Abstract
Objectives
Few studies have examined frailty in Indian adults, despite an increasing population of older adults and an escalating burden of chronic diseases. We aimed to study the prevalence and correlates of frailty in middle-aged and older Indian adults.
Setting
Cross-sectional data from Wave 1 of Longitudinal Ageing Study in India, conducted in 2017–2018 across all states and union territories, were used.
Participants
The final analytical sample included 57 649 participants aged 45 years and above who had information on frailty status.
Primary outcome measure
The deficits accumulation approach to measuring frailty was employed, creating a frailty index between 0 and 1, based on 40 deficits. Individuals with a frailty index of 0.25 or more were defined as ‘frail’.
Results
Prevalence of frailty among 45+ adults was 30%. 60+ women were two times as likely to be frail compared with 60+ men, after adjusting for a wide range of sociodemographic, economic and lifestyle factors. The sex difference was more pronounced in adults aged 45–59 years. Odds of hospitalisation in the last 12 months, and having falls in the past 2 years, were two times as high in frail adults compared with non-frail adults. Frail middle-aged and older adults had 33% and 39% higher odds, respectively, of having poor cognition than non-frail adults. The relative increase was higher in women for all three outcomes, although not statistically significant.
Conclusions
There needs to be careful consideration of sex differences when addressing frailty, particularly for optimising frailty interventions. Frailty, although typically assessed in older adults, was shown in this study to be also prevalent and associated with adverse outcomes in middle-aged Indian adults. More research into assessment of frailty in younger populations, its trajectory and correlates may help develop public health measures for prevention of frailty.
Keywords: EPIDEMIOLOGY, GERIATRIC MEDICINE, PUBLIC HEALTH, Quality of Life
Strengths and limitations of this study.
The analyses were based on a nationally representative sample of 45+ years old Indian adults from all states and union territories except Sikkim, allowing for estimation of national, as well as state-level, estimates of prevalence of frailty.
We examined prevalence of frailty, its risk factors and association with adverse outcomes in middle-aged adults, in addition to older adults.
Our frailty index was constructed using 40 deficits, including deficits pertaining to mental impairment and instrumental activities of daily living aimed at assessing cognitive functioning, thus capturing the multidimensionality of frailty.
Due to cross-sectional nature of data, we were unable to look at temporal associations between frailty and adverse health outcomes.
We were not able to define other frailty measures such as the frailty phenotype, based on the available data.
Background
Frailty is characterised by a decline in functioning across multiple physiological systems, accompanied by an increased vulnerability to stressors.1 As a result, frail people are more likely to have adverse health outcomes when exposed to stressors than non-frail people.2 A frailty score can help identify people with unique health needs, who need intervention to address the causes of poor health and improve outcomes in them. It can therefore be useful in clinical and community settings for risk stratification. However, there are multiple approaches and various tools to measure frailty and there is considerable disagreement between these instruments.3 This is, in part, responsible for the marked variation in prevalence estimates across countries, and even within countries.4
Most studies on frailty are from high-income countries (HICs).4 There exist several systematic reviews across geographical regions, but studies from low/middle-income countries (LMICs) are limited and have used a variety of methods.5 A few studies have shown that frailty prevalence and incidence are higher in LMICs compared with HICs.4 6–8 In contrast, a multicounty study comparing 14 HICs and 6 LMICs (China, Ghana, India, Mexico, Russian Federation and South Africa) reported a higher mean frailty index in HICs compared with the LMICs.9 However, interpretation of differences in prevalence between countries or regions is limited by the few data from LMICs. In a recent systematic review on the prevalence of frailty in LMICs, only one of the 56 studies was from a low-income country (Tanzania) and only two were from a lower middle-income country (India); the rest were from upper middle-income countries—Brazil, Colombia, Mexico, Chile, Cuba, China, Malaysia, Russia, Turkey and Lebanon.5 Robust disaggregated data on frailty in the Indian population are rare,10–14 while no studies have provided subnational estimates on the prevalence of frailty.
Further, while there are many frailty studies among adults aged 60 years and above,4 5 8 15–17 the extent of the problem and its significance in adults less than 60 years is poorly understood. Studies have shown that frailty is prevalent in younger adults and suggested that it be examined across the adult age spectrum.18–20 This is especially true for India where chronic diseases develop a decade earlier than in HICs.21 Furthermore, studies characterising sex differences in frailty, and how frailty differently impacts health outcomes in women and men are rare in LMICs.12 22–26
With a rapidly ageing population and a fragmented healthcare system, there is an urgent need to quantify frailty in India reliably, so as to inform the development of interventions and plan targeted service delivery. In this study, we examine frailty prevalence, its state-level and socioeconomic patterning and association, including sex-specific association, with key health outcomes in middle-aged (45–59 years old) and older (60+ years) Indian adults.
Methods
Data
We used data from Wave 1 of the Longitudinal Ageing Study in India (LASI), conducted in 2017–2019 in all of India’s states and union territories.27 Detailed descriptions of sampling design, participants, questionnaires and response rates and are available elsewhere.28 Briefly, LASI is a nationwide panel survey of adults aged 45 and older and their spouses, designed to provide longitudinal data on the broad domains of social, health and economic well-being of the elderly Indian population. Data include demographics, household economic status, mental health, functional health, biomarkers, health insurance and healthcare usage, family and social networks, welfare programmes, work and employment, retirement, and life satisfaction. While measures in LASI are specific and sensitive to the Indian context, they have been harmonised with international surveys on ageing and retirement. LASI adopted a multistage stratified cluster sampling design. Data from LASI Wave 1 include 65 562 45+ individuals from all states and union territories except Sikkim. Data are available in the public domain and can be accessed by filling out the form available online (https://iipsindia.ac.in/sites/default/files/LASI_DataRequestForm_0.pdf).29
Variables
Assessment of frailty
We used the frailty index measure based on a deficit accumulation approach, proposed by Rockwood and Mitnitski.30 We included 40 deficits across different domains31—general health (1 deficit), diagnosed conditions (9 deficits), medical symptoms (4 deficits), mobility restrictions (9 deficits), basic activities of daily living (ADL) and instrumental activities of daily living (IADL) limitations (13 deficits), any mental impairment (1 deficit), body mass index (1 deficit), grip strength (1 deficit) and gait speed (1 deficit). All deficits were assigned scores between 0 and 1, with one indicating complete deficit and 0 lack of any deficit. A detailed description is presented in online supplemental S1 table. The frailty index is the sum of deficit scores divided by the total number of deficits considered (40 in our case), yielding a continuous score between 0 and 1. This index will be missing for an individual with missing data on any deficit. We used a cut-off of 0.25 to define presence or absence of frailty32–34—individuals with frailty index ≥0.25 were defined as ‘frail’ and others as ‘non-frail’.
bmjopen-2023-071842supp001.pdf (689.3KB, pdf)
In sensitivity analyses, we explored another commonly used frailty index cut-off, 0.21.35 Also, an alternative approach to calculating the frailty index that accounts for missing deficit scores was examined—up to three deficits were allowed to be missing and the frailty index for an individual was calculated by summing the non-missing health deficit scores and then dividing by the total number of deficits measured in that individual.
Covariates
Demographic, socioeconomic and lifestyle factors were included as covariates—age, sex, place of residence, educational status, living arrangement, monthly per capita consumption expenditure (MPCE), working status, food constraint, religion, caste, tobacco use, alcohol use and region. Food constraint referred to household food unavailability in the past 12 months. MPCE was defined as total monthly household consumption expenditure divided by household size. Expenditure here includes the household’s per capita spending on food and non-food items, including spending on health, education and utilities. We used consumption expenditure as our economic indicator as we consider this a better measure of living standards and poverty than income. Also, household income information was missing for 1216 45+ adults. As part of sensitivity analyses, we examined annual per capita household income as the economic indicator.
Adverse outcomes
The respondents were asked about number of hospitalisations and number of nights spent in the hospital in the last 12 months. In addition to these count outcome variables, a binary outcome variable, ever hospitalised in last 12 months, was defined based on the number of hospitalisations (online supplemental S2 table). Another binary outcome variable, any fall in past 2 years, was defined based on responses to questions about having fallen down or sustaining a major injury from a fall in the past 2 years (online supplemental S2 table).
Cognitive measures in LASI were derived from the cognition module of the Health and Retirement Study—Harmonised Cognitive Assessment Protocol.36 A detailed description of the different cognitive domains measured in LASI is presented in online supplemental S3 table. A composite cognition score, ranging from 0 to 43, was constructed by combining scores across five domains: memory, orientation, arithmetic function, executive functioning skills and object naming. A higher score indicated better cognitive ability and poor cognition was defined as a score below the 10th percentile, which was 18.
Statistical analyses
Continuous variables were summarised as mean and SD or median and interquartile interval (IQI) and categorical variables as frequencies and percentages. State-level and national-level sampling weights were used to produce weighted prevalence estimates. Multivariable logistic regressions were used to obtain ORs, with 95% CIs for the association between frailty status (frail vs non-frail) and individuals’ background characteristics—sex, age, place of residence, education, consumption expenditure, living arrangement, work status, food constraint, tobacco use, alcohol use, religion and caste, separately for the middle-aged and older participants. Age was analysed as a continuous variable, and all other variables were treated as categorical. Logistic and linear regressions were used to study associations between frailty status (frail vs non-frail) and binary and continuous adverse outcomes, respectively. Poisson hurdle models were used for count outcomes with a high percentage of zeros—number of hospitalisations and number of nights spent in hospital in last 12 months. The Poisson hurdle model specifies a logistic regression for the zero counts and a truncated (at zero) Poisson model for the positive counts.37 The association between frailty status and cognition score was examined using linear regression. All regressions examining associations between frailty and adverse outcomes were adjusted for participants’ background characteristics. Sex differences in the associations with binary adverse outcomes were studied using the full interaction model, with all main effects and sex interactions with frailty as well as each confounding variable; sex-specific ORs were compared through women-to-men ratios of ORs (RORs).38 All regressions were adjusted for state fixed effects to account for state-level variation. All statistical analyses were carried out using Stata V.13 (StataCorp) and R V.4.2.0.39 40
Patient and public involvement
Patients or the public were not involved in this secondary analysis of publicly available survey data.
Results
Description of study participants
LASI included 34 098 middle-aged adults (45–59 years) and 31 464 older adults (60 years and above). 7913 participants for whom information related to frailty was missing were excluded from analyses, resulting in a total sample of 57 649 participants. Participants were further excluded while studying associations with outcomes, because of missing outcome data (online supplemental S1 figure). There were small differences between participants with missing frailty information and those included in analyses (online supplemental S4 table). Participants with missing frailty data (n=7913) were more likely to be older, residing in urban areas, living with children and/or others and not working currently. Of the 57 649 study participants, 55% of middle-aged adults and 52% of older participants were female (table 1). Around 60% of the participants had no or less than 5 years of schooling, 66% lived in the rural areas, around a quarter had never worked, and 82% and 63% reported never consuming alcohol and never using any tobacco product, respectively.
Table 1.
Characteristics of study participants
| Characteristic | Overall, N=57 649 | 45–60 years, N=30 568 | 60+ years, N=27 081 |
| Sex | |||
| Female | 30 874 (54%) | 16 912 (55%) | 13 962 (52%) |
| Male | 26 775 (46%) | 13 656 (45%) | 13 119 (48%) |
| Age, median (Q1, Q3)* | 58 (50, 66) | 51 (48, 55) | 67 (63, 72) |
| Place of residence | |||
| Rural | 37 805 (66%) | 19 730 (65%) | 18 075 (67%) |
| Urban | 19 844 (34%) | 10 838 (35%) | 9006 (33%) |
| Educational status | |||
| No schooling | 26 961 (47%) | 12 562 (41%) | 14 399 (53%) |
| Less than 5 years | 6738 (12%) | 3404 (11%) | 3334 (12%) |
| 5–9 years | 13 280 (23%) | 7995 (26%) | 5285 (20%) |
| 10 years or more | 10 670 (19%) | 6607 (22%) | 4063 (15%) |
| MPCE fifths† | |||
| Poorest | 11 358 (20%) | 5846 (19%) | 5512 (20%) |
| Poorer | 11 673 (20%) | 6067 (20%) | 5606 (21%) |
| Middle | 11 676 (20%) | 6081 (20%) | 5595 (21%) |
| Richer | 11 633 (20%) | 6276 (21%) | 5357 (20%) |
| Richest | 11 309 (20%) | 6298 (21%) | 5011 (19%) |
| Living arrangement | |||
| Living alone | 2034 (3.5%) | 627 (2.1%) | 1407 (5.2%) |
| Living with spouse with or without children | 42 607 (74%) | 25 346 (83%) | 17 261 (64%) |
| Living with children and others | 10 709 (19%) | 3641 (12%) | 7068 (26%) |
| Living with others only | 2299 (4.0%) | 954 (3.1%) | 1345 (5.0%) |
| Employment | |||
| Currently working‡ | 28 939 (50%) | 19 365 (63%) | 9574 (35%) |
| Worked in the past | 13 045 (23%) | 2961 (9.7%) | 10 084 (37%) |
| Never worked | 15 665 (27%) | 8242 (27%) | 7423 (27%) |
| Food constraint§ | |||
| No | 53 801 (93%) | 28 624 (94%) | 25 177 (93%) |
| Yes | 3848 (6.7%) | 1944 (6.4%) | 1904 (7.0%) |
| Tobacco use | |||
| Never used tobacco | 36 252 (63%) | 19 919 (65%) | 16 333 (60%) |
| Current/past user | 21 373 (37%) | 10 633 (35%) | 10 740 (40%) |
| Missing | 24 | 16 | 8 |
| Alcohol use | |||
| Never consumed | 47 218 (82%) | 24 848 (81%) | 22 370 (83%) |
| Less than once a month in past 3 months | 6024 (10%) | 3123 (10%) | 2901 (11%) |
| 1–3 days per month or more frequently | 4397 (7.6%) | 2591 (8.5%) | 1806 (6.7%) |
| Missing | 10 | 6 | 4 |
| Caste | |||
| Scheduled caste | 9695 (17%) | 5278 (17%) | 4417 (16%) |
| Scheduled tribe | 10 140 (18%) | 5656 (19%) | 4484 (17%) |
| Other backward class | 21 813 (38%) | 11 461 (37%) | 10 352 (38%) |
| None of the above/no caste or tribe/do not know/missing | 16 001 (28%) | 8173 (27%) | 7828 (29%) |
| Religion | |||
| Hindu | 42 322 (73%) | 22 482 (74%) | 19 840 (73%) |
| Muslim | 6806 (12%) | 3625 (12%) | 3181 (12%) |
| Christian | 5802 (10%) | 3069 (10%) | 2733 (10%) |
| Other | 2719 (4.7%) | 1392 (4.6%) | 1327 (4.9%) |
| Region | |||
| North | 10 537 (18%) | 5536 (18%) | 5001 (18%) |
| Central | 7975 (14%) | 4257 (14%) | 3718 (14%) |
| East | 10 443 (18%) | 5344 (17%) | 5099 (19%) |
| Northeast | 7551 (13%) | 4285 (14%) | 3266 (12%) |
| West | 7580 (13%) | 3977 (13%) | 3603 (13%) |
| South | 13 563 (24%) | 7169 (23%) | 6394 (24%) |
Numbers presented in table are unweighted.
*Q1: first quartile, Q3: third quartile.
†MPCE (monthly per capita expenditure) which is defined as total monthly household consumption expenditure divided by household size. It includes household’s per capita spending on food and non-food items including spending on health, education, utilities, etc.
‡Includes temporarily laid off, on sick or other leave, or in job training.
§Household food unavailability in the past 12 months, where household members either reduced their meal size, did not eat even though they were hungry, or did not eat for a whole day because enough food was not available in the household.
Prevalence of frailty
The observed frailty index values ranged between 0 and 0.83, with a median of 0.14 (IQI=0.08–0.25) and mean of 0.18 (SD=0.13) (online supplemental S2 figure, panel A). Using the cut-off of 0.25, the prevalence of frailty among adults 45 years and older was 29.5% (95% CI 28.7 to 30.4). Prevalence was higher among older adults compared with middle-aged adults (43.2% vs 16.2%) and among women compared with men (36.1% vs 21.7%) (online supplemental S5 table). For middle-aged adults, prevalence of frailty among females was double that in males (21.4% vs 9.6%). For older participants, frailty prevalence was almost 20 percentage points higher in females than in males (52.2% vs 33.2%).
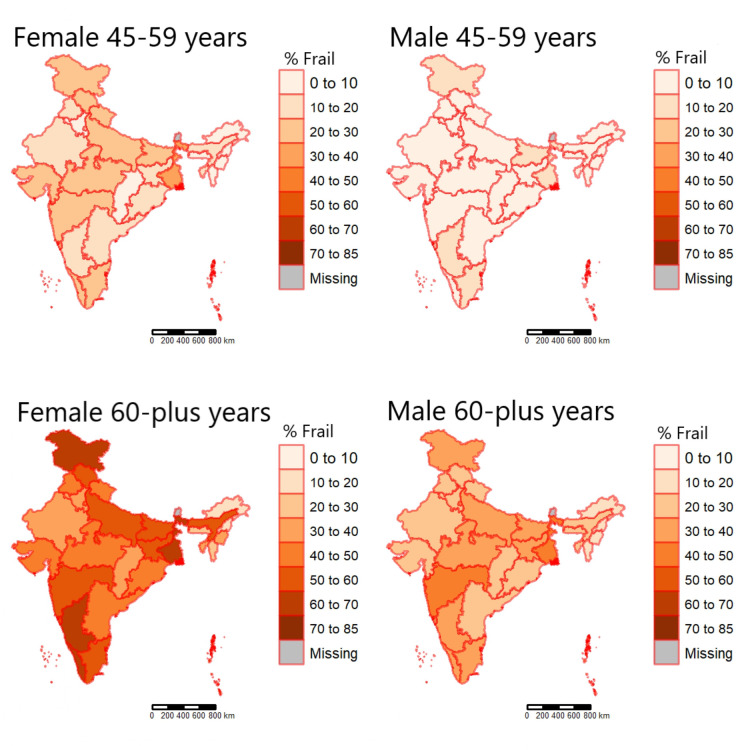
There was substantial geographical variation in the prevalence of frailty, ranging between 8.8% in Arunachal Pradesh and 38.2% in West Bengal (figure 1). Among older males, the prevalence varied between 11.8% in Nagaland and 42.7% in West Bengal. In 14 out of 35 states, more than 50% of the older women were frail, with the highest prevalence in Jammu and Kashmir (69%). Region-wise, five out of the seven north-eastern states covered always appeared among the bottom eight states with lowest prevalence, for both the age groups and sexes.
Figure 1.
State-wise prevalence of frailty, by sex and age group. Individuals with frailty index ≥0.25 are defined as ‘frail’. Prevalence estimates are weighted, using state-level individual sampling weights provided in data.
Sociodemographic, economic and lifestyle factors associated with frailty
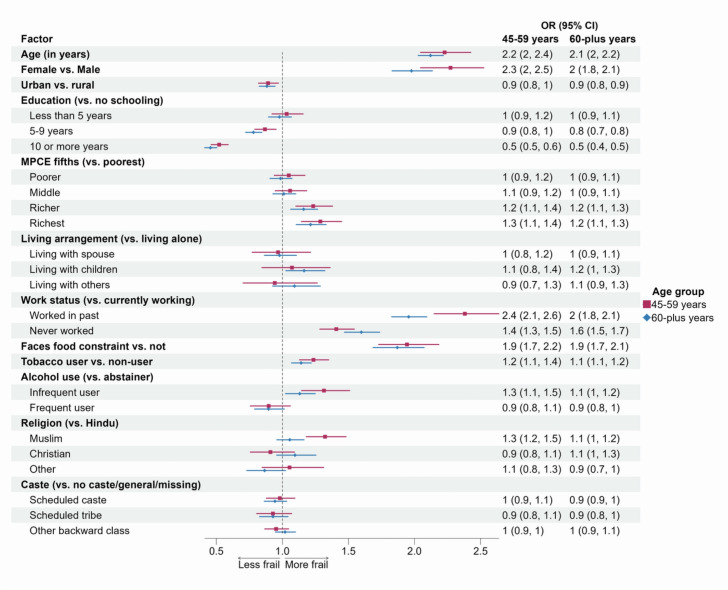
Frailty prevalence varied widely across different social strata (online supplemental S5 table). Females had higher odds of being frail than males (OR (95% CI)=2.3 (2 to 2.5) among middle-aged adults and 2.0 (1.8 to 2.1) among older adults), after adjusting for other background characteristics (figure 2). Among middle-aged participants, Muslims had 32% (95% CI 18% to 48%) higher odds of being frail, compared with Hindus; the difference was attenuated in the older ages (OR (95% CI)=1.1 (1 to 1.2)). Adjusted odds of being frail increased by 23% and 12% with 1 year increase in age, among middle-aged and older participants, respectively. While higher education was negatively associated with frailty, with more educated people having lower odds, the individuals in the two highest expenditure fifths were likely to be frailer than those in the lowest 20%. The odds of being frail were higher among participants from rural areas compared with urban areas, tobacco users compared with non-users, infrequent drinkers compared with abstainers and among participants facing food constraint.
Figure 2.
Forest plot of adjusted ORs (95% CI) for frailty, by participants’ background characteristics. MPCE (monthly per capita expenditure) is defined as total monthly household consumption expenditure divided by household size. Food constraint refers to household food unavailability in the past 12 months, where household members either reduced their meal size, did not eat even though they were hungry, or did not eat for a whole day because enough food was not available in the household.
Association with adverse health outcomes
Six per cent of the middle-aged and 8% of the older adults were hospitalised in past 12 months (table 2). Fall in the past 2 years was recorded among 16% of middle-aged adults and 20% of older adults. The median cognition score was 27 (IQI=22–32) and 7% and 15% of the middle-aged and older populations, respectively, had poor cognition, that is, were in the lowest 10% (online supplemental S2 figure, panel B). In both age groups, these adverse outcomes were more frequent, often double, among the frail participants compared with the non-frail. After adjusting for background characteristics of participants, frailty was associated with higher odds of all three outcomes studied—hospitalisation in the last 12 months (OR (95% CI)=2.4 (2.1 to 2.7) among middle-aged adults and 2.2 (2.0 to 2.4) among older adults), fall in the past 2 years (OR (95% CI)=2.17 (2.01 to 2.36) and 1.9 (1.77 to 2.03) in middle-aged and older adults, respectively) and poor cognition (OR (95% CI)=1.33 (1.16 to 1.53) and 1.39 (1.26 to 1.54) in middle-aged and older adults, respectively) (table 2).
Table 2.
Association between frailty and adverse outcomes—hospitalised in last 12 months, any fall in past 2 years and poor cognition
| Outcome | 45–59 years old adults | 60+ adults | ||||||
| All | Non-frail | Frail | Adjusted* OR (95% CI) | All | Non-frail | Frail | Adjusted* OR (95% CI) | |
| Hospitalised in last 12 months | ||||||||
| No | 28 440 (94%) | 24 658 (95%) | 3782 (89%) | – | 24 631 (92%) | 15 364 (94%) | 9267 (89%) | – |
| Yes | 1681 (5.6%) | 1215 (4.7%) | 466 (11%) | 2.35 (2.09 to 2.66) | 2038 (7.6%) | 911 (5.6%) | 1127 (11%) | 2.19 (1.98 to 2.42) |
| Missing | 447 | 393 | 54 | 412 | 226 | 186 | ||
| Any fall in past 2 years | ||||||||
| No | 25 651 (84%) | 22 605 (86%) | 3046 (71%) | – | 21 712 (80%) | 14 005 (85%) | 7707 (73%) | – |
| Yes | 4914 (16%) | 3658 (14%) | 1256 (29%) | 2.17 (2.01 to 2.36) | 5365 (20%) | 2495 (15%) | 2870 (27%) | 1.9 (1.77 to 2.03) |
| Missing | 3 | 3 | 0 | 4 | 1 | 3 | ||
| Poor cognition† | ||||||||
| No | 22 017 (93%) | 19 343 (93%) | 2674 (88%) | – | 15 521 (85%) | 10 540 (88%) | 4981 (78%) | – |
| Yes | 1727 (7.3%) | 1362 (6.6%) | 365 (12%) | 1.33 (1.16 to 1.53) | 2750 (15%) | 1375 (12%) | 1375 (22%) | 1.39 (1.26 to 1.54) |
| Missing | 6824 | 5561 | 1263 | 8810 | 4586 | 4224 | ||
*Adjusted for participants’ sex, age, rural place of residence, education, consumption expenditure, living arrangement, work status, food constraint, tobacco use, alcohol use, religion, caste and state.
†Poor cognition was defined as a cognition score below the 10th percentile, which was 18.
Being frail was associated with a 74% (95% CI 45% to 109%) and 122% (95% CI 83% to 170%) increase in mean number of hospitalisations in the last 12 months and a 15% (95% CI 10% to 21%) and 18% (95% CI 13% to 23%) increase in mean number of nights spent in the hospital in last 12 months, among the middle-aged and older adults, respectively (table 3). Frailty was associated with one-unit lower cognition scores in both the age groups—the mean difference, for frailty versus not, was −1.02 (–1.2 to –0.84) in middle-aged adults and −1.05 (–1.2 to –0.89) in the older adults.
Table 3.
Association between frailty and adverse outcomes—number of times hospitalised in last 12 months, number of nights spent in hospital in last 12 months and cognition score
| Outcome | 45–59 years old adults | 60+ adults | ||||||
| All | Non-frail | Frail | Adjusted* effect estimate (95% CI) |
All | Non-frail | Frail | Adjusted* effect estimate (95% CI) | |
| Number of times hospitalised in last 12 months | ||||||||
| N | 30 121 | 25 873 | 4248 | Rate ratio= 1.74 (1.45 to 2.09) |
26 669 | 16 275 | 10 394 | Rate ratio= 2.22 (1.83 to 2.7) |
| Range | 0–23 | 0–14 | 0–23 | 0–20 | 0–7 | 0–20 | ||
| Mean (SD) | 0.07 (0.42) | 0.06 (0.33) | 0.16 (0.75) | 0.10 (0.43) | 0.06 (0.30) | 0.15 (0.58) | ||
| Median (IQR) | 0 (0, 0) | 0 (0–, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | ||
| Number of nights spent in hospital in last 12 months | ||||||||
| N | 30 120 | 25 872 | 4248 | Rate ratio= 1.15 (1.1 to 1.21) |
26 669 | 16 275 | 10 394 | Rate ratio= 1.18 (1.13 to 1.23) |
| Range | 0–169 | 0–169 | 0–120 | 0–120 | 0–120 | 0–90 | ||
| Mean (SD) | 0.34 (2.57) | 0.27 (2.35) | 0.74 (3.64) | 0.48 (2.88) | 0.33 (2.43) | 0.71 (3.47) | ||
| Median (IQR) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | ||
| Cognition score | ||||||||
| N | 23 744 | 20 705 | 3039 | Mean difference=−1.02 (−1.2 to 0.84) | 18 271 | 11 915 | 6356 | Mean difference=−1.05 (−1.2 to 0.89) |
| Range | 7–43 | 7–43 | 8–42 | 4–43 | 7–43 | 4–43 | ||
| Mean (SD) | 28 (6) | 28 (6) | 26 (6) | 26 (6) | 27 (6) | 24 (6) | ||
| Median (IQR) | 28 (24, 33) | 29 (24, 33) | 26 (22, 30) | 26 (21, 31) | 27 (22, 31) | 24 (19, 29) | ||
*Adjusted for participants’ sex, age, rural place of residence, education, consumption expenditure, living arrangement, work status, food constraint, tobacco use, alcohol use, religion, caste and state.
Sex differences
Of the 40 deficits that were considered, men fared worse than women only for grip strength, stroke, chronic obstructive pulmonary disease and asthma; whereas more women than men had poor general health, most diagnosed conditions, medical symptoms, mobility restrictions, difficulties with normal daily self-care activities and needed supervision or assistance, were either underweight, overweight or obese, and had slow gait speed (online supplemental S6 table). The sex differences in mobility restrictions and ADL/IADL limitations were especially pronounced, even in the middle-aged adults.
The adjusted odds of hospitalisation in the past 12 months, falls in the past 2 years and poor cognition were higher for frail compared with non-frail adults, in both women and men. In women the ORs were higher than in men, in both the age groups. Women-to-men RORs were thus higher than unity for all three outcomes, although their CIs included zero, except for falls in past 2 years in the 60+ age group, so that chance findings could not be ruled out (online supplemental S7 table).
Sensitivity analyses
Of the 40 deficits considered, all deficits, except body mass index, grip strength and gait speed, were missing in <2% of the 45+ participants; and these three measurements were missing in 10%–11% of participants (online supplemental S3 figure). The frailty index calculated using non-missing health deficit scores allowed up to three deficits to be missing and therefore could be calculated for 64 331 participants, resulting in <2% with missing frailty index (n=1231). There were small differences between participants with frailty index missing (n=1231) or not (n=64 331) (online supplemental S4 table). This alternative construction made no difference to the prevalence estimates—17% of middle-aged adults and 44% of older participants were frail using this metric (online supplemental S8 table). ORs for the association between frailty and adverse outcomes were also similar (online supplemental S9 table), suggesting that findings hold true irrespective of the proportion missing frailty information.
Using an alternative cut-off value of 0.21,35 41 the prevalence of frailty increased to 37%. Even though frailty prevalence was inevitably higher using this cut-off (online supplemental S8 table and S4 figure), the associations with adverse outcomes were similar (online supplemental S9 table).
No association between frailty and income was found after adjusting for other factors, when using household income instead of consumption expenditure as the economic indicator in analysis exploring sociodemographic, economic and lifestyle factors associated with frailty (online supplemental S5 figure).
Discussion
Our study provides national, as well as state-level, estimates of prevalence of frailty and its association with outcomes across the age spectrum among 45+ Indian adults. Our study showed that frailty is common among 45+ Indian adults and it varies across the states. We found that women were more than two times as likely to be frail than men, after adjusting for a wide range of factors. We showed that frailty, usually assessed only in older adults, was also prevalent in 45–59 years old middle-aged adults, and was associated with hospitalisation, falls and poor cognitive functioning (box 1).
Box 1. Key findings.
Frailty, typically assessed in older adults, was also prevalent in middle-aged Indian adults (43.2% in 60+ vs 16.2% in 45–59 years old).
The odds of frailty were two times as high in women than in men, after adjusting for background characteristics.
In both age groups, after adjusting for background characteristics of participants, frailty was associated with higher odds of all three outcomes studied—hospitalisation in the last 12 months (OR=2.4 and 2.2 in middle-aged and older adults, respectively), fall in the past two years (2.17 and 1.9) and poor cognition (1.33 and 1.39).
Associations between frailty and adverse outcomes were consistently stronger for women relative to men, although not statistically significant.
Frailty prevalence in LMICs
Based on a nationally representative sample of 45+ years old Indian adults, we estimated a frailty prevalence of 29.5%, using a frailty index with 40 deficits. A recent systematic review in 62 countries across the world reported a pooled frailty index prevalence of 24% (95% CI 22% to 26%) based on 71 studies.4 Region-wise, these estimates were 38% (95% CI 37% to 39%) in sub-Saharan Africa, 30% (95% CI 28% to 31%) in Latin America and the Caribbean, 25% (95% CI 19% to 32%) in Asia, 22% (95% CI 20% to 24%) in Europe and 21% (95% CI 11% to 33%) in Northern America. Another systematic review focussing on LMICs reported a pooled prevalence of 18.0% (95% CI 5.8% to 35.0%) based on four studies using a frailty index approach.5 Comparison, however, is difficult because prevalence estimates vary greatly by frailty assessment method, and estimates from studies using frailty indices are available only from few LMICs.4 5 It is further compounded by differences in the cut-off value and the type of study population.
Factors associated with frailty
Our findings are in line with associations observed in other studies—female sex,22 lower education12 and tobacco use42 are well-known determinants of frailty. Our analyses pointed out that sex-differences in mobility restrictions and ADL/IADL limitations were especially pronounced, even among the middle-aged adults. Interestingly, we found frailty to be more prevalent in upper fifths of consumption expenditure, while many studies have shown an inverse gradient with economic well-being. We hypothesise that this may be because frail people tend to incur more healthcare expenditure, resulting in higher consumption expenditure. The positive association, however, was no longer present when per capita household income was instead used as the economic indicator. Another intriguing finding was that infrequent drinking was associated with higher odds of frailty compared with abstaining, but the same was not true for frequent drinking. Other studies have shown similar associations with infrequent and frequent alcohol intakes compared with zero consumption.20 43 44 This, however, should be treated with caution, as it can be due to residual confounding or healthy survivor bias. Our results suggest that vulnerable groups should be targeted when developing interventions to prevent and mange frailty. For achieving best results, the interventions should be customised per their needs.45 For this, knowledge of underlying mechanisms is essential and should be explored in future frailty research.
Outcomes associated with frailty
Frailty was associated with hospitalisation, falls and poor cognition, across both the age groups and sexes. A systematic review of 13 prospective studies in community-dwelling older adults found physical frailty to be a predictor of hospitalisation.46 The authors speculated that fall-related injuries could be one of the contributors. Another systematic review of 11 studies showed that frailty, however defined, is a significant predictor of future falls among community-dwelling older people. Fall risk according to frailty was found to be higher in men than in women. A prospective population-based study, using data from the Canadian Study of Health and Ageing, showed that frailty status, defined using various criteria, is strongly associated with changes in cognition.47
Frailty in middle-aged adults
Inclusion of over 34 000 adults aged 45–59 years in LASI allowed us to examine frailty, its risk factors and its association with adverse outcomes for the first time in the middle-aged Indian population. The association between frailty and hospitalisation and falls was even stronger in middle-aged adults compared with older adults. Although the prevalence of frailty increases with age, it is not limited to the elderly. Studies looking into associations between frailty and adverse outcomes in middle-aged adults are rare, and they highlight the need to identify, manage and prevent frailty across the age spectrum.20 48 49 The frailty index has been validated in young and middle-aged adults in few studies and there exits limited evidence of predictive validity of frailty index in younger populations.50 51 However, it is not clear if frailty, as a construct, is similar for older and younger adults.52 Comparison of distribution of deficits in middle-aged and older adults (online supplemental S10 table) suggests that frailty in middle-aged adults is probably due to long-term health problems that adversely affect their overall functioning. More studies are needed to understand how frailty can be conceptualised and measured in middle-aged and younger adults, and whether assessing frailty in them makes any difference to their health or the care they receive.
Our study has many strengths. First, our study provides frailty prevalence estimates among 45+ adults for all Indian states and union territories (except Sikkim), in addition to a national prevalence estimate. Second, we examined prevalence of frailty, its risk factors and association with adverse outcomes in middle-aged adults, in addition to older adults. Third, our frailty index was constructed using 40 deficits, 30 being the minimum number to ensure sufficient accuracy in predicting adverse events. We included deficits pertaining to mental impairment and IADL aimed at assessing cognitive functioning, thus capturing the multidimensionality of frailty. Finally, the sensitivity analyses helped demonstrate that our findings about variation in frailty and its association with outcomes are robust to the cut-off used to define frailty.
We also recognise certain limitations. First, we were not able to define other frailty measures such as the frailty phenotype, based on available data. Given that prevalence estimates vary widely depending on the assessment method,4 5 11 41 it would have been more informative if we were able to compare our findings using other frailty measures. Second, our cross-sectional study is unable to look at temporal associations between frailty and adverse health outcomes. LASI is designed as a panel study and data from subsequent waves will allow for examination of temporal associations in the future. Third, LASI employed a multistage cluster sampling design but variables identifying participants belonging to the same cluster have not been made publicly available, limiting our ability to account for the cluster sampling design in analyses and generate robust SEs.53 Fourth, there is but limited evidence to support the use of frailty index in middle-aged adults52 54 55 and future research should explore suitable frailty measures and cut-offs.
Conclusion
Our study has implications for healthcare delivery planning. We show that women are significantly more likely to be frail compared with men, across both age groups studied. These high levels of frailty among women will have a significant impact on patient-reported and clinical outcomes. Strategies to mitigate frailty should consider these sex differences. Also, we have demonstrated that frailty is prevalent in 45–59 years old middle-aged adults, exhibits social patterning and is associated with adverse outcomes, suggesting that younger adults may be identified as frail and may benefit from early detection and delivery of timely care. In a resource-constrained setting such as India, the focus must be on prevention and early detection of frailty. Both management of risk factors and screening for frailty have to be implemented, preferably at the primary care level. Given the strong links between social inequalities and frailty, marginalised populations must be prioritised.
Supplementary Material
Acknowledgments
We would like to thank International Institute for Population Sciences, LASI survey team and study participants who made this analysis possible.
Footnotes
Contributors: AG and MK conceived the idea for the study, performed literature review, conducted data preparation, carried out statistical analyses and wrote the first draft. All authors contributed to interpretation of the study findings. VJ, MW, ND and AG contributed to reviewing and editing the final draft. All authors have read and approved the final manuscript. AG is the guarantor of the study.
Funding: No funding was received to conduct this study. LASI Wave 1 was financially supported by Ministry of Health and Family Welfare, Govt. of India, National Institute on AgingAgeing (NIA/NIH), USA and United Nations Population Fund, India.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: AG, MK and ND have no conflicts of interest to declare. MW is a consultant to Amgen, and Freeline. VJ has received grant funding from GSK, Baxter Healthcare, and Biocon and honoraria from Bayer, AstraZeneca, Boeringer Ingelheim, NephroPlus and Zydus Cadilla, under the policy of all honoraria being paid to the organisation.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Ethics approval and consent to participate: Not applicable. We used LASI survey data available in the public domain from the International Institute for Population Sciences website. Ethics approval for LASI survey was granted by all collaborating institutions and the Indian Council for Medical Research. Written informed consent was obtained for household survey, individual survey and dried blood spot collection.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
LASI survey data are available in the public domain from the International Institute for Population Sciences (IIPS) website. Application has to be made for access to data and access is granted after review by IIPS for legitimate academic research purposes. Link for application can be accessed at https://www.iipsindia.ac.in/content/LASI-data.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Hoogendijk EO, Afilalo J, Ensrud KE, et al. Frailty: implications for clinical practice and public health. The Lancet 2019;394:1365–75. 10.1016/S0140-6736(19)31786-6 [DOI] [PubMed] [Google Scholar]
- 2.Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. The Lancet 2013;381:752–62. 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aguayo GA, Donneau A-F, Vaillant MT, et al. Agreement between 35 published frailty scores in the general population. Am J Epidemiol 2017;186:420–34. 10.1093/aje/kwx061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Caoimh R, Sezgin D, O’Donovan MR, et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing 2021;50:96–104. 10.1093/ageing/afaa219 [DOI] [PubMed] [Google Scholar]
- 5.Siriwardhana DD, Walters K, Rait G, et al. Cross-cultural adaptation and Psychometric evaluation of the Sinhala version of Lawton instrumental activities of daily living scale. PLoS One 2018;13:e0199820. 10.1371/journal.pone.0199820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alvarado BE, Zunzunegui M-V, Béland F, et al. Life course social and health conditions linked to frailty in Latin American older men and women. J Gerontol A Biol Sci Med Sci 2008;63:1399–406. 10.1093/gerona/63.12.1399 [DOI] [PubMed] [Google Scholar]
- 7.Da Mata FAF, Pereira PP da S, Andrade KRC de, et al. Prevalence of frailty in Latin America and the Caribbean: a systematic review and meta-analysis. PLoS One 2016;11:e0160019. 10.1371/journal.pone.0160019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ofori-Asenso R, Chin KL, Mazidi M, et al. Global incidence of frailty and Prefrailty among community-dwelling older adults: a systematic review and meta-analysis. JAMA Netw Open 2019;2:e198398. 10.1001/jamanetworkopen.2019.8398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harttgen K, Kowal P, Strulik H, et al. Patterns of frailty in older adults: comparing results from higher and lower income countries using the survey of health, ageing and retirement in Europe (SHARE) and the study on global ageing and adult health (SAGE). PLoS One 2013;8:e75847. 10.1371/journal.pone.0075847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kshatri JS, Palo SK, Bhoi T, et al. Associations of Multimorbidity on frailty and dependence among an elderly rural population: findings from the AHSETS study. Mech Ageing Dev 2020;192:111384. 10.1016/j.mad.2020.111384 [DOI] [PubMed] [Google Scholar]
- 11.Kendhapedi KK, Devasenapathy N. Prevalence and factors associated with frailty among community-dwelling older people in rural Thanjavur District of South India: a cross-sectional study. BMJ Open 2019;9:e032904. 10.1136/bmjopen-2019-032904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biritwum RB, Minicuci N, Yawson AE, et al. Prevalence of and factors associated with frailty and disability in older adults from China, Ghana, India, Mexico, Russia and South Africa. Maturitas 2016;91:8–18. 10.1016/j.maturitas.2016.05.012 [DOI] [PubMed] [Google Scholar]
- 13.Chaudhary M, Arokiasamy P. Patterns of frailty and quality of life among older adults: comparative analysis using SAGE States of India. J Popul Ageing 2019;12:1–23. [Google Scholar]
- 14.Dasgupta A, Bandyopadhyay S, Bandyopadhyay L, et al. How frail are our elderly? an assessment with Tilburg frailty indicator (TFI) in a rural elderly population of West Bengal. J Family Med Prim Care 2019;8:2242–8. 10.4103/jfmpc.jfmpc_445_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Collard RM, Boter H, Schoevers RA, et al. Prevalence of frailty in Community‐Dwelling older persons: a systematic review. J Am Geriatr Soc 2012;60:1487–92. 10.1111/j.1532-5415.2012.04054.x [DOI] [PubMed] [Google Scholar]
- 16.He B, Ma Y, Wang C, et al. Prevalence and risk factors for frailty among community-dwelling older people in China: a systematic review and meta-analysis. J Nutr Health Aging 2019;23:442–50. 10.1007/s12603-019-1179-9 [DOI] [PubMed] [Google Scholar]
- 17.Kojima G, Iliffe S, Taniguchi Y, et al. Prevalence of frailty in Japan: A systematic review and meta-analysis. J Epidemiol 2017;27:347–53. 10.1016/j.je.2016.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conroy S, Maynou L. Frailty: time for a new approach to health care? Lancet Healthy Longev 2021;2:e60–1. 10.1016/S2666-7568(20)30064-7 [DOI] [PubMed] [Google Scholar]
- 19.Blodgett JM, Rockwood K, Theou O. Changes in the severity and lethality of age-related health deficit accumulation in the USA between 1999 and 2018: a population-based cohort study. Lancet Healthy Longev 2021;2:e96–104. 10.1016/S2666-7568(20)30059-3 [DOI] [PubMed] [Google Scholar]
- 20.Hanlon P, Nicholl BI, Jani BD, et al. Frailty and pre-frailty in middle-aged and older adults and its association with Multimorbidity and mortality: a prospective analysis of 493 737 UK Biobank participants. Lancet Public Health 2018;3:e323–32. 10.1016/S2468-2667(18)30091-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arokiasamy P. India's escalating burden of non-communicable diseases. The Lancet Global Health 2018;6:e1262–3. 10.1016/S2214-109X(18)30448-0 [DOI] [PubMed] [Google Scholar]
- 22.Gordon EH, Peel NM, Samanta M, et al. Sex differences in frailty: A systematic review and meta-analysis. Exp Gerontol 2017;89:30–40. 10.1016/j.exger.2016.12.021 [DOI] [PubMed] [Google Scholar]
- 23.Ahrenfeldt LJ, Möller S, Thinggaard M, et al. Sex differences in Comorbidity and frailty in Europe. Int J Public Health 2019;64:1025–36. 10.1007/s00038-019-01270-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kane AE, Howlett SE. Sex differences in frailty: comparisons between humans and Preclinical models. Mech Ageing Dev 2021;198:111546. 10.1016/j.mad.2021.111546 [DOI] [PubMed] [Google Scholar]
- 25.Gordon E, Hubbard R. Physiological basis for sex differences in frailty. Current Opinion in Physiology 2018;6:10–5. 10.1016/j.cophys.2018.02.013 [DOI] [Google Scholar]
- 26.Gordon EH, Hubbard RE. Do sex differences in chronic disease underpin the sex-frailty paradox? Mech Ageing Dev 2019;179:44–50. 10.1016/j.mad.2019.02.004 [DOI] [PubMed] [Google Scholar]
- 27.International Institute for Population Sciences (IIPS), National Programme for Health Care of Elderly (NPHCE), MoHFW, Harvard T. H. Chan School of Public Health (HSPH) and the University of Southern California (USC) 2020 . Longitudinal ageing study in India (LASI) wave 1, 2017-18, India report, international Institute for population sciences, Mumbai. 2020.
- 28.Perianayagam A, Bloom D, Lee J, et al. Cohort profile: the longitudinal ageing study in India (LASI). Int J Epidemiol 2022;51:e167–76. 10.1093/ije/dyab266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.International Institute for population sciences, longitudinal ageing study in India (LASI), wave – I, 2017-18. n.d. Available: https://www.iipsindia.ac.in/content/LASI-data
- 30.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 2007;62:722–7. 10.1093/gerona/62.7.722 [DOI] [PubMed] [Google Scholar]
- 31.Searle SD, Mitnitski A, Gahbauer EA, et al. A standard procedure for creating a frailty index. BMC Geriatr 2008;8:1–10. 10.1186/1471-2318-8-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gordon EH, Reid N, Khetani IS, et al. How frail is frail? A systematic Scoping review and synthesis of high impact studies. BMC Geriatr 2021;21:719. 10.1186/s12877-021-02671-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rockwood K, Andrew M, Mitnitski A. A comparison of two approaches to measuring frailty in elderly people. J Gerontol A Biol Sci Med Sci 2007;62:738–43. 10.1093/gerona/62.7.738 [DOI] [PubMed] [Google Scholar]
- 34.Song X, Mitnitski A, Rockwood K. And 10‐Year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc 2010;58:681–7. 10.1111/j.1532-5415.2010.02764.x [DOI] [PubMed] [Google Scholar]
- 35.Rockwood K, Song X, Mitnitski A. Changes in relative fitness and frailty across the adult LifeSpan: evidence from the Canadian national population health survey. CMAJ 2011;183:E487–94. 10.1503/cmaj.101271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Direk N, Williams S, Smith JA, et al. An analysis of two genome-wide Association meta-analyses identifies a new locus for broad depression phenotype. Biol Psychiatry 2017;82:322–9. 10.1016/j.biopsych.2016.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mullahy J. Specification and testing of some modified count data models. Journal of Econometrics 1986;33:341–65. 10.1016/0304-4076(86)90002-3 [DOI] [Google Scholar]
- 38.Woodward M. Rationale and Tutorial for analysing and reporting sex differences in cardiovascular associations. Heart 2019;105:1701–8. 10.1136/heartjnl-2019-315299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.R Core Team . R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, 2020. Available: https://www.R-project.org/ [Google Scholar]
- 40.Zhu Y, Edwards D, Mant J, et al. Characteristics, service use and mortality of clusters of Multimorbid patients in England: a population-based study. BMC Med 2020;18:78. 10.1186/s12916-020-01543-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blodgett J, Theou O, Kirkland S, et al. Frailty in NHANES: comparing the frailty index and phenotype. Arch Gerontol Geriatr 2015;60:464–70. 10.1016/j.archger.2015.01.016 [DOI] [PubMed] [Google Scholar]
- 42.Kojima G, Iliffe S, Walters K. Smoking as a Predictor of frailty: a systematic review. BMC Geriatr 2015;15:131. 10.1186/s12877-015-0134-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ortolá R, García-Esquinas E, León-Muñoz LM, et al. Patterns of alcohol consumption and risk of frailty in community-dwelling older adults. GERONA 2016;71:251–8. 10.1093/gerona/glv125 [DOI] [PubMed] [Google Scholar]
- 44.Kojima G, Liljas A, Iliffe S, et al. A systematic review and meta-analysis of prospective associations between alcohol consumption and incident frailty. Age Ageing 2018;47:26–34. 10.1093/ageing/afx086 [DOI] [PubMed] [Google Scholar]
- 45.Hanlon P, Blane DN, Macdonald S, et al. Our response to rising frailty in younger people must address prevention burden. The Lancet Healthy Longevity 2021;2:e245. 10.1016/S2666-7568(21)00052-0 [DOI] [PubMed] [Google Scholar]
- 46.Kojima G. Frailty as a Predictor of Hospitalisation among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health 2016;70:722–9. 10.1136/jech-2015-206978 [DOI] [PubMed] [Google Scholar]
- 47.Mitnitski A, Fallah N, Rockwood MRH, et al. Transitions in cognitive status in relation to frailty in older adults: a comparison of three frailty measures. J Nutr Health Aging 2011;15:863–7. 10.1007/s12603-011-0066-9 [DOI] [PubMed] [Google Scholar]
- 48.Segaux L, Broussier A, Oubaya N, et al. Several frailty parameters highly prevalent in middle age (50-65) are independent predictors of adverse events. Sci Rep 2021;11:8774. 10.1038/s41598-021-88410-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lu Z, Er Y, Zhan Y, et al. Association of frailty status with risk of fall among middle-aged and older adults in China: a nationally representative cohort study. J Nutr Health Aging 2021;25:985–92. 10.1007/s12603-021-1655-x [DOI] [PubMed] [Google Scholar]
- 50.Blodgett JM, Theou O, Howlett SE, et al. A frailty index from common clinical and laboratory tests predicts increased risk of death across the life course. Geroscience 2017;39:447–55. 10.1007/s11357-017-9993-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kehler DS, Ferguson T, Stammers AN, et al. Prevalence of frailty in Canadians 18-79 years old in the Canadian health measures survey. BMC Geriatr 2017;17:28. 10.1186/s12877-017-0423-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kunonga TP, Spiers GF, Beyer FR, et al. Effects of Digital Technologies on older people's access to health and social care: umbrella review. J Med Internet Res 2021;23:e25887. 10.2196/25887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Graubard BI, Korn EL. Regression analysis with clustered data. Statist Med 1994;13:509–22. 10.1002/sim.4780130514 Available: http://doi.wiley.com/10.1002/sim.v13:5/7 [DOI] [PubMed] [Google Scholar]
- 54.Hanlon P, Jani BD, Butterly E, et al. An analysis of frailty and Multimorbidity in 20,566 UK Biobank participants with type 2 diabetes. Commun Med (Lond) 2021;1:28. 10.1038/s43856-021-00029-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kanters DM, Griffith LE, Hogan DB, et al. Assessing the measurement properties of a frailty index across the age spectrum in the Canadian longitudinal study on aging. J Epidemiol Community Health 2017;71:794–9. 10.1136/jech-2016-208853 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-071842supp001.pdf (689.3KB, pdf)
Data Availability Statement
LASI survey data are available in the public domain from the International Institute for Population Sciences (IIPS) website. Application has to be made for access to data and access is granted after review by IIPS for legitimate academic research purposes. Link for application can be accessed at https://www.iipsindia.ac.in/content/LASI-data.