Abstract
Background
Distressing low libido is common among women and has significant negative impacts; mindfulness has shown promise to increase sexual desire in women with low libido, but existing interventions are not tailored to midlife and older women.
Aim
We adapted a mindfulness intervention to meet the needs of this population and conducted a pilot randomized controlled trial to assess feasibility and acceptability.
Methods
Women aged ≥45 years with low libido were randomized to the mindfulness intervention or an education group that met over videoconferencing. The intervention included mindfulness instruction and practice, group discussion, and education on sexuality and aging. The education group included general information on menopause and health.
Outcomes
We defined feasibility by the number of screened women who enrolled and completed their group. We defined acceptability as satisfaction with the group and likelihood of recommending it to another woman with low libido. We assessed sexual function (Female Sexual Function Index) and sexual distress (Female Sexual Distress Scale–Revised) at 6 weeks postconclusion.
Results
Of 81 women screened, 31 were randomized to mindfulness and 30 to education. Eighteen women in the intervention group and 23 in the control group attended at least 1 session. Time conflict was the main reason for nonattendance. Of the 41 women who started attending groups, 37 (90%) attended at least 5 sessions. In the mindfulness group, 73% of women were very or extremely satisfied. Women in the mindfulness group were more likely to recommend it to another person with low libido as compared with those in the education group (P = .031); 67% said that they would probably or definitely recommend it. There were no significant changes in sexual function in either group (mean Female Sexual Function Index score, 22.6 to 18.6 [P = .101] with mindfulness and 21.2 to 19.7 [P = .537] with education). Women in the mindfulness group had significant improvements in sexual distress (mean Female Sexual Distress Scale–Revised score, 27.1 to 19.7; P = .021) while women in the education group did not (19.0 to 15.8; P = .062).
Clinical Implications
Mindfulness may reduce sexual distress in older women with low libido.
Strengths and Limitations
This is the first trial testing mindfulness for midlife and older women with low libido.
Conclusion
A virtual mindfulness intervention for midlife and older women with low libido is feasible and acceptable and appears to improve sexual distress as compared with an education control; these findings provide data that can be used to design a larger clinical trial.
Keywords: mindfulness, libido, pilot projects, feasibility studies, sexuality, menopause, aging
Introduction
Low libido is the most common sexual problem among women of all ages.1,2 When accompanied by sexual distress and persisting or recurrent for at least 6 months, low libido is officially diagnosed as sexual interest/arousal disorder.3 The prevalence of distressing low libido peaks between 40 and 70 years of age, affecting 12% of women in this age group.1 The reasons for low libido in midlife and older women are multifactorial, including changes in reproductive hormones with the menopause transition, changes in relationships with divorce or other life transitions, increases in sleep problems and depression and anxiety symptoms, and changes in self-perception with regard to aging and sexuality.4,5 General stress is also a major predictor of sexual dysfunction in midlife and older women.6,7
Low libido causes significant distress and has negative impacts on quality of life.2,8,9 Women with low libido experience feelings of depressed mood and guilt.10 They have lower quality-of-life ratings as compared with age-matched women without low libido,9 and they have similar quality-of-life ratings to other chronic conditions, such as lung disease and low back pain. Women with libido worry about the negative impact that it can have on their self-image and interpersonal relationships.11
Most women with low libido want treatment, but accessing treatment can be difficult. The Food and Drug Administration has approved 2 medications for low libido in women,12,13 but side effects, medication interactions, limited data in postmenopausal women, and cost make access and use of these medications challenging. Many women are interested in nonpharmaceutical approaches to managing low libido.14 Behavioral interventions, including cognitive behavioral therapy and mindfulness-based interventions,15-20 have been shown to improve sexual desire in women with low libido. Mindfulness is a practice that emphasizes present-moment nonjudgmental bodily awareness. Mindfulness may improve sexual outcomes in women in several ways (Figure 1). Mindfulness has been shown to decrease rumination.21,22 In our prior research, midlife and older women discussed having repetitive, distracting thoughts during sexual activity that impaired their ability to enjoy sexual encounters.23,24 Mindfulness, with its focus on body awareness, may also help women better attend to and experience sexual sensations in the moment.22 This may be particularly pertinent for older women, who can experience decreased genital sensation and physical arousal with aging.4 Because mindfulness encourages nonjudgment, it may also allow women to feel more self-compassion and positivity about their physical bodies, which may have changed with aging.22 This improvement in body image may boost sexual outcomes.25 Finally, mindfulness training frequently includes a discussion of mindful listening,26 which may improve a woman’s ability to communicate effectively with her romantic partner, which can in turn enhance intimacy and bolster sexual outcomes.
Figure 1.
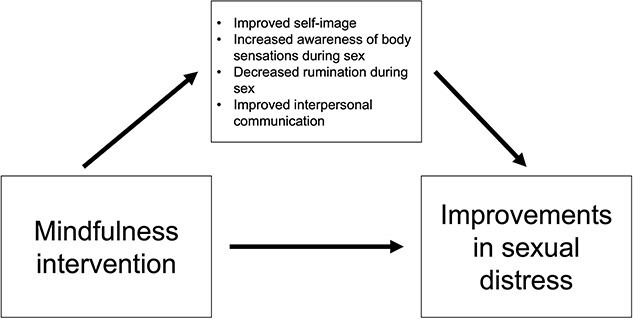
Potential mechanisms for mindfulness effects on sexual outcomes.
However, prior mindfulness interventions have not been tailored to the unique needs of midlife and older women. This population differs from women of other ages; they are more likely to have other chronic health conditions that may affect libido, such as diabetes mellitus or cardiovascular disease. In addition, midlife and older women experience symptoms related to the menopause transition and postmenopause that can affect sexual function, such as sleep disruption, mood symptoms, and vaginal dryness.23,24
Therefore, we adapted an existing mindfulness-based group intervention20 for women with low libido. Using findings from prior qualitative research,11,14,23-25 we adapted an existing mindfulness-based intervention for older women, including more information regarding body image, partner sexual dysfunction, and menopause changes in sexuality. We then conducted a pilot randomized controlled trial of the adapted intervention to assess its feasibility and acceptability as well as to examine, in a preliminary fashion, the initial efficacy of the treatment in improving sexual function and reducing sexual distress. We used a mixed methods approach, involving surveys and qualitative interviews, to assess facilitators and barriers to implementation.
Methods
We recruited participants through multiple methods. Fliers were placed at local internal medicine and gynecology clinics and in community spaces in Pittsburgh, Pennsylvania, United States. Information regarding the study was sent to University of Pittsburgh and UPMC employees via email. The principal investigator partnered with local clinics to facilitate recruitment and referral. Participants were also recruited via Pitt + Me, an electronic registry of individuals who agree to be contacted about studies at the University of Pittsburgh. The study was registered with ClinicalTrials.gov (NCT03232801).
Participants were eligible if they were a cisgender woman aged ≥45 years who (1) screened positive for bothersome low libido based on the Decreased Sexual Desire Screener,27,28 (2) spoke English, and (3) provided informed consent. Women were excluded if they: had inability to perform basic activities of daily living without assistance; elevated depression symptoms (score ≥3 on the Patient Health Questionnaire–2)29; current use of recreational drugs (except for marijuana); consumed >7 alcoholic beverages per week; started a new antidepressant in the prior 3 months; were currently experiencing physical intimate partner violence as measured by the HITS screener30; had high dissatisfaction with their current romantic partner; did not have a current partner with whom they would like to be sexually active; or had high or very high levels of pain with vaginal intercourse (as measured by the sexual pain question on the Female Sexual Function Index [FSFI]). We did not exclude women with other types of chronic pain or other psychiatric disorders. Participants were screened for eligibility over the telephone with a trained research assistant. The University of Pittsburgh Institutional Review Board approved this study, and all participants provided informed consent.
Participants were randomized 1:1 via block randomization according to a computer-generated randomization sequence by the study statistician (J.Y.). Participants were randomized to the experimental or control condition by a trained research assistant. The study principal investigator, study statistician, and mindfulness teacher were not involved in the randomization of participants. Participants who met inclusion criteria and consented to participate were randomized and assigned a group. Masking of participants and group facilitators was not possible, as participants were aware whether they were receiving mindfulness or not, and the teachers were aware whether they were teaching mindfulness or not. The study was originally planned to be face-to-face. However, due to the COVID-19 pandemic, the study was changed to a virtual intervention. Women in both groups participated in groups via video teleconferencing software (Zoom; Zoom Video Communications). Participants were therefore required to have a device capable of using Zoom software and a stable internet connection. A research assistant was available to teach participants to use the software if they did not have prior experience.
The intervention was a 6-session mindfulness-based intervention focused on sexual health and function. Groups met weekly for 2 hours over the course of 6 weeks. Groups were co-led by a primary care physician (the principal investigator) and a trained mindfulness instructor with >10 years of experience in mindfulness meditation instruction. The intervention contained elements of mindfulness-based stress reduction and sexual psychoeducation. Intervention components included instruction in mindfulness meditation, body scan, awareness of breathing, mindful yoga, and loving kindness meditation, as well as application of these practices to sexual function. At least 30 minutes of each session were spent in mindfulness practice. Sessions also consisted of facilitated group discussions and participant-to-participant breakout rooms to facilitate discussions about the mindfulness practices. Based on prior qualitative research,11,23-25 the intervention provided information about partner sexual dysfunction, body image, and how menopause can affect sexuality. Participants were encouraged to do 60 minutes of mindfulness home practice daily and were provided with audio recordings to facilitate it. Home practice included sexuality-specific mindfulness exercises.
The comparator condition was a 6-session health education intervention. Groups met weekly for 2 hours over the course of 6 weeks. Groups were led by a primary care physician (the principal investigator). The education group covered general educational topics relevant to the health of midlife women, such as osteoporosis and heart disease. This content was different from the information in the mindfulness group. Sexual health was discussed in 1 session but not in detail. At the conclusion of their participation, women in the education group were given a brochure with local resources for learning about mindfulness meditation. Participants did not have any homework to complete for this group.
Women completed measures at baseline (time 1), within 1 week of group completion (time 2), and then 5 weeks after group completion (time 3). Measures were self-completed by participants remotely through REDCap software (Research Electronic Data Capture; Vanderbilt University). Email and telephone reminders were sent to patients to complete assessments. A research assistant was made available to conduct measures over the telephone if participants had difficulty with self-completion, but none required assistance. Participants were paid for each questionnaire, for a total of $100 if they completed all questionnaires.
We gathered data on general demographics by self-report. The primary outcomes were feasibility and acceptability of the intervention. Feasibility was defined by the number of screened women who participated and the number of women who completed their group (ie, at least 5 of the 6 sessions). Acceptability was assessed by 2 questions with a 5-point Likert scale: “How satisfied were you with the group you attended?” (extremely satisfied, very satisfied, moderately satisfied, a little satisfied, not at all satisfied) and “Would you recommend this group to another woman with low libido?” (definitely, probably, maybe, a little, not at all).
Prespecified exploratory outcomes included sexual function, as assessed by the FSFI total score. The FSFI is a 19-item measure that assesses female sexual function across 6 domains (desire, arousal, lubrication, orgasm, satisfaction, and pain). The total score ranges from 2 to 36, with higher scores indicating better sexual function. The FSFI was previously validated.31 It should be noted that the FSFI evaluates sexual function over the prior 4 weeks; as noted, a diagnosis of sexual dysfunction requires recurrence or persistence of symptoms for 6 months. Another prespecified exploratory outcome was sexual distress, as assessed by the Female Sexual Distress Scale–Revised (FSDS-R). The FSDS-R is a 13-item scale that measures clinical distress related to female sexual dysfunction, including low desire, such that higher scores denote more sex-related distress. The FSDS-R was previously validated.32
To understand barriers to participation in groups, we conducted brief telephone interviews with a portion of the women who were enrolled and randomized to groups but chose not to participate (n = 9, total; n = 7, mindfulness; n = 2, education). The aim was to gather data regarding reasons for nonparticipation and to assess what adaptations could be applied in future research to enhance participation and retention. Interviews lasted approximately 10 minutes and were conducted by the principal investigator. Interviews were audio recorded and transcribed. The principal investigator developed a codebook based on an initial reading of the interviews and then applied codes to all data. The codes were examined to identify key themes.
To understand how satisfied participants were with the mindfulness and education arms, we completed qualitative interviews via video teleconference with women after they finished attending their groups (n = 25, total; n = 10, mindfulness; n = 15, education). At the final group session, all participants were given the option to participate in a follow-up interview. Interviews were conducted by an experienced qualitative research specialist who did not have other involvement in the study. Interviews were guided by a semistructured interview guide. For data collection and analysis, we used a thematic approach rooted in phenomenology (ie, emphasis on participants’ perceptions and experiences).33 Questions evaluated what participants liked and did not like about the study process and the groups; what they would change about the study process or the groups; and what impact, if any, the group had on their lives. Interviews lasted about 30 minutes. Interviews were audio recorded and transcribed, and then a codebook was developed inductively by 2 investigators (the interviewer and the principal investigator). Codes were applied to all data and then grouped into those with similar subthemes. From these subthemes, broader key themes were identified.
Data were examined for missingness and outliers. Means, standard deviations, and percentages were calculated. Chi-square tests were used to compare proportions between the mindfulness and education groups at time 2 (group completion). Two-tailed t-tests were used to compare mean scores on sexual function and distress outcomes between time 1 and time 3 (week 12). We chose the 12-week time point for the FSFI and FSDS-R because these measures ask participants to reflect on their experiences over the prior 4 weeks. Conducting these measures 5 weeks after group completion would give time for the mindfulness group to implement the home practices in their lives, and we were interested in capturing this in our outcomes. We also constructed mixed effects multilinear regression models, including group, time, and group × time effects, to examine changes in sexual outcomes over time. P < .05 was considered statistically significant. Only women who had time 2 data were included in analyses of satisfaction and likelihood of recommending their groups. Only women who had time 3 data were included in analyses of sexual function and sexual distress. All analyses were conducted with Stata 16 (StataCorp).
Results
Eighty-one women were screened and 20 were excluded (Figure 2). The most common reasons for exclusion were high sexual pain (n = 9) and severe depression symptoms (n = 5). Other reasons for exclusion were high relationship dissatisfaction (n = 3), heavy alcohol use (n = 1), and no current sexual partner (n = 1). Sixty-one women were randomized: 31 to mindfulness and 30 to education. Of these, 18 women in the mindfulness group and 23 in the education group attended at least 1 group session. After group conclusion, 15 women in the mindfulness group and 22 in the education group completed outcome measures at time 2. Women who completed time 1 measures but did not outcome measures tended to be younger (P = .034) and had more difficulty paying for basics (P = .045). There were no differences in completion based on race, ethnicity, relationship status, history of intimate partner violence, education, or baseline FSFI or FSDS-R scores.
Figure 2.
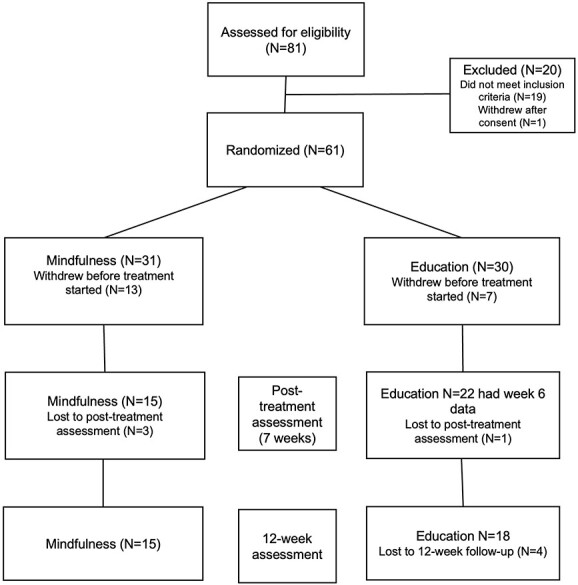
CONSORT diagram of pilot randomized controlled trial of mindfulness for older women with low libido.
The demographics of women who were randomized are seen in Table 1. The mean age was 57 years, and the majority were non-Hispanic White, although Hispanic, Black, multiracial, and Asian women were represented. Most women (98%) had college education or higher and self-identified as heterosexual. Most (84%) were currently married or cohabitating with a partner, and 85% had not used hormone therapy in the last 3 months. Twenty-four percent of women had a hysterectomy or bilateral oophorectomy, and 67% of those without a hysterectomy or oophorectomy were postmenopausal.
Table 1.
Baseline data for all women randomized.
| Participants, No. (%) | |||
|---|---|---|---|
| Mindfulness | Education | Overall | |
| Age, y, mean (SD; range) | 55.9 (7.1; 45-71) | 55.7 (7.5; 47-76) | 55.8 (7.3; 45-76) |
| Ethnicity | |||
| Hispanic/Latina/Latinx | 1 (4) | 0 (0) | 1 (2) |
| Not Hispanic/Latina/Latinx | 27 (96) | 27 (100) | 54 (98) |
| Primary race | |||
| White | 20 (71) | 24 (89) | 44 (80) |
| African American/Black | 2 (7) | 3 (11) | 5 (9) |
| Asian | 3 (11) | 0 (0) | 3 (5) |
| >1 race | 3 (11) | 0 (0) | 3 (5) |
| Education | |||
| High school or less | 0 | 1 (4) | 1 (2) |
| Some college or graduated college | 13 (46) | 13 (48) | 26 (47) |
| Some professional school or degree | 15 (54) | 13 (48) | 28 (51) |
| Difficulty paying for basics | |||
| No | 26 (93) | 23 (85) | 49 (89) |
| Yes | 2 (7) | 4 (15) | 6 (11) |
| Current marital status | |||
| Married/cohabitating | 24 (86) | 22 (81) | 46 (84) |
| Divorced/separated | 3 (11) | 5 (19) | 8 (15) |
| Never married | 1 (4) | 0 (0) | 1 (2) |
| Hormone therapy use in the past 3 mo | |||
| No | 23 (85) | 22 (85) | 45 (85) |
| Yes | 4 (15) | 4 (15) | 8 (15) |
| Started a new antidepressant medication in the past 3 mo | |||
| No | 17 (63) | 16 (62) | 33 (62) |
| Yes | 10 (37) | 10 (38) | 20 (38) |
| Menopause status | |||
| Pre- or perimenopausal | 1 (4) | 3 (14) | 4 (9) |
| Postmenopausal | 15 (65) | 15 (68) | 30 (67) |
| Hysterectomy or oophorectomy | 7 (30) | 4 (18) | 11 (24) |
| History of sexual assault | |||
| No | 15 (56) | 19 (73) | 34 (64) |
| Yes | 12 (44) | 7 (27) | 19 (36) |
| History of physical/emotional abuse from a romantic partner | |||
| No | 17 (63) | 17 (65) | 34 (64) |
| Yes | 10 (37) | 9 (35) | 19 (36) |
Among the women who attended at least 1 session (n = 41), 37 (90%) completed the mindfulness intervention. Completion rates were not different between the groups (83% mindfulness vs 95% education, P = .163). Women in both groups reported high satisfaction with the group (Figure 2), and there were no differences in satisfaction by group assignment (P = .244). In the mindfulness group, 7% were not at all or a little satisfied, 20% were moderately satisfied, and 73% were very or extremely satisfied. A larger proportion of women in the mindfulness group reported that they would recommend the group to another woman with low libido as compared with women in the education group (P = .031). In the mindfulness group, 0% of women said that they would not recommend it at all or would recommend it only a little; 33% said that they might recommend it; and 67% said that they would probably or definitely recommend it.
Women in both groups had nonsignificant changes in overall sexual function from time 1 to time 3 (mean FSFI score, 22.6 to 18.6 [P = .101] in the mindfulness group and 21.2 to 19.7 [P = .537] in the education group; Table 2). The group × time interaction term for sexual function was nonsignificant (P = .097).
Table 2.
Exploratory sexual outcomes.
| Mean (SD) | ||||
|---|---|---|---|---|
| Outcome: group | Time 1 | Time 3 | Change | P value * |
| Sexual function: FSFIa | .097 | |||
| Mindfulness (n = 15) | 22.6 (6.4) | 18.6 (6.4) | 4.0 (5.1) | |
| Education (n = 18) | 21.2 (7.5) | 19.7 (7.5) | 1.5 (3.1) | |
| Sexual distress: FSDS-Rb | .085 | |||
| Mindfulness (n = 15) | 27.1 (10.0) | 20.0 (11.0) | 7.4 (7.6) | |
| Education (n = 18) | 19.1 (6.9) | 15.3 (6.8) | 3.1 (7.3) | |
Abbreviations: FSDS-R, Female Sexual Distress Scale–Revised; FSFI, Female Sexual Function Index.
FSFI: range of possible scores, 2-36.
FSDS-R: range of possible scores, 0-52.
P value for group × time interaction term in multivariable mixed effects models.
Women in the mindfulness group had significant improvements in sexual distress from time 1 to time 3 (mean FSDS-R score, 27.1 to 19.7; P = .021). Women in the education group had improvements in sexual distress that did not reach statistical significance (19.1 to 15.8, P = .062). The group × time interaction term for sexual distress was nonsignificant (P = .085).
Women randomized to the mindfulness group were more likely to have a history of sexual assault as compared with women in the education group (66% vs 32%; P = .037). When limited to women with a sexual assault history, those in the mindfulness group had higher sexual distress at time 1 than those in the education group (FSDS-R score, 30.1 vs 19.0; P = .009). Women who had a history of sexual assault and were assigned to mindfulness had greater improvements in sexual distress (mean FSDS-R, 30.1 to 21.0; P = .052) than women with a history of sexual assault who were assigned to education (19.0 to 18.8; P = .927).
Two women in the mindfulness group described feeling some emotional distress in relation to discussing sensitive topics (relationships, sexuality) that they did not usually spend as much time considering. These women were offered mental health resources, including local resources for obtaining individual psychotherapy.
We conducted 9 telephone interviews with women who were randomized but did not participate in any sessions. Women in these interviews were randomized to mindfulness as well as education. The majority stated that they were highly interested but were not able to participate due to time conflicts. Other reasons for not participating included not having a private space in which to participate and feeling uncomfortable about the idea of discussing sexuality in a group.
We conducted 25 interviews with women who participated in the study (11 from mindfulness, 14 from education; Table 3). Women in both groups reported that they appreciated sharing with a group of peers, which led to a sense of community and feeling less alone with regard to the menopause experience. Women in the mindfulness group discussed having a greater sense of present-moment awareness in everyday life after participating. Women in the mindfulness group also reported positive changes in mood and sexuality that they experienced as a result of participating. Women did recommend some changes to the study procedures and groups. They requested a more detailed orientation process to ensure a clear understanding of what the groups would entail prior to participation. Many women felt that the groups should have been longer (eg, 8 weeks instead of 6 weeks).
Table 3.
Qualitative data from women who participated in their assigned group.
| Women appreciated the group aspect, especially given pandemic-related social isolation, as it normalized the menopause experience | So just having a group of women that I could talk to and relate to, that was a really good thing for me during the pandemic. I definitely got to know a little bit about that. I’m not the only one going through menopause. I’m not the only one who doesn’t want to have sex. I’m not the only one in pain. We found out some fears about some people and the pandemic about being alone. | 53-y-old Black woman, postmenopausal, educational group |
| I liked coming together as a group. It made me look forward to it. I made time for it for myself, which doesn’t usually happen. Everybody put a little bit out there about their own relationships and you could relate. I’m not the only one going through this. That was probably the most helpful. And just being allowed to explore and not feel like you’re being looked down upon. Other people felt the same way I did. It was like, permission to try this or do that. Just having that push to go ahead and try it and that other people had the same kind of standoffish concerns was encouraging that okay, I can do this. I’m not abnormal. | 53-y-old White woman, history of bilateral oophorectomy, mindfulness group | |
| Women experienced positive outcomes from the intervention rooted in mindfulness principles and improved communication | I’m more in the moment. It used to be, when my husband made advances, I was always thinking, “I wish you would pick this up today and why didn’t you do that, and why are you touching me like that when I told you to do it like this,” and all of a sudden, it just went. I was totally focused in the moment without any distractions from the past or expectations of the moment. I was in the moment and that kind of brought me back to almost dating because, you know, when you’ve been married so long, everything is the same. But it put me back in the wonder of the touch when you’re dating in your early times. | 61-y-old White woman, postmenopausal, mindfulness group |
| I feel on a lot closer to my husband. There was a time where he’d come and touch me and I would flinch and I had a hard time with that. But now I’m more relaxed around him. We’re doing more together, we’re talking more, and I think that was the biggest thing. I think since my husband and I have gotten a little bit past some of the communication, and we’re being more affectionate towards each other. And that doesn’t always lead to sex, but at least we’re touching each other and being closer. | 67-y-old White woman, history of bilateral oophorectomy, mindfulness group |
Discussion
We conducted a pilot randomized controlled trial of a group-based mindfulness intervention for midlife and older women with low libido. Women reported high satisfaction with both the mindfulness and education groups. The majority of women in the mindfulness group would recommend it to another woman with low libido, and the proportion of women who would recommend it was higher than the educational group. This study was not powered to detect differences in sexual function and sexual distress; however, exploratory analyses showed that women in the mindfulness group had significant improvements in sexual function and reductions in sexual distress, while women in the educational group did not. In follow-up interviews, women randomized to mindfulness expressed higher present-moment awareness during sexual activity, which led to better overall sexual satisfaction.
Women in the mindfulness group experienced significant improvements in sexual function and sexual distress. Mindfulness may improve these parameters by various mechanisms. Prior research has suggested that mental distraction, rumination, and self-spectatoring during sexual activity can decrease sexual arousal,22,34,35 which leads to less pleasurable sexual encounters and an overall decrease in sexual desire. Mindfulness training may allow women to be more mentally “present” and more aware of their bodily sensations during sexual activity (also called interoceptive awareness), thereby enhancing arousal and in turn satisfaction and desire.22 A recently published study of mechanisms of mindfulness in a randomized controlled trial found that self-compassion, interoceptive awareness, self-criticism, mindfulness, and depression symptoms mediated the relationship between assignment to the mindfulness group and improvements in sexual outcomes.36 In our qualitative follow-up interviews, women did endorse these mechanisms. Mindfulness may also lead to improvements in body image, communication with one’s romantic partner, sleep, and mood, which in turn contribute to enhanced libido.22 Larger studies are necessary to more deeply explore the mechanisms by which mindfulness affects sexual function and satisfaction.
In this pilot trial, we found improvements in sexual distress but not in sexual function. Sexual function, especially as measured by the FSFI, places much emphasis on the physical aspects of sexuality, such as the ability to become lubricated or the ease of reaching orgasm. In contrast, sexual distress typically focuses on the degree to which sexual symptoms bother or cause negative impacts in the life of the respondent. Sexual distress places more emphasis on how an individual responds to deficits or changes in sexual function. Mindfulness may be more likely to exert effects on a person’s response to changes in one’s sexuality (ie, sexual distress), as opposed to improvements in physical sexual function. The distinction between function and distress may be particularly pertinent in aging women. Many women experience changes in physical sexual function with aging, such as vaginal dryness, but those who are able to adapt their sexual behavior or their thinking in response to these changes are more likely to maintain high sexual satisfaction with aging.24
A considerable number of women in this pilot study who originally agreed to participate were not able to attend. Most did not attend due to scheduling conflicts. One way to mitigate low group initiation after enrollment would be to set a day and time for the group intervention prior to randomization. In this study, we selected the day and time of the intervention after randomization. Another way to mitigate this complication is to ensure that orientation and informed consent are thorough and robust so that participants fully understand the nature of the study and the time commitment prior to randomization. A future study could employ a method such as video or electronic interactive informed consent with a knowledge check. Over 90% of women who attended at least 1 session completed their group.
We explored outcomes among women with a history of sexual assault and found that such women who participated in the mindfulness group had the largest improvements in sexual distress. In a prior study of a mindfulness intervention for women with sexual arousal disorders, women with a history of sexual abuse improved more than women without this history.37 This study was not large enough to test interactions between sexual assault history and group assignment. These interactions between sexual assault history and treatment effects could be explored in a larger study. It is important for any intervention of this nature to use a trauma-informed approach with an experienced facilitator to ensure that women with a history of sexual assault are supported.38
Women in this study felt positive about participating in a group intervention over Zoom. They appreciated the connections and sense of belonging that they had in the group. They were glad that the group was able to meet despite the COVID-19 pandemic. A few women stated that they would have preferred face-to-face group meetings, but most actually preferred virtual meeting, citing convenience and comfort of joining from home. It should be noted that a few women who were not able to participate noted that they had no private space at home in which to participate in a virtual meeting that discussed sensitive issues. Technological difficulties were rare, and women reported high satisfaction with the virtual meetings as well as the virtual follow-up data collection. Future studies on sexual function should compare the efficacy of face-to-face and virtual interventions.
This study has limitations. As this is a pilot study, the sample size is small, and the study is not powered to detect differences in sexual function outcomes. As previously discussed, the number of women who were enrolled but did not participate was high. Although the primary sexual concern was low sexual desire, we used a generic measure of overall sexual function that may have limited the improvements that participants experienced to their sexual desire. The majority of participants were White and college educated. The control group did not receive the same sexuality education group as the mindfulness group. It is possible that if the education group received education on sexuality, it would have had greater satisfaction with the group and less sexual distress. The research question for this study focused on how the mindfulness intervention, as a package that includes psychoeducation on sexuality, affects sexual outcomes while controlling for potential therapeutic effects of attention from a facilitator and participation in a discussion group with peers. There have been studies that tested mindfulness interventions against psychoeducation on sexuality specifically.20 This study also has strengths. We used an active comparator group, as opposed to a wait-list control or usual care. The use of a virtual intervention is novel.
Conclusion
This pilot study revealed that a group-based mindfulness intervention for midlife and older women with low libido is feasible and acceptable and may result in improvements in sexual distress. A fully powered randomized controlled trial is recommended to confirm efficacy and explore mechanisms.
Author contributions
H.N.T.: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, resources, visualization, writing–original draft, writing–review and editing. L.A.B.: conceptualization, formal analysis, methodology, resources, writing–review and editing. F.A.C.: data curation, methodology, writing–review and editing. J.Y.: formal analysis, methodology, writing–review and editing. R.C.T.: conceptualization, formal analysis, funding acquisition, investigation, methodology, resources, supervision, writing–review and editing.
Funding
This study was funded by a grant from the National Institute of Health’s (NIH’s) National Institute on Aging (K23AG052628). Rebecca C. Thurston is supported by a grant from the NIH’s National Heart Lung and Blood Institute (K24HL123565). This study used the Pitt + Me research registry, which is a program of the University of Pittsburgh Clinical and Translational Science Institute (CTSI). The University of Pittsburgh CTSI is supported by the NIH’s Clinical and Translational Science Award program (U1TR001857).
Conflicts of interest
None declared.
Data availability
The data that support the findings of this study are available from the corresponding author, Holly N. Thomas, upon reasonable request.
Contributor Information
Holly N Thomas, Department of Medicine, University of Pittsburgh, Pittsburgh, PA 15217, United States.
Lori A Brotto, Department of Obstetrics and Gynecology, University of British Columbia, Vancouver V5Z 4M2, Canada.
Flor de Abril Cameron, Department of Medicine, University of Pittsburgh, Pittsburgh, PA 15217, United States.
Jonathan Yabes, Department of Medicine, University of Pittsburgh, Pittsburgh, PA 15217, United States.
Rebecca C Thurston, Department of Psychiatry, University of Pittsburgh, Pittsburgh, PA 15217, United States.
References
- 1. Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008;112(5):970–978. 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 2. Mitchell KR, Mercer CH, Ploubidis GB, et al. Sexual function in Britain: findings from the Third National Survey of Sexual Attitudes and Lifestyles (NATSAL-3). Lancet. 2013;382(9907):1817–1829. 10.1016/S0140-6736(13)62366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American Psychiatric Association ed. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 4. Thomas HN, Thurston RC. A biopsychosocial approach to women’s sexual function and dysfunction at midlife: a narrative review. Maturitas. 2016;87:49–60. 10.1016/j.maturitas.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Quinn-Nilas C, Milhausen RR, McKay A, Holzapfel S. Prevalence and predictors of sexual problems among midlife Canadian adults: results from a national survey. J Sex Med. 2018;15(6):873–879. 10.1016/j.jsxm.2018.03.086. [DOI] [PubMed] [Google Scholar]
- 6. Avis NE, Zhao X, Johannes CB, Ory M, Brockwell S, Greendale GA. Correlates of sexual function among multi-ethnic middle-aged women: results from the Study of Women’s Health Across the Nation (SWAN). Menopause. 2005;12(4):385–398. 10.1097/01.GME.0000151656.92317.A9. [DOI] [PubMed] [Google Scholar]
- 7. Woods NF, Mitchell ES, Smith-Di Julio K. Sexual desire during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. J Womens Health (Larchmt). 2010;19(2):209–218. 10.1089/jwh.2009.1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ventegodt S. Sex and the quality of life in Denmark. Arch Sex Behav. 1998;27(3):295–307. [DOI] [PubMed] [Google Scholar]
- 9. Biddle AK, West SL, D’Aloisio AA, Wheeler SB, Borisov NN, Thorp J. Hypoactive sexual desire disorder in postmenopausal women: quality of life and health burden. Value Health. 2009;12(5):763–772. 10.1111/j.1524-4733.2008.00483.x. [DOI] [PubMed] [Google Scholar]
- 10. Leiblum SR, Koochaki PE, Rodenberg CA, Barton IP, Rosen RC. Hypoactive sexual desire disorder in postmenopausal women: US results from the Women’s International Study of Health and Sexuality (WISHeS). Menopause. 2006;13(1):46–56. 10.1097/01.gme.0000172596.76272.06. [DOI] [PubMed] [Google Scholar]
- 11. Thomas HM, Hamm M, Krishnamurti T, Hess R, Borrero S, Thurston RC. “How much desire should I have?” A qualitative study of low libido in postmenopausal women. J Women Aging. 2021;34(5):649–657. 10.1080/08952841.2021.1977070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jaspers L, Feys F, Bramer WM, Franco OH, Leusink P, Laan ET. Efficacy and safety of flibanserin for the treatment of hypoactive sexual desire disorder in women: a systematic review and meta-analysis. JAMA Intern Med. 2016;176(4):453–462. 10.1001/jamainternmed.2015.8565. [DOI] [PubMed] [Google Scholar]
- 13. Kingsberg SA, Clayton AH, Portman D, et al. Bremelanotide for the treatment of hypoactive sexual desire disorder: two randomized phase 3 trials. Obstet Gynecol. 2019;134(5):899–908. 10.1097/AOG.0000000000003500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thomas HN, Hamm M, Hess R, Borrero S, Thurston RC. Patient-centered outcomes and treatment preferences regarding sexual problems: a qualitative study among midlife women. J Sex Med. 2017;14(8):1011–1017. 10.1016/j.jsxm.2017.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brotto LA, Basson R. Group mindfulness-based therapy significantly improves sexual desire in women. Behav Res Ther. 2014;57:43–54. 10.1016/j.brat.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 16. Brotto LA, Bergeron S, Zdaniuk B, Basson R. Mindfulness and cognitive behavior therapy for provoked vestibulodynia: mediators of treatment outcome and long-term effects. J Consult Clin Psychol. 2020;88(1):48–64. 10.1037/ccp0000473. [DOI] [PubMed] [Google Scholar]
- 17. Brotto LA, Bergeron S, Zdaniuk B, et al. A comparison of mindfulness-based cognitive therapy vs cognitive behavioral therapy for the treatment of provoked vestibulodynia in a hospital clinic setting. J Sex Med. 2019;16(6):909–923. 10.1016/j.jsxm.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 18. Brotto LA, Erskine Y, Carey M, et al. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol Oncol. 2012;125(2):320–325. 10.1016/j.ygyno.2012.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brotto LA, Seal BN, Rellini A. Pilot study of a brief cognitive behavioral versus mindfulness-based intervention for women with sexual distress and a history of childhood sexual abuse. J Sex Marital Ther. 2012;38(1):1–27. 10.1080/0092623X.2011.569636. [DOI] [PubMed] [Google Scholar]
- 20. Brotto LA, Zdaniuk B, Chivers ML, et al. A randomized trial comparing group mindfulness-based cognitive therapy with group supportive sex education and therapy for the treatment of female sexual interest/arousal disorder. J Consult Clin Psychol. 2021;89(7):626–639. 10.1037/ccp0000661. [DOI] [PubMed] [Google Scholar]
- 21. Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1–12. 10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 22. Arora N, Brotto LA. How does paying attention improve sexual functioning in women? A review of mechanisms. Sex Med Rev. 2017;5(3):266–274. 10.1016/j.sxmr.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 23. Thomas HN, Hamm M, Hess R, Borrero S, Thurston RC. “I want to feel like I used to feel”: a qualitative study of causes of low libido in postmenopausal women. Menopause. 2020;27(3):289–294. 10.1097/GME.0000000000001455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thomas HN, Hamm M, Hess R, Thurston RC. Changes in sexual function among midlife women: “I’m older . . . and I’m wiser.”. Menopause. 2018;25(3):286–292. 10.1097/GME.0000000000000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Thomas HN, Hamm M, Borrero S, Hess R, Thurston RC. Body image, attractiveness, and sexual satisfaction among midlife women: a qualitative study. J Womens Health (Larchmt). 2019;28(1):100–106. 10.1089/jwh.2018.7107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kabat-Zinn J. Mindfulness-based stress reduction (MBSR). Constructivism in the Human Sciences. 2003;8(2):73–107. [Google Scholar]
- 27. Clayton AH, Goldfischer ER, Goldstein I, Derogatis L, Lewis-D’Agostino DJ, Pyke R. Validation of the Decreased Sexual Desire Screener (DSDS): a brief diagnostic instrument for generalized acquired female hypoactive sexual desire disorder (HSDD). J Sex Med. 2009;6(3):730–738. 10.1111/j.1743-6109.2008.01153.x. [DOI] [PubMed] [Google Scholar]
- 28. Clayton AH, Goldfischer E, Goldstein I, et al. Validity of the decreased sexual desire screener for diagnosing hypoactive sexual desire disorder. J Sex Marital Ther. 2013;39(2):132–143. 10.1080/0092623X.2011.606496. [DOI] [PubMed] [Google Scholar]
- 29. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire–2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 30. Punukollu M. Domestic violence: screening made practical. J Fam Pract. 2003;52(7):537–543. [PubMed] [Google Scholar]
- 31. Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208. 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 32. Derogatis L, Clayton A, Lewis-D’Agostino D, Wunderlich G, Fu Y. Validation of the Female Sexual Distress Scale–Revised for assessing distress in women with hypoactive sexual desire disorder. J Sex Med. 2008;5(2):357–364. 10.1111/j.1743-6109.2007.00672.x. [DOI] [PubMed] [Google Scholar]
- 33. Crabtree BF, Miller WL. Doing Qualitative Research. 3rd ed. Sage Publications; 2022. [Google Scholar]
- 34. Pascoal PM, Raposo CF, Roberto MS. A transdiagnostic approach to sexual distress and sexual pleasure: a preliminary mediation study with repetitive negative thinking. Int J Environ Res Public Health. 2020;17(21):7864. 10.3390/ijerph17217864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Carvalheira A, Godinho L, Costa P. The impact of body dissatisfaction on distressing sexual difficulties among men and women: the mediator role of cognitive distraction. J Sex Res. 2017;54(3):331–340. 10.1080/00224499.2016.1168771. [DOI] [PubMed] [Google Scholar]
- 36. Brotto LA, Zdaniuk B, Chivers ML, Jabs F, Grabovac AD, Lalumiere ML. Mindfulness and sex education for sexual interest/arousal disorder: mediators and moderators of treatment outcome. J Sex Res. 2022;60(4):508–521. 10.1080/00224499.2022.2126815. [DOI] [PubMed] [Google Scholar]
- 37. Brotto LA, Basson R, Luria M. A mindfulness-based group psychoeducational intervention targeting sexual arousal disorder in women. J Sex Med. 2008;5(7):1646–1659. 10.1111/j.1743-6109.2008.00850.x. [DOI] [PubMed] [Google Scholar]
- 38. Elliott DE BP, Fallot RD, Markoff LS, Reed BG. Trauma-informed or trauma-denied: principles and implementation of trauma-informed services for women. J Community Psychol. 2005;33(4):461–477. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, Holly N. Thomas, upon reasonable request.


