Abstract
Although historically overlooked, medial meniscus posterior root (MMPR) tears are now increasingly recognized as a substantial cause of biomechanical impairment and morbidity. MMPR tears, when left untreated, are strongly correlated to meniscal extrusion and ultimately lead to altered kinematics and loading functionally equivalent to a total meniscectomy. To prevent progressive joint degeneration and alleviate pain while re-establishing native joint kinematics, MMPR repair is generally recommended in appropriately selected patients. In this Technical Note, the authors describe a detailed checklist with 10 crucial points of emphasis when performing the gold-standard transtibial pull-out repair of the MMPR, with an additional centralization stitch, providing technical pearls backed up by previous literature and ample experience treating this condition.
Technique Video
In this Technical Note, we highlight the senior-author’s top 10 pearls on how to approach a medial meniscal posterior root tear of the right knee, from recognition to surgical considerations during transtibial pull-out repair and rehabilitation.
The menisci are crescent-shaped fibrocartilaginous structures that are attached to the tibial plateau via anterior and posterior roots.1,2 Biomechanically, the meniscal roots play a critical role in converting axial loads to hoop stresses in the tibiofemoral joint, thereby playing a critical role in the menisci’s load distribution function.1 Although historically overlooked or treated with a meniscectomy, medial meniscus posterior root (MMPR) tears have since been shown to impair knee biomechanics and are pointed to as “the silent epidemic” behind spontaneous knee osteonecrosis and rapid progression of osteoarthritis.3,4 Altered kinematics as a result of MMPR tears include increased external rotation and lateral translation of the tibia. MMPR tears are also strongly associated with meniscal extrusion, although it is controversial which event occurs first.5 Ultimately, these alterations result in an increase in medial compartment contact pressure equivalent to that of a total meniscectomy.4, 5, 6
Whether treated with a partial meniscectomy or nonoperatively, patients with unrepaired MMPR tears are reported to experience clinical failure in 87% of cases, with nearly a third of them requiring total knee arthroplasty within 5 years.7 Except in cases of prohibitive severe cartilage damage or joint space narrowing, arthroscopic MMPR repair is generally recommended to prevent rapid progression of degenerative joint disease and relieve pain.8,9 In addition to decreasing the rate of arthritic progression,9,10 repaired MMPRs exhibit improved clinical outcomes and long-term cost-effectiveness when compared with partial meniscectomy.11,12
Although techniques involving suture anchor repair have been described in the previous literature,13 emerging evidence characterizes the transtibial pull-out as the gold-standard for MMPR repair.14, 15, 16 This technique restores the root attachment to the tibial plateau by means of passing sutures though tunnels in the tibia. Use of an additional centralization stitch has also been found to decrease extrusion postoperatively.17,18 In this Technical Note, we highlight the senior-author’s top 10 pearls on how to approach a MMPR tear, from recognition to surgical considerations during transtibial pull-out repair and rehabilitation (Video 1), with an aim to improve efficiency and reproducibility while minimizing the risks of complications.
Surgical Technique (With Video Illustration)
Pearl 1. Identify the Root Tear—Systematically Look for It!
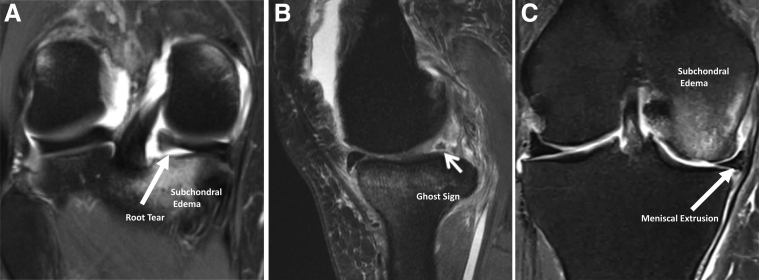
Preoperative identification of MMPR tears is the first step in ensuring a successful repair. Nevertheless, clinical suspicion of a root tear is often elusive, as more than 70% of patients with a root tear do not recall an inciting event, less than 15% present with mechanical symptoms, and only 50% will exhibit a combination of pain in deep flexion, positive McMurray’s test, and palpable extrusion upon physical examination.16,19 With that context, magnetic resonance imaging (MRI) assumes a paramount role and is now established as the definitive preoperative diagnostic tool. Previous investigations by LaPrade et al.20 report MRI sensitivity and specificity for MMPR tears at greater than 80% and a notable 98% negative predictive value. Physicians must, however, strive to systematically look for signs of a root tear when reviewing MRI examinations with significant meniscal extrusion (≥3 mm); otherwise, it can go unnoticed, as was often the case in decades past. Classic findings include the presence of the “ghost sign” on the sagittal view, a “cleft” of linear fluid signal indicating a radial tear ≤1 cm of the root insertion on coronal view, increased fluid around the root, as well as evidence of medial subchondral insufficiency fractures and bone edema (Fig 1 A-C).21
Fig 1.
Magnetic resonance imaging of medial meniscal root tear of right knee. (A) Coronal T2 view of the medial meniscal root tearing with associated tibial subchondral bone edema, (B) evidence in the sagittal T2 view of the presence of the “ghost sign,” and (C) evidence in the coronal T2 view of medial meniscal extrusion with femoral subchondral bone edema.
Pearl 2. Portal Placement and Anteromedial Approach
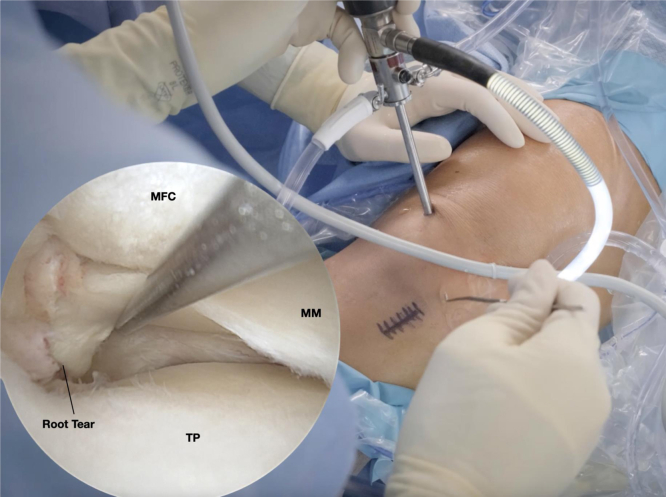
Patients are placed in a standard supine position under general anesthesia with a regional nerve block. A well-padded lateral post and high tourniquet are also used. A high anterolateral viewing portal is established, whereas an anteromedial (AM) portal just proximal to the medial meniscus is made under direct arthroscopic visualization. Portal placement is essential to ensure adequate access without damaging the articular cartilage. An AM portal placed too proximally will prevent access to the posterior aspect of the joint due to obstruction of the instruments by the femoral condyle, whereas a low portal will direct the instruments upward as they collide with the tibial spines, as well as endangering the integrity of the anterior root. In addition, once a root tear is confirmed, a 3-cm longitudinal AM incision is made adjacent to the tibial tubercle and proximal to the pes anserinus (Fig 2). Subfascial dissection is followed by a thorough exposure of the flat AM tibial bone bed—where the tunnels and fixation will be placed—with use of a Cobb elevator.
Fig 2.
Routine arthroscopic probing of the meniscal root of the right knee. With a high anterolateral viewing portal and working anteromedial portal just proximal to the medial meniscus, a probe is inserted. Probing of the root should be considered a procedural step during arthroscopic articular inventory and will reveal insufficiency of the meniscus root whenever a tear is present. (MFC, medial femoral condyle; MM, medial meniscus; TP, tibial plateau.)
Pearl 3. Arthroscopic Confirmation and Classification—Probe Every Root!
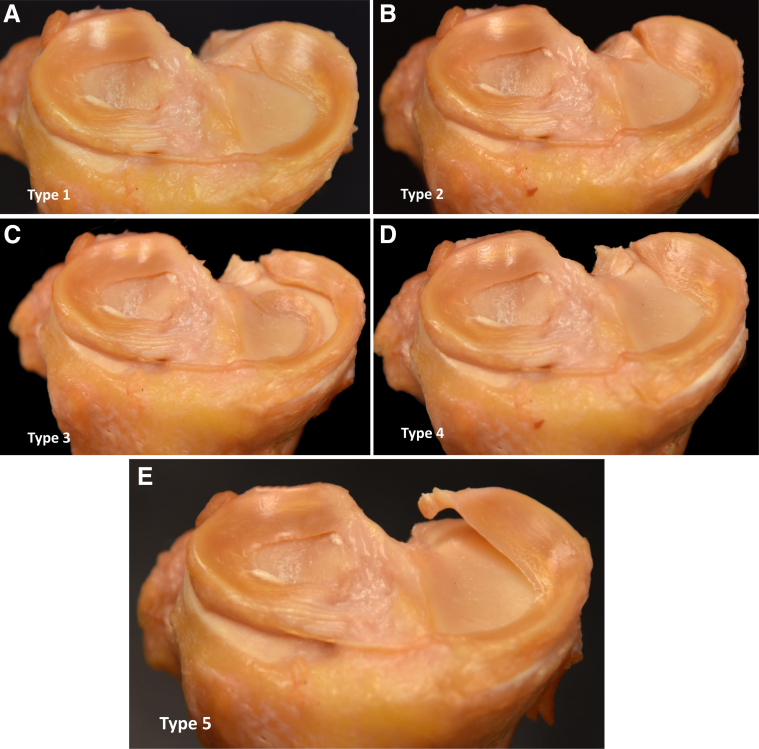
Arthroscopic confirmation and subsequent classification of the MMPR tear is key before moving forward with the repair. Upon diagnostic arthroscopy, visualization of a floating meniscus, excessive displacement when using aspiration (deemed a positive “aspiration test”), as well as the absence of the “medial meniscal flounce sign” can all serve as alerts to potential damage to the root.22, 23, 24 Notwithstanding, even a diligent inspection that screens for all the aforementioned signs can miss a MMPR tear if the root attachments are not routinely probed. The probe is inserted in the AM portal and used to confirm if the MMPR is damaged or nonfunctional (Fig 2), determine the severity, and classify the tear—as described by LaPrade et al. and highlighted in Figure 3 A-E.16 Mobilization of the root to its anatomic location is necessary to ensure that it is amenable to repair. In chronic cases in which the periphery of the meniscus is adhered to the capsule in an extruded position, a shaver may be used to perform a release and allow for anatomic reduction.
Fig 3.
Cadaveric depiction of LaPrade’s classification of meniscal root tears in a right knee. (A) Type I is defined as a partial tear but with stable pattern; (B) type II, which is a complete radial tear near the root attachment, with 3 subcategories (<3 mm, 3-<6 mm, and 6-9 mm from the center of the attachment)—this is the most common root tear pattern; (C) type III tears are considered “disaster tears” and consist of a complete root detachment combined with a bucket-handle tear; (D) type IV, where an oblique tear propagates into the root attachment site; and (E) type V tears, which are bony avulsions from the attachment site, often found as meniscal ossicle chronically during arthroscopy.
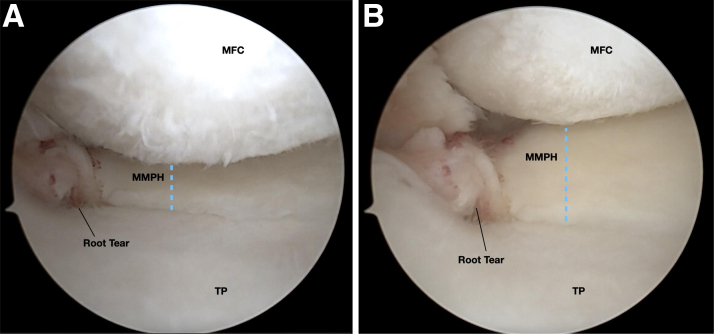
Pearl 4. Medial Collateral Ligament Release—Always!
In our experience, tightness of the medial compartment that is not addressed by a release of the medial collateral ligament (MCL) is the single most common cause of technical difficulty, prolonged surgical time, and iatrogenic damage to the cartilage when repairing a MMPR. Accordingly, we argue that a percutaneous release via pie-crusting of the MCL should be employed routinely in every repair. It is the authors’ preference to perform a trephination of the MCL with a spinal needle at the posterior aspect of its femoral insertion, under valgus stress, until satisfactory opening of the compartment is obtained (Fig 4 A and B). In that way, adequate visualization is ensured, and the risk for iatrogenic cartilage damage during instrumentation is minimized.
Fig 4.
Effect of medial collateral ligament pie crusting while arthroscopic viewing of the medial meniscal root tear from the anterolateral portal of the right knee. (A) Evidence of a LaPrade type II tear in a tight medial tibiofemoral compartment prior to medial collateral ligament pie-crusting procedure of a right knee. (B) Increased visualization and access to the posterior horn and root attachment of the medial meniscus after medial collateral ligament pie crusting. (MFC, medial femoral condyle; MMPH, medial meniscus posterior horn; TP, tibial plateau.)
Pearl 5. Anatomic Tunnel Placement
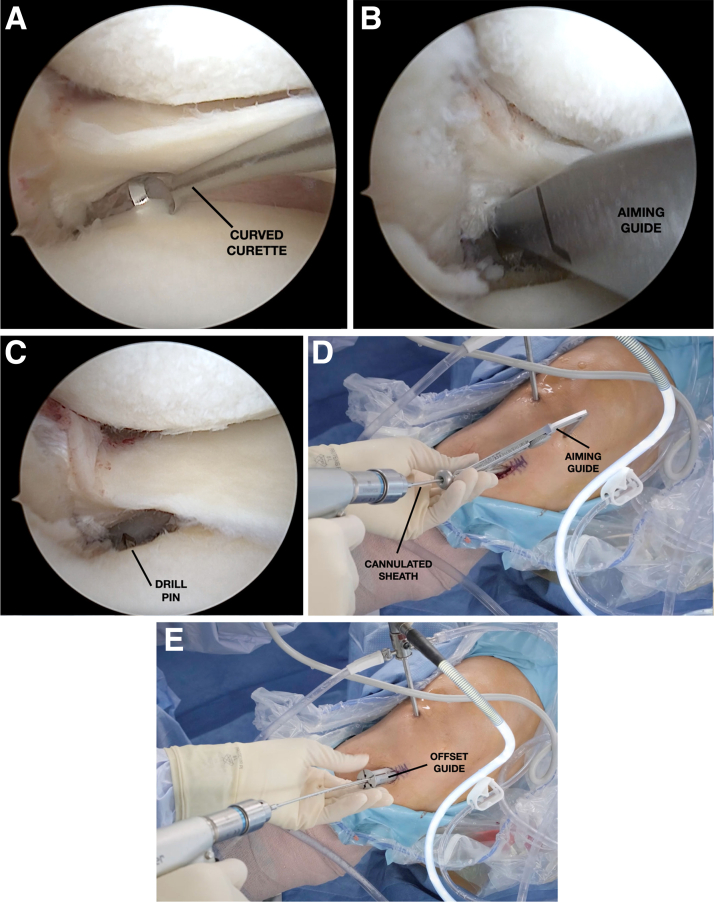
Restoring the anatomical relationship of the meniscus to its root attachment on the plateau is imperative to success, as previous biomechanical evidence suggests nonanatomic root repair may still functionally equate a subtotal meniscectomy.25,26 The posterior root of the medial meniscus is located approximately 9.6 mm posterior and 0.8 mm lateral to the apex of the medial tibial eminence (total distance of 11.5 mm).1 The anatomic footprint of the MMPR is decorticated using a curved curette (Meniscal Root Repair System, Smith & Nephew, Andover, MA) and the area is then further prepared with an arthroscopic shaver, making sure to remove any loose articular cartilage or remnant root stump tissue (Fig 5A). A curved aimer guide (contralateral guide when repairing a medial root and ipsilateral guide when repairing a lateral root) is positioned at the desired site of the first of the 2 tunnels, typically the posterior one (Fig 5B). It is key to ensure that the tunnel is positioned posterior enough in the plateau in order to reproduce the insertion of the shiny white fibers, which account for nearly half of the native root strength.1 A 2.7-mm cannulated sheath with a guide pin is then positioned in the aimer guide set at 55° and drilled to create the first tunnel (Fig 5 C and D). The position is verified, and the sheath tip placed approximately flush with the plateau in order to avoid suture damage. After the first tunnel is drilled, a second tunnel is placed 5 mm anterior to the first using an offset guide (Fig 5E). Creating 2 transtibial tunnels allows for improved approximation of the meniscus to its native footprint and increase the chance of biologic healing. The drill pins are removed, but the cannulated sheaths are left in place for passing of the sutures. In the setting of concomitant cruciate ligament reconstruction, it is desirable to adjust the root tunnel orientation to 65°, parallel to the tibial tunnels of the cruciate reconstruction, to minimize the risk of convergence.27
Fig 5.
Anatomic tibial tunnel placement with arthroscopic viewing of the medial meniscal root tear from the anterolateral portal and a working anteromedial portal of the right knee. (A) The anatomic footprint of the meniscal root is decorticated using a curved curette and the area is then further prepared with an arthroscopic shaver. (B) A curved aimer guide is positioned at the desired site of the posterior tunnel. (C, D) A 2.7-mm cannulated sheath with a guide pin is then positioned in the aimer guide set at 55° and drilled to create the first tunnel. (E) After the first tunnel is drilled, a second tunnel is placed 5 mm anterior to the first using an offset guide.
Pearl 6. Use of a Cannula
Routine use of an arthroscopic cannula whenever available is strongly advised. This is critical to avoid soft-tissue bridging and difficulty when passing the suture near the retropatellar fat pad, which would inevitably add time-consuming extra steps during suture management. The cannula (8.25 mm × 7 cm Twist-In Cannula; Arthrex, Naples, FL) is placed in the AM working portal before insertion of the suture-passing device and is kept in place until the repair has been completed.
Pearl 7. Suture Configuration
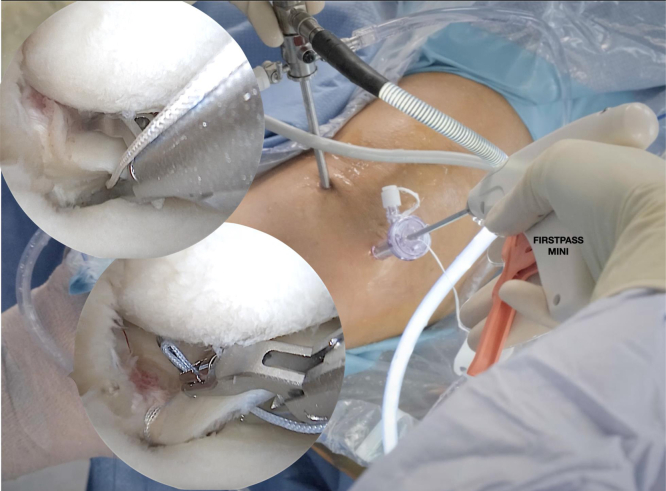
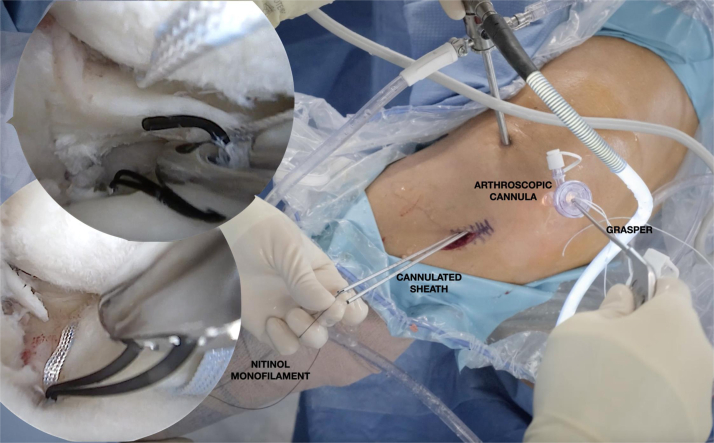
Using a self-retrieving all-inside suture-passing device (FIRSTPASS MINI; Smith & Nephew), loaded with high-strength suture tape, the first suture is inserted into the posterior aspect of the detached MMPR, approximately 5 mm medial from the lateral aspect of the meniscal tear edge, with the needle passed from the tibial to the femoral side and pulled back through the cannula on the AM portal (Fig 6). A monofilament nitinol wire is then inserted into the posterior transtibial tunnel and retrieved with a grasper through the AM cannula to allow for the first suture to be shuttled through the posterior tunnel without tangling (Fig 7). The steps are then repeated with the second suture, positioning it through the midportion of the root, anterior to the placement of the first suture, in order to avoid eversion of the central free end of the meniscus. The second suture is shuttled through the more anterior transtibial tunnel. A configuration with 2 simple stitches is preferred, as it is fast and technically straightforward, while also generating similar mechanical properties and clinical outcomes relative to other suture configurations.28,29
Fig 6.
Suture passage with arthroscopic viewing of the medial meniscal root tear from the anterolateral portal and a working anteromedial portal of the right knee. Using a self-retrieving all-inside suture-passing device, the first suture (upper arthroscopic view image) is inserted into the posterior aspect of the detached medial meniscal posterior root approximately 5 mm medial from the lateral meniscal edge going from the tibial to the femoral side and pulled back through the cannula on the anteromedial portal. After passage of the first suture (as demonstrated in Fig 7), the steps are repeated with the second suture (lower arthroscopic view image), positioning it through the midportion of the root, anterior to the placement of the first suture, in order to avoid eversion of the central free end of the meniscus.
Fig 7.
Suture shuttling in a 2-tunnel transtibial repair with arthroscopic viewing from the anterolateral portal and a working anteromedial portal of the right knee. A monofilament nitinol wire is inserted into the posterior transtibial tunnel and retrieved with a grasper through the anteromedial cannula to allow for the first suture (upper arthroscopic view image) to be shuttled through the posterior tunnel without tangling. The nitinol wire is pulled out of the tibial tunnel, which shuttles the repair suture down and out of the tunnel. The shuttling steps are then repeated with the second repair suture (lower arthroscopic view image), as similarly noted in Figure 6, through the more anterior transtibial tunnel.
Pearl 8. Centralization Stitch—When to Add?
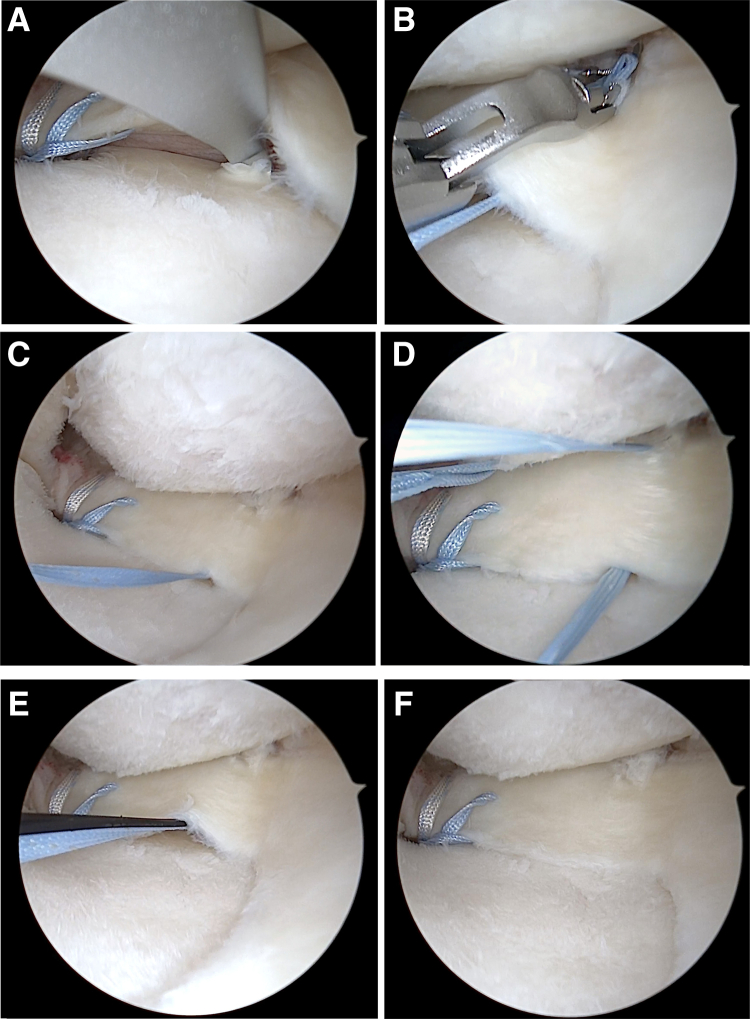
Next, arthroscopic evaluation of the meniscus with a probe can help to identify whether there is any residual extrusion. If present, the use of a centralization stitch can aid in anatomic reduction of the meniscus. In cases of significant preoperative medial extrusion (>3 mm), it is also wise to consider adding a centralization stich, considering the incidence of persistent postoperative extrusion.30 Viewing through the AM portal, an additional transtibial tunnel is drilled just lateral to the medial rim of the tibial articular surface with the 2.7-mm cannulated sheath through the same aiming guide used earlier, now placed through the anterolateral portal (Fig 8A). Once the tunnel is established, the self-retrieving suture device is again used to pass a third suture, in a horizontal mattress configuration (Fig 8B), first from bottom to top on the periphery of the meniscus, and then from top to bottom, incorporating the meniscocapsular junction (Fig 8 C and D). Both ends of the suture tape are then retrieved with a grasper and shuttled through the cannulated sheath with the aid of the monofilament nitinol wire (Fig 8 E and F). Whenever a centralization stich is performed, its fixation to the tibial cortex should be carried out before that of the root repair stiches, in order to produce optimal reduction.
Fig 8.
Centralization stich with arthroscopic viewing from the anteromedial portal and a working anterolateral portal of the right knee. (A) A transtibial tunnel is drilled just lateral to the medial rim of the tibial articular surface with a cannulated sheath through the same aiming guide used earlier, now placed through the anterolateral portal. (B-D) A horizontal mattress suture is passed from bottom to top on the periphery of the meniscus, and then from top to bottom, incorporating the meniscocapsular junction. (E, F) Both ends of the suture tape are then retrieved with a grasper and shuttled through the cannulated sheath with the aid of the monofilament nitinol wire.
Pearl 9. Tension and Fixation Under Arthroscopic Visualization
Once all sutures are placed and pulled out of their respective tunnels, the knee is positioned at 90° of flexion. A pilot hole for anchor fixation (FOOTPRINT Suture Anchor; Smith & Nephew) is drilled distal to the tunnels, with a 2.4 guide-pin and a 4.5 reamer, followed by debridement with a shaver. The 2 pairs of suture tape limbs are shuttled through the eyelet in the anchor, which is then malleted flush with the tibial cortex. All sutures are manually tensioned under direct arthroscopic visualization (Fig 9), ensuring optimal reduction and tension prior to definitive fixation and locking of the construct, which is achieved by turning the handle on the anchor in a clockwise direction until an audible sound sets in. The tension and integrity of the meniscus root attachment—and the centralization stich, whenever performed—are probed arthroscopically for final verification.
Fig 9.
Tensioning of the sutures and anchor fixation of the medial meniscal root repair construct under arthroscopic visualization from the anterolateral portal of the right knee. All sutures are manually tensioned under direct arthroscopic visualization, ensuring optimal reduction and tension of the repair construct.
Pearl 10. Rehabilitation: Non–Weight-Bearing!
For the first 6 weeks after a MMPR repair, the patient is mandatorily non–weight-bearing. A hinged knee brace is positioned immediately postoperatively in order to promote stability and adequate healing of the MCL, in addition to the meniscal repair. Early range of motion is encouraged, but restricted to 90° during the first 2 weeks, to avoid undesirable increases in contact pressure and extrusion caused by deeper flexion angles. The emphasis on non–weight-bearing status is paramount early on to protect the repair construct. Biomechanical evidence by Steineman et al.31 shows unrecoverable and progressive loosening of root repairs upon simulated load cycles, showing the importance of healing before loading. Physical therapy is progressed in a stepwise fashion, with running progression exercises beginning at 12 weeks. A medial unloader brace may be used during closed chain exercises until 6 months postoperatively.
Discussion
Transtibial repair is currently widely accepted as the gold-standard technique for treatment of root tears, providing a biomechanically reliable suture construct, while also limited to familiar standard arthroscopic portals.5,21 The efficacy of MMPR repair is highlighted in a recent comprehensive systematic review by Perry et al.30 The authors report ample qualitative evidence of overall improvement in mean and peak contact pressures after transtibial repair across 12 biomechanical studies, as well as improved patient-reported outcomes and delaying osteoarthritis progression across 24 clinical studies. Nevertheless, some still question the ability to reliably repair torn meniscal roots, as second-look arthroscopy frequently reveals incomplete or lax healing and meniscal extrusion often persists—albeit still providing significant clinical benefit.21 In the context of approximately 32% incidence of lax healing,32 optimizing a surgical technique to maximize the restoration of native anatomy and creation of a stable construct are paramount in an effort to improve post-operative outcomes. This article describes our preferred technique for a successful transtibial pull-out repair for a MMPR tear. In addition, there is some heterogeneity in terms of surgical technique in previous literature,30 with many technical aspects still the subject of debate. Thereafter, we detail the senior author’s preferences on each topic where consensus is often lacking.
In order to mitigate the risks of iatrogenic cartilage damage while providing optimal visualization and working space for adequate instrumentation, routine release of the MCL via percutaneous pie-crusting is encouraged. Multiple previous investigations have demonstrated improved postoperative patient outcomes with a controlled percutaneous MCL release relative to standard of care without release.33 Fakioglu et al.34 reported radiographic gapping of the medial compartment upon valgus stress, revealing that preoperative values were restored at 6 months following MCL release in tight medial compartments. The findings by Fakioglu, paired with the notoriously poor healing capabilities inherent to chondral tissue illustrate our anecdote that “the MCL will heal almost every time, but the cartilage will heal none of the time.”
In terms of tunnel configuration, our preference is the 2-tunnel technique. It is important to note that biomechanically, no significant difference in displacement values or load to failure have been reported when comparing single- versus double-tunnel transtibial pull-out techniques.31,35 However, we encourage the 2-tunnel technique due to the increased coverage of the anatomical footprint,35 allowing for better approximation of the meniscus back to its native root attachment. Despite largely favorable clinical and biomechanical results, root repair frequently does not significantly improve meniscal extrusion post-operatively.30 Although even lax healing of the meniscal root still yields clinical benefit, the phenomenon of persistent residual extrusion is an area of concern. Residual extrusion may result in unfavorable biomechanical kinematics and was highlighted by Chung et al.36 as a potential predictor of clinical failure of meniscal root repair. Thus, we argue that the use of a centralization stitch should be considered whenever significant extrusion over 3 mm is present preoperatively. Multiple retrospective investigations have reported improved patient-reported outcomes at 2-year follow up following root repair with the addition of meniscal centralization, as well as decreased medial extrusion distance and no progression of varus deformity.18,37
Overall, current literature reflects the compelling evidence of the biomechanical and clinical benefits, cost-effectiveness, and safety of medial meniscus root repairs.12,38 Emerging evidence favors expanding the indications of a root repair, with comparable outcomes between patients younger and older than 50 years of age.39 The present Technical Note contains our points of emphasis and technical pearls (Table 1) for efficient and reproducible steps for the gold-standard transtibial pull-out repair of MMPR using a 2-tunnel technique with an aim of optimizing patient outcomes and minimizing complications.
Table 1.
Pearls and Pitfalls
| Pearls |
|
|
|
|
|
|
|
|
| Pitfalls |
|
|
|
|
|
MCL, medial collateral ligament; MRI, magnetic resonance imaging.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C. reports paid consultant for Arthrex, CONMED Linvatec, Ossur, and Smith & Nephew; and board/committee member: American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, and International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
In this Technical Note, we highlight the senior-author’s top 10 pearls on how to approach a medial meniscal posterior root tear of the right knee, from recognition to surgical considerations during transtibial pull-out repair and rehabilitation.
References
- 1.Mameri E.S., Dasari S.P., Fortier L.M., et al. Review of meniscus anatomy and biomechanics. Curr Rev Musculoskelet Med. 2022;15:323–335. doi: 10.1007/s12178-022-09768-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 3.Cinque M.E., Chahla J., Moatshe G., Faucett S.C., Krych A.J., LaPrade R.F. Meniscal root tears: a silent epidemic. Br J Sports Med. 2018;52:872–876. doi: 10.1136/bjsports-2017-098942. [DOI] [PubMed] [Google Scholar]
- 4.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 5.Krych A.J., LaPrade M.D., Hevesi M., et al. Investigating the chronology of meniscus root tears: Do medial meniscus posterior root tears cause extrusion or the other way around? Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120961368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swamy N., Wadhwa V., Bajaj G., Chhabra A., Pandey T. Medial meniscal extrusion: Detection, evaluation and clinical implications. Eur J Radiol. 2018;102:115–124. doi: 10.1016/j.ejrad.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Krych A.J., Reardon P.J., Johnson N.R., et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25:383–389. doi: 10.1007/s00167-016-4359-8. [DOI] [PubMed] [Google Scholar]
- 8.Bernard C.D., Kennedy N.I., Tagliero A.J., et al. Medial meniscus posterior root tear treatment: A matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med. 2020;48:128–132. doi: 10.1177/0363546519888212. [DOI] [PubMed] [Google Scholar]
- 9.Chahla J., LaPrade R.F. Meniscal root tears. Arthroscopy. 2019;35:1304–1305. doi: 10.1016/j.arthro.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Kim J.H., Chung J.H., Lee D.H., Lee Y.S., Kim J.R., Ryu K.J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 11.Chung K.S., Ha J.K., Yeom C.H., et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: A minimum 5-year follow-up. Arthroscopy. 2015;31:1941–1950. doi: 10.1016/j.arthro.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 12.Faucett S.C., Geisler B.P., Chahla J., et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: Clinical and economic effectiveness. Am J Sports Med. 2019;47:762–769. doi: 10.1177/0363546518755754. [DOI] [PubMed] [Google Scholar]
- 13.Kim J.H., Shin D.E., Dan J.M., Nam K.S., Ahn T.K., Lee D.H. Arthroscopic suture anchor repair of posterior root attachment injury in medial meniscus: Technical note. Arch Orthop Trauma Surg. 2009;129:1085–1088. doi: 10.1007/s00402-008-0810-8. [DOI] [PubMed] [Google Scholar]
- 14.Kim Y.M., Rhee K.J., Lee J.K., Hwang D.S., Yang J.Y., Kim S.J. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 2006;22 doi: 10.1016/j.arthro.2005.12.040. 795.e791-794. [DOI] [PubMed] [Google Scholar]
- 15.Cerminara A.J., LaPrade C.M., Smith S.D., Ellman M.B., Wijdicks C.A., LaPrade R.F. Biomechanical evaluation of a transtibial pull-out meniscal root repair: Challenging the bungee effect. Am J Sports Med. 2014;42:2988–2995. doi: 10.1177/0363546514549447. [DOI] [PubMed] [Google Scholar]
- 16.LaPrade R.F., Floyd E.R., Carlson G.B., Moatshe G., Chahla J., Monson J.K. Meniscal root tears: Solving the silent epidemic. J Arthrosc Surg Sports Med. 2021;2:47–57. [Google Scholar]
- 17.Koga H., Muneta T., Watanabe T., et al. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32:2000–2008. doi: 10.1016/j.arthro.2016.01.052. [DOI] [PubMed] [Google Scholar]
- 18.Koga H., Nakamura T., Katagiri H., et al. Two-year outcomes after meniscoplasty by capsular advancement with the application of arthroscopic centralization technique for lateral compartment knee osteoarthritis. Am J Sports Med. 2020;48:3154–3162. doi: 10.1177/0363546520957367. [DOI] [PubMed] [Google Scholar]
- 19.James E.W., Johannsen A.M., Cinque M.E., Chahla J., Laprade R.F. An evidence-based approach to the diagnosis and treatment of meniscal root tears. Minerva Ortop Traumatol. 2017;68:81–90. [Google Scholar]
- 20.LaPrade R.F., Ho C.P., James E., Crespo B., LaPrade C.M., Matheny L.M. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc. 2015;23:152–157. doi: 10.1007/s00167-014-3395-5. [DOI] [PubMed] [Google Scholar]
- 21.Krych A.J., Hevesi M., Leland D.P., Stuart M.J. Meniscal root injuries. J Am Acad Orthop Surg. 2020;28:491–499. doi: 10.5435/JAAOS-D-19-00102. [DOI] [PubMed] [Google Scholar]
- 22.Bikkina R.S., Tujo C.A., Schraner A.B., Major N.M. The "floating" meniscus: MRI in knee trauma and implications for surgery. AJR Am J Roentgenol. 2005;184:200–204. doi: 10.2214/ajr.184.1.01840200. [DOI] [PubMed] [Google Scholar]
- 23.Jacquet C., Magosch A., Mouton C., Seil R. The aspiration test: An arthroscopic sign of lateral meniscus posterior horn instability. J Exp Orthop. 2021;8:17. doi: 10.1186/s40634-021-00327-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta Y., Mahara D.P., Lamichhane A.P. Validity of flounce sign to rule out medial meniscus tear in knee arthroscopy. BMC Musculoskelet Disord. 2015;16:337. doi: 10.1186/s12891-015-0800-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.LaPrade C.M., Foad A., Smith S.D., et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43:912–920. doi: 10.1177/0363546514566191. [DOI] [PubMed] [Google Scholar]
- 26.Stärke C., Kopf S., Gröbel K.H., Becker R. The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: A biomechanical study. Arthroscopy. 2010;26:358–365. doi: 10.1016/j.arthro.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 27.Gursoy S., Perry A.K., Brady A., et al. Optimal tibial tunnel placement for medial and lateral meniscus root repair on the anteromedial tibia in the setting of anterior and posterior cruciate ligament reconstruction of the knee. Am J Sports Med. 2022;50:1237–1244. doi: 10.1177/03635465221074312. [DOI] [PubMed] [Google Scholar]
- 28.Vertullo C.J., Cadman J., Dabirrahmani D., Appleyard R. Biomechanical comparison of an all-inside meniscal repair device construct versus pullout sutures for arthroscopic transtibial repair of posterior medial meniscus root tears: A matched-pair cadaveric study. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211000464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ulku T.K., Kaya A., Kocaoglu B. Suture configuration techniques have no effect on mid-term clinical outcomes of arthroscopic meniscus root repairs. Knee. 2020;27:676–682. doi: 10.1016/j.knee.2020.04.017. [DOI] [PubMed] [Google Scholar]
- 30.Perry A.K., Lavoie-Gagne O., Knapik D.M., et al. Examining the efficacy of medial meniscus posterior root repair: A meta-analysis and systematic review of biomechanical and clinical outcomes. Am J Sports Med. 2022 doi: 10.1177/03635465221077271. [DOI] [PubMed] [Google Scholar]
- 31.Steineman B.D., LaPrade R.F., Haut Donahue T.L. Loosening of transtibial pullout meniscal root repairs due to simulated rehabilitation is unrecoverable: A biomechanical study. Arthroscopy. 2019;35:1232–1239. doi: 10.1016/j.arthro.2018.11.041. [DOI] [PubMed] [Google Scholar]
- 32.Edwards C., Goldman B.H., Turley J., Richey B., Deal M.J., Kalbac D. Outcomes after surgical repair of medial meniscal root tears: a review. J Knee Surg. 2021;34:1599–1602. doi: 10.1055/s-0040-1710565. [DOI] [PubMed] [Google Scholar]
- 33.Hauer T.M., Wengle L.J., Whelan D.B. Adjuvant medial collateral ligament release at the time of knee arthroscopy: A controlled percutaneous technique. Arthrosc Tech. 2022;11:e1541–e1546. doi: 10.1016/j.eats.2022.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fakioglu O., Ozsoy M.H., Ozdemir H.M., Yigit H., Cavusoglu A.T., Lobenhoffer P. Percutaneous medial collateral ligament release in arthroscopic medial meniscectomy in tight knees. Knee Surg Sports Traumatol Arthrosc. 2013;21:1540–1545. doi: 10.1007/s00167-012-2128-x. [DOI] [PubMed] [Google Scholar]
- 35.LaPrade C.M., LaPrade M.D., Turnbull T.L., Wijdicks C.A., LaPrade R.F. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015;43:899–904. doi: 10.1177/0363546514563278. [DOI] [PubMed] [Google Scholar]
- 36.Chung K.S., Ha J.K., Ra H.J., Kim J.G. Preoperative varus alignment and postoperative meniscus extrusion are the main long-term predictive factors of clinical failure of meniscal root repair. Knee Surg Sports Traumatol Arthrosc. 2021;29:4122–4130. doi: 10.1007/s00167-020-06405-7. [DOI] [PubMed] [Google Scholar]
- 37.Mochizuki Y., Kawahara K., Samejima Y., Kaneko T., Ikegami H., Musha Y. Short-term results and surgical technique of arthroscopic centralization as an augmentation for medial meniscus extrusion caused by medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. 2021;31:1235–1241. doi: 10.1007/s00590-021-02874-9. [DOI] [PubMed] [Google Scholar]
- 38.Chung K.S., Ha J.K., Ra H.J., Yu W.J., Kim J.G. Root repair versus partial meniscectomy for medial meniscus posterior root tears: Comparison of long-term survivorship and clinical outcomes at minimum 10-year follow-up. Am J Sports Med. 2020;48:1937–1944. doi: 10.1177/0363546520920561. [DOI] [PubMed] [Google Scholar]
- 39.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In this Technical Note, we highlight the senior-author’s top 10 pearls on how to approach a medial meniscal posterior root tear of the right knee, from recognition to surgical considerations during transtibial pull-out repair and rehabilitation.
In this Technical Note, we highlight the senior-author’s top 10 pearls on how to approach a medial meniscal posterior root tear of the right knee, from recognition to surgical considerations during transtibial pull-out repair and rehabilitation.