Abstract
Purpose:
Our study’s goal was to investigate the individuals who took a pre-military examination and were pronounced “unfit for military service,” in terms of etiological grouping, legal blindness, and whether or not the illness could have been prevented.
Methods:
The files of 174 individuals deemed “unfit for military service” due to eye disease at the State Hospital Ophthalmology Department between January 2018 and January 2022 were retrospectively evaluated. The disorders were classified as refractive error, strabismus, amblyopia-related, congenital, hereditary, infectious/inflammatory, degenerative, and trauma-related pathologies. The reasons for unsuitability for military service were classified according to monocular and binocular legal blindness, preventability, and treatability with early diagnosis.
Results:
In our study, the reasons associated with refractive error, strabismus, and amblyopia were placed first in the etiology of unsuitability for military service (40.2%). The next most prevalent condition was trauma (19.5%), which was followed by degenerative (18.4%), congenital (10.9%), hereditary (6.9%), and infectious/inflammatory disorders (4.0%). There was a history of penetrating trauma in 79.4% of trauma patients and blunt trauma in 20.6% of patients. When the etiology was evaluated, 19.5% were in preventable and 51.2% were in treatable group with early diagnosis. In our study, legal blindness was detected in 116 patients. Of these patients, 79% had monocular legal blindness and 21% had binocular legal blindness.
Conclusion:
It is vital to investigate the etiology of visual disorders, control preventable causes, and determine the methods that will provide early diagnosis and treatment of curable causes.
Keywords: Blindness, military medicine, military personnel, vision disorders
According to the Military Law governing the recruitment of Turkish military forces, men aged 20 and older are required to perform military duty. However, citizens who are found to be unfit for military service in their health examinations are exempt from this obligation according to the Turkish Armed Forces Health Capability Regulation.[1] The etiology, frequency, distribution, and preventability of pathologies identified during the examination performed for this purpose are crucial for establishing the distribution of eye diseases among young male patients. Due to the fact that the group covered in the study consists of young men in their productive years, low vision and eye diseases in this group can cause socioeconomic and psychosocial issues for both the individuals and society. By highlighting the diseases that can be prevented and treated with early diagnosis, it is intended that the examination of this study group would increase awareness to prevent workforce loss and psychosocial issues.
According to the Turkish Armed Forces Health Capability Regulation, eligibility for military duty in terms of health is evaluated for those of mandatory military age. Eye diseases that reduce visual acuity are categorized as follows; eyelid diseases (item 2), trachoma and other cicatricial diseases (item 3), lacrimal sac diseases (item 4), strabismus and nystagmus (item 5), anterior segment diseases (item 6) refraction defects and anisometropic amblyopia (item 7), color vision disorders and albinism (item 8) and posterior segment diseases, deterioration of the anatomical integrity of the eye and glaucoma (item 9).[1] Before 2016, the pre-military medical examination was only administered in military hospitals. Since then, it has been administered in all state hospitals. In our study, it was aimed to examine and group the patients who had applied to our clinic for the purpose of pre-military examination and who were given a decision as “not suitable for military service,” and to evaluate them in terms of legal blindness and preventability.
Methods
The study was done in conformity with the Declaration of Helsinki’s principles. The files of patients who had applied to our eye clinic for a pre-military medical examination between January 2018 and January 2022 and were deemed “not suitable for military service” were reviewed retrospectively. A total of 174 patient files of those who were examined and deemed unfit for service were included in the study.
Patients’ demographic information, presence of systemic disease, refraction values, best corrected visual acuity (BCVA) with Snellen chart, anterior segment examinations, and fundus examination results were recorded from the file data. In the study of the disorders, the results of optical coherence tomography, corneal topography, visual field, and fundus fluorescein angiography tests were also reviewed, if necessary.
According to the Turkish Armed Forces Health Capability Regulation, the decision “not suitable for military service” was made in the following situations: [1]
An eye disease with sequelae is characterized by a BCVA <0.2 on the Snellen chart in one eye, regardless of the vision in the other eye.
An eye disease with sequelae that reduced the total BCVA in both eyes to less than 10/10 on the Snellen chart
Refractive error of 14.00 D or greater in both eyes
Spherical equivalent (SE) difference between two eyes 6.25 D or greater for myopia and 4.25 D or greater for hyperopia and astigmatism
Retinitis pigmentosa disease.
Diseases causing unsuitability for military service were divided into six groups as follows: refractive errors/strabismus/amblyopia-related diseases, congenital diseases, hereditary diseases, infectious/inflammatory diseases, degenerative diseases, and trauma-related pathologies. Disability etiologies were also evaluated separately for patients with and without legal blindness. After all necessary corrections were made in our study, patients with a BCVA of 0.1 or less were accepted into the legal blindness group, considering their monocular or binocular status.
Diseases that could be prevented and treated with early diagnosis were also analyzed. Trauma-related diseases were considered in the preventable group. Amblyopia, keratoconus, congenital cataract, and congenital ptosis were classified as curable with early diagnosis, as early detection determines the visual prognosis of the patient.
Results
The study comprised 174 people who were assessed at our clinic between January 2018 and January 2022 and deemed unfit for military service. The mean age of the patients was 25.99 ± 4.89 years and all patients were male. Only three of the patients had systemic disease (epilepsy in two patients and muscular dystrophy in one patient), while the others did not have systemic disease.
In our study, refractive errors, strabismus, and amblyopia topped the list of causes for unsuitability for military service (n = 70, 40.2%). Then, the order of prevalence was trauma (n = 34, 19.5%), degenerative (n = 32, 18.4%), congenital (n = 19, 10.9%), hereditary (n = 12, 6.9%), and infectious/inflammatory (n = 7, 4.0%) diseases [Fig. 1].
Figure 1.
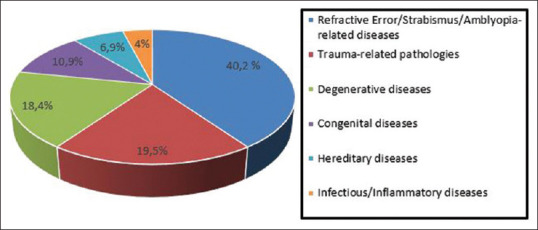
Distribution of etiologies that lead to unsuitability for military service
The diseases categorized as refractive errors, strabismus, and amblyopia were grouped as anisometropic amblyopia, high refractive error, and strabismus-related amblyopia. Twenty-six patients with anisometropic amblyopia were evaluated: eight patients had myopic astigmatism, seven patients mixed astigmatism, five patients hyperopic astigmatism, four patients hyperopia, and two patients had myopia. Of the patients who were deemed unfit due to high refractive error (n = 28), nine were associated with degenerative myopia, eight with myopic astigmatism, six with myopia, four with hyperopia, and one with hyperopic astigmatism. Thirteen of the 16 individuals with strabismus-related amblyopia were linked with esotropia, two with exotropia, and one with strabismus syndromes.
Trauma-related diseases are the second most prevalent disorders. Trauma patients were classified as those with blunt (n = 27, 79.4%) and penetrating (n = 7, 20.6%) trauma. The number and percentage of diseases are shown in Table 1. In the third position in the order of frequency, there is a group of degenerative diseases consisting of keratoconus patients. While congenital, hereditary, and infectious/inflammatory causes are ranked fourth, fifth, and sixth, respectively, the numbers and percentages of diseases in these groups are shown in Table 1.
Table 1.
Classification of reasons for unsuitability for military service
| Patients not suitable for military, n=174 (100%) | |
|---|---|
|
| |
| Traumatic group, n=34 (19.5%) | Nontraumatic group, n=140 (80.5%) |
| Corneal nephelion, n=11 (6.3%) Traumatic retinal detachment, n=6 (3.4%) Trauma-related evisceration, n=5 (2.9%) Corneal and retinal scar, n=3 (1.7%) Traumatic macular hole, n=2 (1.1%) Traumatic retinal scar, n=2 (1.1%) Phthisis bulbi, n=2 (1.1%) Traumatic cataract, n=1 (0.6%) Aphakia, n=1 (0.6%) Traumatic optic atrophy, n=1 (0.6%) |
Refractive errors, strabismus, and amblyopia-related diseases, n=70 (40.2%) Anisometropic amblyopia, n=26 (14.9%) Strabismus-related amblyopia, n=16 (9.2%) High refraction, n=28 (16.1%) |
| Degenerative diseases, n=32 (18.4%) Keratoconus, n=32 (18.4%) | |
| Congenital diseases, n=19 (10.9%) Nystagmus, n=7 (4%) Congenital cataract, n=6 (3.4%) Congenital glaucoma, n=3 (1.7%) Congenital ptosis, n=1 (0.6%) Microphthalmia, n=1 (0.6%) Anophthalmia, n=1 (0.6%) | |
| Hereditary diseases, n=12 (6.9%) Retinitis pigmentosa, n=7 (4%) Hereditary optic atrophy, n=2 (1.1%) Fundus dystrophy, n=2 (1.1%) Retinoblastoma, n=1 (0.6%) | |
| Infectious/inflammatory diseases, n=7 (4%) Corneal leukoma, n=3 (1.7%) Phthisis bulbi, n=2 (1.1%) Uveitis sequelae, n=2 (1.1%) | |
In terms of preventability and treatability with early diagnosis, there were 34 (19.5%) trauma patients in the preventable group and 89 (51.2%) patients in the group treated with early diagnosis (amblyopia n = 50, congenital cataract n = 6, congenital ptosis n = 1, and keratoconus n = 32).
In our study, 116 people were diagnosed with legal blindness. Monocular blindness was detected in 79% (n = 92) and binocular legal blindness in 21% (n = 24). The most common causes of monocular legal blindness were trauma-related disorders (34.8%), followed by refraction, strabismus, and amblyopia-related causes (31.5%) and degenerative diseases (13%). The most prevalent causes of binocular legal blindness were determined to be congenital diseases (37.5%), followed by refraction, strabismus, and amblyopia-related causes (33.3%) and genetic diseases (20.8%).
Discussion
The test population for pre-military health examinations is the young, productive male population. Due to this, vision impairment and eye problems in this group may result in economic and psychosocial issues for the person and society.
In our study, refractive errors, strabismus, and amblyopia-related diseases were the most common causes of unsuitability among all etiological factors (40.2%). The most common refractive error was myopic astigmatism. In their studies analyzing the causes of unsuitability for military service, Durukan et al.[2] and Karaca and Usta[3] found the most common cause to be refractive error, similar to our finding, and reported that myopic astigmatism was the most common refractive defect. Also, in their study analyzing the causes of unsuitability for military service, the most common cause was found as refractive error, similar to our results, and they reported that myopic astigmatism was the most common refractive defect. Mutlu Sönmez and Ertan[4] identified hypermetropic astigmatism as the most prevalent refractive error and amblyopia as the most common reason of unsuitability for military service. Studies demonstrate that the cost of providing the training and constructing and managing the necessary facilities to address visual impairment due to uncorrected refractive error is a small proportion of the global loss of productivity associated with visual impairment.[5] The favorable visual prognosis associated with the early detection of refractive problems and amblyopia demonstrates the significance of screening programs and routine eye examinations.[6] Our nation has adopted the “National Vision Screening Program” since 2016 to plan for the early detection and treatment of prevalent pediatric eye illnesses.[7]
Eye trauma was the second most common cause of unsuitability in our study. In the study in which they evaluated the reasons for unsuitability for military service in and around Bitlis, Köylü et al.[8] discovered that trauma was the most common reason for unsuitability. Eye trauma can cause problems that lead to visual loss in both childhood and adulthood. The prevalence and severity of eye injuries are influenced by socioeconomic and geographic factors, social structure, and individual awareness. According to reports, 90% of eye injuries are preventable.[9] It has been reported that 20%–59% of all ocular traumas occur in childhood due to the limitations of children in detecting risks compared to adults and their facial morphology being more vulnerable to damage. Due to the potential for visual immaturity and amblyopia, the effects of eye injuries in childhood are worse than in adults.[10] Raising the awareness of parents and caregivers about issues such as protective measures against potential risks in childhood, the use of protective glasses during sports activities, and the need for supervision when using potentially dangerous appliances in the home environment helps prevent negative outcomes that may result from eye trauma in children. Adults, especially those working in high-risk jobs, should be made aware of the need to use protective equipment. It has been reported that 90% of eye injuries can be prevented by the use of appropriate safety glasses at work.[11] In addition, workplaces should be designed with occupational health and safety in mind, and both employers and employees should get training in this area.
All of our patients who were deemed unfit for military service as a result of degenerative disorders had keratoconus. We found a significant prevalence of keratoconus, 18.4%, among all the illnesses investigated. In their study, Köylü et al.[8] reported that the most common causes of legal blindness and severe visual impairment were fundus dystrophy, congenital cataract, and keratoconus. It is known that the incidence of keratoconus increases due to environmental factors such as sun exposure, the amount of dust that induces eye rubbing in dry climates, and the amount of pollen that induces allergies.[12] The population which was evaluated in our study is geographically close to Köylü et al.’s[8] study population. The high prevalence of keratoconus in both studies may be attributable to regional environmental triggers. Early diagnosis and treatment of keratoconus disease is essential for preventing progression and improving visual prognosis.[13]
When evaluating congenital diseases, we discovered that congenital nystagmus (4%), followed by congenital cataract (3.4%) were the most prevalent. Mutlu Sönmez and Ertan[4] reported in their study that nystagmus was the most prevalent disease in the congenital diseases group, followed by pseudophakia due to congenital cataract.
In the population evaluated in our study, the total prevalence of preventable (19.5%) and treatable (51.2%) diseases with early diagnosis was 70.7%. In their investigation of the etiology of childhood blindness in Turkey, Cetin et al.[14] found that in 69.6% of children, the reasons for visual impairment were preventable or treatable. The high prevalence rate in our study is significant in terms of emphasizing the frequency of the diseases that can be prevented and treated with early diagnosis of visual impairment.
Conclusion
Findings of our study showed that as a result of the etiological categorization and analysis of the pre-military eye examination results of young, productive men, it is possible to reduce the majority of the individual, social, and economic losses caused by visual impairments through education and social control mechanisms. It is vital to investigate the etiology of visual disorders, control the preventable causes, and determine the methods that will provide early diagnosis and treatment of curable causes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Türk SilahlıKuvvetleri Sağlık Yeteneği Yönetmeliği. [Last addressed on 2022 Aug 05]. Available from:https://www.mevzuat.gov.tr/MevzuatMetin/21.5.20169431.pdf .
- 2.Durukan AH, Mumcuoğlu T, Hürmeriç V, Köksal S, Bayraktar MZ. Göz HastalıklarıNedeniyle Askerliğe Elverişli Değildir KararıAlmışYükümlülerin Tanısal Yönden Değerlendirilmesi. Gülhane Tıp Derg. 2005;47:44–48. [Google Scholar]
- 3.Karaca U, Usta G. Bir Göz HastalıklarıUzmanınca Askerliğe Elverişsiz Olduğu KararıVerilen Yükümlülerin Etyolojik Değerlendirmesi. SDÜTıp Fakültesi Derg. 2021 doi:10.17343/SDUTFD.506691. [Google Scholar]
- 4.Mutlu Sönmez M, Ertan E. Göz HastalıklarıAçısından Askerliğe Elverişsiz Olduğu KararıVerilen Yükümlülerin Etiyolojik Değerlendirmesi:Kesitsel Araştırma. Türkiye Klin Oftalmol Derg. 2021;30:191–5. [Google Scholar]
- 5.Fricke TR, Holden BA, Wilson DA, Schlenther G, Naidoo KS, Resnikoff S, et al. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ. 2012;90:728–38. doi: 10.2471/BLT.12.104034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hunter D, Cotter S. Early diagnosis of amblyopia. Vis Neurosci. 2018;35:E013. doi: 10.1017/S0952523817000207. [DOI] [PubMed] [Google Scholar]
- 7.Şahin T, Buyru Y. Çocuklarda Ambliyopi ve Ülkemizdeki Görme Tarama Programı. Ortadoğu Tıp Derg. 2017;9:79–87. [Google Scholar]
- 8.Köylü MT, Gökhan Ö, Tarkan M, Gökçen G. Bitlis ili ve çevresinde askerlik çağındaki gençerkeklerin yasal körlük ve şiddetli görme bozukluğu sebepleri. Gülhane Tıp Derg. 2016;58:157–60. [Google Scholar]
- 9.Hoskin AK, Watson SL. Ocular trauma and prevention measures. Clin Exp Ophthalmol. 2020;48:875–6. doi: 10.1111/ceo.13850. [DOI] [PubMed] [Google Scholar]
- 10.Hoskin AK, Philip SS, Yardley AME, MacKey DA. Eye ınjury prevention for the pediatric population. Asia Pac J Ophthalmol (Phila) 2016;5:202–11. doi: 10.1097/APO.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 11.Sahraravand A, Haavisto AK, Puska P, Leivo T. Work tool-related eye injuries:Helsinki ocular trauma study. Int Ophthalmol. 2020;40:753–61. doi: 10.1007/s10792-019-01237-y. [DOI] [PubMed] [Google Scholar]
- 12.Gordon-Shaag A, Millodot M, Shneor E, Liu Y. The genetic and environmental factors for keratoconus. Biomed Res Int. 2015;2015 doi: 10.1155/2015/795738. doi:10.1155/2015/795738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santodomingo-Rubido J, Carracedo G, Suzaki A, Villa-Collar C, Vincent SJ, Wolffsohn JS. Keratoconus:An updated review. Cont Lens Anterior Eye. 2022;45:101559. doi: 10.1016/j.clae.2021.101559. [DOI] [PubMed] [Google Scholar]
- 14.Cetin E, Yaman A, Berk AT. Etiology of childhood blindness in Izmir, Turkey. Eur J Ophthalmol. 2004;14:531–7. doi: 10.1177/112067210401400613. [DOI] [PubMed] [Google Scholar]


