Abstract
BACKGROUND:
The North Carolina Cancer Hospital at the University of North Carolina Medical Center serves patients with a variety of malignant conditions and discharges more than 130 patients each month. Processes to improve transitions of care prompted implementation of a first-cycle, pharmacist-led chemotherapy consultation service on the inpatient oncology units. This process provides education to improve patient engagement and activation. High patient activation has been associated with better patient outcomes; poor patient activation has been associated with increased health care costs.
OBJECTIVE:
To determine the effect of pharmacist-led comprehensive chemotherapy consultation services on adherence to outpatient follow-up appointments within 30 days of discharge.
METHODS:
This was a single-center, retrospective chart review. This study consisted of 2 groups: adult patients who received comprehensive consultation services between April 2017 and September 2017 and a 2:1 historical group of adult control patients randomly selected from a list of patients who received their first cycle of chemotherapy during a hospital admission between April 2014 and April 2017. The primary endpoint was the effect of comprehensive consultation services on adherence to outpatient follow-up appointments within 1 month after discharge.
RESULTS:
Ninety-six patients were included in this study. The percentage of appointments attended was 98.0% for the intervention group and 92.3% for the control group (P = 0.0018).
CONCLUSIONS:
This study demonstrates that pharmacy consultation in the inpatient oncology setting is associated with improved adherence to outpatient appointments within 30 days of discharge. This represents the first published data on pharmacist interventions resulting in improved outpatient appointment adherence.
What is already known about this subject
Pharmacist intervention has previously been associated with improved medication adherence.
Higher patient activation scores have been associated with improved patient outcomes, and lower scores have been associated with increased health care costs.
What this study adds
Patients who received comprehensive pharmacist-led inpatient chemotherapy consultation services were more likely to complete outpatient appointments within 30 days of discharge when compared with patients who did not receive these services (98.0% vs. 92.3%, respectively; P = 0.0018).
This study demonstrates the positive effect of pharmacists on transitions of care within an interdisciplinary oncology team.
The North Carolina Cancer Hospital (NCCH) at the University of North Carolina Medical Center (UNCMC) serves patients with a variety of malignant conditions and discharges more than 130 patients each month. Cancer care is a complex process in which patients have multiple appointments with a variety of medical disciplines.1 During the transition from an inpatient stay to outpatient care, the patient is vulnerable to medical complications and medical errors.2,3 Close follow-up after discharge from the hospital has the potential to decrease medical complications, but if patients do not attend appointments they will not benefit. The oncology services at UNCMC developed new strategies for improving the transition of care model to optimize close follow-up
In early 2017, UNCMC pharmacists began implementing comprehensive chemotherapy consultation services (3CS).4 These services include first-cycle chemotherapy counseling, comprehensive medication management, and a formal evaluation for medication-related problems. This patient-centric process begins with a medication therapy review, followed by an in-person inpatient interview and education regarding the proposed therapy. From there, a medication-related action plan is developed, and further interventions are made as necessary. At the end of the process, the pharmacist writes a transition of care note in the health record, and the patient is scheduled for outpatient appointments with an oncology pharmacist, advanced practice provider, oncologist, and additional medical teams, as applicable. Additional details focused on the structure of 3CS at UNC have been published previously.4
The 3-part goal of 3CS is to provide targeted patient education, enhance patient engagement, and facilitate patient activation. Engagement and activation have been identified as areas for targeted health care reform.5,6 Engagement involves patients working cohesively with providers and other members of the health care team towards common health-related goals.5 Activation is a component of engagement that refers to a patient’s ability and desire to independently manage their own health.6 It has further been considered analogous to “understanding one’s role in the care process and having the knowledge, skill, and confidence to manage one’s health and health care” by Hibbard and Greene (2013).6
One validated method for measuring patient activation is the patient activation measure (PAM) survey.7 This scoring system is a survey that evaluates a patient’s ability to navigate several domains that are vital to the health care experience. These domains include self-management, preventive care, collaboration with providers, and access to health care. A shorter form of this questionnaire has been compared with the original and was found to be both reliable and valid.8
Activation has been shown to have direct effects on health care costs and outcomes.6,9-12 One study reported that for every 10-point increase in PAM scores, the risk of emergency department visits, obesity, or smoking was decreased by 1%.9 Additionally, each 10-point increase in PAM scores correlated to a 1% increased likelihood of having normal values for high-density lipoprotein, hemoglobin A1c, or triglycerides. Other studies demonstrated that better PAM scores correlate with improved outcomes related to diabetes and cardiovascular disease.10,11
Hibbard et al. (2013) reported on the relationship between PAM scores and health care costs.12 Patients were divided into subgroups based on their PAM score categories (1-4, with 1 being the lowest PAM score and 4 being the highest PAM score). Patients with the lowest PAM scores had higher health care costs when compared with patients who had the highest PAM scores. Average costs were 8% higher in the year of the study and 21% higher in the first half of the year after study completion in the group of patients with lower PAM scores.
Authors of the current study previously published an article describing the benefits of the 3CS approach at UNCMC.4 Patients enrolled in the study were administered the PAM-10 survey. Mean PAM-10 scores were measured at baseline and 2 business days after the 3CS encounter. The study demonstrated a statistically significant mean PAM-10 increase of 7.5 and identified some common medication-related problems that pharmacists were able to resolve. Based on the previously mentioned data about PAM scores and the importance of patient activation, it is reasonable to believe that the increase in PAM scores seen in the study would correlate with better patient outcomes and reduced health care expenditures.
The current study aimed to further define the benefit of pharmacist involvement across transitions of care. In particular, the authors hoped to identify if inpatient pharmacist-led 3CS promoted increased appointment adherence in the outpatient setting. Influenced by the previous data that pharmacist-led 3CS improves patient activation, the authors hypothesized that patients who received inpatient 3CS would be more likely to attend outpatient appointments than those who did not receive inpatient 3CS. This is largely because of the premise that increased patient activation correlates to an increase in the ability of patients to manage their own health care. Therefore, it is expected that patients with higher activation will be more likely to participate in their care by attending all of their scheduled appointments. Although previous studies have demonstrated the positive effect of pharmacist involvement on medication adherence, to the authors’ knowledge, there are no published studies on the effect of pharmacist involvement on appointment adherence.13,14 This study therefore represents the first to show that inpatient pharmacist involvement is associated with improved outpatient appointment adherence.
From a managed care perspective, an increase in appointment adherence would be quite favorable. This increased attendance would be expected to translate to better patient outcomes related to more optimized management of associated malignancies. As the U.S. health care model moves toward quality-based metrics, this expected increase in positive outcomes would be expected to correlate with better revenue for the health system. Furthermore, as cancer becomes a more chronic medical condition, these improvements align well with current pharmaceutical care strategies for improving disease management.15 Additionally, increased appointment attendance would correlate with increased revenue for the health system, since the literature has demonstrated the contribution of missed appointments to revenue loss.16,17
Methods
This was a single-center, retrospective chart review of patients who received oncology care at the NCCH. Patients in this study were aged ≥ 18 years, admitted to and discharged from an inpatient oncology service between April 2014 and October 2017, had an inpatient length of stay greater than 48 hours, and received first-cycle chemotherapy during the admission. Patients were excluded if they were admitted to the bone marrow transplant or gynecology oncology services, had no appointments within 30 days from original discharge, transferred all care to another institution immediately following discharge, or were transferred to acute inpatient rehabilitation immediately following discharge. The intervention arm of this study consisted of the 36 patients previously defined by Bates et al. (2019).4 Two control patients from a historical group before implementation of 3CS were included for every 1 intervention patient.
The primary outcome of this study was the effect of 3CS on adherence to any outpatient follow-up encounters within 30 days of discharge. To analyze this, the electronic health record system Epic, version 2018 (Epic Systems, Madison, WI) was reviewed using the hospital encounter number as the primary identifier. Once the discharge date was determined, a list of appointments was analyzed. All appointments marked as “completed” were counted as an attendance and, therefore, adherence. Any appointments marked as “no show” were counted as an absence (nonadherence). If an appointment was canceled by the patient, but rescheduled within the 30-day window, the canceled appointment was not counted as an absence. If the appointment was canceled by the patient without evidence of rescheduling, the appointment was counted as an absence. Any appointment canceled by anyone other than the patient was not counted as an attendance or absence. Information about appointments external to the UNC system was not available.
No power calculation was performed, since expansion of the intervention group was not feasible. Statistical significance was defined as a two-sided α value of 0.05. Statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC). Descriptive statistics (student t-test and chi-square) were used to compare demographic characteristics between groups. For the primary endpoint, data were compared using a repeated measures logistic regression model to estimate the difference in the likelihood of completing an appointment between the 2 groups while controlling for homoscedasticity due to repeated appointments by the same patient.
To evaluate the possibility of secular trends over time, the same modeling technique was used to assess differences in baseline likelihood of completing an appointment. P values for comparisons between baseline years were adjusted for multiple comparisons using the Tukey method. No subcategorization was reported for the types of appointments attended, since the low number of some appointment types made it unlikely to determine a meaningful difference among them. Furthermore, not all patients had the same types of appointments. This study was approved by the UNC Institutional Review Board.
Results
Baseline demographic information is represented in Table 1. Of the 36 patients included in the prospective study by Bates et al., 32 patients were eligible for inclusion in this study.4 The original Bates et al. study enrolled 49 patients, but only 36 received 3CS. Two patients were excluded because they did not have any outpatient encounters within 30 days from the date of discharge. One patient was excluded, since they were transitioned to the acute inpatient rehabilitation unit immediately following discharge. One patient was excluded because all care was transitioned to another institution immediately following discharge. Data from included patients were compared with data from 64 control patients. An initial group of 64 control patients was randomly obtained by searching the electronic health record for patients who had received inpatient chemotherapy during the specified time frame. Eleven of these patients met the exclusion criteria, so an additional 11 patients were randomly obtained, all of which met inclusion criteria.
TABLE 1.
Baseline Characteristics
| Characteristic | Intervention Group (n = 32) | Control Group (n = 64) | P Value (t-test/chi-square) |
|---|---|---|---|
| Median age, years (range) | 58 (20-86) | 56 (21-85) | 0.9454 |
| Male sex, n (%) | 18 (56.2) | 38 (59.4) | 0.7697 |
| Race, n (%) | |||
| Caucasian | 24 (75.0) | 33 (51.6) | 0.0985 |
| African American | 5 (15.6) | 25 (39.1) | |
| Hispanic | 0 (0.0) | 1 (1.6) | |
| Other | 3 (9.4) | 5 (7.8) | |
| Previous chemotherapy, n (%) | 11 (34.4) | 14 (21.9) | 0.0995 |
| Discharge location, n (%) | |||
| Home | 28 (87.5) | 43 (67.2) | 0.1883 |
| Skilled nursing facility | 1 (3.1) | 4 (6.3) | |
| Home with home health | 3 (9.4) | 17 (26.6) | |
| Diagnosis, n (%) | |||
| Acute leukemias | 25 (78.1) | 29 (45.3) | 0.0097 |
| Chronic leukemias | 0 (0.0) | 2 (3.1) | |
| Myeloma/plasma cell leukemia | 1 (3.1) | 12 (18.8) | |
| Lymphomas | 6 (18.8) | 7 (10.9) | |
| Myeloproliferative neoplasms | 0 (0.0) | 3 (4.7) | |
| Aplastic anemia | 0 (0.0) | 2 (3.1) | |
| Solid tumors | 0 (0.0) | 9 (14.1) | |
The predominant gender of both groups was male, representing 58.3% of the total patient population. The primary race of the total patient population was Caucasian (59.4%). Home was the location to which the majority of patients were discharged (74.0%). Significant differences were observed only for the type of malignancy (P = 0.0097). The most common type of malignancies were acute leukemias (56.3%), including acute myeloid leukemia and acute lymphoblastic leukemia. A notable difference between groups was that there were no patients with solid malignancies in the treatment group, but these patients accounted for 14% of the control group.
A total of 396 and 426 appointments were scheduled for patients in the intervention group and control group, respectively. On the patient level, 81.25% of patients in the intervention group had perfect appointment attendance, while only 70.31% of patients in the control group had perfect appointment attendance (P = 0.2497). Analysis of differences among appointment types was not possible because of the small sample size and counts across many appointment types.
Results for the primary outcome of adherence to outpatient appointments are included in Figure 1. The unadjusted percentage of appointments attended in the intervention group was 98.0%, compared with 92.3% in the control group. Repeated measures logistic regression models demonstrated a statistically significant difference in odds of appointment attendance based on group with P = 0.0018. When assessing for differences between groups that could have independently contributed to differences in likelihood of appointment attendance, of the potential confounders included in data collection (see Table 1), only receipt of previous chemotherapy was significantly associated with the likelihood of appointment attendance. Adjusted models accounting for this potential confounder did not meaningfully change results (Figure 1). For the control group, there was no significant trend in the percentage of appointments attended across baseline years, with probabilities for 2014-2016 equaling 90.6%, 92.8%, and 89.3%, respectively (pairwise comparisons P = 0.4961-0.8383).
FIGURE 1.
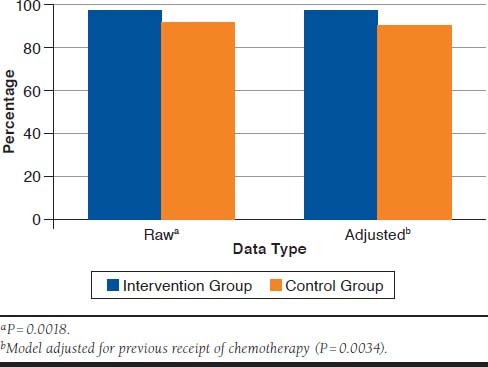
Percentage of Appointments Attended
Discussion
In this retrospective study, 3CS performed by a pharmacist was associated with an increase in the likelihood that an outpatient appointment would be attended compared with patients who had not received 3CS from a pharmacist. If applied to the 64 patients in the control group, this 5.72% increase in appointment adherence could have resulted in approximately 24 additional attended appointments. This increase in appointment adherence could have theoretically led to improved patient outcomes, better chemotherapy adherence, and increased revenue for the health system.
Limitations
Limitations of this study included the retrospective design, small sample size, the non-uniform documentation of appointment cancelation, and the inability to capture non-UNC encounters. Although cancellation by the patient was quite clear, internal personnel documentation was not always consistent with regard to cancelation notes. Many appointments were canceled with the reason “treatment plan change,” which was intentionally not counted as an absent appointment, since this was often at the provider’s discretion. Canceled appointments without a reason or a reason of “other” were also not documented to reduce the risk of a type I error. More detailed appointment cancellation documentation would strengthen the results of future studies with similar methods.
In addition, some potential confounding factors were not controlled for. These factors included variables such as in-network primary care providers; the specific types of appointments (e.g., physician, advanced practice provider, laboratory, and pharmacist); presence of insurance coverage; and geographic locations of patients relative to the clinic locations. Patients in the intervention group had a higher number of scheduled appointments per patient compared with the patients in the control group. This difference could be explained by improvements in coordination of care over time.
Improvements in arranging closer follow-up before discharge for patients with hematologic malignancies has led to more scheduled outpatient bone marrow biopsy, central line placement, transfusion, lab, advanced practice provider, and pharmacist appointments within 30 days of discharge. A specific initiative began in May 2016 to schedule follow-up visits with an advanced practice provider and pharmacist within 72 hours of hospital discharge. At the 72-hour visit, there would be another opportunity for the provider to schedule additional appointments that were needed. Based on timing, this particular initiative would have affected all the intervention patients and only some of the control patients. This and other time-related factors that may have influenced the appointment and attendance differences (e.g., potential changes in referral procedures from 2014 to 2017) were not accounted for in this study.
Conclusions
This study demonstrated an association between inpatient pharmacist-led consultation services and improved outpatient appointment adherence. This improvement of 5.72% appointment adherence may translate to better outcomes regarding patients’ malignancies, improved disease control through chemotherapy adherence, and increased revenue for the health system. Future studies with alternative service lines would be beneficial for determining which ones may benefit from services similar to 3CS. Future studies could also be designed to show the effect on revenue related to the oncology clinics and the oncology infusion clinic. Such financial studies would need to account for the revenue offset by the cost of employing pharmacists who provide the service. Confirmatory studies in hematologic malignancies or solid malignancies would also be beneficial given the small sample size and the fact that some malignancies were not shared across the groups.
ACKNOWLEDGMENTS
The authors acknowledge and thank the Pharmacy Analytics Team at the UNC Medical Center Department of Pharmacy for its support of this study.
REFERENCES
- 1.Ose D, Winkler EC, Berger S, et al. Complexity of care and strategies of self-management in patients with colorectal cancer. Patient Prefer Adherence. 2017;11:731-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Joint Commission Center for Transforming Healthcare. Transitions of care: the need for a more effective approach to continuing patient care. 2012. Available at: https://www.jointcommission.org/assets/1/18/Hot_Topics_Transitions_of_Care.pdf. Accessed April 21, 2020.
- 3.Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18(8):646-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bates JS, Auten JJ, Sketch MR, et al. Patient engagement in first cycle comprehensive chemotherapy consultation pharmacy services and impact on patient activation. J Oncol Pharm Practice. 2019;25(4):896-902. [DOI] [PubMed] [Google Scholar]
- 5.Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). 2013;32(2):223-31. [DOI] [PubMed] [Google Scholar]
- 6.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fever data on costs. Health Aff (Millwood). 2013:32(2):207-14. [DOI] [PubMed] [Google Scholar]
- 7.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4):1005-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6):1918-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes.J Gen Intern Med. 2011;27(5):520-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE, Jones C. Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? J Ambul Care Manage. 2009;32(4):320-27. [DOI] [PubMed] [Google Scholar]
- 11.Begum N, Donald M, Ozolins IZ, Dower J. Hospital admissions, emergency department utilisation and patient activation for self-management among people with diabetes. Diabetes Res Clin Pract. 2011;93(2):260-67. [DOI] [PubMed] [Google Scholar]
- 12.Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients’ ‘scores’. Health Aff (Millwood). 2013;32(2):216-22. [DOI] [PubMed] [Google Scholar]
- 13.Lam MS, Cheung N. Impact of oncology pharmacist-managed oral anticancer therapy in patients with chronic myelogenous leukemia. J Oncol Pharm Pract. 2016;22(6):741-48. [DOI] [PubMed] [Google Scholar]
- 14.McNamara E, Redoutey L, Mackler E, Severson JA, Petersen L, Mahmood T. Improving oral oncolytic patient self-management. J Oncol Pract. 2016;12(9):e864-69. [DOI] [PubMed] [Google Scholar]
- 15.Academy of Managed Care Pharmacy. Concept series paper on disease management. Available at: https://www.amcp.org/sites/default/files/2019-03/Disease%20Management.pdf. Accessed April 21, 2020.
- 16.Perez FD, Xie J, Sin A, et al. Characteristics and direct costs of academic pediatric subspecialty outpatient no-show events. J Healthc Qual. 2014;36(4):32-42. [DOI] [PubMed] [Google Scholar]
- 17.Guzek LM, Gentry SD, Golomb MR. The estimated cost of “no-shows” in an academic pediatric neurology clinic. Pediatr Neurol. 2015;52(2):198-201. [DOI] [PubMed] [Google Scholar]


