties between 2010 and 2012. BMJ Mil Health. 2021;167(2):140. [DOI] [PubMed] [Google Scholar]
- 13.Beranger F Lesquen HD Aoun O Roqueplo C Meyrat L Natale C, et al. Management of war-related vascular wounds in French role 3 hospital during the Afghan campaign. Injury. 2017;48(9):1906–1910. [DOI] [PubMed] [Google Scholar]
- 14.de Lesquen H Beranger F Berbis J Boddaert G Poichotte A Pons F, et al. Challenges in war-related thoracic injury faced by French military surgeons in Afghanistan (2009–2013). Injury. 2016;47(9):1939–1944. [DOI] [PubMed] [Google Scholar]
- 15.Schmitt J Boutonnet M Goutorbe P Raynaud L Carfantan C Luft A, et al. Acute respiratory distress syndrome in the forward environment. Retrospective analysis of acute respiratory distress syndrome cases among French Army war casualties. J Trauma Acute Care Surg. 2020;89(2S Suppl 2):S207–S212. [DOI] [PubMed] [Google Scholar]
- 16.Bonnet S, Gonzalez F, Poichotte A, Duverger V, Pons F. Lessons learned from the experience of visceral military surgeons in the French role 3 Medical Treatment Facility of Kabul (Afghanistan): an extended skill mix required. Injury. 2012;43(8):1301–1306. [DOI] [PubMed] [Google Scholar]
- 17.Barbier O, Malgras B, Versier G, Pons F, Rigal S, Ollat D. French surgical experience in the role 3 medical treatment facility of KaIA (Kabul International Airport, Afghanistan): the place of the orthopedic surgery. Orthop Traumatol Surg Res. 2014;100(6):681–685. [DOI] [PubMed] [Google Scholar]
- 18.Robert J, Tourtier JP, Vitalis V, Coste S, Gaspard W, Bourrilhon C. Air medical-evacuated battle injuries: French Army 2001 to 2014 in Afghanistan. Air Med J. 2017;36(6):327–331. [DOI] [PubMed] [Google Scholar]
- 19.Dagain A Aoun O Bordes J Roqueplo C Joubert C Esnault P, et al. Management of war-related ballistic craniocerebral injuries in a French role 3 hospital during the Afghan campaign. World Neurosurg. 2017;102:6–12. [DOI] [PubMed] [Google Scholar]
- 20.Dagain A Aoun O Sellier A Desse N Joubert C Beucler N, et al. Acute neurosurgical management of traumatic brain injury and spinal cord injury in French armed forces during deployment. Neurosurg Focus. 2018;45(6):E9. [DOI] [PubMed] [Google Scholar]
- 21.Schweizer MA, Janak JC, Stockinger ZT, Monchal T. Description of trauma among French service members in the Department of Defense Trauma Registry: understanding the nature of trauma and the care provided. Mil Med Res. 2019;6(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Travers S Carfantan C Luft A Aigle L Pasquier P Martinaud C, et al. Five years of prolonged field care: prehospital challenges during recent French military operations. Transfusion. 2019;59(S2):1459–1466. [DOI] [PubMed] [Google Scholar]
- 23.Carfantan C Goudard Y Butin C Duron-Martinaud S Even JP Anselme A, et al. Forward Medevac during Serval and Barkhane operations in Sahel: a registry study. Injury. 2017;48(1):58–63. [DOI] [PubMed] [Google Scholar]
- 24.Guénot P Beauchamps V Madec S Carfantan C Boutonnet M Bareau L, et al. Fixed wing tactical aircraft for air medical evacuation in Sahel. Air Med J. 2019;38(5):350–355. [DOI] [PubMed] [Google Scholar]
- 25.Malgras B, Barbier O, Petit L, Rigal S, Pons F, Pasquier P. Surgical challenges in a new theater of modern warfare: the French role 2 in Gao, Mali. Injury. 2016;47(1):99–103. [DOI] [PubMed] [Google Scholar]
- 26.Dubost C, Goudard Y, Soucanye de Landevoisin E, Contargyris C, Evans D, Pauleau G. Combat casualties from two current conflicts with the Seventh French Forward Surgical Team in Mali and Central African Republic in 2014. J R Army Med Corps. 2016;162(6):450–455. [DOI] [PubMed] [Google Scholar]
- 27.Kandel M. U.S. Strategy in Africa, Etude de l'IRSEM n°36. 2014. Available at: https://www.irsem.fr/publications-de-l-irsem/etudes.html. Accessed May 31, 2023. [Google Scholar]
- 28.Hamada SR Rosa A Gauss T Desclefs JP Raux M Harrois A, et al. Development and validation of a pre-hospital « red flag » alert for activation of intra-hospital haemorrhage control response in blunt trauma. Crit Care. 2018;22(1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maegele M Lefering R Yucel N Tjardes T Rixen D Paffrath T, et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury. 2007;38(3):298–304. [DOI] [PubMed] [Google Scholar]
- 30.Dorgalaleh A, Favaloro EJ, Bahraini M, Rad F. Standardization of prothrombin time/international normalized ratio (PT/INR). Int J Lab Hematol. 2021;43(1):21–28. [DOI] [PubMed] [Google Scholar]
- 31.Poyat C, Boutonnet M, Pelée de Saint Maurice G, Ausset S, Daban JL, Blot RM. Profil des blessés de guerre Français en Afghanistan: expérience du service de santé des armées sur la période 2001–2010. Anesth Réanimation. 2017;3(5):403–412. [Google Scholar]
- 32.Jackson PC, Foster M, Fries A, Jeffery SLA. Military trauma care in Birmingham: observational study of care requirements and resource utilisation. Injury. 2014;45(1):44–49. [DOI] [PubMed] [Google Scholar]
- 33.Brewster CT Forbes K Handford C Scallan N Eskell M Hettiaratchy S, et al. Planning for UK terror attacks: analysis of blast and ballistic injuries. Injury. 2021;52(5):1221–1226. [DOI] [PubMed] [Google Scholar]
- 34.Brethauer SA Chao A Chambers LW Green DJ Brown C Rhee P, et al. Invasion vs insurgency: US Navy/Marine Corps forward surgical care during Operation Iraqi Freedom. Arch Surg. 2008;143(6):564–569. [DOI] [PubMed] [Google Scholar]
- 35.Eastridge BJ Hardin M Cantrell J Oetjen-Gerdes L Zubko T Mallak C, et al. Died of wounds on the battlefield: causation and implications for improving combat casualty care. J Trauma. 2011;71(1 Suppl):S4–S8. [DOI] [PubMed] [Google Scholar]
- 36.Eastridge BJ Mabry RL Seguin P Cantrell J Tops T Uribe P, et al. Death on the battlefield (2001-2011): implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012;73(6 Suppl 5):S431–S437. [DOI] [PubMed] [Google Scholar]
- 37.Mazuchowski EL Kotwal RS Janak JC Howard JT Harcke HT Montgomery HR, et al. Mortality review of US Special Operations Command battle-injured fatalities. J Trauma Acute Care Surg. 2020;88(5):686–695. [DOI] [PubMed] [Google Scholar]
- 38.Janak J Stockinger Z Mazuchowski E Kotwal R Sosnov J Montgomery H, et al. Military preventable death conceptual framework: a systematic approach for reducing battlefield mortality. Mil Med. 2018;183(suppl 2):15–23. [DOI] [PubMed] [Google Scholar]
- 39.Kotwal RS Staudt AM Mazuchowski EL Gurney JM Shackelford SA Butler FK, et al. A US military Role 2 forward surgical team database study of combat mortality in Afghanistan. J Trauma Acute Care Surg. 2018;85(3):603–612. [DOI] [PubMed] [Google Scholar]
- 40.Pidcoke HF Aden JK Mora AG Borgman MA Spinella PC Dubick MA, et al. Ten-year analysis of transfusion in Operation Iraqi Freedom and Operation Enduring Freedom: increased plasma and platelet use correlates with improved survival. J Trauma Acute Care Surg. 2012;73(6 suppl 5):S445–S452. [DOI] [PubMed] [Google Scholar]
- 41.Poller L. International normalized ratios (INR): the first 20 years. J Thromb Haemost. 2004;2(6):849–860. [DOI] [PubMed] [Google Scholar]
- 42.Fröhlich M Mutschler M Caspers M Nienaber U Jäcker V Driessen A, et al. Trauma-induced coagulopathy upon emergency room arrival: still a significant problem despite increased awareness and management? Eur J Trauma Emerg Surg. 2019;45(1):115–124. [DOI] [PubMed] [Google Scholar]
- 43.Peltan ID, Vande Vusse LK, Maier RV, Watkins TR. An international normalized ratio-based definition of acute traumatic coagulopathy is associated with mortality, venous thromboembolism, and multiple organ failure after injury. Crit Care Med. 2015;43(7):1429–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tribble DR Li P Warkentien TE Lloyd BA Schnaubelt ER Ganesan A, et al. Impact of operational theater on combat and noncombat trauma-related infections. Mil Med. 2016;181(10):1258–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shah S, Spinella PC, Muszynski JA. Immunologic effects of trauma and transfusion. J Trauma Acute Care Surg. 2017;82(6S suppl 1):S50–S56. [DOI] [PubMed] [Google Scholar]
- 46.Moyer JD Hamada SR Josse J Auliard O Gauss T, Traumabase Group . Trauma reloaded: trauma registry in the era of data science. Anaesth Crit care Pain Med. 2021;40(2):100827. [DOI] [PubMed] [Google Scholar]
- 47.Moore L Champion H O’Reilly G Leppaniemi A Cameron P Palmer C, et al. Impact of trauma system structure on injury outcomes: a systematic review protocol. Syst Rev. 2017;6(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gauss T Balandraud P Frandon J Abba J Ageron FX Albaladejo P, et al. Strategic proposal for a national trauma system in France. Anaesth Crit Care Pain Med. 2019;38(2):121–130. [DOI] [PubMed] [Google Scholar]
- 49.Deming WE. Opportunities in mathematical statistics, with special reference to sampling and quality control. Science. 1943;97(2514):209–214. [DOI] [PubMed] [Google Scholar]
- 50.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–1379. [DOI] [PubMed] [Google Scholar]


