Abstract
Anterior cruciate ligament (ACL) injuries are common to athletes and non-athletes alike. Whereas the literature has historically supported bone–patellar tendon–bone as the gold standard for active patients who elect to undergo ACL reconstruction, other studies have suggested that soft-tissue grafts do not increase the risk of rerupture. Because graft diameter has a direct effect on revision rates, we share a technique for all-inside ACL reconstruction using quadrupled semitendinosus and gracilis autograft that allows for a predictable, robust graft. Reproducible steps of graft harvesting, tunnel preparation, graft passage, and fixation are shared to achieve a robust anatomic reconstruction.
Technique Video
Intraoperative and supplemental arthroscopic imaging of all-inside anterior cruciate ligament (ACL) reconstruction using quadrupled semitendinosus autograft in left knee. The patient is positioned supine, with the surgeon primarily operating through anteromedial and anterolateral portals.
With an incidence of 100,000 to 200,000 cases per year, anterior cruciate ligament (ACL) injury is far too common. Most active patients are treated with ACL reconstruction (ACLR) surgery with plans to return to preinjury activity levels.1,2 Many studies have compared surgical techniques to minimize the risk of retear and to assess return to sport, long-term anterior knee pain, and increased risk of osteoarthritis.3, 4, 5, 6, 7 The historical gold standard of ACLR graft techniques for many surgeons has been bone–patellar tendon–bone (BPTB) as the literature has shown that the risk of retear in young patients and elite, contact sport athletes is minimized.3,8 However, other studies have shown that there are no differences in graft rupture when comparing BPTB with soft-tissue grafts such as hamstring tendon graft.4 The aim of this technical note is to describe a technique for graft preparation and ACLR to ensure an adequate graft diameter when using hamstring autograft.9, 10, 11 We share various tips and pearls to achieve successful all-inside ACLR using quadrupled semitendinosus and gracilis. Details of graft harvest, tunnel preparation, graft passage, and fixation are shared to achieve a robust anatomic reconstruction.
Surgical Technique
Patient Positioning and Preparation
At the time of surgery, the patient is placed supine and a thigh tourniquet is applied. The operative leg is prepared and draped in a sterile fashion. A leg holder or post can be used per the usual ACLR setup.
Graft Harvest and Preparation
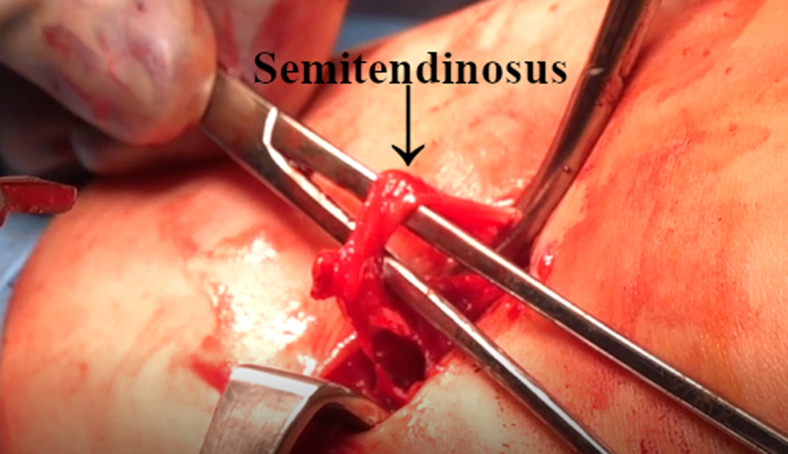
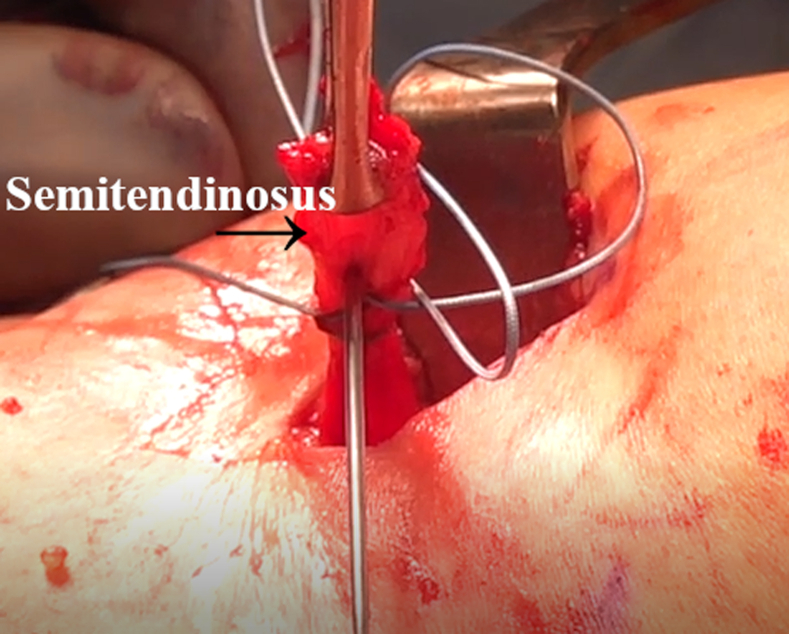
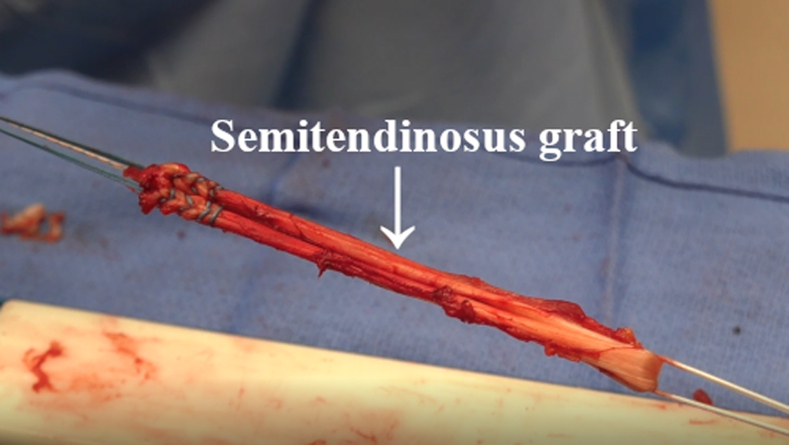
A small incision (approximately 2-3 cm) is centered over the pes anserinus tendons. The incision is carried down through the skin and the subcutaneous tissue. Both the semitendinosus and gracilis tendons are identified. The semitendinosus is released from the tibial attachment site (Fig 1). A looped suture is placed in the distal 1 to 2 cm of the tendon (Fig 2). All fascial bands are released with care taken to ensure that the band to the gastrocnemius muscle is released. A tendon stripper is used to harvest the semitendinosus, which is then passed off to the back table. A similar technique is used to harvest the gracilis tendon. The tendons are cleaned and trimmed to a length of 230 to 280 mm depending on the size of the patient and the desired quadrupled graft length.
Fig 1.
Intraoperative image of left knee from medial viewpoint. After careful dissection at the pes anserine, the semitendinosus tendon is resected from the tibial insertion.
Fig 2.
Intraoperative image of left knee from medial viewpoint. After release from its insertion, the semitendinosus tendon is harvested with a tendon stripper.
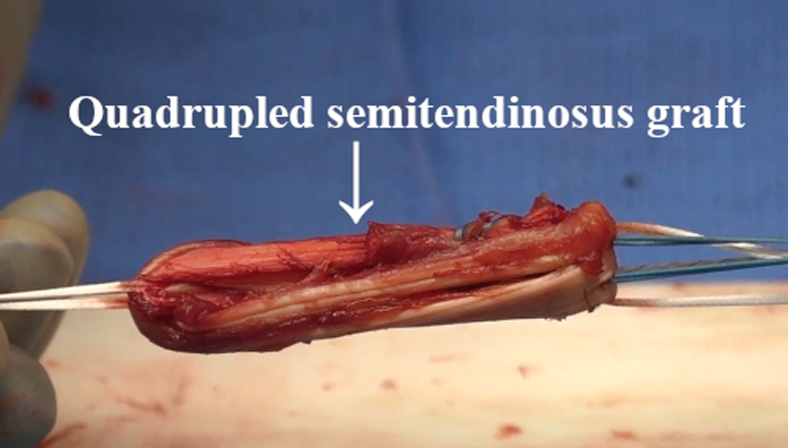
Adjustable suspensory buttons (TightRope RT; Arthrex) are loaded onto the graft preparation board (Graftmaster; Arthrex). The harvested tendons are passed through the adjustable suspensory button loop, and the tail ends from both the semitendinosus and gracilis are sutured together using a looped suture (Fig 3). The graft is then quadrupled, and the tail ends are tucked into the graft using the needle of the looped sutures (Fig 4). Care is taken to make sure the cortical button fixation suture loop is not pierced.
Fig 3.
Intraoperative image of graft preparation on back table. The harvested semitendinosus tendon is passed through a TightRope loop, and the tail ends are tied together with looped suture.
Fig 4.
Intraoperative image of graft preparation on back table. The semitendinosus graft is quadrupled by folding twice, and the tail ends are secured with looped suture.
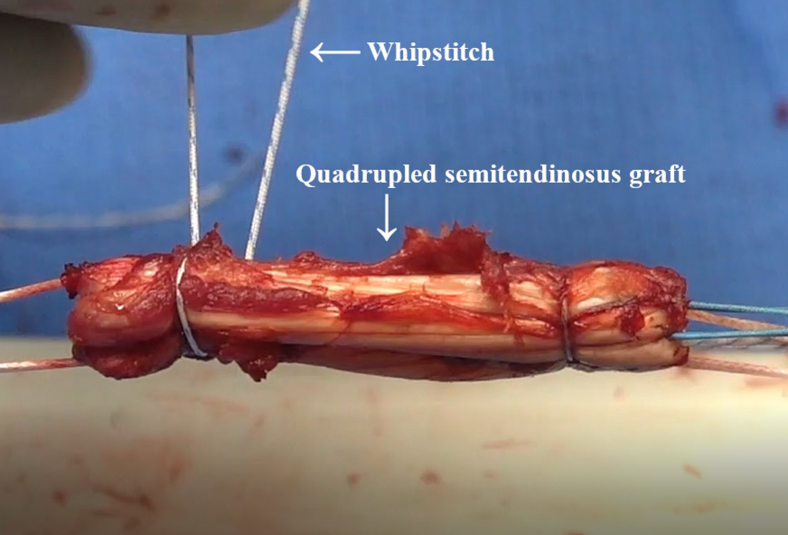
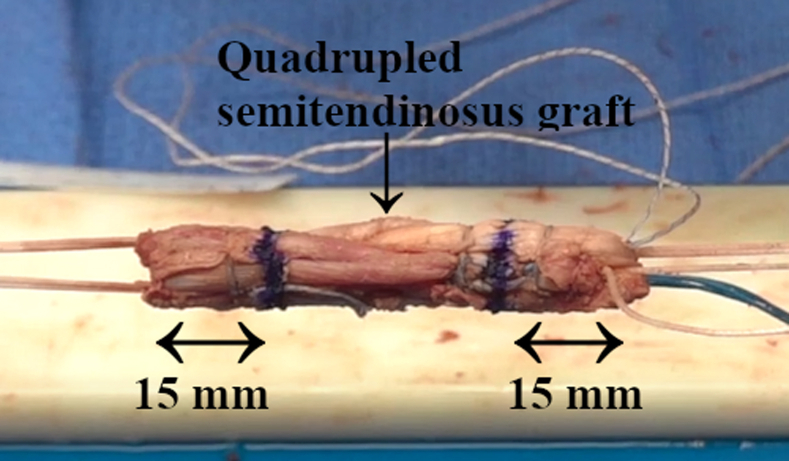
Next, wrapped whipstitch sutures are passed around the quadrupled graft construct (Fig 5). This can be repeated 4 times (2 wrapped sutures on each end, approximately 1 cm apart) with a buried-knot technique. At this point, by use of the Graft Sizing Block (Arthrex), the graft diameter can be checked, which should be a minimum of 9 mm. The graft is wrapped in a vancomycin-soaked sponge and placed in 10 to 15 lb of tension.12
Fig 5.
Intraoperative image of graft preparation on back table. Whipstitch sutures are passed through the quadrupled semitendinosus graft, and the knots are buried. This step can be performed twice on each side of the graft prior to final measurement.
Diagnostic Arthroscopy
A standard diagnostic knee arthroscopy is performed using anterolateral (AL) and anteromedial (AM) portals. All intra-articular pathology of the menisci and cartilage is addressed. The torn ACL fibers are debrided, and the femoral wall is prepared with an arthroscopic shaver and radiofrequency probe as indicated.
Anatomic Femoral Tunnel Preparation
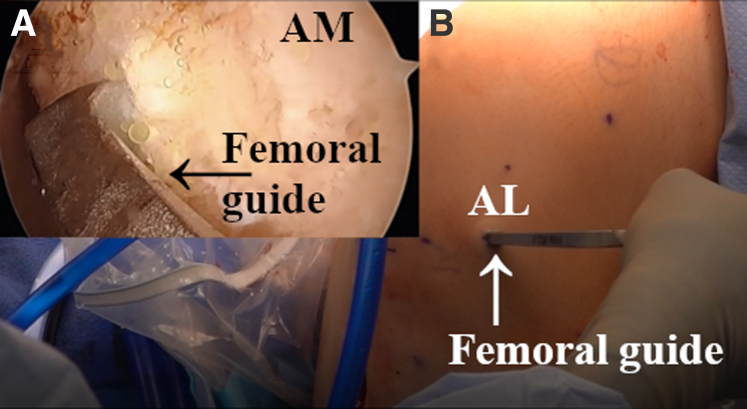
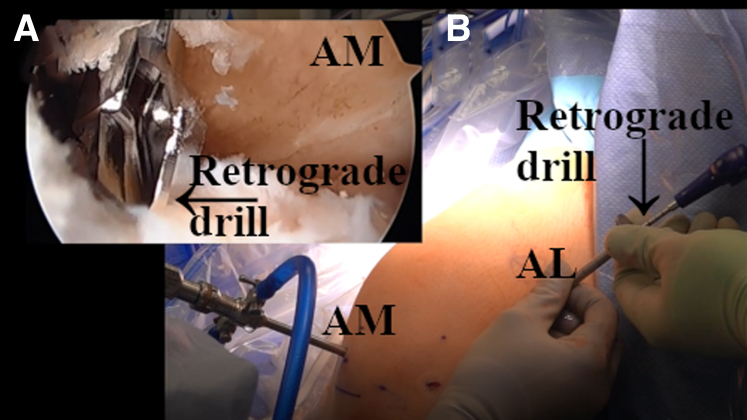
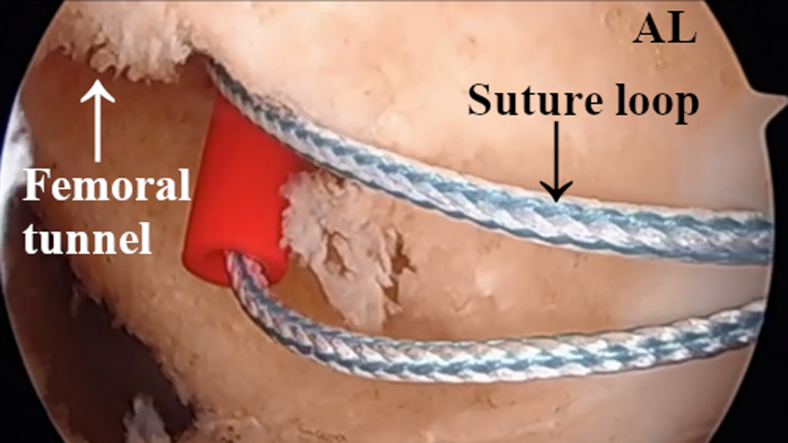
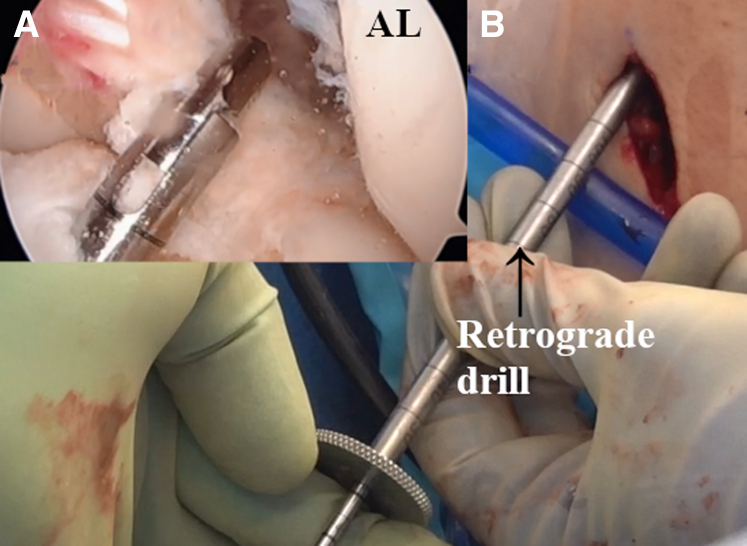
The arthroscope is placed into the AM portal with the outside-in femoral guide (Footprint Femoral Guide; Arthrex) placed into the AL portal and usually set at 105° to 110° (Fig 6). The guide is placed into the anatomic ACL footprint. A retrograde drill–reamer (FlipCutter; Arthrex) with a diameter equal to that of the graft is used to create the femoral tunnel. The tunnel length is usually 25 to 35 mm depending on the size of the patient. Care is taken to preserve the cortex (Fig 7). The arthroscopic shaver is used to ensure all loose debris is removed from the knee. A looped passing suture or FiberStick (Arthrex) is passed through the femoral tunnel for later graft passage (Fig 8). The looped suture is not pulled out of the AL portal until after tibial tunnel preparation is complete.
Fig 6.
(A) Arthroscopic image of left knee through anteromedial (AM) portal. (B) Intraoperative image of left knee from anterolateral (AL) viewpoint. With the knee flexed to 105° to 110°, an outside-in femoral guide is placed through the AL portal onto the anterior cruciate ligament footprint.
Fig 7.
(A) Arthroscopic image of left knee through anteromedial (AM) portal. (B) Intraoperative image of left knee from anterolateral (AL) viewpoint. A retrograde drill is inserted through the AL portal, and a 30-mm-long femoral tunnel is made. The flipped end of the drill has a diameter equal to that of the graft.
Fig 8.
Arthroscopic image of left knee through anterolateral (AL) portal. In preparation for later graft passage, a suture loop is passed through the femoral tunnel.
The arthroscope is placed back into the AL portal, and the tibial guide (Tibial ACL Marking Hook for RetroConstruction Drill Guide; Arthrex) is placed through the AM portal and set at 55° to 60°. The same retrograde drill is used to create the tibial tunnel to a desired length of usually 35 to 45 mm (Fig 9). Care is again taken to preserve the tibial cortex for cortical button (TightRope RT) fixation. The arthroscopic shaver is again used to remove loose debris from the knee. Another looped passing suture or FiberStick is passed through the tibial tunnel. It is important to note that the femoral and tibial tunnel lengths plus approximately 25 mm for the ACL should measure at least 10 mm longer than the graft length to ensure that the graft can be tensioned completely and not bottom out (Table 1).
Fig 9.
(A) Arthroscopic image of left knee through anterolateral (AL) portal. (B) Intraoperative image of left knee from anterior viewpoint. A retrograde drill is placed through a separate incision at the medial aspect of the tibial tubercle for drilling of the tibial tunnel.
Table 1.
Pearls and Pitfalls
| Step | Pearl | Pitfall |
|---|---|---|
| Marking of graft 15 mm from femoral and tibial ends | Marking will ensure a minimum of 15 mm of graft into the femoral and tibial tunnels. | Failure to mark the graft ends may increase the risk of having too much graft in one tunnel and too little graft in the other. |
| “Triple T lengthening” | The tibial cortical looped suture–TightRope should be lengthened prior to removing the graft and looped cortical buttons from the post to ensure that the suspensory button is long enough to pass outside the tibial tunnel. | Failure to lengthen the cortical looped suture–TightRope may result in the suspensory button becoming stuck in the tibial tunnel. |
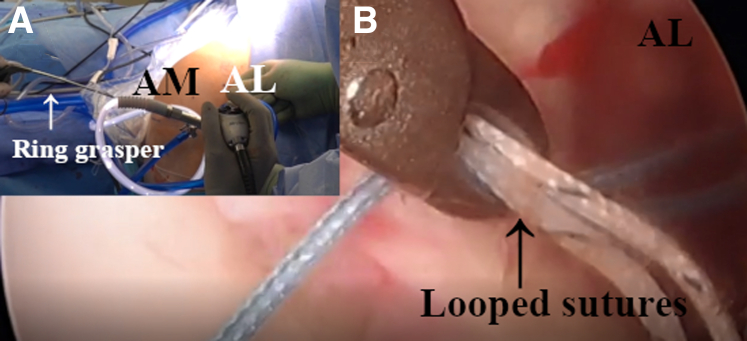
| “Smooth operator” | A ring grasper should be used to pull the looped sutures through the AM portal multiple times to ensure no soft-tissue bridges. | Soft-tissue bridges may cause graft entanglement during graft delivery. |
| “Flip or flop” | The arthroscope and incision used for the femoral guide can be used to visualize and confirm that the femoral button is flipped outside of the cortex and deep to the iliotibial band. | Failure to achieve direct visualization may lead to suspensory button misplacement and failed fixation. |
AM, anteromedial.
Final Graft Preparation
The graft is marked using a marking pen for visualization of landmarks. These landmarks can be used during graft placement via the arthroscope. First, by use of the lateral femoral intraosseous distance, the length from the femoral condyle to the outer cortex is measured and marked on the graft loop from the tip of the suspensory button. In most cases, this is approximately 30 to 40 mm. This allows an arthroscopic visual aid to anticipate the correct suspensory button placement outside the cortex. The graft is then marked 15 mm from the femoral and tibial ends (Fig 10). This allows for a minimum of 15 mm of graft into both the femoral and tibial tunnels prior to tensioning on both sides (Table 1). Prior to removal of the graft and looped cortical buttons (TightRope RT) from the posts, the tibial looped cortical button (TightRope RT) should be lengthened to ensure that it is longer than the length of the tibial tunnel to pass outside. Before shuttling the graft into place, the surgeon should confirm that there are no soft-tissue bridges between the looped sutures and AM portal. The femoral and tibial tunnel looped sutures are pulled through the AM portal with a ring grasper several times until smooth passage is achieved; this step is critical for easy graft passage (Fig 11).
Fig 10.
Intraoperative image of graft preparation on back table. The quadrupled semitendinosus graft is marked 15 mm from both ends to aid in sufficient placement during graft tightening.
Fig 11.
(A) Arthroscopic image of left knee through anterolateral (AL) portal. (B) Intraoperative image of left knee from AL viewpoint. The femoral and tibial tunnel looped sutures are pulled through the anteromedial (AM) portal with a ring grasper. This can be performed several times until smooth passage is achieved.
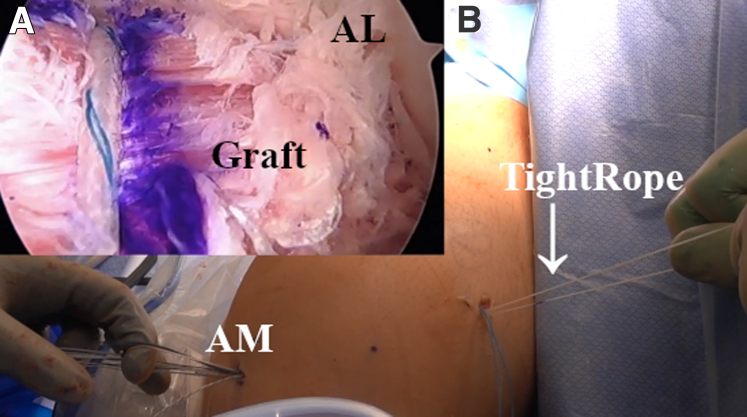
By use of the previously passed looped suture or FiberStick, the graft is shuttled through the AM portal and into the femoral tunnel. The femoral-sided adjustable suspensory fixation–TightRope RT is deployed on the femoral side. To ensure that the button is properly deployed on the femoral cortex and is deep to the iliotibial band, direct visualization can be performed with the arthroscope in the small femoral incision used for placement of the outside-in femoral guide or with a mini C-arm. By use of the markings previously placed on the graft, the graft can be slowly advanced approximately 15 to 20 mm into the femoral tunnel (Fig 12, Table 1). The graft is then passed through the tibial tunnel, and the cortical button fixation is deployed on the tibial side, again with a minimum of 15 to 20 mm in the tibial tunnel (Fig 13).
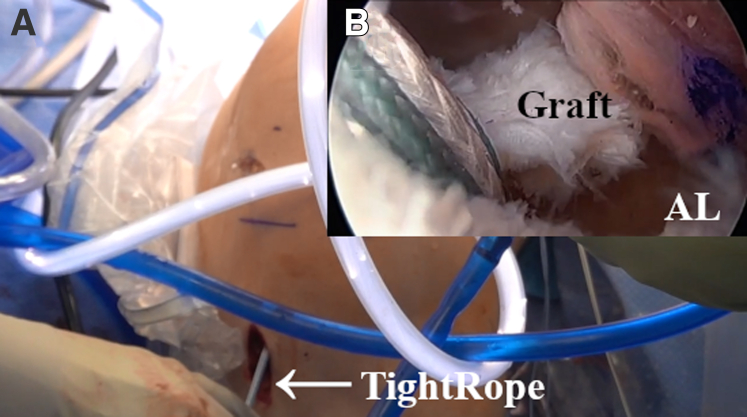
Fig 12.
(A) Arthroscopic image of left knee through anterolateral (AL) portal. (B) Intraoperative image of left knee from AL viewpoint. The graft is shuttled through the anteromedial (AM) portal by using a looped suture, and the femoral-sided TightRope is deployed on the femoral side.
Fig 13.
(A) Arthroscopic image of left knee through anterolateral portal. (B) Intraoperative image of left knee from anterolateral (AL) viewpoint. The graft is passed through the tibial tunnel, and the TightRope is then deployed on the tibial side.
Suture Buttons and Tensioning
The graft is sequentially tightened on both sides until it is taut to probing (Video 1). The knee is cycled multiple times to remove any creep in the system through range of motion, and the surgeon checks for impingement on the lateral wall, on the posterior cruciate ligament, or in full extension (Fig 14). This can be repeated until the graft is at the desired tension and the Lachman examination shows a grade of 1A.
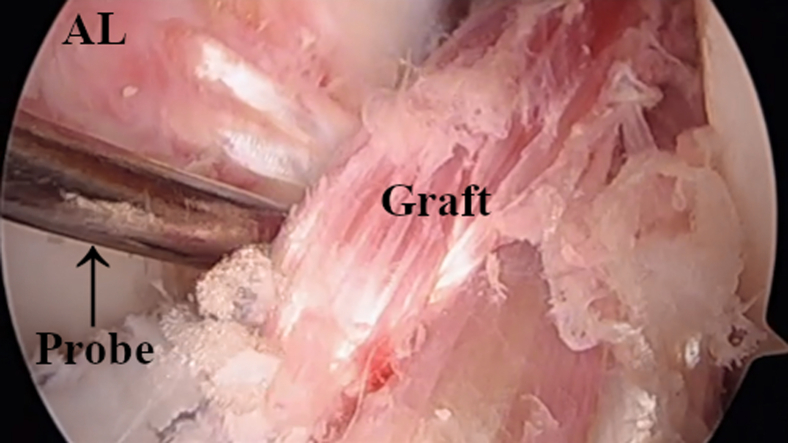
Fig 14.
Arthroscopic image of left knee through anterolateral (AL) portal. After placement and tensioning, the graft is inspected with a probe to check for impingement on the lateral femoral wall or posterior cruciate ligament.
Discussion
ACLR is one of the most common orthopaedic procedures performed for athletes and non-athletes.1 Whereas BPTB grafts have historically been the gold standard of treatment for reconstruction, there is literature that has shown no difference in rerupture rates between BPTB and soft-tissue grafts.4 All-inside ACLR with quadrupled semitendinosus and gracilis tendon has shown excellent outcomes. We present such a technique and emphasize the importance of an adequate graft diameter. This technique can reproducibly ensure a graft with a robust diameter of a minimum of 9 mm to help minimize the risk of retear and maximize return to sport while providing predictable and consistent outcomes for all patients undergoing ACLR.9 Graft diameter has been shown in several studies to have a direct effect on revision rates.8,13 Traditional doubled-over hamstring autograft often does not provide a graft with an adequate diameter, which may increase the risk of rerupture. The use of quadrupled semitendinosus and gracilis allows for a robust graft (diameter ≥ 9 mm) for all patients, which is especially important in young female athletes. A recent study has shown comparable outcomes at 1 and 2 years postoperatively between male and female patients receiving quadrupled semitendinosus autograft with a minimum diameter of 9 mm.9 Furthermore, there is a recent report of a 5-strand hamstring graft showing comparable biomechanical strength to a quadrupled graft and indicating that this may be an option if the final graft diameter is insufficient.14
There are several other noteworthy advantages to this technique. Using an independent femoral guide allows for precise anatomic placement onto the ACL footprint and attachment site to increase the likelihood of restoring normal knee kinematics, which is especially important for smaller patients. In addition to a guaranteed robust graft diameter, this technique avoids the potential risks of a short tunnel, posterior wall blowout, and impingement of the lateral wall of the intercondylar notch. In comparison to interference screws, adjustable suture buttons allow for ideal graft tensioning after range-of-motion testing. Although the all-inside technique allows for a shorter graft to be used, disadvantages to this technique include the technically demanding nature of the procedure. In addition, operative time is increased owing to autograft harvest and preparation (Table 2). Although the choice of graft and technique performed is at the discretion and comfort level of the individual surgeon, further studies should be performed to quantify whether this technique is superior to other conventional reconstruction techniques.
Table 2.
Advantages and Disadvantages
| Advantages |
| Use of an independent femoral guide allows for anatomic placement on the ACL footprint to increase the likelihood of restoring normal knee kinematics, which is especially important for smaller patients. |
| Use of an independent femoral guide avoids the potential risks of a short tunnel and posterior wall blowout. |
| Quadrupled ST and gracilis provide a reliable and robust graft diameter. |
| Adjustable suture buttons, rather than interference screws, allow for ideal graft tensioning after range-of-motion testing. |
| Graft length can be shorter when using an all-inside technique with suspensory button fixation, making it ideal for a quadrupled hamstring graft. |
| Disadvantages |
| Surgeons unfamiliar with the all-inside technique may find the procedure and graft preparation to be technically demanding. |
| Operative time and donor-site morbidity are increased owing to autograft harvesting. |
ACL, anterior cruciate ligament; ST, semitendinosus.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: E.G.M. receives speaker fees from Arthrex WINS Conference, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Intraoperative and supplemental arthroscopic imaging of all-inside anterior cruciate ligament (ACL) reconstruction using quadrupled semitendinosus autograft in left knee. The patient is positioned supine, with the surgeon primarily operating through anteromedial and anterolateral portals.
References
- 1.Desai V.S., Anderson G.R., Wu I.T., et al. Anterior cruciate ligament reconstruction with hamstring autograft: A matched cohort comparison of the all-inside and complete tibial tunnel techniques. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967118820297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaeding C.C., Pedroza A.D., Reinke E.K., Huston L.J., MOON Consortium, Spindler K.P. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MOON Knee Group, Spindler K.P., Huston L.J., et al. Anterior cruciate ligament reconstruction in high school and college-aged athletes: Does autograft choice influence anterior cruciate ligament revision rates? Am J Sports Med. 2020;48:298–309. doi: 10.1177/0363546519892991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinczewski L.A., Lyman J., Salmon L.J., Russell V.J., Roe J., Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: A controlled, prospective trial. Am J Sports Med. 2007;35:564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 5.Smith P.A., Cook C.S., Bley J.A. All-inside quadrupled semitendinosus autograft shows stability equivalent to patellar tendon autograft anterior cruciate ligament reconstruction: Randomized controlled trial in athletes 24 years or younger. Arthroscopy. 2020;36:1629–1646. doi: 10.1016/j.arthro.2020.01.048. [DOI] [PubMed] [Google Scholar]
- 6.Poehling-Monaghan K.L., Salem H., Ross K.E., et al. Long-term outcomes in anterior cruciate ligament reconstruction: A systematic review of patellar tendon versus hamstring autografts. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117709735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oiestad B.E., Holm I., Aune A.K., et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: A prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38:2201–2210. doi: 10.1177/0363546510373876. [DOI] [PubMed] [Google Scholar]
- 8.Magnussen R.A., Lawrence J.T., West R.L., Toth A.P., Taylor D.C., Garrett W.E. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 9.Lowenstein N.A., Haber D.B., Ostergaard P.J., Collins J.E., Matzkin E.G. All-inside anterior cruciate ligament reconstruction using quadrupled semitendinosus: Comparable 2-year outcomes in male and female patients. Arthroscopy. 2021;37:3140–3148. doi: 10.1016/j.arthro.2021.03.077. [DOI] [PubMed] [Google Scholar]
- 10.Haber D.B., Brook E.M., Whitlock K., Matzkin E.G. Predicting quadrupled graft length and diameter using single-strand tendon dimensions in all-inside anterior cruciate ligament reconstruction. Arthroscopy. 2018;34:243–250. doi: 10.1016/j.arthro.2017.08.257. [DOI] [PubMed] [Google Scholar]
- 11.Lubowitz J.H. All-inside anterior cruciate ligament graft link: Graft preparation technique. Arthrosc Tech. 2012;1:e165–e168. doi: 10.1016/j.eats.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pérez-Prieto D., Torres-Claramunt R., Gelber P.E., Shehata T.M.A., Pelfort X., Monllau J.C. Autograft soaking in vancomycin reduces the risk of infection after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:2724–2728. doi: 10.1007/s00167-014-3438-y. [DOI] [PubMed] [Google Scholar]
- 13.Alkhalaf F.N.A., Hanna S., Alkhaldi M.S.H., Alenezi F., Khaja A. Autograft diameter in ACL reconstruction: Size does matter. SICOT J. 2021;7:16. doi: 10.1051/sicotj/2021018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brzezinksi A., Nasra M., Pfaff W., et al. Five-strand hamstring grafts are biomechanically comparable to four-strand grafts and offer greater diameter for anterior cruciate ligament reconstruction. Arthrosc Sports Med Rehabil. 2022;4:E1731–E1738. doi: 10.1016/j.asmr.2022.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative and supplemental arthroscopic imaging of all-inside anterior cruciate ligament (ACL) reconstruction using quadrupled semitendinosus autograft in left knee. The patient is positioned supine, with the surgeon primarily operating through anteromedial and anterolateral portals.
Intraoperative and supplemental arthroscopic imaging of all-inside anterior cruciate ligament (ACL) reconstruction using quadrupled semitendinosus autograft in left knee. The patient is positioned supine, with the surgeon primarily operating through anteromedial and anterolateral portals.