Abstract
Background:
Multiple-revision anterior cruciate ligament reconstruction (ACLR) presents several technical challenges, often due to residual hardware, tunnel widening, malposition, or staged surgeries.
Purpose:
To compare failure and complication rates between the over-the-top (OTT) and transportal drilling (TD) techniques in patients undergoing surgery for failed revision ACLR.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
The medical records of patients with at least 2 revision ACLRs using either the OTT or TD technique were reviewed retrospectively. Data on patient demographics, graft characteristics, number of revisions, concomitant procedures, complications, and failures were collected. Between-group comparisons of continuous and categorical variables were conducted with the independent-samples t test and the Fisher exact or chi-square test, respectively.
Results:
A total of 101 patients undergoing multiple-revision ACLR with OTT (n = 37, 37%) and TD (n = 64, 63%) techniques were included for analysis. The mean follow-up time was 60 months (range, 12-196 months). There were no significant differences in age, sex, body mass index, laterality, or follow-up length between groups (P > .05). Allograft was the graft used most frequently (n = 64; 67.3%) with no significant differences between groups in graft diameter (P > .05). There were no statistically significant differences between groups regarding rate of concurrent medial and lateral meniscus, cartilage, or lateral extra-articular procedures (P > .05). There was also no significant66 between-group difference in complication rate (OTT: n = 2 [5.4%]; TD: n = 8 [13%]) or graft failure rate (OTT: n = 4 [11%]; TD: n = 14 [22%]) (P > .05 for both).
Conclusion:
The results of this study showed notably high failure and complication rates in challenging multiple-revision ACLR. Complication and failure rates were similar between techniques, demonstrating that the OTT technique is a valuable alternative that can be used in a revision ACLR, particularly as a single-stage approach when the single-stage TD technique is not possible.
Keywords: ACLR, graft failure, multiple-revision, OTT, over-the-top-technique, revision
Graft failure after anterior cruciate ligament (ACL) reconstruction (ACLR) is a devastating outcome for patients, manifesting as impaired function or a career-ending event. Recurrent instability also results in downstream consequences, including further damage to structures essential for knee stability, as well as accelerated progression of osteoarthritis. 19 Multiple factors are responsible for the incidence of graft failure after ACLR. 2,13 Tunnel malposition of the femoral tunnel has been shown to be the cause of more than 80% of graft failures after ACLR. 14
Revision ACLR is important for restoring knee stability and function in patients with graft failure. Studies evaluating causes of poor patient outcomes have identified multiple factors: arthrofibrosis, allograft use, increased posterior tibial slope, misplaced grafts, and meniscal or cartilage injury. 5,22,26 While revision ACLR has a 3- to 4-fold greater graft failure rate compared with primary ACLR, multiple-revision ACLR has a 26-fold increased failure rate compared with first-revision ACLR. 23,24 Given the technical difficulties associated with revision ACLR and the high rate of failure in the setting of multiple-revision ACLR, there exist only a few studies investigating outcomes between different technical approaches to multiple-revision ACLR. 3,8,20
The over-the-top (OTT) technique avoids the previous femoral tunnel and confers no risk of tunnel malposition by placing the graft over the superomedial border of the lateral femoral condyle and fixing it to extra-articular bone. 15,16 Biomechanically, OTT has demonstrated equivalent restoration of anterior-posterior and rotatory knee stability as compared with anatomic ACLR with the transportal drilling (TD) technique. 1,12,15 While clinical studies show improvements in functional outcomes and stability after ACLR with the OTT technique, conclusions from these investigations are limited by short-term follow-up, focus on skeletally immature patients, and the lack of assessment of multiple-revision ACLR. 7,11,15,16
The objective of this study was to evaluate failure and complication rates in patients undergoing multiple-revision ACLR with the OTT technique compared with the TD technique. We hypothesized that the OTT technique would yield similar graft survival and complication rates as compared with the TD technique at long-term follow-up.
Methods
The protocol for this study was granted institutional review board approval. Eligible were patients who had been treated with multiple-revision ACLR surgery using either the OTT or TD technique as performed by 4 sports-medicine-trained, high-volume ACL surgeons at a multicenter single institution between January 1, 2000, and January 1, 2020. Multiple-revision surgery was defined as 2 or more revision ACLRs for a specific patient who undergone at least 1 previous revision ACLR surgery in the same extremity. Patients with hybrid fixation (involving both OTT and TD techniques), transtibial technique, and less than 1-year follow-up were excluded from further analysis. A total of 101 patients, 64 who underwent TD and 37 who underwent OTT, were included in this analysis (Figure 1).
Figure 1.
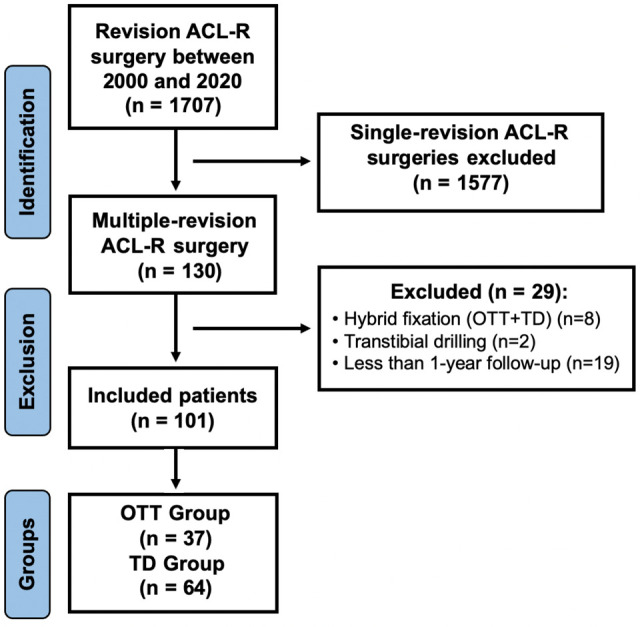
STROBE flowchart. ACLR, anterior cruciate ligament reconstruction; OTT, over-the-top; STROBE, strengthening the reporting of observational studies in epidemiology; TD, transportal drilling.
A retrospective review of patient records was conducted to identify and dichotomize patients treated with multiple-revision ACLR into 2 groups, according to whether the OTT or the TD technique was performed. The surgical technique was determined by surgeon preference and performed as described in previous studies. 15,28 Revision ACLR surgery of patients whom previous bone tunnels were not expanded and anatomically located previous bone tunnel were not expanded and anatomically located, was performed with a single-stage TD technique. Revision ACLR surgery was performed via OTT technique in patients who needed staged surgery because of previous femoral bone tunnel malposition and/or enlargement to avoid staged surgery.
Demographic data including age, sex, body mass index, date of surgery (most recent revision), date of final clinical visit, follow-up length (months), and injury laterality were extracted from the electronic medical record. Queried surgical variables included the number of revision surgeries, number of surgical stages (1 or 2), graft choice, graft diameter, medial and lateral meniscus procedure, cartilage procedure, lateral extra-articular procedure, reoperation, complications, and revision ACLR failure rate.
The primary outcome measure was the rate of ACLR failure. Failure of the ACL graft was confirmed with magnetic resonance imaging after the treating surgeons’ diagnosis. Reoperations due to hardware failure, meniscectomy, meniscus allograft transplantation, total knee arthroplasty, and complications (arthrofibrosis, cyclops lesion, septic arthritis) were also collected.
Statistical Analysis
Statistical analyses were performed using SAS Version 9.4 (SAS Institute). Descriptive statistics of categorical variables included counts and corresponding percentages. Continuous variables were presented as means and standard deviations. The Levene test was applied to assess for equality of variances. Between-group comparison of categorical variables was performed using the Fisher exact or chi-square test. Continuous variables were compared between groups with the independent-sample t test. The level of significance was set at P < .05.
Results
The baseline characteristics of the DT group (mean age at surgery, 28.6 years; range, 18-44 years) and OTT cohorts (mean age at surgery, 27.5 years; range, 16-49 years) are displayed in Table 1. There were no significant differences between the groups in baseline data. While 25 (39%) of the patients in the TD group underwent staged surgery, 39 (61%) of the patients underwent single-stage surgery. The TD cohort comprised 61 (95%) patients undergoing a second-revision ACLR and 3 (5%) undergoing a third-revision ACLR, while the OTT cohort had 34 (92%) patients undergoing a second-revision ACLR, 2 (5%) undergoing a third-revision ACLR, and 1 (3%) undergoing a fourth-revision ACLR. The graft used most frequently was allograft (67.3%) throughout the study population. Within the OTT cohort, allograft was used for 30 (81%) of cases and hamstring tendon autograft was used in the remaining 7 (19%) of cases, while the TD cohort received 4 (6%) hamstring tendon autograft, 11 (17%) all soft tissue quadriceps tendon autograft, 4 (6%) quadriceps tendon autograft with bone block, 7 (11%) bone-patellar tendon-bone autograft, and 38 (59%) allografts.
Table 1.
Baseline Characteristics of the Study Cohort (N = 101) a
| Variable | OTT (n = 37) | TD (n = 64) | P |
|---|---|---|---|
| Age, y, mean (range) | 27.5 (16-49) | 28.6 (18-44) | .54 |
| Male sex | 22 (59%) | 33 (52%) | .44 |
| BMI, kg/m2 | 26.5 ± 4.4 | 26.8 ± 5.4 | .81 |
| Right side affected | 14 (38) | 28 (44) | .56 |
| Follow-up length, mo | 50.21 ± 9.8 | 43.10 ± 6.2 | .49 |
| Revision number | .59 | ||
| Second | 34 (92) | 61 (95) | |
| Third | 2 (5) | 3 (5) | |
| Fourth | 1 (3) | 0 (0) |
a Data are reported as mean ± SD or n (%) unless otherwise indicated. BMI, body mass index; OTT, over-the-top; TD, transportal drilling.
Regarding intraoperative data, the TD and OTT cohorts had mean graft diameters of 9.6 ± 1.0 mm and 9.8 ± 1.1 mm, respectively (P > .05). The rate of medial meniscal procedures for the TD and OTT cohorts were 50.0% and 35.1%, respectively (P > .05). Similarly, the rate of lateral meniscus procedure for the TD and OTT cohorts was 15% and 18%, respectively (P > .05). The rate of cartilage procedures for TD and OTT cohorts were 5% and 0.0%, respectively (P > .05). Lateral extra-articular procedure was performed in 16% and 5% of the TD and OTT cohorts, respectively (P > .05). Intraoperative data are displayed in Table 2.
Table 2.
Intraoperative Data a
| Variable | OTT (n = 37) | TD (n = 64) | P |
|---|---|---|---|
| Graft diameter, mm | 9.8 ± 1.1 | 9.6 ± 1 | .51 |
| Specific graft | NA | ||
| HT autograft | 7 (19%) | 4 (6%) | |
| sQT autograft | 0 (0%) | 11 (17%) | |
| bQT autograft | 0 (0%) | 4 (6%) | |
| BPTB autograft | 0 (0%) | 7 (11%) | |
| Allograft | 30 (81%) | 38 (59%) | |
| Medial meniscal procedure | 13 (35%) | 32 (50%) | .15 |
| Medial meniscectomy | 5 (13%) | 10 (15%) | |
| Medial meniscal repair | 1 (2%) | 8 (12%) | |
| MAT | 7 (18%) | 14 (21%) | |
| Lateral meniscal procedure | 7 (18%) | 10 (15%) | .67 |
| Lateral meniscectomy | 5 (13%) | 3 (5%) | |
| Lateral meniscal repair | 1 (2%) | 3 (5%) | |
| Lateral meniscal posterior root repair | 1 (2%) | 4 (6%) | |
| Cartilage procedure | 0 (0%) | 3 (5%) | .3 |
| LEP | 3 (5%) | 6 (16%) | .07 |
a Data are reported as mean ± SD or n (%). BPTB, bone-patellar tendon-bone; bQT, quadriceps tendon autograft with bone block; HT, Hamstring tendon; LEP, lateral extra-articular procedures; MAT, meniscal allograft transplantation; N/A, not available; OTT, over-the-top; sQT, all soft tissue quadriceps tendon; TD, transportal drilling.
Analysis of postoperative failure, complication, and reoperation rates are displayed in Table 3. The failure rates for the TD and OTT cohorts were 22% and 11%, respectively (P = .16). No difference was observed in complication rates, with the TD and OTT cohorts experiencing complications in 13% and 5.4% of cases, respectively (P = .74). More specifically, there was 1 (2.7%) case of arthrofibrosis and 1 (2.7%) case of cyclops lesion within the OTT cohort. Within the TD cohort, there were 5 (7.8%) cases of arthrofibrosis, 2 (3.1%) cases of septic arthritis, and 1 (1.5%) case of cyclops lesion. No difference was observed in reoperation rates with the TD and OTT cohorts undergoing consequent surgeries (28.1% and 13.5%, respectively; P > .05) (Table 4).
Table 3.
Postoperative Outcomes a
| Variable | OTT (n = 37) | TD (n = 64) | P |
|---|---|---|---|
| Reoperation | 5 (13.5%) | 18 (28.1%) | .52 |
| Complication | 2 (5.4%) | 8 (13%) | .74 |
| Arthrofibrosis | 1 (2.7%) | 5 (7.8%) | |
| Septic arthritis | 0 (0.0%) | 2 (3.1%) | |
| Cyclops lesion | 1 (2.7%) | 1 (1.5%) | |
| Graft failure | 4 (11%) | 14 (22%) | .16 |
a Data are reported as n (%). OTT, over-the-top; TD, transportal drilling.
Table 4.
Specific Reoperation Procedures Performed a
| Reoperation Procedure | OTT (n = 37) | TD (n = 64) |
|---|---|---|
| Hardware removal | 0 (0%) | 5 (7.8%) |
| Arthrolysis | 1 (2.7%) | 5 (7.8%) |
| Cyclops lesion excision | 1 (2.7%) | 0 (0%) |
| Meniscectomy | 2 (5.4%) | 3 (4.6%) |
| Medial meniscal transplantation | 0 (0%) | 1 (1.5%) |
| Lateral meniscal transplantation | 0 (0%) | 1 (1.5%) |
| Irrigation and debridement | 0 (0%) | 2 (3.1%) |
| Total knee arthroplasty | 1 (2.7%) | 1 (1.5%) |
a Data are reported as n (%). OTT, over-the-top; TD, transportal drilling.
Discussion
The key finding of this study was the notably high failure and complication rate after multiple-revision ACLR. Similar complication (8% vs 13%, respectively) and failure rates (11% vs 22%, respectively) were observed in the OTT compared with the TD group as the between-group difference was not statistically significant for either of these outcomes (P > .05). Previous studies reported a 13.3% to 20% failure rate in patients treated with multiple-revision ACLR. 3,6,8 A recent retrospective study identified that the most common complication after these surgeries was arthrofibrosis. 6 Our study similarly identified the most common complication to be arthrofibrosis (5.9%), and failure was detected in 18 (17.8%) patients after multiple-revision ACLR. The Multicenter ACL Revision Study (MARS) group found 53% of ACLR failures to be due to technical errors, and 80% of these technical errors to be caused by femoral tunnel malplacement. 26 In another study from the MARS group, 78% of patients treated with multiple-revision ACLR required a new femoral tunnel, and 22% of these patients required 2-stage revision surgery. 4 However, satisfactory postoperative results were reported with the OTT technique in revision ACLR, where an anatomic femoral tunnel cannot be created in a single stage. 3,15,16 While a 14% failure rate was reported after revision ACLR using the OTT technique combined with lateral extra-articular procedure, it was shown that satisfactory knee stability can be achieved after revision ACLR performed with the same technique. 3,27 Usman et al 18 compared the OTT technique without lateral extra-articular procedure with the anatomic TD technique for revision ACLR and found no difference in functional outcomes nor knee laxity between groups at 1-year follow-up. In our study, we similarly compared the OTT and TD groups, which were homogeneous in terms of demographics, follow-up times, body mass index, concomitant surgery, graft type, and thickness, and found the rates of lateral extra-articular procedures to be 16% and 5% for the OTT and TD groups, respectively (P > .05). Satisfactory rates of failure and complication rates were observed with the OTT technique. In addition, there was no statistical difference between the OTT and TD groups in terms of postoperative failure or complication rate. Although not statistically significant, a 22% failure rate in the TD group compared with an 11% failure rate in the OTT group, may be clinically significant.
While the risk of reoperation after revision ACLR is reported to be over 20%, meniscal pathologies are the most common causes of reoperation at a reported rate of 12%. 10,17,21 Existing literature provides a possible explanation, as meniscus repair failure after primary ACLR has been reported at 4%, as compared with 10% after revision ACLR. 25 In our study, the reoperation rate due to meniscal pathologies was found to be 6.9%. Arthrofibrosis is another common cause of reoperation after revision ACLR surgery and has been reported at a rate of 4% to 5% after primary and revision surgeries. 9,10 Similarly, the rate of reoperation of arthrolysis was found to be 5.9% in our study.
Limitations
This study has several limitations. First, preoperative and postoperative patient-reported outcomes were not available for all patients given the retrospective study design. Second, additional clinical outcomes including patient-reported outcome measures and activity level were not included. Third, the surgical technique used for each patient was not randomized but decided by the surgeon. All surgeons used both techniques during revision ACLR, and no surgeon exclusively used 1 technique, reducing but not eliminating the risk of selection bias. Fourth, the sample size was limited by the relative rarity of multiple-revision ACLR surgery. Last, it is possible that some patients sought care outside of our health care system for revision surgery, preventing our ability to capture this data.
Conclusion
The current study identified satisfactory results in terms of failure and complication rates after multiple-revision ACLR performed with the OTT technique. Complication and failure rates were similar between techniques, demonstrating that the OTT technique is a valuable alternative that can be used in a revision ACLR.
Acknowledgment
In memoriam and appreciation of Dr Freddie H. Fu (1950-2021).
Footnotes
Final revision submitted March 6, 2023; accepted April 14, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: E.A.O. was awarded a grant by ESSKA-University of Pittsburgh Sports Medicine Clinical and Research Fellowship, and The Scientific and Technological Research Council of Turkey (TUBITAK) outside the submitted work. B.P.L. has received education payments from Mid-Atlantic Surgical and royalties from Wolters Kluwer Health-Lippincott Williams & Wilkins. V.M. has received consulting fees from Smith & Nephew, nonconsulting fees from Arthrex, and royalties from Springer. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Pittsburgh (ref No. STUDY20050226).
References
- 1. Asai S, Maeyama A, Hoshino Y, et al. A comparison of dynamic rotational knee instability between anatomic single-bundle and over-the-top anterior cruciate ligament reconstruction using triaxial accelerometry. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):972–978. [DOI] [PubMed] [Google Scholar]
References
- 2. Benedetto Di P, Benedetto Di E, Fiocchi A, Beltrame A, Causero A. Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res. 2016;28(4):319–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Buda R, Ruffilli A, di Caprio F, et al. Allograft salvage procedure in multiple-revision anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(2):402–410. [DOI] [PubMed] [Google Scholar]
References
- 4. Chen JL, Allen CR, Stephens TE, et al. Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med. 2013;41(7):1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Engler ID, Salzler MJ, Wall AJ, et al. Patient-reported outcomes after multiple-revision ACL reconstruction: good but not great. Arthrosc Sports Med Rehabil. 2020;2(5):e539–e546. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 6. Grassi A, Kim C, Marcheggiani Muccioli GM, Zaffagnini S, Amendola A. What is the mid-term failure rate of revision ACL reconstruction? A systematic review. Clin Orthop Relat Res. 2017;475(10):2484–2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 7. Grassi A, Pizza N, Macchiarola L, et al. Over-the-top anterior cruciate ligament (ACL) reconstruction plus lateral plasty with hamstrings in high-school athletes: results at 10 years. Knee. 2021;33:226–233. [DOI] [PubMed] [Google Scholar]
References
- 8. Griffith TB, Allen BJ, Levy BA, Stuart MJ, Dahm DL. Outcomes of repeat revision anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(6):1296–1301. [DOI] [PubMed] [Google Scholar]
- 9. Huleatt J, Gottschalk M, Fraser K, et al. Risk factors for manipulation under anesthesia and/or lysis of adhesions after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2018;6(9):2325967118794490. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 10. Hunnicutt JL, Haynes WB, Slone HS, Prince JA, Boden SA, Xerogeanes JW. Revision anterior cruciate ligament reconstruction with the all-soft tissue quadriceps tendon autograft has acceptable early and intermediate-term outcomes. Arthroscopy. 2021;37(9):2848–2857. [DOI] [PubMed] [Google Scholar]
References
- 11. Lanzetti RM, Pace V, Ciompi A, et al. Over the top anterior cruciate ligament reconstruction in patients with open physes: a long-term follow-up study. Int Orthop. 2020;44(4):771–778. [DOI] [PubMed] [Google Scholar]
References
- 12. Lertwanich P, Kato Y, Martins CAQ, et al. A biomechanical comparison of 2 femoral fixation techniques for anterior cruciate ligament reconstruction in skeletally immature patients: over-the-top fixation versus transphyseal technique. Arthroscopy. 2011;27(5):672–680. [DOI] [PubMed] [Google Scholar]
- 13. Ménétrey J, Duthon VB, Laumonier T, Fritschy D. “Biological failure” of the anterior cruciate ligament graft. Knee Surg Sports Traumatol Arthrosc. 2008;16(3):224–231. [DOI] [PubMed] [Google Scholar]
References
- 14. Morgan JA, Dahm D, Levy B, et al. Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg. 2012;25(5):361–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 15. Nagai K, Rothrauff BB, Li RT, Fu FH. Over-the-top ACL reconstruction restores anterior and rotatory knee laxity in skeletally immature individuals and revision settings. J Knee Surg. 2012;25(5):361–368. [DOI] [PubMed] [Google Scholar]
- 16. Sarraj M, de Sa D, Shanmugaraj A, Musahl V, Lesniak BP. Over-the-top ACL reconstruction yields comparable outcomes to traditional ACL reconstruction in primary and revision settings: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):427–444. [DOI] [PubMed] [Google Scholar]
References
- 17. Sullivan JP, Huston LJ, Zajichek A, et al. Incidence and predictors of subsequent surgery after anterior cruciate ligament reconstruction: a 6-year follow-up study. Am J Sports Med. 2020;48(10):2418–2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 18. Usman MA, Kamei G, Adachi N, Deie M, Nakamae A, Ochi M. Revision single-bundle anterior cruciate ligament reconstruction with over-the-top route procedure. Orthop Traumatol Surg Res. 2015;101(1):71–75. [DOI] [PubMed] [Google Scholar]
References
- 19. Visnes H, Gifstad T, Persson A, et al. ACL reconstruction patients have increased risk of knee arthroplasty at 15 years of follow-up: data from the Norwegian Knee Ligament Register and the Norwegian Arthroplasty Register from 2004 to 2020. JB JS Open Access. 2022;7(2):e22.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 20. Wegrzyn J, Chouteau J, Philippot R, Fessy MH, Moyen B. Repeat revision of anterior cruciate ligament reconstruction: a retrospective review of management and outcome of 10 patients with an average 3-year follow-up. Am J Sports Med. 2009;37(4):776–785. [DOI] [PubMed] [Google Scholar]
- 21. White NP, Borque KA, Jones MH, Williams A. Single-stage revision anterior cruciate ligament reconstruction: experience with 91 patients (40 elite athletes) using an algorithm. Am J Sports Med. 2021;49(2):364–373. [DOI] [PubMed] [Google Scholar]
References
- 22. Winkler PW, Wagala NN, Hughes JD, Lesniak BP, Musahl V. A high tibial slope, allograft use, and poor patient-reported outcome scores are associated with multiple ACL graft failures. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 23. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wright RW, Huston LJ, Haas AK, et al. Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the multicenter ACL revision study (MARS) cohort. Am J Sports Med. 2014;42(10):2301–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 25. Wright RW, Huston LJ, Haas AK, et al. Meniscal repair in the setting of revision anterior cruciate ligament reconstruction: results from the MARS cohort. Am J Sports Med. 2020;48(12):2978–2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 26. Wright RW, Huston LJ, Spindler KP, et al. Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. Am J Sports Med. 2010;38(10):1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 27. Zanovello J, Rosso F, Bistolfi A, Rossi R, Castoldi F. Combined intra- and extra-articular technique in revision anterior cruciate ligament reconstruction. Joints. 2017;5(3):156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 28. Zhu J, Marshall B, Tang X, Linde MA, Fu FH, Smolinski P. ACL graft with extra-cortical fixation rotates around the femoral tunnel aperture during knee flexion. 2022;30(1):116–123. [DOI] [PubMed] [Google Scholar]


