Abstract
Background
Obesity is a growing, global public health issue. This study aimed to describe the weight management strategies used by a sample of Australian adults; examine the socio-demographic characteristics of using each strategy; and examine whether use of each strategy was associated with 12-month weight change.
Methods
This observational study involved a community-based sample of 375 healthy adults (mean age: 40.1 ± 5.8 years, 56.8% female). Participants wore a Fitbit activity monitor, weighed themselves daily, and completed eight online surveys on socio-demographic characteristics. Participants also recalled their use of weight management strategies over the past month, at 8 timepoints during the 12-month study period.
Results
Most participants (81%) reported using at least one weight management strategy, with exercise/physical activity being the most common strategy at each timepoint (40–54%). Those who accepted their current bodyweight were less likely to use at least one weight management strategy (Odds ratio = 0.38, 95% CI = 0.22–0.64, p < 0.01) and those who reported being physically active for weight maintenance had a greater reduction in bodyweight, than those who did not (between group difference: -1.2 kg, p < 0.01). The use of supplements and fasting were associated with poorer mental health and quality of life outcomes (p < 0.01).
Conclusions
The use of weight management strategies appears to be common. Being physically active was associated with greater weight loss. Individuals who accepted their current body weight were less likely to use weight management strategies. Fasting and the use of supplements were associated with poorer mental health. Promoting physical activity as a weight management strategy appears important, particularly considering its multiple health benefits.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-16277-4.
Keywords: Diet, Physical activity, Weight management, Weight loss, Obesity
Background
Overweight and obesity is a growing, global public health issue, with high rates in high-, middle- and low-income countries [1–3]. Worldwide, 52% of adults aged 18 years and over are overweight or obese, with worldwide prevalence almost tripling between 1975 and 2016 [3]. Over these years in Australia, the prevalence of overweight and obesity in adults increased from 57 to 67%, accounting for 8.4% of the total burden of disease, which is a measure of the years of healthy life lost from living with ill health or dying prematurely from disease and injury [4]. These rates are of public health concern because individuals who are overweight or obese are at increased risk of various comorbid conditions, including cardiovascular disease, gastrointestinal disorders, type 2 diabetes, joint and muscular disorders, respiratory problems, psychological issues, morbidity, mortality, and higher health care costs [5–9].
The increased prevalence of overweight and obesity has contributed to an increased need for effective weight management strategies [10]. A previous systematic review of observational and intervention studies found that, while the strength of evidence is low for all weight management strategies, beneficial strategies include dietary changes (e.g., low-fat diets, eating less fast-food, eating more fruits and vegetables), as well as monitoring intensity during exercise, and participation in group lifestyle sessions with reminder text messages [11]. Cross-sectional findings from a sample of Australian general practitioner patients (n = 1335 adults) reported that 50% had tried to lose weight in the previous 12 months [12]. Of those, 72% reported changing their diet, 54% increased their physical activity or exercise, 7.5% used a professional weight loss program, 6.5% used over-the-counter weight loss supplements and 1.7% used medication [12]. Further, findings from a population-based prospective cohort (the Australian Longitudinal Study of Women’s Health) found that 74% of women (aged 45–52 years) actively used at least one strategy to manage their weight, with decreasing food quantity, cutting down on fats and sugars, using a commercial weight loss program, and exercise associated with preventing weight gain in 2007 [13]. However, these studies of various weight control strategies either did not involve assessment of associated changes in bodyweight [12] or evaluated women only [13]. Therefore, the aims of this study are to: (i) describe the weight management strategies used by a sample of Australian adults; (ii) examine the psychosocial and demographic characteristics of those who used each strategy; and (iii) examine whether use of weight management strategies was associated with weight change over a 12-month period.
Methods
Study design
The “Annual Rhythms In Adults’ lifestyle and health” (ARIA) [14] study was a prospective cohort study that followed participants over a 12-month period to assess daily activity, dietary intake, weight and wellbeing. The study protocol has been registered on the Australian New Zealand Clinical Trial Registry (ACTRN12619001430123, 16/10/2019). The study was approved by the University of South Australia Human Research Ethics committee (Protocol number: 201,901). Participants provided written informed consent prior to enrolment and this project was conducted in accordance with the Declaration of Helsinki [15].
Participants and procedure
A community-based sample of 375 healthy adults, defined as not experiencing or receiving treatment for any life-threatening condition impacting daily lifestyle and health, was recruited from the greater metropolitan Adelaide area, South Australia. Participants were either parents of children who were enrolled in a previous cohort study evaluating children’s lifestyles (Life on Holidays Study [16]; cohorts 1 and 2, N = 119), or were parents of primary school children recruited from the community. An additional cohort (cohort 3, N = 256) of parents of primary school children were recruited from the community to reach the study’s target sample. Recruitment involved social media, community notice boards and mainstream media (cohort 3, N = 256). Recruitment involved 2 waves: Cohort 1 commenced data collection on December 1st, 2019, and cohorts 2 and 3 commenced data collection on December 1st, 2020. Eligibility criteria were: (i) 18 to 65 years old; (ii) living in greater metropolitan Adelaide, Australia; (iii) access to a Bluetooth-enabled mobile device or computer with home internet; (iv) proficiency in English; and (v) ambulant. Participants were excluded if they were (i) pregnant, (ii) had an implanted electronic medical device, or (iii) they were experiencing or receiving treatment for any life-threatening condition impacting daily lifestyle and health. An in-person home visit was conducted at baseline where the research staff gave participants a Fitbit Charge 3 activity monitor and Aria 2 or Aria Air body weight scale (Fitbit Inc, San Francisco, CA, USA). Participants were requested to wear the activity monitor and weigh themselves daily for the 12-month study period. In addition, they were asked to complete eight online surveys regarding their dietary intake, work status, recreational activities, weight loss intention, use of weight management strategies and wellbeing in the past month (timepoints: 1: mid-December; 2: mid-January; 3: mid-March; 4: mid-April; 5: mid-June; 6: mid-August; 7: mid-October; 8: mid-December [the following year]). Height measurements were also undertaken, and participants completed a self-report baseline demographics, health and lifestyle survey.
Variables
Demographics
Demographic characteristics were reported at baseline. These included date of birth, sex, country of birth, marital status (never married, widowed, divorced, separated, married), number of children at home, highest education level (below year 10, year 10, year 11, year 12 or equivalent, certificate III/IV, advanced diploma/diploma, bachelor degree, postgraduate or higher degree), gross household income (AUD; <$50,000, $50,000-$99,999, $100,000-$199,999, >$200,000), occupation (open-ended response classified according to the Australian and New Zealand Standard Classification of Occupations [17]), hours worked per week (none, < 15, 15–35, 36+) and smoking status (yes, no). Height was measured at the baseline home visit (Leister Height Measure MKII).
Body weight
Body weight was assessed using Fitbit Aria 2 smart scales (Fitbit Inc, San Francisco, CA, USA) [18, 19]. Participants were instructed to weigh themselves daily in the morning, wearing minimal clothing, prior to meals and after voiding. Body weight data were collected remotely using our Fitnesslink software. This software was purpose-built for this study by software development company, Portal Australia, Adelaide, Australia. Fitnesslink was used to access participants’ Fitbit user account data, including user profile details, sleep, activity and weight data, and device data (battery status and time of most recent sync). The software automatically harvested the Fitbit weight data, removing the risk of data errors and reducing the risk of reactivity associated with using a participant logbook to collect weight data. Weight at baseline and 12 months was calculated as the mean of all measures taken over 14-day periods at baseline and at 12 months.
Weight change, acceptance, and management strategies
Weight management strategy items were adapted from items used in the Behavioral Risk Factor Surveillance System, collaboration with the Center for Disease Control and Prevention [20]. At baseline, participants were asked whether their weight was stable in the previous three months (“Yes, my weight has been stable [remained within 5% on bodyweight]”, “No, my weight has increased [by ≥ 5%]”, “No, my weight has decreased [by ≥ 5%]”) and whether their weight was acceptable to them. That is, whether an individual accepts their weight, regardless of whether they are an acceptable weight, underweight, or overweight [21, 22].
Data on use of weight management strategies were obtained using a self-report survey at each of the eight time points during the 12 months (Timepoints: 1: mid-December; 2: mid-January; 3: mid-March; 4: mid-April; 5: mid-June; 6: mid-August; 7: mid-October; 8: mid-December [the following year]. Participants responded ‘yes’ or ‘no’ to the following questions: In the past 30 days have you used any of the following to manage your weight: i) restricted calories (i.e., specifically made an effort to reduce calorie intake); ii) counted calories (i.e., monitored calorie intake, but did not specifically reduce or increase calorie intake); iii) exercised or been physically active; iv) taken diet pills; v) used special products such as powdered supplements; vi) fasted; vii) caused self to vomit after eating; or viii) anything else to lose or maintain weight. Participants were advised on the differences between restricting (i.e., specifically made an effort to reduce calorie intake) and counting calories (i.e., monitored calorie intake, but did not specifically reduce or increase calorie intake) when completing the survey.
Wellbeing
Quality of life was measured using the WHO Quality of Life assessment 26-item version (WHOQOL-BREF) at each of the eight timepoints [23]. WHOQOL-BREF is a self-report questionnaire with domains: physical health, psychological health, social relationships and environment. Of note, the environment component of the WHOQOL-BREF assesses an individual’s perception of their physical environment, including their satisfaction with their living conditions, access to healthcare services, transportation, safety, and other environmental factors that can influence their quality of life [23]. The WHOQOL-BREF has good discriminant validity, content validity and test-retest reliability and internal consistency [23, 24]. Symptoms of depression, anxiety and stress were assessed using the 21-item short-form Depression Anxiety Stress Scale (DASS-21) [25]. The DASS-21 has good convergent and discriminant validity, adequate construct validity, and high reliability [25–27].
Statistical analysis
Baseline demographic characteristics and use of weight management strategies were reported using means and standard deviations for continuous data or counts and percentages for categorical data. The relationship between weight management strategies and change in weight over the 12-month period was assessed using linear mixed-effect models with random intercept for household (i.e., whether participants were from the same household, to account for the structure of the data, as some participants were from the same household), and fixed effects for age, sex, income, and baseline weight, and reported as coefficients and 95% confidence intervals (CIs). Univariate multinomial logistic regression was used to evaluate associations between the use of weight management strategies and psycho-sociodemographic characteristics. Missing data analysis was performed to assess the extent and nature of missingness in the dataset. Since the dataset was largely complete and the amount of missing data was low, imputation methods were not utilized, and the analyses were conducted using the available data. A graph of the proportion of total participants using each weight management strategy (expressed as a proportion of the sample size at each timepoint) was created using Microsoft Excel. Variables for which the p-value was < 0.05 in univariate analyses were included in multivariable models using multinomial regression and reported as odds ratios (OR) and 95% CI. Holm-Bonferroni adjustments for multiple testing were performed. This analysis involved conducting a secondary analysis of existing data, therefore, formal sample size calculations were not performed. All analyses were conducted using SPSS, version 25 (IBM, NY, USA).
Results
Participant characteristics
A total of 375 participants were recruited into the study, of whom 7 formally withdrew during the 12-month study period (1.8% drop-out). Their baseline characteristics are shown in Table 1. Just over half the participants were female and half were aged 39 years or less. Participants were predominantly born in Australia and married or living in a relationship. Of the 368 participants who remained enrolled in the study at 12 months, survey data on the use of weight management strategies was available for n = 350 (95.1%), n = 343 (93.2%), n = 344 (93.5%), n = 334 (90.8%), n = 317 (86.1%), n = 327 (88.9%), n = 319 (86.7%), n = 320 (87.0%) at time points 1 to 8, respectively. At baseline, mean body weight was 83.8 kg, and most participants were classed as overweight or obese based on body mass index. Most participants (77%) reported that their weight was stable prior to study enrolment. Weight data at 12 months was available for 368 participants.
Table 1.
Baseline characteristics of participants
| Used any strategy (at least once) at any point | ||||||
|---|---|---|---|---|---|---|
| Yes, n = 297 | No, n = 71 | Total, n = 368 | ||||
| Variable | Mean or n | SD or % | Mean or n | SD or % | Mean or n | SD or % |
| Age, years | 40.2 | 5.8 | 39.8 | 5.9 | 40.1 | 5.8 |
| <39 years | 148 | 49.8% | 37 | 52.1% | 185 | 50.3% |
| ≥40 years | 149 | 50.2% | 34 | 47.9% | 183 | 49.7% |
| Sex | ||||||
| Female | 174 | 58.6% | 35 | 50.7% | 209 | 56.8% |
| Male | 123 | 41.4% | 36 | 49.3% | 159 | 43.2% |
| Weight, kg | 84.6 | 20.5 | 80.8 | 20.0 | 83.8 | 20.4 |
| Body mass index, kg/m2 | 29.4 | 7.9 | 28.0 | 7.7 | 29.1 | 7.9 |
| Underweight | 11 | 3.7% | 5 | 7.0% | 16 | 4.3% |
| Normal | 82 | 27.6% | 23 | 32.4% | 105 | 28.5% |
| Overweight | 90 | 30.3% | 20 | 28.2% | 110 | 29.9% |
| Obese | 114 | 38.4% | 23 | 32.4% | 137 | 37.2% |
| Country of birth | ||||||
| Australia | 223 | 75.1% | 57 | 80.3% | 280 | 76.1% |
| Other | 74 | 24.9% | 14 | 19.7% | 88 | 23.9% |
| Marital status | ||||||
| Married | 43 | 14.5% | 12 | 16.9% | 313 | 85.1% |
| Other | 254 | 85.5% | 59 | 83.1% | 55 | 14.9% |
| Education | ||||||
| Some or completed high school | 66 | 17.9% | 53 | 17.8% | 13 | 18.3% |
| Trade school or certificate | 125 | 34.0% | 100 | 33.7% | 25 | 35.2% |
| University (bachelor or higher degree) | 177 | 48.1% | 144 | 48.5% | 33 | 46.5% |
| Income | ||||||
| <$50,000 | 27 | 9.1% | 10 | 14.1% | 37 | 10.1% |
| $50,000 to$99,999 | 90 | 30.3% | 21 | 29.6% | 111 | 30.2% |
| $100,000 to $199,999 | 141 | 47.5% | 35 | 49.3% | 176 | 47.8% |
| >$200,000 | 39 | 13.1% | 5 | 7.0% | 44 | 12.0% |
| Smoker, yes | 24 | 8.1% | 11 | 15.5% | 35 | 9.5% |
| Weight stable in last 3 months? Yes | 222 | 74.7% | 60 | 84.5% | 282 | 76.6% |
| No, increased | 56 | 18.9% | 7 | 9.9% | 63 | 17.1% |
| No, decreased | 19 | 6.4% | 4 | 5.6% | 23 | 6.3% |
| Weight acceptance | ||||||
| Acceptable weight | 102 | 34.3% | 41 | 57.7% | 143 | 38.9% |
| Underweight | 0 | 0.0% | 2 | 2.8% | 2 | 0.5% |
| Overweight | 195 | 65.7% | 28 | (39.4% | 223 | 60.6% |
Baseline characteristics of total sample (n = 368), and stratified based on use of weight management strategies (yes, n = 297; no = 71) during the 12-month period
Use of weight control strategies
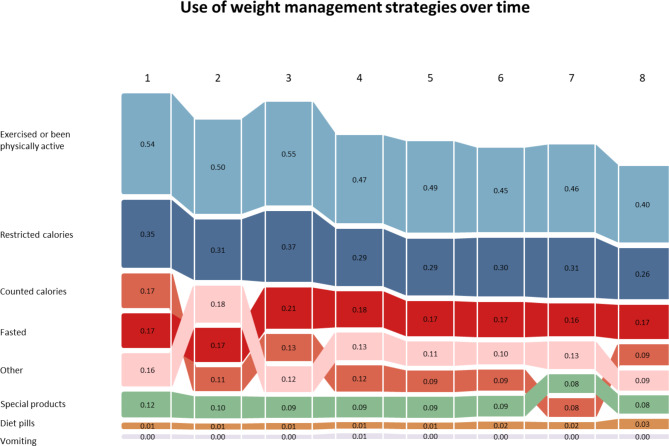
An overview of the use of weight control strategies is shown in Table 2. The majority of participants (81%) reported using at least one weight management strategy. Change in the use of each weight management strategy over eight timepoints (as a proportion of the sample size at each timepoint) is shown in Fig. 1. Exercising or being physically active was the most commonly reported strategy at each timepoint, ranging from 54% at timepoint 1, to 40% at timepoint 8.
Table 2.
Use of weight control strategies over the 12-month period (n = 368)
| Variable | Yes1 n (%) |
No2 n (%) |
|---|---|---|
| Used any strategy (at least once) at any point | 297 (80.7%) | 71 (19.3%) |
| Restricted calories | 230 (62.5%) | 138 (37.5%) |
| Counted calories | 103 (28.0%) | 265 (72.0%) |
| Exercised or been physically active | 282 (76.6%) | 86 (23.4%) |
| Taken diet pills | 21 (5.7%) | 347 (94.3%) |
| Used special products such as powdered supplements | 88 (23.9%) | 280 (76.1%) |
| Fasted | 150 (40.8%) | 218 (59.2%) |
| Caused self to vomit after eating | 5 (1.4%) | 363 (98.6%) |
| Anything else to lose or maintain weight | 131 (35.6%) | 237 (64.4%) |
1 Used the weight management strategy at least once over the 8 timepoints
2Did not use the weight management strategy over the 8 timepoints
Fig. 1.
Graph of changes in the use of each weight management strategy over the 8 timepoints, expressed as a proportion of the sample size at each time point (Timepoints: 1: mid-December; 2: mid-January; 3: mid-March; 4: mid-April; 5: mid-June; 6: mid-August; 7: mid-October; 8: mid-December [the following year])
Change in the use of each weight management strategy over eight timepoints (as a proportion of the sample size at each timepoint)
Relationship between weight management strategies and change in weight over 1 year
The relationships between the use of each weight management strategy and changes in weight are shown in Table 3. Almost none of the weight management strategies were significantly associated with weight change, with the exception of exercising or being physically active. Being physically active or exercising was associated with a greater reduction in body weight than not being physically active (between group difference: -1.2 kg, 95% CI: -2.3, -0.1 kg; p < 0.01).
Table 3.
Effect of weight change strategies on change in weight over 12 months
| Weight change (kg) after 12 months | |||
|---|---|---|---|
| Estimate | 95% CI | p-value | |
| Use any strategy (at least once) at any point | |||
| Yes | -1.1 | -2.3, 0.1 | 0.063 |
| No | REF | ||
| Restricted calories1 | |||
| Yes | -0.3 | -1.3, 0.7 | 0.517 |
| No | REF | ||
| Counted calories1 | |||
| Yes | 0.1 | -1.0, 1.1 | 0.916 |
| No | REF | ||
| Exercised or been physically active1 | |||
| Yes | -1.2 | -2.3, -0.1 | 0.034 |
| No | REF | ||
| Taken diet pills1 | |||
| Yes | 0.2 | -1.9, 2.3 | 0.839 |
| No | REF | ||
| Used special products such as powdered supplements1 | |||
| Yes | 0.4 | -0.8, 1.5 | 0.532 |
| No | REF | ||
| Fasted1 | |||
| Yes | -0.4 | -1.4, 0.5 | 0.371 |
| No | REF | ||
| Caused self to vomit after eating1 | |||
| Yes | -2.8 | -6.9, 1.3 | 0.176 |
| No | REF | ||
| Anything else to lose or maintain weight1 | |||
| Yes | -0.4 | -1.4, 0.6 | 0.460 |
| No | REF | ||
The relationships between the use of each weight management strategy and changes in weight
1 Estimates from linear mixed effect models with random intercept for household, and fixed effects for age, sex, income, and baseline weight,
2 Used the strategy at least once over the 12 months
Association between use of weight management strategies and psycho-sociodemographic characteristics
Association between the use of each weight change strategy and psycho-sociodemographic characteristics are shown in Tables S1-S15. Compared with not accepting one’s bodyweight, the odds of using any weight management strategy over the 12 months was lower in those that accepted their bodyweight (OR = 0.38, 95% CI = 0.22, 0.64, p < 0.01). Compared with having a stable weight in the three months prior to study enrolment, the odds of restricting calories (OR = 0.39, 95% CI = 0.20, 0.74, p < 0.01) and fasting (OR = 0.44, 95% CI = 0.25, 0.77, p < 0.01) were lower in those who increased weight in the three months prior. Compared with not accepting one’s bodyweight, the odds of restricting calories (OR = 0.52, 95% CI = 0.33, 0.80, p < 0.01) and fasting (OR = 0.49, 95% CI = 0.32, 0.77, p < 0.01) were lower in those that accepted their bodyweight. Compared with females, the odds of counting calories (OR = 0.49, 95% CI = 0.30, 0.79, p < 0.01) and using other weight management strategy (OR = 0.41, 95% CI = 0.26, 0.65, p < 0.01) were lower in males. Use of special products (e.g., powders) was positively associated with baseline weight (b = 0.02, SE = 0.00, p < 0.01) and depression (b = 0.04, SE = 0.01, p < 0.01), and negatively associated with physical QOL (b=-0.15, SE = 0.01, p < 0.01) and psychological QOL (b=-0.14, SE = 0.04, p < 0.01). Fasting was negatively associated with psychological QOL (b=-0.17, SE = 0.04, p < 0.01) and environmental QOL (b=-0.19, SE = 0.05, p < 0.01). Further, compared with having a comorbid condition, the odds of fasting were lower than in those without a comorbid condition (OR = 0.34, 95% CI = 0.21, 0.53, p < 0.01).
Discussion
The aims of this study were to describe the weight management strategies used by a sample of Australian adults and assess whether the use of weight management strategies over a 12-month period was associated with weight loss and psycho-sociodemographic characteristics. The findings showed that weight management strategies were commonly used, with 81% of participants using at least one strategy over the 12 months. Exercise/physical activity was the most common strategy at each timepoint and was associated with a -1.2 kg greater reduction in body weight than not being physically active. Other key findings were: (1) those that accepted their weight had a lower odds of using any weight management strategy, (2) the odds of restricting calories and fasting were lower in those who increased weight prior to enrolment, than those who maintained weight, (3) the odds of restricting calories and fasting was lower in those that accepted their bodyweight, than those who didn’t accept their bodyweight, and (4) the odds of counting calories and using any other weight management strategy was lower in males than females.
The use of weight management strategies was common, with 77% being physically active or exercising, 63% restricting calories, 41% fasting, 28% counting calories, 24% using supplements (e.g., powders), 6% using diet pills and 1% vomiting. These findings are reasonably comparable to a previous population-based cohort study of Australian women [28], where the use of various weight management strategies among those who had been on a diet in the past year included cutting down fats/sugars (82%), reducing meal size (81%), exercise (60%), using a commercial weight loss program (19%), fasting (13%), meal replacements or slimming products (6%), laxatives, diuretics and diet pills (3%), vomiting (1.9%). Our sample appeared to use exercise and fasting at slightly higher rates than the previous study (exercise 80% vs. 60% and fasting 41% vs. 13%). This observation might be due to ongoing public health effects promoting the benefits of physical activity for health [29], and a growing interest in fasting practices, such as intermittent fasting [30], in more recent times.
Our findings suggest that the use of weight management strategies decreased over the 12 months (from mid-December to mid-December the following year; exercise or being physically active: 54 to 40%; restricted calories 35 to 26%; counted calories: 17 to 9%; other: 16 to 9%; use of special products: 12 to 8%). All of the weight management strategies appeared to fall at a similar rate, with perhaps the exception of calorie-counting, which appeared to decline at a greater rate. There is evidence to suggest that people who are able to lose weight and keep it off for at least 3 months are more likely to be successful in the long term [31]. However, many individuals do not sustain weight control behaviour long term (i.e., for 12 months or more) [32]. A previous prospective cohort study which evaluated use of weight management strategies over 4 years among 1120 US adults found that the median duration of use for most strategies was 10 months for decreasing fat intake, and 7 months for increased physical activity, over the 4 years [32]. An alternative explanation may be measurement bias - participants in our study were asked to complete the survey at eight times points across the 12-month period. It is possible that measurement fatigue is behind the gradual reduction in reporting over weight management strategies across the study period.
At each timepoint, exercising or being physically active was the most reported weight management strategy, ranging from 54% at timepoint 1, to 40% at timepoint 8. Further, the findings indicated that those who were physically active or exercised, reduced their bodyweight by -1.21 kg more, than those who were not physically active. Whilst weight maintenance is a recognised benefit of physical activity, most research comparing the relative benefits of diet versus exercise for weight loss identify diet as the more potent strategy [33, 34]. Therefore, it was somewhat surprising that physical activity was associated with weight loss in this study, while dietary strategies were not. Findings from previous systematic reviews of randomised controlled trials have found that physical activity combined with diet and behavioural components leads to greater weight loss at 12 months, compared with diet-only or physical activity-only interventions, weight loss mean difference range − 1.17 to 3.02 kg [35, 36]. The popularity of physical activity for weight management reported in this study, and that the use of physical activity appeared to be a more effective weight management strategy, may suggest that physical activity may be a particularly achievable and acceptable weight management strategy (particularly given that physical activity is associated with immediate psychological and cognitive benefits, such as improved mood and vitality [37]).
Weight acceptance was associated with use of weight management strategies, with those that didn’t accept their weight being more likely to use weight management strategies, than those who accepted their bodyweight. These findings are consistent with previous work that has shown that adults who perceive themselves as overweight being more likely to attempt to lose weight [38], and more likely to report using exercise as a weight control strategy than those who do not perceive themselves as overweight [39]. In addition, findings from a recent systematic review showed strong evidence for an association between perceived overweight and weight loss attempts; individuals who perceived themselves as overweight had a higher likelihood of intending or attempting to lose weight than those who perceived themselves as normal weight [40]. Furthermore, individuals who identify as overweight experience higher levels of body dissatisfaction [41] and may therefore have a greater desire to lose weight than individuals who do not identify as overweight. However, longitudinal studies of adolescents and adults have shown that perceiving oneself as overweight is associated with greater long-term weight gain in individuals with both measured normal weight and measured overweight (i.e., measured body mass index using objective methods) [42, 43] therefore, perception of overweight may not necessarily be associated with effective long-term weight management.
Consistent with previous findings [44], our present findings showed that males were less likely to restricted calories, compared with females. In a previous study by Harring et al. [44], higher proportions of US college-aged women reported trying to lose weight compared with men (61% vs. 34%, respectively). Harring et al. [44] also reported higher proportions of women were using the following weight management strategies: exercise (63% vs. 44%), diet (42% vs. 22%), vomiting after meals (4% vs. 0.7%), diet pills (5% vs. 2%), diet and exercise (36% vs. 19%), compared with men, respectively. With the exception of restricting calories, our findings showed no sex differences for the use of counting calories, exercising or being physically active, diet pills, use of special products (such as powdered supplements), fasting and self-vomiting. Previous findings suggest that being a parent can influence attitudes and practices in weight management strategies. For example, a study found that parents of minor children had poorer weight loss outcomes and behavioural adherence, than participants without children, in a rural community-based weight loss intervention [45]. Therefore, the differences in our study compared with Harring et al. [44] is likely attributed to the difference samples (community-dwelling adults who were parents of school-aged children, versus college students). In addition, there was some evidence to suggest that fasting, and the use of special powders or supplements (to manage weight), were associated with worse depression and QOL. It is possible that people who try fasting and using supplements to lose weight may have failed previously to lose weight and are looking for alternative methods to achieve weight loss [46]. Prior work has indicated that repeated failed attempts to manage weight are associated with reductions in psychological well-being [47]. While others have reported that worse psychological well-being is associated with weight gain [48]. Therefore, future research is required to understand the interrelationships between use of weight management strategies, weight changes and wellbeing.
Strengths and limitations
Strengths of this study were that the sample was reasonably reflective of middle-aged Australian adults (in terms of sex, household structure, income, weight status), weight was objectively measured, and retention and data completeness were high. Limitations of this work was that participants were from one Australian city, were all parents, the sample size was modest, and the use of a non-validated questionnaire to assess weight acceptance. Sample size calculations were conducted for the primary analysis [14]. Our analysis involved conducting a secondary analysis of existing data, and as such, formal sample size calculations were not performed. Therefore, the study may have limited power to detect relationships (particularly if they are small in magnitude) and the generalisability of findings to other geographical regions and demographic groups are unclear. An additional limitation is the observational study design which limits the ability to infer causality.
Implications
Given the high, and increasing, rates of overweight and obesity in Australia and many other countries around the world, effective weight management strategies are needed. Our present findings identified physical activity and exercise as the most popular weight management strategy, and the single weight management strategy associated with weight loss at 12 months. This finding supports current national and international weight management guidelines which recommend exercise and healthy eating patterns [49]. It is encouraging, given that physical activity confers many other health benefits in addition to its benefits for weight control [50].
Conclusion
Overall, the use of weight management strategies was common in this sample of Australian adults. The most popular weight management strategies included exercising or being physically active, restricting calories, and fasting. Those who didn’t accept their current bodyweight were more likely to use at least one weight management strategy and those who were reported being physically active for weight maintenance had a greater reduction in bodyweight, than those who did not. Public health weight management approaches should include weight management strategies that are associated with effective weight management, with our findings indicating that physical activity and exercise is a popular weight management strategy and is also associated with weight loss at 12 months.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Authors’ contributions
CM, TF, RC, WB, DD, AE and TO contributed to the study concept and design. CM, WB, AE and TO provided study supervision. CM, TF and RC contributed to data collection. BS analyzed the data and generated the figures. All authors contributed to data interpretation, writing the paper and had final approval of the submitted version.
Funding
This project is funded by the Australian National Health and Medical Research Council (APP1163338). CM is supported by a Medical Research Future Fund Investigator Grant (GNT1193862). DD is supported by a National Health and Medical Research Council Early Career Fellowship (APP1162166) and Heart Foundation Post Graduate Fellowship (APP102084).
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the University of South Australia Human Research Ethics committee (Protocol number: 201901). Participants provided written consent informed prior to enrolment and this project was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Morgen CS, Sørensen TIA. Global trends in the prevalence of overweight and obesity. Nat Reviews Endocrinol. 2014;10:513–4. doi: 10.1038/nrendo.2014.124. [DOI] [PubMed] [Google Scholar]
- 2.Seidell JC, Halberstadt J. The global burden of obesity and the challenges of prevention. Ann Nutr Metab. 2015;66:7–12. doi: 10.1159/000375143. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Obesity and overweight. 2021. url: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 4.Australian Institute of Health and Welfare. Overweight and obesity. 2022. url: https://www.aihw.gov.au/reports/australias-health/overweight-and-obesity.
- 5.Fruh SM, Obesity Risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract. 2017;29:3–14. doi: 10.1002/2327-6924.12510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Australian Institute of Health and Welfare. Impact of overweight and obesity as a risk factor for chronic conditions. 2017. url: https://www.aihw.gov.au/reports/burden-of-disease/impact-of-overweight-and-obesity-as-a-risk-factor-for-chronic-conditions/summary.
- 7.Cercato C, Fonseca FA. Cardiovascular risk and obesity. Diabetol Metab Syndr. 2019;11:74–83. doi: 10.1186/s13098-019-0468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12:131–41. doi: 10.1111/j.1467-789X.2009.00712.x. [DOI] [PubMed] [Google Scholar]
- 9.Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5:161. doi: 10.21037/atm.2017.03.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bish CL, et al. Diet and physical activity behaviors among Americans trying to lose weight: 2000 behavioral risk factor Surveillance System. Obes Res. 2005;13:596–607. doi: 10.1038/oby.2005.64. [DOI] [PubMed] [Google Scholar]
- 11.Hutfless S, et al. Strategies to prevent weight gain in adults: a systematic review. Am J Prev Med. 2013;45:e41–51. doi: 10.1016/j.amepre.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Yoong SL, et al. A cross-sectional study assessing the self-reported weight loss strategies used by adult australian general practice patients. BMC Fam Pract. 2012;13:48. doi: 10.1186/1471-2296-13-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams L, Germov J, Young A. Preventing weight gain: a population cohort study of the nature and effectiveness of mid-age women’s weight control practices. Int J Obes. 2007;31:978–86. doi: 10.1038/sj.ijo.0803550. [DOI] [PubMed] [Google Scholar]
- 14.Curtis RG, et al. Annual rhythms in adults’ lifestyle and health (ARIA): protocol for a 12-month longitudinal study examining temporal patterns in weight, activity, diet, and wellbeing in australian adults. BMC Public Health. 2021;21:70. doi: 10.1186/s12889-020-10054-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;27(20):2191–4. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 16.Watson A, et al. Life on holidays: study protocol for a 3-year longitudinal study tracking changes in children’s fitness and fatness during the in-school versus summer holiday period. BMC Public Health. 2019;19(1):1353. doi: 10.1186/s12889-019-7671-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Australian Bureau of Statistics. ANZSCO–Australian and New Zealand Standard Classification of Occupations. 2019. url: https://www.abs.gov.au/statistics/classifications/anzsco-australian-and-new-zealand-standard-classification-occupations/latest-release.
- 18.Yorkin M, et al. Accuracy and consistency of weights provided by home bathroom scales. BMC Public Health. 2013;13:1194. doi: 10.1186/1471-2458-13-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaffer JA, et al. An inexpensive device for monitoring patients’ weights via automated hovering. Int J Cardiol. 2014;172:e263–4. doi: 10.1016/j.ijcard.2013.12.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Serdula MK, Williamson DF, Anda RF, Levy A, Heaton A, Byers T. Weight control practices in adults: results of a multistate telephone survey. Am J Public Health. 1994;84(11):1821–4. doi: 10.2105/AJPH.84.11.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson M, Ball K, Crawford D. Beliefs about the causes of weight change in the australian population. Int J Obes Relat Metab Disord. 2001;25(10):1512–6. doi: 10.1038/sj.ijo.0801728. [DOI] [PubMed] [Google Scholar]
- 22.Kilpatrick M, Nelson M, Palmer A, Jose K, Venn A. Who discusses reaching a healthy weight with a general practitioner? Findings from the 2014-15 australian National Health Survey. Obes Res Clin Pract. 2018;12(5):459–64. doi: 10.1016/j.orcp.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 24.Krägeloh CU, et al. Validation of the WHOQOL-BREF quality of life questionnaire for general use in New Zealand: confirmatory factor analysis and rasch analysis. Qual Life Res. 2013;22:1451–7. doi: 10.1007/s11136-012-0265-9. [DOI] [PubMed] [Google Scholar]
- 25.Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales, A. psychology Foundation of, editor. Psychology Foundation of Australia: Sydney, N.S.W; 1995.
- 26.Henry JD, Crawford JR. The short-form version of the Depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–39. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 27.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression anxiety stress scales (DASS) with the Beck Depression and anxiety inventories. Behav Res Ther. 1995;33:335–43. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- 28.Madigan CD, et al. Cluster analysis of behavioural weight management strategies and associations with weight change in young women: a longitudinal analysis. Int J Obes. 2015;39:1601–6. doi: 10.1038/ijo.2015.116. [DOI] [PubMed] [Google Scholar]
- 29.Williamson C, Baker G, Mutrie N, Niven A, Kelly P. Get the message? A scoping review of physical activity messaging. Int J Behav Nutr Phys Act. 2020;15(1):51. doi: 10.1186/s12966-020-00954-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harris L, et al. Intermittent fasting interventions for treatment of overweight and obesity in adults: a systematic review and meta-analysis. JBI Evid Synthesis. 2018;16:507–47. doi: 10.11124/JBISRIR-2016-003248. [DOI] [PubMed] [Google Scholar]
- 31.Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–41. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- 32.French SA, Jeffery RW, Murray D. Is dieting good for you?: prevalence, duration and associated weight and behaviour changes for specific weight loss strategies over four years in US adults. Int J Obes. 1999;23:320–7. doi: 10.1038/sj.ijo.0800822. [DOI] [PubMed] [Google Scholar]
- 33.Curioni CC, Lourenço PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes. 2005;29:1168–74. doi: 10.1038/sj.ijo.0803015. [DOI] [PubMed] [Google Scholar]
- 34.Kheniser K, Saxon DR, Kashyap SR. Long-term weight loss strategies for obesity. J Clin Endocrinol Metabolism. 2021;106:1854–66. doi: 10.1210/clinem/dgab091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johns DJ, et al. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J Acad Nutr Diet. 2014;114:1557–68. doi: 10.1016/j.jand.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Avenell A, et al. What interventions should we add to weight reducing diets in adults with obesity? A systematic review of randomized controlled trials of adding drug therapy, exercise, behaviour therapy or combinations of these interventions. J Hum Nutr Diet. 2004;17:293–316. doi: 10.1111/j.1365-277X.2004.00530.x. [DOI] [PubMed] [Google Scholar]
- 37.Chan JSY, et al. Special issue – therapeutic benefits of physical activity for Mood: a systematic review on the Effects of Exercise Intensity, Duration, and modality. J Psychol. 2019;153:102–25. doi: 10.1080/00223980.2018.1470487. [DOI] [PubMed] [Google Scholar]
- 38.Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003–2008 study. Int J Obes. 2011;35:1063–70. doi: 10.1038/ijo.2010.229. [DOI] [PubMed] [Google Scholar]
- 39.Edwards NM, Pettingell S, Borowsky IW. Where perception meets reality: self-perception of weight in overweight adolescents. Pediatrics. 2010;125:e452–8. doi: 10.1542/peds.2009-0185. [DOI] [PubMed] [Google Scholar]
- 40.Haynes A, et al. A systematic review of the relationship between weight status perceptions and weight loss attempts, strategies, behaviours and outcomes. Obes Rev. 2018;19:347–63. doi: 10.1111/obr.12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilson JM, Tripp DA, Boland FJ. The relative contributions of subjective and objective measures of body shape and size to body image and disordered eating in women. Body Image. 2005;2:233–47. doi: 10.1016/j.bodyim.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 42.Sutin AR, Terracciano A. Body weight misperception in adolescence and incident obesity in young adulthood. Psychol Sci. 2015;26:507–11. doi: 10.1177/0956797614566319. [DOI] [PubMed] [Google Scholar]
- 43.Klein EG, Lytle LA, Chen V. Social ecological predictors of the transition to overweight in youth: results from the teens eating for Energy and Nutrition at Schools (TEENS) study. J Am Diet Assoc. 2008;108:1163–9. doi: 10.1016/j.jada.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harring HA, Montgomery K, Hardin J. Perceptions of Body Weight, Weight Management Strategies, and depressive symptoms among US College Students. J Am Coll Health. 2010;59:43–50. doi: 10.1080/07448481.2010.483705. [DOI] [PubMed] [Google Scholar]
- 45.Befort CA, Ross KM, Janicke DM, Perri MG. Parents of minor children lose less weight during a behavioral weight loss intervention: findings from the rural LEAP trial. Obes Sci Pract. 2022;8(6):728–34. doi: 10.1002/osp4.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pillitteri JL, Shiffman S, Rohay JM, Harkins AM, Burton SL, Wadden TA. Use of dietary supplements for weight loss in the United States: results of a national survey. Obesity. 2008;16(4):790–6. doi: 10.1038/oby.2007.136. [DOI] [PubMed] [Google Scholar]
- 47.Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 48.Räikkönen K, Matthews KA, Kuller LH. Depressive symptoms and stressful life events predict metabolic syndrome among middle-aged women: a comparison of World Health Organization, Adult Treatment Panel III, and International Diabetes Foundation definitions. Diabetes Care. 2007;30:872–7. doi: 10.2337/dc06-1857. [DOI] [PubMed] [Google Scholar]
- 49.Centers for Disease Control and Prevention, Healthy Weight, Nutrition, and Physical Activity. U.S. Department of Health & Human Services., 2022. url: https://www.cdc.gov/healthyweight/index.html.
- 50.Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity-a systematic review of longitudinal studies. BMC Public Health. 2013;13:813–21. doi: 10.1186/1471-2458-13-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.