Abstract
We report two adult cases of abducens nerve palsy presenting immediately (within weeks) after they received the first dose of Covishield vaccination. Magnetic resonance imaging (MRI) of the brain obtained after the onset of diplopia demonstrated demyelinating changes. The patients had associated systemic symptoms. Post-vaccination demyelination typically known as acute disseminated encephalomyelitis (ADEM) associated with several vaccines is more common in children. Although the mechanism of the nerve palsy remains unclear, it is suspected to be related to the post-vaccine neuroinflammatory syndrome. Cranial nerve palsies and ADEM-like presentations may represent part of the neurologic spectrum following COVID-vaccination in adults, and ophthalmologists should be aware of these sequelae. Although cases of sixth nerve palsy following COVID vaccination are already reported, associated MRI changes have not been reported from India.
Keywords: Abducens nerve palsy, acute disseminated encephalomyelitis, ADEM, adverse event, COVID-19 vaccination, COVID-19, demyelinating changes post-COVID-19 vaccination, MRI findings post-COVID-19 vaccine
Acute disseminated encephalomyelitis (ADEM) is a demyelinating disorder of the central nervous system that occurs in close association with either a preceding infection or following vaccination.[1]ADEM has an estimated annual incidence of 0.8 per 100,000.[2] Although ADEM can occur at any age, it is more common in children following vaccinations.[3] The presumptive mechanism is immune-mediated demyelination although immune-complex mediated vasculopathy has also been postulated.[3] Spontaneous recovery or improvement after corticosteroids has been reported for post-vaccination ADEM.[3]
Herein, we report two adult patients with no previous history of neurological disorder who developed abducens nerve palsy with ADEM-like changes after receiving inactivated COVID-19 vaccination. The authors adhered to the tenets of the Declaration of Helsinki and the study was approved by both Institutional Ethics Committee and Review boards.
Case Reports
Case 1
A 35-year-male patient presented with sudden-onset diplopia with a headache for 3 days. He denied a history of trauma or recent illness. He gave a history of receiving his first dose of COVID-19 vaccination (Covishield, Serum Institute of India) 7 days before the onset of symptoms. His best-corrected visual acuity (BCVA) was 20/20 in both eyes (BE). On ocular examination, he had left eye (LE) esotropia (Prism Cover Test 40 PD) with an abduction deficit of −4 [Fig. 1]. Dilated fundus examination was unremarkable. Systemic examination revealed the mild weakness of the right upper limb (Medical research council (MRc) grading scale 4/5) with an unremarkable sensory examination. Neuroimaging (MRI) revealed the ill-defined area of hypointense on T1W and hyperintense on T2W images with perilesional Fluid-attenuated inversion recovery (FLAIR) hyperintensity involving the left frontal cortical gray matter, left posterior occipital lobe, and adjoining sulcal spaces [Fig. 2]. Reverse transcription-polymerase chain reaction (RT-PCR) for COVID was negative. All blood investigations, including complete blood count, fasting blood sugar, and antinuclear antibodies (ANA) were normal.
Figure 1.
Patient 1 showing (a) Full dextroversion of both eyes. (b) Left eye esodeviation. (c) Left eye abduction deficit
Figure 2.
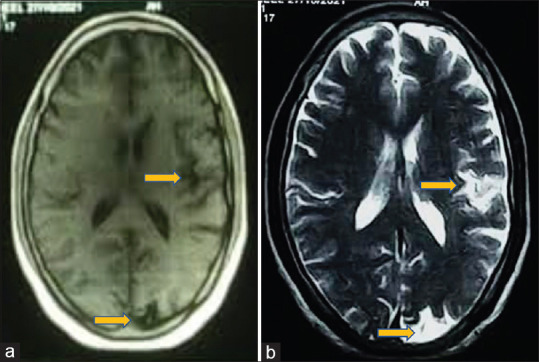
(a) T1W image showing hypointense lesions. (b) Corresponding T2W images show hyperintense lesions involving the left frontal cortical gray matter, left posterior occipital lobe, and adjoining sulcal spaces (indicated by yellow arrows)
Case 2
A 32-year-male patient was referred for acute-onset diplopia for 1 week with a history of receiving the first dose of COVID-19 vaccination (Covishield, Serum Institute) 5 days before the onset of symptom. He gave a history of a single episode of tonic–clonic seizure associated with fever 3 days post-vaccination. He denied a history of trauma or associated headaches. His BCVA in BE was 20/20. On ocular examination, he had right eye (RE) esotropia (Prism Cover Test 45 PD) with slow abducting saccades on dextroversion [Fig. 3a] with normal fundus findings. The rest of the neurological examination at the presentation was unremarkable. His neuroimaging (MRI) revealed multiple small hyperintensities in bilateral frontoparietal and left temporal periventricular white matter on T2W/FLAIR suggestive of demyelination [Fig. 3b].
Figure 3.
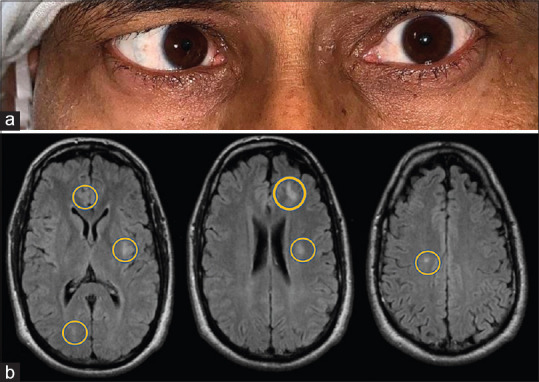
(a) Patient 2 with right eye esotropia. (b) T2/FLAIR images showing multiple hyperintense lesions involving the bilateral frontoparietal lobe, and left temporal lobe (indicated by yellow circles)
Neurologist consultation was taken to rule out other infectious and inflammatory demyelinating etiologies (Cerebro-spinal fluid (CSF) analysis was unremarkable) for both patients and they were given a trial of intravenous methylprednisolone (1 g/day) along with intravenous ceftriaxone for 5 days followed by oral steroid (1 mg/kg) bodyweight for 7 days along with the occlusive patch to avoid diplopia. On follow-up at 3 weeks, both patients showed near complete recovery.
Discussion
Covishield is a vector vaccine, which delivers genetic material (S protein) into the human body once injected. Once the cells display the S proteins on their surfaces, the immune system responds by creating antibodies and defensive white blood cells.[4]
Although it is now well known that there is a myriad of ophthalmic manifestations post-COVID-19 vaccination, the causal relationship is still a mystery.[5,6] Fortunately, these signs and symptoms are transient and have a good prognosis when diagnosed and treated early. Abducens nerve palsy has also been reported following vaccination but without any associated MRI brain findings.[5,6] Our patients also presented with acute abducens nerve palsy but with remarkable MRI brain changes such as that of ADEM, however, without any signs of encephalopathy. Such atypical neuroimaging changes post-vaccination has been labeled as ADEM-like presentation.[7] The cases had symptoms such as headaches, muscle stiffness, extremity weakness, fever, and more restricted lesions in the brain, but not a seizure.
Conclusion
In conclusion, an ADEM-like presentation in adults similar to our cases following SARSCoV-2 vaccination, although rare but important for the clinician to be aware of patients receiving this vaccine to initiate the appropriate treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Boesen MS, Blinkenberg M, Koch-Henriksen N, Thygesen LC, Uldall PV, Magyari M, et al. Implications of the International Paediatric Multiple Sclerosis Study Group consensus criteria for paediatric acute disseminated encephalomyelitis:A nationwide validation study. Dev Med Child Neurol. 2018;60:1123–31. doi: 10.1111/dmcn.13798. [DOI] [PubMed] [Google Scholar]
- 2.Menge T, Kiesseier B. C, Nessler S. Acute disseminated encephalomyelitis:An acute hit against the brain. CurrOpinNeurol. 2007;20:247–54. doi: 10.1097/WCO.0b013e3280f31b45. [DOI] [PubMed] [Google Scholar]
- 3.Hull TP, Bates JH. Optic neuritis after influenza vaccination. Am J Ophthalmol. 1997;124:703–4. doi: 10.1016/s0002-9394(14)70918-3. [DOI] [PubMed] [Google Scholar]
- 4.Understanding how COVID-19 vaccines work. Centres for Disease Control and Prevention. [Last accessed on 2022 Feb 11]. Available from:https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/how-they-work.html .
- 5.Neelam P, Devendra M, Meenakshi R, Padmavathy S. Ophthalmic complications of COVID-19 vaccination. Indian Journal of Ophthalmology. 2021;69:2900–2. doi: 10.4103/ijo.IJO_2122_21. DOI:10.4103/ijo. IJO_2122_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pawar N, Ravindran M, Padmavathy S, Chakrabarty S. Acute abducens nerve palsy after COVID-19 vaccination in a young adult. Indian J Ophthalmol. 2021;69:3764–6. doi: 10.4103/ijo.IJO_1968_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ozgen Kenangil G, Ari BC, Guler C, Demir MK. Acute disseminated encephalomyelitis-like presentation after an inactivated coronavirus vaccine. Acta Neurol Belg. 2021;121:1089–91. doi: 10.1007/s13760-021-01699-x. [DOI] [PMC free article] [PubMed] [Google Scholar]



