Abstract
Purpose:
To compare visual outcomes of early enhancement following small incision lenticule extraction (SMILE) versus laser in situ keratomileusis (LASIK).
Methods:
Retrospective analysis of eyes (patients operated in the setting of a tertiary eye care hospital between 2014 and 2020) requiring early enhancement (within one year of primary surgery) was conducted. Stability of refractive error, corneal tomography, and anterior segment Optical Coherence Tomography (AS-OCT) for epithelial thickness was performed. The correction post regression was done using photorefractive keratectomy and flap lift in eyes, wherein the primary procedure was SMILE and LASIK, respectively. Pre- and post enhancement corrected and uncorrected distance visual acuity (CDVA and UDVA), mean refractive spherical equivalent (MRSE), and cylinder were analyzed. IBM SPSS statistical software.
Results:
In total, 6350 and 8176 eyes post SMILE and LASIK, respectively, were analyzed. Of these, 32 eyes of 26 patients (0.5%) post SMILE and 36 eyes of 32 patients (0.44%) post-LASIK required enhancement. Post enhancement (flap lift in LASIK, and PRK in SMILE group) UDVA was logMAR 0.02 ± 0.05 and 0.09 ± 0.16 (P = 0.009), respectively. There was no significant difference between the refractive sphere (P = 0.33) and MRSE (P = 0.09). In total, 62.5% of the eyes in the SMILE group and 80.5% in the LASIK group had a UDVA of 20/20 or better (P = 0.04).
Conclusion:
PRK post SMILE demonstrated comparable results to flap lift post LASIK and is a safe and effective approach for early enhancement post SMILE.
Keywords: Enhancement, femtosecond, laser in situ keratomileusis, regression, small incision lenticule extraction
The safety and efficacy of small incision lenticule extraction (SMILE) and laser in situ keratomileusis (LASIK) for myopic correction have been well established in literature.[1,2] Earlier recovery of corneal sensitivity and superior biomechanics are potential advantages of SMILE vis-à-vis flap-based keratorefractive procedures.[3,4] These differences in corneal biomechanics and subsequent tissue remodeling can result in the varied incidences of postoperative regression. Additionally, residual error secondary to under correction or astigmatism induction may warrant a secondary enhancement procedure. Multiple factors including the magnitude of refractive error corrected, the type of laser used, and patient dissatisfaction can determine the rate of enhancement following a procedure.[5] Previous studies have reported post LASIK enhancement rates ranging from 5 to 28%.[6-9] It has been postulated that regression rates may be lower following SMILE vis-à-vis LASIK secondary to milder stromal healing response and lesser epithelial remodeling postoperatively.[10] However, the published data thus far is exceedingly limited.
The presence of a flap in LASIK allows a relift in case of early enhancement. This retreatment option, however, is not possible following SMILE, thus warranting the use of alternate methods including surface ablation,[11] thin-flap LASIK,[12] or cap-to-flap conversion with CIRCLE software.[13] The purpose of this study is to analyze the incidence of regression following LASIK and SMILE and to compare the refractive outcomes of early enhancement in these eyes (flap lift following LASIK versus surface ablation following SMILE). To our knowledge, no similar comparative analysis of visual outcomes has been published in literature thus far.
Methods
Ethics committee approval was obtained, informed consent was taken from the patients, and the study adhered to the tenets of Declaration of Helsinki. Retrospective analysis was conducted to include eyes undergoing early enhancement (within 1 year of primary procedure) following SMILE and LASIK at a tertiary eye care hospital between 2014 and 2020. Eyes with complete preoperative and intraoperative data analysis including preoperative corneal tomography, intraoperative parameters including flap or cap thickness, ablation depth, and residual stromal thickness, and a minimum postoperative follow-up of one year were included. Patients with incomplete data, loss of follow-up, intraoperative complications, and history of pregnancy were excluded from the analysis. Enhancement post SMILE was done by transepithelial photorefractive keratectomy (PRK, Wavelight EX 500, Alcon) (Group 1), while flap lift was carried out in eyes with LASIK as the primary procedure (Group 2). Eyes with intraoperative complications in the primary surgery including suction loss and decentered ablation profile were excluded from the analysis. Preoperative data analysis included slit-lamp biomicroscopic evaluation, dilated fundus evaluation, uncorrected and corrected distance visual acuity (UDVA and CDVA), treated mean refractive spherical equivalent (MRSE), and corneal tomography (Pentacam, Oculus Optikgerate, GmBH). parameters. CDVA, UDVA, and refractive error pre and post enhancement were compared between the two groups.
Statistical analysis
IBM SPSS statistical software version 23 was used for data analysis. Snellen corrected distance visual acuity measurements were converted to logarithm of the minimum angle of resolution (logMAR) equivalents for the purpose of data analysis. For normally distributed quantitative parameters, mean values were compared between study groups using an independent sample t-test (two groups). For non-normally distributed quantitative parameters, medians and Interquartile range (IQR) were compared between study groups using Mann Whitney u test (2 groups). For non-normally distributed quantitative parameters, medians and IQR were compared between preoperative and different postoperative follow-up using Wilcoxon singed rank test. P-value < 0.05 was considered as statistically significant.
Results
The retrospective analysis included 6350 and 8176 eyes which had undergone SMILE and LASIK, respectively, from 2014 till 2020. The preoperative patient demographics is provided in Table 1. Thirty-two eyes of 26 patients (0.5%) in the SMILE group (Group 1) and 36 eyes of 32 patients (0.44%) in the LASIK group (Group 2) required an enhancement procedure. Three patients (18.75%) in the SMILE cohort and two patients in the LASIK group required bilateral treatment (P = 0.37). The mean interval between the primary procedure and enhancement was 0.86 ± 0.92 years in Group 1 and 0.75 ± 0.66 years in Group 2 (P = 0.29).
Table 1.
Patient demographics
| Parameter | Small incision lenticule extraction | Laser in situ keratomileusis | p |
|---|---|---|---|
| Data analyzed (number of eyes) | 6350 | 8176 | |
| Age in years (mean±SD) | 27.78±6.51 | 31.81±8.63 | 0.01 |
| Male: Female | 13:19 | 25:11 |
Preoperative (to primary procedure) data analysis of the subset of eyes that later required enhancement is described in Table 2. A significantly higher preoperative sphere and MRSE were treated in the SMILE group (P = 0.04 and 0.03). Corrected refractive error of greater than 6D was seen in 37.5% and 13.8% of the eyes in the SMILE and LASIK group, respectively (P = 0.23).
Table 2.
Preoperative data for primary procedure
| Parameter | SMILE | LASIK | p |
|---|---|---|---|
| Mean sphere (D) | −4.17±2.5 | −3.17±2.12 | 0.04 |
| Mean cylinder (D) | −1.38±1.29 | −1.18±1.21 | 0.26 |
| Mean refractive spherical equivalent treated (Diopter) | −4.73±2.49 | −3.76±1.86 | 0.03 |
| Mean pachymetry (microns) | 531.21±25.33 | 544.52±37.6 | 0.05 |
| Mean keratometry maximum (D) | 45.95±1.33 | 46.39±5.28 | 0.32 |
Table 3 demonstrates the refractive data of the eyes prior to the enhancement procedure.
Table 3.
Refractive data prior to enhancement procedure
| Parameter | SMILE | LASIK | p |
|---|---|---|---|
| Mean sphere (D) | −0.06±0.68 | −0.34±0.82 | 0.07 |
| Mean cylinder (D) | −0.99±0.73 | −0.86±0.65 | 0.22 |
| Mean refractive spherical equivalent (Diopter) | −0.55±0.72 | −0.79±0.85 | 0.11 |
| UDVA (LogMAR) | 0.37±0.13 | 0.03±0.17 | 0.22 |
| CDVA (LogMAR) | 0.02±0.05 | 0.005±0.02 | 0.02 |
Comparison of the post enhancement data demonstrated a statistically significant difference in the UDVA between the two groups, with the LASIK group faring better (P = 0.009). Additionally, there was a significantly lower residual cylinder among the Flap LASIK group (P = 0.004). The remaining measured parameters demonstrated no significant difference between the two cohorts [Table 4].
Table 4.
Refractive data post enhancement procedure
| Parameter | Enhancement by PRK in SMILE | Enhancement by flap lift in LASIK | p |
|---|---|---|---|
| UDVA (LogMAR) | 0.09±0.16 | 0.02±0.05 | 0.009 |
| CDVA (LogMAR) | 0.03±0.05 | 0.01±0.04 | 0.06 |
| Refractive sphere (D) | 0.02±0.42 | −0.006±0.04 | 0.33 |
| Refractive cylinder (D) | −0.22±0.47 | 0±0.15 | 0.004 |
| MRSE (D) | −0.09±0.34 | −0.006±0.09 | 0.09 |
| Mean change in UDVA (LogMAR) | 0.27±0.16 | 0.31±0.18 | 0.16 |
| Mean change in CDVA (LogMAR) | −0.01±0.07 | −0.008±0.02 | 0.38 |
| Mean reduction in MRSE (D) | −0.43±0.9 | −0.79±0.84 | 0.06 |
Twenty eyes (62.5%) in the SMILE group versus 29 eyes (80.5%) in the LASIK group had a UDVA of 20/20 or better (P = 0.04). Eight eyes (25%) versus four eyes (11.11%) had a residual error post enhancement in Group 1 and 2, respectively (P = 0.06). The distribution of the residual error has been elaborated in Fig. 1.
Figure 1.
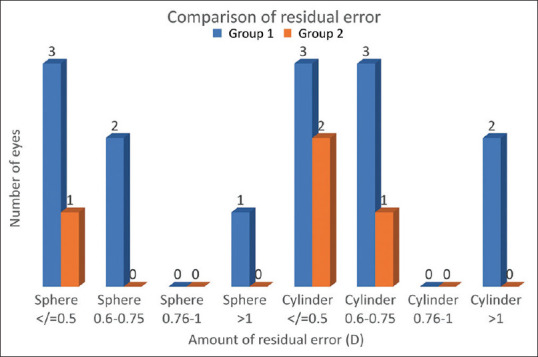
Distribution of residual error post enhancement
Discussion
Limited data regarding enhancement rates following SMILE as well as outcomes following retreatment is available in current literature. Liu and coworkers demonstrated an enhancement rate of 2.1% at one year, with similar numbers published by Siedlecki and colleagues.[11,14] Reinstein et al. reported a prevalence of 4.4%,[12] while Hjordtal and coworkers demonstrated a 20% incidence of residual error greater than 0.5D at 3 months’ postoperative period.[15] Our study demonstrates an enhancement rate of 0.5% following SMILE and 0.44% following LASIK, which is lower than the previously reported rates. Analysis of a significantly larger patient data set could be a possible explanation.
Literature review demonstrates that with SMILE, 77–92% of the eyes achieve a postoperative spherical equivalent within 0.50 D of the intended correction in low to moderate myopia, whereas this reduces up to 77–88% in high myopes.[16,17] The reduction can be attributed to an increased epithelial hyperplasia and stromal wound healing associated with high refractive correction, leading to decreased predictability, and subsequently higher enhancement rates. Similar associations between higher enhancement rates and greater corrected power are seen following LASIK.[18,19] In our study, the mean interval between the primary procedure and enhancement was found to be 0.86 ± 0.92 years following SMILE and 0.75 ± 0.66 years following LASIK. Studies have found that 71% of enhancement procedures are performed within 1 year.[11,14]
Photorefractive keratectomy as an enhancement option post SMILE is well established. The retention of the flap-free nature of SMILE is a major advantage, while postoperative pain and risk of infection and haze are the shortcomings.
Siedlecki reported 40 eyes that underwent enhancement following SMILE using laser epithelial keratomileusis with topography-guided treatment.[11] The study reported a mean pre-enhancement spherical equivalent of − 0.86 ± 0.43 D, which improved to − 0.03 ± 0.57 D at 3 months. This was comparable to the results of our study which showed an improvement of pre-enhancement MRSE from − 0.55 ± 0.72 D to − 0.09 ± 0.34 D in the SMILE group. Similar results were also seen in the LASIK group.
Liu and colleagues demonstrated an improvement of UDVA in 92.9% of the eyes following enhancement.[14] Sixty-three percent of eyes had achieved a UDVA of 20/20 in the study conducted by Siedlecki, comparable to our study results which showed 62.5% of the eyes in the SMILE group had a UDVA of 20/20. However, a higher percentage of eyes (80.5%) achieved the same in the LASIK group.
Persistent stromal haze is a visually significant complication post surface ablation procedure. The risk may be greater with higher residual errors, wherein the depth of excimer laser enhancement goes beyond the initial SMILE interface. A report by Ivarsen and coworkers demonstrated significant stromal haze in two of the five eyes that underwent enhancement post SMILE.[17] However, it is noteworthy that mitomycin C (MMC) was not used in their study, whereas in our cohort, MMC was used in all eyes following ablation and no eyes presented with significant haze.
Another common approach for SMILE enhancement is the use of CIRCLE software, converting the original cap to a flap which can be subsequently raised and the underlying stroma treated.
Siedlecki and coworkers reported the outcomes post CIRCLE in 22 eyes, with an improvement in MRSE from − 0.51 ± 1.08 D preoperative to − 0.18 ± 0.31 D at 3 months’ postoperative period.[11] A UDVA of 20/20 or better was achieved in 77.3% of the eyes. In another comparative analysis between CIRCLE and surface ablation as enhancement modalities, comparable results were demonstrated at 3 months with 83% of eyes achieving UDVA of 20/20 or better in both groups.[20] The potential advantages of CIRCLE vis-à-vis PRK include reduced postoperative pain and earlier visual recovery. However, the initial biomechanical advantage of the flap-free approach with SMILE is lost, especially in deeper cap cut.
Thin flap LASIK entails the creation of a 100-micron flap in the area of the previous SMILE cap. Reinstein demonstrated the outcomes in 100 eyes with a MRSE improvement to 0.19 ± 0.49 D at 1-year postoperative visit.[12,21] Difficulty in surgical technique, especially dissection and flap lift is a potential limitation.[22,23] Persistent haze is also another rare complication that can be expected, probably due to damage to the Bowman’s membrane.[24]
The sub-cap-lenticule-extraction technique was first reported by Donate and Thäeron, wherein a new SMILE lenticule is fashioned under the primary SMILE interface.[25] This method maintains the flap-free advantage of SMILE. Although an effective option for retreatment using a custom-made centering marker,[26] the procedure is difficult, especially in cases of low residual errors. Additionally, the outcomes and safety of the procedure have not yet proven to be equivalent to the already available enhancement options.
Our study demonstrates enhancement rates in the Indian population in a large cohort. Moreover, comparative outcomes between surface ablation following SMILE and flap lift following LASIK have not been previously published. However, the retrospective construct of the study is a potential limitation.
Our study demonstrated no significant difference in post enhancement MRSE or CDVA in both groups. However, there was a significant difference in the number of eyes achieving a UDVA of 20/20, with the LASIK group faring better. A possible hypothesis could be a more effective retreatment in the original interface plane during flap lift vis-à-vis retreatment in a new plane in the SMILE cap.
Conclusion
Photorefractive keratectomy is an easy, cost-effective approach for early enhancement post SMILE, with results comparable to flap lift following LASIK. An understanding of the patient’s expectations and adequate counselling regarding the advantages and limitations of the options is imperative.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Han T, Xu Y, Han X, Zeng L, Shang J, Chen X, et al. Three-year outcomes of small incision lenticule extraction (SMILE) and femtosecond laser-assisted laser in situ keratomileusis (FS-LASIK) for myopia and myopic astigmatism. Br J Ophthalmol. 2019;103:565–8. doi: 10.1136/bjophthalmol-2018-312140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Y, Shen Q, Jia Y, Zhou D, Zhou J. Clinical outcomes of SMILE and FS-LASIK used to treat myopia:A meta-analysis. J Refract Surg. 2016;32:256–65. doi: 10.3928/1081597X-20151111-06. [DOI] [PubMed] [Google Scholar]
- 3.Li M, Zhou Z, Shen Y, Knorz MC, Gong L, Zhou X. Comparison of corneal sensation between small incision lenticule extraction (SMILE) and femtosecond laser-assisted LASIK for myopia. J Refract Surg. 2014;30:94–100. doi: 10.3928/1081597X-20140120-04. [DOI] [PubMed] [Google Scholar]
- 4.Sinha Roy A, Dupps WJ, Jr, Roberts CJ. Comparison of biomechanical effects of small-incision lenticule extraction and laser in situ keratomileusis:Finite-element analysis. J Cataract Refract Surg. 2014;40:971–80. doi: 10.1016/j.jcrs.2013.08.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts C. The cornea is not a piece of plastic. J Refract Surg. 2000;16:407–13. doi: 10.3928/1081-597X-20000701-03. [DOI] [PubMed] [Google Scholar]
- 6.Bragheeth MA, Fares U, Dua HS. Re-treatment after laser in situ keratomileusis for correction of myopia and myopic astigmatism. Br J Ophthalmol. 2008;92:1506–10. doi: 10.1136/bjo.2008.143636. [DOI] [PubMed] [Google Scholar]
- 7.Durrie DS, Aziz AA. Lift-flap retreatment after laser in situ keratomileusis. J Refract Surg. 1999;15:150–3. doi: 10.3928/1081-597X-19990301-12. [DOI] [PubMed] [Google Scholar]
- 8.Alio JL, Muftuoglu O, Ortiz D, Perez-Santonja JJ, Artola A, Ayala MJ, et al. Ten-year follow-up of laser in situ keratomileusis for high myopia. Am J Ophthalmol. 2008;145:55–64. doi: 10.1016/j.ajo.2007.08.035. [DOI] [PubMed] [Google Scholar]
- 9.Hersh PS, Fry KL, Bishop DS. Incidence and associations of retreatment after LASIK. Ophthalmology. 2003;110:748–54. doi: 10.1016/S0161-6420(02)01981-4. [DOI] [PubMed] [Google Scholar]
- 10.Luft N, Ring MH, Dirisamer M. Corneal epithelial remodelling induced by small incision lenticule extraction (SMILE) Invest Ophthalmol Vis Sci. 2016;57:176–83. doi: 10.1167/iovs.15-18879. [DOI] [PubMed] [Google Scholar]
- 11.Siedlecki J, Luft N, Kook D, Wertheimer C, Mayer WJ, Bechmann M, et al. Enhancement after myopic small incision lenticule extraction (SMILE) using surface ablation. J Refract Surg. 2017;33:513–8. doi: 10.3928/1081597X-20170602-01. [DOI] [PubMed] [Google Scholar]
- 12.Reinstein DZ, Carp GI, Archer TJ, Vida RS. Outcomes of re-treatment by LASIK after SMILE. J Refract Surg. 2018;34:578–88. doi: 10.3928/1081597X-20180717-02. [DOI] [PubMed] [Google Scholar]
- 13.Siedlecki J, Luft N, Mayer WJ, Siedlecki M, Kook D, Meyer B, et al. CIRCLE enhancement after myopic SMILE. J Refract Surg. 2018;34:304–9. doi: 10.3928/1081597X-20180308-02. [DOI] [PubMed] [Google Scholar]
- 14.Liu YC, Rosman M, Mehta JS. Enhancement after small-incision lenticule extraction:Incidence, risk factors, and outcomes. Ophthalmology. 2017;124:813–21. doi: 10.1016/j.ophtha.2017.01.053. [DOI] [PubMed] [Google Scholar]
- 15.Hjortdal JØ, Vestergaard AH, Ivarsen A, Ragunathan S, Asp S. Predictors for the outcome of small-incision lenticule extraction for myopia. J Refract Surg. 2012;28:865–71. doi: 10.3928/1081597X-20121115-01. [DOI] [PubMed] [Google Scholar]
- 16.Chan C, Lawless M, Sutton G, Versace P, Hodge C. Small incision lenticule extraction (SMILE) in 2015. Clin Exp Optom. 2016;99:204–12. doi: 10.1111/cxo.12380. [DOI] [PubMed] [Google Scholar]
- 17.Ivarsen A, Hjortdal J. Correction of myopic astigmatism with small incision lenticule extraction. J Refract Surg. 2014;30:240–7. doi: 10.3928/1081597X-20140320-02. [DOI] [PubMed] [Google Scholar]
- 18.Perlman EM, Reinert SE. Factors influencing the need for enhancement after laser in situ keratomileusis. J Refract Surg. 2004;20:783–9. doi: 10.3928/1081-597X-20041101-05. [DOI] [PubMed] [Google Scholar]
- 19.Randleman JB, White AJ, Jr, Lynn MJ. Incidence, outcomes, and risk factors for retreatment after wavefront optimized ablations with PRK and LASIK. J Refract Surg. 2009;25:273–6. doi: 10.3928/1081597X-20090301-06. [DOI] [PubMed] [Google Scholar]
- 20.Siedlecki J, Siedlecki M, Luft N, Kook D, Meyer B, Bechmann M, et al. Surface ablation vs. CIRCLE for myopic enhancement after SMILE:A matched comparative study. J Refract Surg. 2019;35:294–300. doi: 10.3928/1081597X-20190416-02. [DOI] [PubMed] [Google Scholar]
- 21.Reinstein DZ, Carp GI, Archer TJ, Vida RS. Inferior pseudo-hinge fulcrum technique and intraoperative complications of laser in situ keratomileusis retreatment after small-incision lenticule extraction. J Cataract Refract Surg. 2018;44:1355–62. doi: 10.1016/j.jcrs.2018.07.051. [DOI] [PubMed] [Google Scholar]
- 22.Chansue E, Tanehsakdi M, Swasdibutra S. Safety and efficacy of VisuMax(R) circle patterns for flap creation and enhancement following small incision lenticule extraction. Eye Vis (Lond) 2015;2:21. doi: 10.1186/s40662-015-0031-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang JS. Complications of sub-Bowman's keratomileusis with a femtosecond laser in 3009 eyes. J Refract Surg. 2008;24:S97–S101. doi: 10.3928/1081597X-20080101-17. [DOI] [PubMed] [Google Scholar]
- 24.Hafezi F, Seiler T. Persistent subepithelial haze in thin-flap LASIK. J Refract Surg. 2010;26:222–5. doi: 10.3928/1081597X-20090930-02. [DOI] [PubMed] [Google Scholar]
- 25.Donate D, Thaeron R. Preliminary evidence of successful enhancement after a primary SMILE procedure with the sub-cap-lenticule-extraction technique. J Refract Surg. 2015;31:708–10. doi: 10.3928/1081597X-20150928-04. [DOI] [PubMed] [Google Scholar]
- 26.Sedky AN, Wahba SS, Roshdy MM, Ayaad NR. Cap-preserving SMILE enhancement surgery. BMC Ophthalmol. 2018;18:49. doi: 10.1186/s12886-018-0712-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


