Abstract
Aims
United Classification System (UCS) B2 and B3 periprosthetic fractures in total hip arthroplasties (THAs) have been commonly managed with modular tapered stems. No study has evaluated the use of monoblock fluted tapered titanium stems for this indication. This study aimed to evaluate the effects of a monoblock stems on implant survivorship, postoperative outcomes, radiological outcomes, and osseointegration following treatment of THA UCS B2 and B3 periprosthetic fractures.
Methods
A retrospective review was conducted of all patients who underwent revision THA (rTHA) for periprosthetic UCS B2 and B3 periprosthetic fracture who received a single design monoblock fluted tapered titanium stem at two large, tertiary care, academic hospitals. A total of 72 patients met inclusion and exclusion criteria (68 UCS B2, and four UCS B3 fractures). Primary outcomes of interest were radiological stem subsidence (> 5 mm), radiological osseointegration, and fracture union. Sub-analysis was also done for 46 patients with minimum one-year follow-up.
Results
For the total cohort, stem osseointegration, fracture union, and stem subsidence were 98.6%, 98.6%, and 6.9%, respectively, at latest follow-up (mean follow-up 27.0 months (SD 22.4)). For patients with minimum one-year of follow-up, stem osseointegration, fracture union, and stem subsidence were 97.8%, 97.8%, and 6.5%, respectively.
Conclusion
Monoblock fluted stems can be an acceptable modality for the management of UCS B2 periprosthetic fractures in rTHAs due to high rates of stem osseointegration and survival, and the low rates of stem subsidence, and revision. Further research on the use of this stem for UCS B3 periprosthetic fractures is warranted to determine if the same conclusion can be made for this fracture pattern.
Cite this article: Bone Jt Open 2023;4(8):551–558.
Keywords: Revision total hip arthroplasty, Monoblock Femoral Stem, UCS B2, UCS B3, B3 periprosthetic fractures, revision total hip arthroplasties, osseointegration, periprosthetic fractures, radiological outcomes, titanium stems, total hip arthroplasties (THAs), Hip, femoral head, femoral stems
Introduction
United Classification System (UCS) B2 and B3 fractures are defined as periprosthetic fractures (PPFx) around a loose femoral stem, with or without good remaining bone stock, respectively. These have shown challenges in management due to difficulties in treating the fracture in tandem with managing the loose implant, requiring revision total hip arthroplasty (rTHA) surgery, as well as fracture fixation.1-4 UCS B2 and B3 fractures have been traditionally managed with the use of modular long porous-coated tapered cementless stems with optional use of proximal bone allograft and cerclage cables.3,5-8 The construct popularity has been attributed to multiple factors, such as control in the adjustment of leg length, neck anteversion, and offset following implantation of the distal fixation portion of the stem, in addition to imparting stability distal to the PPFx while maintaining the proximal femoral bone.3,5-8 However, studies have also shown several disadvantages, such as higher rates of stem subsidence and intraoperative fracture, as well as implant failures including corrosion and junctional fractures at the proximal and distal segments of the prosthesis.9-11 Although monoblock stems have not been used in the same volume as modular stems for the management of PPFx, they have been shown as an acceptable modality for rTHAs, with similar clinical and functional outcomes as well as similar complication rates compared to modular stems.9,12-16 A main drawback of monoblock stems may be the lack of versatility offered by modular stems; however, they may offer simplicity of use and reduced cost.17
The purpose of the current study was to determine implant survivorship, postoperative complications, postoperative revisions, radiological outcomes, and osseointegration following treatment of a PPFx with a single design fluted tapered titanium monoblock stem.
Methods
Data source
We performed a retrospective review of all patients who underwent rTHA for periprosthetic UCS B2 and B3 fracture with a minimum follow-up of 90 days who received a single-design fluted tapered titanium monoblock stem at two large, tertiary care, academic hospitals (NYU Langone Orthopedic Hospital, and Florida Orthopaedic Institute). After obtaining institutional review board approval, electronic medical records (EMR) were reviewed to identify all rTHAs performed between April 2015 and February 2021. Inclusion criteria for this study was patients who were aged 18 years or older who underwent rTHA of their primary femoral stem using a monoblock stem (Redapt Revision Hip System; Smith & Nephew, USA) for UCS B2 and B3 periprosthetic fractures. Exclusion criteria included primary and conversion THA cases, and use of the same monoblock stem for revisions other than periprosthetic UCS B2 and B3 fractures (Figure 1). Data about UCS B2 and B3 fractures were taken from two surgeons, one from each institution: RS has 11 years of experience and uses the posterior approach, while DTW has 16 years of experience and uses the direct anterior approach. After exposing the hip joint, fracture site, and implants, both surgeons dislocated the hip, explanted the femoral stem, and assessed stability of the acetabular component. None of the cases required an extended trochanteric osteotomy for implant removal. Following thorough debridement and irrigation both surgeons introduced the revision monoblock tapered stem followed by fracture fixation using cerclage wires, cables, and/or plates. After inclusion and exclusion criteria were satisfied, the study total cohort consisted of 72 patients. A sub-analysis was performed to report outcomes for the 46 patients who had a minimum one-year follow-up.
Fig. 1.
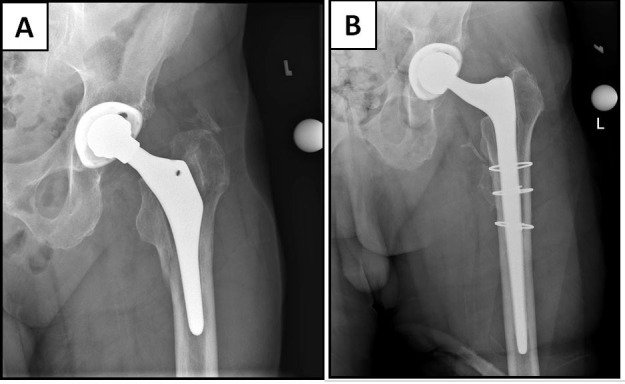
a) Preoperative hip anteroposterior (AP) radiograph of 72-year-old male with Vancouver B2 periprosthetic fracture. b) Two-year postoperative AP hip radiograph with monoblock tapered fluted revision femoral stem with stem osseointegration.
Outcomes
EMRs from both institutions were reviewed for demographic data, including age, race, sex, BMI, smoking status, and American Society of Anesthesiologists (ASA) grade. Surgical data were also collected, including operating time, as measured from time of incision to closing, surgical approach, use of cerclage cables and greater trochanter fixation plates, and implant size, including femoral stem length, size, and femoral head diameter. Clinical outcomes such as length of stay (LOS), discharge disposition, 90-day readmissions, and 90-day readmission indications were collected. LOS was calculated from surgery to discharge time. Immediate postoperative mobility and rehabilitation was allowing weightbearing as tolerated. In addition, number of reoperations, defined as any return to the operating theatre without revision of implants, and reoperation indication was obtained. Furthermore, indication and number of re-revisions were collected. Re-revision was defined as any return to the operating theatre where the acetabular component, femoral component, and/or polyethylene liner were explanted or exchanged. Anteroposterior (AP) and cross-table lateral radiographs were analyzed for radiological outcomes, and these were obtained during the preoperative period, the immediate postoperative period, and subsequent visits. Stem subsidence was assessed by measuring the distance between predetermined landmarks on the prosthesis and the femur such as measuring the distance from the shoulder of the implanted prosthesis to the proximal tip of the greater trochanter of the femur, or the distance from the shoulder of the prosthesis to cerclage cables on the femur, as discussed by Callaghan et al.18 A change of > 5 mm from the immediate postoperative radiograph to the latest radiograph was considered significant subsidence as described by numerous studies.19-22 Furthermore, stem osseointegration was assessed by radiologically analyzing fixation by bony ongrowth, defined as the formation and attachment of new bone onto the femoral prosthesis.23 This was done according to criteria established by Rodriguez et al,24 adapted from Engh et al,25 who defined radiological fixation by bony ongrowth as minimal or no radio-opaque line formation around the stem and no subsidence beyond the initial six weeks of weightbearing. Radiographs were independently reviewed by two orthopaedic surgeons.
Statistical analysis
Descriptive statistics were used to present the data. Categorical variables were presented using chi-squared analysis and reported in count (percentage). Continuous variables were presented in medians (interquartile range (IQR)). Follow-up was presented with means and standard deviations (SDs). Statistical analysis was performed using SPSS v. 25 (IBM, USA).
Results
Demographics
The total cohort mean follow-up time was 27.0 months (SD 22.4). For the total cohort, mean age was 71.5 years (36 to 92). In all, 21 patients (29.2%) were male and 51 (70.8%) were female. Mean BMI was 25.6 kg/m2 (21.0 to 29.4). Additional demographic data can be found in Table I.
Table I.
Demographic data for full cohort.
| Variable | Cohort (n = 72) |
|---|---|
| Median age, yrs (IQR) | 72 (63 to 83) |
| Sex, n (%) | |
| Male | 21 (29.2) |
| Female | 51 (70.8) |
| Median BMI, kg/m2 (IQR) | 24.3 (21.0 to 29.4) |
| ASA grade, n (%) | |
| 1 | 0 (0) |
| 2 | 29 (40.3) |
| 3 | 38 (52.8) |
| 4 | 5 (6.9) |
| Smoking status, n (%) | |
| Current | 51 (70.8) |
| Former | 16 (22.2) |
| Everyday | 5 (6.9) |
| Race, n (%) | |
| White | 64 (88.9) |
| African-American | 5 (6.9) |
| Asian | 2 (2.8) |
| Other race | 1 (1.4) |
ASA, American Society of Anesthesiologists; IQR, interquartile range.
Periprosthetic fracture and surgical characteristics
A total of 68 patients (94.4%) had a UCS B2 fracture, whereas four patients (5.6%) had a UCS B3 fracture. The median stem size, stem thickness, and femoral head diameters were 240 mm, 17 mm, and 36 mm, respectively. Median surgical time was 116 minutes (IQR 96 to 144). Median estimated blood loss was 500 ml (IQR 300 to 800). Additional surgical data can be found in Table II. Of the 72 fractures, one patient with a UCS B3 fracture received cancellous chips as an allograft. Additional surgical data can be found in Table II.
Table II.
Surgical and fracture characteristics for full cohort.
| Variable | Cohort (n = 72) |
|---|---|
| Mean surgical time, mins (IQR) | 116 (96 to 144) |
| Mean estimated blood loss, ml (IQR) | 500 (300 to 800) |
| Mean length of stay, days (IQR) | 5.9 (4.0 to 6.6) |
| Laterality, n (%) | |
| Right | 38 (52.8) |
| Left | 34 (47.2) |
| Median stem size, mm | 240 |
| Median stem thickness, mm | 17 |
| Median femoral head diameter, mm | 36 |
| UCS, n (%) | |
| B2 | 68 (94.4) |
| B3 | 4 (5.6) |
| Greater trochanter plate, n (%) | |
| No | 48 (66.7) |
| Yes | 24 (33.3) |
| Cables, n (%) | |
| No | 4 (5.6) |
| Yes | 68 (94.4) |
| Median (IQR) | 3 (0 to 6) |
IQR, interquartile range.
Outcomes for total cohort
Overall, 11 patients (15.3%) were readmitted within 90 days; seven (9.7%) of these were non-orthopaedic-related readmissions, of whom two (2.8%) were readmitted for cellulitis around the surgical site, two (2.8%) for sepsis (unrelated to the rTHA), one (1.4%) for an ST-elevation myocardial infarction, one (1.4%) for altered mental status, and one (1.4%) for a gout flare up. A total of two patients were readmitted within 90 days for re-revisions, one of which was for instability/dislocation, and another for femoral stem subsidence > 2 cm. One patient (1.4%) suffered a L1 burst fracture from a fall, and one patient (1.4%) had a reoperation within 90 days, due to a closed fracture of the greater trochanter as a result of a fall. This was managed with open reduction and internal fixation (ORIF).
A total of four (5.6%) re-revision THAs were noted, of which two (2.8%) were for instability/dislocation. In the first case of re-revision, for instability/dislocation the liner and femoral head were revised. For the primary THA, this patient received a 32 + 8 mm ceramic head and a neutral liner. In the rTHA for fracture, this was replaced with a 36 mm outer and a 22 + 0 mm inner dual-mobility head. For the re-revision THA for dislocation, this was revised to a 32 + 4 mm ceramic head and a 20° lipped liner. The shell was well fixed and well positioned and therefore retained throughout all three surgeries. In the second case of re-revision for instability/dislocation, the femoral head, and liner were revised. For the primary THA, the patient received a 36 + 4 mm ceramic head and a 20° lipped liner. In the rTHA for fracture, this was replaced with a 36 + 3 oxinium head, while the liner was retained. For the re-revision THA for dislocation, this was replaced with 48 mm outer and a 28 + 4 mm inner dual-mobility head. The shell was well fixed and well positioned and therefore retained throughout all three surgeries. All acetabular cups were assessed for implant stability and position during the index revision. Within our cohort none of the patients had a loose or mal-positioned acetabular component as assessed by the operating surgeon at the time of the surgery, thus none of the acetabular cups were revised. The third re-revision (1.4%) was for aseptic failure of the femoral stem due to significant stem subsidence (> 2 cm). In this case, the liner, femoral head, and femoral stem were revised. The fourth re-revision (1.4%) was for periprosthetic joint infection (PJI). This patient received a two stage re-revision for infection six years after index revision due to Staphylococcus aureus PJI. The stem was explanted in the first stage and an antibiotic spacer was implanted. In the second stage, the spacer was explanted and a monoblock fluted tapered stem was implanted. The femoral head, liner, and acetabular shell were also revised.
Stem radiological osseointegration and fracture union occurred in 71 (98.6%) of implanted stems, while radiological stem subsidence was detected in five patients (6.9%). Of these, four stabilized and achieved radiological osseointegration. These four patients had subsidences of 5.4 mm, 5.3 mm, 15.1 mm, and 15.4 mm, respectively. An example of a patient that had 15.4 mm subsidence that eventually stabilized can be seen in Figure 2.
Fig. 2.
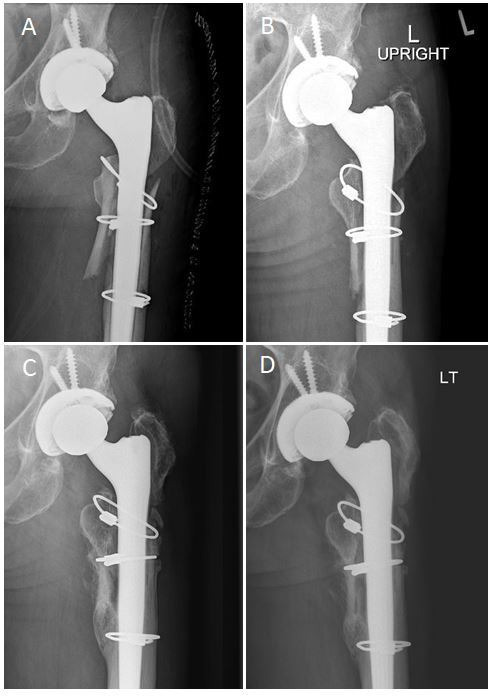
Radiological sequelae of a 58-year-old female patient with subsidence which stabilized over time. a) Immediate postoperative anteroposterior (AP) left hip radiograph demonstating a Vancouver B2 periprosthetic fracture revised with a monoblock tapered fluted stem and three cerclage wires. b) One-month postoperative AP left hip radiograph demonstrating minor femoral implant subsidence compared to initial stem position in a). c) One-year postoperative AP left hip radiograph with continued femoral implant subsidence d) Two-year postoperative AP left hip radiograph with stabilized femoral implant subsidence.
One patient did not achieve radiological osseointegration. Following fixation of the UCS B2 fracture, one patient complained of a leg length discrepancy (LLD) at four weeks postoperatively, after reporting no issues during their two-week visit. Imaging showed 15.1 mm subsidence of the femoral stem is shown in Figure 3. At the six-week visit, the patient continued to complain of a LLD and new onset pain. Radiological analysis demonstrated continued subsidence. The patient was re-revised from a size 15 mm diameter stem to an 18 mm diameter larger stem of the same design, and at two years’ follow-up post-re-revision, the patient was doing well with no reported pain or LLD.
Fig. 3.
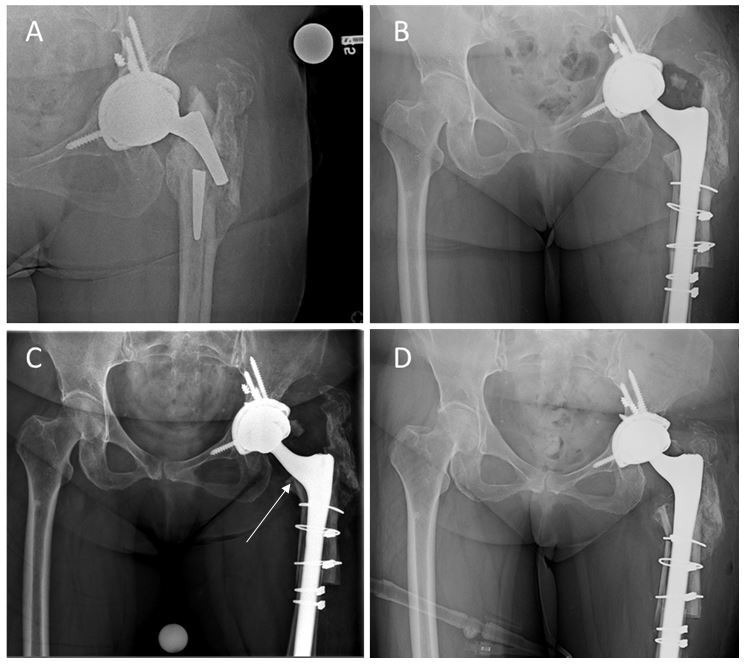
Radiological sequelae of a 61-year-old female who did not achieve osseointegration. a) Preoperative anteroposterior (AP) hip radiograph of a Vancouver B2 fracture, as well as a femoral stem fracture following a minor trauma. b) Immediate postoperative AP pelvis radiograph demonstrating a revised femoral implant using a monoblock tapered fluted revision femoral stem and cerclage wires. c) Four weeks postoperative AP pelvis radiograph showing a femoral stem subsidence compared to the immediate postoperative radiograph. d) Immediate postoperative AP pelvis radiograph following re-revision surgery with a monoblock tapered fluted revision femoral stem.
Outcomes for patients with a minimum two-year follow-up
The mean follow-up time for the sub-analysis (n = 46) with a minimum one-year follow-up was 38.6 months (SD 17.9). Stem radiological osseointegration and fracture union occurred in 45/46 (97.8%) of implanted stems, while stem subsidence was radiologically detected in three patients (6.5%). Of these, two stabilized and achieved radiological osseointegration. The stem that did not achieve osseointegration and was revised was due to significant (> 2 cm) stem subsidence, as mentioned previously. Additional data can be found in Table III.
Table III.
Clinical outcomes of full cohort and sub-analysis.
| Variable | Cohort (n = 72) | Sub-analysis (n = 46) |
|---|---|---|
| Discharge disposition, n (%) | ||
| Home | 28 (38.9) | 19 (41.3) |
| SNF | 37 (51.4) | 24 (52.2) |
| ARF | 7 (9.7) | 3 (6.5) |
| 90-day readmission, n (%) | 11 (15.3) | 6 (13.0) |
| Reason for 90-day readmission, n (%) | ||
| Non-orthopaedic | 7 (9.7) | 4 (8.7) |
| Revision | 2 (2.8) | 1 (2.2) |
| Reoperation | 1 (1.4) | 1 (2.2) |
| Trauma | 1 (1.4) | 0 (0.0) |
| Reason for reoperation, n (%) | ||
| Periprosthetic fracture | 1 (1.4) | 1 (2.2) |
| Revision, n (%) | 4 (5.6) | 4 (8.7) |
| Instability/dislocation | 2 (2.8) | 2 (4.3) |
| Aseptic stem failure | 1 (1.4) | 1 (2.2) |
| PJI | 1 (1.4) | 1 (2.2) |
| Osseointegration, n (%) | 71 (98.6) | 45 (97.8) |
| Fracture union, n (%) | 71 (98.6) | 45 (97.8) |
| Subsidence, n (%) | 5 (6.9) | 3 (6.5) |
ARF, acute rehabilitation facility; PJI, periprosthetic joint infection; SNF, skilled nursing facility.
Discussion
Periprosthetic UCS B2 and B3 fractures are a potential devastating consequence following primary THA, with known challenges in management of the fracture and femoral stem implant. Due to expansion of indications for THA, as well as a growing elderly population, the incidence of periprosthetic fracture is expected to rise.26,27 To our knowledge, this is the first study to report the outcomes of a single monoblock fluted tapered titanium stem in the management of UCS B2 and B3 periprosthetic fractures. Our findings support the use of a monoblock stem as an acceptable modality due to high implant survivorship and radiological osseointegration, and low rates of stem revision and subsidence.
At most recent follow-up, 71 out of 72 stems (98.6%) in the full cohort had achieved radiological osseointegration, as well as 45 out of 46 stems (97.8%) in the minimum one-year follow-up sub-analysis. Although there were no previous studies detailing outcomes for UCS B2 and B3 fractures in solely monoblock stems, the present study’s reported rates of osseointegration and subsidence are consistent with previous studies that evaluated the use of modular tapered fluted titanium stems for the management of UCS B2 and B3 periprosthetic fractures.3,5-8,28-32 In particular, Munegato et al31 observed radiological outcomes of 25 patients with UCS B2 and B3 fractures treated with modular tapered fluted titanium stems, with a mean follow-up time of 29.16 months, similar to our study. They found that 2/25 patients (8.0%) had a subsidence ≥ 5 mm, and 24/25 patients (96%) had radiological union by latest follow-up, comparable to the rates of subsidence and radiological osseointegration in the current study.31 Moreover, they did not observe any cases of re-revision for aseptic stem failure in their cohort as well.31
There were four re-revisions (5.6%) in the total cohort in the current study, the most common aetiology was instability/dislocation (2.8%). Although some studies have previously reported that dislocation is one of the most, if not the most, common complication after rTHA, not all of these dislocations required a re-revision surgery and were instead managed with closed reduction.13,15,33-35 In addition, some studies evaluated older monoblock designs and may not be indicative of outcomes of modern monoblock stems.15,33,34,36,37 A more recent study conducted by Yacovelli et al14 evaluated outcomes of modern revision modular and monoblock tapered fluted titanium femoral stem designs, and found no re-revision surgeries for dislocations in their cohort of 63 patients (out of 335) who were managed with monoblock tapered fluted titanium stems. Moreover, they found no statistically significant difference in re-revision surgeries due to dislocation between both their monoblock and modular cohorts.14 Moreover, Feng et al12 compared outcomes of rTHA for all indications in 108 modular TFT stems compared to 110 monoblock TFT stems, and found no statistical differences with regards to rates of postoperative dislocation between cohorts. Lastly, Koutalos et al38 conducted a systematic review of 46 studies with a combined 4,601 stem revisions that compared outcomes between monoblock and modular tapered fluted stems, and found no statistically significant difference in postoperative dislocation rates.
As previously discussed, modular stems have been a preferred option for periprosthetic UCS B2 and B3 fractures.3,5-8 Reported complications of modular stems include increased risk of femoral fracture and stem fractures at the modular junction compared to monoblock stems.12,39-41 Feng et al12 found that their cohort of 108 modular stems had a statistically significant increase in incidence (16.7%) of intraoperative femoral fractures compared to their cohort of 110 nonmodular stems (4.5%; p = 0.004). Similar studies have corroborated these results.40,42-44 Feng et al12 also postulated that the high rate of intraoperative femoral fractures for modular stems could be due to the design of the modular prosthesis, as well as experience of the operating surgeon, while Huddleston et al40 reported that optimization of the distal and proximal segments of the trial prosthesis may lead to hoop stresses above the threshold for fracture that could lead to inevitable failure once the real prosthesis is implanted. In addition, modular stems have been reported to have risks of stem and junctional fractures, especially in overweight and obese patients.11,45,46 Konan et al46 detailed a series of five fractures (18.5%) at the modular junction of 27 revision modular tapered fluted stems, and suggested that due to this risk of stem fracture, non-modular stems should be considered more for stem revisions for all indications. In a separate study, Konan et al47 also conducted a systemic review of outcomes of revision THAs using a monoblock stem (Wagner; Zimmer Biomet, USA), and found no reports of stem fractures. In the present study, we also did not encounter any reported stem fractures.
However, it is important to note that although the aforementioned studies show no difference in dislocation rates between modular and monoblock stems, modular stems can provide the benefit of optimizing leg length, offset and femoral neck anteversion. Restrepo et al48 discussed the utility of modular femoral stems in 118 patients who required an rTHA due to failure of the femoral component, and they reported that they were able to restore femoral offset and equalize leg length, in addition to providing adequate distal fixation in a majority of their patients.
Limitations
There are several limitations to the present study: it was retrospective in nature, which can introduce potential selection bias. Also, these revision surgeries were not all performed by the same surgeon, and were not all performed in the same institution, leading to potential differences in surgical technique and approach. Although UCS B2 and B3 fractures are similar in nature, we may not have enough UCS B3 fractures in our analysis to conclude that a monoblock fluted tapered stem could be an effective management option for UCS B3 fractures. In addition, there was no comparison group, as we analyzed solely patients who received the same monoblock single-design fluted tapered titanium stem. Moreover, the sample size of this study is relatively limited, and the sample of patients with at least two-year follow-up is even smaller. Furthermore, both surgeons planned to use a monoblock stem preoperatively, and it was used in all cases, but we are unaware of any intraoperative decisions due to the retrospective nature of the study. Lastly, we did not have patient-reported outcome scores due to lack of sufficient data from the cohort and the non-elective nature of the cases.
In conclusion, modular fluted tapered stems have been a preferred choice of management for UCS B2 and B3 periprosthetic fractures, we believe monoblock stems can provide similar postoperative radiological and clinical outcomes for UCS B2 fractures as shown in our study with comparable rates of subsidence, and stem revision. Further work to evaluate the use of monoblock stems for this indication, especially in UCS B3 fractures, is needed to corroborate our results and provide surgeons another valid, efficacious, and evidence-based option for management of UCS B2 and B3 periprosthetic fractures.
Take home message
- Monoblock fluted stems can be an acceptable modality for the management of UCS B2 periprosthetic fractures in revision total hip arthroplasties (rTHAs).
- Rates of stem osseointegration and survival, and low rates of stem subsidence and revision, compared to modular stems, provide surgeons with additional options for rTHAs for UCS B2 fractures.
Author contributions
J. Thomas: Data curation, Formal analysis, Methodology, Writing – original draft.
I. Shichman: Conceptualization, Methodology, Writing – original draft.
L. Ohanisian: Data curation, Formal analysis, Writing - review & editing.
T. K. Stoops: Data curation, Formal analysis, Writing – review & editing.
K. W. Lawrence: Writing – review & editing.
I. Ashkenazi: Metholodogy, Formal analysis, Writing – review & editing.
D. T. Watson: Supervision, Writing – review & editing.
R. Schwarzkopf: Supervision, Conceptualization, Writing – review & editing.
Funding statement
The authors received no financial or material support for the research, authorship, and/or publication of this article.
ICMJE COI statement
R. Schwarzkopf reports royalties from Smith & Nephew, consulting fees from Smith & Nephew, Zimmer, and Intellijoint, speaker payments from Smith & Nephew and Zimmer, leadership or fiduciary role on AAOS, AAHKS, Arthroplasty Today, and Journal of Arthroplasty, and stock or stock options in PSI, Gauss Surgical, and Intellijoint, all of which are unrelated to this study. D. T. Watson reports consulting fees and speaker payments from Smith & Nephew and Corin, unrelated to this study.
Data sharing
The datasets generated and analyzed in the current study are not publicly available due to data protection regulations. Access to data is limited to the researchers who have obtained permission for data processing. Further inquiries can be made to the corresponding author.
Ethical review statement
Our Institutional Review Board (IRB ID#: i17-01223_CR5) has approved this study.
Open access funding
The open access fee for this article was funded by the Division of Adult Reconstruction of the Department of Orthopedic Surgery at NYU Langone Orthopedic Hospital (212-598-6000).
Follow J. Thomas @NYUARResearch
Follow R. Schwarzkopf @MDSchwarzkopf
© 2023 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Contributor Information
Jeremiah Thomas, Email: Jeremiah.Thomas@nyulangone.org.
Ittai Shichman, Email: ittai.shichman@nyulangone.org.
Levonti Ohanisian, Email: Levonti.Ohanisian@gmail.com.
T. K. Stoops, Email: t.kylestoops@gmail.com.
Kyle W. Lawrence, Email: Kyle.Lawrence@nyulangone.org.
Itay Ashkenazi, Email: Itay.Ashkenazi@nyulangone.org.
David T. Watson, Email: dwatson13@hotmail.com.
Ran Schwarzkopf, Email: ran.schwarzkopf@nyulangone.org.
References
- 1. Lindahl H, Garellick G, Regnér H, Herberts P, Malchau H. Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am. 2006;88-A(6):1215–1222. doi: 10.2106/JBJS.E.00457. [DOI] [PubMed] [Google Scholar]
- 2. Khan T, Grindlay D, Ollivere BJ, Scammell BE, Manktelow ARJ, Pearson RG. A systematic review of Vancouver B2 and B3 periprosthetic femoral fractures. Bone Joint J. 2017;99-B(4 Supple B):17–25. doi: 10.1302/0301-620X.99B4.BJJ-2016-1311.R1. [DOI] [PubMed] [Google Scholar]
- 3. Hannon CP, Sheehan KP, Duong SQ, et al. Modular fluted tapered stems for periprosthetic femoral fractures: excellent results in 171 cases. J Bone Joint Surg Am. 2022;104-A(13):1188–1196. doi: 10.2106/JBJS.21.01168. [DOI] [PubMed] [Google Scholar]
- 4. Maggs JL, Swanton E, Whitehouse SL, et al. B2 or not B2? That is the question: a review of periprosthetic fractures around cemented taper-slip femoral components. Bone Joint J. 2021;103-B(1):71–78. doi: 10.1302/0301-620X.103B1.BJJ-2020-0163.R1. [DOI] [PubMed] [Google Scholar]
- 5. Munro JT, Garbuz DS, Masri BA, Duncan CP. Tapered fluted titanium stems in the management of Vancouver B2 and B3 periprosthetic femoral fractures. Clin Orthop Relat Res. 2014;472(2):590–598. doi: 10.1007/s11999-013-3087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Abdel MP, Lewallen DG, Berry DJ. Periprosthetic femur fractures treated with modular fluted, tapered stems. Clin Orthop Relat Res. 2014;472(2):599–603. doi: 10.1007/s11999-013-2936-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moreta J, Uriarte I, Ormaza A, et al. Outcomes of Vancouver B2 and B3 periprosthetic femoral fractures after total hip arthroplasty in elderly patients. HIP Int. 2019;29(2):184–190. doi: 10.1177/1120700018772163. [DOI] [PubMed] [Google Scholar]
- 8. Otero JE, Martin JR, Rowe TM, Odum SM, Mason JB. Radiographic and clinical outcomes of modular tapered fluted stems for femoral revision for paprosky III and IV femoral defects or Vancouver B2 and B3 femoral fractures. J Arthroplasty. 2020;35(4):1069–1073. doi: 10.1016/j.arth.2019.11.039. [DOI] [PubMed] [Google Scholar]
- 9. Clair AJ, Gabor JA, Patel KS, Friedlander S, Deshmukh AJ, Schwarzkopf R. Subsidence following revision total hip arthroplasty using modular and monolithic components. J Arthroplasty. 2020;35(6S):S299–S303. doi: 10.1016/j.arth.2020.03.008. [DOI] [PubMed] [Google Scholar]
- 10. Abdel MP, Cottino U, Larson DR, Hanssen AD, Lewallen DG, Berry DJ. Modular fluted tapered stems in aseptic revision total hip arthroplasty. J Bone Joint Surg Am. 2017;99-A(10):873–881. doi: 10.2106/JBJS.16.00423. [DOI] [PubMed] [Google Scholar]
- 11. Lakstein D, Eliaz N, Levi O, et al. Fracture of cementless femoral stems at the mid-stem junction in modular revision hip arthroplasty systems. J Bone Joint Surg Am. 2011;93-A(1):57–65. doi: 10.2106/JBJS.I.01589. [DOI] [PubMed] [Google Scholar]
- 12. Feng S, Zhang Y, Bao YH, Yang Z, Zha GC, Chen XY. Comparison of modular and nonmodular tapered fluted titanium stems in femoral revision hip arthroplasty: a minimum 6-year follow-up study. Sci Rep. 2020;10(1):13692. doi: 10.1038/s41598-020-70626-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sandiford NA, Garbuz DS, Masri BA, Duncan CP. Nonmodular tapered fluted titanium stems osseointegrate reliably at short term in revision THAs. Clin Orthop Relat Res. 2017;475(1):186–192. doi: 10.1007/s11999-016-5091-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yacovelli S, Ottaway J, Banerjee S, Courtney PM. Modern revision femoral stem designs have no difference in rates of subsidence. J Arthroplasty. 2021;36(1):268–273. doi: 10.1016/j.arth.2020.07.078. [DOI] [PubMed] [Google Scholar]
- 15. Regis D, Sandri A, Bonetti I, Braggion M, Bartolozzi P. Femoral revision with the wagner tapered stem. J Bone Joint Surg Br. 2011;93-B(10):1320–1326. doi: 10.1302/0301-620X.93B10.25927. [DOI] [PubMed] [Google Scholar]
- 16. Gabor JA, Padilla JA, Feng JE, et al. Short-term outcomes with the REDAPT monolithic, tapered, fluted, grit-blasted, forged titanium revision femoral stem. Bone Joint J. 2020;102-B(2):191–197. doi: 10.1302/0301-620X.102B2.BJJ-2019-0743.R1. [DOI] [PubMed] [Google Scholar]
- 17. Nadeau RP, Garbuz DS. Monoblock or modular tapered stems: making the right choice. Seminars in Arthroplasty. 2016;27(4):261–263. doi: 10.1053/j.sart.2017.03.010. [DOI] [Google Scholar]
- 18. Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am. 1985;67-A(7):1074–1085. doi: 10.2106/00004623-198567070-00011. [DOI] [PubMed] [Google Scholar]
- 19. Pattyn C, Mulliez A, Verdonk R, Audenaert E. Revision hip arthroplasty using a cementless modular tapered stem. Int Orthop. 2012;36(1):35–41. doi: 10.1007/s00264-011-1299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Van Houwelingen AP, Duncan CP, Masri BA, Greidanus NV, Garbuz DS. High survival of modular tapered stems for proximal femoral bone defects at 5 to 10 years followup. Clin Orthop Relat Res. 2013;471(2):454–462. doi: 10.1007/s11999-012-2552-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fink B, Oremek D. The transfemoral approach for removal of well-fixed femoral stems in 2-stage septic hip revision. J Arthroplasty. 2016;31(5):1065–1071. doi: 10.1016/j.arth.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 22. Bobovec D, Bohaček I, Juras J, Delimar D. Risk factors for subsidence of modular fluted tapered stem implanted by using transfemoral Wagner approach during revision hip arthroplasty. Int Orthop. 2020;44(9):1685–1691. doi: 10.1007/s00264-020-04582-1. [DOI] [PubMed] [Google Scholar]
- 23. Karuppal R. Biological fixation of total hip arthroplasty: facts and factors. J Orthop. 2016;13(3):190–192. doi: 10.1016/j.jor.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rodriguez JA, Deshmukh AJ, Klauser WU, Rasquinha VJ, Lubinus P, Ranawat CS. Patterns of osseointegration and remodeling in femoral revision with bone loss using modular, tapered, fluted, titanium stems. J Arthroplasty. 2011;26(8):1409–1417. doi: 10.1016/j.arth.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 25. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69-B(1):45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 26. Pivec R, Issa K, Kapadia BH, et al. Incidence and future projections of periprosthetic femoral fracture following primary total hip arthroplasty: an analysis of international registry data. J Long Term Eff Med Implants. 2015;25(4):269–275. doi: 10.1615/jlongtermeffmedimplants.2015012625. [DOI] [PubMed] [Google Scholar]
- 27. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999;30(2):183–190. doi: 10.1016/S0030-5898(05)70073-0. [DOI] [PubMed] [Google Scholar]
- 28. da Assunção RE, Pollard TCB, Hrycaiczuk A, Curry J, Glyn-Jones S, Taylor A. Revision arthroplasty for periprosthetic femoral fracture using an uncemented modular tapered conical stem. Bone Joint J. 2015;97-B(8):1031–1037. doi: 10.1302/0301-620X.97B8.34431. [DOI] [PubMed] [Google Scholar]
- 29. Lizaur-Utrilla A, Gonzalez-Parreño S, Miralles-Muñoz FA, Lopez-Prats FA. Cementless, fluted, long-stem hemiarthroplasty for Vancouver B2 and B3 periprosthetic fractures around hip hemiarthroplasty. J Arthroplasty. 2019;34(6):1179–1183. doi: 10.1016/j.arth.2019.02.036. [DOI] [PubMed] [Google Scholar]
- 30. Parry JA, Hernandez NM, Berry DJ, Abdel MP, Yuan BJ. Risk factors for subsidence of modular fluted tapered stems used during revision total hip arthroplasty for periprosthetic hip fractures. J Arthroplasty. 2018;33(9):2967–2970. doi: 10.1016/j.arth.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 31. Munegato D, Caminita AD, Sotiri R, Rossi A, Bigoni M, Zatti G. Femoral revision in periprosthetic fractures using a titanium modular fluted tapered stem: mortality and clinical and radiological outcomes. HIP Int. 2020;30(2_suppl):101–107. doi: 10.1177/1120700020971313. [DOI] [PubMed] [Google Scholar]
- 32. van Laarhoven SN, Vles GF, van Haaren EH, Schotanus MGM, van Hemert WLW. Tapered, fluted, modular, titanium stems in Vancouver B periprosthetic femoral fractures: an analysis of 87 consecutive revisions. HIP Int. 2021;31(4):555–561. doi: 10.1177/1120700020904933. [DOI] [PubMed] [Google Scholar]
- 33. Gutiérrez Del Alamo J, Garcia-Cimbrelo E, Castellanos V, Gil-Garay E. Radiographic bone regeneration and clinical outcome with the Wagner SL revision stem: a 5-year to 12-year follow-up study. J Arthroplasty. 2007;22(4):515–524. doi: 10.1016/j.arth.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 34. Böhm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am. 2001;83-A(7):1023–1031. doi: 10.2106/00004623-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 35. Boisgard S, Moreau PE, Tixier H, Levai JP. Bone reconstruction, leg length discrepancy, and dislocation rate in 52 Wagner revision total hip arthroplasties at 44-month follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2001;87(2):147–154. [PubMed] [Google Scholar]
- 36. Young PS, Macarico DT, Silverwood RK, et al. Anatomical pelvic loading of a monoblock polyethylene acetabular component. Bone Joint J. 2021;103-B(5):872–880. doi: 10.1302/0301-620X.103B5.BJJ-2020-1321.R2. [DOI] [PubMed] [Google Scholar]
- 37. Takegami Y, Seki T, Osawa Y, Imagama S. Comparison of periprosthetic femoral fracture torque and strain pattern of three types of femoral components in experimental model. Bone Joint Res. 2022;11(5):270–277. doi: 10.1302/2046-3758.115.BJR-2021-0375.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Koutalos AA, Varitimidis S, Malizos KN, Karachalios T. Clinical, functional and radiographic outcomes after revision total hip arthroplasty with tapered fluted modular or non-modular stems: a systematic review. HIP Int. 2022;32(4):475–487. doi: 10.1177/11207000211004383. [DOI] [PubMed] [Google Scholar]
- 39. Molloy DO, Munir S, Jack CM, Cross MB, Walter WL, Walter WK. Fretting and corrosion in modular-neck total hip arthroplasty femoral stems. J Bone Joint Surg Am. 2014;96-A(6):488–493. doi: 10.2106/JBJS.L.01625. [DOI] [PubMed] [Google Scholar]
- 40. Huddleston JI, Tetreault MW, Yu M, et al. Is there a benefit to modularity in simpler femoral revisions? Clin Orthop Relat Res. 2016:415–420. doi: 10.1007/s11999-015-4474-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kiernan S, Kaptein B, Flivik C, Sundberg M, Flivik G. Unexpected varus deformity and concomitant metal ion release and MRI findings of modular-neck hip stems: descriptive RSA study in 75 hips with 8 years’ follow-up. Acta Orthop. 2021;92(1):67–73. doi: 10.1080/17453674.2020.1853387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pattyn C, Mulliez A, Verdonk R, Audenaert E. Revision hip arthroplasty using a cementless modular tapered stem. Int Orthop. 2012;36(1):35–41. doi: 10.1007/s00264-011-1299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Klauser W, Bangert Y, Lubinus P, Kendoff D. Medium-term follow-up of a modular tapered noncemented titanium stem in revision total hip arthroplasty: a single-surgeon experience. J Arthroplasty. 2013;28(1):84–89. doi: 10.1016/j.arth.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 44. Huang Y, Zhou Y, Shao H, Gu J, Tang H, Tang Q. What is the difference between modular and nonmodular tapered fluted titanium stems in revision total hip arthroplasty. J Arthroplasty. 2017;32(10):3108–3113. doi: 10.1016/j.arth.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 45. Efe T, Schmitt J. Analyses of prosthesis stem failures in noncemented modular hip revision prostheses. J Arthroplasty. 2011;26(4):665. doi: 10.1016/j.arth.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 46. Konan S, Garbuz DS, Masri BA, Duncan CP. Modular tapered titanium stems in revision arthroplasty of the hip. Bone Joint J. 2016;98-B(1_Supple_A):50–53. doi: 10.1302/0301-620X.98B1.36442. [DOI] [PubMed] [Google Scholar]
- 47. Konan S, Garbuz DS, Masri BA, Duncan CP. Non-modular tapered fluted titanium stems in hip revision surgery: gaining attention. Bone Joint J. 2014;96-B(11 Supple A):56–59. doi: 10.1302/0301-620X.96B11.34302. [DOI] [PubMed] [Google Scholar]
- 48. Restrepo C, Mashadi M, Parvizi J, Austin MS, Hozack WJ. Modular femoral stems for revision total hip arthroplasty. Clin Orthop Relat Res. 2011;469(2):476–482. doi: 10.1007/s11999-010-1561-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


