Abstract
INTRODUCTION
People with mental health conditions are disproportionately affected by smoking-related diseases and death. The aim of this study was to assess whether health professional (HP) interactions regarding smoking cessation and nicotine vaping products (NVPs) differ by mental health condition.
METHODS
The cross-sectional 2018 International Tobacco Control Four Country (Australia, Canada, England, United States) Smoking and Vaping Survey data included 11040 adults currently smoking or recently quit. Adjusted weighted logistic regressions examined associations between mental health (self-reported current depression and/or anxiety) and visiting a HP in last 18 months; receiving advice to quit smoking; discussing NVPs with a HP; and receiving a recommendation to use NVPs.
RESULTS
Overall, 16.1% self-reported depression and anxiety, 7.6% depression only, and 6.6% anxiety only. Compared with respondents with no depression/anxiety, those with depression (84.7%, AOR=2.65; 95% CI: 2.17–3.27), anxiety (82.2%, AOR=2.08; 95% CI: 1.70–2.57), and depression and anxiety (87.6%, AOR=3.74; 95% CI: 3.19–4.40) were more likely to have visited a HP. Among those who had visited a HP, 47.9% received advice to quit smoking, which was more likely among respondents with depression (AOR=1.58; 95% CI: 1.34–1.86), and NVP discussions were more likely among those with depression and anxiety (AOR=1.63; 95% CI: 1.29–2.06). Of the 6.1% who discussed NVPs, 33.5% received a recommendation to use them, with no difference by mental health.
CONCLUSIONS
People with anxiety and/or depression who smoke were more likely to visit a HP than those without, but only those with depression were more likely to receive cessation advice, and only those with depression and anxiety were more likely to discuss NVPs. There are missed opportunities for HPs to deliver cessation advice. NVP discussions and receiving a positive recommendation to use them were rare overall.
Keywords: depression, anxiety, mental health, smoking cessation, cessation advice, cessation support, quit smoking, vaping products, e-cigarette, health professional discussions
INTRODUCTION
Smoking is a leading preventable cause of illness and premature death in the United Kingdom (UK) and worldwide1. Smoking prevalence is considerably higher in disadvantaged groups, including people with mental health conditions 2-5. For example, in England in 2014, among those with a current common mental health condition, smoking prevalence was 34.1%, compared to 19.6% in people without4. In the United States (US), among those who reported any past-year mental illness in 2019, past-month cigarette smoking was 28.2%, compared to 15.8% in people without past-year mental illness6. People with mental health conditions are more likely to smoke heavily, and be highly dependent on cigarettes4. Smoking is a significant contributor to the discrepancy in life expectancy between people with and without mental health conditions2,7,8; smoking cessation should improve physical and mental health9.
Most adults who smoke say they want to quit smoking10,11, including people with mental health conditions5. Approximately 40–50% of adults who smoke report making a quit attempt annually, but most quit attempts are made without evidence-based treatments and relapse to smoking10,11. Health professionals (HPs) can trigger patients’ interest in quitting12 and provide treatments to support quit attempts, which can markedly increase cessation rates13. However, research has shown that the rate at which HPs provide advice to quit smoking and offer cessation support/treatment is suboptimal, internationally14,15. Nicotine vaping products (NVPs) are substantially less harmful than smoking combustible tobacco16 and improve cessation rates compared to nicotine replacement therapy (NRT) and non-nicotine vaping products17. However, there are concerns due to uncertainty about the long-term health effects of NVPs and youth uptake of NVPs. Some experts recommend that HPs encourage the use of NVPs as another option for smoking cessation on par with medicinally licensed pharmacotherapies and behavioral support18,19.
Policy and guidelines around NVPs vary internationally18. Currently, in the UK, NVPs are widely available as consumer products and clinical guidelines recommend that NVPs are ‘accessible to adults who smoke’20. In Australia, the sale of NVPs is prohibited unless on prescription from a licensed HP – clinical guidelines recommend NVPs for those ‘who have tried to achieve smoking cessation with first-line therapy but failed’21. In Canada, NVPs are widely available in various retail locations, but clinical guidelines do not include NVPs in the list of recommended smoking cessation treatment options22. In the US, historically NVPs were widely available on the open market, but only some tobacco-flavored brands have received market approval since 202123. NVPs are not recommended in US clinical guidelines – ‘recommend that clinicians direct patients who use tobacco to other tobacco cessation interventions with proven effectiveness and established safety’24.
HPs rarely discuss NVPs with patients who smoke: in 2016 among people who smoked who visited a HP, only 6.8% of survey respondents from Australia, Canada, England, and the US reported their HP discussing NVPs with them15. A cohort study found that the prevalence of NVP discussions were low and remained relatively unchanged between 2016, 2018 and 202025. Further, among respondents who discussed NVPs with HPs, only about one-third (37.8%) reported that their HP recommended that they use them15. The likelihood of receiving NVP recommendations from HPs in England was higher and increased significantly between 2016 and 2020, but did not change significantly in Australia, Canada or the US25.
To reduce smoking and narrow the inequalities in smoking prevalence that exist between people with and without mental health conditions, HPs needs to do more to assist those who smoke to quit – such as, increased guidance/encouragement for cessation and advising on harm reduction approaches (switching from smoking to using NVPs)26,27. One study28, using UK electronic health record data collected between 2009 and 2010, found that the annual mean number of consultations for patients who smoke and have a mental health condition was higher than for those without a mental health condition; however, the proportion of consultations in which cessation advice was recorded was lower for people with a mental health condition, compared to those without. Research into discussions and recommendations to use NVPs is sparse. One study15, using 2016 survey data from Australia, Canada, England and the US, found no difference in the proportion of people who smoke with and without self-reported current diagnosis/treatment of depression or anxiety who had discussions with a HP about NVPs; but fewer people who smoke with anxiety were recommended to use an NVP from their HPs, compared to people who smoke without anxiety.
In our study, we build on these findings, focusing on comparing respondents with and without depression and/or anxiety, as these are two of the most common mental health conditions globally29 but receive less attention compared to serious mental health illness30. Using cross-sectional 2018 International Tobacco Control Four Country Smoking and Vaping (ITC 4CV) Survey data from Australia, Canada, England and the US, this study investigated whether there were differences between those with and without a current diagnosis/treatment for depression and/or anxiety in: 1) visiting a HP; 2) receiving advice to quit smoking from a HP; 3) their HP discussing NVPs; and 4) receiving a positive recommendation to use NVPs from a HP. We also aimed to investigate if the association between depression and/or anxiety and each outcome varied by country.
METHODS
Data source and sample
This study used data from Wave 2 (March–June 2018) of the longitudinal ITC 4CV Survey, a cohort study of people who smoke, vape or those who recently quit smoking from Australia, Canada, England, and the US. Respondents (adults aged ≥18 years) were recruited using either probability-based sampling frames or non-probability opt-in sampling frames, or a combination of these methods, aiming to be representative of people who smoke, or vape at least weekly, in each country. Participants included those who were re-contacted from the previous wave and new participants who were recruited to address attrition and maintain sample size over time. Full methodological details are available elsewhere (https://itcproject.org/methods)31. This manuscript adhered to the STROBE guidelines.
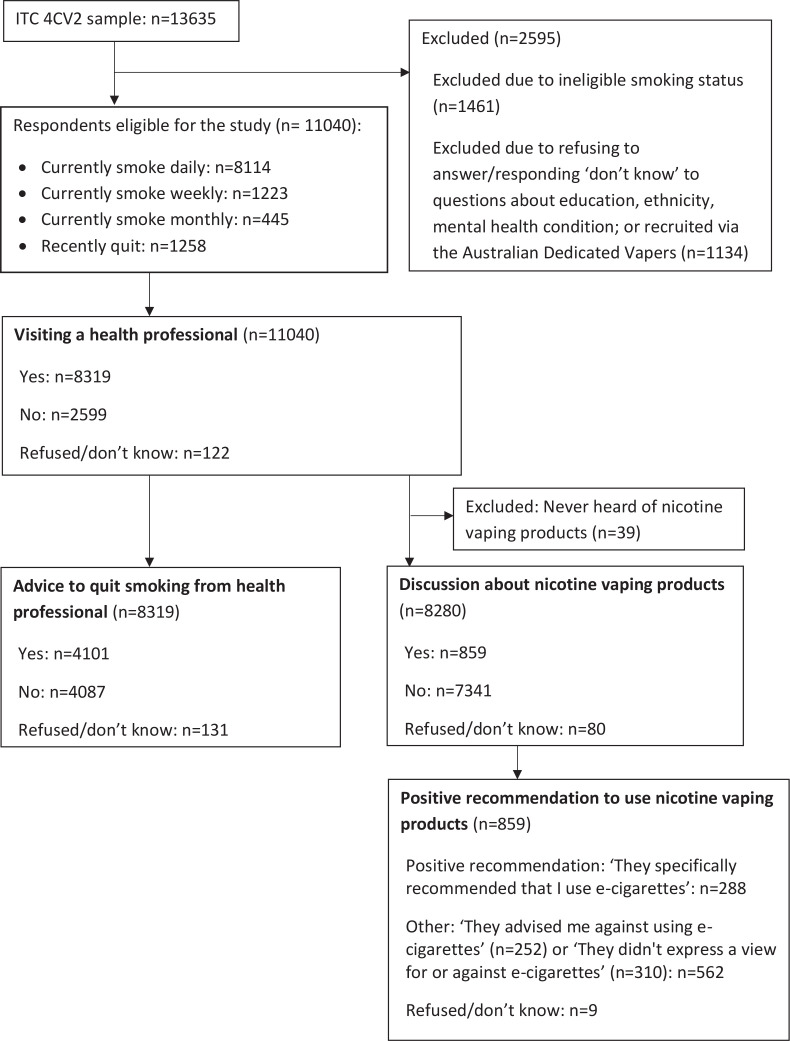
The study sample consisted of 11040 adult respondents who were either currently smoking cigarettes (daily/weekly/monthly) or had recently quit (quit smoking in the last 18 months and had smoked >100 cigarettes in their lifetime), at the time of the 2018 survey (Figure 1).
Figure 1.
Flow diagram showing the inclusion/exclusion criteria to generate the study sample, from Wave 2 (2018) of the ITC 4CV Survey (unweighted frequencies)
A more detailed description of the variables is provided in the pre-registered analysis plan https://osf.io/y72cj31.
Independent variable: mental health condition
The 2018 wave was the most recent ITC 4CV survey wave which contained survey questions about depression and anxiety (assessed with a single item measure, similar to past research)15,32. All respondents were asked: ‘Are you currently being treated for, or have you been diagnosed (current diagnosis) with, any of the following… [select all that apply]? Depression. Anxiety. …’. Response options: Selected/Not selected/Refused (excluded)/Don’t know (excluded). The answers were recoded into the mutually exclusive categories:
No depression/anxiety: ‘Not selected’ to both depression and anxiety.
Depression only: ‘Selected’ to depression but ‘Not selected’ to anxiety.
Anxiety only: ‘Selected’ to anxiety but ‘Not selected’ to depression.
Depression and anxiety: ‘Selected’ to both depression and anxiety.
Outcome measures
Visiting a HP
All respondents were asked: ‘In the last 18 months, have you visited a doctor or other health professional?’. Responses options were: yes, no, or refused to answer/don’t know (excluded).
Advice to quit smoking from HP
Respondents who indicated visiting a HP were asked: ‘On any visit to a doctor or health professional in the last 18 months, did you receive any advice to quit smoking?’. Responses options were: yes, no, or refused to answer/don’t know (excluded).
Discussion about NVPs
Respondents who indicated visiting a HP were asked: ‘On any visit to a doctor or health professional in the last 18 months, did the doctor or health professional talk to you about e-cigarettes?’. Responses options were: yes, no, or refused to answer/don’t know (excluded).
Positive recommendation to use NVPs
Respondents who indicated visiting a HP and indicated that their HP had discussed NVPs were asked: ‘What advice did the doctor or health professional give you about e-cigarettes?’. The response options were: ‘They specifically recommended that I use e-cigarettes’ (yes); ‘They advised me against using e-cigarettes’ (no); ‘They didn’t express a view for or against e-cigarettes’ (no); or refused to answer/don’t know (excluded).
Covariates
Covariates included: sex (male, female), age group (18–24, 25–39, 40–54, ≥55 years), country of residence (Australia, Canada, England, US), education level (low, moderate, high), ethnicity (Minority group, Majority group), annual household income level (low, moderate, high, no answer [valid response option]), cigarette smoking status (daily, non-daily [including weekly and monthly], former [quit smoking in the last 18 months and had smoked >100 cigarettes in their lifetime]), and problematic alcohol use (total score out of 12 based on the Alcohol Use Disorders Identification Test Consumption (AUDIT C)33 where: ≥5 points [yes], ≤4 points [no], or no answer [valid response option]).
Respondents who refused to answer or answered ‘don't know’ to the education level or ethnicity questions were excluded from the sample (Figure 1).
Statistical analysis
Unweighted frequencies and weighted proportions were calculated. The sample was weighted using derived cross-sectional survey weights31 to account for the stratified sampling design (defined by geographical regions within each country). Respondents who refused to answer or responded ‘don’t know’ to a question related to the outcome measures were excluded from logistic regression analyses (Supplementary file Table 1). Three separate weighted logistic regression models were generated to investigate the relationship between mental health condition and the four outcomes: 1) visiting a HP; 2) receiving advice to quit smoking from a HP, among those who visited a HP; 3) their HP discussing NVPs, among those who visited a HP; and 4) receiving a positive recommendation to use NVPs from a HP, among those who visited a HP and whose HP discussed NVPs. The weighted regression models were: Model 1, unadjusted model with mental health condition as the only independent variable; Model 2, adjusted for country, sex, age, education level, ethnicity, and income level; and Model 3, fully adjusted model, using Model 2 but additionally adjusted for cigarette smoking status and problematic alcohol use. To assess whether the association between mental health condition and each outcome varies by country, for each outcome, a likelihood-ratio test assessed whether there was a significant difference between Model 3 and a new model (Model 4) which contained interaction terms between mental health condition and country.
Assumptions of logistic regression were met34. The analysis plan was pre-registered: https://osf.io/y72cj. Analyses were conducted using RStudio (version 4.0.3), regression models were generated using the glm command of the mlogit package. As the regressions were weighted, the ‘family=quasibinomial’ argument was used. Exact p-values and 95% (likelihood ratio-based34) confidence intervals (CIs) are reported. Results were adjusted for multiple comparisons, where the significance level, alpha, was evaluated at 0.0125 level, as per the Bonferroni correction (α=0.05/4 outcomes= 0.0125).
RESULTS
Sample characteristics
The unweighted analytical sample included 11040 respondents (Table 1). The weighted sample was 54.2% male, and respondents were more likely to be in the majority ethnic group (White) and aged ≥40 years. Most of the respondents were residing in England (38.6%), followed by Canada (27.8%), then the US (21.1%), and then Australia (12.5%). The most common cigarette smoking status was current ‘daily’ (77.7%). The ‘non-daily’ smoking category (11.8%) was made up of 8.4% who currently smoked weekly, and 3.4% who currently smoked monthly. People who recently quit smoking comprised 10.5% of respondents. The majority of respondents had a moderate education level (47.7%), moderate annual household income level (33.9%), and did not have problematic alcohol use (62.9%). Slightly less than one-third of the respondents had self-reported depression and/or anxiety (30.3%), 7.6% had depression only, 6.6% had anxiety only, and 16.1% had both depression and anxiety.
Table 1.
Mental health condition and covariates by study sample and healthcare professional interactions regarding smoking cessation and nicotine vaping, cross-sectional ITC 4CV Survey, 2018 (N=11040)
| Variable | Study sample (N=11040) n (%) | Visiting a health professional (N=11040) n (%) | Advice to quit smoking from health professional (N=8319) n (%) | Discussion about nicotine vaping products (N=8280) n (%) | Positive recommendation to use nicotine vaping products (N=859) n (%) |
|---|---|---|---|---|---|
| Total | 11040 (100) | 8319a (74.6)b | 4101a (47.9)b | 859a (6.1)b | 288a (33.5)b |
| Mental health status | |||||
| No depression or anxiety | 7393 (69.7) | 5279 (69.8) | 2550 (47.2) | 459 (5.4) | 150 (31.3) |
| Depression only | 918 (7.6) | 763 (84.7) | 437 (57.0) | 110 (7.4) | 42 (38.8) |
| Anxiety only | 844 (6.6) | 662 (82.2) | 317 (44.1) | 89 (6.9) | 28 (37.1) |
| Depression and anxiety | 1885 (16.1) | 1615 (87.6) | 797 (47.3) | 201 (8.0) | 68 (35.0) |
| Country | |||||
| Australia | 1372 (12.5) | 1222 (85.7) | 650 (53.5) | 52 (3.0) | 12 (16.6) |
| Canada | 3157 (27.8) | 2473 (79.3) | 1159 (45.5) | 228 (5.2) | 64 (35.2) |
| England | 4217 (38.6) | 2822 (67.1) | 1242 (42.1) | 389 (8.4) | 166 (39.0) |
| US | 2294 (21.1) | 1802 (75.3) | 1050 (56.8) | 190 (6.0) | 46 (24.8) |
| Gender | |||||
| Male | 5372 (54.2) | 3777 (69.1) | 1940 (49.5) | 488 (6.8) | 170 (38.0) |
| Female | 5668 (45.8) | 4542 (81.0) | 2161 (46.2) | 371 (5.5) | 118 (27.9) |
| Age (years) | |||||
| 18–24 | 2167 (9.8) | 1427 (66.2) | 610 (36.4) | 262 (8.6) | 93 (34.6) |
| 25–39 | 2406 (33.6) | 1617 (67.0) | 708 (42.5) | 215 (6.7) | 83 (44.5) |
| 40–54 | 2872 (28.6) | 2198 (76.5) | 1088 (48.1) | 187 (5.8) | 58 (27.1) |
| ≥55 | 3595 (28.0) | 3077 (84.5) | 1695 (55.7) | 195 (5.3) | 54 (26.4) |
| Ethnicity | |||||
| Minority group | 1636 (13.2) | 1168 (72.7) | 603 (50.9) | 190 (8.3) | 66 (33.5) |
| Majority group | 9404 (86.8) | 7151 (74.9) | 3498 (47.4) | 669 (5.8) | 222 (33.4) |
| Education level | |||||
| Low | 3519 (31.1) | 2616 (74.5) | 1283 (51.9) | 224 (5.2) | 72 (26.0) |
| Moderate | 4627 (47.7) | 3543 (74.5) | 1771 (47.6) | 346 (6.5) | 97 (33.4) |
| High | 2894 (21.2) | 2160 (75.0) | 1047 (42.7) | 289 (6.8) | 119 (42) |
| Income level | |||||
| Low | 3533 (31.0) | 2725 (76.5) | 1347 (49.2) | 242 (5.4) | 67 (29.5) |
| Moderate | 3706 (33.9) | 2673 (72.7) | 1331 (47.9) | 278 (6.1) | 94 (32.8) |
| High | 3249 (30.0) | 2499 (75.3) | 1239 (46.7) | 308 (6.9) | 118 (38.8) |
| No answer | 552 (5.1) | 422 (71.0) | 184 (45.8) | 31 (6.0) | 9 (22.6) |
| Cigarette smoking status | |||||
| Daily | 8114 (77.7) | 6142 (74.7) | 3252 (51.8) | 611 (6.0) | 227 (34.6) |
| Non-daily | 1668 (11.8) | 1143 (69.8) | 455 (32.1) | 181 (8.2) | 48 (31.5) |
| Former | 1258 (10.5) | 1034 (78.7) | 394 (35.5) | 67 (5.5) | 13 (27.0) |
| Problematic alcohol use | |||||
| No | 6951 (62.9) | 5451 (76.9) | 2735 (48.9) | 501 (5.7) | 160 (28.8) |
| Yes | 3669 (33.4) | 2599 (71.3) | 1263 (46.2) | 340 (7.2) | 120 (41.0) |
| No answer | 420 (3.7) | 269 (65.1) | 103 (43.3) | 18 (4.3) | 8 (33.3) |
Unweighted frequency of respondents who responded ‘Yes’ to the outcome.
Weighted proportion of respondents who responded ‘Yes’ to the outcome (refused to answer and don't know responses were excluded from the denominator).
Visiting a HP
Most (74.6%) respondents reported visiting a HP in the last 18 months (Table 1).
In all three regression models, compared to respondents with no depression/anxiety, the odds of visiting a HP in the last 18 months were significantly higher for respondents with these mental health conditions (Table 2). In the fully adjusted model (Model 3), the odds of visiting a HP were significantly higher for respondents with depression alone (AOR=2.65; 95% CI: 2.17–3.27, p<0.001), anxiety alone (AOR=2.08; 95% CI: 1.70–2.57, p<0.001), and both depression and anxiety (AOR=3.74; 95% CI: 3.19–4.40, p<0.001), compared to respondents with no depression/anxiety (Table 2).
Table 2.
Logistic regression models to assess the association between mental health condition and healthcare professional interactions regarding smoking cessation and nicotine vaping, cross-sectional ITC 4CV Survey, 2018
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | AOR | 95% CI | p | AOR | 95% CI | p | |
| Visiting a health professional (N=11040) | |||||||||
| No depression/anxiety (Ref.) | 1 | 1 | 1 | ||||||
| Depression only | 2.40 | 1.98–2.93 | <0.001 | 2.62 | 2.15–3.23 | <0.001 | 2.65 | 2.17–3.27 | <0.001 |
| Anxiety only | 2.00 | 1.64–2.44 | <0.001 | 2.08 | 1.70–2.57 | <0.001 | 2.08 | 1.70–2.57 | <0.001 |
| Depression and anxiety | 3.08 | 2.65–3.58 | <0.001 | 3.71 | 3.17–4.36 | <0.001 | 3.74 | 3.19–4.40 | <0.001 |
| Advice to quit smoking from health professional (N =8319) | |||||||||
| No depression/anxiety (Ref.) | 1 | 1 | 1 | ||||||
| Depression only | 1.48 | 1.27–1.74 | <0.001 | 1.58 | 1.34–1.86 | <0.001 | 1.58 | 1.34–1.86 | <0.001 |
| Anxiety only | 0.88 | 0.74–1.05 | 0.152 | 0.95 | 0.80–1.14 | 0.601 | 0.94 | 0.79–1.12 | 0.493 |
| Depression and anxiety | 1.00 | 0.90–1.12 | 0.951 | 1.15 | 1.02–1.30 | 0.022 | 1.14 | 1.01–1.29 | 0.031 |
| Discussion about nicotine va ping products (N=8280) | |||||||||
| No depression/anxiety (Ref.) | 1 | 1 | 1 | ||||||
| Depression only | 1.40 | 1.02–1.88 | 0.032 | 1.44 | 1.04–1.95 | 0.023 | 1.44 | 1.04–1.95 | 0.023 |
| Anxiety only | 1.30 | 0.92–1.81 | 0.126 | 1.45 | 1.01–2.03 | 0.036 | 1.45 | 1.01–2.03 | 0.037 |
| Depression and anxiety | 1.52 | 1.22–1.89 | <0.001 | 1.65 | 1.30–2.09 | <0.001 | 1.63 | 1.29–2.06 | <0.001 |
| Positive recommendation to use nicotine vaping products (N=8 59) | |||||||||
| No depression/anxiety (Ref.) | 1 | 1 | 1 | ||||||
| Depression only | 1.39 | 0.87–2.21 | 0.166 | 1.39 | 0.83–2.30 | 0.204 | 1.36 | 0.81–2.26 | 0.240 |
| Anxiety only | 1.30 | 0.76–2.17 | 0.331 | 1.06 | 0.60–1.86 | 0.831 | 1.02 | 0.57–1.81 | 0.954 |
| Depression and anxiety | 1.18 | 0.83–1.67 | 0.343 | 1.28 | 0.86–1.90 | 0.218 | 1.27 | 0.85–1.89 | 0.240 |
Model 1: unadjusted model with mental health condition as the only independent variable. Model 2: model adjusted for country, sex, age, education level, ethnicity, and income level. Model 3: fully adjusted model adjusted for country, sex, age, education level, ethnicity, income level, cigarette smoking status, and problematic alcohol use. The p-values smaller than our Bonferroni correction adjusted p=0.0125 are indicated in bold. AOR: adjusted odds ratio.
Advice to quit smoking from HP
Among respondents who reported visiting a HP in the last 18 months, less than half (47.9%) reported receiving advice to quit smoking (Table 1).
In all three models, the odds of reporting receiving advice to quit smoking from a HP were significantly higher for respondents with depression alone, compared to respondents with no depression/anxiety (Table 2). In the fully adjusted model, the odds of reporting receiving advice to quit smoking from a HP were 1.58 times higher (95% CI: 1.34–1.86, p<0.001) for respondents with depression alone, compared to respondents with no depression/anxiety (Table 2). There was no significant difference in the odds of receiving advice to quit smoking between respondents with anxiety alone, and those with both depression and anxiety, compared to respondents with no depression/anxiety in any of the three models (Table 2).
Discussion about NVPs
Among respondents who reported visiting a HP in the last 18 months, 6.1% (n=859) reported that their HP discussed NVPs with them (Table 1).
In all three models, there was a statistically significant difference in the odds of reporting a discussion about NVPs between respondents with both depression and anxiety compared to respondents with no depression/anxiety (Table 2). In the fully adjusted model (Model 3), the odds of reporting that their HP discussed NVPs were 1.63 times higher (95% CI: 1.29–2.06, p<0.001) for respondents with both depression and anxiety, compared to respondents with no depression/anxiety (Table 2). There was no significant difference in the odds of reporting HP NVP discussions between respondents with anxiety alone, and those with depression alone, compared to respondents with no depression/anxiety in any of the three models (Table 2).
Positive recommendation to use NVPs
Among respondents who reported visiting a HP in the last 18 months and reported that the HP discussed NVPs with them, one-third (33.5%, n=288) reported receiving a positive recommendation from their HP to use NVPs (Table 1).
We did not find a significant association between mental health condition and the odds of receiving a positive recommendation to use NVPs in any of the three regression models (Table 2); however, sample sizes were small, so findings should be treated with caution.
Country differences
Likelihood-ratio tests indicated a significant difference between the model with and without the mental health condition × country interaction terms for the ‘visiting a HP’ (p=0.002) and ‘receiving advice to quit smoking’ (p=0.009) outcomes. When we examined the individual interaction terms for mental health condition × country for these outcomes, only the depression and anxiety × Canada individual interaction term for ‘visiting a HP’ (p=0.001) was significant at p<0.01 (Supplementary file Tables 2d and 2h). We did not investigate country differences further.
DISCUSSION
Most (74.6%) respondents reported visiting a HP in the last 18 months; the odds were higher for those respondents who reported anxiety and/or depression, compared to those with no depression/anxiety. Less than half of respondents (47.9%) who visited a HP reported receiving advice to quit smoking, with higher odds for those with depression alone. Among respondents who visited a HP, only 6.1% of respondents reported that their HP discussed NVPs with them; those with both depression and anxiety had higher odds. Lastly, among respondents who visited a HP and discussion with HPs included NVPs, one-third of respondents (33.5%) reported receiving a positive recommendation to use them and the odds did not differ by mental health condition (but our sample size was small). We also found that there may be a significant interaction between mental health condition and country regarding visiting a HP and receiving advice to quit smoking.
Our finding concerning HP visits was consistent with past research (which used 2009–2010 UK electronic health record data) which found that people with mental health conditions were more likely to visit HPs than those without28. Regarding cessation advice provision, past research found that the proportion of consultations in which cessation advice was recorded was lower for people with a mental health condition, compared to those without28. In our study, we found that people who had depression alone had higher odds of reporting being given advice to quit smoking from a HP compared to people with no depression/anxiety, with no significant differences for anxiety alone or having both conditions. However, as the number of consultations was not collected in the ITC survey, we could not explore whether this was due to a higher consultation rate among those with depression.
Regarding NVP discussions with HPs, consistent with existing studies which used survey data from Australia, Canada, England, and US from 201615 and 2016–202025, we found that a very low proportion of respondents who visited their HP reported their HP discussing NVPs with them. However, we found some evidence that those with both depression and anxiety had higher odds of their HPs discussing NVPs, compared to respondents with no depression/anxiety. The study investigating this in 201615 found no difference by mental health status; however, they analyzed no anxiety versus anxiety and no depression versus depression. It may be that people who smoke who have both depression and anxiety were more likely to ask their doctor about NVPs or they may experience greater difficulty in quitting which may prompt their HP to mention NVPs as an alternative method to obtain nicotine. Further research is needed to substantiate this finding.
Lastly, unlike previous research – which found, using a previous wave (2016) of this survey, that people who smoke with anxiety were less likely to be recommended by their HP to use an NVP, compared to people who smoke without anxiety15 – we did not find an association between mental health condition and receiving a positive recommendation from a HP to use NVPs. Perhaps between 2016 and 2018, HPs increased the rate of recommendation of NVPs to their patients who have anxiety, so it was in line with their recommendation rate to patients who smoke without mental health conditions.
The consistency between older studies14,15 and our finding (using 2018 data) that less than half of all respondents received advice to quit smoking is notable because it indicates a lack of improvement in cessation advice provision in healthcare settings. It is promising that respondents with depression had a higher rate of receiving cessation advice (albeit only 57.2%), than respondents with no depression or anxiety, but this may be due to having a higher number of consultations in the last 18 months, as opposed to having a higher cessation intervention per visit rate28. Additionally, although those with anxiety either alone or with depression were also more likely to visit a HP, they were not more likely to receive cessation advice from their doctor (compared to those with no depression/anxiety), suggesting lower overall rates of intervention per visit among these groups. We advise that HPs increase the rate that they provide cessation advice and support to all their patients who smoke; this is particularly important for those who have mental health conditions to close the inequality gap of differential smoking rates2-5. Our finding that people who smoke with mental health conditions had higher odds of visiting a HP suggests that there are more opportunities for HPs to deliver cessation advice.
Our findings that only 6.1% of respondents who visited their HP reported their HP discussing NVPs with them, and only 2% received a positive recommendation to use them, are concerning given that NVPs have been found by Cochrane systematic reviews to be an effective quit method17. Furthermore, there was no association between receiving a positive recommendation by a HP to use NVPs and having anxiety or depression. It is especially important for people with anxiety/depression to be given accurate information about and access to NVPs, as various studies using surveys (e.g. 1993–2014 data from Great Britain)4 have found that people with mental health conditions are more likely to smoke heavily and be highly dependent on cigarettes, and are motivated to quit smoking (e.g. 2016–2017 data from England)5, but are less likely to succeed (e.g. 2016–2017 data from England5,35, 2016 data from Australia, Canada, England, and the US36).
To summarize, the main implications of this study are that there are missed opportunities for HPs to deliver cessation advice and to discuss NVPs in an evidence-based way with people who smoke with anxiety and/or depression. Given the higher smoking rates among people with mental health conditions2-5, to reduce the resultant health inequalities, HPs should increase the rate that they provide cessation advice and support per visit among people with mental health conditions. Also, although HPs should always consider the potential risks and benefits of recommending certain treatments, given that evidence suggests that using NVPs is substantially less harmful than smoking combustible tobacco16 and that NVPs have been shown to be a more efficacious smoking cessation aid than NRT17, HPs should at least discuss NVPs with their patients who smoke (with and without mental health conditions) when advising them about cessation options. This is particularly important given that currently effective licensed medications for smoking cessation (varenicline and bupropion) have been limited since 2021 and 2022.
Future research
Future research could explore reasons behind why HPs provide differing care regarding smoking cessation to people with mental health conditions, and investigate if other forms of cessation support that HPs recommend to people who smoke (such as licensed cessation aids) differ by mental health status. Also, the effect of other mental health conditions should be investigated. To further investigate country effects, we recommend stratification by country, but a larger sample size will be required.
Strengths and limitations
The strength of our cross-sectional study is that it used data from large population-based samples of people who smoke from four countries. However, there are some limitations. The study relies on self-reported measures which were not verified with health records, or other external measures, and may be subject to recall and other biases. It is not possible to know when a respondent was first diagnosed with depression and/or anxiety and the question used was not intended as a diagnostic tool. The sample size for some of our analyses was small.
CONCLUSIONS
Using cross-sectional 2018 ITC Four Country (Australia, Canada, England, US) Survey data, this study found that people with anxiety and/or depression who smoke were more likely to visit a HP, but only people with depression alone were more likely to receive cessation advice, and only people with both depression and anxiety were more likely to discuss NVPs with their HP. Receiving a positive recommendation to use NVPs did not differ by mental health condition and few respondents received positive recommendations overall. More people who smoke should be given smoking cessation advice and information about effective smoking cessation support (including NVPs) to increase the likelihood of smoking cessation.
Supplementary Material
CONFLICTS OF INTEREST
The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none was reported.
FUNDING
The ITC Four Country Smoking and Vaping Survey was supported by grants from the US National Cancer Institute (P01 CA200512), the Canadian Institutes of Health Research (FDN-148477), and the National Health and Medical Research Council of Australia (APP1106451). This work was conducted as a part of BET’s PhD (Economic and Social Research Council London Interdisciplinary Social Science Doctoral Training Partnership 1 + 3 award, es/p000703/1). This work was supported by the UK Prevention Research Partnership (MR/S037519/1), which is funded by the British Heart Foundation, Cancer Research UK, Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Health and Social Care Research and Development Division (Welsh Government), Medical Research Council, National Institute for Health Research, Natural Environment Research Council, Public Health Agency (Northern Ireland), The Health Foundation and Wellcome. The funders had no role in the design of the study, or the collection, analysis, and interpretation of data, or in writing of the manuscript. AM is a National Institute for Health and Care Research (NIHR) Senior Investigator (2019-2023). The views expressed in this article are those of the authors and not necessarily those of the NIHR, or the Department of Health and Social Care. KE is the recipient of Fellowship funding from the Society for Fellowship funding from the Society for the Study of Addiction and is also partly supported by a P01 Grant (1P01CA200512) from the US National Institutes of Health (NIH). GTF is supported by a Senior Investigator Grant from the Ontario Institute for Cancer Research (IA-004). CWLL is also supported by a National Health Medical Research Council (NHMRC) of Australia Postgraduate Scholarship [APP2005317], The University of Queensland Living Stipend and Tuition Scholarship and a National Centre for Youth Substance Use Research (NCYSUR) top-up scholarship. GCKC is supported by a NHMRC Investigator Fellowship [APP1176137].
ETHICAL APPROVAL
The survey protocols and all materials of the Wave 2 (2018) ITC 4CV Survey, including the survey questionnaires, were cleared for ethics by Office of Research Ethics, University of Waterloo, Canada (REB#20803/30570, REB#21609/30878); Research Ethics Office, King’s College London, UK (RESCM-17/18-2240); Human Research Ethics, Cancer Council Victoria, Australia (HREC1603) and, Human Ethics, Research Management Office, University of Queensland, Australia (2016000330/HREC1603); and Institutional Review Board Medical University of South Carolina (waived due to minimal risk). All participants had provided informed consent.
DATA AVAILABILITY STATEMENT
In each country participating in the international Tobacco Control Policy Evaluation (ITC) Project, the data are jointly owned by the lead researcher(s) in that country and the ITC Project at the University of Waterloo. Data from the ITC Project are available to approved researchers 2 years after the date of issuance of cleaned data sets by the ITC Data Management Centre. Researchers interested in using ITC data are required to apply for approval by submitting an International Tobacco Control Data Repository (ITCDR) request application and subsequently to sign an ITCDR Data Usage Agreement. The criteria for data usage approval and the contents of the Data Usage Agreement are described online (http://www.itcproject.org).
PROVENANCE AND PEER REVIEW
Not commissioned; externally peer reviewed.
REFERENCES
- 1.Tobacco Factsheet. World Health Organization; Published May 24, 2022. Accessed February 23, 2022. https://www.who.int/news-room/fact-sheets/detail/tobacco. [Google Scholar]
- 2.Smoking and mental health. Royal College of Physicians and Royal College of Psychiatrists; Published March 28, 2013. Accessed September 27, 2022. https://www.rcplondon.ac.uk/projects/outputs/smoking-and-mental-health. [Google Scholar]
- 3.Fluharty M, Taylor AE, Grabski M, Munafò MR. The Association of Cigarette Smoking With Depression and Anxiety: A Systematic Review. Nicotine Tob Res. 2017;19(1):3–13. doi: 10.1093/NTR/NTW140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson S, McNeill A, Brose LS. Smoking and quitting behaviours by mental health conditions in Great Britain (1993-2014) Addict Behav. 2019;90:14–9. doi: 10.1016/j.addbeh.2018.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brose LS, Brown J, Robson D, McNeill A. Mental health, smoking, harm reduction and quit attempts – a population survey in England. BMC Public Health. 2020;20(1):1237. doi: 10.1186/S12889-020-09308-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute on Drug Abuse Do people with mental illness and substance use disorders use tobacco more often? Accessed March 7, 2023. https://nida.nih.gov/publications/research-reports/tobacco-nicotine-e-cigarettes/do-people-mental-illness-substance-use-disorders-use-tobacco-more-often.
- 7.Chesney E, Robson D, Patel R, et al. The impact of cigarette smoking on life expectancy in schizophrenia, schizoaffective disorder and bipolar affective disorder: An electronic case register cohort study. Schizophr Res. 2021;238:29–35. doi: 10.1016/J.SCHRES.2021.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tam J, Warner KE, Meza R. Smoking and the Reduced Life Expectancy of Individuals With Serious Mental Illness. Am J Prev Med. 2016;51(6):958–966. doi: 10.1016/J.AMEPRE.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Taylor GM, Lindson N, Farley A, et al. Smoking cessation for improving mental health. Cochrane Database of Syst Rev. 2021;3(3):CD013522. doi: 10.1002/14651858.CD013522.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting Smoking Among Adults — United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–1464. doi: 10.15585/mmwr.mm6552a1. [DOI] [PubMed] [Google Scholar]
- 11.Rigotti NA, Kruse GR, Livingstone-Banks J, Hartmann-Boyce J. Treatment of Tobacco Smoking: A Review. JAMA. 2022;327(6):566–577. doi: 10.1001/JAMA.2022.0395. [DOI] [PubMed] [Google Scholar]
- 12.Brown J, Raupach T, West R. GPs have key role in helping patients to stop smoking. Practitioner. 2012;256(1751):23–25. doi. [PubMed] [Google Scholar]
- 13.West R, Papadakis S. Stop smoking services: increased chances of quitting. NCSCT; Accessed June 12, 2023. https://www.ncsct.co.uk/usr/pub/Stop%20smoking%20services%20effectiveness.pdf. [Google Scholar]
- 14.Bartsch AL, Härter M, Niedrich J, Brütt AL, Buchholz A. A Systematic Literature Review of Self-Reported Smoking Cessation Counseling by Primary Care Physicians. PLoS One. 2016;11(12):e0168482. doi: 10.1371/journal.pone.0168482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gravely S, Thrasher JF, Cummings KM, et al. Discussions between health professionals and smokers about nicotine vaping products: results from the 2016 ITC Four Country Smoking and Vaping Survey. Addiction. 2019;1(1):71–85. doi: 10.1111/add.14527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McNeill A, Simonavicius E, Brose L, et al. Nicotine vaping in England: an evidence update including health risks and perceptions, 2022. GOVUK; Accessed March 14, 2023. https://www.gov.uk/government/publications/nicotine-vaping-in-england-2022-evidence-update. [Google Scholar]
- 17.Hartmann-Boyce J, Lindson N, Butler AR, et al. Electronic cigarettes for smoking cessation. Cochrane Database of Syst Rev. 2022;11(11):CD010216. doi: 10.1002/14651858.CD010216.pub7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warner KE, Benowitz NL, McNeill A, Rigotti NA. Nicotine e-cigarettes as a tool for smoking cessation. Nat Med. 2023;29(3):520–524. doi: 10.1038/s41591-022-02201-7. [DOI] [PubMed] [Google Scholar]
- 19.Balfour DJK, Benowitz NL, Colby SM, et al. Balancing Consideration of the Risks and Benefits of E-Cigarettes. Am J Public Health. 2021;111(9):1661–1672. doi: 10.2105/AJPH.2021.306416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tobacco: preventing uptake, promoting quitting and treating dependence. National Institute for Health and Care Excellence; Publishes November 30, 2021. Accessed February 23, 2022. https://www.nice.org.uk/guidance/ng209. [PubMed] [Google Scholar]
- 21.Pharmacotherapy for smoking cessation. Royal Australian College of General Practitioners; Αccessed March 28, 2022. https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/supporting-smoking-cessation/pharmacotherapy-for-smoking-cessation. [Google Scholar]
- 22.Quitting smoking: How to quit. Government of Canada; Accessed January, 2023. https://www.canada.ca/en/health-canada/services/smoking-tobacco/quit-smoking/how.html. [Google Scholar]
- 23.E-Cigarettes, Vapes, and other Electronic Nicotine Delivery Systems (ENDS) US Food and Drug Administration; Accessed January 27, 2023. https://www.fda.gov/tobacco-products/products-ingredients-components/e-cigarettes-vapes-and-other-electronic-nicotine-delivery-systems-ends. [Google Scholar]
- 24.Tobacco Smoking Cessation in Adults, Including Pregnant Persons: Interventions. United States Preventive Services Task Force; 2021. Published Janyuary 19, 2021. Accessed March 28, 2023. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions. [DOI] [PubMed] [Google Scholar]
- 25.Cho YJ, Thrasher JF, Gravely S, et al. Adult smokers’ discussions about vaping with health professionals and subsequent behavior change: a cohort study. Addiction. 2022;117(11):2933–2942. doi: 10.1111/add.15994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jarvis MJ, Wardle J. Social patterning of individual health behaviours: The case of cigarette smoking. In: Marmot M, Wilkinson RG, editors. Social Determinants of Health. 2nd ed. Oxford University Press; 2005. pp. 224–237. [DOI] [Google Scholar]
- 27.King BA. Bringing Health Equity to the Forefront of Tobacco Product Regulation. HPHR Journal Published. 2022:61. doi: 10.54111/0001/III2. [DOI] [Google Scholar]
- 28.Szatkowski L, McNeill A. The delivery of smoking cessation interventions to primary care patients with mental health problems. Addiction. 2013;108(8):1487–1494. doi: 10.1111/add.12163. [DOI] [PubMed] [Google Scholar]
- 29.GBD 2019 Mental Disorders Collaborators Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–150. doi: 10.1016/S2215-0366(21)00395-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharma R, Gartner CE, Hall WD. The challenge of reducing smoking in people with serious mental illness. Lancet Respir Med. 2016;4(10):835–844. doi: 10.1016/S2213-2600(16)30228-4. [DOI] [PubMed] [Google Scholar]
- 31.ITC Four Country Smoking and Vaping Survey Wave 2 (4CV2) ITC; 2020. Accessed September 27, 2022. https://itcproject.s3.amazonaws.com/uploads/documents/4CV2_Technical_Report_15Jan202.pdf. [Google Scholar]
- 32.Li L, Borland R, O’Connor RJ, et al. The association between smokers’ self-reported health problems and quitting: Findings from the ITC Four Country Smoking and Vaping Wave 1 Survey. Tob Prev Cessat. 2019;5:49. doi: 10.18332/tpc/114085. Published 2019 Dec 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31(7):1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- 34.Field A, Miles J, Field Z. Logistic regression. In: Field A, Miles J, Field Z, editors. Discovering Statistics Using R. SAGE Publications; 2012. [Google Scholar]
- 35.Brose LS, Brown J, McNeill A. Mental health and smoking cessation-a population survey in England. BMC Med. 2020;18(1):161. doi: 10.1186/s12916-020-01617-7. Published 2020 Jun 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li L, Borland R, Cummings KM, et al. Are health conditions and concerns about health effects of smoking predictive of quitting? Findings from the ITC 4CV Survey (2016-2018) Tob Prev Cessat. 2020;6:60. doi: 10.18332/tpc/127471. Published 2020 Oct 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
In each country participating in the international Tobacco Control Policy Evaluation (ITC) Project, the data are jointly owned by the lead researcher(s) in that country and the ITC Project at the University of Waterloo. Data from the ITC Project are available to approved researchers 2 years after the date of issuance of cleaned data sets by the ITC Data Management Centre. Researchers interested in using ITC data are required to apply for approval by submitting an International Tobacco Control Data Repository (ITCDR) request application and subsequently to sign an ITCDR Data Usage Agreement. The criteria for data usage approval and the contents of the Data Usage Agreement are described online (http://www.itcproject.org).